- 1Department of Neurosurgery, Cleveland Clinic, Cleveland, OH, United States
- 2Department of Molecular Medicine, Case Western Reserve University, Cleveland, OH, United States
- 3Department of Neurosurgery, Washington University, St. Louis, MO, United States
- 4Center for Cancer and Blood Disorders, Phoenix Children’s Hospital, Phoenix, AZ, United States
- 5Pediatric Hematology/Oncology, Nationwide Children’s Hospital, Columbus, OH, United States
- 6Department of Pediatrics, Sylvester Comprehensive Cancer Center, Miami, FL, United States
- 7Department of Pediatric Hematology-Oncology and Blood & Marrow Transplant, Cleveland Clinic, Cleveland, OH, United States
Pediatric diffuse midline glioma (DMG), including diffuse intrinsic pontine glioma (DIPG), are aggressive brainstem tumors with a dire prognosis, traditionally diagnosed based on MRI characteristics. The recognition that molecular characteristics may determine prognosis and response to therapy has led to a reevaluation of biopsy necessity. This comprehensive review addresses the evolving role of brainstem biopsies in diagnosing and managing these tumors – both within the context of a clinical trial and in routine clinical care. We examine practice variability around brainstem biopsies for DMG/DIPG, revealing a global inconsistency in biopsy application and perceptions amongst providers. We show that safety profiles from contemporary studies demonstrate a high diagnostic success rate with minimal permanent morbidity, supporting the feasibility of biopsies in expert centers. Beyond the safety angle, we discuss the utility of biopsies in enabling personalized medicine, highlighting how molecular profiling has been used in multiple centers to guide targeted therapies. We present initial evidence from case studies and registry reports to address whether these molecularly targeted approaches are 1) clinically feasible, and 2) likely to extend survival. Furthermore, we present evidence to support the notion that biopsies facilitate the design of more refined clinical trials, shifting from a one-size-fits-all model to molecularly stratified studies. We discuss how this new paradigm for trial design is likely necessary in the context of DMG/DIPG given the lack of progress in this disease for the last several decades. Future directions discussed in the review include liquid biopsy techniques to complement or replace tissue sampling, aiming to enhance diagnostic precision and treatment monitoring.
1 Introduction
The role of biopsies in the diagnosis and management of children with brainstem tumors has been debated in the academic literature for several decades. The majority of primary pediatric brainstem tumors are H3K27-altered diffuse midline gliomas (DMGs), and outcomes for these patients are universally poor. The median overall survival in a contemporary registry was less than 12 months (1, 2). In a seminal report from the Children’s Cancer Group in 1993, Albright et al. argued that “MR scans provide images that are virtually diagnostic of brain stem gliomas and yield prognostic information equivalent to that obtainable from biopsies [ … ] as yet no one has demonstrated that modifications in therapy based on the biopsy results contribute to improved outcome.” (3) In the three decades since the Albright report, several investigations have called into question the notion of DMG as a radiographic diagnosis by raising concerns around inter-observer variability (4) and limited specificity (5). This has left the question of biopsy as a diagnostic necessity largely unresolved. Concurrently, a vibrant debate persists over the utility of biopsy-derived molecular information in the clinical management of DMG patients given that outcomes have historically been universally poor. It is unknown if a biopsy improves progression free survival or overall outcomes. Finally, the question of whether biopsies in the pediatric brainstem are safe in contemporary neurosurgical practice has also been a focus of the literature. Collectively, these issues constitute a complex and important debate for the pediatric neuro-oncology community with important implications for patient management.
In this comprehensive review, we aim to provide a broad overview of multiple themes related to the safety and utility of pediatric brainstem biopsies. Our analyses are focused primarily on the question of biopsies as they relate to suspected diffuse midline glioma or ‘DMG’. Consistent with the 2021 WHO CNS tumors classification scheme, we employ the term ‘DMG’ to refer to diffuse midline glioma H3K27-altered. The term diffuse intrinsic pontine glioma or ‘DIPG’ is of historical significance and, as of the 2016 WHO classification, refers to a subset of diffuse midline gliomas. Classically, DIPG refers to an aggressive, expansile tumor centered specifically within the pons. In this review, we employ the updated ‘DMG’ terminology except where the source literature explicitly refers to DIPG.
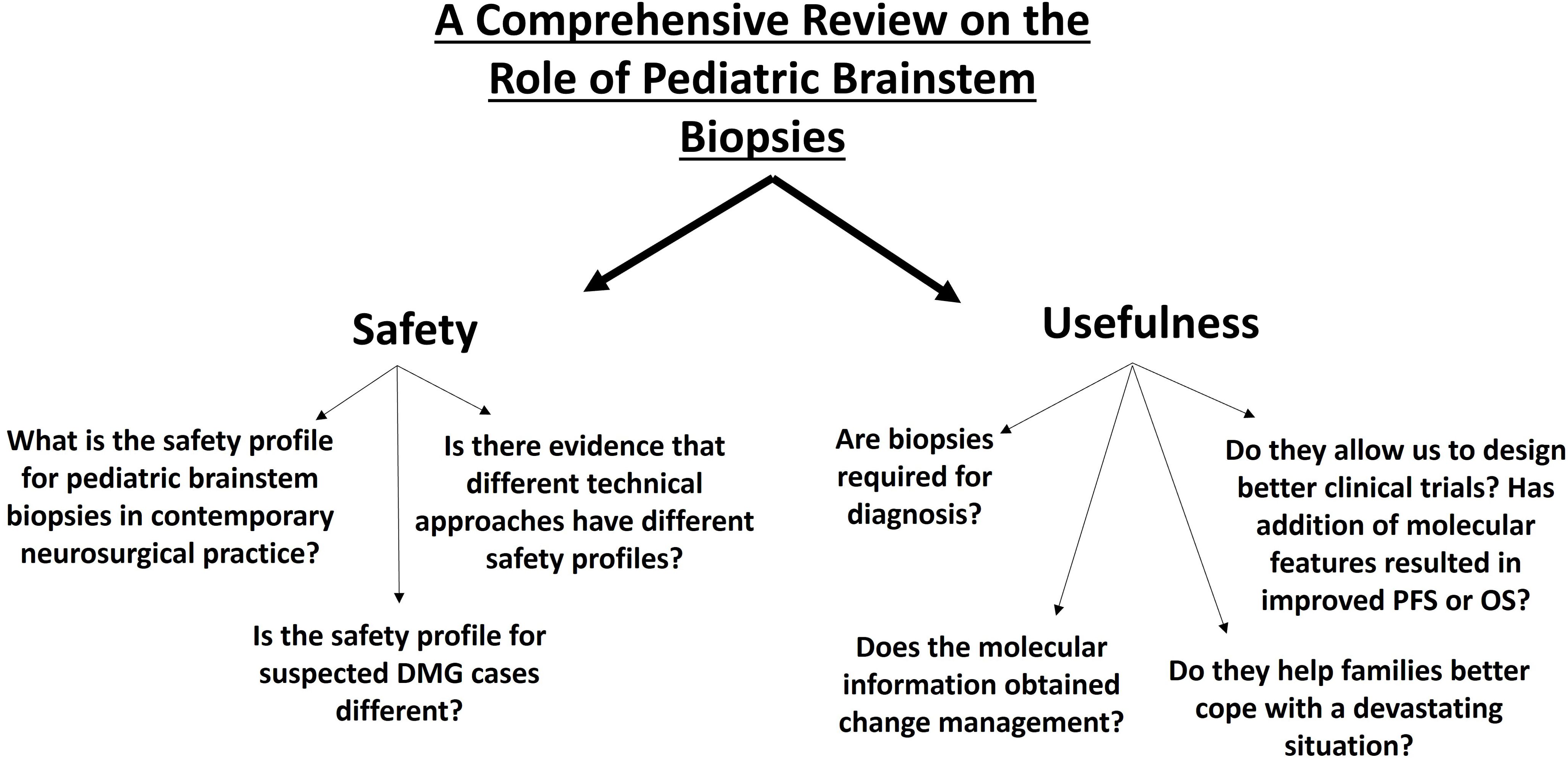
The text is arranged in the following sections (Figure 1):
1. Establishing practice variability related to pediatric brainstem biopsies.
2. Safety of pediatric brainstem biopsies.
3. Utility of pediatric brainstem biopsies.
2 Establishing practice variability related to pediatric brainstem biopsies
The 1993 Children’s Cancer Group serves as an important historical marker in the evolution of neurosurgical practice related to pediatric brainstem biopsies (3). Published at a time when MRI was rapidly becoming ubiquitous standard of care in neuro-oncology, the report is widely cited as the basis for a shift away from using biopsies to diagnose suspected brainstem gliomas. In 1996, Fredstein and Constantini formalized MRI-based radiographic hallmarks of diffuse intrinsic pontine gliomas: diffuse pontine expansion without demarcated borders, T1 hypo-intensity with T2 hyperintensity, absent (or minimal) contrast enhancement (6). In patients with these imaging findings and a rapidly progressive clinical syndrome, they argued that “performing a biopsy, whether open or stereotactic, exposes the patient to additional unnecessary risk”. As recently as 2009, Fisher, Carson et al. argued that in patients with diffusely infiltrative brainstem gliomas, expeditious enrollment in trials with aggressive therapy was reasonable and “biopsy is rarely indicated” (7).
A marked shift in the tone of the literature related to brainstem biopsies has occurred in the last decade following the publication of multiple landmark studies that have shed new light onto the molecular underpinning of brainstem gliomas. In 2012, a series of seminal studies showed that alteration in histone H3 (most notably, lysine to methionine substitution at position 27 of H3 i.e. H3K27M) was a hallmark of the disease occurring in 70-80% of DIPGs (8–10). We now understand that H3K27M induces defective spread of the Polycomb Repressive Complex2 (PRC2) across chromatin which normally catalyzes histone methylation thereby causing gene repression (11–13). H3K27M mutation thus leads to a reduction of epigenetic gene repression driving tumorigenesis. This growing molecular understanding was reflected in the 2016 WHO CNS tumor classification scheme with the definition of the new entity “diffuse midline glioma H3 K27M-mutant” and a recognition that tumors bearing this molecular alteration are Grade 4 irrespective of histological features (14). Other less frequent but significant molecular features have been identified and have potential as druggable targets including ACVR1 (15, 16), PDGFRA (17), FGFR1, PP2A (18), EGFR (19), as well as a targetable surface antigen B7-H3 (20). It is now also appreciated that enrichment of MAPK pathway alterations correlates with long term survival in patients with H3K27M-mutant tumors (21). As these molecular targets have emerged, a palpable shift in the literature around brainstem biopsies has followed with multiple voices advocating for a more widespread use of biopsies (22–25). At a minimum, it has become accepted standard of care to discuss the risks/benefits of a biopsy within a nuanced discussion with patients and their families.
Neurosurgeons have been the most widely surveyed regarding opinions and practice patterns related to brainstem biopsies in children. In 2011, Hankinson et al. published results from a survey of 86 neurosurgeons in North America. Respondents were presented 16 representative cases (including imaging and clinical scenario) and asked to comment on whether they believed the lesion to be ‘typical’ or ‘atypical’, whether they would biopsy the lesion, and which surgical approach they would use. The study showed that no tumor was universally judged to be either typical or atypical by all neurosurgeons. In fact, 75% agreement regarding whether a tumor was typical or atypical was found in a minority (44%) of cases. Even where surgeons judged that a lesion was typical, many (range 1.2% to 66.7% based on the lesion) would still offer biopsy. When asked if, as a general matter, surgeons would offer biopsy for a typical diffuse pontine glioma as part of a multicenter trial, 69.4% said they would (4). In 2020, Tejada et al. published results from a survey of 73 neurosurgeons undertaken by the Neurosurgery Working Group of the International Society of Pediatric Oncology (SIOP) Europe Brain Tumor Group. Only 14% of surgeons felt that biopsy was necessary for the diagnosis of DIPG. 57% stated that they would only perform a biopsy within the context of a prospective trial. Notably, 65% felt that the biopsy was justified if the trial investigated molecular targets without planning to use its outcome directly towards treatment. In another European survey-based study from the SIOP-BTG, Khouly et al. reported responses from 74 healthcare providers of whom the majority (88%) were pediatric oncologists. 13.5% of respondents stated that they biopsied all DIPG patients, while 28.4% stated that they biopsied most. Notably, 16% said that they never biopsied DIPG patients (26).
The role of biopsy in the care of children with diffuse midline glioma continues to evolve within the neuro-oncology community. It is clear that concurrent with the growing understanding of the molecular pathophysiology of the disease and resultant molecular heterogeneity, there has been a gradual shift away from the position of treating DIPG as a purely radiographic diagnosis.
3 Safety of pediatric brainstem biopsies
3.1 What are the rates of temporary and permanent morbidity in contemporary case series particularly for suspected DMG cases?
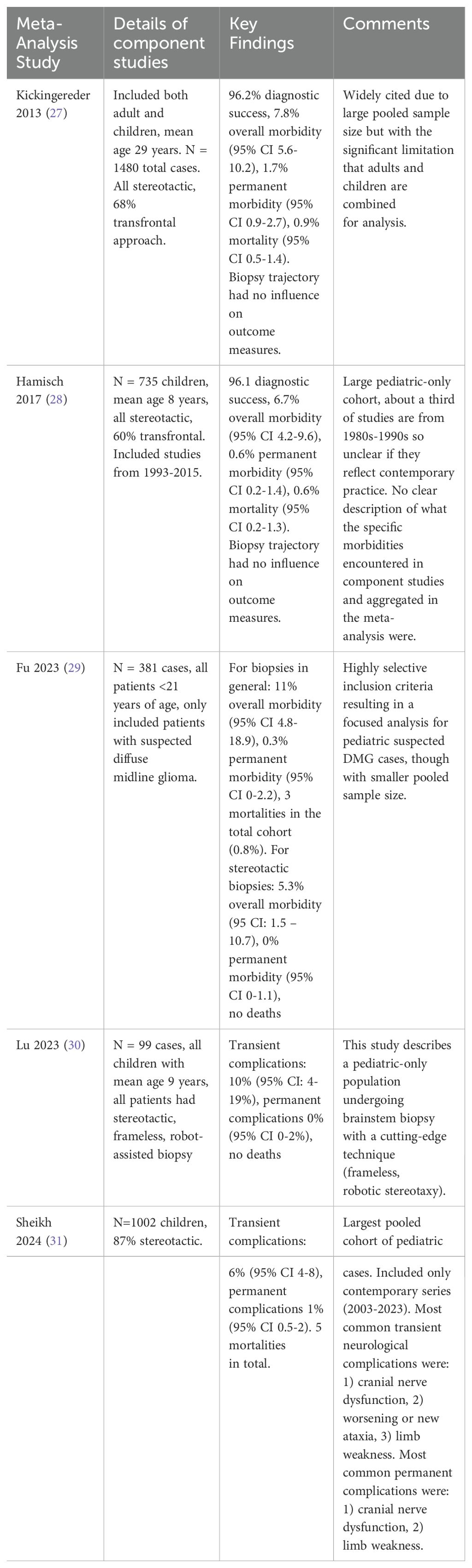
Given the highly eloquent nature of the brainstem structures that usually form the epicenter of diffuse midline gliomas, there has been sustained interest in ascertaining accurate safety profile data related to biopsies. Several case series from around the world have been published over the last three decades. Data from these case series have been aggregated for review in a handful of meta-analyses (Table 1).
A key limitation for these analyses is that data are principally derived from retrospective case-series, which limits the quality of pooled evidence. Furthermore, surgical case series with high complication rates are less likely to appear in the academic literature than studies with favorable complication rates. These limitations notwithstanding, some basic risk estimates are ascertainable:
a. Across meta-analyses, the rate of permanent complications after pediatric brainstem biopsies is low: the upper limit of the 95% confidence interval (CI) of the pooled estimates does not exceed 2.2% for any of the pediatric meta-analyses. The most commonly encountered permanent complication is new or worsening cranial neuropathy or limb weakness.
b. Though permanent complications are rare, temporary complications occur in a significant proportion of patients, with two of the pediatric meta-analyses reporting upper limit of 95% CI transient complication rate around 19%. The most frequently encountered are new/worsening cranial neuropathies, ataxia, or limb weakness. Studies have not consistently reported the time to resolution for these temporary complications.
c. Mortalities are rare. In the largest pediatric meta-analysis (pooled cohort of 1002 children), only 5 mortalities were found (Table 2):
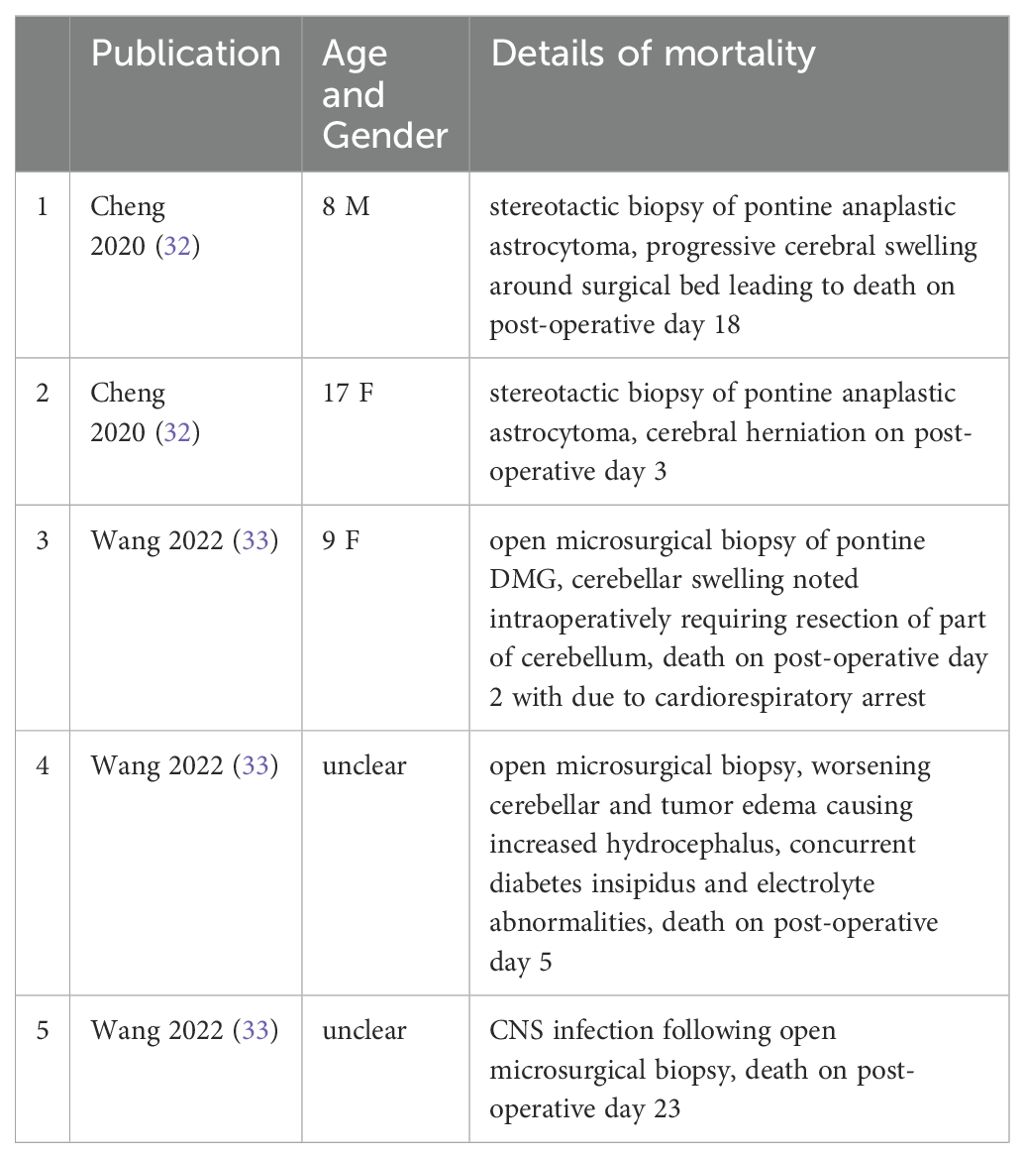
Table 2. List of reported mortalities from published pediatric brainstem biopsy surgical case series.
In addition to the above listed meta-analyses, one important contemporary prospective multi-center study has added notable insights. In 2018, Gupta et al. published the results of the DIPG Biology and Treatment Study (DIPG-BATS) (34). This prospective trial involved upfront biopsy of suspected DIPG prior to definitive treatment. 50 pediatric brainstem biopsies were performed at 23 institutions across the United States, with a standardized operative protocol (stereotactic, trans-cerebellar via the middle cerebellar peduncle, an initial 3mmx1mm specimen was taken for diagnosis and up to 6 total specimens could be taken). No deaths were reported related to the surgery, however 1 death occurred 2 weeks postoperatively and was attributed to disease progression. In that one patient, worsening hydrocephalus after biopsy prompted ventriculoperitoneal shunt placement. The patient continued to deteriorate with diffuse brainstem edema and punctate hemorrhage. Only one patient experienced a permanent neurological complication attributed to surgery (hemiparesis). One patient developed dysarthria that did not resolve though this was thought to be partially related to radiation. The DIPG-BATS study is valuable because it is multi-centered and highly specific to the case of pediatric patients with suspected DIPG. The major lesson of the DIPG-BATS experience is that safe stereotactic trans-cerebellar biopsies in these children are feasible in high-volume academic centers in North America.
3.2 What technical variations exist and is there evidence of differential safety outcomes?
Multiple surgical approaches to biopsy of brainstem lesions have been described:
1. Open microsurgical approaches were the earliest described. A suboccipital craniectomy can be used to access the floor of the fourth ventricle where sampling can be performed. Alternatively, a small retrosigmoid craniotomy can be used to sample the ventrolateral pons and cerebellopontine angle (35). In our experience, open microsurgical biopsies of brainstem lesions have become relatively uncommon in contemporary practice though they may still be appropriate in cases where it is possible to directly sample the exophytic component of atypical brainstem lesions.
2. Stereotactic approaches have been described with multiple variations (36). Frame-based and frameless stereotaxy are both commonplace. The use of robotic stereotaxy (with or without frames) has been safely used for brainstem biopsies (30). Both trans-frontal and trans-cerebellar approaches have been used, though the trans-cerebellar is now more common in our experience (37, 38). In a meta-analysis of 1002 pediatric brainstem biopsies from 2003-2023 (31), we found that 87% of cases reported were stereotactic biopsies. In the earlier half of studies (2003-2013), 90% of stereotactic cases were frame based, while in the later half (2014-2023) only 37% were frame based with the remainder being either frameless or robotic.
3. Endoscopic approaches have been described which allow for concurrent treatment of obstructive hydrocephalus (39, 40).
There have not been any trials to assess differential safety outcomes with technical variations of pediatric brainstem biopsies for presumed DMG. In their analysis of 381 cases, Fu et al. conducted a separate subgroup analysis for stereotactic biopsies finding that overall morbidity rate was 5.3% (95% CI 1.5-10.7), likely lower than the rate for the combined stereotactic and open biopsy cases (11% overall morbidity, 95% CI 4.8-18.9). There was no sub-group analysis comparing trans-frontal and trans-cerebellar approaches in terms of safety profiles. In the five mortalities we found in our meta-analysis of 1002 cases (Table 2), 2 deaths occurred after stereotactic biopsy (1 through a trans-occipital approach, and 1 through a trans-frontal approach) while 3 occurred after open biopsy. Overall, no conclusive evidence exists to suggest that one technical variation for pediatric brainstem biopsies is clearly safer than the other; permanent complications and death are rare with all technical variations described. It is reasonable for surgeons to implement the technique they are most experienced and comfortable with.
4 Utility of pediatric brainstem biopsies
4.1 Is biopsy necessary for diagnosis?
The paradigm of treating DMGs as a radiographic diagnosis was based in large part on the belief that diffusely expansile minimally enhancing lesions centered primarily in the pons could not represent any entity that would be surgically resected and thus empiric treatment with radiation (with or without chemotherapy) was considered reasonable. It is worth examining whether existing literature supports this notion or if, instead, evidence exists that lower grade lesions (such as pilocytic astrocytomas) can mimic DMG and a presumptive radiographic diagnosis would be misguided.
A central problem with evaluating the validity of radiographic diagnosis for DMG is the issue of interrater variability which is made even more complicated by the fact that the oncopathological definition of DMG has evolved over the decades concurrent with dramatic progress in the quality of magnetic resonance imaging. It is thus not clear whether a group of neuro-oncologists reviewing an MRI study obtained in 2024 would arrive at the same radiographic diagnosis as an equally expert group of reviewers two decades prior. Notwithstanding this problem, the issue of interrater variability is mitigated in part by the use of multi-reviewer panels as is common in well-designed prospective trials. In the DIPG-BATS study (34), patients with MRI consistent with ‘classic DIPG’ diagnosed at a large-volume academic center were considered and atypical features (if present) were reviewed by study chairs before participants could be enrolled in a trial. Notably, of the 50 children who underwent biopsy after this careful selection process, 100% received a histopathological diagnosis of DIPG. The largest case series from a single center where all patients were already diagnosed with classic DIPG on the basis of MRI findings at the time of biopsy was published by Puget et al. in 2015 (n = 130 children) (41). 100% of these biopsies resulted in a histopathological diagnosis of DIPG.
Nonetheless, there are several case series of pediatric brainstem biopsies in which non-high-grade glioma pathologies have been reported; notable examples are detailed in Table 3. These case series highlight the now well understood principle that non-high-grade glioma pathologies are not uncommon in the pediatric brainstem, even if they represent a minority of the total neoplastic disease in this region. A key limitation of these case series is inconsistency in the description for why a biopsy was being conducted with only a minority stating that a presumptive diagnosis of DMG had been made before the procedure was performed. Thus, it is difficult to ascertain whether the non-glioma pathologies identified in these case series represent true radiographic mimics of DMG (in which case, the existence of these entities would support the notion that biopsy is required for diagnosis).
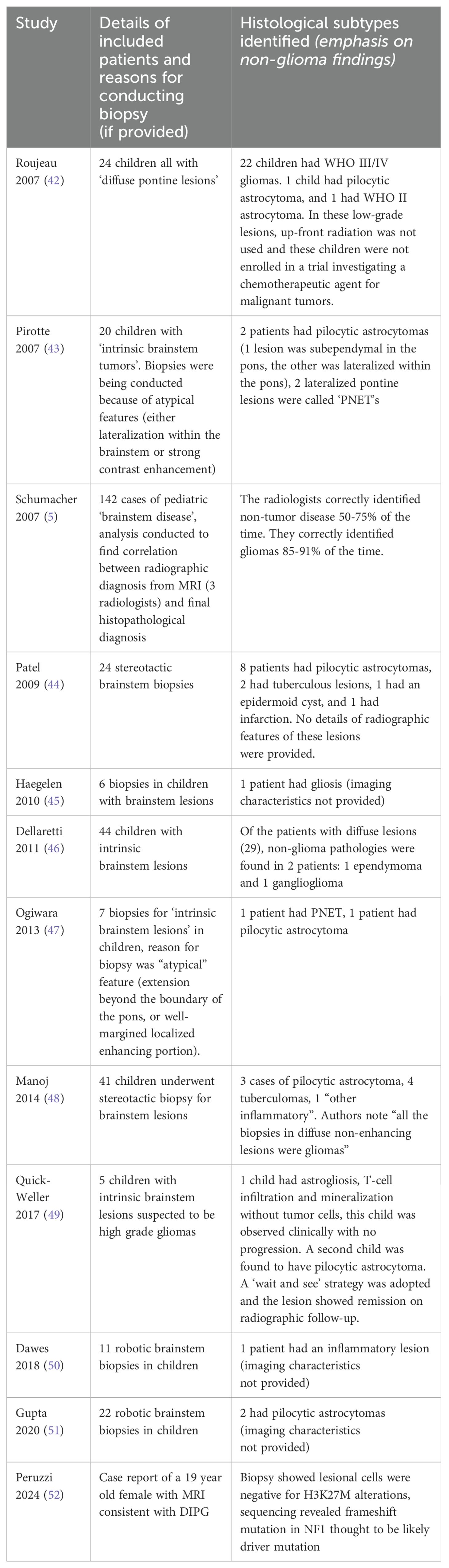
Table 3. Summary of non-high-grade glioma pathologies reported in surgical case series of pediatric brainstem biopsy.
In summary, for cases evaluated at high-volume centers with clinical course and radiographic information closely reviewed by experts, the radiographic diagnosis of DMG appears to be highly reliable. Case reports of situations where non-glioma pathologies were found in suspected DMG cases are present in the literature, but it is unclear whether the biopsies being discussed in those reports were being conducted in part because the diagnosis of DMG was uncertain. Uncontroversially, where the diagnosis of DMG is not clear based on clinical course or atypical radiographic findings, biopsy is indicated.
4.2 Are medical treatment schema based on molecular targets useful outside the context of trial enrollment?
The INFORM registry has provided compelling insights into the potential utility of molecular markers as the basis of targeted treatment schema for DMG patients (53). In a report from 2019, Pfaff et al. reported initial experience with 21 biopsy-proven DIPG cases submitted to the registry. They showed that it was possible to conduct molecular analysis on samples for all cases. It took 3-4 weeks (median 22 days) from arrival of tumor tissue to availability of preliminary target analysis report. This short turn-around time is vital given the aggressive clinical course of the disease.
‘Potential targetable alterations’ were identified in 16 cases. 5 of these alterations were used as the basis for targeted therapy as detailed below. Notably, patients were not enrolled in an early phase clinical trial as no matching open phase I/II trials were available in Germany at the time.
a. 2 patients had genetic alteration in platelet derived growth factor receptor alpha (PDGFRA), which is a cell surface tyrosine kinase receptor. These patients were treated with receptor tyrosine kinase inhibitors dasatinib or sorafenib in addition to the standard of care at their center i.e. temozolomide (TMZ) and irradiation.
b. One patient had a genetic alteration in PIK3CA which encodes a subunit of the PI3K enzyme involved in the PI3K/AKT/mTOR pathway. This patient was treated with mTOR inhibitor everloimus in addition to radiation + TMZ.
c. One patient had a KRAS amplification. This gene encodes a protein involved in the RAS/MAPK signaling pathway. This patient was treated with radiation as well as an inhibitor of MEK (a key enzyme in the RAS/MAPK pathway) in the form of trametinib, and cetuximab (a monoclonal antibody targeting epidermal growth factor receptor which disrupts downstream signaling pathways including RAS/MAPK).
d. One patient had both a PDGFRA amplification as well as a MET fusion (also a tyrosine receptor kinase). The patient was treated with radiation and 2 tyrosine kinase inhibitors: crizotinib and dasatinib.
The INFORM registry experience with DIPG patients is most valuable as a demonstration of the real-world feasibility of efficient molecular profiling of tumors, while laying the foundations for rational molecularly targeted treatment even outside the context of a clinical trial.
In 2022, Del Baldo et al. published their experience of implementing a targeted therapies approach to 25 DIPG patients at a single academic center in Italy (Bambino Gesu Children’s Hospital, Rome). 23 patients presented at time of diagnosis and two presented at time of disease progression (having previously been treated with temozolomide and radiotherapy). All patients underwent biopsy with molecular profiling. Newly diagnosed patients were all treated with the same standard of care regimen (radiotherapy, nimotuzumab, and vinorelbine). At time of progression, patients could either receive a standard therapy (bevacizumab and temozolomide) or a targeted therapy if molecular targets were identified and the disease course was not too advanced.
In 15 cases (60%), targetable alterations were found. 9 of these patients were treated with targeted therapies at time of progression (in addition to the standard progression protocol) based on the following schema:
a. patients whose tumor expressed mTOR/p-mTOR by immunohistochemistry (IHC) were treated with everolimus.
b. patients with PDGFRA alterations were given pazopanib (a tyrosine kinase inhibitor).
c. those with ACVR1 mutation (associated with BMP signaling) were given palovarotene (a RARγ agonist that can inhibit BMP signaling).
d. one child had BRAFv600E mutation as well as mTOR/p-mTOR expression and was treated with both everolimus and vemurafenib (an inhibitor of BRAF V600E kinase).
2 year overall survival was 19.8% for the whole study population. Notably, median overall survival was longer in the targeted treatment group (20.26 months) compared to the non-targeted treatment group (14.18 months). Thus, this report provides a compelling real-world example of how molecular profiles can be used to create targeted treatment schema with preliminary evidence that some survival advantage may be accessible through this paradigm.
The INFORM registry study and the Bambino Gesu series both used existing knowledge of molecular oncopathogenic processes to create rational targeted-treatment schema. In contrast, it is possible to use biopsy-derived tumor cell lines from a patient to create in vitro drug response assays which can in turn be used to choose medical treatment (54). In 2019, Tsoli et al. demonstrated that cell lines could be generated for 32 out of 38 DIPG biopsy samples (84.2%) (55), though the time frame in which this was accomplished is unclear. Mueller et al. have recently published an elegant demonstration of this approach in a real-world clinical workflow (56). In 24 patients with biopsy confirmed DMG, they were able to develop patient-derived cell lines that could be used for real-time drug screening for 9 patients (38%). Median time to develop the cell line (from time of biopsy) was 2.5 months, with a range of 1.5 to 5 months. The cell lines were used to test drug response to four agents in different combinations: ONC201, ONC206, paxalisib, and panobinostat. In one case, a patient was treated with paxalisib based on the demonstrated in vitro drug sensitivity from the patient derived cell line.
The reports reviewed in this section present an evolving model for creating targeted treatment schema for DMG patients on the basis of biopsy derived clinical targets even outside the context of a clinical trial. Multiple centers around the world have demonstrated the feasibility of rapid molecular profiling for DMG patients, which is a pre-requisite for targeted therapies. Specialized centers are also able to generate patient-derived cell lines which can be used for drug sensitivity analyses, though technical efficacy and efficiency of this process requires continued optimization. As the Bambino Gesu report highlights, there is some initial promise that the use of targeted therapies even outside a trial context may provide an overall survival benefit to selected patients; this will undoubtedly be the subject of active inquiry in the coming years.
4.3 Do biopsies allow for the design of better trials?
Conventional clinical trials for DMG did not rely on biopsy derived molecular features. Inherent within this kind of trial design was the obligate assumption that the disease was sufficiently homogenous (at least in terms of its response to therapy) that a signal of improved survival for a given therapy under investigation would nonetheless become apparent. Given the lack of progress in improving survival over multiple decades of investigation using this approach to trial design, it is vital to re-evaluate the paradigm. This is especially true given that we now appreciate that DMG is a molecularly heterogenous disease with different molecular subtypes associated with different survival rates and response to therapy (57).
The DIPG-BATS trial (NCT01182350, initial results published 2018) was the first large multi-center trial to require biopsy for all children and use molecular profiling as the basis of treatment arm allocation (34). All patients were treated with bevacizumab and radiotherapy but patients could also receive erlotinib based on the presence of EGFR mutation and temozolomide on the basis of MGMT promoter methylation. Perhaps the most important lesson from the DIPG-BATS experience was that this molecular-target driven workflow was feasible. All patients except one received radiation within 21 days of biopsy and there was sufficient tissue for genetic studies and treatment arm stratification in 96% of patients.
In 2019, Mueller et al. published results of PNOC003, a pilot precision medicine trial from the Pacific Pediatric Neuro-Oncology Consortium. DIPG patients underwent biopsy and samples were used for whole exome sequencing and RNA sequencing of paired tumor and normal tissues. Based on the molecular profile, up to 4 FDA approved drugs could be administered following evaluation by a specialized tumor board. For all 15 subjects in the pilot study, a treatment plan was successfully issued within 21 business days of tissue acquisition. Taken together, the DIPG-BATS and PNOC003 experience provide evidence that clinical workflows that incorporate tumor biopsy, molecular profiling, and patient-tailored treatment plans can be implemented within clinically relevant timeframes.
In 2023, Grill et al. published results from BIOMEDE (NCT02233049): a large, international, phase II platform trial comparing 3 targeted therapies in combination with radiotherapy for patients with biopsy proven DIPG (age < 25) (58). All patients underwent biopsy and central pathological review was used to confirm H3K27me3 loss and to obtain a molecular profile. All patients received 54 Gy radiation and, depending on the molecular profile, received erlotinib (for EGFR overexpression), everolimus (for mTOR activation), or dasatinib (tyrosine kinase inhibitor, no specific biomarker was needed for this drug in the trial). 233 patients were enrolled at 45 centers in 7 countries over 5 years. Overall survival was not different between different treatment arms. The BIOMEDE experience demonstrated that international multicenter trials for DIPG involving biopsy at diagnosis and biomarker-driven treatment allocation are feasible.
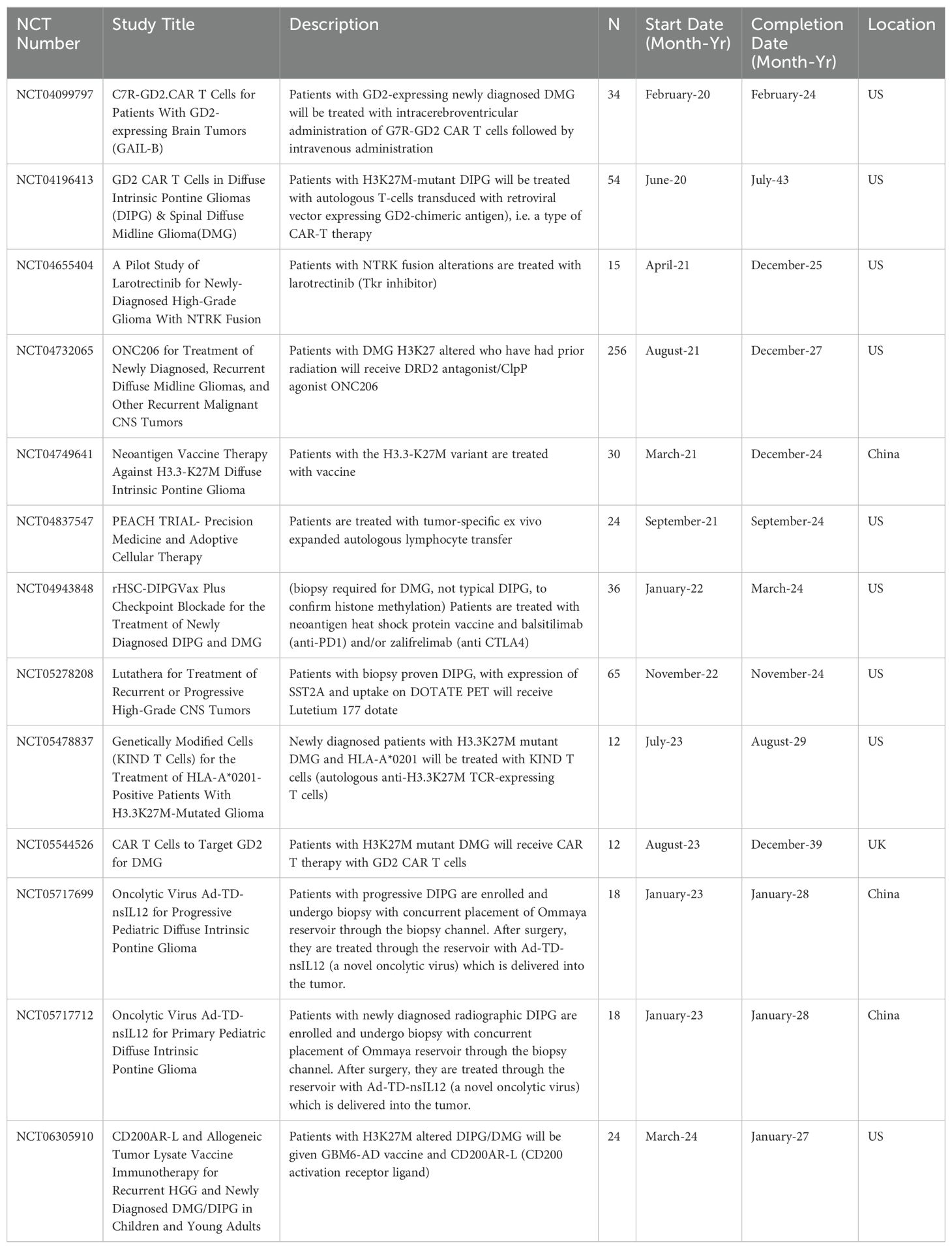
At the time of writing, we found 38 early phase interventional trials for children with DIPG/DMG in the active recruitment phase on clinicaltrials.gov. 14 of these trials (38%) require biopsy for enrollment (Table 4). The reason for requiring biopsy is variable across the trials:
1. Utilization of CAR T primed against a specific antigen that must first be confirmed to be expressed by the tumor.
2. Targeted small molecules which would only be expected to be efficacious if the tumor had specific gene alterations.
3. Tumor specific ex-vivo expanded immune cells which cannot be generated without tumor sample.
4. Delivery of oncolytic agents directly into the tumor bed through a biopsy tract.
5. Some trials are requiring the confirmation of H3K27M alteration for diagnosis but do not make use of any additional molecular features in treatment arm allocation.
As yet, all clinical trials (irrespective of whether biopsy-derived molecular alterations were targeted) have failed to identify medical treatments that increase survival for DIPG/DMG. However, as reviewed here, multiple large multicenter trials have now demonstrated the safety and feasibility of using a biopsy-driven approach for all children diagnosed with DMG/DIPG. This new paradigm of trial design for DMG/DIPG is necessary given our existing knowledge of the molecularly heterogenous nature of the disease.
4.4 Do biopsies help families cope with a devastating situation?
Entirely independent of the utility of biopsies as a tool to guide treatment decisions, it is important to examine the notion that biopsies may play a role in helping the family unit better cope with a devastating situation. Holistic care of the family unit is a vital component of the care of DIPG/DMG patients; if indeed biopsies can provide a sense of direction and even hope for the family, the procedure may have some value for this reason alone.
In their qualitative study of interviews with the parents of children who had died of DIPG/DMG, De Clerq et al. have provided valuable insights into the lived experience of impacted families (59). Several key findings provide a basic framework of the family mindset in this context. One of the most prominent findings that investigators discerned from interviews was the parents’ need “to have at least the feeling that they were ‘doing something.’” Importantly, this desire to feel like something was being done co-occurred with the knowledge that the tumor was likely fatal. In spite of this insight, the family perceived value in taking some action: “So actually already from the reaction before the biopsy, one could conclude that it would go the wrong way. So between doing everything or nothing … Well, you can’t tell your kid that you’re doing nothing. Because the child wants to try to see if it’s going to be okay. (father 3)” In the same vein, speaking about their treatment path, one mother shared “…it’s still right in retrospect, because otherwise I would have a bad conscience…” This latter quotation highlights the important notion that a biopsy may fit into a family’s perception of “doing everything possible” which may prove to be a point of unification and source of emotional strength for the family unit even after the demise of the patient.
5 Discussion
In regards to the safety of biopsies, we have examined the evidence generated by broad systematic review of existing case series (i.e. meta-analyses) as well as evidence from contemporary trials for DMG/DIPG. Our review of this literature shows that biopsies of the pediatric brainstem are highly efficacious in yielding a diagnosis (>96%) with very low rates of permanent morbidity (<2%); this trend is particularly true for stereotactic biopsies in this region though all technical variations reviewed shared comparable safety profiles. Multiple large-scale multi-instituational trials have now been conducted with biopsy required for enrollment; safety profile of biopsy in these trial settings was similar if not better than the safety profile gleaned from historical cohorts. Given the abundance of evidence reviewed on this topic, we feel that children with suspected DMG/DIPG can safely have a biopsy at high-volume centers.
The potential usefulness of biopsies can be analyzed separately both within and outside the context of clinical trials. We feel that the use of biopsies within the context of trials is largely uncontroversial given our growing understanding of the molecular heterogeneity inherent in DIPG/DMG and evidence that molecular subtypes have different expected survival and are variably responsive to different therapies. As we have reviewed here, multiple large multi-instituational trials have now been published which used molecular target information as the basis of treatment arm allocation. Though none of these trials have clearly found superior survival outcomes associated with targeted therapies, they are nonetheless an invaluable demonstration of the fesability of large-scale targeted trials for this disease. In addition to the use of molecularly targeted therapies, biopsies have allowed for investigations using immune cells primed against a patient’s tumor (e.g. CAR T and ex-vivo expanded autologous lymphocytes) as well as the development of cell lines, organoids, and xenografts, all of which have the potential to offer insight into putative therapies.
Outside the context of a clinical trial, we have reviewed how different centers around the world have developed treatment schema to incorporate targeted therapies into their treatment of DIPG/DMG patients. These early studies have shown the feasibility of this approach. For the practicing pediatric neuro-oncologist, our review of these ‘off-study’ approaches may serve as a starting point to show the fesability of developing targeted schema in response to molecular profiles while being sensitive to personal experience and local drug availabilities.
6 Future directions
As enumerated above, over a dozen registered trials are currently recruiting children with DIPG/DMG for biopsy-directed investigational treatments. In the coming years, the results of these targeted therapy trials will be highly informative and will shed valuable light not only on the efficiacy of individual targeted therpies but also on the utility of the paradigm of biopsy-driven treatments as a whole.
There is enormous interest in the development of non-invasive ‘liquid biopsy’ tests in the context of DIPG/DMG with the dual intent of providing molecular profiles as well as monitoring response to treatment (60, 61). ‘Liquid biopsies’ in this context would consist of blood and CSF based laboratory tests that can detect non-cellular DNA fragments from the tumor to provide molecular information that is otherwise only available through tissue sampling. In 2017, Huang et al. reported that they had used PCR to identify the H3F3A c.83A > T transversion (H3.3K27M) in 4 out of 5 patient samples of CSF which was concordant with the H3K27M status obtained by analysis of tumor biopsy sample (62). The work has since been replicated and optimized by multiple groups (63, 64), with Li et al. reporting in 2021that they had developed (and validated across three institutions) an assay to detect H3K27M mutation using CSF with a sensitivity of 100% using digital droplet PCR (ddPCR) (65). The key limitation of the technology, as it has been developed so far, is that the information obtained from it is limited to select mutations for which primer pairs are developed, and so the full molecular profile that can be obtained from a tissue sample is not available. This limitation would be obviated if, in the future, the technology could use tumor DNA to perform targeted sequencing panels or whole exome sequencing. Nonetheless, we note that many DMP/DIPG trials require tissue diagnosis primarily to confirm H3K27M mutation status. If indeed a liquid biopsy could provide this limited molecular information in a highly sensitive and specific manner, it is not hard to imagine that CSF-based evidence of mutation status may be deemed sufficient for enrollment (66). In that scenario, patients would have a new ‘middle ground’ between a completely biopsy-undirected and a fully biopsy-directed treatment path. In addition to its potential role in obtaining molecular profiles, we also note the potential of liquid biopsies as a way monitoring treatment response. If future iterations of the technology could provide information analagous to ‘tumor titers’ in the CSF, we would gain a vital tool that would allow early discontinuaiton of therapies that a patient is not responding to and subsequent initiation of alterantive therapies that may be more efficacious; this would represent a significant improvement over the current standard of relying on radiographic progression.
7 Conclusion
The existing evidence supports the notion that contemporary pediatric brainstem biopsies are likely to be safe and moelcular profiles can be obtained in clinically relevant timeframes as a standard of care. DMG/DIPG is a molecularly heterogeneous disease and a gradual shift towards molecular target oriented trials is essential to improving known dismal outcomes. Outside of the context of a trial, targeted treatment schema made on the basis of molecular profiles have been applied and are faesible to implement. Ongoing and future studies will be centered on establishing the survival benefit of targeting specific molecular targets and on developing less invasive means of obtaining molecular profiles that could obviate the need for tissue sampling.
Author contributions
SS: Conceptualization, Formal analysis, Investigation, Visualization, Writing – original draft. VR: Writing – review & editing. ET: Writing – review & editing. RM: Writing – review & editing. MW-N: Writing – review & editing. BG: Writing – review & editing. NP: Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Freeman CR, Farmer J-P. Pediatric brain stem gliomas: a review. Int J Radiat Oncol Biol Phys. (1998) 40:265–71. doi: 10.1016/S0360-3016(97)00572-5
2. Recinos PF, Sciubba DM, Jallo GI. Brainstem tumors: where are we today? Pediatr Neurosurg. (2007) 43:192–201. doi: 10.1159/000098831
3. Albright AL, Packer RJ, Zimmerman R, Rorke LB, Boyett J, Hammond GD. Magnetic resonance scans should replace biopsies for the diagnosis of diffuse brain stem gliomas: A report from the children's cancer group. Neurosurgery. (1993) 33:1026–30. doi: 10.1227/00006123-199312000-00010
4. Hankinson TC, Campagna EJ, Foreman NK, Handler MH. Interpretation of magnetic resonance images in diffuse intrinsic pontine glioma: a survey of pediatric neurosurgeons. J Neurosurgery: Pediatr. (2011) 8:97–102. doi: 10.3171/2011.4.PEDS1180
5. Schumacher M, Schulte-Mönting J, Stoeter P, Warmuth-Metz M, Solymosi L. Magnetic resonance imaging compared with biopsy in the diagnosis of brainstem diseases of childhood: a multicenter review. J Neurosurgery: Pediatr. (2007) 106:111–9. doi: 10.3171/ped.2007.106.2.111
6. Epstein F, Constantini S. Practical decisions in the treatment of pediatric brain stem tumors. Pediatr Neurosurg. (1996) 24:24–34. doi: 10.1159/000121011
7. Fisher PG, Breiter SN, Carson BS, Wharam MD, Williams JA, Weingart JD, et al. A clinicopathologic reappraisal of brain stem tumor classification: Identification of pilocytic astrocytoma and fibrillary astrocytoma as distinct entities. Cancer: Interdiscip Int J Am Cancer Soc. (2000) 89:1569–76. doi: 10.1002/1097-0142(20001001)89:7<1569::AID-CNCR22>3.0.CO;2-0
8. Khuong-Quang D-A, Buczkowicz P, Rakopoulos P, Liu X-Y, Fontebasso AM, Bouffet E, et al. K27M mutation in histone H3. 3 defines clinically and biologically distinct subgroups of pediatric diffuse intrinsic pontine gliomas. Acta neuropathologica. (2012) 124:439–47. doi: 10.1007/s00401-012-0998-0
9. Schwartzentruber J, Korshunov A, Liu X-Y, Jones DT, Pfaff E, Jacob K, et al. Driver mutations in histone H3. 3 and chromatin remodelling genes in paediatric glioblastoma. Nature. (2012) 482:226–31. doi: 10.1038/nature10833
10. Wu G, Broniscer A, McEachron TA, Lu C, Paugh BS, Becksfort J, et al. Somatic histone H3 alterations in pediatric diffuse intrinsic pontine gliomas and non-brainstem glioblastomas. Nat Genet. (2012) 44:251–3. doi: 10.1038/ng.1102
11. Harutyunyan AS, Krug B, Chen H, Papillon-Cavanagh S, Zeinieh M, Jay De N, et al. H3K27M induces defective chromatin spread of PRC2-mediated repressive H3K27me2/me3 and is essential for glioma tumorigenesis. Nat Commun. (2019) 10:1262. doi: 10.1038/s41467-019-09140-x
12. Justin N, Zhang Y, Tarricone C, Martin SR, Chen S, Underwood E, et al. Structural basis of oncogenic histone H3K27M inhibition of human polycomb repressive complex 2. Nat Commun. (2016) 7:11316. doi: 10.1038/ncomms11316
13. Krug B, Harutyunyan AS, Deshmukh S, Jabado N. Polycomb repressive complex 2 in the driver’s seat of childhood and young adult brain tumours. Trends Cell Biol. (2021) 31:814–28. doi: 10.1016/j.tcb.2021.05.006
14. Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, et al. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro-oncology. (2021) 23:1231–51. doi: 10.1093/neuonc/noab106
15. Fontebasso AM, Papillon-Cavanagh S, Schwartzentruber J, Nikbakht H, Gerges N, Fiset P-O, et al. Recurrent somatic mutations in ACVR1 in pediatric midline high-grade astrocytoma. Nat Genet. (2014) 46:462–6. doi: 10.1038/ng.2950
16. The genomic landscape of diffuse intrinsic pontine glioma and pediatric non-brainstem high-grade glioma. Nat Genet. (2014) 46:444–50. doi: 10.1038/ng.2938
17. Paugh BS, Zhu X, Qu C, Endersby R, Diaz AK, Zhang J, et al. Novel oncogenic PDGFRA mutations in pediatric high-grade gliomas. Cancer Res. (2013) 73:6219–29. doi: 10.1158/0008-5472.CAN-13-1491
18. Schramm K, Iskar M, Statz B, Jäger N, Haag D, Słabicki M, et al. DECIPHER pooled shRNA library screen identifies PP2A and FGFR signaling as potential therapeutic targets for diffuse intrinsic pontine gliomas. Neuro-oncology. (2019) 21:867–77. doi: 10.1093/neuonc/noz057
19. Li G, Mitra SS, Monje M, Henrich KN, Bangs CD, Nitta RT, et al. Expression of epidermal growth factor variant III (EGFRvIII) in pediatric diffuse intrinsic pontine gliomas. J Neurooncol. (2012) 108:395–402. doi: 10.1007/s11060-012-0842-3
20. Majzner RG, Theruvath JL, Nellan A, Heitzeneder S, Cui Y, Mount CW, et al. CAR T cells targeting B7-H3, a pan-cancer antigen, demonstrate potent preclinical activity against pediatric solid tumors and brain tumors. Clin Cancer Res. (2019) 25:2560–74. doi: 10.1158/1078-0432.CCR-18-0432
21. Roberts HJ, Ji S, Picca A, Sanson M, Garcia M, Snuderl M, et al. Clinical, genomic, and epigenomic analyses of H3K27M-mutant diffuse midline glioma long-term survivors reveal a distinct group of tumors with MAPK pathway alterations. Acta Neuropathol. (2023) 146:849–52. doi: 10.1007/s00401-023-02640-7
22. Rutka JT. Biopsy of diffuse intrinsic pontine gliomas? J Neurosurgery: Pediatr. (2012) 10:79–80. doi: 10.3171/2012.2.PEDS1237
24. Kieran MW. Time to rethink the unthinkable: upfront biopsy of children with newly diagnosed diffuse intrinsic pontine glioma (DIPG). Pediatr Blood Cancer. (2014) 62:3–4. doi: 10.1002/pbc.25266
25. Williams JR, Young CC, Vitanza NA, McGrath M, Feroze AH, Browd SR, et al. Progress in diffuse intrinsic pontine glioma: advocating for stereotactic biopsy in the standard of care. Neurosurgical Focus. (2020) 48:E4. doi: 10.3171/2019.9.FOCUS19745
26. El-Khouly FE, Zanten van Veldhuijzen SEM, Lopez Santa-Maria V, Hendrikse NH, Kaspers GJL, Loizos G, et al. Diagnostics and treatment of diffuse intrinsic pontine glioma: where do we stand? J Neurooncol. (2019) 145:177–84. doi: 10.1007/s11060-019-03287-9
27. Kickingereder P, Willeit P, Simon T, Ruge MI. Diagnostic value and safety of stereotactic biopsy for brainstem tumors: a systematic review and meta-analysis of 1480 cases. Neurosurgery. (2013) 72:873–82. doi: 10.1227/NEU.0b013e31828bf445
28. Hamisch C, Kickingereder P, Fischer M, Simon T, Ruge MI. Update on the diagnostic value and safety of stereotactic biopsy for pediatric brainstem tumors: a systematic review and meta-analysis of 735 cases. J Neurosurgery: Pediatr. (2017) 20:261–8. doi: 10.3171/2017.2.PEDS1665
29. Fu AY, Kavia J, Yadava Y, Srinivasan A, Hargwood P, Mazzola CA, et al. Biopsy of diffuse midline glioma is safe and impacts targeted therapy: a systematic review and meta-analysis. Child's Nervous System. (2023) 40:1–10. doi: 10.1007/s00381-023-06208-4
30. Lu VM, Koester SW, Di L, Elarjani T, Luther EM, Eichberg DG, et al. Frameless robotic-assisted biopsy of pediatric brainstem lesions: a systematic review and meta-analysis of efficacy and safety. World Neurosurg. (2023) 169:87–93. e81. doi: 10.1016/j.wneu.2022.10.071
31. Sheikh SR, Patel NJ, Recinos VM. Safety and technical efficacy of pediatric brainstem biopsies: an updated meta-analysis of 1000+ Children. World Neurosurg. (2024) 189:428–438. e422. doi: 10.1016/j.wneu.2024.06.163
32. Cheng G, Yu X, Zhao H, Cao W, Li H, Li Q, et al. Complications of stereotactic biopsy of lesions in the sellar region, pineal gland, and brainstem: A retrospective, single-center study. Med (Baltimore). (2020) 99:e18572. doi: 10.1097/md.0000000000018572
33. Wang M, Zhang Y, Shi W, Zhu R, Li H, Zhao R, et al. Frameless robot-assisted stereotactic biopsy: an effective and minimally invasive technique for pediatric diffuse intrinsic pontine gliomas. J Neuro-Oncology. (2022) 160:107–14. doi: 10.1007/s11060-022-04122-4
34. Gupta N, Goumnerova LC, Manley P, Chi SN, Neuberg D, Puligandla M, et al. Prospective feasibility and safety assessment of surgical biopsy for patients with newly diagnosed diffuse intrinsic pontine glioma. Neuro-oncology. (2018) 20:1547–55. doi: 10.1093/neuonc/noy070
35. Baghai P, Vries JK, Bechtel PC. Retromastoid approach for biopsy of brain stem tumors. Neurosurgery. (1982) 10:574–9. doi: 10.1227/00006123-198205000-00005
36. Jaradat A, Nowacki A, Fichtner J, Schlaeppi J-A, Pollo C. Stereotactic biopsies of brainstem lesions: which approach? Acta neurochirurgica. (2021) 163:1957–64. doi: 10.1007/s00701-021-04733-2
37. Abernathey CD, Camacho A, Kelly PJ. Stereotaxic suboccipital transcerebellar biopsy of pontine mass lesions. J Neurosurg. (1989) 70:195–200. doi: 10.3171/jns.1989.70.2.0195
38. Amundson EW, McGirt MJ. amp]]amp; Olivi, A. A contralateral, transfrontal, extraventricular approach to stereotactic brainstem biopsy procedures. J Neurosurg. (2005) 102:565–70. doi: 10.3171/jns.2005.102.3.0565
39. Torres-Corzo JG, Sanchez-Rodriguez J, Castillo-Rueda JL, Falcon-Escobedo R, Cervantes D, Vecchia Rodriguez-Della R, et al. Biopsy of brainstem gliomas using flexible endoscopes. J Neurological Surg Part A: Cent Eur Neurosurg. (2015) 76:291–7. doi: 10.1055/s-0034-1373661
40. Miki T, Nakajima N, Akimoto J, Wada J, Haraoka J. Neuroendoscopic trans-third ventricle approach for lesions of the ventral brainstem surface. min-Minimally Invasive Neurosurg. (2008) 51:313–8. doi: 10.1055/s-0028-1085446
41. Puget S, Beccaria K, Blauwblomme T, Roujeau T, James S, Grill J, et al. Biopsy in a series of 130 pediatric diffuse intrinsic Pontine gliomas. Child's Nervous System. (2015) 31:1773–80. doi: 10.1007/s00381-015-2832-1
42. Roujeau T, Machado G, Garnett MR, Miquel C, Puget S, Geoerger B, et al. Stereotactic biopsy of diffuse pontine lesions in children. J Neurosurgery: Pediatr. (2007) 107:1–4. doi: 10.3171/PED-07/07/001
43. Pirotte BJ, Lubansu A, Massager N, Wikler D, Goldman S, Levivier M. Results of positron emission tomography guidance and reassessment of the utility of and indications for stereotactic biopsy in children with infiltrative brainstem tumors. J Neurosurgery: Pediatr. (2007) 107:392–9. doi: 10.3171/PED-07/11/392
44. Patel P, Balamurugan M. Transcerebellar stereotactic biopsy for brainstem lesions in children. J Pediatr Neurosci. (2009) 4:17. doi: 10.4103/1817-1745.49101
45. Haegelen C, Touzet G, Reyns N, Maurage C-A, Ayachi M, Blond S. Stereotactic robot-guided biopsies of brain stem lesions: experience with 15 cases. Neurochirurgie. (2010) 56:363–7. doi: 10.1016/j.neuchi.2010.05.006
46. Dellaretti M, Touzet G, Reyns N, Dubois F, Gusmão S, Pereira JLB, et al. Correlation among magnetic resonance imaging findings, prognostic factors for survival, and histological diagnosis of intrinsic brainstem lesions in children. J Neurosurgery: Pediatr. (2011) 8:539–43. doi: 10.3171/2011.9.PEDS1167
47. Ogiwara H, Morota N. The efficacy of a biopsy of intrinsic brainstem lesions for decision making of the treatments. Child's Nervous System. (2013) 29:833–7. doi: 10.1007/s00381-013-2042-7
48. Manoj N, Arivazhagan A, Bhat D, Arvinda H, Mahadevan A, Santosh V, et al. Stereotactic biopsy of brainstem lesions: techniques, efficacy, safety, and disease variation between adults and children: a single institutional series and review. J Neurosci Rural Pract. (2014) 5:32–9. doi: 10.4103/0976-3147.127869
49. Quick-Weller J, Tritt S, Behmanesh B, Mittelbronn M, Spyrantis A, Dinc N, et al. Biopsies of pediatric brainstem lesions display low morbidity but strong impact on further treatment decisions. J Clin Neurosci. (2017) 44:254–9. doi: 10.1016/j.jocn.2017.06.028
50. Dawes W, Marcus HJ, Tisdall M, Aquilina K. Robot-assisted stereotactic brainstem biopsy in children: prospective cohort study. J Robotic Surg. (2019) 13:575–9. doi: 10.1007/s11701-018-0899-x
51. Gupta M, Chan TM, Santiago-Dieppa DR, Yekula A, Sanchez CE, Elster JD, et al. Robot-assisted stereotactic biopsy of pediatric brainstem and thalamic lesions. J Neurosurgery: Pediatr. (2020) 27:317–24. doi: 10.3171/2020.7.PEDS20373
52. Bernstock JD, Karandikar PV, Chen JA, Seidlitz J, Friedman GK, Meredith DM, et al. Case Report: Low-grade glioma with NF1 loss of function mimicking diffuse intrinsic pontine glioma. Front Surg. (2024) 11:1356660. doi: 10.3389/fsurg.2024.1356660
53. Pfaff E, Damaty El A, Balasubramanian GP, Blattner-Johnson M, Worst BC, Stark S, et al. Brainstem biopsy in pediatric diffuse intrinsic pontine glioma in the era of precision medicine: the INFORM study experience. Eur J Cancer. (2019) 114:27–35. doi: 10.1016/j.ejca.2019.03.019
54. Xu C, Liu X, Geng Y, Bai Q, Pan C, Sun Y, et al. Patient-derived DIPG cells preserve stem-like characteristics and generate orthotopic tumors. Oncotarget. (2017) 8:76644. doi: 10.18632/oncotarget.19656
55. Tsoli M, Shen H, Mayoh C, Franshaw L, Ehteda A, Upton D, et al. International experience in the development of patient-derived xenograft models of diffuse intrinsic pontine glioma. J neuro-oncology. (2019) 141:253–63. doi: 10.1007/s11060-018-03038-2
56. Mueller T, Laternser S, Stücklin Guerreiro AS, Gerber NU, Mourabit S, et al. Real-time drug testing of paediatric diffuse midline glioma to support clinical decision making: The Zurich DIPG/DMG centre experience. Eur J Cancer. (2023) 178:171–9. doi: 10.1016/j.ejca.2022.10.014
57. Castel D, Philippe C, Calmon R, Dret Le L, Truffaux N, Boddaert N, et al. Histone H3F3A and HIST1H3B K27M mutations define two subgroups of diffuse intrinsic pontine gliomas with different prognosis and phenotypes. Acta Neuropathol. (2015) 130:815–27. doi: 10.1007/s00401-015-1478-0
58. Grill J, Teuff Le G, Varlet P, Hargrave DR, Nysom K, Blomgrenn K, et al. Biological medicines for diffuse intrinsic pontine glioma (DIPG) eradication (BIOMEDE): Final results of an international randomized phase II platform trial comparing 3 targeted therapies in combination with radiotherapy from ITCC, SIOPE-Brain and ANZCHOG. J Clin Oncol. (2023) 41:10003–3. doi: 10.1200/JCO.2023.41.16_suppl.10003
59. De Clercq E, Grotzer M, Landolt MA, Helversen von B, Flury M, Rössler J, et al. No wrong decisions in an all-wrong situation. A qualitative study on the lived experiences of families of children with diffuse intrinsic pontine glioma. Pediatr Blood Cancer. (2022) 69:e29792. doi: 10.1002/pbc.29792
60. Azad TD, Jin MC, Bernhardt LJ, Bettegowda C. Liquid biopsy for pediatric diffuse midline glioma: a review of circulating tumor DNA and cerebrospinal fluid tumor DNA. Neurosurg Focus. (2020) 48:E9. doi: 10.3171/2019.9.Focus19699
61. Lu VM, Power EA, Zhang L, Daniels DJ. Liquid biopsy for diffuse intrinsic pontine glioma: an update. J Neurosurgery: Pediatr. (2019) 24:593–600. doi: 10.3171/2019.6.PEDS19259
62. Huang TY, Piunti A, Lulla RR, Qi J, Horbinski CM, Tomita T, et al. Detection of Histone H3 mutations in cerebrospinal fluid-derived tumor DNA from children with diffuse midline glioma. Acta neuropathologica Commun. (2017) 5:1–12. doi: 10.1186/s40478-017-0436-6
63. Martínez-Ricarte F, Mayor R, Martínez-Sáez E, Rubio-Pérez C, Pineda E, Cordero E, et al. Molecular diagnosis of diffuse gliomas through sequencing of cell-free circulating tumor DNA from cerebrospinal fluid. Clin Cancer Res. (2018) 24:2812–9. doi: 10.1158/1078-0432.CCR-17-3800
64. Pan C, Diplas BH, Chen X, Wu Y, Xiao X, Jiang L, et al. Molecular profiling of tumors of the brainstem by sequencing of CSF-derived circulating tumor DNA. Acta neuropathologica. (2019) 137:297–306. doi: 10.1007/s00401-018-1936-6
65. Li D, Bonner ER, Wierzbicki K, Panditharatna E, Huang T, Lulla R, et al. Standardization of the liquid biopsy for pediatric diffuse midline glioma using ddPCR. Sci Rep. (2021) 11:5098. doi: 10.1038/s41598-021-84513-1
Keywords: DMG, DIPG, diffuse midline glioma, diffuse intrinsic pontine glioma, brainstem biopsy, targeted therapy, H3K27M
Citation: Sheikh SR, Recinos VMR, Thompson EM, Mangum R, Wright-Nadkarni M, Gampel B and Patel NJ (2024) The role of brainstem biopsy and targeted therapies in pediatric diffuse midline glioma/diffuse intrinsic pontine glioma. Front. Oncol. 14:1504440. doi: 10.3389/fonc.2024.1504440
Received: 30 September 2024; Accepted: 03 December 2024;
Published: 23 December 2024.
Edited by:
Ashley Sloane Margol, Children’s Hospital of Los Angeles, United StatesReviewed by:
Joshua D. Bernstock, Harvard Medical School, United StatesJoji Ishida, Okayama University, Japan
Copyright © 2024 Sheikh, Recinos, Thompson, Mangum, Wright-Nadkarni, Gampel and Patel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Neha J. Patel, cGF0ZWxuMjJAY2NmLm9yZw==
†These authors have contributed equally to this work and share senior authorship
 Shehryar R. Sheikh
Shehryar R. Sheikh Violette M. R. Recinos1†
Violette M. R. Recinos1† Ross Mangum
Ross Mangum Bradley Gampel
Bradley Gampel Neha J. Patel
Neha J. Patel