- 1School of Social Sciences and Humanities, University of Suffolk, Ipswich, United Kingdom
- 2Centre for Pain Research, School of Health, Leeds Beckett University, Leeds, United Kingdom
In this perspective paper, we argue for incorporating personal narratives in positive psychology interventions for chronic pain. Narratives refer to the telling and retelling of events. Narratives detail accounts of events and provide rich, in-depth information on human interactions, relationships, and perspectives. As such, narratives have been used to understand people’s experiences with pain and pain coping mechanisms—as well as to facilitate therapeutic outcomes. Furthermore, narrative research has shown that narration can help restore and promote relief, calm, hope, self-awareness, and self-understanding in chronic pain sufferers. Positive psychology interventions have been successful in improving the lives of people living with chronic pain, but these psychology interventions do not typically incorporate personal narratives. Still, narrative, and positive psychology scholarship foci overlap, as both aim to enhance people’s quality of life, happiness, and well-being, and to promote the understanding of psychosocial strengths and resources. In this article, we provide a rationale for incorporating personal narratives as an agentic form of positive psychology intervention. To that aim, we outline areas of convergence between positive psychology and narrative research and show how combining positive psychology exercises and narration can have additive benefits for pain sufferers. We also show how integrating narration in positive psychology intervention research can have advantages for healthcare research and policy.
Introduction
Chronic (persistent or long-standing) pain is defined by the World Health Organisation and by the International Association for the Study of Pain as pain persisting or recurring for longer than 3 months (1, 2). It is estimated to affect more than 20% of the adult population contributing significantly to the global burden of disease with significant impact on mortality and disability across human societies worldwide (3). Chronic pain is associated with reduced functional capacity, low sense of wellbeing, impaired social interactions, medication over-prescription, illegal substance use and abuse, mood disorders, suicidal ideation and suicide attempts; this results in low quality of life (4).
It is widely acknowledged that a multidisciplinary person-centred biopsychosocial approach using pharmacotherapy, restorative therapies, behavioural treatments, complementary and integrative therapies, and self-care is optimal to manage chronic pain (5). It is recommended that safe, less invasive treatments should be indicated first (5–8), yet biomedical interventions (i.e., surgical and pharmacological) still dominate clinical practice, despite evidence of unfavourable risk benefit profiles (5, 9, 10).
The biopsychosocial model of pain, evolved from Melzack and Wall’s theory of pain (11) and Engel’s new model for medicine (12) over 40 years ago [for a historical account see (13)]. The biopsychosocial model describes a dynamic interaction of biological (e.g., tissue injury, genetics, neurobiology, sex differences, physical health conditions), psychological (e.g., thoughts, beliefs, attitudes, emotions, coping patterns), and social (e.g., poverty, access to welfare, stigma, discrimination) influences to explain between and within person variability in pain experience, including cognitive appraisal of symptoms. Biopsychological approaches to the management of pain are incorporated within an interdisciplinary model of care, emphasizing holistic patient-centred strategies, that combine pharmacotherapy, physical therapy, cognitive-behavioural counselling and other psychotherapeutic modalities, progressive muscle relaxation, risk-reduction training, biofeedback training, social support groups and networking (14, 15).
In this article, we explore the psychological aspect of the biopsychosocial model of pain and advocate the inclusion of personal narratives as part of psychological interventions used in chronic pain management. Specifically, we advocate a positive psychology approach to personal narration and outline areas of convergence between positive psychology and narrative research. We show how combining positive psychology techniques and narration can have synergistic benefits for pain sufferers, and how narration can have advantages for healthcare research and policy.
Personal narratives and healthcare
Narratives are personal stories through which humans tell and retell events (16). Narratives describe events but also become part of the events. Narratives merge with the narrator’s reality but may not be accurate depictions of events and may or may not be linear in time and place. Narratives provide rich, in-depth insights on human experiences, interactions, relationships, and behaviours; they are a tool for sense-making and meaning-making (17).
In recent years narrative literature in healthcare has been used to gain insight to the attitudes of individuals about treatments, therapy, barriers preventing treatment, and unaddressed means for enhancing overall quality of life (18). Research evidence suggests short/medium term benefit of using narrative as part of therapy and there are calls for narrative to be included in health care policies (19, 20).
Therapeutically, personal narratives have been shown to support personal values, identity formation, positive emotions, resilience and purpose (21). For example, encountering a negative event such as a life-threatening diagnosis, can turn into a positive story of experiencing redemption via personal courage and realisation of deeper meaning and a new purpose in life. This can increase self-worth and resilience (22, 23).
Personal narratives and pain management
Pain is a private, complex, organic, multidimensional experience that is idiosyncratic in nature (24, 25). People living with persistent pain experience difficulties constructing meaningful explanations for their pain and suffering (26, 27). People struggle to articulate their personal pain story in a way that is understood, heard, or taken seriously by others, including health care professionals (28–31). In clinical consultation, patients are often forced to express pain through assessment tools that collapse the multi-faceted nature of pain into simplified generalisations or into individual, disconnected, items that fragment pain experience (31). Being unable to express pain through personal narrative results in decontextualise care that is detrimental to health and well-being (32).
Human social groups bond through gossiping and storytelling (33, 34). The act of storytelling personally significant events and contemplating towards lessons learnt and future actions, confers benefit for people living with chronic pain (35). Evidence suggests that personal narrations can improve wellbeing when linked to positive expectations of longer-term recovery, such as relief from pain and improvement in functioning (36). An appraisal of the value of personal story for people living with chronic pain by Hovey et al. suggested that narratives help people interpret their pain and their new lived experience with pain (37). Personal narratives with optimistic content have been associated with beneficial outcomes including enhanced psychological states such as acceptance of areas beyond personal control, positive reinforcement, progress to new achievements, new personal meaning, and motivation to continue exercise, which improve health, well-being and quality of life (35, 38).
Positive psychology for pain management
Equally, recent findings support the ability of positive psychology interventions to improve quality of life and the severity and impact of pain. The operational mechanism of positive psychology intervention is relatively simple. During pain, negative emotions may exist to instigate behaviours to protect tissue from actual or potential harm (39). However, adhering to action preventing negative emotions may exacerbate negative thinking and destructive behavioural patterns (i.e., heightened worry and avoidance of movement), with pain becoming chronic and increasingly devastating (40). Engaging in frequent positive psychology exercises seems to offset the links between pain and negative emotions (e.g., fear, anxiety and sadness) and cognitions (e.g., rumination, worry, helplessness and catastrophising), eliciting positive sentiments instead (41).
A systematic review of 16 RCTs by Braunwalder et al. (42) provides tentative evidence that positive psychology interventions, delivered as online self-help or guided face-to-face interventions are efficacious to alleviate chronic pain. Thus, simple, regular, positive psychology exercises, may help to reduce the severity and impact of chronic pain. Examples of positive exercises that encourage strengthening and enjoyment of social connections and human relationships to improve perceived pain, emotional states and physical function include performing good deeds to other people, reflecting on blessings, appreciating life circumstances, feeling grateful, and pursuing meaningful and significant goals in daily living (42, 43).
Positive psychology interventions aiming to alleviate chronic pain and its consequences in daily living are usually delivered online and asynchronously (without the presence of a specialist) providing a cost-effective technique (42). Successful implementation requires participants to dedicate personal time and effort to execute these exercises repetitively, based on self-selected pace and personal understanding.
Practitioners define the nature of the intervention to meet desired outcomes (i.e., improved social connection), although sometimes participants are given an opportunity to select which type of positive psychology technique they wish to use (44). For example, in a study by Muller et al. (43) participants had the option to engage in one or more of four types of positive psychology exercises; relationships, kindness, gratitude, optimism. Through this methodology design, autonomy of choosing a positive psychology exercise seems to be enhanced. Positive psychology intervention seems contrary to the concept of “agency” as defined by Seligman (45). Seligman (45) defines agency as the power behind each person’s belief that can change the world, or more precisely here, change an individual’s sense making of the world. Agency relates to the efficacy to act, based on self-defined criteria, with optimism and inspiration being integral to the will to control one’s own fate irrespective of life’s adversities (45). Clearly, agency requires personal freedom to implement self-defined priorities in one’s life. Such degree of freedom seems to be missing from existing positive psychology techniques aiming to support wellbeing indices in chronic pain. This is based on the philosophical, epistemological and practical background of positive psychology, which can be significantly enriched with an emphasis on agency and personal responsibility (46).
Personal narratives in positive psychology interventions to manage pain
We advocate the use of personal narratives as an innovative positive psychology technique through protocols that support personal agency and autonomy for the participants. Positive psychology interventions provide encouraging results when used for people living with chronic pain (42), and this is achieved by improving components of the Positive emotions, Engagement, valued/supported Relationships, Meaningfulness and Achievement (PERMA) model (47). Personal narratives empower individuals with greater ownership of the direction, pace and content of sense making through exploration of personal memories, that make autobiographical sense, through the realisation of dispositional traits and how these may adapt under current circumstances. Hence, personal narratives define identity in various ways but most importantly, via the capacity to keep a unique agentic and personally-defined narrative, using dispositional traits under certain socio-cognitive, developmental, and environmental requests (23). Applying personal narratives to a previously challenging or traumatising event improves quality of life and daily functioning (48, 49). However, the use of personal narrative has not been integrated with positive psychology techniques that have shown capacity to support positive emotions by improving engagement, purpose, achievement, and human relationships.
One way to combine agency and positive psychology techniques is starting with the examination of personal beliefs and values through the use of the Values In Action (VIA) Inventory of Strengths instrument (VIA-IS instrument, http://www.viacharacter.org/ (50), updated in 2019 to the VIA Inventory of Strengths-Revised [VIA-IS-R (51)]). The original VIA-IS was a 240-item questionnaire and the VIA-IS-R consists of 196 items (52) measuring 24 key character strengths (e.g., creativity, bravery, teamwork) based on 6 distinct virtues (wisdom and knowledge, courage, humanity, justice, temperance, transcendence).
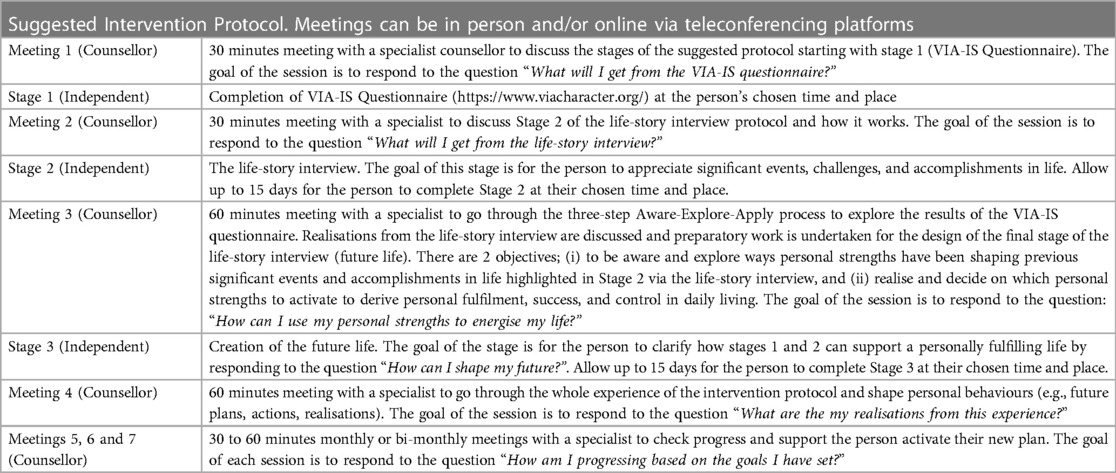
The VIA-IS instrument is used to profile personal strengths to aid integration of these character strengths into daily living, by setting goals and acting purposefully to enhance well-being, improve self-acceptance, and boost life-satisfaction (53). The results of the VIA-IS questionnaire are applied to a three-step process, Aware-Explore-Apply, to create a framework to navigate how identified strengths can improve happiness, boost relationships, and contribute to a better outlook for the future (54). After recognising preferred virtues and personal strengths, individuals are invited to narrate their personal story based on significant past events, and by looking at their present and future lives, with special reference to experiences that contain those preferred virtues and strengths. We provide a possible intervention schedule in Table 1.
The life story interview
We advocate the use of a “life story interview” in the form of a personal written narrative, to facilitate this process (55). The life story interview relates to a metaphor based on which major life events are contributing to the main chapters of one’s life. After defining those, the individual considers the high, the low and the turning point, as well as the positive experience and wisdom that derives from each one of those important life events. The ultimate phase relates to the individual’s aspiration regarding the next chapter of their life story, personal hopes and future life project that is expected to be in accordance with the report of the already completed VIA-IS questionnaire. Personal agency is manifested here on three levels:
1. The exploration of personal values and strengths,
2. The availability of ample time and self-selected pace to complete one’s life story interview, and
3. The future life project and its numerous options for the individual.
Based on significant events and challenges, and through the comparison of already performed behaviours versus personally valued actions, each individual has an increased chance to realise areas of reduced control and opportunities for personal growth. It also allows for contemplating continuity of personal identity based on valued activities and actions (53).
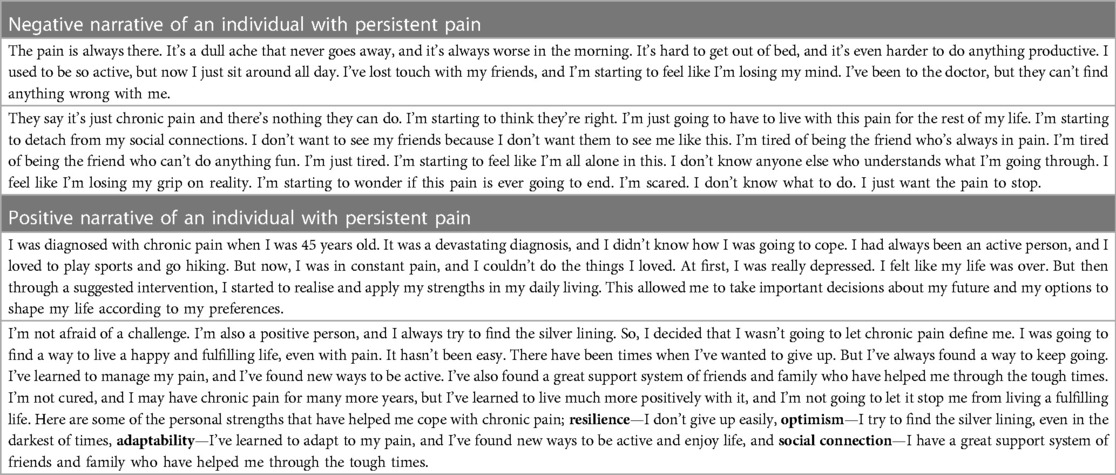
With an aim to reverse the negative experiences of chronic pain, the goal of the life story narrative technique is to create personal and agentic experiences of redemption leading to a revitalised connection to personal meaning, engaging behaviours and flow, synergetic relationships, personal activation, optimism, and increased resilience (see example in Table 2). Similarly to other positive psychology interventions, this technique can be implemented repetitively (thematically and until long-term resilience is established), online and in an asynchronous way, providing a low-cost alternative to expensive pain treatments.
Narratives in healthcare pain policy development
The National Institute for Health and Care Excellence (NICE) guidelines on chronic pain highlight the importance of person-centred assessment and management (7). The NICE guidelines emphasise the need to support individuals’ control and autonomy over their condition and social/psychological circumstances, while using an active exploration of personal strengths to improve management of chronic pain. Even though these guidelines propose a holistic approach to the management of chronic pain (i.e., psychological, social, and pharmacological) they endorse psychological approaches that are relatively expensive and time consuming (i.e., Acceptance and Commitment Therapy (ACT) and Cognitive Behavioural Therapy (CBT)). Positive psychology with personal narrative aligns with a whole-person-centred biopsychosocial paradigm of care and empowers people to take an active role in their healing journey to foster adaptive, resilient and autonomous lifestyles against adversities linked to chronic pain (19).
The cost of interventions using personal narratives within a framework of positive psychology is likely to be competitive compared with existing psychological approaches e.g., four hours to learn how to self-administer a positive psychology approach to personal narration (Table 1) compared with 6–20, one hour clinically supervised sessions of CBT. For these reasons we call for evaluations of positive psychology with personal narratives to provide robust research evidence to enable health policy and clinical decision makers to judge the cost-benefit-safety profile.
Conclusion
A positive psychology approach to personal narration sits within a whole-person paradigm capturing a holistic and biopsychosocial multidimensional method of care (56). Following our appraisal of extant literature, we conclude that integration of personal narratives within a framework of positive psychology offers an innovative agentic technique to assist the psychological states for people living with chronic pain in clinical and non-clinical settings. A recent systematic review provides tentative evidence that positive psychology interventions are efficacious for chronic pain. There is a paucity of research on which to judge the efficacy of integrating personal narrative into positive psychology interventions. Thus, we recommend a scoping review and evidence gap map to inform the direction of future research. We hope that this article stimulates further debate on the topic.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
EG: Conceptualization, Writing – original draft, Writing – review & editing. MJ: Conceptualization, Writing – review & editing.
Acknowledgments
Special thanks to Dr Cleo Protogerou for valuable comments on the manuscript.
Conflict of interest
In the previous 5 years, MJ’s employer has received income for expert consultancy activities from GlaxoSmithKline, TENSCare, and LifeCare Ltd. that lie outside of the submitted work. MJ declares book royalties from Oxford University Press.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organisation. Icd-11: international classification of diseases (11th revision). (2019).
2. Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. (2020) 161(9):1976–82. doi: 10.1097/j.pain.0000000000001939
3. Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396(10258):1204–22. doi: 10.1016/S0140-6736(20)30925-9
4. Cáceres-Matos R, Gil-García E, Barrientos-Trigo S, Porcel-Gálvez AM, Cabrera-León A. Consequences of chronic non-cancer pain in adulthood. Scoping Review. Rev Saúde Pública. (2020) 54:39. doi: 10.11606/s1518-8787.2020054001675
5. Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. Lancet. (2021) 397(10289):2082–97. doi: 10.1016/S0140-6736(21)00393-7
6. National Institute for Health and Care Excellence. Osteoarthritis in over 16s: Diagnosis and management. Nice guideline [Ng226]. London: National Institute for Health and Care Excellence (NICE) (2022).
7. National Institute for Health and Care Excellence. Chronic pain (primary and secondary) in over 16s: Assessment of all chronic pain and management of chronic primary pain (Ng193). London, UK: National Institute for Health and Care Excellence (NICE) (2021). 1–36.
8. National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: Assessment and management. London, UK:Clinical Guideline [Ng59]: National Institute for Health and Care Excellence (NICE) (2016). 1–18. Available at: https://www.nice.org.uk/guidance/ng59
9. Inoue S, Kamiya M, Nishihara M, Arai Y-CP, Ikemoto T, Ushida T. Prevalence, characteristics, and burden of failed back surgery syndrome: the influence of various residual symptoms on patient satisfaction and quality of life as assessed by a nationwide internet survey in Japan. J Pain Res. (2017) 10:811–23. doi: 10.2147/JPR.S129295
10. Neuman MD, Bateman BT, Wunsch H. Inappropriate opioid prescription after surgery. Lancet. (2019) 393(10180):1547–57. doi: 10.1016/S0140-6736(19)30428-3
11. Melzack R, Wall PD. Pain mechanisms: a new theory. Science. (1965) 150(3699):971–9. doi: 10.1126/science.150.3699.971
12. Engel GL. The need for a new medical model: a challenge for biomedicine. Science. (1977) 196(4286):129–36. doi: 10.1126/science.847460
13. Nicholas MK. The biopsychosocial model of pain 40 years on: time for a reappraisal? Pain. (2022) 163(S1):S3–S14. doi: 10.1097/j.pain.0000000000002654
14. Cheatle MD. Biopsychosocial approach to assessing and managing patients with chronic pain. Med Clin N Am. (2016) 100(1):43–53. doi: 10.1016/j.mcna.2015.08.007
15. Bevers K, Watts L, Kishino ND, Gatchel RJ. The biopsychosocial model of the assessment, prevention, and treatment of chronic pain. US Neurol. (2016) 12(2):98–104. doi: 10.17925/USN.2016.12.02.98
17. Harding S-A. “How do I apply narrative theory?”: socio-narrative theory in translation studies. Targ Intern J Transl Stud. (2012) 24(2):286–309. doi: 10.1075/target.24.2.04har
18. Cuyul-Vásquez I, Barría JA, Perez NF, Fuentes J. The influence of verbal suggestions in the management of musculoskeletal pain: a narrative review. Phys Ther Rev. (2019) 24(3-4):175–81. doi: 10.1080/10833196.2019.1639011
19. Overcash JA. Narrative research: a review of methodology and relevance to clinical practice. Crit Rev Oncol Hematol. (2003) 48(2):179–84. doi: 10.1016/j.critrevonc.2003.04.006
20. Owens JE, Menard M, Plews-Ogan M, Calhoun LG, Ardelt M. Stories of growth and wisdom: a mixed-methods study of people living well with pain. Glob Adv Health Med. (2016) 5(1):16–28. doi: 10.7453/gahmj.2015.065
21. Rutledge PB. Everything is story: telling stories and positive psychology. California: ABC-CLIO LLC (2016). 01–25.
22. Baumeister RF, Wilson B. Life stories and the four need for meaning. Psychol Inq. (1996) 7(4):322–5. doi: 10.1207/s15327965pli0704_2
23. McAdams DP. The psychology of life stories. Rev Gen Psychol. (2001) 5(2):100–22. doi: 10.1037/1089-2680.5.2.100
24. Facco E. Pain, the unknown: epistemological issues and related clinical implications. Minerva Anestesiol. (2021) 87(11):1255–67. doi: 10.23736/S0375-9393.21.15920-6
26. Scarry E. The body in pain: the making and unmaking of the world. USA: Oxford University Press (1985).
27. van Hout F, van Rooden A, Slatman J. Chronicling the chronic: narrating the meaninglessness of chronic pain. Med Humanit. (2022) 49(1):1–8. doi: 10.1136/medhum-2021-012331
28. Toye F, Seers K, Barker KL. Meta-ethnography to understand healthcare professionals’ experience of treating adults with chronic non-malignant pain. BMJ Open. (2017) 7(12):e018411. doi: 10.1136/bmjopen-2017-018411
29. Toye F, Belton J, Hannink E, Seers K, Barker K. A healing journey with chronic pain: a meta-ethnography synthesizing 195 qualitative studies. Pain Med. (2021) 22(6):1333–44. doi: 10.1093/pm/pnaa373
30. Toye F, Seers K, Allcock N, Briggs M, Carr E, Andrews J, et al. Patients’ experiences of chronic non-malignant musculoskeletal pain: a qualitative systematic review. Br J Gen Pract. (2013) 63(617):e829–41. doi: 10.3399/bjgp13X675412
31. Johnson MI, Chazot P, Cole F, Cruickshank R, Fuller D, Keyse C, et al. Pain through the perspective of art and creativity: insights from the unmasking pain project. Front Pain Res (Lausanne). (2023) 4:1179116. doi: 10.3389/fpain.2023.1179116
32. Miglio N, Stanier J. Beyond pain scales: a critical phenomenology of the expression of pain. Front Pain Res (Lausanne). (2022) 3:895443. doi: 10.3389/fpain.2022.895443
34. Dunbar RI. Group Size. Vocal grooming and the origins of language. Psychon Bull Rev. (2017) 24(1):209–12. doi: 10.3758/s13423-016-1122-6
35. Angel S, Jensen LD, Maribo T, Gonge BK, Buus N. Narratives of life with long-term low back pain: a follow up interview study. Scand J Pain. (2017) 17(1):382–9. doi: 10.1016/j.sjpain.2017.09.018
36. Hydén L-C. Illness and narrative. Sociol Health Ill. (2008) 19(1):48–69. doi: 10.1111/j.1467-9566.1997.tb00015.x
37. Hovey RB, Khayat VC, Feig E. Listening to and letting pain speak: poetic reflections. Br J Pain. (2018) 12(2):95–103. doi: 10.1177/2049463717741146
38. Wainwright E, Wainwright D, Coghill N, Walsh J, Perry R. Resilience and return-to-work pain interventions: systematic review. Occup Med (Chic Ill). (2019) 69(3):163–76. doi: 10.1093/occmed/kqz012
39. Cook AJ, Brawer PA, Vowles KE. The fear-avoidance model of chronic pain: validation and age analysis using structural equation modeling. Pain. (2006) 121(3):195–206. doi: 10.1016/j.pain.2005.11.018
40. Costanza A, Chytas V, Piguet V, Luthy C, Mazzola V, Bondolfi G, et al. Meaning in life among patients with chronic pain and suicidal ideation: mixed methods study. JMIR Form Res. (2021) 5(6):e29365. doi: 10.2196/29365
41. Zale EL, Lange KL, Fields SA, Ditre JW. The relation between pain-related fear and disability: a meta-analysis. J Pain. (2013) 14(10):1019–30. doi: 10.1016/j.jpain.2013.05.005
42. Braunwalder C, Muller R, Glisic M, Fekete C. Are positive psychology interventions efficacious in chronic pain treatment? A systematic review and meta-analysis of randomized controlled trials. Pain Med. (2022) 23(1):122–36. doi: 10.1093/pm/pnab247
43. Müller R, Segerer W, Ronca E, Gemperli A, Stirnimann D, Scheel-Sailer A, et al. Inducing positive emotions to reduce chronic pain: a randomized controlled trial of positive psychology exercises. Disabil Rehabil. (2022) 44(12):2691–704. doi: 10.1080/09638288.2020.1850888
44. Brady A, Grenville-Cleave B. Positive psychology in sport and exercise. New York, NY: Routledge (2018).
45. Seligman M. Agency in greco-roman philosophy. J Posit Psychol. (2021) 16(1):1–10. doi: 10.1080/17439760.2020.1832250
46. Waterman AS. The humanistic psychology–positive psychology divide: contrasts in philosophical foundations. American Psychologist. (2013) 68(3):124–33. doi: 10.1037/a0032168
47. Seligman M. Flourish: a visionary new understanding of happiness and well-being. London, UK: Simon and Schuster (2012).
48. Bauer JJ, McAdams DP, Pals JL. Narrative identity and eudaimonic well-being. J Happiness Stud. (2008) 9(1):81–104. doi: 10.1007/s10902-006-9021-6
49. Pals JL, McAdams DP. The transformed self: a narrative understanding of posttraumatic growth. Psychol Inq. (2004) 15(1):65–59.
50. Peterson CA, Seligman MEP. Character strengths and virtues: a handbook and classification. Washington DC, USA: Oxford University Press (2004). p. 800.
51. McGrath RE. Technical report: the via assessment suite for adults: development and initial evaluation (rev. Ed.). Cincinnati, OH: VIA Institute on Character (2019).
52. McGrath RE, Wallace N. Cross-validation of the via inventory of strengths-revised and its short forms. J Pers Assess. (2021) 103(1):120–31. doi: 10.1080/00223891.2019.1705465
53. Schutte NS, Malouff JM. The impact of signature character strengths interventions: a meta-analysis. J Happiness Stud. (2019) 20(4):1179–96. doi: 10.1007/s10902-018-9990-2
54. Niemiec RM. Character strengths interventions: a field guide for practitioners. Boston, MA: Hogrefe Publishing GmbH (2018).
55. Lilgendahl JP, McAdams DP. Constructing stories of self-growth: how individual differences in patterns of autobiographical reasoning relate to well-being in midlife: stories of self-growth. J Pers. (2011) 79(2):391–428. doi: 10.1111/j.1467-6494.2010.00688.x
Keywords: personal narrative, chronic pain, positive psychology, agency, healthcare
Citation: Georgiadis E and Johnson MI (2023) Incorporating personal narratives in positive psychology interventions to manage chronic pain. Front. Pain Res. 4:1253310. doi: 10.3389/fpain.2023.1253310
Received: 5 July 2023; Accepted: 26 September 2023;
Published: 6 October 2023.
Edited by:
Sayyed Mohsen Fatemi, York University, CanadaReviewed by:
David Erekson, Brigham Young University, United States© 2023 Georgiadis and Johnson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mark I. Johnson bS5qb2huc29uQGxlZWRzYmVja2V0dC5hYy51aw==
 Emmanouil Georgiadis
Emmanouil Georgiadis Mark I. Johnson
Mark I. Johnson