- 1Centre for Pain Research, School of Health, Leeds Beckett University, Leeds, United Kingdom
- 2Mind Help Limited, Durham, United Kingdom
This article explores how paternalistic control and power reside within the family system and how this may influence pain and its persistence. Drawing upon clinical case studies and existing literature, this exploration emphasises the role of paternal dysfunction in creating emotional memory images and delves into how this may influence the chronification and treatment resistance of pain (i.e., making pain “sticky”). We argue that a dysfunctional paternalistic family system, often characterised by authoritarian dynamics, emotional neglect, and abuse, results in adverse experiences and emotional memory images that create a fertile ground for the entrenchment and propagation of psychosomatic symptoms, including pain. Further, the paper emphasizes the potential intergenerational effects of such a scenario, where inherited “Family Rules” drive maladaptive coping mechanisms, which contribute to the persistence of psychological and physiological distress across generations. Understanding these complexities offers new perspectives on treating psychological disorders and their physiological ramifications. It also highlights the urgency of addressing dysfunctional familial dynamics in psychotherapeutic interventions for both immediate and long-term psychophysiological health outcomes.
Introduction
A nurtured child forms the foundation for health, wellbeing, and human development (1). Family strain and dysfunction have a negative impact on the flourishing of a child (2). Childhood adversity is associated with poorer health and the occurrence, severity, and impact of chronic pain in later life (3–9). Chronic pain negatively impacts family dynamics (10–12), and conversely, family strain negatively impacts pain experience (13–16). Chronic pain in parents is associated with non-specific chronic pain in adolescents and young adults (3, 17–21).
Paternalistic system power remains on the periphery of a pain practitioner's clinical practice. Adversity and trauma resulting from paternalistic system power may influence chronification and treatment resistance of pain later in life (i.e., making pain “sticky”). Pain stickiness is a nickname introduced by Borsook et al. (22) to capture numerous social, psychological, and biological factors that influence pain persistence, pain behavior, and resistance to therapeutic intervention. Borsook et al. argued a need for neurobiologically informed psychotherapy, focused on pain as a motivational drive to avoid harm, to assist people in overcoming pain behavior that prevents exploration of possible alternatives to a life with persistent pain. Our perspective is that “Family Rules” causing adversity and trauma produce emotional memory images (EMIs) that may contribute to pain stickiness.
Reviews of the literature provide evidence that internal family systems contribute to chronic pain and treatment outcomes and should be a target for intervention (23–25). In 2023, a systematic review by Nicolson et al. of 68 studies found strong associations between chronic pain in adulthood and a broad range of adverse childhood events including household dysfunction, bullying, living in fear, emotional trauma, and weak parental attachment (9). Nicolson et al. (9) identified 15 different types of adverse childhood experiences, with emotional abuse being common, although there were no studies that specifically investigated childhood adversity through the lens of paternalistic family system power. In this article, we seek to uncover where paternalistic control and power reside within the family system, and how this may influence pain and its persistence.
Family rules, myths, and secrets
Within an open paternalistic system of a family dynamic model/framework, shared responsibility among parents/caregivers allows the child to freely express their fears, hopes, and dreams (26). A closed paternalistic system demands power and control over those within it, creating censorship, isolation, and fear (27, 28). Satir suggested that family members would develop various behavioural strategies termed “Survival Stances” to describe how individuals acted out their roles to “survive,” such as placating, blaming, super-reasonable, and irrelevant (27).
The Family Rule maintains a closed paternalistic system. When a parent (or caregiver) is perceived as uncaring by the child or is caught doing something that they should not be doing, the parent may attempt to suppress the child’s knowledge of the event by explaining that the child has misunderstood the situation. By discrediting the child's understanding of a situation in this way, a parent “saves face,” hiding the event from others and psychologically suppressing the event for the child and the parent. As the child grows older, the experience may be assigned to a myth or kept a secret, following a Family Rule of maintaining silence out of fear of reprisal. It is as if the secret “hangs” in the relationship as an “ever-present noose,” ready to tighten if it should ever be approached (29).
Societal norms that prioritize materialism through a culture of having rather than being contribute to the decline of mental and physical wellbeing, as the focus becomes possessing rather than experiencing (30, 31). When fundamental human needs for autonomy, relationships, security, and purpose are not met, the detrimental effects of materialism become more pronounced (32). Consequently, individuals conditioned to adhere to these norms may favor materialistic remedies such as medication over conversational therapies (33, 34). Thus, we posit a pain patient raised in a closed paternalistic system perpetuating harm and dysfunction via a Family Rule would favor biomedical physicalist or mechanistic explanations for their pain and would seek “physical treatments” for a “physical ailment,” even when they are aware that they have been a casualty of psychological trauma. Speaking out or asking for help from the clinician may be psychologically impossible for the patient, as they may be trapped inside a subconscious Family Rule, which enforces the rule of the dominant family member over the health and wellbeing of the individual. The patient may aggressively or passive-aggressively deny any psychological sensitivity. In contrast, a pain patient raised in an open paternalistic system may present to the clinic able to discuss any emotional factors that may be contributing to their pain.
Family system power—a metaphorical folie à deux?
Here, we use the concept of a folie à deux as a metaphor to enlighten the pain practitioner about the nature of patients who may have a non-conscious Family Rule. Folie à deux is considered a delusional belief system held by two or more individuals within the field of mental illness. In 1860, Jules Baillarger coined the term “folie à communiqué” to describe a shared psychotic disorder, and in 1877, Laségue and Falret coined the phrase “folie à deux” (“madness for two”) to describe a psychotic disorder shared by two people. American psychiatrist Theodore Lidz and his colleagues carefully observed 14 families of people diagnosed with schizophrenia (35–37) and found that behaviors would be shared between the dominant individual (inducer) who would apply rules to the family (induced) (38, 39) but not to themselves, which to the “induced” would appear as an admonition—“Do as I say, not as I do.” The inducer would clearly set themselves up to be seen as a hypocrite, yet the rest of the induced family would suffer punishment if they were to point out that this was the case—“the Emperor has no clothes” (40, 41).
Originally, it was assumed that the primary partner (the inducer) who initiated the delusions had a domineering personality, and the secondary partner (the induced) was generally submissive. This idea has been superseded by the concept of an adaptive mutual delusional system that allows members and partners to identify with each other, channel aggressive drives, and preserve intimacy (42–45). Today, the term folie à deux has been broadened to encompass a delusional belief system concurrently held by two or more individuals, so despite the wording, the disorder is not confined to pairs; it can encompass larger groups, adjusting to “folie à trois,” “folie à famille,” (44) and “folie en société” (46). This is to represent the number of people engulfed in the shared delusion. In psychiatry, a folie à deux is analogous to the “double bind” first proposed by Bateson in 1956 (47), as a miscommunication within a paternalistic relationship that can lead an individual to schizophrenia.
We caution that our use of folie à deux as a metaphor should not be interpreted to imply that pain is a form of psychosis. Our viewpoint is that the Family Rule is a form of miscommunication within a closed paternalistic system, a metaphorical folie à deux and double bind, that is a potent source of EMIs that, in turn, are realized as changes in neurobiology, including neurophysiological sensitization and bioplasticity that contribute to hyperalgesia, allodynia, and “sticky pain” (48). Furthermore, the relationship between cognitive distortions induced by dysfunctional closed paternalistic systems and pain is complex and far wider in scope than simply a shared delusional disorder (29), e.g., to include family system effects on assuming a “sick role” and illness behaviour (49).
Family rules and emotional memory images
Emotional memory images are central to our theory of Split-Second Unlearning and psychophysiological disease. We proposed that adverse, emotionally overwhelming first-time experiences create EMIs (50) defined as “Trauma induced, non-conscious, contiguously formed multimodal mental imagery, which triggers an amnesic, anachronistic, stress response within a split-second” (51). In brief, traumatic events instigate psychophysiological stress responses and the formation of EMIs within very short “split-second” time frames, and these EMIs can be retriggered in daily living “replaying” stress responses, the recurring nature of which results in chronic “disease.” We posit that a Family Rule creates a multimodal EMI resulting from auditory (verbal and non-verbal sounds) and visual cues from the inducer, such as anger, disapproval, and rejection.
The EMI “holds” the unspoken, non-conscious rule, which must be obeyed to prevent severe punishment. The ultimate punishment as an infant may be abandonment by the parent or caregiver (inducer) or the withholding of love and attention (29). Generally, adults can rationalise rejection, whereas cognitive areas of the brain are still developing in children, and therefore, a “primitive” fight–flight–freeze reaction applicable to survival is more likely, i.e., the sense that the situation is “life or death.” In infancy and childhood, fighting or fleeing are implausible options, so freeze responses of hyperarousal or hypoarousal are activated to avoid punishment. Bateson et al. (47) suggest that repeated experiences embed adversity, although we assert that EMIs are a contiguously formed response to a single first-time emotionally overwhelming experience.
The EMI is formed when a child is in a state of heightened vulnerability and is learning to grapple with ambiguity and uncertainty stemming from the parent or caregiver's actions. This “learning” becomes encoded within the EMI. Empirical research into adverse childhood experiences underscores the profound psychophysiological repercussions in adults who endured harm during their formative years (52–55). Hence, the EMI traps the child in a psychological double bind, in which they seek assurance from a figure whose behavior is inconsistent. This predicament may precipitate an intolerance of uncertainty, compelling the individual to eschew scenarios that could trigger the EMI [see (56, 57)].
Activation of a Family Rule results in a non-conscious limbic system sympathetically mediated freeze response. In stressful circumstances that enable fight or flight, stress hormones are produced to mediate energy-consuming physical activity. The freeze response, however, puts the person into a heightened state of “pause,” and the person is held in a perpetual state of hypoarousal, manifesting as withdrawal and avoidance of sensory stimuli. This may explain, at least in part, the sluggishness observed in psychophysiological states of disease including depression, chronic fatigue syndrome (myalgic encephalomyelitis), and chronic primary pain (58). Chronic primary pain is defined as pain associated with significant emotional distress or functional disability that is not better explained by another chronic pain condition and includes non-specific chronic musculoskeletal pains (e.g., low back pain, neck pain), widespread pain, fibromyalgia, and irritable bowel syndrome (58–60).
The Imbalance of Threat and Soothing Systems model, proposed by Pinto et al. (61), corroborates this theory. In the Family Rule scenario, the freeze response is an optimal survival strategy as the induced do not have the fortitude to flee from or fight the perpetrator. Thus, children or vulnerable adults remain subservient. Releasing a person from a state of hypoarousal may enable a person to act out a fight or flight, assisting escape from the freeze response. We posit that the censorship created by the inducer proliferates the delusion, and the threat of neglect or abuse creates an EMI in the “induced,” suppressing their “spirit,” resulting in their silence.
We contend that EMIs facilitate psychophysiological disease through dysregulation of the hypothalamic–pituitary–adrenal (HPA) axis, triggering the stress response that augments physiological processes associated with persistent (primary) pain. Genes influence the response of the HPA axis to traumatic events in early life (e.g., FKBP5 and CRHR1 polymorphisms) (62) and how people respond to experiences in early life (63) and in adulthood (64); this may affect risk for chronification of pain (65). Borsook et al. (22) focused their discussion of the stickiness of pain on the contribution of neurobiological processes to a “stuck pain state”, including stress-induced epigenetic modifications, central sensitization, synaptic plasticity, HPA axis activity, brain circuitry, and opioidergic and dopaminergic tone, and how these may influence vulnerability or resilience to chronification. We advocate exploring the relationship between paternalistic family dynamics and the stickiness of pain at neurobiological and psychological levels, including health anxiety and reinforcement through caregiving behavior by formerly hostile or critical family members.
Previously, we have described a Split-Second Unlearning theory as a therapeutic framework to diagnose and “clear” EMIs created by trauma and adversity (50). Here, we describe how Split-Second Unlearning techniques can be used for clients presenting with trauma and adversity arising from codes of conduct (behavioral rules) imposed on family members by a dominant family member who does not follow the behavioral rules themselves.
Childhood abuse and trauma
There is strong evidence that adverse childhood experiences are associated with mental health disorders and persistent pain later in life (5, 54, 66, 67). Adverse childhood experiences include emotional and physical neglect and sexual, physical, and emotional abuse. Adverse childhood experiences that are created during a child's formative years when the brain is developing, may leave a lasting imprint within the brain structure or, at the very least, an EMI that perpetuates a cascade of molecular and neurobiological effects, which hinders neuronal development (68, 69). This past adversity subsequently becomes the lens through which the child filters their experience of the world around them. This “experience” can develop into psychiatric symptoms like psychosis, aggression, or anxiety, as well as hostile behaviour as non-conscious physiological processes in the brain “hide” the person's awareness (observer) from the perpetual threat (70).
Globally, it has been estimated that up to 1 billion children have suffered abuse within dysfunctional Family Rule structures (71–74), contributing to adversity and the potential for intractable pain later in life (3–5). Previously, we have explored “Past Adversity Influencing Now” (PAIN) through the lens of temporal language and how this may impact the persistence of pain (75). Considering the relationship between hidden Family Rules and PAIN can assist the practitioner in affecting a positive outcome for the patient presenting with persistent pain.
Detecting PAIN in clinical practice
The literature on childhood and preverbal trauma suggests that adverse experiences associated with Family Rules are difficult to identify. This is likely due to the young age at which adversity has taken place, within the child's development, and the nature of the traumatic event, e.g., varying severity of sexual, physical, or psychological abuse.
In 2023, we introduced a framework called PAIN to encourage exploration of pain through a temporal lens, guiding individuals toward a more positive future (75). Our PAIN framework encompassed temporal phases of pain: past perfect, past imperfect, present, future imperfect, and future perfect. We suggested that EMIs may contribute to a future imperfect and “sticky pain.” We described how detecting PAIN requires the practitioner to observe the client's eyes, breathing, voice tonality, and skin tone while completing a case history. The client may not be able to answer obvious questions such as “Were you raped or severely traumatized as a child?” due to the amnesic and anachronistic nature of the EMI formed by the original trauma (51), serving to “keep the family secret safe.”
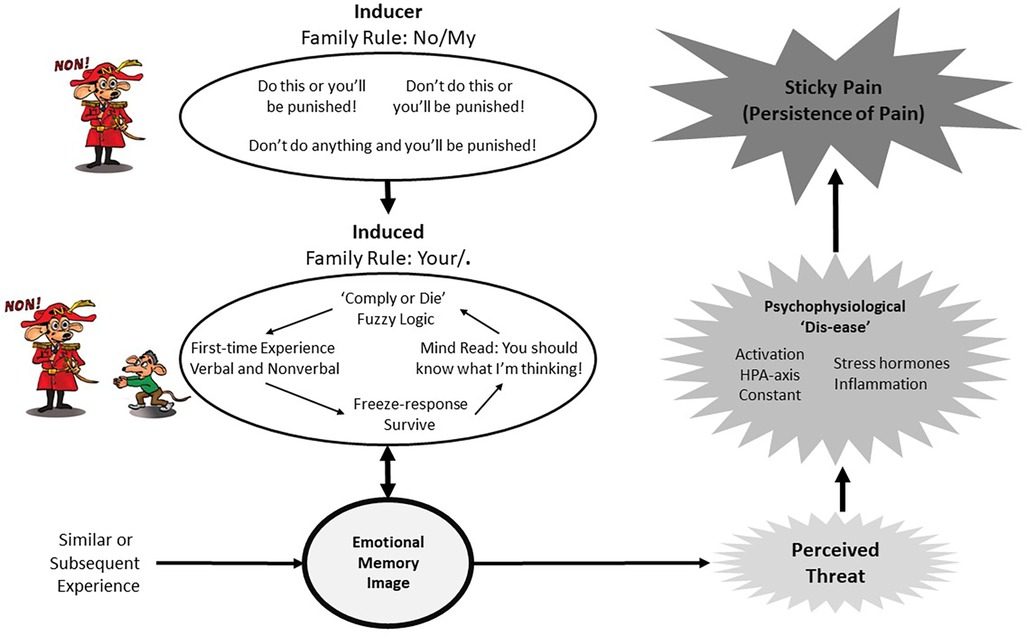
The practitioner can gently coax the client by explaining that EMIs are created via experiences that are emotionally overwhelming at the time. For example, a parent or caregiver yelling at a child playing with a spider, “Don't touch the spider!” produces a fear-induced EMI in the child. Prior to the yell, the child was not afraid of the spider, and the new EMI motivates fear-avoidance reactions to spiders, promoting safety and survival in future encounters. EMIs are created within a dysfunctional paternalistic system, whereby as a child the individual is powerless and complies with the wishes of the “ruler” (inducer), even when illogical, to “survive.” This makes sense to those who are within the paternalistic system but may appear to be “fuzzy logic” to an outsider (see Figure 1). By providing the client with a simple explanation of this process, practitioners “allow” clients more scope to be open to the prospect of having PAIN.
Structure of compliance
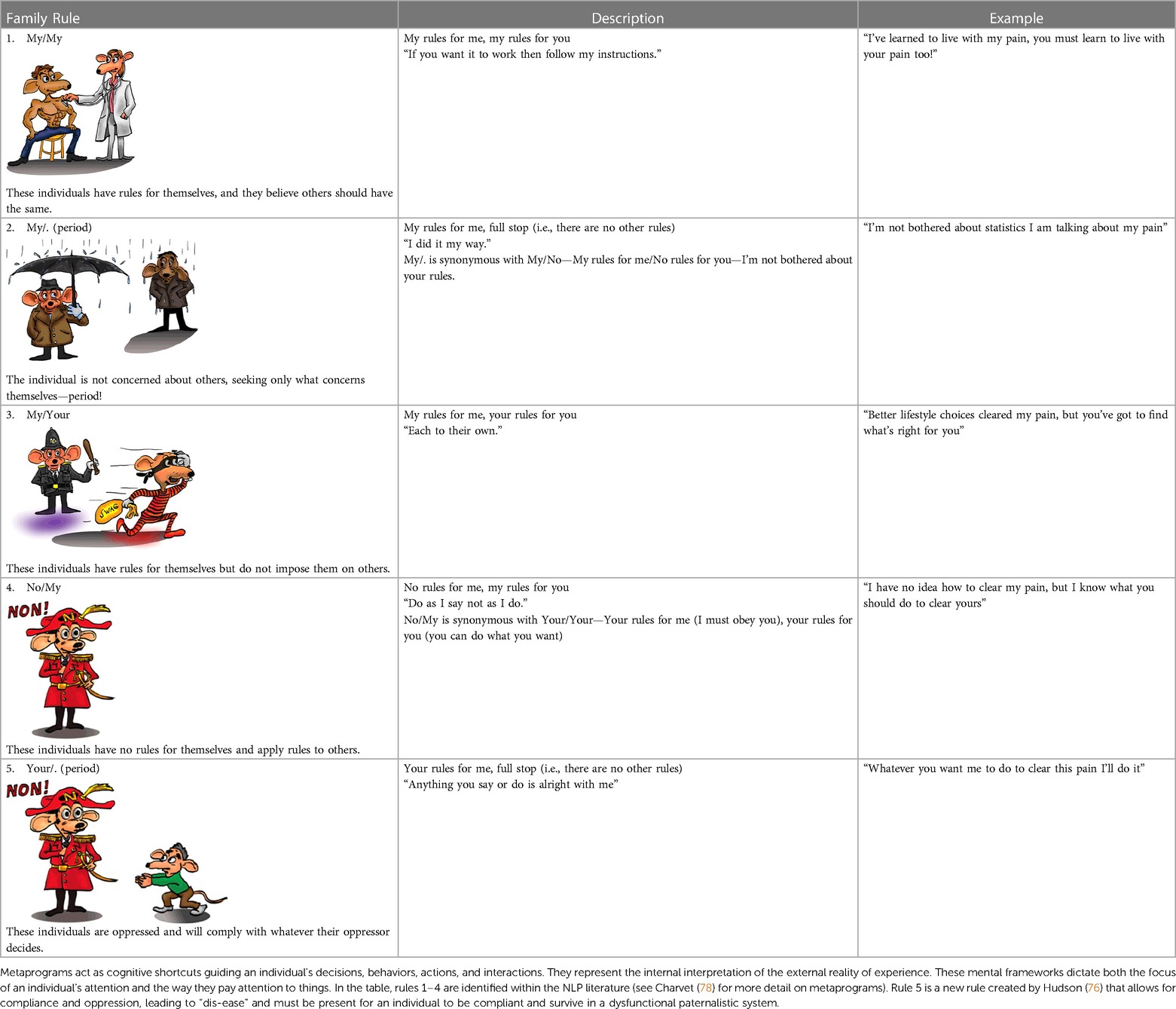
Children are reliant on parents or caregivers as a route to survival. From an evolutionary perspective, children are adapted to promote behaviors that seek alliances with parents or caregivers who provide protection and access to food. Disobeying parents or caregivers may be catastrophic to health and wellbeing, with the possibility of death. Parents or caregivers may impose codes of conduct (behavioral rules) on their children without following the behavioral rules themselves. Neurolinguistic programming (NLP) describes this process from the perspective of the parent or caregiver as a No/My rule structure, i.e., No rules for me/My rules for you. Compliance is the “safest” strategy for a child to “survive” (exist without confrontation) in this rule structure; from the child's perspective (induced), the rule structure is Your/. (period), i.e., your rules for me, full stop—there are no other rules (76). A synopsis of Family Rule structures is provided in Table 1, where the EMI is seen as a psychophysiological heuristic.
Practitioners can incorporate knowledge about Family Rules when using Split-Second Unlearning techniques to “clear” an EMI from a client presenting with bodily pain with no ostensible pathology (e.g., chronic primary pain). PAIN can be revealed via microexpressions that manifest while taking the case history. Making the client aware of their microexpressions (i.e., a biobehavioral marker) indicative of an EMI and engaging the client in a curious exploration of PAIN may be enough to shift their conceptual understanding of their painful condition, opening new opportunities for recovery [further details on these techniques can be found in our previous studies (75, 77)].
Case vignettes
Here, MH uses case vignettes as examples of Split-Second Unlearning to treat PAIN in practice.
Case vignette 1
A 12-year-old girl presented with chronic, widespread, non-specific musculoskeletal pain. The girl had been adopted from an unkempt orphanage in Eastern Europe, where she had been placed by her birth mother. The girl's adoptive mother presented with anxiety regarding her daughter's adoption, and I believed that this anxious tension was translating to her adopted daughter, precipitating musculoskeletal pain. The adoptive mother was diagnosed as having an EMI of her daughter as an infant, resulting in PAIN. As the adoptive mother spoke, both the mother and the daughter sat with their eyes transfixed on the spot within the peripersonal space between them. The mother was encouraged to look through the image of the past and to see her daughter with today's eyes. This action simultaneously cleared the EMI and the Family Rule of compliance; without the EMI, no rule is necessary. Clearing the adoptive mother's EMI reduced all pain from the girl within 30 minutes of treatment. The client was given an appointment for an online follow-up call 1 month later, at which the child reported no recurrence of symptoms; this was maintained at the 2-month, 6-month, and 12-month follow-ups. It is as though the child's pain was acting as a cry for help on behalf of both the mother and child, who were trapped in PAIN.
Case vignette 2
A 15-year-old girl with myalgic encephalomyelitis and chronic widespread non-specific musculoskeletal pain presented to the clinic with her mother. The girl had physically matured early, which her mother reported to be of great concern to her father. The mother reported that the father was lavishing extra attention on the girl to ensure his daughter did not start dating, destabilising the family system. It was suggested to the mother that this may be precipitating her daughter's symptoms while the daughter listened indignantly. It was fascinating to note the mother's eyes were averted, while her daughter's eyes were fixated. Both aversion and fixation are signs of fear. The mother was listening, avoiding looking at her daughter, and her daughter was glaring when the Family Rule was brought to their conscious awareness. This is against the rules! The EMI in this situation is held in place by the Family Rule “Though must obey!”; both are induced, and the EMI oppresses them. The action of naming the source frees all from the rule, including the father, and restabilises the family system. The client was given an appointment for an online follow-up call in 1-month. The mother reported that she had discussed our session with her husband, and the couple had begun spending more time on their relationship. Thus, the father had reduced the overwhelming attention given to his daughter. The daughter's pain and fatigue had diminished greatly. At the 6- and 12-month follow-ups, the daughter reported that she was without pain or fatigue.
Case vignette 3
A 48-year-old woman presented with finger joint pain associated with rheumatoid arthritis that had persisted for the past 3 years. When talking about her past experiences, the client's eyes looked to her left; this was interpreted as an experiential timeline from left (her past) to the right (her future). Interestingly, when the client spoke of her arthritis, her eyes fixated upward and to the right. This was interpreted as indicative of an EMI that was generalizing over time. I described my observations and deductions to the client, who appeared astonished and began to recall a conversation with her mother approximately 35 years earlier. The client explained that her mother had early-onset rheumatoid arthritis at age 45 and had been told that if she had a daughter, the daughter would suffer the same fate. This EMI, created from the conversation with her mother, remained dormant until the client reached 45 years of age. As the client spoke, she displayed a PAIN; her eyes were wide as she appeared detached from the present and fully associated with her EMI of the past. By bringing the EMI to the client's awareness and explaining how her mother's adversity had transferred to her, the EMI cleared, and the client was fully associated with the present once more. At the 1-month follow-up appointment, pain and swelling had diminished, and flexibility had returned to the client's fingers. At the 6- and 12-month follow-ups, there was no recurrence of any pain.
Summary of case vignettes
The case vignettes demonstrate that bodily pain may be driven by PAIN. Attention to PAIN within a framework of Split-Second Unlearning may rapidly resolve bodily pain by clearing an EMI, allowing the HPA axis to return to a prestress state. The vignettes are examples of psychotherapeutic intervention; however, practitioners must appreciate that these clients did not require “talking therapy.” Often, clients are unaware that they are traumatised, either with a capital T or a lowercase t, although they are aware of bodily pain and require help from a practitioner. In vignettes 1 and 2, the parent and child must be present for the Family Rule to be broken or cleared. By gaining new insight into the psychological aspect of pathology, no blame is apportioned to the caregiver, and the EMI is cleared. We concur with Ecker and Vaz (79) that the process of erasure clears any psychophysiological attachment to this emotional learning. In all cases, the Family Rule is the elephant in the room, which will continue to create misery and pain if the practitioner is unable or unwilling to address it.
Closed paternalistic systems and painogenic environments
In a broader context, closed paternalistic systems with the potential for dysfunctional rules, structures, and maladaptive beliefs can operate at various levels in society. This may include idiosyncratic beliefs of an individual, beliefs shared by a few individuals (shared delusions), and beliefs shared by subgroups, subcultures within and between communities, regions, and nations, resulting in, for example, prejudice, discrimination, or dogma. A “collapsing tin can” metaphor describes people living within a “closed-societal system”: A social milieu of threat, fear, and anxiety mediated by complex societal structures, settings, and narratives compresses the mental wellbeing of individuals, creating a closed societal system, like high atmospheric pressure compressing the walls of a tin can with a low-pressure interior. Forces producing this constraining milieu may be insidious and invisible to individuals (32, 80, 81). Individuals utilize a variety of strategies for existing and surviving within the pressure of the closed system. Psychophysiological disease may be a consequence and/or a survival strategy of being immersed in insidious macrolevel forces. This promotes the rise in mental illness and non-communicable diseases, including chronic primary pain, chronic fatigue syndrome, depression, generalised anxiety, and so on (82).
Societal settings creating closed systems operating within a No/My authoritarian rule structure (i.e., No rules for me/My rules for you) may fall foul of groupthink. Groupthink is when no one will challenge the thoughts of a group and people just go along blindly obeying in a Your rules for me/full stop fashion (i.e., Your/.).
“They are playing a game. They are playing at not playing a game. If I show them I see they are, I shall break the rules and they will punish me. I must play their game, of not seeing I see the game” (83, p. 1).
We contend that a dominant biomedical groupthink may be detrimental to alleviating the societal burden of chronic pain, leading to personal suffering. Insights may be gained by exploring dysfunctional paternalistic systems within the socio-ecological framework of painogenicity (84). The concept of painogenicity provides a socio-ecological framework to explore the persistence of pain (84, 85). Painogenicity is the sum of influences that the surroundings, opportunities, or conditions of life have on promoting persistent pain in individuals or populations, encompassing micro-, meso-, and macrolevel factors (85, 86). Macrolevel factors such as built or natural habitats, geopolitics, and economic sectors are often neglected in models of pain, despite their potential to foster a social milieu of threat, fear, and anxiety through illness narratives of pain grounded in tissue damage, pathological causation, and warmongering of biomedical remedy (80, 87).
Increasingly, scholars argue that biomedicalisation of mental health conditions and chronic (primary) pain has perpetuated rather than diminished the burden of disease (32, 88). No doubt, biomedical remedy assists resolution of episodes of pain in many people, some of the time, although the global burden of persistent pain remains high irrespective of a country's social and economic development and despite ever-increasing varieties of treatment (89–91). We advocate exploration of this treatment-prevalence paradox through the lens of a closed paternalistic biomedical system to deepen an understanding of socio-ecological factors influencing the persistence of pain and other intractable non-communicable diseases, including mental illness.
Conclusion
In this article, we describe how dysfunctional family structures may lead to Family Rules resulting in PAIN and EMIs that contribute to the persistence (stickiness) of bodily pain. We describe a Split-Second Unlearning approach to “clear” EMIs and unblock the detrimental effects of PAIN, with the potential for a “healing journey” toward recovery from persistent pain (92). We position this approach within a salutogenic framework of care (93) that may be more successful than biomedical interventions in “unsticking” pain.
We conclude that exploring pain and its persistence within a dysfunctional paternalistic context could deepen an understanding of factors contributing to chronification and treatment resistance and may provide opportunities to assist people on a “healing journey”. Emphasizing a holistic, socio-ecological model of pain encourages healthcare practitioners to think beyond traditional diagnoses and treatment strategies. In this regard, consideration of the influence of family dynamics and psychosocial factors on a person's experience of persistent pain may improve intervention strategies and potentially break intergenerational cycles of disease.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
MH: Conceptualization, Writing – original draft, Writing – review & editing. MJ: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors thank Lisa Mcloughlin, co-founder of Mind Help Limited, for providing constructive feedback on drafts of the manuscript.
Conflict of interest
MH is the co-founder and co-creator of the MindReset app, which is supported by individual subscribers. In the previous 5 years, MJ's employer has received income for expert consultancy activities from GSK, TENSCare, and LifeCare Ltd. that lie outside the submitted work. MJ declares book royalties from Oxford University Press. MH was employed by Mind Help Limited.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Clark H, Coll-Seck AM, Banerjee A, Peterson S, Dalglish SL, Ameratunga S, et al. A future for the world’s children? A WHO-UNICEF-Lancet commission. Lancet. (2020) 395(10224):605–58. doi: 10.1016/S0140-6736(19)32540-1
2. Westphaln KK, Lee E, Fry-Bowers EK, Kleinman LC, Ronis SD. Examining child flourishing, family resilience, and adversity in the 2016 national survey of children’s health. J Pediatr Nurs. (2022) 66:57–63. doi: 10.1016/j.pedn.2022.05.014
3. Hoftun GB, Romundstad PR, Rygg M. Association of parental chronic pain with chronic pain in the adolescent and young adult: family linkage data from the hunt study. JAMA Pediatr. (2013) 167(1):61–9. doi: 10.1001/jamapediatrics.2013.422
4. Zadro JR, Nilsen TIL, Shirley D, Amorim AB, Ferreira PH, Mork PJ. Parental chronic widespread pain and the association with chronic widespread pain in adult offspring: family-linkage data from the Norwegian hunt study. Eur J Pain. (2018) 22(8):1485–93. doi: 10.1002/ejp.1237
5. Lumley MA, Yamin JB, Pester BD, Krohner S, Urbanik CP. Trauma matters: psychological interventions for comorbid psychosocial trauma and chronic pain. Pain. (2022) 163(4):599–603. doi: 10.1097/j.pain.0000000000002425
6. Davis DA, Luecken LJ, Zautra AJ. Are reports of childhood abuse related to the experience of chronic pain in adulthood? A meta-analytic review of the literature. Clin J Pain. (2005) 21(5):398–405. doi: 10.1097/01.ajp.0000149795.08746.31
7. Paras ML, Murad MH, Chen LP, Goranson EN, Sattler AL, Colbenson KM, et al. Sexual abuse and lifetime diagnosis of somatic disorders: a systematic review and meta-analysis. JAMA. (2009) 302(5):550–61. doi: 10.1001/jama.2009.1091
8. Yavne Y, Amital D, Watad A, Tiosano S, Amital H. A systematic review of precipitating physical and psychological traumatic events in the development of fibromyalgia. Semin Arthritis Rheum. (2018) 48(1):121–33. doi: 10.1016/j.semarthrit.2017.12.011
9. Nicolson KP, Mills SEE, Senaratne DNS, Colvin LA, Smith BH. What is the association between childhood adversity and subsequent chronic pain in adulthood? A systematic review. BJA Open. (2023) 6:100139. doi: 10.1016/j.bjao.2023.100139
10. Boone D, Kim SY. Family strain, depression, and somatic amplification in adults with chronic pain. Int J Behav Med. (2019) 26(4):427–36. doi: 10.1007/s12529-019-09799-y
11. Benjamin JZ, Harbeck-Weber C, Sim L. Pain is a family matter: quality of life in mothers and fathers of youth with chronic pain. Child Care Health Dev. (2019) 45(3):440–7. doi: 10.1111/cch.12662
12. de Sola H, Salazar A, Duenas M, Ojeda B, Failde I. Nationwide cross-sectional study of the impact of chronic pain on an individual’s employment: relationship with the family and the social support. BMJ Open. (2016) 6(12):e012246. doi: 10.1136/bmjopen-2016-012246
13. Woods SB, Roberson PNE, Abdelkhaleq H. Family strain, but not family support, is linked to worse pain interference among midlife adults reporting new chronic pain. Fam Syst Health. (2023). doi: 10.1037/fsh0000825
14. Saito T, Shibata M, Hirabayashi N, Honda T, Morisaki Y, Anno K, et al. Family dysfunction is associated with chronic pain in a community-dwelling Japanese population: the Hisayama study. Eur J Pain. (2023) 27(4):518–29. doi: 10.1002/ejp.2076
15. Hayaki C, Anno K, Shibata M, Iwaki R, Kawata H, Sudo N, et al. Family dysfunction: a comparison of chronic widespread pain and chronic localized pain. Medicine (Baltimore). (2016) 95(49):e5495. doi: 10.1097/MD.0000000000005495
16. Signs TL, Woods SB. Linking family and intimate partner relationships to chronic pain: an application of the biobehavioral family model. Fam Syst Health. (2020) 38(1):38–50. doi: 10.1037/fsh0000459
17. Roth-Isigkeit A, Thyen U, Stoven H, Schwarzenberger J, Schmucker P. Pain among children and adolescents: restrictions in daily living and triggering factors. Pediatrics. (2005) 115(2):e152–62. doi: 10.1542/peds.2004-0682
18. Petersen S, Brulin C, Bergstrom E. Recurrent pain symptoms in young schoolchildren are often multiple. Pain. (2006) 121(1–2):145–50. doi: 10.1016/j.pain.2005.12.017
19. Hoftun GB, Romundstad PR, Zwart JA, Rygg M. Chronic idiopathic pain in adolescence—high prevalence and disability: the young HUNT study 2008. Pain. (2011) 152(10):2259–66. doi: 10.1016/j.pain.2011.05.007
20. King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, et al. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain. (2011) 152(12):2729–38. doi: 10.1016/j.pain.2011.07.016
21. Koechlin H, Beeckman M, Meier AH, Locher C, Goubert L, Kossowsky J, et al. Association of parental and adolescent emotion-related factors with adolescent chronic pain behaviors. Pain. (2022) 163(7):e888–98. doi: 10.1097/j.pain.0000000000002508
22. Borsook D, Youssef AM, Simons L, Elman I, Eccleston C. When pain gets stuck: the evolution of pain chronification and treatment resistance. Pain. (2018) 159(12):2421–36. doi: 10.1097/j.pain.0000000000001401
23. Payne B, Norfleet MA. Chronic pain and the family: a review. Pain. (1986) 26(1):1–22. doi: 10.1016/0304-3959(86)90169-7
24. Lewandowski W, Morris R, Draucker CB, Risko J. Chronic pain and the family: theory-driven treatment approaches. Issues Ment Health Nurs. (2007) 28(9):1019–44. doi: 10.1080/01612840701522200
25. Lewandowski AS, Palermo TM, Stinson J, Handley S, Chambers CT. Systematic review of family functioning in families of children and adolescents with chronic pain. J Pain. (2010) 11(11):1027–38. doi: 10.1016/j.jpain.2010.04.005
26. Lau WK-W, Leung PP-Y, Chung CL-P. Effects of the Satir model on mental health: a randomized controlled trial. Res Soc Work Pract. (2019) 29(7):775–85. doi: 10.1177/1049731518819829
28. Banmen J. The Satir model: yesterday and today. Contemp Fam Ther. (2002) 24(1):7–22. doi: 10.1023/A:1014365304082
29. Bowlby J. On knowing what you are not supposed to know and feeling what you are not supposed to feel. Can J Psychiatry. (1979) 24(5):403–8. doi: 10.1177/070674377902400506
31. Dittmar H, Bond R, Hurst M, Kasser T. The relationship between materialism and personal well-being: a meta-analysis. J Pers Soc Psychol. (2014) 107(5):879–924. doi: 10.1037/a0037409
32. Davies J. Sedated. How modern capitalism created our mental health crisis. London: Atlantic Books (2022).
33. Khalsa SR, McCarthy KS, Sharpless BA, Barrett MS, Barber JP. Beliefs about the causes of depression and treatment preferences. J Clin Psychol. (2011) 67(6):539–49. doi: 10.1002/jclp.20785
34. Kimerling R, Calhoun KS. Somatic symptoms, social support, and treatment seeking among sexual assault victims. J Consult Clin Psychol. (1994) 62(2):333–40. doi: 10.1037//0022-006x.62.2.333
35. Lidz RW, Lidz T. The family environment of schizophrenic patients. Am J Psychiatry. (1949) 106(5):332–45. doi: 10.1176/ajp.106.5.332
36. Lidz T, Cornelison AR, Fleck S, Terry D. The intrafamilial environment of the schizophrenic patient. I. The father. Psychiatry. (1957) 20(4):329–42. doi: 10.1080/00332747.1957.11023099
37. Lidz T, Fleck S, Cornelison A, Terry D. The intrafamilial environment of the schizophrenic patient. IV. Parental personalities and family interaction. Am J Orthopsychiatry. (1958) 28(4):764–76. doi: 10.1111/j.1939-0025.1958.tb03991.x
38. Lasègue EC, Falret J. La folie À deux (ou folie communiquee). Dialogues Philos Ment Neuro Sci. (2016) 9(2):62–8.
40. Lidz T, Cornelison AR, Fleck S, Terry D. The intrafamilial environment of schizophrenic patients. II. Marital schism and marital skew. Am J Psychiatry. (1957) 114(3):241–8. doi: 10.1176/ajp.114.3.241
41. Hahlweg K, Baucom DH. Family therapy for persons with schizophrenia: neglected yet important. Eur Arch Psychiatry Clin Neurosci. (2023) 273(4):819–24. doi: 10.1007/s00406-022-01393-w
42. Balducci PM, Gobbicchi C, Moretti P, Tortorella A. Delusional sharing: a history focus-on and case report of folie a deux. Riv Psichiatr. (2017) 52(4):168–71. doi: 10.1708/2737.27910
43. Shimizu M, Kubota Y, Toichi M, Baba H. Folie a deux and shared psychotic disorder. Curr Psychiatry Rep. (2007) 9(3):200–5. doi: 10.1007/s11920-007-0019-5
44. Srivastava A, Borkar HA. Folie a famille. Indian J Psychiatry. (2010) 52(1):69–70. doi: 10.4103/0019-5545.58899
45. Loh YL, Wong HK. Folie a famille—a case report of three sisters. East Asian Arch Psychiatry. (2007) 17:64–6.
47. Bateson G, Jackson DD, Haley J, Weakland J. Toward a theory of schizophrenia. Behav Sci. (1956) 1(4):251–64. doi: 10.1002/bs.3830010402
48. You DS, Meagher MW. Childhood adversity and pain sensitization. Psychosom Med. (2016) 78(9):1084–93. doi: 10.1097/PSY.0000000000000399
49. Petroni FA. Preferred right to the sick role and illness behavior. Soc Sci Med (1967). (1971) 5(6):645–53. doi: 10.1016/0037-7856(71)90014-x
50. Hudson M, Johnson MI. Split-Second unlearning: developing a theory of psychophysiological disease. Front Psychol. (2021) 12:716535. doi: 10.3389/fpsyg.2021.716535
51. Hudson M, Johnson MI. Definition and attributes of the emotional memory images underlying psychophysiological disease. Front Psychol. (2022) 13:947952. doi: 10.3389/fpsyg.2022.947952
52. Herzog JI, Schmahl C. Adverse childhood experiences and the consequences on neurobiological, psychosocial, and somatic conditions across the lifespan. Front Psychiatry. (2018) 9:420. doi: 10.3389/fpsyt.2018.00420
53. Hughes K, Ford K, Bellis MA, Glendinning F, Harrison E, Passmore J. Health and financial costs of adverse childhood experiences in 28 European countries: a systematic review and meta-analysis. Lancet Public Health. (2021) 6(11):e848–57. doi: 10.1016/S2468-2667(21)00232-2
54. Antoniou G, Lambourg E, Steele JD, Colvin LA. The effect of adverse childhood experiences on chronic pain and major depression in adulthood: a systematic review and meta-analysis. Br J Anaesth. (2023) 130(6):729–46. doi: 10.1016/j.bja.2023.03.008
55. Tidmarsh LV, Harrison R, Ravindran D, Matthews SL, Finlay KA. The influence of adverse childhood experiences in pain management: mechanisms, processes, and trauma-informed care. Front Pain Res (Lausanne). (2022) 3:923866. doi: 10.3389/fpain.2022.923866
56. Boswell JF, Thompson-Hollands J, Farchione TJ, Barlow DH. Intolerance of uncertainty: a common factor in the treatment of emotional disorders. J Clin Psychol. (2013) 69(6):630–45. doi: 10.1002/jclp.21965
57. Wu S, Sun S, Camilleri JA, Eickhoff SB, Yu R. Better the devil you know than the devil you don't: neural processing of risk and ambiguity. Neuroimage. (2021) 236:118109. doi: 10.1016/j.neuroimage.2021.118109
58. World Health Organisation. ICD-11: International classification of diseases (11th revision). Geneve, Switzerland: WHO Press - World Health Organization (2019).
59. Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the International Classification of Diseases (icd-11). Pain. (2019) 160(1):19–27. doi: 10.1097/j.pain.0000000000001384
60. Nicholas M, Vlaeyen JWS, Rief W, Barke A, Aziz Q, Benoliel R, et al. The IASP classification of chronic pain for icd-11: chronic primary pain. Pain. (2019) 160(1):28–37. doi: 10.1097/j.pain.0000000000001390
61. Pinto AM, Geenen R, Wager TD, Lumley MA, Hauser W, Kosek E, et al. Emotion regulation and the salience network: a hypothetical integrative model of fibromyalgia. Nat Rev Rheumatol. (2023) 19(1):44–60. doi: 10.1038/s41584-022-00873-6
62. Lessard J, Holman EA. FKBP5 and CRHR1 polymorphisms moderate the stress-physical health association in a national sample. Health Psychol. (2014) 33(9):1046–56. doi: 10.1037/a0033968
63. Binder EB, Bradley RG, Liu W, Epstein MP, Deveau TC, Mercer KB, et al. Association of FKBP5 polymorphisms and childhood abuse with risk of posttraumatic stress disorder symptoms in adults. JAMA. (2008) 299(11):1291–305. doi: 10.1001/jama.299.11.1291
64. Bortsov AV, Smith JE, Diatchenko L, Soward AC, Ulirsch JC, Rossi C, et al. Polymorphisms in the glucocorticoid receptor co-chaperone FKBP5 predict persistent musculoskeletal pain after traumatic stress exposure. Pain. (2013) 154(8):1419–26. doi: 10.1016/j.pain.2013.04.037
65. Holliday KL, McBeth J. Recent advances in the understanding of genetic susceptibility to chronic pain and somatic symptoms. Curr Rheumatol Rep. (2011) 13(6):521–7. doi: 10.1007/s11926-011-0208-4
66. Runyan D, Wattam C, Ikeda R, Hassan F, Ramiro L. Child abuse and neglect by parents and other caregivers. In: Krug EGDJ, Mercy AB, Lozano Z, Lozano R, editors. World report on violence and health. Geneve, Switzerland: World Health Organization (2002). p. 57–86.
67. Brown RC, Plener PL, Braehler E, Fegert JM, Huber-Lang M. Associations of adverse childhood experiences and bullying on physical pain in the general population of Germany. J Pain Res. (2018) 11:3099–108. doi: 10.2147/JPR.S169135
68. De Bellis MD, Keshavan MS, Clark DB, Casey BJ, Giedd JN, Boring AM, et al. A.E. Bennett research award. Developmental traumatology. Part II: brain development. Biol Psychiatry. (1999) 45(10):1271–84. doi: 10.1016/s0006-3223(99)00045-1
69. De Bellis MD, Baum AS, Birmaher B, Keshavan MS, Eccard CH, Boring AM, et al. A.E. Bennett research award. Developmental traumatology. Part I: biological stress systems. Biol Psychiatry. (1999) 45(10):1259–70. doi: 10.1016/s0006-3223(99)00044-x
70. Teicher MH. Scars that won't heal: the neurobiology of child abuse. Sci Am. (2002) 286(3):68–75. doi: 10.1038/scientificamerican0302-68
71. Hillis SD, Mercy JA, Saul JR. The enduring impact of violence against children. Psychol Health Med. (2017) 22(4):393–405. doi: 10.1080/13548506.2016.1153679
72. van Der Kolk B, Ford JD, Spinazzola J. Comorbidity of developmental trauma disorder (DTD) and post-traumatic stress disorder: findings from the DTD field trial. Eur J Psychotraumatol. (2019) 10(1):1562841. doi: 10.1080/20008198.2018.1562841
73. Moody G, Cannings-John R, Hood K, Kemp A, Robling M. Establishing the international prevalence of self-reported child maltreatment: a systematic review by maltreatment type and gender. BMC Public Health. (2018) 18(1):1164. doi: 10.1186/s12889-018-6044-y
74. Lee H, Kim E. Global prevalence of physical and psychological child abuse during COVID-19: a systematic review and meta-analysis. Child Abuse Negl. (2023) 135:105984. doi: 10.1016/j.chiabu.2022.105984
75. Hudson M, Johnson MI. Past adversity influencing now (pain): perspectives on the impact of temporal language on the persistence of pain. Front Pain Res. (2023) 4:1244390. doi: 10.3389/fpain.2023.1217721
76. Hudson M. Family rules okay: becoming whole without the need for approval. (2023). p. 216. https://www.amazon.co.uk/Family-Rules-Okay-Becoming-Approval/dp/1838495118
77. Hudson M, Johnson MI. Perspectives on emotional memory images and the persistence of pain. Front Pain Res. (2023) 4:1217721. doi: 10.3389/fpain.2023.1217721
78. Charvet SR. Words that change minds: the 14 patterns for mastering the language of influence. 3rd edn. Wilmington, DE: Bloomanity LLC. (2019).
79. Ecker B, Vaz A. Memory reconsolidation and the crisis of mechanism in psychotherapy. New Ideas Psychol. (2022) 66:100945. doi: 10.1016/j.newideapsych.2022.100945
80. Johnson MI, Bonacaro A, Georgiadis E, Woodall J. Reconfiguring the biomedical dominance of pain: time for alternative perspectives from health promotion? Health Promot Int. (2022) 37(4):1–9. doi: 10.1093/heapro/daac128
81. Sik D. Power from indirect pain: a historical phenomenology of medical pain management. Cont Philos Rev. (2021) 54:41–59. doi: 10.1007/s11007-020-09518-5
82. World Health Organisation. Noncommunicable diseases. Geneve, Switzerland: World Health Organization (2023). Available at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases.
84. Johnson MI. Opinions on paleolithic physiology living in painogenic environments: changing the perspective through which we view chronic pain. Pain Manag. (2019) 9(3):219–24. doi: 10.2217/pmt-2018-0095
85. Johnson MI, Woodall J. A healthy settings approach to addressing painogenic environments: new perspectives from health promotion. Front Pain Res. (2022) 3:1000170. doi: 10.3389/fpain.2022.1000170
86. Zimmer Z, Fraser K, Grol-Prokopczyk H, Zajacova A. A global study of pain prevalence across 52 countries: examining the role of country-level contextual factors. Pain. (2022) 163(9):1740–50. doi: 10.1097/j.pain.0000000000002557
87. Johnson MI, Hudson M, Ryan CG. Perspectives on the insidious nature of pain metaphor: we literally need to change our metaphors. Front Pain Res. (2023) 4:1224139. doi: 10.3389/fpain.2023.1224139
88. Scull A. American psychiatry in the new millennium: a critical appraisal. Psychol Med. (2021) 51(16):2762–70. doi: 10.1017/S0033291721001975
89. Elzahaf RA, Tashani OA, Unsworth BA, Johnson MI. The prevalence of chronic pain with an analysis of countries with a human development index less than 0.9: a systematic review without meta-analysis. Curr Med Res Opin. (2012) 28(7):1221–9. doi: 10.1185/03007995.2012.703132
90. GBD 2019 BBoDC. The burden of diseases and risk factors in Bangladesh, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Global Health. (2023) 11:e1931–42. doi: 10.1016/S2214-109X(23)00432-1
91. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396(10258):1204–22. doi: 10.1016/S0140-6736(20)30925-9
92. Toye F, Belton J, Hannink E, Seers K, Barker K. A healing journey with chronic pain: a meta-ethnography synthesizing 195 qualitative studies. Pain Med. (2021) 22(6):1333–44. doi: 10.1093/pm/pnaa373
Keywords: family, family rule, pain, folie à deux, dysfunctional paternalistic system, painogenicity, emotional memory image (EMI), Split-Second Unlearning
Citation: Hudson M and Johnson MI (2023) Hidden family rules: perspective on a dysfunctional paternalistic system and the persistence of pain. Front. Pain Res. 4:1303853. doi: 10.3389/fpain.2023.1303853
Received: 28 September 2023; Accepted: 22 November 2023;
Published: 14 December 2023.
Edited by:
Maral Tajerian, Queens College (CUNY), United StatesReviewed by:
Ravi Philip Rajkumar, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), India© 2023 Hudson and Johnson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mark I. Johnson bS5qb2huc29uQGxlZWRzYmVja2V0dC5hYy51aw==
 Matt Hudson
Matt Hudson Mark I. Johnson
Mark I. Johnson