
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol. , 12 June 2024
Sec. Neuro-Oncology and Neurosurgical Oncology
Volume 14 - 2024 | https://doi.org/10.3389/fonc.2024.1391002
Objective: To review our single-institution experience in the surgical management of foramen magnum tumors via a far-lateral approach using an oblique straight incision.
Methods: From October 2023 to January 2024, four cases of tumors in the foramen magnum area treated at the Capital Medical University-affiliated XuanWu hospital neurosurgery department were involved in this study. All cases were managed with a far-lateral approach using an oblique straight incision. We retrospectively reviewed the clinical and imaging data, as well as the surgical strategies employed.
Results: Three cases of foramen magnum meningiomas and one case of glioma of the ventral medulla. All cases underwent a far-lateral approach using an oblique straight incision; all cases had a gross total resection, and the wounds healed well without cerebral fluid leakage or scalp hydrops. Except for one case of right foramen magnum meningioma, which had dysphagia and pneumothorax, the other cases were without any postoperative complications.
Conclusion: A far-lateral approach using an oblique straight incision can preserve muscle integrity and minimize subcutaneous exposure, allowing for complete anatomical reduction of muscles. This craniectomy method is simple and replicable, making it worthy of further clinical practice.
Although the morbidity of tumors in the foramen magnum area is low (1–3), surgical treatment of tumors in this area is still a major challenge due to the deep and narrow surgical field. A far-lateral approach is the most common approach for dealing with lesions in this area (4–7). Until recently, the high complication rate was still concerning among neurosurgeons, especially involving cerebral fluid leakage and scalp hydrops (8). Some researchers attribute CSF leakage to the inadequate suture of muscles (9). Hence, ensuring the integrity of muscle structure during craniectomy is of utmost importance to prevent CSF leakage and scalp hydrops. A straight incision applied in a far-lateral approach has been reported, but the clinical application value is still not explicit (10). In this study, we applied an oblique straight incision in four cases of tumor in the foramen magnum area using a far-lateral approach to evaluate its application value.
Four cases of tumors in the foramen magnum were surgically treated from October 2023 to January 2024. The age, sex, clinical presentation, radiological findings, tumor location, surgical details, pathology, postoperative complications, surgical outcome, and follow-up data of the patients were collected (Table 1).
All cases were performed by a senior neurosurgeon. Each patient was placed in a 3/4 prone position with their head slightly turned to the opposite side, their faces slightly rotated to the ventral side, and their neck slightly bent to ensure the lateral external auditory canal was at the highest point. The shoulder was pulled downward, and fixation was achieved using the Mayfield head frame (Figure 1A). The incision was a straight oblique one within the hairline behind the ear, with the lower boundary reaching the C4 spinous process of the midline and the upper boundary reaching 1 cm above the level of the external occipital protuberance (Figure 1B). The splenius capitis muscle was stretched along its fibers without cutting it up (Figure 1C). The semispinalis capitis muscle was cut from the upper margin and turned towards the lower edge of the incision (Figure 1D). Care was taken to identify the suboccipital triangle and vertebral artery during this process. The rectus capitis posterior major muscle was then peeled downward to expose bony landmarks (Figure 1E). Intraoperative resection followed the tumor boundary with piecemeal resection performed to protect surrounding structures and ensure surgical safety. After the tumor resection procedure, dura closure with a water-tight suture and retention of the bone flap were performed (Figure 1F). Muscles were sutured with full anatomical reduction, and the scalp was sutured intradermally (Figures 1G–I).
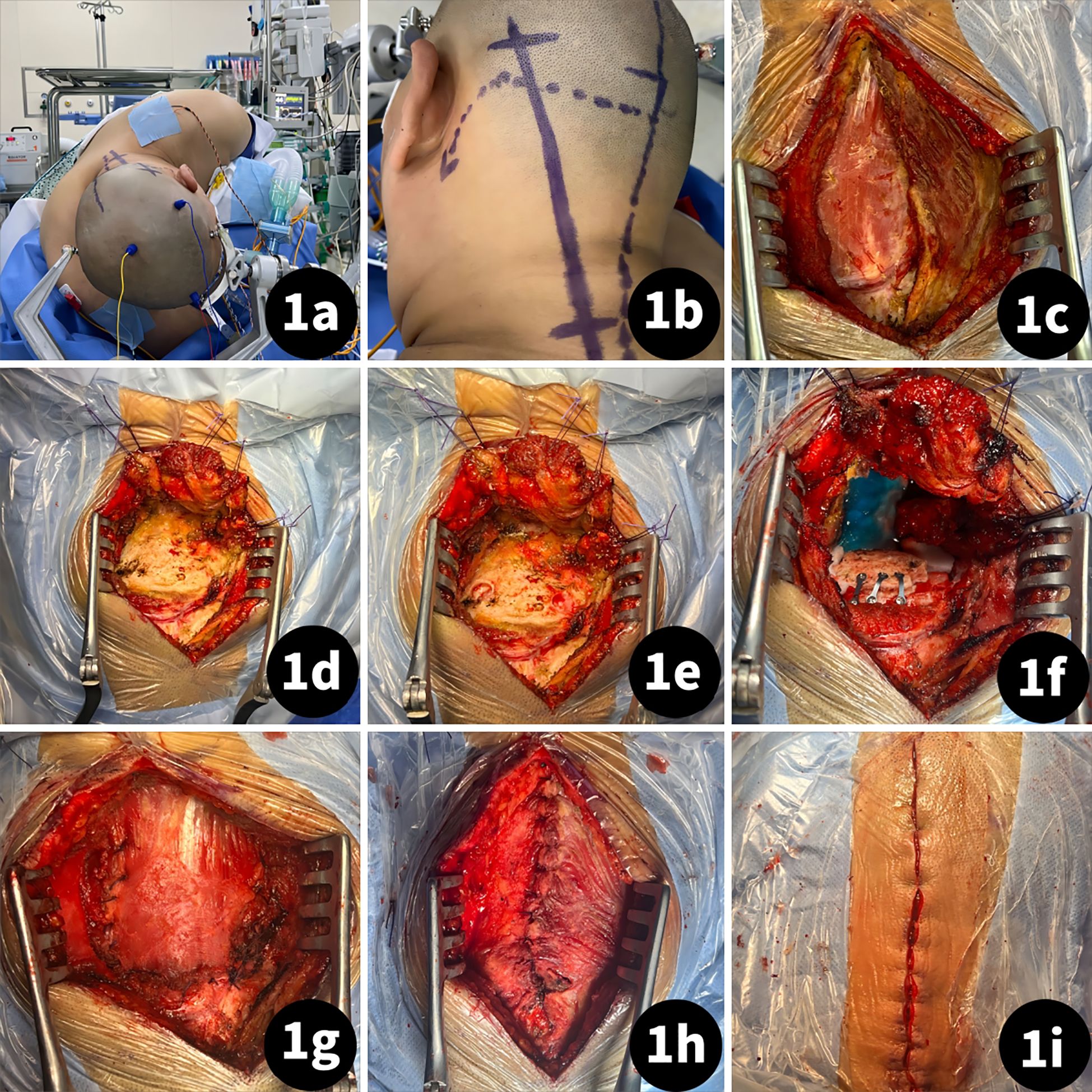
Figure 1 Craniectomy procedure of a far-lateral approach using an oblique straight incision. (A) Patient was placed in lateral position; (B) Incision designed as a straight oblique incision within the hairline behind the ear, with the lower boundary reaching the C4 spinous process of the midline and the upper boundary reaching 1 cm above the level of external occipital protuberance; (C) Stretch the splenius capitis muscle follow the fiber; (D) Cut the semispinalis capitis muscle from the upper margin and turn to Lower edge of incision; (E) peel the rectus capitis posterior major muscle downward to expose the bony landmarks; (F) bone flap retained after tumor resection and dura suture; (G) semispinalis capitis muscle suture with fully anatomical reduction; (H) splenius capitis muscle suture with fully anatomical reduction; (I) scalp suture.
Four patients (two men and two women) were included. The average age of the patients was 45.11 ± 11.62 years (range, 34–69 years). The cases involved one case of left foramen magnum meningioma, one case of right foramen magnum meningioma, one case of meningioma in the ventral medulla area, and one case of glioma of the ventral medulla.
Among all patients, there was a gross total resection and no recurrence after surgery. All cases exhibited satisfactory wound healing. Except for one case of left foramen magnum meningioma, which initially presented with dysphagia and pneumothorax but recovered within 6 months postoperatively, the other cases were without postoperative complications. All four cases were successful, and patients were followed up after discharge for 3–6 months, with an average of 4.12 ± 2.62 months. There were no new complications or recurrences in all cases.
The patient was a 35-year-old woman suffering from limb weakness for 2 months. A physical exam revealed that both upper and lower limbs had grade III muscle strength. An MR scan showed an occupation in the right foramen magnum area, with the medulla compressed by the tumor mass (Figure 2).

Figure 2 Surgical treatment of the right foramen magnum meningioma. (Case 1). (A–C) Preoperative MR scan; (D–F) Tumor resection procedure; (G–I) Postoperative MR scan.
The patient was a 55-year-old man suffering from intermittent headaches for more than 6 months. There was no neurological deficit found during physical examination. An MR scan showed a tumor was on the right side of the foramen magnum with homogeneous enhancement (Figure 3).
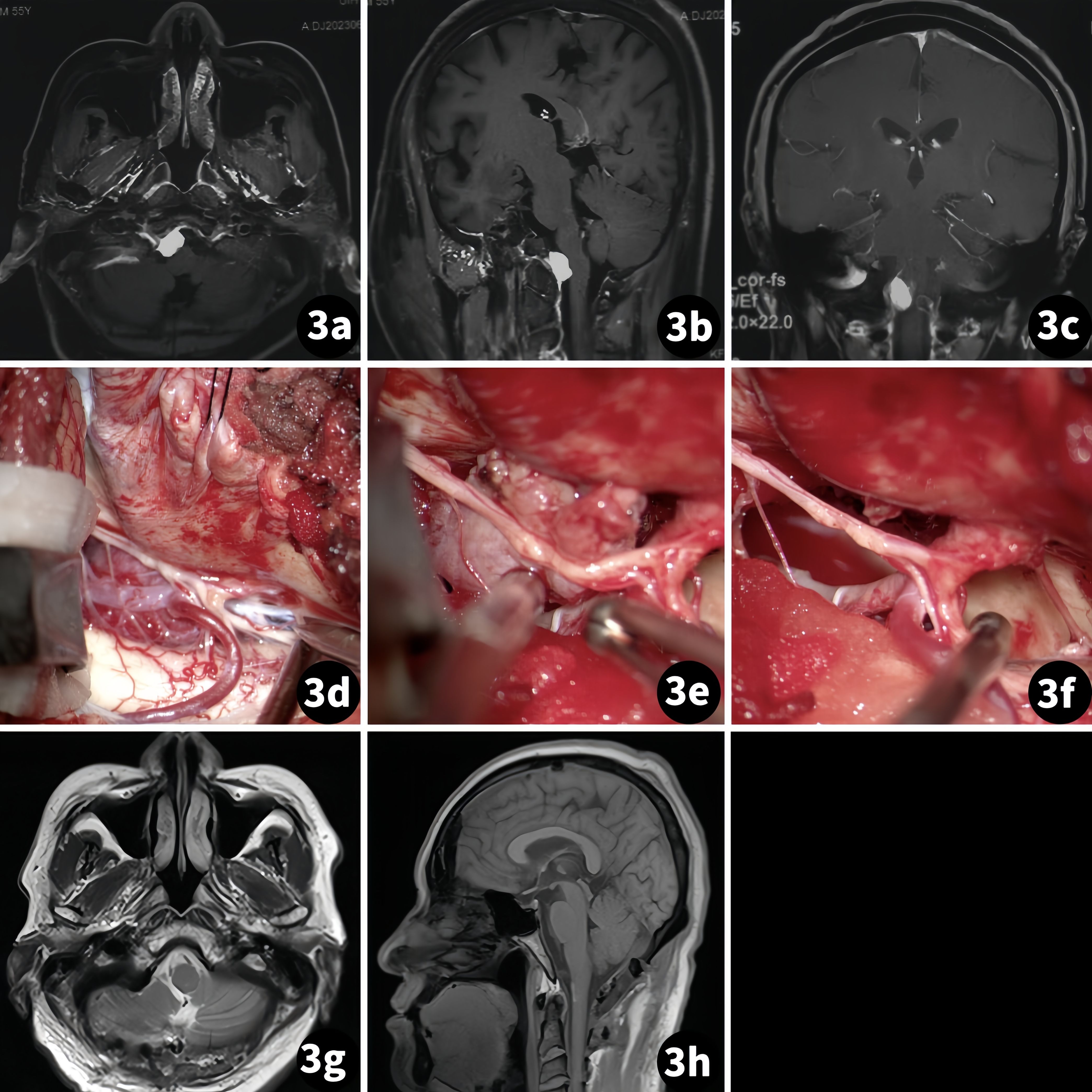
Figure 3 Surgical treatment of the right foramen magnum meningioma. (Case 2) (A–C) Preoperative MR scan; (D–F) Tumor resection procedure; (G, H) Postoperative MR scan.
The patient was a 69-year-old woman suffering from dizziness accompanied by intermittent headaches for over 5 months. A physical exam revealed limitations in the fine motor skills of both upper limbs. An MR scan showed homogeneous enhancement of a tumor mass located on the ventral side of the medulla (Figure 4).
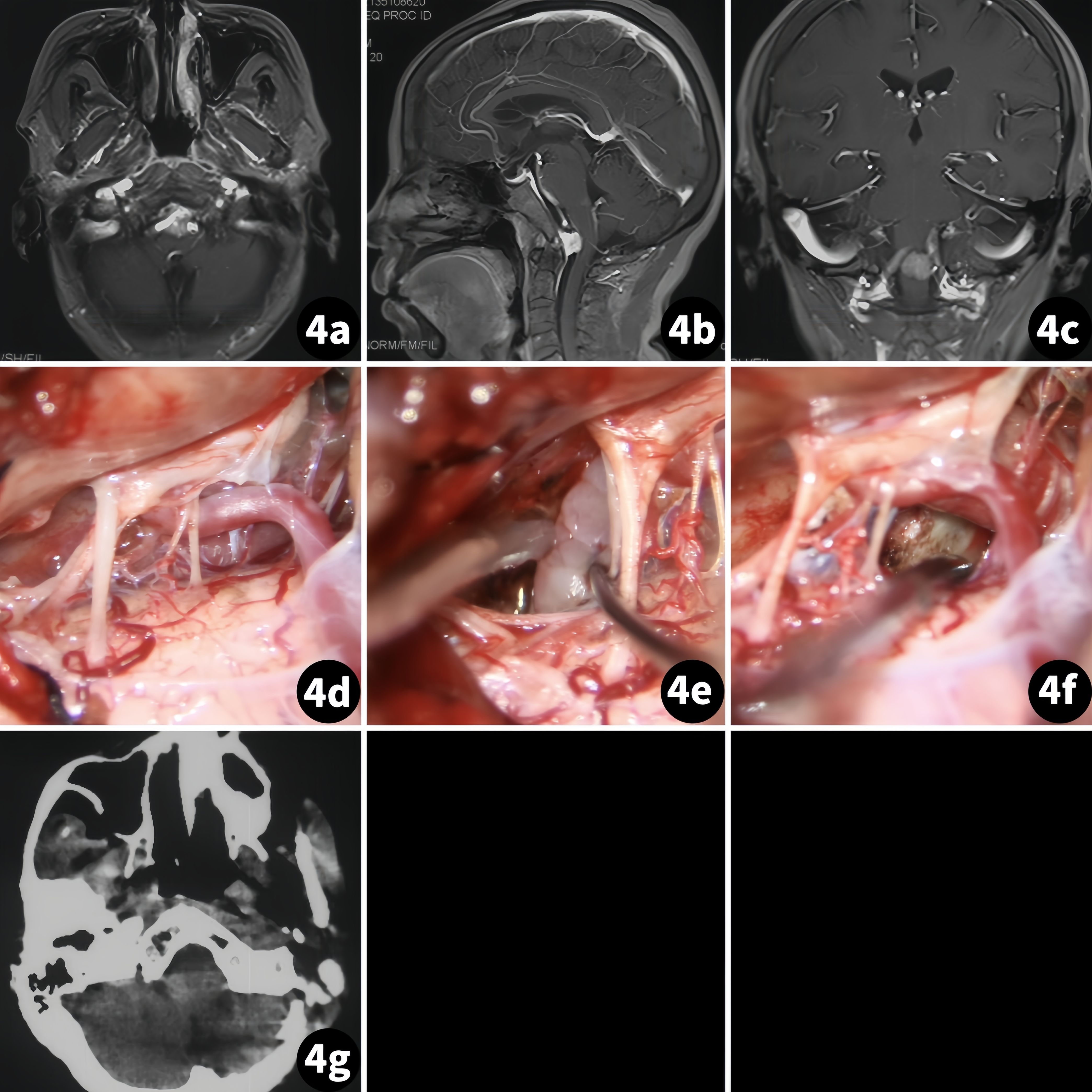
Figure 4 Surgical treatment of the foramen magnum meningioma in the ventral medulla. (Case 3) (A–C) Preoperative MR scan; (D–F) Tumor resection procedure; (G) Postoperative MR scan.
The patient was a 34-year-old man. A routine examination found a mass in the left brainstem for 2 weeks. A physical exam revealed that both the left upper and lower limbs had grade III muscle strength. An MR scan showed no obvious enhancement, and the T2 sequence presented a relative high density (Figure 5).
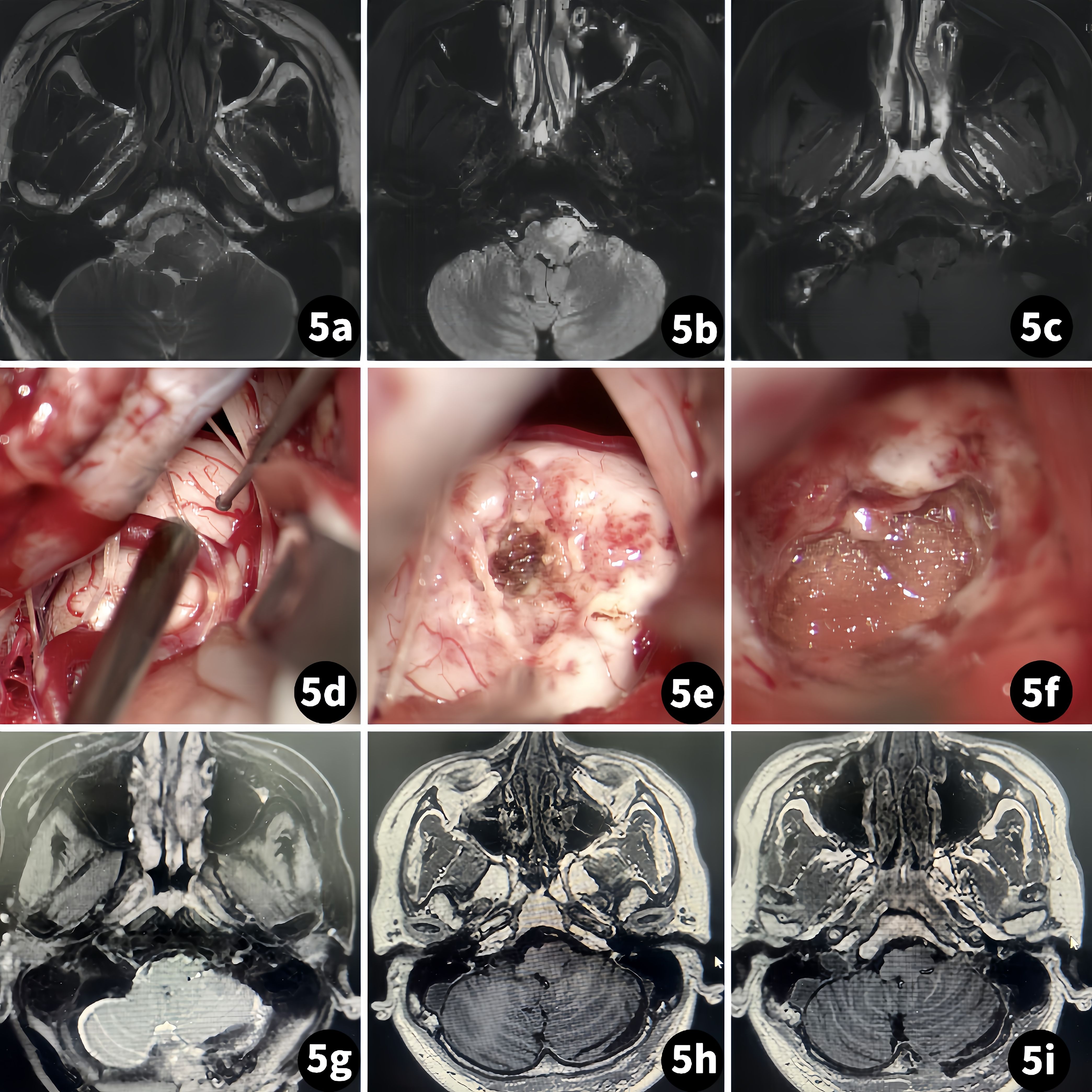
Figure 5 Surgical treatment of a glioma of the ventral medulla. (Case 4) (A–C) Preoperative MR scan; (D–F) Tumor resection procedure; (G–I) Postoperative MR scan.
A far-lateral approach is a common approach to dealing with lesions on the ventral side of the foramen magnum area and jugular foramen area (11, 12). Various surgical incisions using this approach have been reported in the literature, such as the “C”-shaped incision, the reverse “U”-shaped incision, the crutch-shaped incision, and the lateral retrooccipital “S”-shaped incision (13–17). These incisions often result in larger exposure to the subcutaneous area and greater trauma, leading to complications such as CSF leakage and scalp hydrops. Few researchers attribute these postoperative complications to muscle damage during craniectomy, failure of anatomical reduction, and extensive subcutaneous exposure (18–20). In clinical practice, we have encountered similar situations. Minimizing exposure and keeping the muscle intact for complete anatomical reduction may reduce these complications (Table 2).
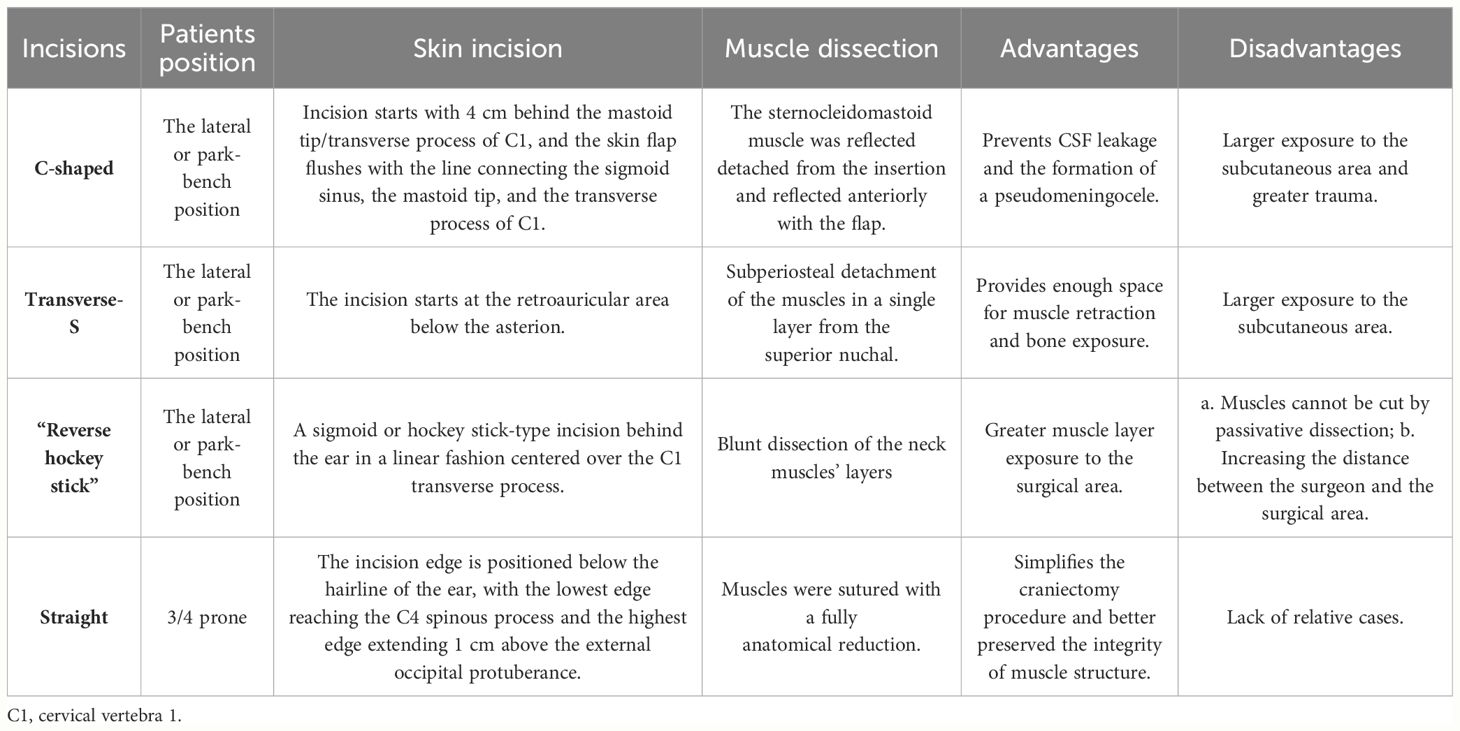
Table 2 Comparison of different incisions: C-shaped, transverse-S, “reverse hockey stick,” and straight.
We use an oblique straight incision over the C4 spinous process and 1 cm above the level of the external occipital protuberance. The main advantage of this incision is the reduction of subcutaneous area exposure. Secondly, stretching the splenius capitis muscle to follow its fibers, not cut through it, ensured its integrity. Thirdly, the semispinalis capitis muscle was cut from the upper margin and turned to the lower edge, maximizing exposure to the suboccipital triangle. In all four cases, this method provided adequate exposure and fully met the requirements of the intracranial procedure. All muscles were fully anatomically reduced with a close suture. Ensuring a close suture of the dural membrane after surgery is still a crucial step (if unable to suture, dural substitute and fibril glue are needed). Additionally, bone wax seals the mastoid air chamber, closes the scalp suture, etc. (21–25).
Except for one case of a patient with a right foramen magnum meningioma with dysphagia who recovered after conservative treatment postoperatively (6 months) and pneumothorax postoperatively (4 h) after conservative and ventilator therapy, other cases were without postoperative complications. The pneumothorax was likely caused by a subclavian puncture during anesthesia. The postoperative dysphagia was attributed to the tight adhesion of the tumor to the glossopharyngeal nerve, making the dissection procedure difficult.
Firstly, the small number of cases may have influenced our results. Secondly, some variation was inevitable when clinically applying this method. Therefore, more studies are needed to further validate our findings.
A far-lateral approach using an oblique straight incision can preserve muscle integrity and minimize subcutaneous exposure, allowing for complete anatomical reduction of muscles. This craniectomy method is simple and replicable, making it worthy of further clinical practice.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
JB: Writing – review & editing. Z-hJ: Writing – original draft. PC: Conceptualization, Investigation, Methodology, Software, Writing – review & editing, Writing – original draft. YC: Conceptualization, Formal Analysis, Writing – review & editing. Y-mW: Data curation, Validation, Writing – review & editing. GC: Conceptualization, Formal Analysis, Writing – review & editing. X-rX: Conceptualization, Methodology, Project administration, Supervision, Validation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Zhuhai Medical Research Foundation (grant nos. 2220009000150) to Z-hJ.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2024.1391002/full#supplementary-material
1. Luzzi S, Giotta Lucifero A, Bruno N, Baldoncini M, Campero A, Galzio R. Far lateral approach. Acta Biomed. (2022) 92:e2021352. doi: 10.23750/abm.v92iS4.12823
2. Flores BC, Boudreaux BP, Klinger DR, Mickey BE, Barnett SL. The far-lateral approach for foramen magnum meningiomas. Neurosurg Focus. (2013) 35:E12. doi: 10.3171/2013.10.FOCUS13332
3. Payman A, Rios Zermeno J, Hirpara A, El-Sayed IH, Abla A, Rodriguez Rubio R. Immersive surgical anatomy of the far-lateral approach. Cureus. (2022) 14:e31257. doi: 10.7759/cureus.31257
4. Rennert RC, Stephens ML, Palmer AW, Rodriguez A, Kazemi N, Morris TW 3rd, et al. Basilar decompression via a far lateral transcondylar approach: technical note. Acta Neurochir (Wien). (2022) 164:2563–72. doi: 10.1007/s00701–022-05312–9
5. Budohoski KP, Barone DG, Kirollos RW, Santarius T, Trivedi RA. Far lateral approaches: far lateral approach with minimal condylectomy for C2 schwannoma: 3-dimensional operative video. Oper Neurosurg (Hagerstown). (2022) 22:e49. doi: 10.1227/ONS.0000000000000032
6. Vasquez C, Yang A, Youssef AS. Foramen magnum meningioma: far lateral approach. J Neurol Surg B Skull Base. (2019) 80:S363–4. doi: 10.1055/s-0039–1695701
7. Sai Kiran NA, Sivaraju L, Furtado SV, Vidyasagar K, Raj V, Aryan S, et al. Far lateral approach without occipital condylar resection for intradural ventral/ventrolateral foramen magnum tumors and aneurysms of V4 segment of vertebral artery: Review of surgical results. Clin Neurol Neurosurg. (2020) 197:106163. doi: 10.1016/j.clineuro.2020.106163
8. Alshafai NS, Klepinowski T. The far lateral approach to the craniovertebral junction: an update. Acta Neurochir Suppl. (2019) 125:159–64. doi: 10.1007/978–3-319–62515-7_23
9. Ali MS, Magill ST, McDermott MW. Far lateral craniotomy closure technique for preservation of suboccipital musculature. J Neurol Surg B Skull Base. (2021) 82:562–6. doi: 10.1055/s-0040–1715561
10. George B, Dematons C, Cophignon J. Lateral approach to the anterior portion of the foramen magnum. Application to surgical removal of 14 benign tumors: technical note. Surg Neurol. (1988) 29:484–90. doi: 10.1016/0090–3019(88)90145–0
11. Liu JK, Dodson VN, Meybodi AT. Far lateral transcondylar transtubercular approach for microsurgical resection of foramen magnum meningioma: operative video and technical nuances. J Neurol Surg B Skull Base. (2021) 82:S19–21. doi: 10.1055/s-0040–1716533
12. Tang K, Feng X, Yuan X, Li Y, Chen X. Volumetric comparative analysis of anatomy through far-lateral approach: surgical space and exposed tissues. Chin Neurosurg J. (2022) 8:1. doi: 10.1186/s41016–021-00268–8
13. Komatsu F, Komatsu M, Di Ieva A, Tschabitscher M. Endoscopic far-lateral approach to the posterolateral craniovertebral junction: an anatomical study. Neurosurg Rev. (2013) 36:239–47; discussion 247. doi: 10.1007/s10143-012-0433-y
14. Beucler N, Haikal C, Sellier A, May A, Meyer M, Fuentes S. Far-lateral approach for foramen magnum meningioma: an anatomical study with special reference to bulbopontine junction. Asian J Neurosurg. (2022) 17:656–60. doi: 10.1055/s-0042–1758841
15. Shiban E, Török E, Wostrack M, Meyer B, Lehmberg J. The far-lateral approach: destruction of the condyle does not necessarily result in clinically evident craniovertebral junction instability. J Neurosurg. (2016) 125:196–201. doi: 10.3171/2015.5.JNS15176
16. Moscovici S, Umansky F, Spektor S. “Lazy” far-lateral approach to the anterior foramen magnum and lower clivus. Neurosurg Focus. (2015) 38:E14. doi: 10.3171/2015.2.FOCUS14784
17. Lau T, Reintjes S, Olivera R, van Loveren HR, Agazzi S. C-shaped incision for far-lateral suboccipital approach: anatomical study and clinical correlation. J Neurol Surg B Skull Base. (2015) 76:117–21. doi: 10.1055/s-0034–1390396
18. Scoville JP, Mazur MD, Couldwell WT. Unique far-lateral closure technique: technical note. Oper Neurosurg (Hagerstown). (2020) 18:384–90. doi: 10.1093/ons/opz168
19. Dowd GC, Zeiller S, Awasthi D. Far lateral transcondylar approach: dimensional anatomy. Neurosurgery. (1999) 45:95–9; discussion 99–100. doi: 10.1097/00006123–199907000–00023
20. Bir SC, Maiti TK, Nanda A. Foramen magnum meningiomas. Handb Clin Neurol. (2020) 170:167–74. doi: 10.1016/B978–0-12–822198–3.00038–0
21. Bernardo A, Evins AI. Posterolateral routes to the skull base, craniocervical junction, and jugular foramen-the far lateral transcondylar approach and combined transpetrosal transcervical approaches. World Neurosurg. (2023) 172:163–74. doi: 10.1016/j.wneu.2022.11.053
22. Kwon SM, Na MK, Choi KS, Bang JH, Byoun HS, Han H, et al. Comparative cadaveric analysis for surgical corridor and maneuverability: far-lateral approach and its transcondylar extension. World Neurosurg. (2021) 146:e979–84. doi: 10.1016/j.wneu.2020.11.063
23. Dao I, Sanou A, Alzouma H, Bako F, Hema Y, Zabsonré SD, et al. Far lateral approach: “Trans-tumor approach” on huge dumbbell-shape neurofibroma of anterior foramen magnum without craniectomy-anatomical consideration and new trend. Acta Neurochir Suppl. (2023) 135:125–30. doi: 10.1007/978–3-031–36084-8_21
24. Gomez-Paz S, Kicielinski KP, Thomas A, Ogilvy CS. Microsurgical resection of a medullary cavernous malformation through a far lateral approach. Neurosurg Focus Video. (2019) 1:V28. doi: 10.3171/2019.7.FocusVid.19180
Keywords: incision, microsurgery, complication, far lateral approach, suboccipital triangle
Citation: Bai J, Jian Z-h, Chen P, Cheng Y, Wang Y-m, Chen G and Xiao X-r (2024) Surgical management of a foramen magnum tumor via a far-lateral approach using an oblique straight incision: a case series report and technique note. Front. Oncol. 14:1391002. doi: 10.3389/fonc.2024.1391002
Received: 24 February 2024; Accepted: 13 May 2024;
Published: 12 June 2024.
Edited by:
Alessandro Frati, Sapienza University of Rome, ItalyReviewed by:
Roberto Colasanti, Maurizio Bufalini Hospital, ItalyCopyright © 2024 Bai, Jian, Chen, Cheng, Wang, Chen and Xiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin-ru Xiao, eHJ0dHl5MjAxM0AxNjMuY29t; Gang Chen, amh5XzUwMUAxNjMuY29tQDE2My5jb20=
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.