
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol. , 21 February 2025
Sec. Cancer Imaging and Image-directed Interventions
Volume 15 - 2025 | https://doi.org/10.3389/fonc.2025.1501165
Background: While there have been prior reports on pulmonary nodule (PN) localization through computed tomography (CT)-guided soft hook-wire (SHW) placement, there remains a dearth of studies specifically focused on the CT-guided SHW localization of multiple PNs. This study was thus designed to specifically evaluate the efficacy and safety of this localization strategy in patients with multiple PNs.
Methods: In total, 43 consecutive patients with multiple PNs underwent CT-guided SHW localization followed by video-assisted thoracoscopic surgery (VATS) to resent these PNs in our hospital between January 2022 and December 2022. A control group consisting of 140 individuals who underwent the CT-guided SHW localization of a single PN during the same interval was also selected. Both groups were analyzed retrospectively for safety and efficacy outcomes.
Results: The final study population included 43 patients (94 PNs) in the multiple PN group, and 140 patients (140 PNs) in the single PN group, with all patients having undergone CT-guided SHW localization of these PNs. A one-stage procedure was employed for the localization of multiple PNs. The respective rates of technical success for SHW localization in the multiple and single PN groups were 98.9% and 100% (P = 0.402). The duration of localization in the multiple PN group was significantly longer than that in the single PN group (P = 0.001). The respective pneumothorax rates in the multiple and single PN groups were 32.5% (14/43) and 15.7% (22/140) (P = 0.015), while the corresponding lung hemorrhage incidence rates were 48.8% (21/43) and 36.4% (51/140) (P = 0.145). All PNs successfully underwent limited VATS resection, with a one-stage VATS procedure having been used for the resection of multiple PNs in a given patient.
Conclusions: CT-guided SHW localization is a safe and effective means of localizing multiple PNs in a single patient. This simultaneous localization of multiple PNs can provide effective guidance for the subsequent one-stage limited VATS resection of these nodules.
Computed tomography (CT)-based screening is often used to evaluate patients facing a high risk of lung cancer, and it has been estimated to decrease lung cancer-associated mortality rates by 20% (1–3). Early-stage lung cancer is generally characterized by pulmonary nodules (PNs) detectable through CT scanning (1–3). While CT-based follow-up is generally employed for low-risk PNs (4), additional procedures are generally necessary for high-risk PNs, including CT-guided biopsy and video-assisted thoracoscopic surgery (VATS) resection (4). While CT-guided biopsy is a mini-invasive procedure with high levels of diagnostic accuracy, the rate of diagnostic failure for this procedure is still in the range of 10% (5).
Limited wedge or segmental VATS resection procedures remain the standard diagnostic approach for PNs, and in cases where PN staging is lower than invasive lung cancer, such resection can also be curative (6–8). To ensure that limited VATS resection is a success, clinicians have performed the CT-guided hook-wire (HW) localization of target PNs before VATS procedures (9–11). In patients with more than one high-risk PN, these multiple nodules can still be resected through a one-stage VATS procedure. In these cases, preoperative localization of the multiple nodules is particularly important, given that successful limited resection allows for the maximal preservation of respiratory function (12).
Conventional HW localization strategies generally lead to high rates of complications for patients harboring multiple PNs (13), with these rates reportedly rising as high as 64% (14). The primary cause of these complications is the rigidity of the HW material conventionally used in this approach. This issue has prompted some researchers to substitute soft HW (SHW) materials in place of the conventional rigid HW apparatus (15). While both such devices contain the hook structure, in the SHW version a soft suture is substituted in place of the stiff wire. This affords marked reductions in the incidence of localization-related complications (16). However, there has been little research to date specifically examining outcomes associated with the CT-guided SHW localization for multiple PNs.
This study was devised to evaluate the safety and clinical efficacy of the preoperative CT-guided SHW localization of multiple PNs.
This study was retrospective in design and received approval from the Ethics Committee of Xuzhou Central Hospital, and the Ethics Committee waived the requirement for written informed consent.
In total, 43 consecutive multiple PNs patients who received CT-guided SHW localization of these nodules followed by VATS resection between January 2022 and December 2022 were included in the present study. Inclusion criteria for these patients were as follows: (i) patients with more than one high-risk PN; (ii) patients with multiple unilateral PNs; (iii) the solid PNs with the > 10 mm PN-pleura distance, the GGNs regardless of PN-pleura distance; and (iv) patients 18-75 years of age. Patients were excluded if they exhibited (i) hilar PNs; (ii) PNs < 6 mm in diameter; and (iii) patients with severe cardiac, liver, kidney, pulmonary, or coagulatory disorders. As a control group, 140 patients who had undergone the CT-guided SHW localization for a single PN over the same period were also included in this study. High-risk PNs were assessed as per the Fleischner Society Guideline Recommendations (4).
SHW localization procedures were performed with local anesthesia using a 16-row CT instrument (Figures 1A, B). The positioning of patients was selected according to target LN location and the related rib and vascular structures. The selection of the needle pathway was based on the position of the patient, selecting the pathway that minimized the distance between the skin and the target nodule. This procedure utilized a 20G guiding needle that was 10-15 cm in length (Senscure, Ningbo, China). This needle was placed into the lung lobe according to the selected needle pathway, and repeated CT scanning was used to confirm the position of needle tip. If the tip of the needle was located within 10 mm of the target nodule, SHW placement was performed (Figures 1C, D). During SHW placement, the anchor was inserted close to the target PN, and the needle was then removed, leaving the tri-colored suture attached to the anchor within the needle track while the distal suture end remained outside of the pleura. A one-stage procedure was used to localize multiple PNs in patients (Figures 1E, F). A final series of CT scans was used to evaluate patients for post-localization complications.
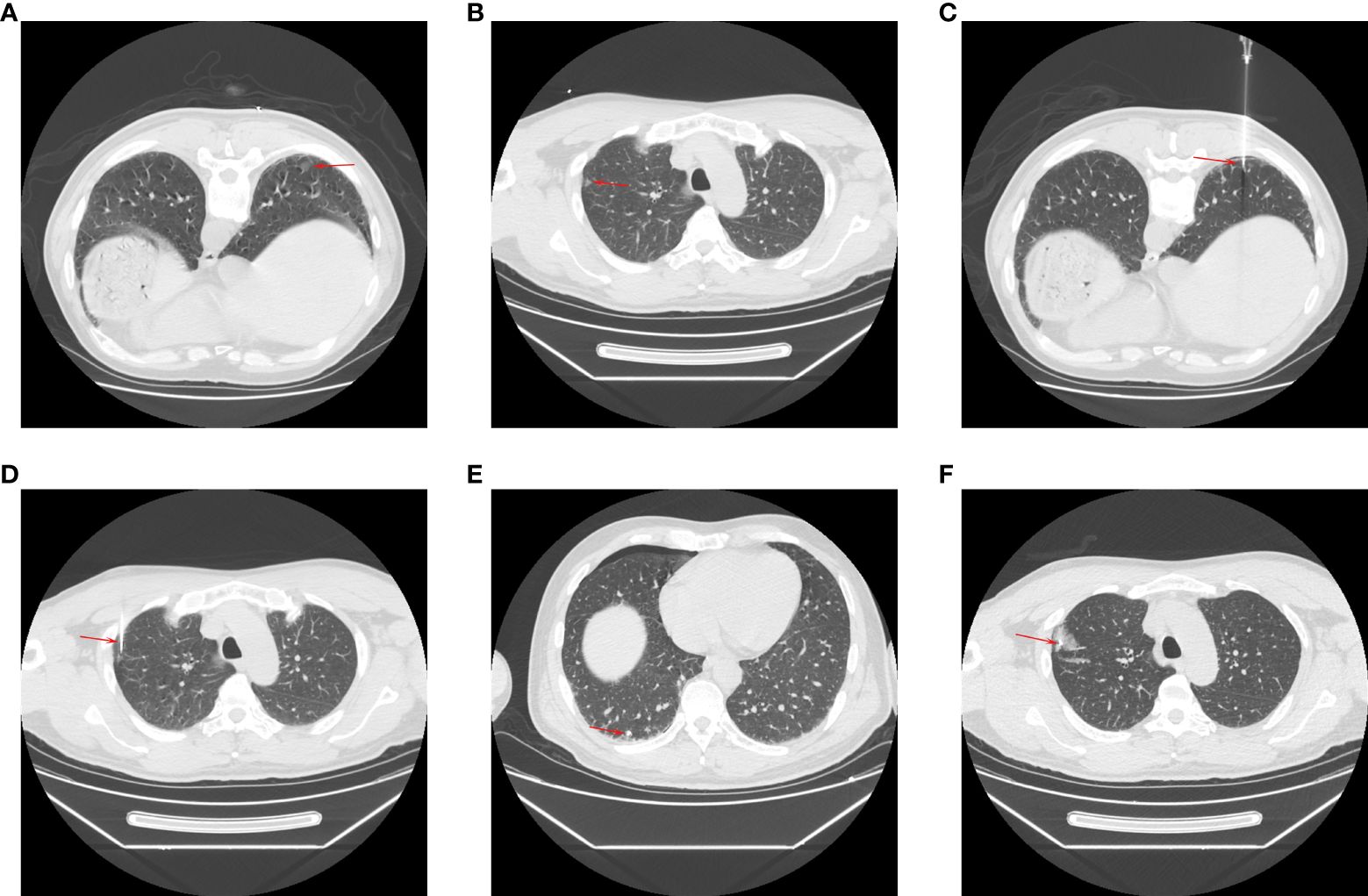
Figure 1. The procedures of CT-guided SHW localization for multiple PNs. The CT showed the PNs in (A) right lower (arrow) and (B) right upper (arrow) lobes. The needles (C, D) were inserted (arrows) near the PNs. The SHWs (e and f) were placed (arrows) near the PNs. (E, F) The intraoperative photos of the localization.
All VATS procedures were performed via a standard two-incision approach under general anesthesia within 3 h of localization. For resection, patients were placed in the lateral decubitus position, after which a 3-5 mm incision through the 4/5th intercostal space was made along the anterior axillary line. The SHW localization marker was then used to guide limited resection. PN depth was evaluated based on preoperative CT images and the palpation of the SHW tip intraoperatively. A cutting suture device was used to perform limited resection based on PN depth. Segmental resection was performed if the margin was more than 2 cm from the edge of the PN, while wedge resection was performed in the remaining cases. Rapid pathological examination was performed for all resected PNs. In cases where PNs were diagnosed as invasive cancers, further lobectomy and lymphadenectomy were performed. For cases in which patients were diagnosed with mini-invasive cancer, lymph node sampling was performed. PNs staged at or below cancer in situ did not require any further procedures. A one-stage VATS procedure was used to resect all PNs. When patients had invasive tumors, lobectomy was performed for the nodule with the most advanced staging.
SHW localization procedures were defined as a technical success if (i) the SHW localization marker was visible while performing the VATS procedure, (ii) SHW dislodgement did not occur, and (iii) the target PN was located within the resected lung parenchymal tissue (wedge or segment). The duration of localization was calculated from the first to the last CT scans points. VATS time was measured as the interval between the first incision and wound closure.
Localization technical success was the primary endpoint for this study. Secondary endpoints included duration of localization, localization-related complications, VATS duration, surgery type, and final diagnosis.
Normally distributed [skewed] data were reported as means ± standard deviations [medians], and were compared with independent sample t-tests [Mann-Whitney U tests]. Categorical data were reported as numbers (%) and compared with χ2 tests. Risk factors related to post-localization complications were detected through logistic regression analyses, with factors exhibiting significance in univariate analyses (P < 0.1) being incorporated into multivariate analyses. P < 0.05 was the threshold for significance, and SPSS 16.0 (SPSS Inc., IL, USA) was used to perform all analyses.
A total of 43 patients underwent the CT-guided SHW localization of multiple PNs (94 total PNs) from January 2022 through December 2022, while 140 patients underwent SHW localization for single PNs over this same interval. One, 6, and 36 patients in the multiple PN group underwent the localization of 4, 3, and four 2 PNs. Baseline data for these patients are presented in Table 1.
SHW localization achieved respective technical success rates of 98.9% and 100% in the multiple PN and single PN groups (P = 0.402). SHW dislodgement resulted in technical failure for one PN in a patient in the multiple PN group. The localization of multiple PNs was associated with the significant prolongation of localization time relative to that for a single PN (P = 0.001). In the multiple PN group, 23 patients underwent positional changes during localization (Table 2).
Pneumothorax rates in the multiple PN and single PN groups were 32.5% (14/43) and 15.7% (22/140), respectively (P = 0.015). Longer localization time was identified as being independently associated with the risk of pneumothorax through univariate and multivariate analyses (Table 3).
Lung hemorrhage rates in the multiple PN and single PN groups were 48.8% (21/43) and 36.4% (51/140), respectively (P = 0.145). No independent risk factors for lung hemorrhage were successfully identified (Table 4).
No localization-associated complications resulted in subsequent VATS resection procedures being delayed or otherwise affected. Therefore, the localization-associated complications were not specially managed.
Limited VATS resection procedures were successful for all target PNs among patients in this study (Table 5). Even though one nodule experienced technical failure for the SHW localization procedure in the multiple PN group, limited resection was successfully performed as the site of the needle puncture remained visible in the visceral pleura intraoperatively while performing VATS resection. In all instances, a one-stage VATS procedure was used to resect multiple PNs. Both groups were comparable in terms of limited VATS resection types (P = 0.577) and VATS duration (P = 0.200). Three of the patients in the multiple PN group exhibited multiple invasive adenocarcinoma lesions, and in these cases, additional lobectomy was performed for the most advanced lesion. Table 5 presents the pathological diagnoses for all lesions in this study.
Of patients exhibiting high-risk PNs, 22.2%-24.5% present with more than one high-risk nodule (17, 18). In these patients with multiple PNs, advantages to CT-guided one-stage localization procedures include (i) the ability of one-stage procedures to enable VATS resection through a one-stage procedure, obviating the requirement for stages resection, and (ii) one-stage localization procedures can aid in the resection of all PNs with a minimal resection range.
In this study, both the safety and efficacy of the CT-guided SHW localization of ipsilateral multiple PNs were assessed. This approach yielded respective technical success rates for the localization procedure itself and subsequent limited VATS resection of 98.9% and 100%. Relative to the localization of a single PN, localizing multiple PNs required more time but was still an effective one-stage localization procedure in these patients, facilitating the one-stage limited VATS resection of multiple target nodules.
Pneumothorax and lung hemorrhage rates following the localization of multiple PNs have previously been reported to range from 27.5%–56.8% and 18.9%–60%, respectively (9, 17, 19). The corresponding rates in this study (32.5% and 48.8%) fell within this range. The high complication rates were mainly attributed to that the multiple PNs localization required more needle puncture procedures. While these complications were more common among patients who underwent the localization of multiple PNs, none resulted in any delays or other changes in the VATS resection procedures, emphasizing the safety of CT-guided SHW localization for multiple PNs.
Coil and liquid-based materials have also been employed to localize multiple PNs (17–19). Liquid-based materials are inexpensive, have a good safety profile, and can be readily deployed, but they suffer from diffusion such that localization failure can arise in some cases. Coil localization is a more complex procedure as a consequence of the shape of the coil and the requirement that its distal end be proximal to the PN while its proximal end extends beyond the visceral pleura (19). Coils also suffer from the risk of unintentionally being inserted fully into the parenchyma of the lung. In such cases, fluoroscopy-based VATS procedures must be conducted such that both patients and the surgeons themselves are exposed to radiation.
VATS procedure durations and blood loss volumes were similar in both patient groups (P = 0.200 and 0.213). This may be related to the fact that the rate of invasive adenocarcinoma was lower in the multiple PN group relative to the single PN group (12.8% vs. 32.1%, P = 0.007), and invasive adenocarcinomas generally necessitate additional lobectomy. In addition, this study included 3 patients with multiple invasive adenocarcinoma lesions, and additional lobectomy was only performed for the most advanced lesion in these cases. As a result, the rate of additional lobectomy was reduced in the multiple PN group relative to the single PN group (9.6% vs. 32.1%, P = 0.001).
There are certain limitations to this study, the most prominent of which is the retrospective study design. As the number of PNs per patient cannot be controlled, performing a randomized controlled trial was not possible. Secondly, some of the baseline data were not balanced between patient groups, including PN etiology, location, and diameter, potentially contributing to additional bias. Third, no comparisons were made between SHW and other localization materials in this patient population, underscoring the need for future comparative analyses aimed at establishing the optimal materials for the localization of multiple PNs.
In summary, CT-guided SHW localization is a safe and effective means of localizing multiple PNs in a single patient. This simultaneous localization of multiple PNs can provide effective guidance for the subsequent one-stage limited VATS resection of these nodules.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethics Committee of Xuzhou Central Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because this is a retrospective study.
G-CL: Methodology, Writing – original draft. Z-LW: Data curation, Methodology, Writing – original draft. Y-BS: Methodology, Validation, Writing – review & editing. J-YW: Supervision, Writing – review & editing. Y-FF: Conceptualization, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Jiangsu Important Subject Development (ZDXK202237).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. (2011) 365:395–409. doi: 10.1056/NEJMoa1102873
2. National Lung Screening Trial Research Team, Church TR, Black WC, Aberle DR, Berg CD, Clingan KL, et al. Results of initial low-dose computed tomographic screening for lung cancer. N Engl J Med. (2013) 368:1980–91. doi: 10.1056/NEJMoa1209120
3. Prokop M. Lung cancer screening: the radiologist’s perspective. Semin Respir Crit Care Med. (2014) 35:91–8. doi: 10.1055/s-0033-1363455
4. MacMahon H, Naidich DP, Goo JM, Lee KS, Leung ANC, Mayo JR, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: from the fleischner society 2017. Radiology. (2017) 284:228–43. doi: 10.1148/radiol.2017161659
5. Liu GS, Wang SQ, Liu HL, Liu Y, Fu YF, Shi YB. Computed tomography-guided biopsy for small (≤20 mm) lung nodules: A meta-analysis. J Comput Assist Tomogr. (2020) 44:841–6. doi: 10.1097/RCT.0000000000001071
6. Fu YF, Zhang M, Wu WB, Wang T. Coil localization-guided video-assisted thoracoscopic surgery for lung nodules. J Laparoendosc Adv Surg Tech A. (2018) 28:292–7. doi: 10.1089/lap.2017.0484
7. Zhang ZD, Wang HL, Liu XY, Xia FF, Fu YF. Methylene blue versus coil-based computed tomography-guided localization of lung nodules. Thorac Cardiovasc Surg. (2020) 68:540–4. doi: 10.1055/s-0040-1708836
8. Aoun HD, Littrup PJ, Heath KE, Adam B, Prus M, Beydoun R, et al. Methylene blue/collagen mixture for CT-guided presurgical lung nodule marking: high efficacy and safety. J Vasc Interv Radiol. (2020) 31:1682.e1–1682.e7. doi: 10.1016/j.jvir.2020.04.028
9. Wang JL, Xia FF, Dong AH, Lu Y. Comparison between coil and hook-wire localization before video-assisted thoracoscopic surgery for lung nodules: a systematic review and meta-analysis. Wideochir Inne Tech Maloinwazyjne. (2022) 17:441–9. doi: 10.5114/wiitm.2022.116396
10. Wang SJ, Gao XX, Hui H, Li N, Zhou Y, Yin HT. Comparison between preoperative hook-wire and liquid material localization for pulmonary nodules: a meta-analysis. Wideochir Inne Tech Maloinwazyjne. (2023) 18:401–9. doi: 10.37766/inplasy2023.5.0082
11. Wang T, Ma S, Yan T, Song J, Wang K, He W, et al. Computed tomography guided hook-wire precise localization and minimally invasive resection of pulmonary nodules. Zhongguo Fei Ai Za Zhi. (2015) 18:680–5. doi: 10.5114/wiitm.2023.130330
12. Fu YF, Gao YG, Zhang M, Wang T, Shi YB, Huang YY. Computed tomography-guided simultaneous coil localization as a bridge to one-stage surgery for multiple lung nodules: a retrospective study. J Cardiothorac Surg. (2019) 14:43. doi: 10.1186/s13019-019-0870-6
13. Tang X, Jian HM, Guan Y, Miao J, Liang X. Computed tomography-guided localization for multiple pulmonary nodules: a meta-analysis. Wideochir Inne Tech Maloinwazyjne. (2021) 16:641–7. doi: 10.5114/wiitm.2021.104199
14. Kadeer X, Wang L, Zhang L, Shi W, Chen C. Modified hook-wire placement technique for localizing multiple pulmonary nodules. J Surg Oncol. (2018) 118:1188–93. doi: 10.1002/jso.v118.7
15. Huang YY, Liu X, Shi YB, Wang T. Preoperative computed tomography-guided localization for lung nodules: localization needle versus coil. Minim Invasive Ther Allied Technol. (2022) 31:948–53. doi: 10.1080/13645706.2022.2034647
16. Zhou WJ, Chen G, Huang YY, Peng P, Lv PH, Lv JL. Preoperative computed tomography-guided localization for pulmonary nodules: comparison between hook-wire and anchored needle localization. Wideochir Inne Tech Maloinwazyjne. (2024) 19:91–9. doi: 10.5114/wiitm.2023.134158
17. Xu L, Wang J, Liu L, Shan L, Zhai R, Liu H, et al. Computed tomography-guided cyanoacrylate injection for localization of multiple ipsilateral lung nodules. Eur Radiol. (2022) 32:184–93. doi: 10.1007/s00330-021-08101-7
18. Lin J, Wang LF, Wu A, Teng F, Xian YT, Han R. Computed tomography-guided indocyanine green localization of multiple ipsilateral lung nodules. Wideochir Inne Tech Maloinwazyjne. (2023) 18:305–12. doi: 10.5114/wiitm.2023.124272
Keywords: hook-wire, soft, localization, pulmonary nodule, multiple
Citation: Li G-C, Wu Z-L, Shi Y-B, Wang J-Y and Fu Y-F (2025) Preoperative computed tomography-guided soft hook-wire localization for multiple pulmonary nodules. Front. Oncol. 15:1501165. doi: 10.3389/fonc.2025.1501165
Received: 24 September 2024; Accepted: 10 February 2025;
Published: 21 February 2025.
Edited by:
Sharon R. Pine, University of Colorado Anschutz Medical Campus, United StatesReviewed by:
Paola Ciriaco, San Raffaele Scientific Institute (IRCCS), ItalyCopyright © 2025 Li, Wu, Shi, Wang and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing-Ya Wang, d2p5aGV0YW9AMTYzLmNvbQ==; Yu-Fei Fu, ZnV5dWZlaTE5ODVAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.