- 1Department of Anesthesiology, University of Michigan, Ann Arbor, MI, United States
- 2Department of Pediatric Neurology, Vanderbilt University Medical Center, Nashville, TN, United States
- 3Department of Family Medicine, University of Michigan, Ann Arbor, MI, United States.
Higher perceived social support has been shown to buffer the impact of negative stressful events like childhood abuse on health outcomes. Yet, the role of perceived social support as a mediator of the association between childhood abuse and pain-related characteristics is not well understood. The present study explored this premise. Patients (n = 1,542) presenting to a tertiary-care, outpatient pain clinic completed a cross-sectional survey consisting of regularly collected clinical data and validated measures. Path analysis suggested that the impact of childhood abuse on sensory and affective pain-related characteristics was partially explained by perceived emotional support. Survivors of childhood abuse display a more complex clinical pain phenotype and this extends to more negative perceptions of social support. Our findings may reflect processes whereby childhood abuse negatively impacts social relationships across the lifespan, and these negative social perceptions and relationships influence sensory and affective components of pain.
Introduction
Trauma exposure and chronic pain are strongly associated (1). Childhood abuse, in particular, has been linked to the prevalence of chronic pain and pain-related characteristics. A history of childhood maltreatment is associated with more physical symptoms, a higher likelihood of a number of pain conditions (e.g., back pain; headaches), greater anxiety and depressive symptoms in adulthood, and a more complex clinical phenotype among chronic pain patients (2–5). Investigating mechanisms of the association between childhood abuse and pain-related characteristics is imperative to understanding and addressing this complexity. Indeed, numerous factors have been proposed as mechanisms driving the mutual maintenance of trauma and pain symptoms, including attentional biases toward threat or pain-related stimuli and expectations of negative outcomes (1). In the present study, we propose that the association between childhood abuse and chronic pain may be partially explained by perceptions of social support, or the belief that others are available to provide help and care (6).
Childhood abuse may be particularly damaging to perceptions of social support by altering the way in which individuals perceive and relate to others (7, 8). According to Miller et al. (9), childhood abuse is associated with negative behavioral tendencies including threat vigilance and mistrust of others, which can make social relationships in adulthood more tenuous and have downstream effects on physical health (8, 9). This extends to lower perceptions of social support, which have been linked to a history of childhood maltreatment (10–13).
Perceived social support is an important predictor of health and well-being in general (14) and in the development and maintenance of chronic pain in particular (15, 16). Previous research suggests that higher perceived social support buffers the impact of negative stressful events on health outcomes, including pain-related and psychological outcomes (14, 17). Yet, research also suggests a direct association between lower social support and pain-related characteristics, including higher pain severity, higher pain sensitivity, and higher negative affect (17–22). Mechanistically, higher perceived social support is associated with lower levels of inflammation (23), whereas chronic stress resulting from negative relationship experiences may lead to physiological dysregulation (24). In turn, neuroendocrine and inflammatory biomarkers are hypothesized to play a role in chronic pain for some patients (25, 26).
Interestingly, few studies have considered social support as a potential mechanistic pathway linking childhood maltreatment to physical and mental health in adulthood despite evidence that childhood abuse impacts social perceptions. Some studies provide evidence of this pathway (12, 13, 27) while others do not (28). To our knowledge, only one study has evaluated social perceptions in the association between childhood abuse and pain-related characteristics. Alhalal et al. (27) found that, in a sample of married Saudi women, perceptions of family support mediated the association between childhood abuse and depressive symptoms, which then exhibited a direct association with chronic pain severity (i.e., pain intensity and disability).
Despite finding support for this potentially important association, their study was limited by a narrow conception of social support and pain-related outcomes. We sought to advance this research in three ways. First, we assessed these associations in a sample of patients with pain. Second, we evaluated both perceived emotional (perception of love and caring from others) and perceived instrumental social support (perception of tangible help being available when needed). Third, because pain is a multifaceted experience (15, 16), we considered both sensory (i.e., widespread pain and pain severity) and affective (i.e., anxiety and depressive symptoms) components as outcomes. We sought to determine: (a) whether childhood abuse was associated with perceived emotional and instrumental social support, as well as widespread pain, pain severity, anxiety symptoms and depressive symptoms; (b) whether perceived emotional and instrumental social support were associated with widespread pain, pain severity, anxiety symptoms, and depressive symptoms; and (c) whether perceived emotional and instrumental social support partially mediated the association between childhood abuse and the aforementioned pain-related characteristics. We hypothesized that the impact of childhood abuse on widespread pain, pain severity, anxiety symptoms, and depressive symptoms would be partially mediated through perceived emotional and instrumental social support.
Methods
Participants and procedure
Patients 18 years of age and older presenting for care at the University of Michigan Back & Pain Center between June 2018 and March 2020 were included in the present analyses. The Back & Pain Center is a tertiary-care, outpatient clinic servicing chronic pain patients across a range of conditions. All new patients are provided with a packet of questionnaires to complete prior to their first visit to be used for clinical care and research purposes (29). University of Michigan Medical School Institutional Review Board (HUM00041820) approval was obtained. A waiver of informed consent was obtained due to the extensive use of the survey in a clinical setting. Remuneration was not provided. Prior studies have utilized the patient data obtained through the Back & Pain Center; however, our specific sample and research question are unique compared to these previous studies (4, 30).
Measures
Demographics
Age, sex, and marital status were obtained.
Abuse history
Patients were asked three questions assessing abuse history: Do you have a history of psychological or emotional abuse?; Do you have a history of physical abuse?; and Do you have a history of sexual abuse? Response options included 1 (Yes) and 0 (No). Patients who responded yes were asked to indicate when the abuse occurred, including childhood (<13 years), adolescence (13–18 years), and adulthood. For the present study, childhood abuse included experiences in childhood and adolescence. We combined psychological or emotional, physical, and sexual abuse into a single measure of abuse for multiple reasons. First, our central question focused on social support as a mediator, rather than potential differentiation of types of abuse. Second, different types of abuse frequently co-occur. In the present data, 85% of individuals who self-reported physical abuse also reported emotional abuse and 47% reported sexual abuse. Similarly, 66% of individuals reporting sexual abuse also reported emotional abuse. Conversely, of those who did not report emotional abuse, only 1.5% reported physical abuse and 3.5% reported sexual abuse. Third, this is a simpler way for clinicians to assess heightened risk rather than evaluating specific types of abuse experienced by patients, making the findings more clinically useful. Therefore, if a participant indicated a history of any form of abuse during childhood or adolescence, they were considered to have had a history of childhood abuse.
Widespread pain
Widespread pain was assessed with the Michigan Body Map (31), which included a sum of 35 potential body areas. Participants were asked to mark the areas of the body where they felt persistent or recurrent pain present for the last three months or longer. Scores ranged from 0 to 35 (31–33).
Pain severity
The 4-item Brief Pain Inventory was used to assess pain severity (34). Patients were asked to rate their pain at its worst in the last week, least in the last week, on the average, and right now, with options ranging from 0 (no pain) to 10 (pain as bad as you can imagine). An average score was calculated.
Anxiety and depressive symptoms
Anxiety and depressive symptoms were assessed using the Patient Reported Outcomes Measurement Information System (PROMIS) 8-item scales (Anxiety-Short Form 8 and Depression-Short Form 8a, respectively). Patients were asked to consider symptoms in the past seven days (e.g., I felt fearful [anxiety symptoms]; I felt worthless [depressive symptoms]). Response options ranged from 1 (never) to 5 (always). Sum scores were obtained for each scale and ranged from 8 to 40.
Perceptions of social support
Perceptions of emotional and instrumental support were assessed with the PROMIS four-item social support scales. Perceived emotional support was assessed using the PROMIS Item Bank v2.0—Emotional Support—Short Form 4a (e.g., I have someone who will listen to me when I need to talk). Perceived instrumental support was assessed using the PROMIS Item Bank v2.0—Instrumental Support—Short Form 4a (e.g., Do you have someone to help you if you are confined to bed?). For both measures, response options ranged from 1 (Never) to 5 (Always). Scores are summed for each scale and range from 4 to 20.
Data analysis plan
Patients were excluded if they did not provide information regarding abuse history. Additionally, if a participant indicated “no” to one or two forms of abuse, but left any missing, they were treated as missing in the final analyses. Sex, marital status, and childhood abuse were dummy coded, such that male sex, being nonmarried, and no childhood abuse were reference categories. Descriptive statistics were obtained for the variables of interest. Differences in the variables of interest by history of childhood abuse were assessed using t-tests and contingency analyses with associated χ2 tests. Bivariate correlations were also assessed. Variance inflation factor did not exceed 3.0 for any variable; thus, multicollinearity was not a concern for the path model.
Path analysis was used to assess whether perceived emotional and instrumental support mediated the association between childhood abuse and widespread pain, pain severity, and negative affect. Mediators were allowed to covary as were the outcome variables. Childhood abuse was allowed to associate with outcomes conditional on the mediators. Thus, the model evaluated the presence of partial mediation using a saturated model and model fit statistics were not obtained. Sex, age, and marital status were included as covariates for each mediator and outcome. Full information maximum likelihood method of estimation and robust standard errors were used to account for missing values and non-normal data. Squared multiple correlation coefficients (R2) were used to determine the variance explained in each dependent variable.
A bootstrap procedure with 10,000 replicates was used to create bias-corrected and accelerated (BCa) 95% confidence intervals (95% CI) for the indirect effects. Complete case analysis was used to evaluate the significance of the indirect effects. Confidence intervals not including zero were considered significant. Total indirect effect coefficients were divided by total effect coefficients for each outcome to determine how much of the total effect was accounted for by the indirect effects through perceived emotional and instrumental support. Additionally, specific indirect path coefficients were divided by the total indirect effect coefficients to determine the relative importance of each pathway. The sum of the absolute values was used for the total indirect effect. Analyses were run using Stata version 15 (College Station, TX).
Results
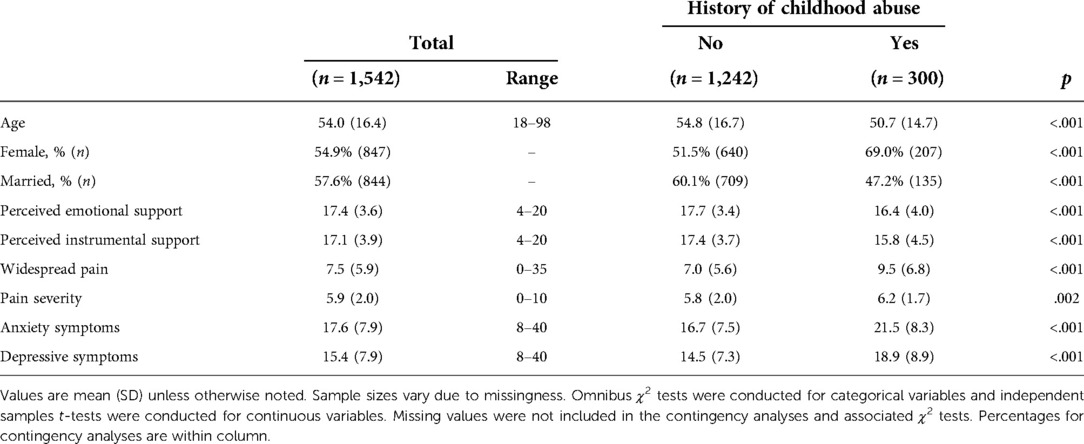
The full sample consisted of 1,542 patients (Mage = 54.0, SD = 16.4; 54.9% female). Approximately 19.5% (n = 300) reported a history of childhood abuse. Individuals who reported a history of childhood abuse were younger, more often female, and less often married. Additionally, compared to individuals who reported no history of childhood abuse, those who reported childhood abuse exhibited lower perceived emotional support, lower perceived instrumental support, more widespread pain, higher pain severity, higher anxiety symptoms, and higher depressive symptoms. See Table 1 for descriptive statistics and comparisons by history of childhood abuse.
Perceived emotional and instrumental support were significantly positively correlated. Higher perceived emotional support and perceived instrumental support were also significantly associated with less widespread pain, lower anxiety symptoms, and lower depressive symptoms. All of the model outcomes were significantly correlated. See Supplementary Table S1.
As shown in Table 2 and Figure 1, the path model showed significant direct associations from history of childhood abuse to perceived emotional and instrumental support. Approximately 6.9% of the variance in perceived emotional support and 15.4% of the variance in perceived instrumental support were accounted for by the model. Childhood abuse also exhibited significant direct associations with widespread pain, pain severity, anxiety symptoms, and depressive symptoms. Perceived emotional support was significantly associated with lower widespread pain, lower anxiety symptoms, and lower depressive symptoms. Perceived instrumental support was significantly associated with lower anxiety symptoms. Approximately 5.3% of the variance in widespread pain, 2.8% of the variance in pain severity, 14.4% of the variance in anxiety symptoms, and 16.9% of the variance in depressive symptoms were accounted for by the model.
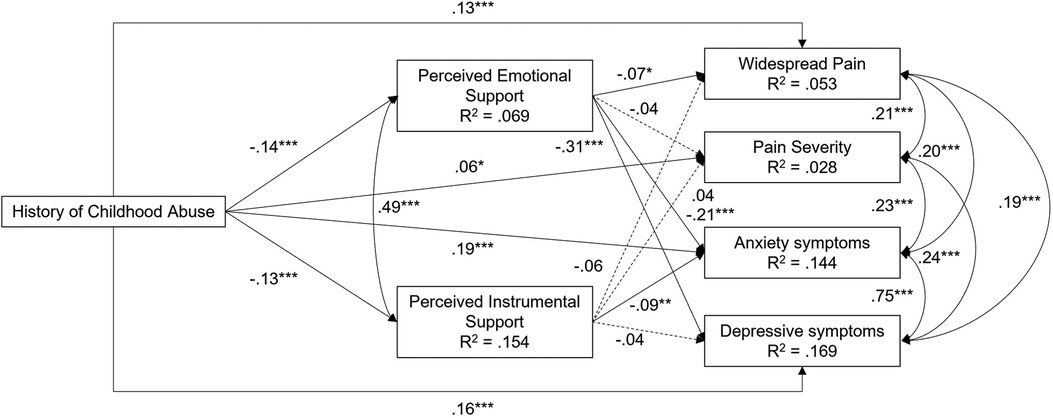
Figure 1. Final mediation model of the effect of history of childhood abuse on pain-related characteristics via perceived emotional support and perceived instrumental support (n = 1,542). Standardized coefficients are presented. Significance is determined using unstandardized coefficients and robust standard errors. Solid lines indicate significant paths. Dashed lines indicate nonsignificant paths. ‡p < .10. *p < .05. **p < .01. ***p < .001. Covariates were included in estimation but are not shown.
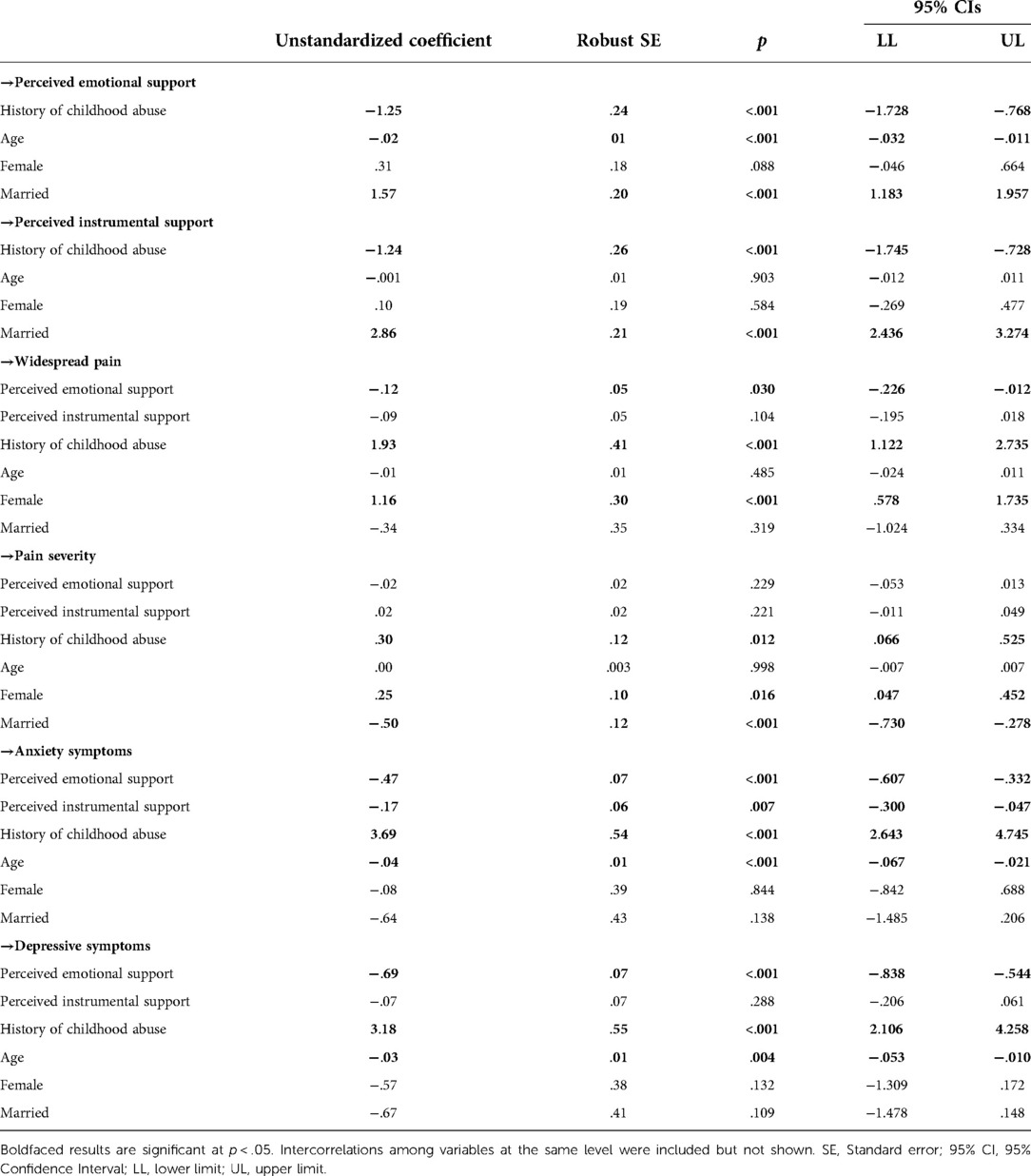
Table 2. Unstandardized coefficients, robust SEs, and 95% CIs for final mediation model of the association between history of childhood abuse and pain-related characteristics (n = 1,542).
Total and specific indirect effects are summarized in Table 3. Childhood abuse exhibited a significant total indirect effect on higher widespread pain. Approximately 11.8% of the total effect of childhood abuse on widespread pain was indirect through perceived emotional and instrumental support. This was driven by a significant specific indirect effect through perceived emotional support, which accounted for 54.6% of the total indirect effect. Although the total indirect effect on pain severity was nonsignificant, this was partly due to opposing effects of perceived emotional and instrumental support. Evaluation of the coefficients suggests that 0.6% of the total effect was indirect through perceived emotional and instrumental support. Childhood abuse exhibited a significant total effect on higher anxiety symptoms. Approximately 17.8% of the total effect was indirect through perceived emotional and instrumental support. Perceived emotional support exhibited a higher proportion of the indirect effect (69.1%). Finally, childhood abuse showed a significant total indirect effect on depressive symptoms. Approximately 23.0% of the total effect was indirect through perceived emotional and instrumental support. This was driven by the significant specific indirect effect through perceived emotional support which accounted for 88.1% of the total indirect effect.
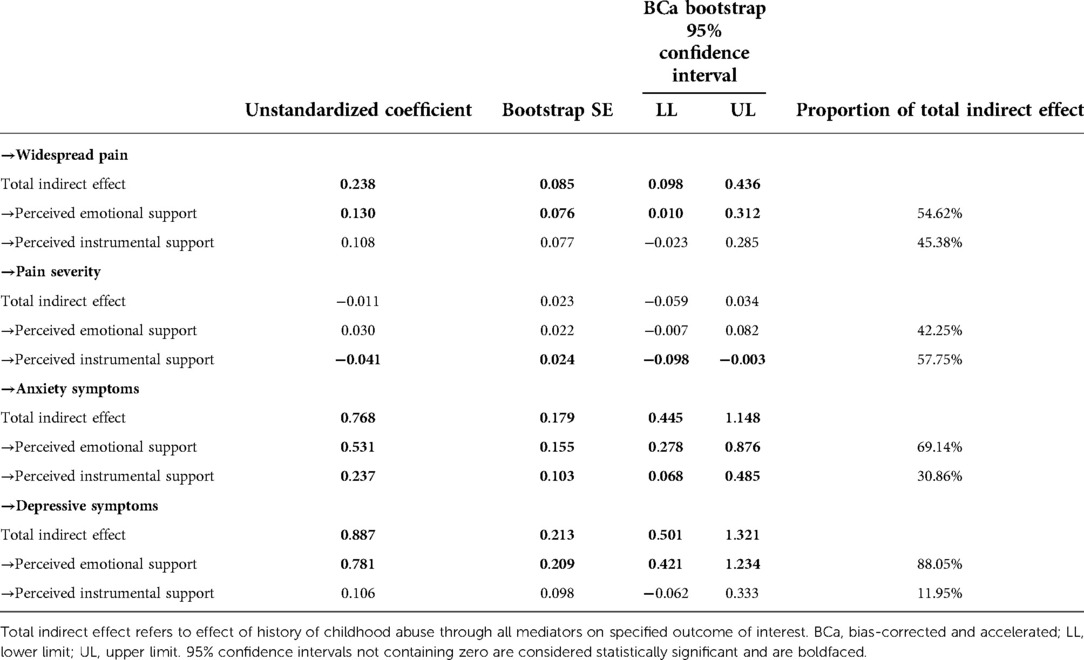
Table 3. Total and specific indirect effects, bootstrap standard errors, and bias-corrected and accelerated 95% confidence intervals for mediation model of the association between history of childhood abuse and pain-related characteristics (n = 1,349).
Discussion
Childhood abuse can have long-lasting deleterious effects on social, physical, and psychological health. Investigations into the mechanisms through which childhood abuse impacts health outcomes has seldom considered perceptions of social support. Furthermore, social support is frequently considered as a protective buffer that reduces the impact of adversity on health outcomes. Our study instead explored a potential indirect association, whereby childhood abuse is associated with decrements in perceptions of social support, and more negative perceptions of social support are associated with worse symptoms. The present study provides partial support for our hypotheses and suggests that the association between childhood abuse and sensory and affective pain-related characteristics is partially conveyed through perceptions of social support, particularly emotional support.
Childhood abuse was associated with poorer perceptions of social support and a more complex pain phenotype
In the present study, patients living with chronic pain who have a history of childhood abuse reported lower perceptions of social support. These findings are in line with previous research. Childhood abuse may mold negative perceptions of others and impact how social information is interpreted (9, 11, 35–37), which may be reflected in less positive perceptions of and less satisfaction with social support (10–12). Childhood abuse may also fuel unhealthy relationship interactions marked by more negativity and less positive behavior that, in turn, results in less support being provided by others (38–40). How accurate these perceptions are and how well they fit the reality of support provision may not be particularly important; previous research suggests that perceptions of support are more important for health-related outcomes than actual support received (41). Additionally, perceptions of social support may be primarily dependent upon observer characteristics (41), including schema and expectations driven by prior experiences like abuse. Similar findings have been reported for the impact of childhood abuse on marital satisfaction in adulthood, which suggest that neither positive nor negative partner characteristics moderated the association (37).
Our findings also suggest that childhood abuse was associated with more widespread pain, higher pain severity, and higher anxiety and depressive symptoms. Indeed, previous research and theory suggests that childhood abuse is associated with poor physical and psychological health outcomes in adulthood (2–5, 42). This extends to a more complex clinical pain phenotype, including more widespread pain, higher pain severity, and higher anxiety and depressive symptoms (4).
The association between childhood abuse and pain-related characteristics is partially conveyed through perceived emotional support
Although the association between childhood abuse and psychological and physical health outcomes has been well-established in the literature, researchers have highlighted the necessity of understanding the mechanisms of this association. As considered in the current study, perceptions of social relationships may be important to consider. Indeed, social factors (e.g., interpersonal style and social cognition) have been proposed as potential pathways conveying the impact of childhood abuse on health outcomes (8). Yet, other pathways are important as well, including the influence of childhood abuse on health risk and promotive behavior and posttraumatic stress symptoms (8). Thus, it is unsurprising that significant, direct associations were found and maintained even in the present mediation model.
Our findings, however, suggest that the association between childhood abuse and sensory and affective pain-related characteristics, including widespread pain, anxiety symptoms, and depressive symptoms, could be partially explained by perceptions of social support. Similar to our findings, previous research has found that perceptions of social support and perceived relationship quality were important mechanisms linking childhood abuse with depressive symptoms (27), allostatic load in middle adulthood (12), as well as worse health perceptions, worse mental health, and more somatic complaints (13). Furthermore, recent research found that marital quality, composed of perceptions of support, strain, and disagreement, conveyed the association between childhood abuse and negative affect among older adults (43). Thus, perceptions of social support are a potentially modifiable mechanism that should be further investigated. Of note, although variance in widespread pain was better accounted for by the model than variance in pain severity, both outcomes exhibited low variance explained suggesting that other predictors are important to consider for sensory pain-related characteristics. Instead, the present model appears to better predict affective pain-related characteristics.
The association between childhood abuse and widespread pain is particularly interesting. Compared to pain severity, widespread pain may be more characteristic of nociplastic pain, in which central nervous system factors are believed to play a part in the spread or amplification of pain (25, 44). Stressors have been implicated as precipitating factors of nociplastic pain (25). Thus, low satisfaction with social support, negative social perceptions, and accompanying relationship distress may be sources of chronic stress that contribute to poor physical health including nociplastic pain (8). Alternatively, survivors of childhood abuse may not benefit from favorable perceptions of social support, which are shown to reduce perceptions of stress, improve coping strategies, and reduce the physiological stress response to pain (17).
The lack of findings with pain severity may also be associated with the time frame in which it is evaluated. The measure of widespread pain is indicative of chronicity, whereas the measure of pain severity considered the preceding week. Our model likely reflects long processes in which childhood abuse negatively impacts social relationships across the lifespan, and dissatisfying social perceptions and relationships influence perceptions of stress as well as present direct sources of distress that compound over time (45). On the other hand, pain severity may be a brief snapshot of sensory experiences. Future research should consider dynamic trajectories of pain severity and whether these instead are associated with social perceptions.
Additionally, instrumental support was associated with higher pain severity in the model, although this direct association was nonsignificant. This likely contributed to the significant indirect effect linking childhood abuse to lower pain severity through instrumental support. The model findings suggest that instrumental support may function as a solicitous form of social support that promotes and reinforces pain behavior like expressions of severity (46). Thus, the availability of instrumental support may encourage individuals to acknowledge the severity of their pain in order to receive much needed assistance with daily tasks.
The findings also suggest that, overall, perceived emotional support better predicts sensory and affective pain-related characteristics compared to perceived instrumental support. The benefit of each form of support may depend on what the individual requires in specific situations (14). Emotional support may be more beneficial for chronic health conditions (47), whereas instrumental support may be more valuable for specific needs.
Strengths and limitations
The present study had many strengths. We evaluated these associations in a large sample of patients with pain using measures of both emotional and instrumental social support, and also broadly conceptualized pain-related characteristics as encompassing both sensory and affective components. Numerous limitations should also be acknowledged. We tested a mediation model which imposed a specific directional effect and our results reflect our statistical approach. However, the data were cross-sectional which limits our ability to make any causal claims. There are likely bidirectional relationships between social support perceptions and pain-related characteristics. Our goal, however, was not to propose a specific direction of effects to the exclusion of alternative models, but to evaluate a model that may have implications for chronic pain interventions. Our measure of abuse was limited due to the data being collected in the context of clinical care and the necessity to keep measures brief to ease participant burden. Type and timing of abuse should be investigated in future research. Additionally, many victims of abuse do not acknowledge or label the experience as abuse. Measures that provide behavioral descriptions of what the abuse would entail would likely result in higher prevalence rates. The participants also had various pain diagnoses and mixed etiology. This may contribute to important, yet indistinguishable, heterogeneity in the current sample. Future research should consider these factors. Additionally, due to the secondary nature of the present analyses, we did not have measures related to other forms of social integration or negative social perceptions such as hostility and perceived rejection. Future research should consider the role of social integration, which may be more likely to exhibit direct effects on health outcomes (14), as well as the impact of negative social perceptions on health outcomes, which may be more strongly associated with poor health outcomes compared to conceptually positive experiences of emotional and instrumental support (48).
Clinical implications and conclusion
Despite these limitations, understanding the impact of childhood abuse on perceptions of social support and, in turn, social support on pain-related characteristics is important to understand as chronic pain management techniques and interventions that promote the value of social support (e.g., support groups, engaging spouses or loved ones in care) are often recommended. Yet, patients with a history of childhood abuse victimization may perceive support differently which would have important implications for these pain management techniques and interventions. Thus, it is critical for healthcare providers to consider the interpersonal history of patients. Previous studies have demonstrated the importance of screening all chronic pain patients for a history of abuse (49, 50). Doing so can help guide intervention administration and modifications. Indeed, patients with a history of childhood abuse may especially benefit from interventions that improve the sense of safety and care in their relationships.
The findings also extend to the patient-provider relationship. Patients' trust in the recommendations of their provider is predicated on trust in the relationship they have with that provider. There is evidence that childhood abuse results in patients having less trust in their providers, as well as providers rating these patients as more difficult (50–53). This bidirectional challenge can undermine the very safety and trust needed to be able to bring up and discuss the role that childhood abuse could have or be having on the overall management of their pain, thus making long term success and improvement even harder to achieve. Further research into the impact of trauma-informed care and abuse screening in the setting of chronic pain management is needed to explore ways to make the seeking of care safe and supportive.
Survivors of childhood abuse exhibit a worse clinical pain phenotype, highlighting the critical need to understand the various mechanisms driving this association. Researchers and clinicians should consider the role of social perceptions within this complex relationship, including their impact on the patient-provider relationship. Interventions that improve patients' sense that others love and care for them may contribute to symptom improvement.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by University of Michigan Medical School Institutional Review Board (HUM00041820). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
JPierce was responsible for study conceptualization, contributing to formal analysis, methodology, data presentation, and writing the original draft and editing. JPresto and EH: contributed to the original draft, review and editing. ALH: contributed to study conceptualization, study supervision, and review and editing. JD: contributed to the formal analysis. JRS and KG contributed to writing the original draft and editing. JM: contributed to study conceptualization, study supervision, and review and editing. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by the Department of Anesthesiology, University of Michigan. J Pierce was also supported by a Postdoctoral Translational Scholar Program training grant from the Michigan Institute for Clinical and Health Research (UL1TR002240; PI: George Mashour). The funder was not involved in study design, data collection, data analysis, or manuscript preparation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpain.2022.1075605/full#supplementary-material.
References
1. Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: mutual maintenance? Clin Psychol Rev. (2001) 21(6):857–77. doi: 10.1016/S0272-7358(00)00071-4
2. McCauley J, Kern DE, Kolodner K, Dill L, Schroeder AF, DeChant HK, et al. Clinical characteristics of women with a history of childhood abuse: unhealed wounds. JAMA. (1997) 277(17):1362–8. doi: 10.1001/jama.1997.03540410040028
3. Walker EA, Gelfand A, Katon WJ, Koss MP, Von Korff M, Bernstein D, et al. Adult health status of women with histories of childhood abuse and neglect. Am J Med. (1999) 107(4):332–9. doi: 10.1016/S0002-9343(99)00235-1
4. Nicol AL, Sieberg CB, Clauw DJ, Hassett AL, Moser SE, Brummett CM. The association between a history of lifetime traumatic events and pain severity, physical function, and affective distress in patients with chronic pain. J Pain. (2016) 17(2):1334–48. doi: 10.1016/j.jpain.2016.09.003
5. Davis DA, Luecken LJ, Zautra AJ. Are reports of childhood abuse related to the experience of chronic pain in adulthood? A meta-analytic review of the literature. Clin J Pain. (2005) 21(5):398–405. doi: 10.1097/01.ajp.0000149795.08746.31
6. Haber MG, Cohen JL, Lucas T, Baltes BB. The relationship between self-reported received and perceived social support: a meta-analytic review. Am J Community Psychol. (2007) 39(1-2):133–44. doi: 10.1007/s10464-007-9100-9
7. Hazan C, Shaver PR. Attachment as an organization framework for research on close relationships. Psychol Inq. (1994) 5(1):1–22. doi: 10.1207/s15327965pli0501_1
8. Kendall-Tackett K. The health effects of childhood abuse: four pathways by which abuse can influence health. Child Abuse Negl. (2002) 26(6-7):715–29. doi: 10.1016/S0145-2134(02)00343-5
9. Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull. (2011) 137(6):959–97. doi: 10.1037/a0024768
10. Steine IM, Winje D, Krystal JH, Bjorvatn B, Milde AM, Gronli J, et al. Cumulative childhood maltreatment and its dose-response relation with adult symptomatology: findings in a sample of adult survivors of sexual abuse. Child Abuse Negl. (2017) 65:99–111. doi: 10.1016/j.chiabu.2017.01.008
11. Pierce J, Abbey A, Wegner R. Mediators of the association between childhood emotional maltreatment and young adult Men's life satisfaction. J Interpers Violence. (2018) 33(4):595–616. doi: 10.1177/0886260515609584
12. Horan JM, Widom CS. From childhood maltreatment to allostatic load in adulthood: the role of social support. Child Maltreat. (2015) 20(4):229–39. doi: 10.1177/1077559515597063
13. Herrenkohl TI, Jung H, Klika JB, Mason WA, Brown EC, Leeb RT, et al. Mediating and moderating effects of social support in the study of child abuse and adult physical and mental health. Am J Orthopsychiatry. (2016) 86(5):573–83. doi: 10.1037/ort0000136
14. Cohen S. Social relationships and health. Am Psychol. (2004) 59(8):676–84. doi: 10.1037/0003-066X.59.8.676
15. Edwards RR, Dworkin RH, Sullivan MD, Turk DC, Wasan AD. The role of psychosocial processes in the development and maintenance of chronic pain. J Pain. (2016) 17(9 Suppl):T70–92. doi: 10.1016/j.jpain.2016.01.001
16. Sturgeon JA, Zautra AJ. Social pain and physical pain: shared paths to resilience. Pain Manag. (2016) 6(1):63–74. doi: 10.2217/pmt.15.56
17. Che X, Cash R, Ng SK, Fitzgerald P, Fitzgibbon BM. A systematic review of the processes underlying the main and the buffering effect of social support on the experience of pain. Clin J Pain. (2018) 34(11):1061–76. doi: 10.1097/AJP.0000000000000624
18. Lopez-Martinez AE, Esteve-Zarazaga R, Ramirez-Maestre C. Perceived social support and coping responses are independent variables explaining pain adjustment among chronic pain patients. J Pain. (2008) 9(4):373–9. doi: 10.1016/j.jpain.2007.12.002
19. Freitas RPA, Andrade SC, Spyrides MHC, Micussi M, Sousa MBC. Impacts of social support on symptoms in Brazilian women with fibromyalgia. Rev Bras Reumatol Engl Ed. (2017) 57(3):197–203. doi: 10.1016/j.rbr.2016.05.002
20. Hughes S, Jaremka LM, Alfano CM, Glaser R, Povoski SP, Lipari AM, et al. Social support predicts inflammation, pain, and depressive symptoms: longitudinal relationships among breast cancer survivors. Psychoneuroendocrinology. (2014) 42:38–44. doi: 10.1016/j.psyneuen.2013.12.016
21. Crockett KB, Turan B. Moment-to-moment changes in perceived social support and pain for men living with HIV: an experience sampling study. Pain. (2018) 159(12):2503–11. doi: 10.1097/j.pain.0000000000001354
22. Richmond NL, Meyer ML, Hollowell AG, Isenberg EE, Domeier RM, Swor RA, et al. Social support and pain outcomes after trauma exposure among older adults: a multicenter longitudinal study. Clin J Pain. (2018) 34(4):366–74. doi: 10.1097/AJP.0000000000000545
23. Uchino BN, Trettevik R, Kent de Grey RG, Cronan S, Hogan J, Baucom BRW. Social support, social integration, and inflammatory cytokines: a meta-analysis. Health Psychol. (2018) 37(5):462–71. doi: 10.1037/hea0000594
24. Liu YZ, Wang YX, Jiang CL. Inflammation: the common pathway of stress-related diseases. Front Hum Neurosci. (2017) 11:316. doi: 10.3389/fnhum.2017.00316
25. Harte S, Harris R, Clauw D. The neurobiology of central sensitization. J Appl Biobehav Res. (2018) 23:e12137. doi: 10.1111/jabr.12137
26. Zhou W, Meng J, Zhang J. Does low grade systemic inflammation have a role in chronic pain? Front Mol Neurosci. (2021) 14:785214. doi: 10.3389/fnmol.2021.785214
27. Alhalal E, Ford-Gilboe M, Wong C, AlBuhairan F. Factors mediating the impacts of child abuse and intimate partner violence on chronic pain: a cross-sectional study. BMC Womens Health. (2018) 18(1):160. doi: 10.1186/s12905-018-0642-9
28. Springer KW. Childhood physical abuse and midlife physical health: testing a multi-pathway life course model. Soc Sci Med. (2009) 69(1):138–46. doi: 10.1016/j.socscimed.2009.04.011
29. Hassett AL, Wasserman R, Goesling J, Rakovitis K, Shi B, Brummett CM. Longitudinal assessment of pain outcomes in the clinical setting: development of the “APOLO” electronic data capture system. Reg Anesth Pain Med. (2012) 37(4):398–402. doi: 10.1097/AAP.0b013e3182524672
30. Pierce J, Moser S, Hassett AL, Brummett CM, Christianson JA, Goesling J. Influence of abuse history on concurrent benzodiazepine and opioid use in chronic pain patients. J Pain. (2019) 20(4):473–80. doi: 10.1016/j.jpain.2018.10.009
31. Brummett CM, Bakshi RR, Goesling J, Leung D, Moser SE, Zollars JW, et al. Preliminary validation of the Michigan body map. Pain. (2016) 157(6):1205–12. doi: 10.1097/j.pain.0000000000000506
32. Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, et al. The American college of rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. (2010) 62(5):600–10. doi: 10.1002/acr.20140
33. Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Hauser W, Katz RS, et al. Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR preliminary diagnostic criteria for fibromyalgia. J Rheumatol. (2011) 38(6):1113–22. doi: 10.3899/jrheum.100594
34. Cleeland CS, Ryan KM. Pain assessment: global use of the brief pain inventory. Ann Acad Med Singapore. (1994) 23:129–38. PMID: 80802198080219
35. van Reemst L, Fischer TF, Zwirs BW. Social information processing mechanisms and victimization: a literature review. Trauma Violence Abuse. (2016) 17(1):3–25. doi: 10.1177/1524838014557286
36. Gibb BE, Schofield CA, Coles ME. Reported history of childhood abuse and young adults’ information-processing biases for facial displays of emotion. Child Maltreat. (2009) 14(2):148–56. doi: 10.1177/1077559508326358
37. Nguyen TP, Karney BR, Bradbury TN. Childhood abuse and later marital outcomes: do partner characteristics moderate the association? J Fam Psychol. (2017) 31(1):82–92. doi: 10.1037/fam0000208
38. Whisman MA. Dyadic perspectives on trauma and marital quality. Psychol Trauma Theory Res Pract Policy. (2014) 6(3):207–15. doi: 10.1037/a0036143
39. Banford Witting A, Busby D. The long arm of trauma during childhood: associations with resources in couple relationships. J Marital Fam Ther. (2019) 45(3):534–49. doi: 10.1111/jmft.12354
40. Knapp AE, Knapp DJ, Brown CC, Larson JH. Conflict resolution styles as mediators of female child sexual abuse experience and heterosexual couple relationship satisfaction and stability in adulthood. J Child Sex Abus. (2017) 26(1):58–77. doi: 10.1080/10538712.2016.1262931
41. Lakey B, Cassady PB. Cognitive processes in perceived social support. J Pers Soc Psychol. (1990) 59(2):337–43. doi: 10.1037/0022-3514.59.2.337
42. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am J Prev Med. (1998) 14(4):245–58. doi: 10.1016/S0749-3797(98)00017-8
43. Fitzgerald M, Berthiaume K. A longitudinal investigation into marital quality as a mediator linking childhood abuse to positive and negative affective symptoms. J Gerontol B Psychol Sci Soc Sci. (2021) 76(10):2112–20. doi: 10.1093/geronb/gbab095
44. Schrepf A, Williams DA, Gallop R, Naliboff BD, Basu N, Kaplan C, et al. Sensory sensitivity and symptom severity represent unique dimensions of chronic pain: a MAPP research network study. Pain. (2018) 159(10):2002–11. doi: 10.1097/j.pain.0000000000001299
45. Woods SB, Priest JB, Kuhn V, Signs T. Close relationships as a contributor to chronic pain pathogenesis: predicting pain etiology and persistence. Soc Sci Med. (2019) 237:112452. doi: 10.1016/j.socscimed.2019.112452
46. McCracken LM. Social context and acceptance of chronic pain: the role of solicitous and punishing responses. Pain. (2005) 113(1–2):155–9. doi: 10.1016/j.pain.2004.10.004
47. Hill EM. Quality of life and mental health among women with ovarian cancer: examining the role of emotional and instrumental social support seeking. Psychol Health Med. (2016) 21(5):551–61. doi: 10.1080/13548506.2015.1109674
48. Helgeson VS. Two important distinctions in social support: kind of support and perceived versus received. J Appl Soc Psychol. (1993) 23(10):825–45. doi: 10.1111/j.1559-1816.1993.tb01008.x
49. Hart-Johnson T, Green CR. The impact of sexual or physical abuse history on pain-related outcomes among blacks and whites with chronic pain: gender influence. Pain Med. (2012) 13(2):229–42. doi: 10.1111/j.1526-4637.2011.01312.x
50. Havig K. The health care experiences of adult survivors of child sexual abuse: a systematic review of evidence on sensitive practice. Trauma Violence Abuse. (2008) 9(1):19–33. doi: 10.1177/1524838007309805
51. Clark L, Beesley H, Holcombe C, Salmon P. The influence of childhood abuse and adult attachment style on clinical relationships in breast cancer care. Gen Hosp Psychiatry. (2011) 33(6):579–86. doi: 10.1016/j.genhosppsych.2011.07.007
52. Green B, Kaltman S, Frank L, Glennie M, Subramanian A, Fritts-Wilson M, et al. Primary care providers’ experiences with trauma patients: a qualitative study. Psychol Trauma Theory Res Pract Policy. (2011) 3(1):37–41. doi: 10.1037/a0020097
Keywords: childhood abuse, emotional support, instrumental support, widespread pain, pain severity, depressive symptoms, anxiety symptoms, social support
Citation: Pierce J, Presto J, Hinckley E, Hassett AL, Dickens J, Schneiderhan JR, Grace K and McAfee J (2022) Perceived social support partially mediates the association between childhood abuse and pain-related characteristics. Front. Pain Res. 3:1075605. doi: 10.3389/fpain.2022.1075605
Received: 20 October 2022; Accepted: 23 November 2022;
Published: 22 December 2022.
Edited by:
Cheryl L. Stucky, Medical College of Wisconsin, United StatesReviewed by:
Natasha Gallant, University of Regina, CanadaLaura Payne, Harvard Medical School, United States
© 2022 Pierce, Presto, Hinckley, Hassett, Dickens, Schneiderhan, Grace and McAfee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jennifer Pierce am1ib2lrQG1lZC51bWljaC5lZHU=
Specialty Section: This article was submitted to Non-Pharmacological Treatment of Pain, a section of the journal Frontiers in Pain Research
 Jennifer Pierce
Jennifer Pierce Jacob Presto1
Jacob Presto1 Afton L. Hassett
Afton L. Hassett