
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol., 23 July 2024
Sec. Surgical Oncology
Volume 14 - 2024 | https://doi.org/10.3389/fonc.2024.1402360
This article is part of the Research TopicSurgical Oncology in the Elderly: The State of the Art and Future Challenges - Vol. IIView all 5 articles
Objective: Radical cystectomy with ileal conduit is the current mainstay of treatment for muscle-invasive bladder cancer and is also a high-risk procedure. Existing studies have limited targeted assessment of the efficacy and safety of this procedure, and the patient population appropriate for this procedure is still poorly defined. We sought to longitudinally analyze differences in the efficacy and safety of radical cystectomy with ileal conduit by age subgroups to assess whether the age factor should be used as an exclusion criterion when selecting this procedure.
Materials and methods: We retrospectively examined the clinicopathological data of patients with MIBC treated with RC with IC at the Cancer Hospital of Harbin Medical University between February 2014 and October 2023. Additionally, we utilized clinical and pathological data from the SEER database (2000-2020) for external validation of our findings. Patients were categorized into elderly (≥70 years at diagnosis) and non-elderly (<70 years) groups. Statistical analyses included t-tests, non-parametric tests for continuous data, chi-square tests for categorical data, and Kaplan-Meier survival analysis.
Results: In this study, 152 patients were included: 119 were categorized as non-elderly and 33 as elderly. For external validation, data from 416 patients in the SEER database were analyzed, with 172 classified as non-elderly and 244 as elderly. The results indicated that elderly patients were more likely to require ICU transfer postoperatively but exhibited a lower incidence of stoma inflammation. Additionally, both the data from our center and the external validation from the SEER database showed a concordance in cancer-specific survival (CSS) between the elderly and non-elderly groups. The efficacy of RC with IC was comparable in both elderly and non-elderly patients.
Conclusion: For longitudinal age subgroups, RC with IC for both elderly and non-elderly MIBC had good efficacy and safety, and good quality of life after surgery. Although there are surgical and perioperative risks in elderly patients, there is no significant difference compared with non-elderly patients. In elderly patients requiring RC for bladder cancer, IC should remain the preferred mode of urinary diversion, and old age should not be used as an absolute exclusion criterion for IC.
Bladder cancer is the ninth most common cancer globally, with approximately 610,000 new cases and 220,000 deaths annually, as reported in the 2022 Global Cancer Statistics (1). The disease predominantly affects the elderly; statistical data reveal that the median age at diagnosis is 73 years, and individuals over 65 years old constitute about 75% of all bladder cancer patients. As bladder cancer incidence increases with age, and with the global population aging, it is projected that the number of elderly patients will continue to rise. (2).
Muscle-invasive bladder cancer(MIBC) represents a severe pathological stage of bladder cancer. Radical cystectomy(RC) with pelvic lymph node dissection is the established standard treatment for this condition. After RC, the choice of urinary diversion method is crucial and must be tailored to each patient’s specific circumstances. The primary methods of urinary diversion include cutaneous ureterostomy, ileal conduit(IC), and neobladder construction. Among these, the IC is the most widely adopted globally due to its favorable impact on urinary function and quality of life, as well as its relatively low demands on patient compliance (3).
Previous studies on the use of RC for treating MIBC in elderly patients have shown conflicting results. Some research indicates that older patients experience higher complication rates (4), and that increasing age correlates with poorer survival outcomes (2, 5). However, other studies assert that RC is safe for elderly patients, arguing that it does not necessitate routine intensive postoperative monitoring and is associated with acceptable perioperative morbidity and mortality rates (6). Given the conflicting results from previous studies and the lack of focused analysis on specific urinary diversion modalities, we conducted a retrospective and follow-up study of both elderly and non-elderly patients who underwent RC with IC at our institution. Additionally, we utilized data from the SEER database to externally validate our findings.
Inclusion criteria were patients with bladder cancer who underwent RC with extracorporeal IC from February 2014 to October 2023 at the Affiliated Cancer Hospital of Harbin Medical University and defined patients whose age was greater than or equal to 70 years old at the time of diagnosis as elderly patients and patients younger than 70 years old as non-elderly patients. Exclusion criteria: ① patients with bladder cancer who had undergone neoadjuvant chemotherapy or neoadjuvant immunotherapy before surgery, and patients with recurrent bladder cancer who were still in the cycle of cystoperfusion chemotherapy ② patients with non-muscle invasive bladder cancer with postoperative pathological confirmation of pT stage less than T2 (Due to the high risk of progression to pT2, pT is still included in this study) ③ patients with distant metastases confirmed by imaging before surgery, i.e., clinical stage Patients with bladder cancer with cM>0 ④ Patients who had been lost to telephone follow-up and those who were unable to complete the questionnaire by answering the questions on their own or without the assistance of a relative to complete the questionnaire.
Surgeries were performed according to Chinese urological guidelines (7), The general procedure of laparoscopic RC with IC is to clear the pelvic lymph nodes → resection the bladder → establish the ileocecal channel, and open IC of the bladder with IC to resect the bladder → clear the pelvic lymph nodes → establishment of the ileocecal channel. The surgical scope of both procedures is the bladder and surrounding tissues, the distal ureter, and pelvic lymph on both sides, including the prostate and seminal vesicles in male patients; and the uterus, part of the anterior vaginal wall, and adnexa in female patients. Intraoperative rapid frozen pathology was performed for any suspected positive tissue breaks. Pelvic lymph nodes were cleared medially to the ureter, laterally to the genitofemoral nerve, proximally to the bifurcation of the common iliac vessels, and distally to the deep spinothalamic vein. For the IC, a 15 cm length of ileal intestinal segment 15 cm from the ileocecal region was selected, preserving the mesenteric blood supply, with a distal stoma in the right rectus abdominis muscle paraspinalis, and proximally connecting to the right and left ureters of the lateral anastomosis. Intraoperative drains were placed, one abdominal drain, one pelvic drain, and one transurethral pelvic drain.
Patient information, including clinical, pathological, and surgical characteristics, is extracted from the electronic medical record (EMR) system.
Post-operative follow-up was done by telephone. If the patient died, the cause and time of death were asked, and if the death was related to the bladder tumor, the patient was further asked about the time of diagnostic recurrence; if the patient survived, the patient was investigated for postoperative disease up to the last week, with questions about complications and the patient’s tumor progression. Complications included urinary tract infections, gastrointestinal dysfunction, and ileal access fistulae within 1 week of the follow-up time. Urinary tract infection was defined as patients presenting with fever, chills, low back pain, and a bacterial colony count ≥10^5 CFU/ml confirmed by urine bacteriological culture. Gastrointestinal dysfunction was defined as patients presenting with abdominal pain, abdominal cramps, vomiting, and cessation of defecation with imaging to rule out other acute abdominal conditions. Stoma injury was categorized as complications affecting both the stoma and its adjacent skin. Specifically, stoma skin inflammation was identified as irritant contact dermatitis, clinically presenting with symptoms such as redness, swelling, hard nodules, papules, and herpetic lesions on the stoma and surrounding skin, as reported by patients within one week of follow-up. Stoma obstruction was defined by imaging-confirmed fluid accumulation in unilateral or bilateral kidneys or ureters, caused by stones in the stoma or other factors. Additionally, stoma hemorrhage was described as bleeding from the stoma due to causes other than stones, infections, or inflammation, including bleeding related to stoma care operations or unexplained gross hematuria. The primary endpoints for survival analysis were overall survival (OS), recurrence-free survival time (RFS), and cancer-specific survival (CSS). OS is the time between the initial MIBC diagnosis and the time of death from any cause or the time of the last follow-up visit. RFS is the time between the initial MIBC diagnosis and the time of clinically confirmed recurrence is the time between the initial MIBC diagnosis and death due to MIBC.
Patients were also asked to complete the modified Complications Clavien Classification System (CCS) at 30 days postoperatively and 90 days postoperatively at follow-up and to complete the FACT-BL questionnaire asking about their recent quality of life. The Clavien Classification System is a strategy proposed by Clavien et al. in 1992 to rank surgical complications based on the consequences of treatment (8), it has been popularized and widely used for postoperative assessment in urology, especially after modification and improvement in large cohort studies (9, 10). The FACT-BL is a bladder cancer-specific quality of life (QOL) measure that includes five dimensions: physical health, social/family health, emotional health, functional health, and bladder cancer-specific concerns, with specific questions scored on a 5-point scale (11), with higher scores being associated with better quality of life. The subscales were summed to give a total FACT-BL score (range 0 - 156) after the patient completed the questionnaire to assess the patient’s quality of life in the last 1 week (12).
Patients diagnosed with bladder cancer between 2000 and 2020 were identified by the Surveillance, Epidemiology, and End Results (SEER) Cancer Registry using the SEER*STAT (version 8.4.3) software, following approval from the National Cancer Institute. Patients were identified using the original site of the tumor as the bladder. The patient population was selected to be essentially the same as the patient population in our center, and the inclusion criteria were (1) pathological diagnosis of bladder cancer from 2000-2019; (2) complete clinical information; and (3) patients of patients who underwent RC with IC. The exclusion criteria were as follows: (1) pT stage less than 2 and pM stage greater than 0; (2) missing or unknown clinical information; and (3) patients who had undergone preoperative radiotherapy and neoadjuvant chemotherapy. The following clinicopathological factors were retrieved as variables for analyzing differences between groups: age, sex, TNM stage, survival time, and cause of death. Since the seer database does not contain detailed perioperative laboratory tests and the recovery process of the patients, only external validation of efficacy, i.e., OS and CSS, was performed.
Descriptive statistics were used to describe demographic and clinical characteristics. For measurements that conformed to a normal distribution with chi-square, differences between groups were analyzed using the independent samples t-test, otherwise, the Mann-Whitney U non-parametric test was used. For count data, the chi-square test was used to analyze differences between groups. For outcomes that included time of occurrence the Kaplan-Meier method was used to plot survival curves and analyze differences between groups. All the above analyses were done using SPSS (version 20, IBM, Armonk, NY, United States). A P<0.05 was considered by statistical significance.
All 152 patients included in our center underwent RC of the bladder with an IC at the Cancer Hospital of Harbin Medical University and were followed up. Most of the patients were male (n=131,86%). Patients were divided into elderly patients (n=33,22%) and non-elderly patients (n=119,78%) according to whether they were >70 years old at the time of diagnosis of bladder cancer. There was no statistically significant difference between the two groups in terms of pathological stage and whether it was accompanied by poor histological differentiation (P=0.618, P=0.524). The basic information and clinical characteristics of the patients are shown in Table 1.
In this study, we initially compared the preoperative risk scores between two patient groups. The results demonstrated statistically significant differences in ASA, CCI, and PNI scores (ASA: P=0.001, CCI: P=0.017, PNI: P<0.001). Specifically, elderly patients had higher CCI scores compared to the non-elderly group (CCI 1 [12% vs. 19%], CCI 2 [18% vs. 9%], CCI ≥3 [15% vs. 1%]; P=0.017), higher ASA scores (ASA 1 [42% vs. 70%], ASA 2 [24% vs. 23%], ASA 3 [21% vs. 6%], ASA 4 [12% vs. 1%]; P=0.001), and lower PNI scores (43.5 vs. 47.9; P<0.001). These findings are detailed in Table 2.
The analysis of patients’ surgical characteristics revealed that the only statistically significant difference between the groups was the likelihood of ICU transfer post-surgery, with elderly patients being at a higher risk ([30% vs. 6%]; p<0.001). There were no significant differences in surgery duration (370 vs. 335 minutes; p=0.459), intra-operative hemorrhage (300 ml vs. 200 ml; p=0.071), or the rate of blood transfusions (33% vs 42%; p=0.368), as detailed in Table 3. Subgroup analyses were conducted to assess potential biases due to surgical modality and operator factors. The results indicated that variations in surgical modality and operator did not significantly affect the risk of postoperative ICU transfers, as shown in Supplementary Table 1. Differences in reasons for ICU transfers and the duration of ICU stays are presented in Supplementary Table 2.
For a comparison of perioperative risks between elderly and non-elderly patients, the length of parenteral nutrition (6 days vs. 6 days; p=0.559), antibiotic use (7 days vs. 7 days; p=0.426), and the duration of drain drainage (abdominal drainage [7 days vs. 7 days; p=0.248], pelvic drainage [8 days vs. 7.9 days; p=0.064], urethral drainage [9 days vs. 9 days; p=0.93]) showed no statistically significant differences between the two groups. These findings are detailed in Table 3.
Comparative analyses of all postoperative complications were conducted between groups, including urinary tract infections, gastrointestinal dysfunction, and stoma-related issues observed during the final week of follow-up. A modified Clavien classification system was used to evaluate these complications, as detailed in Table 4. Statistically significant differences were noted in the incidence of stoma inflammation and in the severity according to the modified Clavien classification. Older patients exhibited a lower incidence of stoma inflammation (15% vs. 32%; p=0.04) and higher complication severity, as indicated by the Clavien classification scores at 30 days (p=0.001) and 90 days (p=0.001) compared to the non-elderly group. However, there were no statistically significant differences in the rates of urinary tract infections (15% vs. 22%; p=0.398), gastrointestinal dysfunction (9% vs. 3%; p=0.165), stoma obstruction (3% vs. 4%; p=0.734), and stoma bleeding (12% vs. 24%; p=0.125) at follow-up. An analysis of the factors influencing stoma inflammation is shown in Supplementary Table 3, which shows that a higher percentage of stoma discs were replaced by others in the elderly group than in the non-elderly group (patients replaced themselves [9% vs 60%], cooperatively [36% vs 40%], and by others [55% vs 0%]; P<0.001), with the same frequency of replacement (less than 1 week [52% vs 37%], 1-2 weeks [37% vs 55%], greater than 2 weeks [21% vs 8%]; P= 0.968). Defining the emergence of the first postoperative urinary tract infection and gastrointestinal dysfunction as the outcome, and the time of the first occurrence of both complications as the time of the occurrence of the outcome, the survival analysis of postoperative urinary tract infection and postoperative gastrointestinal dysfunction was carried out and the survival curves were plotted, and the results showed that there was no statistically significant difference between the groups of urinary tract infection and intestinal obstruction, as shown in Figure 1.
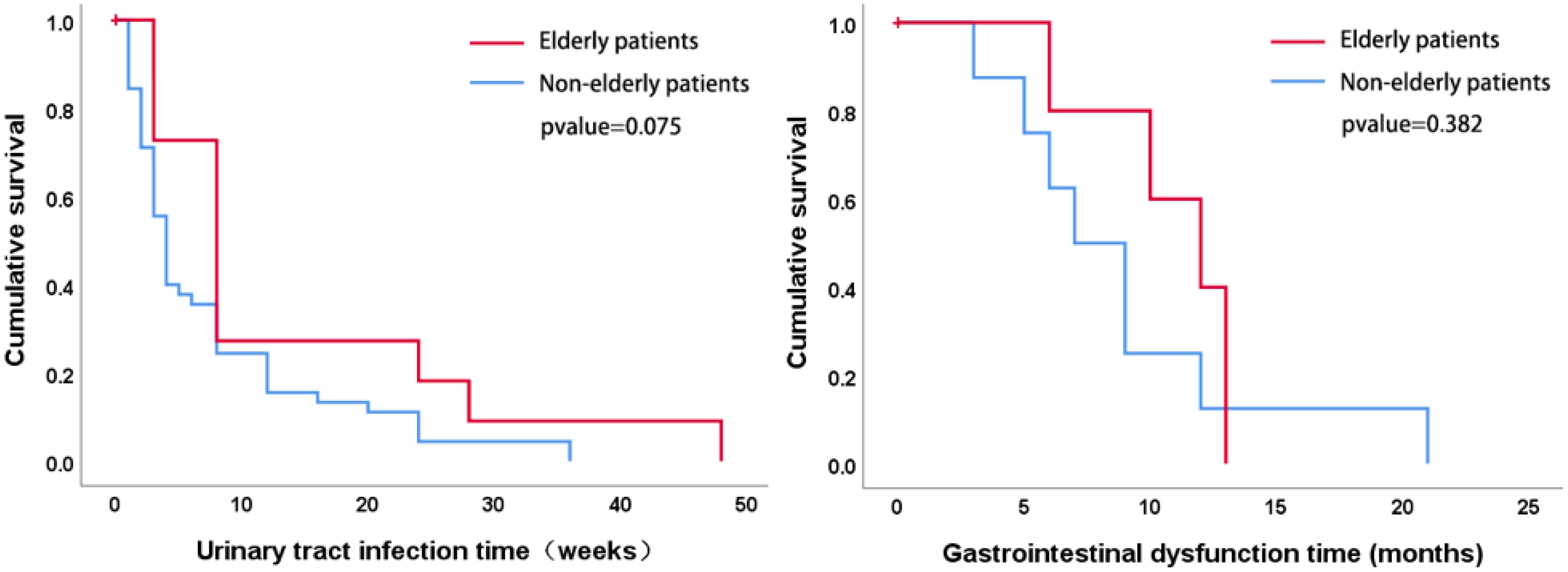
Figure 1 Survival analyses were performed on indicators that included time to first postoperative presentation and survival curves were plotted, which showed no statistically significant differences between the urinary tract infection and bowel obstruction groups.
The analysis of the treatment effect primarily focused on the surgical outcomes, clinical survival, and patients’ FACT-BL scores. Surgical outcomes compared included the number of cleared lymph nodes, the percentage of pathologically positive lymph nodes, 1-year and 3-year postoperative survival rates, rates of urethral recurrence, and distant metastasis. The between-group analysis showed no statistically significant differences in the number of cleared lymph nodes (14.06 vs. 12.19; p=0.44), percentage of positive lymph nodes (4.7% vs. 3.7%; p=0.937), 1-year (96.9% vs. 95.8%; p=0.76) and 3-year survival rates (87.9% vs. 89.9%; p=0.74), urethral recurrence (0% vs. 4.38%; p=0.23), and distant metastasis rate (15.15% vs. 15.96%; p=0.91), as presented in Table 5. Additionally, survival analyses comparing cancer-specific survival (CSS), recurrence-free survival (RFS), and overall survival (OS) over an average follow-up of 34 months (Figure 2) indicated no significant differences in therapeutic efficacy between elderly and non-elderly patients. Furthermore, comparisons of FACT-BL scores revealed mean total scores of 111 for non-elderly patients and 112 for elderly patients, with no significant differences across the dimensions of physical, social/family, emotional, functional health, and specific concerns about bladder cancer, as detailed in Table 5.
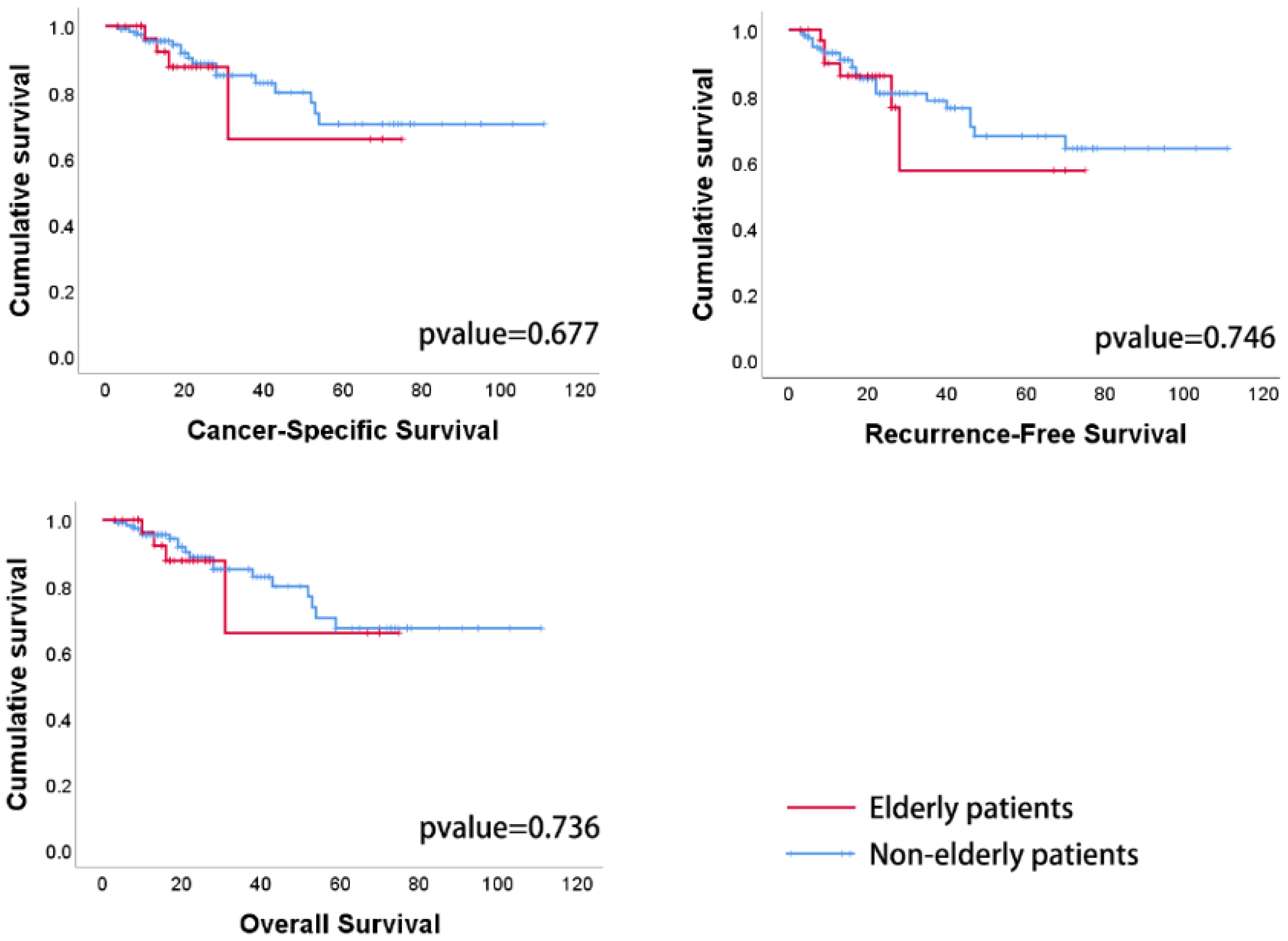
Figure 2 Patient survival times are expressed in months. There were no statistically significant differences in CSS, RFS, or OS between elderly and nonelderly patients.
A total of 416 patients were included in the Seer database, including 172 patients (41%) in the non-elderly group and 244 patients (59%) in the elderly group, and the process of screening and grouping of patients is shown in Figure 3. There was no statistically significant difference in the gender composition, T-stage, and N-stage between the two groups of patients, and the results are shown in Table 6. The Kaplan-Meier method was used to compare the OS and CSS of elderly patients with those of non-elderly patients, and the OS was shorter in elderly patients (p= 0.021) than in non-elderly patients, but the difference in CSS was not statistically significant (p=0.241), and the surgical efficacy of the elderly group was comparable to that of the non-elderly group, and the externally validated results were basically in line with the results of the analysis of our center (Figure 4).
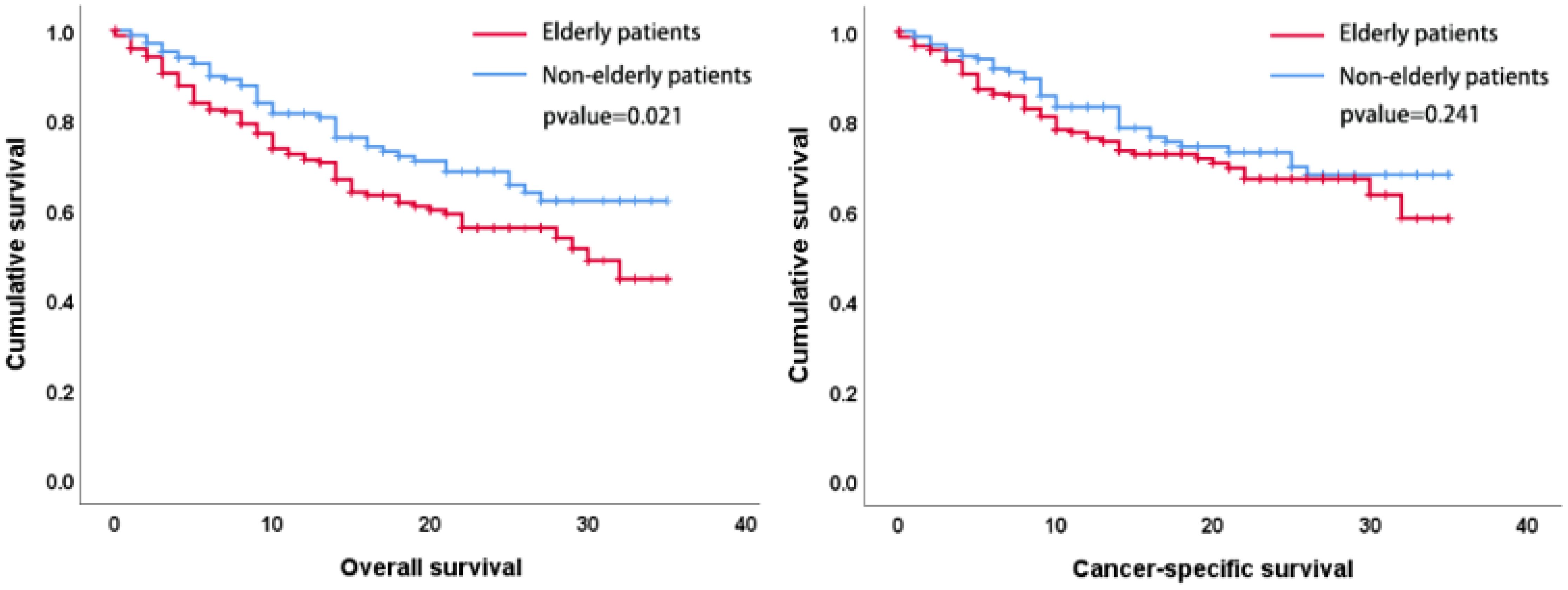
Figure 4 Patient survival times are expressed in months. The OS was shorter in elderly patients (p=0.021) than in non-elderly patients, but the difference in CSS was not statistically significant (p=0.241).
RC is the current standard procedure for the treatment of MIBC, especially with the current development of minimally invasive surgical techniques in urology, more and more relevant studies have reported the advantages of LRC and RARC over traditional ORC in terms of reducing intraoperative bleeding, perioperative blood transfusion, and many other aspects (13–15). The minimally invasive surgical approach to RC seems to have become a paradigm for doctors and patients in clinical practice, but there has been no uniform standard on how to divert urinary flow after RC, whether minimally invasive or open surgery. The mode of urinary diversion has been associated with a variety of postoperative complications, and the selection of an appropriate urinary diversion for a patient requires careful consideration of a number of factors, including the patient’s age, concomitant diseases, preoperative renal function, and life expectancy.CU, IC, and in situ neobladder are the common choices for urinary diversion in current clinical practice. Although IC has the disadvantages of longer operative time, higher bleeding, and longer recovery of bowel function than CU, and does not have the advantages of in situ neobladder in controlling urination and eliminating the need for urinary bags, IC is still the first choice for urinary diversion in elderly patients due to the fact that it does not require frequent catheter changes, long-term functional exercise, relatively fewer complications, and easier care. For the assessment factor of age, there are now many studies comparing cross-sectional efficacy and safety between different surgical procedures in elderly patients with MIBC (16–20). However, there is still a gap in studies comparing the differences of a single surgical procedure under different age subgroups. Therefore, a longitudinal analysis of the efficacy and safety of RC with IC in the treatment of different age subgroups to determine whether old age should be used as an exclusion criterion for the selection of IC is of great clinical significance and reference value.
To define the grouping criteria of elderly and non-elderly patients, we conducted a review of the literature on RC. The global median age for bladder cancer patients is 73 years, while the average and median ages of the 349,800 patients in the SEER database are 69 years and 70 years, respectively. Based on these statistics and current published research, we determined that using 70 years as the cut-off point for classifying elderly patients is a more appropriate choice. Although neoadjuvant chemotherapy (NAC) has been confirmed by several studies for its role in MIBC prognosis (21–23), NAC still suffers from low adherence among patients and age factors can influence patients’ choice of NAC (24), so the criteria were set to exclude patients who had undergone preoperative NAC to remove the effect of NAC on the survival of patients in the two groups, and to compare only the therapeutic impact of RC with IC in patients of different age subgroups.
According to this study’s analysis, both our center’s data and external validation indicate that the difference in treatment efficacy across different age subgroups is not statistically significant, demonstrating that elderly patients exhibit similar efficacy to non-elderly patients. In terms of surgical safety, our center identified three notable differences between the two age groups: variations in CCS grading, the need for postoperative ICU transfer, and the occurrence of stoma inflammation during the last week of follow-up.
We analyzed the reasons behind the higher CCS grading observed in elderly patients and found that this was attributable to a greater proportion of elderly patients receiving a score of 4. This higher scoring was linked to a higher rate of ICU transfers among the elderly, which coincides with the factors discussed in the ICU transfer analysis. These interconnected issues are discussed in further detail in the following section. In the study by Kai W Cheng et al, advanced age was identified as an influencing factor for unplanned postoperative transfer of patients to the ICU (25), whereas Wei-Yu Lin demonstrated in his study that advanced age does not lead to prolonged ICU stays (26). The results of their study are generally consistent with the results of the analysis of our center’s data. For the comparison of the risk of transfer to the ICU, there were no statistically significant differences between groups in terms of procedure, operator, and operator proficiency, and there were no significant confounders or biases in the analyses for whether or not to transfer to the ICU. Subsequently, we investigated the reasons for transferring patients to the ICU, and among the patients transferred to the ICU due to postoperative anesthesia factors that could not maintain vital signs accounted for 71% of all patients, followed by postoperative delirium (18%). All patients transferred to ICU could be transferred back to the normal ward within 2 days on average, also there were no patients in the study who had injuries or prolonged hospital stay due to transfer to ICU, and with the combined score we concluded that the risk of postoperative transfer to ICU in elderly patients was higher but it did not affect the overall surgical safety of elderly patients.
Currently, few studies have been conducted on irritant contact dermatitis of the ileal passage and surrounding skin after IC. Thirty-three percent of the patients in our center’s follow-up results had experienced peristoma itching or developed peristoma papules and herpes in the last 1 week. Grouped according to age, the analyses showed that the percentage of older patients presenting with contact dermatitis in the last week was even lower. In response to this counterintuitive finding, we further analyzed the factors that may have contributed to the offset, including differences in stoma replacement patterns and frequency of replacement in different age groups. The results showed that a higher proportion of older patients had their stomas changed by a chaperone or with the assistance of a chaperone and that more careful inspection of the stoma status and more careful cleaning may have contributed to the lower incidence of irritant dermatitis in the older group. The lack of recall of this symptom due to reduced skin sensation in the elderly group cannot be excluded.
In summary, we concluded that although there were differences in the occurrence of postoperative complications in the elderly group of patients compared with the non-elderly group, the associated health risks due to complications were still within manageable limits. Combining the survival status of the elderly group with that of the non-elderly group, we conclude that the efficacy and safety of RC with IC for the treatment of MIBC in the elderly is consistent with that of the non-elderly patients.
Finally, there are some limitations of our study. Firstly, due to the small sample size, we were unable to stratify the patients into more detailed age groups to investigate the differences in safety and efficacy between different age groups. Second, clinical retrospective studies may be affected by confounding factors, and the safety of surgery for elderly patients needs to be further verified in multicenter prospective studies.
For longitudinal age subgroups, there was concordance in the efficacy of RC with IC for the treatment of MIBC in the elderly versus the non-elderly. Although there are surgical risks in elderly patients, they do not affect the overall recovery of patients, and the difference in safety between elderly and nonelderly patients is not significant. Based on the results of the current study, old age should not be used as an absolute exclusion criterion for RC with IC.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author/s.
The studies involving humans were approved by The Ethics Committee of the Cancer Hospital of Harbin Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
HZ: Data curation, Methodology, Writing – original draft, Writing – review & editing. AL: Writing – review & editing. WW: Investigation, Writing – review & editing. SX: Data curation, Software, Writing – review & editing. CL: Writing – review & editing. LT: Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Haiyan Foundation of Harbin Medical University Cancer Hospital (NO.JJMS 2022-14).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2024.1402360/full#supplementary-material
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2018) 68:394–424. doi: 10.3322/caac.21492
2. Fonteyne V, Ost P, Bellmunt J, Droz JP, Mongiat-Artus P, Inman B, et al. Curative treatment for muscle invasive bladder cancer in elderly patients: a systematic review. Eur Urol. (2018) 73:40–50. doi: 10.1016/j.eururo.2017.03.019
3. Rammant E, Van Wilder L, Van Hemelrijck M, Pauwels NS, Decaestecker K, Van Praet C, et al. Health-related quality of life overview after different curative treatment options in muscle-invasive bladder cancer: an umbrella review. Qual Life Res. (2020) 29:2887–910. doi: 10.1007/s11136-020-02544-z
4. Froehner M, Brausi MA, Herr HW, Muto G, Studer UE. Complications following radical cystectomy for bladder cancer in the elderly. Eur Urol. (2009) 56:443–54. doi: 10.1016/j.eururo.2009.05.008
5. Dehayni Y, Tetou M, Khdach Y, Janane A, Alami M, Ameur A. [Prognostic of older age for patients with invasive-muscle-bladder cancer and treated by radical cystectomy]. Prog Urol. (2018) 28:166–72. doi: 10.1016/j.purol.2017.12.005
6. Chang SS, Alberts G, Cookson MS, Smith JA. Radical cystectomy is safe in elderly patients at high risk. J Urol. (2001) 166:938–41. doi: 10.1016/S0022-5347(05)65868-5
7. Huang J, Wang J, Kong C, Li H, Xie L, Zhou L, et al. Chinese Urology and Andrology Disease Diagnosis and Treatment Guidelines: 2019 Edition. Beijing: China Science Publishing & Media (2020). p. 51.
8. Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. (1992) 111:518–26.
9. Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. (2004) 240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae
10. Mamoulakis C, Efthimiou I, Kazoulis S, Christoulakis I, Sofras F. The modified Clavien classification system: a standardized platform for reporting complications in transurethral resection of the prostate. World J Urol. (2011) 29:205–10. doi: 10.1007/s00345-010-0566-y
11. Philipps L, Porta N, James N, Huddart R, Hafeez S, Hall E. Correlation of clinician- and patient-reported outcomes in the BC2001 trial. Clin Oncol (R Coll Radiol). (2023) 35:331–8. doi: 10.1016/j.clon.2023.02.003
12. Volz Y, Eismann L, Pfitzinger P, Westhofen T, Ebner B, Jokisch JF, et al. Long-term health-related quality of life (HRQOL) after radical cystectomy and urinary diversion - A propensity score-matched analysis. Clin Genitourin Cancer. (2022) 20:e283–90. doi: 10.1016/j.clgc.2022.03.003
13. Mastroianni R, Tuderti G, Ferriero M, Anceschi U, Bove AM, Brassetti A, et al. Robot-assisted radical cystectomy with totally intracorporeal urinary diversion versus open radical cystectomy: 3-year outcomes from a randomised controlled trial. Eur Urol. (2024) 85:422–30. doi: 10.1016/j.eururo.2024.01.018
14. Flammia RS, Licari LC, Bologna E, Mastroianni R, Proietti F, Tuderti G, et al. Comparative outcomes of open radical cystectomy vs. Robot-assisted approaches with intracorporeal and extracorporeal urinary diversion: a meta-analysis and network meta-analysis of perioperative and quality of life outcomes. J Clin Med. (2024) 13. doi: 10.3390/jcm13082421
15. Mastroianni R, Ferriero M, Tuderti G, Anceschi U, Bove AM, Brassetti A, et al. Open radical cystectomy versus robot-assisted radical cystectomy with intracorporeal urinary diversion: early outcomes of a single-center randomized controlled trial. J Urol. (2022) 207:982–92. doi: 10.1097/JU.0000000000002422
16. Chen W, Yokoyama M, Waseda Y, Kobayashi M, Fan B, Fukuda S, et al. Surgical outcomes of robot-assisted radical cystectomy in octogenarian or older patients: a Japanese nationwide study. Int J Urol. (2023) 30:1014–9. doi: 10.1111/iju.15250
17. Moeen AM, Faragallah MA, Zarzour MA, Elbehairy AA, Behnsawy HM. Ileal conduit versus single stoma uretero-cutanoustomy after radical cystectomy in patients ≥ 75 years; which technique is better? A prospective randomized comparative study. Int Urol Nephrol. (2023) 55:1719–26. doi: 10.1007/s11255-023-03609-x
18. Kadoriku F, Sasaki Y, Fukuta K, Atagi Y, Shiozaki K, Daizumoto K, et al. A propensity score matching study on robot-assisted radical cystectomy for older patients: comparison of intracorporeal ileal conduit and cutaneous ureterostomy. BMC Urol. (2022) 22:174. doi: 10.1186/s12894-022-01123-3
19. Fuschi A, Al Salhi Y, Sequi MB, Velotti G, Martoccia A, Suraci PP, et al. Evaluation of Functional Outcomes and Quality of Life in Elderly Patients (>75 y.o.) Undergoing Minimally Invasive Radical Cystectomy with Single Stoma Ureterocutaneostomy vs. Bricker Intracorporeal Ileal Conduit Urinary Diversion. J Clin Med 11. (2021). doi: 10.3390/jcm11010136
20. Adamczyk P, Kadłubowski M, Pobłocki P, Adamowicz J, Ostrowski A, Drewa T, et al. Age and risk of major complications in patients undergoing radical cystectomy for muscle invasive bladder cancer. Wideochir Inne Tech Maloinwazyjne. (2021) 16:722–7. doi: 10.5114/wiitm.2021.103918
21. Li R, Nocera L, Rose KM, Raggi D, Naidu S, Mercinelli C, et al. Comparative effectiveness of neoadjuvant pembrolizumab versus cisplatin-based chemotherapy or upfront radical cystectomy in patients with muscle-invasive urothelial bladder cancer. Eur Urol Oncol. (2024) 7(3):614–24. doi: 10.1016/j.euo.2023.12.008
22. Lu L, Chen C, Cheng H, Ding H, Tian J, Wang H, et al. Comparison of 3 and 4 cycles of neoadjuvant gemcitabine and cisplatin for muscle-invasive bladder cancer: a systematic review and meta-analysis. BMC Cancer. (2023) 23:1066. doi: 10.1186/s12885-023-11572-0
23. Kaczmarek K, Małkiewicz B, Lemiński A. Adequate pelvic lymph node dissection in radical cystectomy in the era of neoadjuvant chemotherapy: A meta-analysis and systematic review. Cancers (Basel). (2023) 15. doi: 10.3390/cancers15164040
24. Kohut-Jackson A, Orf J, Barresi D, Davaro F, Hamilton Z. Age related trends in the utilization of neoadjuvant chemotherapy for muscle invasive bladder cancer. Urol Oncol. (2024) 42(5):160.e25–160.e31. doi: 10.1016/j.urolonc.2024.01.006
25. Cheng KW, Shah A, Bazargani S, Miranda G, Cai J, Aron M, et al. Factors influencing ICU admission and associated outcome in patients undergoing radical cystectomy with enhanced recovery pathway. Urol Oncol. (2019) 37:572.e513–572.e519. doi: 10.1016/j.urolonc.2019.06.019
26. Lin W-Y, Wu CT, Chen MF, Chang YH, Lin CL, Kao CH. Cystectomy for bladder cancer in elderly patients is not associated with increased 30- and 90-day mortality or readmission, length of stay, and cost: propensity score matching using a population database. Cancer Manag Res. (2018) 10:1413–8. doi: 10.2147/CMAR.S161566
Keywords: bladder cancer, urinary diversion, radical cystectomy, ileal conduit, elderly patients, security, effectiveness, transfer
Citation: Zhang H, Li A, Wang W, Xu S, Li C and Teng L (2024) Efficacy and safety of radical cystectomy with ileal conduit for muscle-invasive bladder cancer in the elderly: a multicenter retrospective study. Front. Oncol. 14:1402360. doi: 10.3389/fonc.2024.1402360
Received: 25 March 2024; Accepted: 24 June 2024;
Published: 23 July 2024.
Edited by:
Sharon R. Pine, University of Colorado Anschutz Medical Campus, United StatesReviewed by:
Giuseppe Simone, Hospital Physiotherapy Institutes (IRCCS), ItalyCopyright © 2024 Zhang, Li, Wang, Xu, Li and Teng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lichen Teng, dGVuZ2xpY2hlbkAyMDA4LnNpbmEuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.