- 1Department of Nursing, College of Medicine and Health Sciences, Injibara University, Injibara, Ethiopia
- 2Department of Midwifery, College of Medicine and Health Sciences, Injibara University, Injibara, Ethiopia
- 3Department of Surgical Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Breast cancer is the most common cancer among women globally, and early detection through breast self-examination can improve survival rates. However, this practice is limited in developing countries like Ethiopia.
Objective: This study aimed to assess the factors influencing knowledge and practices related to breast self-examination among female governmental school teachers in Gondar Town, Northwest Ethiopia.
Methods: A cross-sectional study was conducted from May 1 to 30, 2019, with 422 female teachers in Gondar metropolis governmental schools selected through simple random sampling. Data were collected using a self-administered questionnaire and analyzed using EPI INFO version 7 and SPSS version 20.
Result: A total of 415 female teachers participated in the study, with a response rate of 98.3%. The mean age of respondents was 38.64 years. Only 41.9% had good knowledge of breast self-examination, while 14.5% reported good practice. Factors associated with knowledge included secondary education, higher degrees, and exposure to information. Factors influencing practice included having a degree or higher education and prior experience with breast self-examination.
Conclusion and recommendation: The study revealed low levels of knowledge and practice of breast self-examination among female teachers. Educational level was significantly associated with both knowledge and practice. Recommendations include implementing health education campaigns, organizing events like breast cancer awareness days, and forming support groups in schools to promote awareness and encourage regular breast self-examination among female teachers in Ethiopia.
Introduction
Breast cancer (BC) is a prevalent form of cancer that primarily affects women (1). It is a significant public health concern, resulting in high levels of morbidity and mortality. Each year, over 2.1 million women are diagnosed with breast cancer worldwide, with more than half of them succumbing to the disease (2). The incidence of breast cancer is increasing in both developed and developing countries. In 2020, there were 2.3 million newly diagnosed cases and 685,000 deaths worldwide (3).
According to statistics, breast cancer accounts for approximately 25% of cases and 15% of deaths worldwide (4). By the end of 2020, it is projected that 43.1% of women globally and 36.8% in underdeveloped countries will succumb to breast cancer (5). This regional trend of increasing morbidity and mortality due to breast cancer is concerning, particularly in countries with limited resources, as a result of factors such as increased lifespan, urbanization, and adoption of Western lifestyles (6). Therefore, there is an urgent need for action to prevent and detect breast cancer early through various screening methods in order to achieve the sustainable development goal by 2030 (7). In contrast, the rise in cancer cases was observed in developing areas, accounting for 56% of new cancer cases and 63% of cancer-related deaths (8). In Ethiopia, breast cancer is the most prevalent type among adults, making up 30.2% of cases. The majority of reported annual cancer-related deaths in Ethiopia are women (9). Breast cancer is the second leading cause of death, responsible for 2.7% of all mortalities and ranking among the top five causes of non-communicable deaths. While efforts are being made to establish cancer centers in Ethiopia, these facilities are not as extensive as needed (10). Compared to those in Tanzania, Ethiopia’s service centers for cancer care are more advanced but fall short of those in Zambia (11). Many healthcare facilities in Ethiopia lack the necessary modern laboratory equipment for breast cancer screening and diagnosis.
Therefore, early detection programs such as breast self-examination, objective breast health checkups, and mammography can help minimize the morbidity and mortality associated with breast cancer (12). In Ethiopia, a National Cancer Control Plan was established in 2015 (9), with breast self-examination (BSE) being promoted as a crucial method for early detection to improve survival rates (13). The key components of BSE involve pictorial checkups and palpation of the breast, which have been shown to empower women to take control of their breast health (14, 15). Additionally, BSE is a valuable screening tool, with nursing and teaching professions playing a significant role in raising community awareness through education (16). Increased awareness of BSE among female teachers can directly or indirectly improve the resistance and quality of life for breast cancer patients (17) and themselves by enabling early detection and treatment initiation (18, 19).
Various studies have found varying levels of knowledge and performance of breast self-examination among women, despite its importance. For example, research in Iraq found that only 15.7% had good knowledge of BSE (20), while in Sudan, the number was 34% (21); in Cameroon, it was 78% (22); in different regions of Ethiopia (specifically Arba Minch, Jima, and Adwa Town), the percentages ranged from 34.2% to 55.5% (23–25).
According to the practices of women in various countries, the percentage of study participants implementing BSE was as follows: University Putra Malaysia 36.7% (26), Pakistan 24.9% (27), Ghana 37.6% (28), Cameroon 38.5% (29), Egypt 39.2% (30), and Sudan 20.6% (21). In Addis Ababa, Ethiopia, the percentages were 18.6% and 13.1% (31, 32).
Different researchers have identified various factors that may influence the knowledge and practice of BSE among women, including age, income, educational level, the educational and professional status of the husband, and source of information (32–35). However, these findings are inconclusive.
In developing countries where diseases are often diagnosed late due to limited resources, early detection of cases through breast self-examination is crucial. The practice of BSE has been shown to empower women to take control of their health (5). Female teachers who are knowledgeable about and perform BSE can have a positive impact on mothers, students, and other women in the community by sharing information and serving as role models. However, there is limited evidence in the specific study area. Therefore, this study aims to evaluate the knowledge, practices, and factors associated with breast self-examination among governmental school teachers in Gondar Town, Northwest Ethiopia.
Materials and methods
Sample and setting
A facility-based cross-sectional study was conducted in Gondar Town, Northwest Ethiopia, from May 1 to 30, 2019. Gondar Town, located 734 km from the capital city of Addis Ababa, is an ancient and densely populated town in Ethiopia. The town has experienced growth and currently has eight health centers and one referral hospital serving the population and surrounding areas. According to the 2019 report from the central Gondar zonal educational office, there are a total of 81 schools in Gondar Town, with 55 being governmental and 26 non-governmental. Among the teachers, 1,596 are female, with 1,229 in governmental schools and 367 in non-governmental schools.
The study population consisted of all female teachers working at governmental schools in Gondar Town, Northwest Ethiopia, during the data collection period. Only female teachers between the ages of 20 and 70 who were not undergoing treatment for mastectomy or were seriously ill were included in the study.
The sample size was determined using the single population proportion formula by , considering the 50% assumption of 95% confidence interval, 5% margin of error, and 10% possible non-response rate. Then, the final sample size was 422.
The sample was acquired by distributing the sample size proportionally among each level of school (574 for elementary, 396 for secondary, 206 for high school, and 53 for preparatory). Each study participant was then selected using a simple random sampling technique with the lottery method, based on the female teachers’ roster from the Gondar Town educational office, from each school (179 from elementary, 136 from secondary, 71 from high school, and 18 from preparatory). Ultimately, 422 female teachers were chosen. Elementary schools include first to fourth grades, secondary schools encompass fifth to eighth grades, high school covers ninth and 10th grades, and preparatory schools involve 11th and 12th grades.
Operational definitions
In this study, good knowledge of BSE was defined as those who answered more than 60% of the knowledge questions correctly, with those scoring 60% or below considered to have poor knowledge. Similarly, good practice was defined as scoring more than 60% on the practice-related questions, while those scoring 60% or lower were considered to have poor practice (36).
Data collection tool and data analysis
We utilized a standardized structured self-administered questionnaire adapted from relevant literature for our study (27, 36). The questionnaire comprised four sections covering socio-demographic factors, sources of information and history of breast cancer-related factors, knowledge of BSE, and practice of BSE. To maintain data integrity, efforts were made from developing the data gathering tools to thoroughly checking the completed questionnaires. Necessary modifications were made based on the results of a pretest, which involved 5% of female teachers from Dessie Town. The reliability of the questionnaire was assessed using Cronbach’s alpha, with knowledge scoring 0.82 and practice scoring 0.74. Data collectors and supervisors received 1 day of training on the instruments to ensure quality data collection.
Before analysis, the gathered information was reviewed for completeness, accuracy, and clarity. The data were then entered into EPI INFO version 7.2 and analyzed using SPSS version 20. Descriptive statistics, such as frequencies and proportions, were used to summarize the study variables. Binary logistic regression models were employed to identify associated factors, with variables having a p-value ≤0.2 in the bivariate analysis being included in the multivariate analysis to control for confounding factors. Odds ratios with 95% confidence intervals were calculated to determine the strength of the associations. A significance level of p < 0.05 was considered statistically significant.
Result
Socio-demographic characteristics of the study participants
A total of 415 individuals participated in the study, resulting in a response rate of 98.3%. Within the age category of 33–43 years, 145 participants were identified, accounting for 34.9% of the total. The majority of respondents, 285 individuals (68.7%), identified as Orthodox Christians. In terms of salary/income, 68% of participants earned more than or equal to 4,000.00 ETB, while 32% earned less than 4,000.00 ETB. The distribution of participants according to department level was as follows: 26.7% social, 29.6% cluster, and 43.6% natural (Supplementary Table S1).
The source of information about BSE and history of breast cancer
The majority, 401 (96.6%), of the study participants did not have previous breast cancer or any cancer, and only 35 (8.4%) of their families had a history of breast cancer. Of the study participants, 297 (71.6%) respondents have heard information about breast self-examination. Of those who had information about BSE, 164 (55.2%) of them were heard from healthcare workers and 59 (19.9%) from friends/peer groups, and only 74 (24.9%) were from newspapers, magazines, and the Internet.
Knowledge of school teachers towards BSE
More than half of the study participants, 243 (58.6%), recognized the importance of BSE in the early detection of breast cancer. Of the participants, 172 (41.2%) correctly stated that BSE should be performed monthly. However, 311 (74.9%) of participants inaccurately believed that a history of a breast lump does not increase the risk of breast cancer, and 197 (47.5%) thought that examining the armpit during BSE is necessary for detecting lumps. Only 81 (19.5%) of participants knew that both men and women can perform BSE. The majority of participants, 328 (79%), believed that BSE should be conducted by health professionals.
The practice of school teachers of BSE
Regarding questions related to practice, 167 (40.2%) of participants in the study indicated that breast self-examination should be conducted when it is thought of, while 164 (39.5%) correctly stated that palpation with the palm and three fingers is the appropriate method for conducting breast self-examination. In addition, 189 (45.5%) of participants believed that breast self-examination should start at the age of 40 and above, and 237 (57.1%) thought that examining only the left side of the breast was sufficient during the process. Only 37.0% of participants had ever performed breast self-examination, with 29.6% of those who had not performed stating that they did not know how to perform it. Fear of detecting an abnormality was the reason given by only 2.4% of participants for not conducting breast self-examination. Overall, the study found that 14.5% of participants demonstrated good practice in performing breast self-examination, scoring between 1 and 7 on the practice assessment scale (Supplementary Table S2).
Factors associated with knowledge of BSE
In the bivariate logistic regression model, all independent variables were included, and those with a p-value ≤0.2 were further analyzed in a multivariate analysis to control for confounding factors. In the multivariate analysis, three variables showed a significant association with the knowledge of female school teachers on BSE. Female school teachers with qualifications of a Bachelor of Science (BSc) or higher were approximately six times more likely to be knowledgeable about BSE compared to those with certificates and diplomas [adjusted odds ratio (AOR): 5.5, 95% CI: 1.65–18.4]. Additionally, secondary school (grades 5–8) female teachers were approximately three times more likely to have knowledge of BSE compared to primary school teachers (AOR: 2.6, 95% CI: 1.12–8.87). Female school teachers who had exposure to information were nearly five times more likely to be knowledgeable about BSE compared to those without exposure (AOR: 4.9, 95% CI: 1.71–4.63) (Table 1).
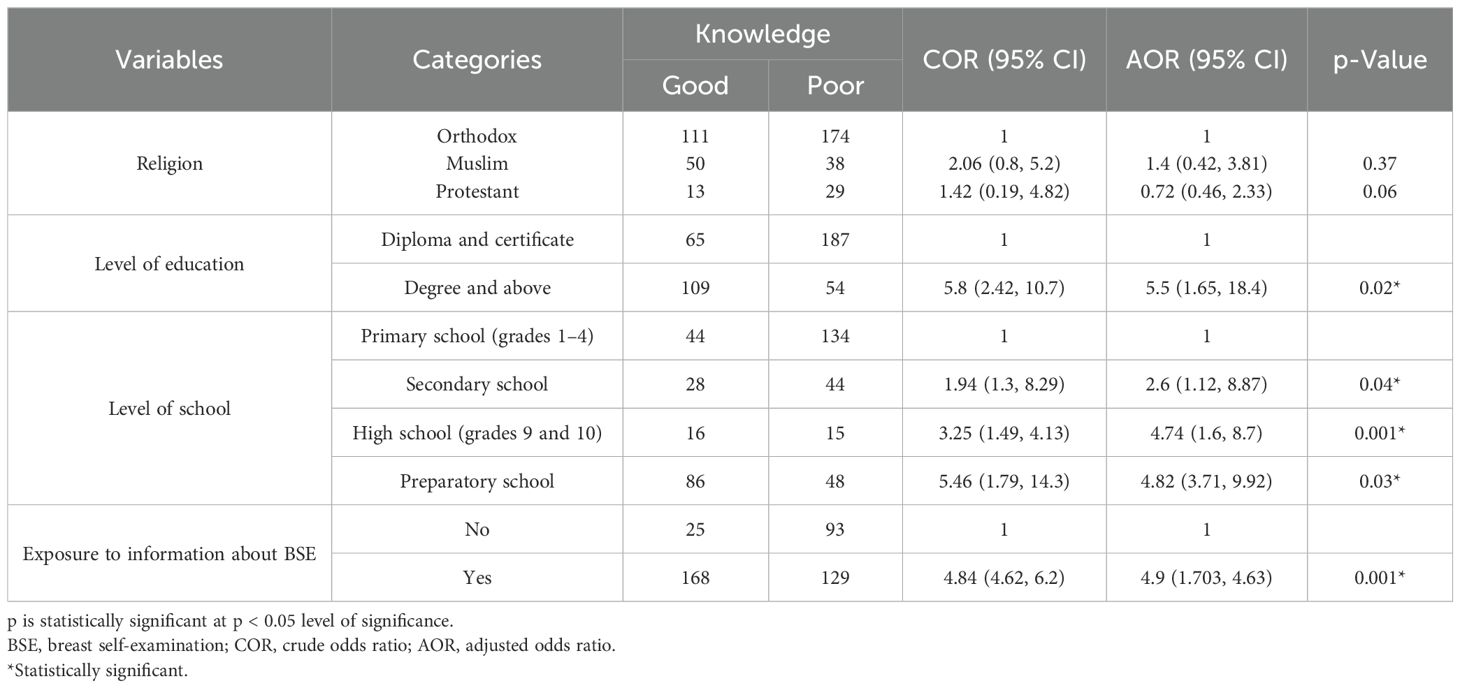
Table 1. Bivariable and multivariate logistic regression analysis for factors that affect knowledge of female school teachers on BSE, Gondar town, Northwest Ethiopia, 2019 (n = 415).
Factors associated with the practice of breast self-examination
In the multivariate analysis, two variables were found to be independently associated with the practice of BSE among female school teachers. According to the results, female school teachers with a degree or master’s degree were approximately three times more likely to have good practice compared to those holding certificates or diplomas (AOR: 2.94, 95% CI: 1.01–8.58). Additionally, female teachers who had previously performed BSE were two times more likely to have good practice compared to those who had not performed BSE (AOR: 2.38, 95% CI: 1.04–5.41) (Table 2).
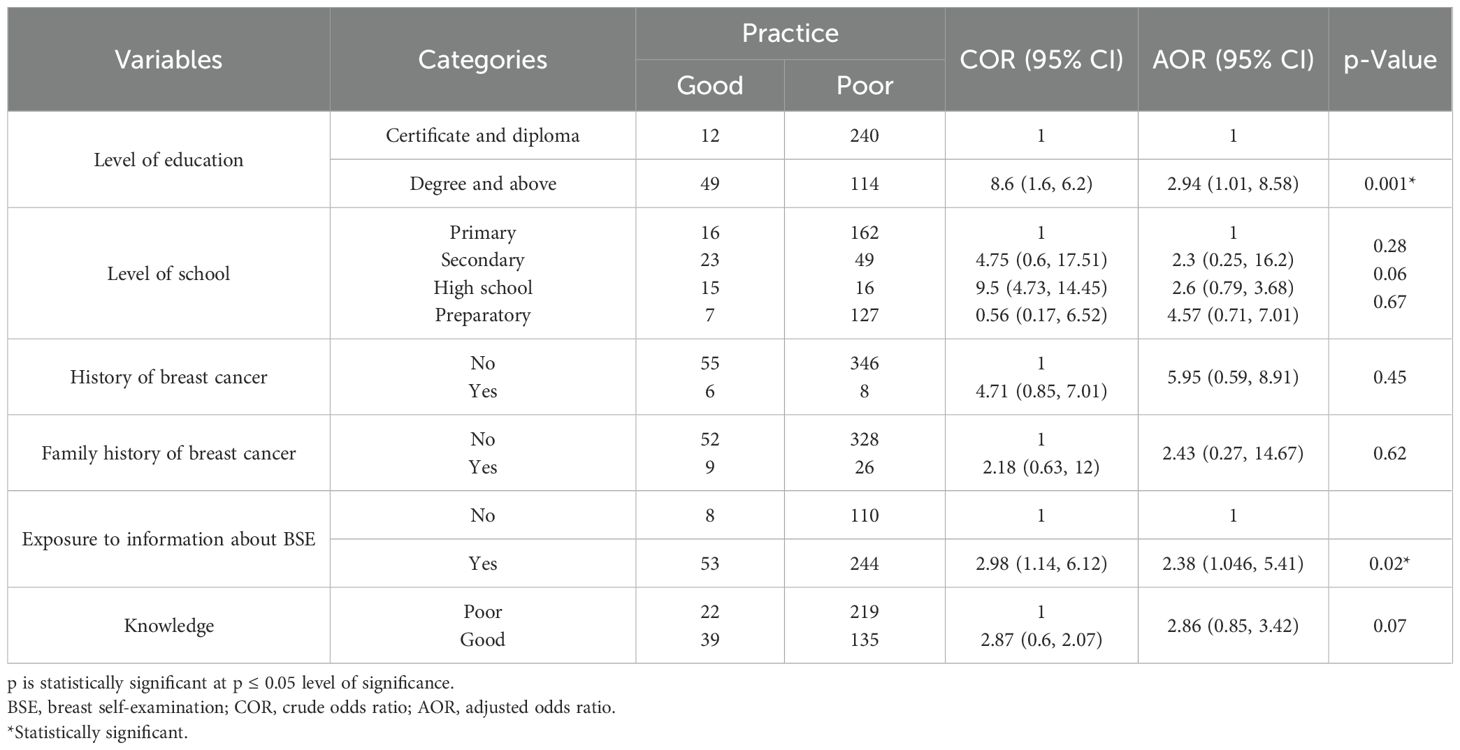
Table 2. Bivariable and multivariate logistic regression analysis for factors that affect the practice of female school teachers on BSE, Gondar town, Northwest Ethiopia, 2019 (n = 415).
Discussion
The World Health Organization (WHO) is stressing the importance of including cancer prevention efforts in overall cancer control strategies, as nearly 40% of cancer deaths are currently being overlooked (37). BSE is considered a key part of these strategies, and this research aimed to investigate the factors influencing the knowledge and practice of BSE among female school teachers in Gondar Town. The study found that 41.9% of governmental school teachers had good knowledge of BSE, a similar percentage to a study conducted in Addis Ababa, Ethiopia (38). The similarity may be due to alike socio-cultural and economic status. However, this finding was lower than that of the studies conducted in other countries: Pakistan 71.4% (27), India (39), Jordan 93.1% (40), Sub-Saharan countries 81.5% (41), Nigeria 54% (42), and Cameroon 78% (22). The possible justification may be due to study setting difference (22), the difference in sampling method (non-probability in Sub-Saharan African study) (41), the study population, with some of the above studies conducted among health students (41), and a surgical outpatient (22). Furthermore, it may be due to the difference in socioeconomics, access to sources of information (Internet and media access), and healthcare services (27, 39, 40).
In contrast, the findings of this study were higher than those of the studies conducted in Arab American University (43), Iraq 15.7% (20), Sudan 34% (21), and different regions of Ethiopia (Debre Berhan 30.25% and Adama 8.7%) (44, 45). The possible justification for these discrepancies may be the study settings (21, 43), the student population (44), the small sample size (210) (20), and the method of analysis they used (ordinal logistic regression) at Adama, Ethiopia (45).
The other outcome variable of this study was the implementation or practice of BSE. Then, the good practice of BSE among female teachers was 14.5% (95% CI: 10.6%–19.1%). This finding was similar to that of the studies conducted in Malaysia 19% (46) and Sub-Saharan Africa (41). This may be due to a similar study population (the Malaysian study was conducted among female teachers) and Sub-Saharan African countries having similar health-seeking behavior.
However, the finding of this study on good practice of BSE was lower than that of the studies conducted in other countries: Malaysia 36.7% (26), Pakistan 24.9% (27), India 33.3% (47), Ghana 37.6% (28), Cameroon 38.5% (29), Egypt 39.2% (30), Sudan 20.6% (21), Zambia 28.2% (48), Nigeria 38% (42), and different regions of Ethiopia (Jimma 21%, Adama 39.4%, and Addis Ababa 21.4%) (36, 45, 49). The reason for the differences in findings between this study and others may be attributed to variations in study settings (26–28, 30, 42, 47, 48) and access to healthcare (50). Other studies may have included populations with different characteristics, such as students enrolled in health-related courses or excluding individuals under the age of 21, which could impact their ability to practice and promote breast self-examination (21, 29, 36, 45, 49). Conversely, the results of this study showed a higher percentage of participants practicing BSE compared to studies conducted in India (4.5%) (39) and Adwa, Ethiopia (6.25%) (25). These variations could be due to differences in study settings, tools used, cutoff points for defining good practice, and the educational levels of the study populations.
Regarding factors associated with good knowledge of BSE in this study, the level of education of study participants was positively associated with knowledge of BSE. Thus, those with degrees (BSc) and above were approximately six times more likely to be knowledgeable about BSE than certificate and diploma holders. This was supported by the study conducted in Adama, Ethiopia, which reported that a statistically significant association was obtained between knowledge of BSE and the level of education of the participant (45). This may be due to the fact that if someone’s educational status increases, his/her knowledge status is also concomitantly enhanced (51).
In terms of factors associated with good knowledge of BSE in this study, participants with higher levels of education (BSc degrees and above) were significantly more knowledgeable about BSE compared to those with certificates or diplomas. This finding is consistent with a study conducted in Adama, Ethiopia (45), which also found a significant association between level of education and knowledge of BSE (52). This suggests that as individuals’ educational levels increase, so does their knowledge and understanding of BSE. Participants who had knowledge of breast self-examination were more likely to have a good understanding of BSE, similar to research conducted in Malaysia (53). This could be attributed to increased awareness leading to participation in campaigns and following health personnel guidance on BSE.
The study also found a positive correlation between educational level and practicing breast self-examination. Women with a degree or master’s degree were three times more likely to have good practice compared to those with certificates or diplomas, in line with findings from studies in Adama, Ethiopia (45), and Nigeria (54). Higher educational levels may enable women to access information and develop effective techniques for performing BSE to prevent diseases (55).
In addition, regularly performing BSE was linked to better practice of breast self-examination. Female teachers who had previously conducted BSE were twice as likely to have good practice compared to those who had not. This is consistent with previous research (56, 57) suggesting that a lack of prior BSE performance may result in lower competence in practicing the technique. A history of performing BSE can positively influence the ability to conduct breast examinations effectively.
Conclusion
This research indicated a lack of knowledge and limited practice of breast self-examination among female school teachers. The study also found that educational level, receiving information about BSE, and school level positively correlated with better knowledge of breast self-examination. Additionally, educational level and practicing BSE correlated positively with better performance on the examination. Therefore, it is crucial to implement health education campaigns, observe events like breast cancer awareness day, and establish groups within schools to promote awareness and encourage regular practice of breast self-examination among female teachers.
Strength and limitation
This study may be subjected to response bias, and it may be underreported or over-reported. Furthermore, it focused only female teachers only.
Data availability statement
Requests to access these datasets should be directed to BY, S2Fzc2lzaDZAZ21haWwuY29t.
Ethics statement
All study procedures were carried out according to the ISSCR Guidelines (58) and approved by the local Ethical Review Committee of the University of Gondar, College of Medicine and Health Sciences, School of Nursing (reference number was S/N 2011/05/2011). Written informed consent was obtained from all subjects prior to their enrollment. All methods were performed in accordance with the relevant guidelines and regulations (Declaration of Helsinki).
Author contributions
BY: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. BA: Conceptualization, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. TW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and authorship of this article. This work was supported by the University of Gondar.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2024.1481714/full#supplementary-material
Abbreviations
BC, breast cancer; BSE, breast self-examination; CBE, clinical breast examination; ECA, Ethiopia Cancer Association; EPI INFO, epidemiological information; ETB, Ethiopian birr; AOR, adjusted odds ratio; SPSS, Statistical Package for Social Sciences; UOG, University of Gondar; WHO, World Health Organization.
References
1. Akram M, Iqbal M, Daniyal M, Khan AU. Awareness and current knowledge of breast cancer. Biol Res. (2017) 50:1–23. doi: 10.1186/s40659-017-0140-9
2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin. (2018) 68:394–424. doi: 10.3322/caac.21492
3. WHO. Breast cancer 2021 (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/breast-cancer (accessed October 12, 2024).
4. Iacorossi L, Gambalunga F, Fabi A, Giannarelli D, Facchinetti G, Piredda M, et al. Adherence to hormone therapy in women with breast cancer: a quantitative study. Professioni infermieristiche. (2016) 69:113–21.
5. ETHIOPIA FMOH. NATIONAL CANCER CONTROL PLAN 2016-2020 OCTOBER 2015 (2022). Available online at: https://www.iccp-portal.org/sites/default/files/plans/NCCP%20Ethiopia%20Final%20261015.pdf (accessed October 15, 2024).
6. WHO. Africa cancer 2018 (2022). Available online at: https://www.afro.who.int/health-topics/cancer (accessed September 20, 2024).
7. Cf O. Transforming our world: the 2030 Agenda for Sustainable Development. United Nations: New York, NY, USA: BioOne Complete (2015).
8. Negeri EL, Heyi WD, Melka AS. Assessment of breast self-examination practice and associated factors among female health professionals in Western Ethiopia: A cross sectional study. Int J Med Med Sci. (2017) 9:148–57. doi: 10.5897/IJMMS2016.1269
9. Federal Ministry of Health E. National cancer control plan 2016-2020 of Ethiopia. This Prev Control Dir. (2015) 2015:83.
10. Ayele W, Führer A, Braun GA, Formazin F, Wienke A, Taylor L, et al. Breast cancer morbidity and mortality in rural Ethiopia: data from 788 verbal autopsies. BMC women’s Health. (2022) 22:1–9. doi: 10.1186/s12905-022-01672-7
11. Organization WH. Service availability and readiness assessment (SARA). Geneva, Switzerland: World Health Organization (2015).
12. Ergin A, Şahin N, Sahin F, Şimşek Yaban Z, Acar Z, Bektas H. Meta analysis of studies about breast self examination between 2000-2009 in Turkey. Asian Pac J Cancer Prev. (2012) 13. doi: 10.7314/APJCP.2012.13.7.3389
13. Shrivastava S, Shrivastava PS, Ramasamy J. Self breast examination: A tool for early diagnosis of breast cancer. Am J Public Health Res. (2013) 1:135–9. doi: 10.12691/ajphr-1-6-2
14. Fatimah M, Juni MH, Rosliza A. Factors associated with the practice of breast self examination: A systematic review. Int J Public Health Clin Sci. (2018) 5:86–90.
15. Al-Sakkaf KA, Basaleem HO. Breast cancer knowledge, perception and breast self-examination practices among Yemeni Women: an application of the health belief model. Asian Pac J Cancer Prev. (2016) 17:1463–7. doi: 10.7314/APJCP.2016.17.3.1463
16. Nichols M. The nurse’s role in self–breast examination education. Plast Surg Nursing. (2012) 32:143–5. doi: 10.1097/PSN.0b013e318274e81b
17. Ebrahim S. Knowledge of students toward breast cancer and breast self-examination practice at high school nursing in Basra city. Rev J Kufa Nurs Sci. (2014) 4:0–. doi: 10.36321/kjns.vi20141.2453
18. DeSantis C, Siegel R, Jemal A. Breast cancer facts and figures 2013-2014. Am Cancer Soc. (2013) 2013:1–38.
19. Tarver T. Cancer facts & figures 2012. American cancer society (ACS) Atlanta, GA: American Cancer Society (2012). 66 p. Taylor & Francis; 2012.
20. Ebrahim SM. Knowledge of students toward breast cancer and breast self-examination practice at high school nursing in Basra city. Kufa J Nurs Sci. (2014) 4:84–92. doi: 10.36321/kjns.vi20141.2453
21. Nugod SMAM. Breast Self Examination Knowledge Among Females In Salha, Omdurman locality, Khartoum State, Sudan. United States and the United Kingdom: University of Gezira (2016).
22. Alegbeleye BJ, Jantchou P. Knowledge and practices of breast self-examination amongst women attending a surgical outpatient clinic, Cameroon. Breast Cancer. (2018) 13.
23. Mereta B, Shegaze M, Mekonnen B, Desalegn N, Getie A, Abdilwohab MG. Assessment Of Breast Self-Examination And Associated Factors Among Women Age 20-64 Years At Arba Minch Zuria District, Gamo Zone Snnpr Ethiopia, 2019. Sudan (2020).
24. Terfa YB, Kebede EB, Akuma AO. Breast self-examination practice among women in Jimma, Southwest Ethiopia: A community-based cross-sectional study. Breast Cancer: Targets Ther. (2020) 12:181.
25. Abay M, Tuke G, Zewdie E, Abraha TH, Grum T, Brhane E. Breast self-examination practice and associated factors among women aged 20–70 years attending public health institutions of Adwa town, North Ethiopia. BMC Res Notes. (2018) 11:1–7. doi: 10.1186/s13104-018-3731-9
26. Akhtari-Zavare ZIM, Hanafiah JM, Abdul MR, Zarina II. Knowledge on breast cancer and practice of breast self examination among selected female university students in Malaysia. Med Health Sci J. (2011) 7:49–56. doi: 10.15208/mhsj.2011.132
27. Ahmed A, Zahid I, Ladiwala ZFR, Sheikh R, Memon AS. Breast self-examination awareness and practices in young women in developing countries: A survey of female students in Karachi, Pakistan. J Educ Health Promotion. (2018) 7. doi: 10.4103/jehp.jehp_147_17
28. Dadzi R, Adam A. Assessment of knowledge and practice of breast self-examination among reproductive age women in Akatsi South district of Volta region of Ghana. PloS One. (2019) 14:e0226925. doi: 10.1371/journal.pone.0226925
29. Sama C-B, Dzekem B, Kehbila J, Ekabe CJ, Vofo B, Abua NL, et al. Awareness of breast cancer and breast self-examination among female undergraduate students in a higher teachers training college in Cameroon. Pan Afr Med J. (2017) 28:164–. doi: 10.11604/pamj.2017.28.91.10986
30. Salem MAA, Al Shazly HA, Ibrahem RA, Kasemy ZA, Abd El-Roaf SY. Knowledge, attitude, and practice of breast self-examination among women attending primary health care facility, Menoufia Governorate, Egypt. Menoufia Med J. (2020) 33:44. doi: 10.4103/mmj.mmj_557_15
31. Abeje S, Seme A, Tibelt A. Factors associated with breast cancer screening awareness and practices of women in Addis Ababa, Ethiopia. BMC women’s Health. (2019) 19:1–8. doi: 10.1186/s12905-018-0695-9
32. Dinegde NG, Demie TG, Diriba AB. Knowledge and practice of breast self-examination among young women in tertiary education in Addis Ababa, Ethiopia. Breast Cancer: Targets Ther. (2020) 12:201.
33. Sharaa HM. Beliefs and reported practices related to breast self-examination among sample of Egyptian women. Acad J Cancer Res. (2013) 6:99–110.
34. Petro-Nustus W, Mikhail BI. Factors associated with breast self-examination among Jordanian women. Public Health Nursing. (2002) 19:263–71.
35. Dye TD, Bogale S, Hobden C, Tilahun Y, Deressa T, Reeler A. Experience of initial symptoms of breast cancer and triggers for action in Ethiopia. Int J Breast Cancer. (2012) 2012. doi: 10.1155/2012/908547
36. Desta F, Workicho A, Atomsa A, Workneh D, Tebeje B. Knowledge, practice and associated factors of breast self examination among female students of the College of Public Health and Medical Science, Jimma University, Ethiopia. Am J Health Res. (2018) 6:44–50. doi: 10.11648/j.ajhr.20180602.12
37. Organization WH. Cancer control: knowledge into action. WHO guide for effective programmes. Early detection. Cancer control: knowledge into action WHO guide for effective programmes Early detection. U.S., Europe, Asia, Canada, and Australia (2007).
38. Zeru Y, Sena L, Shaweno T. Knowledge, attitude, practice, and associated factors of breast cancer self-examination among urban health extension workers in addis ababa, central Ethiopia. J Midwifery Reprod Health. (2019) 7:1662–72.
39. Veena K, Kollipaka R, Rekha R. The Knowledge and attitude of breast self examination and mammography among rural women. Int J Reproduct Contraception Obstet Gynecol. (2015) 4:1511–7.
40. Odwan MIA, Khreisat IF, Farhan A, Khasawneh AA, Sqour RA. Knowledge attitude and practice of breast self examination among female graduates in Princess Muna College of nursing and royal medical services college of allied health professions. JRMS. (2016) 23:41–53. doi: 10.12816/0032200
41. Obaikol R, Galukande M, Fualal J. Knowledge and practice of breast self examination among female students in a sub Saharan African University. East Cent Afr J Surg. (2010) 15:22–7.
42. Faronbi JO, Abolade J. Breast self examination practices among female secondary school teachers in a rural community in Oyo State, Nigeria. Open J Nursing. (2012) 2:111. doi: 10.4236/ojn.2012.22017
43. Ayed A, Lubna FE, Fashafsheh HI, Nazzal S, Deena BT, Awawdeh HR. Breast self-examination in terms of knowledge, attitude, and practice among nursing students of arab american university/jenin. J Educ Pract. (2015) 6:37–48.
44. Birhane K, Alemayehu M, Anawte B, Gebremariyam G, Daniel R, Addis S, et al. Practices of breast self-examination and associated factors among female debre berhan university students. Int J Breast Cancer. (2017) 2017:8026297. doi: 10.1155/2017/8026297
45. Segni MT, Tadesse D, Amdemichael R, Demissie H. Breast self-examination: knowledge, attitude, and practice among female health science students at Adama Science and Technology University, Ethiopia. Gynecol Obstet (Sunnyvale). (2016) 6:2161–0932.
46. Parsa P, Kandiah M, Parsa N. Factors associated with breast self-examination among Malaysian women teachers. Eastern Mediterr Health J. (2011) 17. doi: 10.26719/2011.17.6.509
47. Sujindra E, Elamurugan TP. Knowledge, attitude, and practice of breast self-examination in female nursing students. Int J Educ psychol Res. (2015) 1:71. doi: 10.4103/2395-2296.152216
48. Lombe Mumba R. Knowledge attitude and practice of breast-self examination for early detectoin of breast cancer among women in roan constituency in luanshya, Copperbelt province, Zambia. Asian Pac J Health Sci. (2017) 4:74–82. doi: 10.21276/apjhs.2017.4.3.12
49. Getu MA, Kassaw MW, Tlaye KG, Gebrekiristos AF. Assessment of breast self-examination practice and its associated factors among female undergraduate students in Addis Ababa University, Addis Ababa, Ethiopia, 2016. Breast Cancer: Targets Ther. (2019) 11:21.
50. CEOWORLD Health Care Index. Best Healthcare in the World 2022 (2022). Available online at: https://worldpopulationreview.com/country-rankings/best-healthcare-in-the-world (accessed November 01, 2024).
51. Sani AM, Naab F, Aziato L. Influence of educational level on knowledge and practice of breast self−examination among women in sokoto, Nigeria. J Basic Clin Reprod Sci. (2017) 5.
52. Ibrahim SQ AW, Ahmed HM, Al-Banna DA. Impact of education program on breast self examination among a group of women in the Kurdistan Women Union, Erbil city. Zanco J Med Sci (Zanco J Med Sci). (2016) 20:1450_7. doi: 10.15218/zjms.2016.0044
53. Hassan MR, Ghazi HF, Mohamed AS, Jasmin SJ. Knowledge and practice of breast self-examination among female non-medical students in universiti Kebangasaan Malaysia (UKM) in Bangi. MJPHM. (2017) 17:51–8.
54. Olaogun JG, Emmanuel EE, Dada SA, Odesanmi OM, Adesua OA. The prevalence of practicing breast self-examination and knowledge of breast cancer disease among women attending secondary health facility. Int Surg J. (2017) 4:3211–7. doi: 10.18203/2349-2902.isj20174491
55. Ojewusi AA, Arulogun OS. Breast cancer knowledge and screening practices among female secondary schools teachers in an urban local government area, Ibadan, Nigeria. J Public Health Epidemiol. (2016) 8:72–81. doi: 10.5897/JPHE2015.0781
56. Al-Azmy SF, Alkhabbaz A, Almutawa HA, Ismaiel AE, Makboul G, El-Shazly MK. Practicing breast self-examination among women attending primary health care in Kuwait. Alexandria J Med. (2013) 49:281–6. doi: 10.1016/j.ajme.2012.08.009
57. Jelinski SE, Maxwell CJ, Onysko J, Bancej CM. The influence of breast self-examination on subsequent mammography participation. Am J Public Health. (2005) 95:506–11. doi: 10.2105/AJPH.2003.032656
Keywords: breast self-examination, knowledge, practice, female teachers, Ethiopia
Citation: Yazew BG, Alemu BW and Walle TA (2024) Factors associated with knowledge and practice of breast self-examination among female governmental school teachers in Gondar Town, Northwest Ethiopia, 2019. Front. Oncol. 14:1481714. doi: 10.3389/fonc.2024.1481714
Received: 16 August 2024; Accepted: 25 November 2024;
Published: 24 December 2024.
Edited by:
Giorgio De Nunzio, University of Salento, ItalyReviewed by:
Emanuele Rizzo, University of Salento, ItalyMulugeta Tenna Wolde, University of Global Health Equity, Rwanda
Copyright © 2024 Yazew, Alemu and Walle. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Birhaneslasie Gebeyehu Yazew, a2Fzc2lzaDZAZ21haWwuY29t
 Birhaneslasie Gebeyehu Yazew
Birhaneslasie Gebeyehu Yazew Biresaw Wassihun Alemu
Biresaw Wassihun Alemu Tarkie Abebe Walle3
Tarkie Abebe Walle3