- 1Department of General Surgery, West China Hospital, Sichuan University, Chengdu, China
- 2Breast Center, West China Hospital, Sichuan University, Chengdu, China
Background: Our center proposes a new technique that effectively provides space to broaden the surgical field of view and overcomes the limitations of endoscopy-assisted nipple-sparing mastectomy (E-NSM) by changing the dissection sequence and combining it with air inflation. The purpose of this study was to compare the clinical outcomes of the new technique designated “reverse-sequence endoscopic nipple-sparing mastectomy (R-E-NSM) with subpectoral breast reconstruction (SBR)“ and the conventional E-NSM (C-E-NSM) with SBR.
Method: All patients undergoing E-NSM with SBR at our breast center between April 2017 and December 2022 were included in this study. The cohort was divided into the C-E-NSM group and the R-E-NSM group. The operation time, anesthesia time, medical cost, complications, cosmetic outcomes, and oncological safety were compared.
Results: Twenty-six and seventy-nine consecutive patients were included in the C-E-NSM and R-E-NSM groups, with average ages of 36.9 ± 7.0 years and 39.7 ± 8.4 years (P=0.128). Patients in the R-E-NSM group had significantly shorter operation time (204.6 ± 59.2 vs. 318.9 ± 75.5 minutes, p<0.001) and anesthesia time (279.4 ± 83.9 vs. 408.9 ± 87.4 minutes, p<0.001) and decreased medical costs [5063.4 (4439.6-6532.3) vs. 6404.2 (5152.5-7981.5), USD, p=0.001] and increase SCAR-Q scores (77.2 ± 17.1 vs. 68.8 ± 8.7, P=0.002) compared to the C-E-NSM group. Although trends increased in both the excellent rate of Ueda scores (53.8% vs. 42.3%, P = 0.144), excellent rate of Harris scores (44.0% vs. 63.1%, P=0.102), and decreased surgical complications (7.6% vs. 19.2%, P = 0.135) were observed in the R-E-NSM group, the differences were not significant. There were no significant differences in oncological outcomes between the two groups.
Conclusion: R-E-NSM improves cosmetic outcomes and efficiency of C-E-NSM, reduces medical costs, and has a trend of lower surgical complications while maintaining the safety of oncology. It is a safe and feasible option for oncological procedures that deserves to be promoted and widely adopted in practice.
1 Introduction
Endoscopy-assisted nipple-sparing mastectomy (E-NSM) is a minimal access breast surgery that minimizes and hides the scar inconspicuously, thus optimizing aesthetic outcomes and patient satisfaction (1, 2). Moreover, E-NSM has also demonstrated acceptable oncological safety in some studies (3). However, E-NSM has been controversial as a treatment option, mainly because popular working space-building methods such as liposuction and/or skin lifting systems have some drawbacks (4–6). In addition, E-NSM often requires additional instruments and increases interference, operation time, surgical trauma, and medical costs (6, 7). Furthermore, the superficial nature of the breast and the relatively low morbidity of conventional open breast surgery could also be factors (8).
Surgeons at our center have also tried to conduct E-NSM using retractors to raise the pectoralis major muscle, gland, and skin. However, as in some reports, complications are increased due to uneven stress and unclear dissection layers, and the operation time is very long (9, 10). Through the sum of our experience, our team proposed an innovative technique that involves a changed dissection sequence and incorporates air-insufflation for submuscular space and gland dissection; the technique is named “reverse-sequence endoscopic nipple-sparing mastectomy (R-E-NSM).” Our previous studies have demonstrated that R-E-NSM could create sufficient space, improve dissection access, and avoid interference of instruments. For some challenging part dissection areas, such as the inner-lower quadrant, a small accessory incision (HUAXI hole 1) located at the upper-outer quadrant margin of the areola was introduced so that the final operation time was significantly shortened (11, 12). Because no particular instrument is needed and the operation time is short, this technology is widely accepted in China (13), and we even perform R-E-NSM with breast reconstruction surgeries in the 24-hour surgery center (14–17). We have also used this technology to perform breast reconstruction with endoscopic harvesting of the latissimus dorsi flap (18, 19). Up to now, we have considered R-E-NSM to address the drawbacks of conventional E-NSM (C-E-NSM) and expect it to become a standard surgical procedure. To demonstrate the superiority of the R-E-NSM technique, in this retrospective analysis study, we compared the efficiency, oncological safety, surgical safety, and cosmetic results of patients who underwent C-E-NSM with those of patients who underwent R-E-NSM, followed in each case by subpectoral breast reconstruction (SBR).
2 Method
2.1 Patients
All patients who underwent C-E-NSM and R-E-NSM followed by SBR between April 2017 and December 2022 at the Breast Center, West China Hospital, Sichuan University, by a single physician were consecutively included in this study. A research assistant prospectively collected and recorded all data for the E-NSM patient database, which was then verified by the principal investigator. This study collected data regarding demographic, clinicopathologic, surgical, and therapeutic characteristics, hospitalization time, medical cost, postoperative complications, aesthetic outcomes, recurrence, metastasis, and survival status. The study was approved by the Biomedical Ethics Committee of West China Hospital, Sichuan University (No. 2022-570). An exemption from the requirement for informed consent was granted due to the use of retrospective data. Photos and videos of several patients who consented to the release of their photographs were included in the current research.
The inclusion criteria were as follows: breast cancer in early stages, with a breast tumor less than 5 cm, cN0-1, no skin or chest infiltration, and no evidence of distant metastasis on clinical or radiographic examination. A prophylactic mastectomy was performed in women with RCA1/2 mutations, high-risk lesions such as lobular carcinoma in situ, atypical ductal hyperplasia, or women who desired a risk-reducing mastectomy after risk counseling. When the tumor involvement of the nipple-areola complex (NAC) was suspected by intraoperative sub-nipple biopsy, skin-sparing mastectomy was performed rather than NSM.
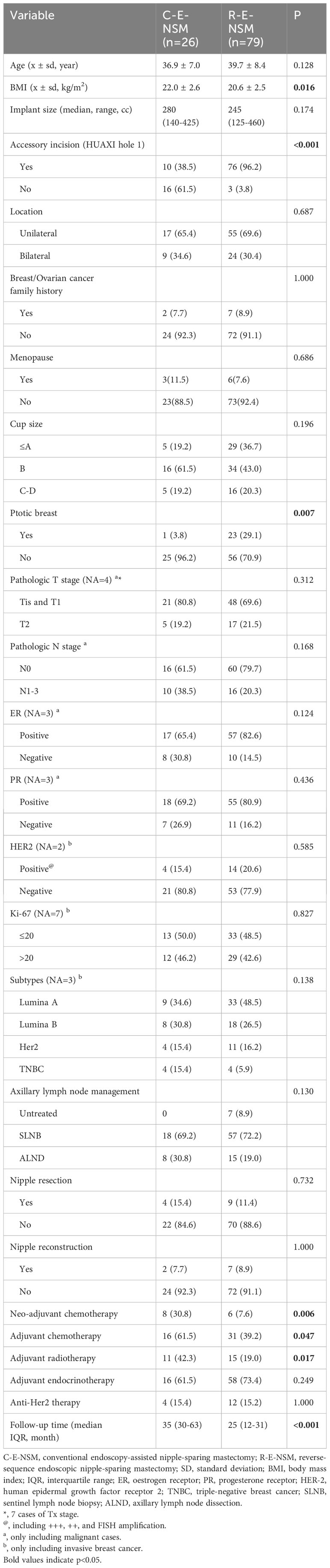
Surgery was contraindicated in patients with severe comorbidities (such as organ dysfunction and immune deficiency) and a poor general condition. We also recommend this procedure for patients with breasts small to moderate in size and mild or no ptosis because unilateral SBR is not recommended for patients with large breasts or moderate-severe ptosis. Because no patients underwent dual-plane implant-based breast reconstruction (dual-plane BR) or prepectoral implant-based breast reconstruction (PBR) in the C-E-NSM group, patients treated with dual-plane BR and PBR were also excluded for the reason that different reconstruction techniques could affect the operation time. The flow chart of participant selection is shown in Figure 1.
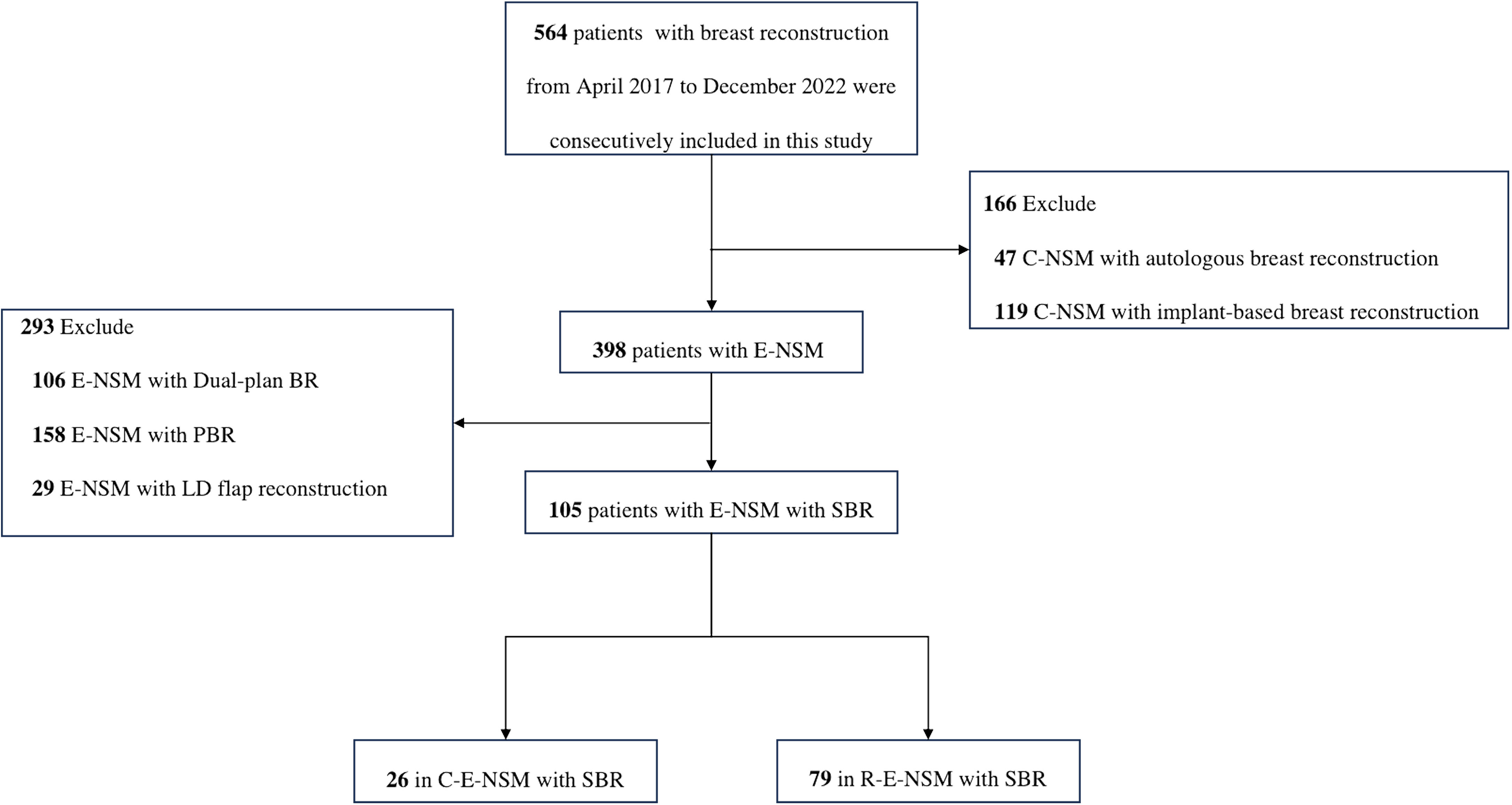
Figure 1 Flow chart of participant selection. C-NSM, conventional nipple-sparing mastectomy; E-NSM, endoscopy-assisted nipple-sparing mastectomy; Dual-plan BR, subpectoral dual-plane implant-based breast reconstruction; PBR, prepectoral implant-based breast reconstruction; LD, latissimus dorsi; SBR, subpectoral implant-based breast reconstruction; C-E-NSM, conventional endoscopy-assisted nipple-sparing mastectomy; R-E-NSM, reverse-sequence endoscopic nipple-sparing mastectomy.
2.2 C-E-NSM operation method
Incisions are made along the outer upper edge of the breast (Figures 2A–G). Under direct vision, axillary lymph node surgery is performed. The gland dissection sequence is just the same as conventional open surgery, which begins with the superficial layer of superficial fascia, followed by the pectoralis major fascia. These two layers should be dissected under direct vision as far as possible, and the endoscope should be replaced if direct vision is unclear. When the gland is removed, an intraoperative sub-nipple biopsy is taken, and the pectoralis major muscle is lifted with a retractor to build the implant envelope in the post-pectoralis major muscle space. The prosthesis is placed after flushing all layers, and the operation is complete after inserting the indwelling drainage tube and closing the incision.
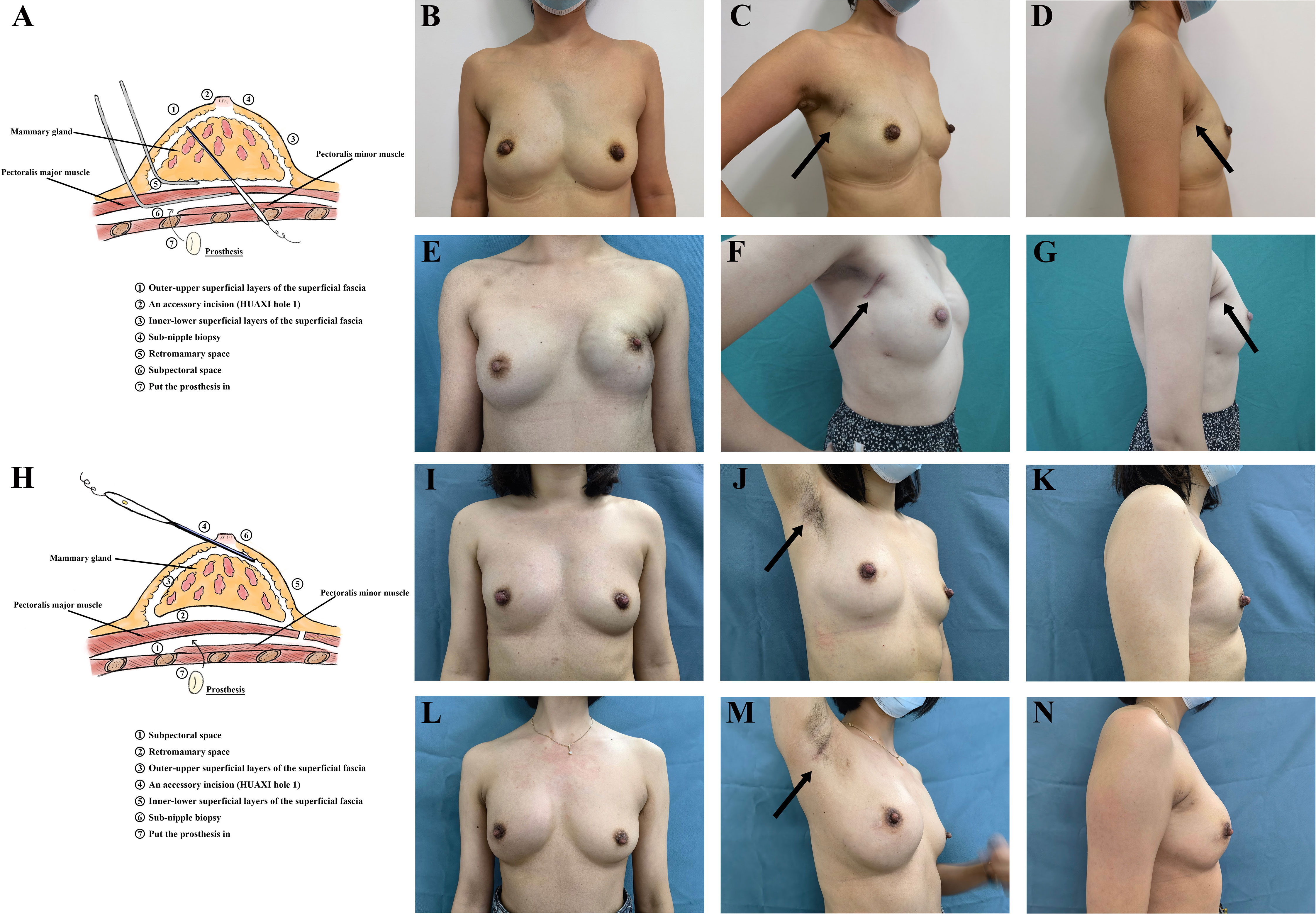
Figure 2 (A) The process of the C-E-NSM with SBR. (B–D) Photographs of a patient with right breast cancer who underwent C-E-NSM with SBR three years ago. (E–G) Photographs of a patient who received bilateral C-E-NSM with SBRs 2.5 years ago. The incision is located on the outer-upper edge of the breast, and the scar can be visible when patients stand erect and hang their arms naturally. (H) The process of the R-E-NSM with SBR. (I–N) Photographs of two patients with right breast cancers who received the C-E-NSM with SBRs 2.5 years and 2 years ago, respectively. The incision is located on the top of the axilla’s natural fold, and no scar is visible when patients stand erect and hang their arms naturally. C-E-NSM, conventional endoscopy-assisted nipple-sparing mastectomy; R-E-NSM, reverse-sequence endoscopic nipple-sparing mastectomy. SBR, subpectoral implant-based breast reconstruction.
2.3 R-E-NSM operation method
An incision is made at the top of the axilla’s natural fold (Figures 2H–N). Dissection of the axillary lymph nodes or sentinel lymph node biopsy (SLNB) is performed under direct vision. In contrast to C-E-NSM, the dissection sequence is reversed, and total endoscopic surgery is utilized. The dissection sequence begins from the subpectoral plane to build the implant envelope. By setting the air pressure to 12 mmHg and the flow rate to 40 L/mL, carbon dioxide (CO2) elevates the pectoralis major muscle and the entire breast. The subpectoral space is dissected using an electric scalpel from the parasternal line to 1cm beyond the inframammary fold marked inferiorly and to the serratus anterior fascia laterally. Then, an electric scalpel is used to dissect the entire pectoralis major fascia with the help of a grasper to pull the pectoralis major muscle downward. Next, skin flap dissection is performed, and an electric scalpel is used to carefully dissect the outer-upper, inner-upper, and outer-lower superficial layers of the superficial fascia. A 2 mm incision is made in the upper-outer margin of the areola (HUAXI hole 1), which makes it possible to remove the inner-lower part of the gland completely. Through the axillary incision, the entire gland is excised and removed. Then, a biopsy is taken from under the NAC with direct visibility for frozen sections. The prosthesis is placed after flushing all layers, and the operation is completed after the indwelling drainage tube is inserted. Full details are given in Video 1. There are some videos from different views of the camera in some articles we have published (16, 17, 20).
2.4 Outcome measures
The following outcome indicators were compared between the two groups: operation time (starting when the physician makes the first incision and ending when sutures are finished), anesthesia time, and medical cost. Surgical safety mainly included complications, which were considered “minor” if they were of Clavien-Dindo classification (C-D-C) grades I or II, and “major” if they were of C-D-C grades III or IV. The oncological safety included local recurrence and distant metastasis at the last follow-up. The patient-reported cosmetic outcomes include the Harris and SCAR-Q scores (19, 21). The appearance scale from the SCAR-Q self-report questionnaire comprises 12 questions to appraise patient satisfaction with a surgical scar when complete healing had taken place; only operative side scars were scored. Higher scores indicate a better cosmetic outcome. Regarding the doctor-reported cosmetic outcomes, three surgeons who did not participate in the surgery adopted the Ueda scoring system to evaluate preoperative and postoperative photographs (22).
2.5 Statistical analysis
The continuous variables were analyzed using the independent t-test and calculated as the mean ± standard deviation. Skewed distribution data are shown as the median and were compared with a nonparametric test. The difference in categorical variables was compared using the Chi-square or Fisher’s exact test analysis of variance. The Wilcoxon rank sum test was used for orderly classified data. Analysis of risk factors for outcome indicators by univariate and multivariate analyses and logistic regression was used to estimate ORs and 95% CIs. Statistical tests were 2-sided, and a P value less than 0.05 was considered statistically significant. All measurements and calculations were analyzed using SPSS 25.0.
3 Results
3.1 Patient demographics and characteristics
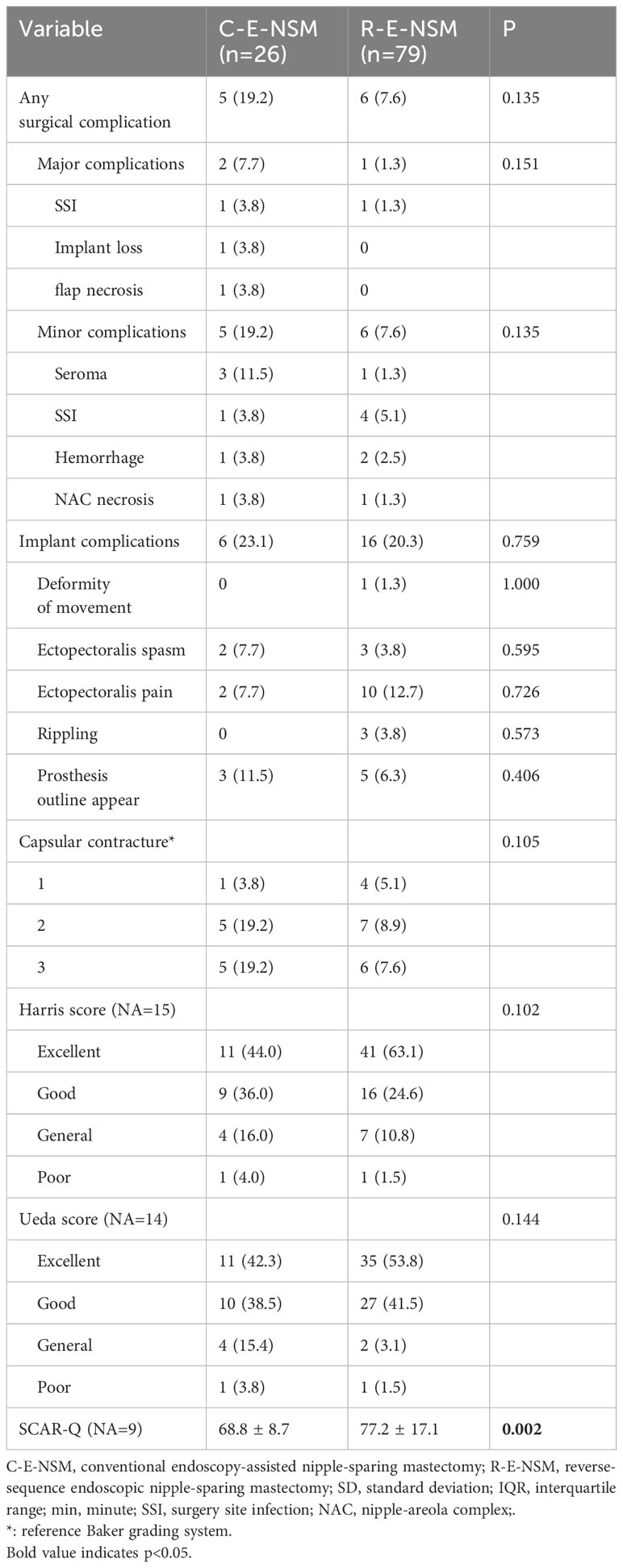
A total of 105 patients who underwent E-NSM with SBR in our breast center between April 2017 and December 2022 were consecutively included in this study. There were 26 patients whose average age was 36.9 ± 7.0 years in the C-E-NSM group and 79 patients whose average age was 39.7 ± 8.4 years in the R-E-NSM group (p=0.128). The comparison between the C-E-NSM group and the R-E-NSM group showed a statistically significant difference in BMI (p=0.016), whether to use an accessory incision (HUAXI hole 1) (p<0.001) and breast ptosis (p<0.007). More patients in the C-E-NSM group than in the R-E-NSM group received neo-adjuvant chemotherapy (p=0.006), adjuvant chemotherapy (p=0.047), and adjuvant radiotherapy (p=0.017). The median follow-up time was 35 months (range 30-63) in the C-E-NSM group and 25 months (range 12-31, p<0.001) in the R-E-NSM group, as described in Table 1.
3.2 Perioperative parameters and medical cost
A comparison of the R-E-NSM group and the C-E-NSM group showed that the operation time was reduced significantly (204.6 ± 59.2 vs. 318.9 ± 75.5 minutes, p<0.001) (Figure 3A). As a result of the shortened operation time and improved efficiency, the ratio of R-E-NSM with SBR increased, and the ratio of C-E-NSM with SBR decreased in our medical team (Figure 3B). The total number of R-E-NSM also increased significantly, despite the number of R-E-NSM with SBR procedures slightly decreased during 2021-2022 because of the great promotion of R-E-NSM with subpectoral dual-plane BR or PBR by changing surgical concepts (Figure 3C). The anesthesia time (279.4 ± 83.9 vs. 408.9 ± 87.4 minutes, p<0.001) (Figure 3D) and medical cost [5063.4(4439.6-6532.3) vs. 6404.2(5152.5-7981.5), USD, p=0.001] (Figure 3E) were also significantly reduced in the R-E-NSM group compared to C-E-NSM group.
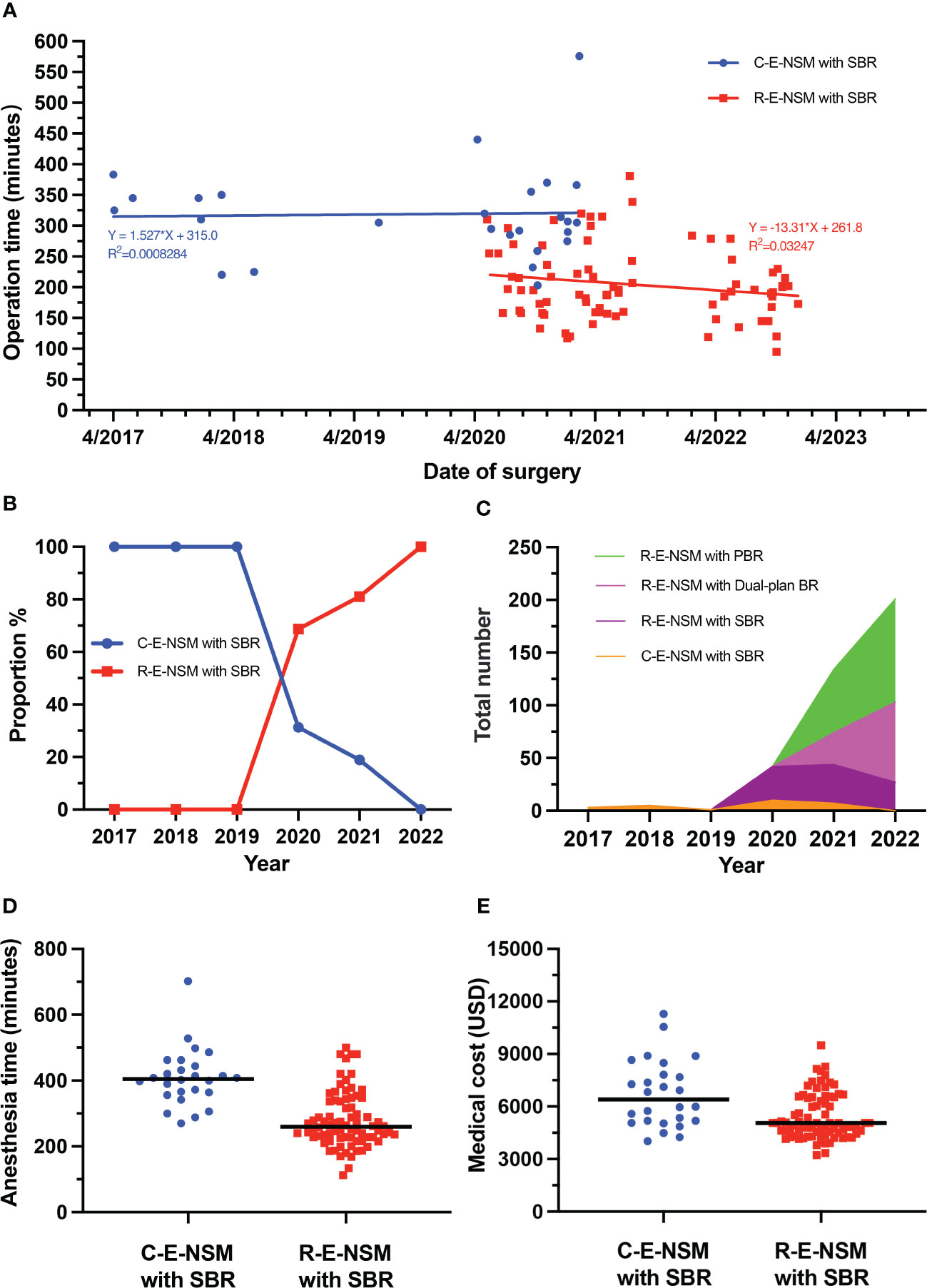
Figure 3 (A) The operation times of patients undergoing C-E-NSM and R-E-NSM with PBR, respectively, between April 2017 and December 2022. (B) The proportion between C-E-NSM and R-E-NSM from 2017 to 2022 in our medical team. (C) The total number of endoscopic nipple-sparing mastectomy followed by implant-based breast reconstruction. (D) The anesthesia times of patients undergoing C-E-NSM and R-E-NSM. (E) The medical cost of patients undergoing C-E-NSM and R-E-NSM. C-E-NSM, conventional endoscopy-assisted nipple-sparing mastectomy; R-E-NSM, reverse-sequence endoscopic nipple-sparing mastectomy; SBR, subpectoral implant-based breast reconstruction; Dual-plan BR, subpectoral dual-plane implant-based breast reconstruction; PBR, prepectoral implant-based breast reconstruction.
To adjust the bias of baseline and explore independent risk factors affecting operation time, the cohort of patients was divided into two groups based on average operation time (232 minutes) for univariate and multivariate logistic regression analysis. Factors (P < 0.1) significant on univariate analyses were subjected to multivariate logistic regression analysis, including dissection sequence, follow-up time, BMI, implant size, accessory incision (HUAXI hole 1), and unilateral or bilateral operation. The independent risk factors for the operation time are illustrated in Table 2, which were dissection sequence (OR, 0.110; 95% CI, 0.021-0.588, p=0.010) and location (OR, 13.73; 95% CI, 3.891-48.463, P <0.001).
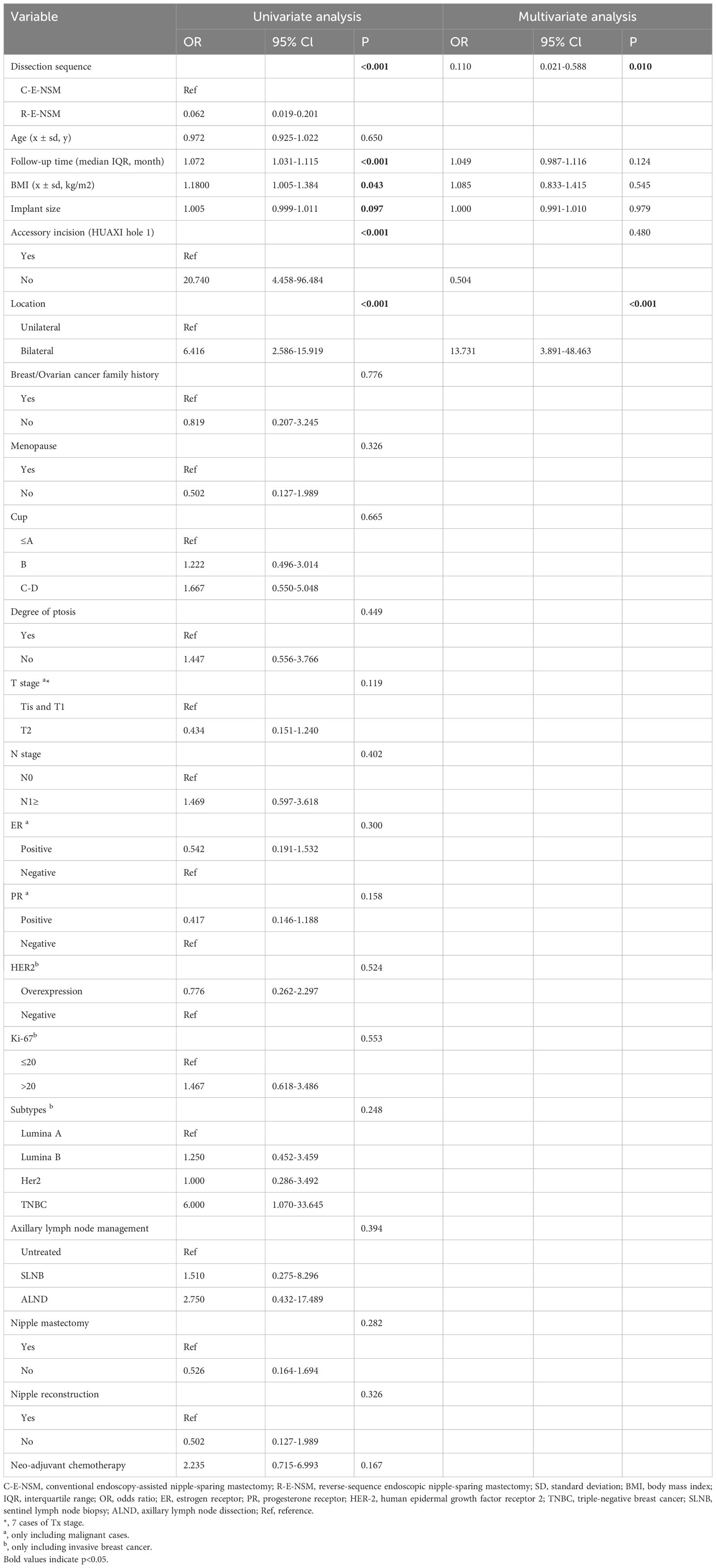
Table 2 Univariate and multivariate analysis of the parameters resulting in operation times longer than the average time (232 minutes).
3.3 Complications and oncological outcomes
In comparing the C-E-NSM and R-E-NSM groups, there were no significant differences in terms of surgical complications (19.2% vs. 7.6%, p=0.135), major complications (7.7% vs. 1.3%, p=0.151), minor complications (19.2% vs. 7.6%, p=0.135), and implant-related complications (23.1% vs. 20.3%, p=0.759) (Table 3). There were no implant loss or flap necrosis cases in the R-E-NSM group. According to univariate analyses of any complications, two factors showed a p <0.1, and multivariate analyses indicated that the follow-up time was the only independent risk factor for any complication (OR,1.015; 95% CI, 1.015-1.095; P = 0.007) (Table 4). There was one local recurrence and two distant metastasis cases in the C-E-NSM group. In contrast, there were no local recurrence or distant metastasis cases in the R-E-NSM group. A two-year disease-free survival (DFS) rate of 96.2% and 100% was observed in the C-E-NSM and R-E-NSM groups, respectively (P=0.248).
3.4 Aesthetic outcomes
Postoperative aesthetic outcome questionnaires included doctor-reported outcomes (Ueda scale) and patient-reported outcomes (Harris scale and SCAR-Q). Ninety patients completed the questionnaires for the Harris scale, 91 patients completed the questionnaires for the Ueda scale, and 96 patients completed the questionnaires for SCAR-Q. When comparing the C-ENS and R-ENS groups, there was no significant difference in Harris scores (P=0.102) and Ueda scores reported by doctors (P=0.144). However, the mean SCAR-Q score showed a significant difference (68.8 ± 8.7 vs. 77.2 ± 17.1, P=0.002) between the two groups.
4 Discussion
This study presents a groundbreaking comparison of two breast cancer surgical procedures, C-E-NSM with SBR and innovation technique R-E-NSM with SBR, in terms of efficiency, safety, and economic results at the first time. The results showed that R-E-NSM outperformed C-E-NSM regarding operation time, anesthesia time, and cost. Moreover, it improved patient satisfaction with the appearance of their scars and revealed a decreasing trend in the incidence of complications. These findings confirm that R-E-NSM is a highly efficient and recommended new surgical procedure that breaks conventional methods. Therefore, R-E-NSM is a promising new surgical procedure that has the potential to revolutionize breast cancer surgery. Given its further development, R-E-NSM is now suitable for a broader range of operations, including subpectoral dual-plane BR, PBR, latissimus dorsi (LD) flap reconstruction, and gynecomastia mastectomy (15, 23, 24).
The operation time was reduced by approximately 2 hours in the R-E-NSM group, and the medical cost and anesthesia time were also reduced compared to C-E-NSM. C-E-NSM increases the difficulty of optimal exposure, such as lifting the pectoralis major muscles, glands, and skin. You cannot have your cake and eat it, too. When the skin-lifting method is chosen, the glands and pectoralis major muscle need to be raised with a retractor and some specific equipment, resulting in poor exposure and difficult dissection of the deep layer. When the air-insufflation method is chosen, using CO2 exposure is beneficial, but lifting the pectoralis major muscle and the gland with this method is difficult. Therefore, the process of C-E-NSM with SBR will take longer, approximately 5 hours (10, 25).
In contrast, R-E-NSM can resolve the above issue and reduce the operation time using a reverse dissection sequence and CO2 insufflation. Now you can have your cake and eat it too. With CO2 insufflation, the field of vision is clearly exposed, and with CO2 simultaneously just as a universal retractor, the pectoralis major muscle, gland, and skin are lifted easily. An accessory incision (HUAXI hole 1) can also be combined with R-E-NSM to dissect the inner-lower part of the superficial layers of the superficial fascia and prevent equipment interference. The follow-up time was also the reason for the operation time decrease by univariate analyses. We know that the follow-up time reflects the learning curve. As time passes, the surgeon becomes more proficient and experienced. Currently, we only need 60-90 minutes for R-E-NSM with SBR and approximately 60-75 minutes for R-E-NSM with PBR.
Regarding cosmetic outcomes, the SCAR-Q appearance scale is used to evaluate patient satisfaction after developing a surgical scar. Higher scores indicate a better cosmetic outcome. In the R-E-NSM group, the SCAR-Q score was higher, and it was speculated that the reason was that scarring would be more subtle and concealed under the axillary area. There is an axillary incision with a length of approximately 50 mm, combined with a “HUAXI hole 1”, which has a size of 2 mm. Scarring around the breasts is barely noticeable when patients stand erect and hang their arms naturally. From C-E-NSM (10, 26), the incision was mainly placed on the lateral upper side of the breast. Because of a gasless technique and retractor, the incision cannot be close to the top of the axilla. The incision was extended to 5-8 cm to remove the mammary gland and axillary tissue. As a result, scars cannot be concealed completely. The Harris score and Ueda score were more associated with the appearance of breasts which are reported by patients and doctors, respectively. Because the operation method for all patients was subpectoral implant-based breast reconstruction, there was no significant difference in the appearance of the breasts. However, we can also notice a trend from the result that the cosmetic outcomes with R-E-NSM and SBR were better than those with C-E-NSM and SBR.
This study also showed a downward trend of complications in R-E-NSM. Follow-up time was the only independent factor of any surgical complications after multivariate analysis. Therefore, the decreasing trend of complications is not caused by different surgical methods but due to the shorter follow-up time of R-E-NSM and the improvement of surgical proficiency. However, the current complication rate is 7.6% in the R-E-NSM group; with the progress of surgical skill proficiency, the incidence of complications in the R-E-NSM group may be further reduced. Following E-NSM, flap necrosis and NAC necrosis are common complications. However, in this study, there were reports of no cases of flap necrosis in R-E-NSM, and necrosis of the NAC in the R-E-NSM group was lower than that in the C-E-NSM group (1.3% vs. 3.8%), as reported in other studies and even lower than other studies (27–30). Tissue necrosis is associated with damage to blood vessels and enlarged incisions during the operation, and periareolar incisions were identified as predictors of NAC necrosis (29, 31). However, in the R-E-NSM group, gas can evenly expand tissue and expose it well, reducing the damage to surrounding tissues and blood vessels and combining minimal peri-areola accessory incision (HUAXI hole 1), thereby decreasing necrosis complications. Furthermore, a long operation time is a risk factor for surgery site infection (SSI) (32, 33), so reducing the operation time could reduce the probability of SSI. All of the above are reasons for the trend of decreased complication rate after R-E-NSM compared with C-E-NSM.
Oncological safety is a major concern in the treatment of breast cancer. The endoscopic procedures in this study followed the same steps and principles as conventional nipple-sparing mastectomy (C-NSM). Therefore, we speculate that the oncological results of the two techniques may be similar (34). By a median follow-up time of 35 months, the locoregional recurrence rate was 3.8%, the distant metastasis rate was 7.7%, and no patients in the C-E-NSM group experienced mortality. By a median follow-up time of 25 months, there was no report of local recurrence or distant metastasis from patients in the R-E-NSM group. The two-year DFS rate was 96.2% in the C-E-NSM group and 100% in the R-E-NSM group, which is consistent with several studies of C-NSM (35, 36). However, the rate of local recurrence within two years in the R-E-NSM group was lower than that in the C-E-NSM group, although there was no significant difference. In addition to the small sample size due to accidental factors, it has been suggested that insufficient exposure of the retractor, uneven resection, and residual tumor may contribute to the risk of local recurrence in C-E-NSM. The R-E-NSM dissection is even and ranges wider, making it a potentially safer procedure. These results indicate that the oncologic safety of R-E-NSM is acceptable, though the recurrence and survival outcomes are still pending.
R-E-NSM significantly reduced operation time, anesthesia time, and medical cost and showed a downward trend of complications. In particular, patients and doctors in China widely accept R-E-NSM with subpectoral dual-plane BR and PBR to reduce trauma, shorten surgical time, and expand the indication population. These even make R-E-NSM with implant-based breast reconstruction has been successfully performed in the 24-hour surgical center of our hospital. Nevertheless, as a retrospective study, the investigation involved a limited number of cases and was based on the expertise of a single physician and center, resulting in a bias in patient selection, insufficient representation of the general population, and insufficient samples. It is recommended that further prospective cohort studies or randomized controlled trials be conducted.
5 Conclusion
In summary, R-E-NSM improves cosmetic outcomes and efficiency of C-E-NSM, reduces medical costs, and has a trend of lower surgical complications while maintaining the safety of oncology. It is a safe and feasible option for oncological procedures that deserves to be promoted and widely adopted in practice.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The study was approved by the Biomedical Ethics Committee of West China Hospital, Sichuan University (No. 2022-570). An exemption from the requirement for informed consent was granted due to the use of retrospective data.
Author contributions
KC: Writing – original draft, Data curation, Formal analysis, Methodology, Writing – review & editing. YX: Data curation, Writing – review & editing. FL: Data curation, Formal analysis, Supervision, Writing – review & editing. MQ: Data curation, Writing – review & editing. HY: Data curation, Writing – review & editing. QZ: Data curation, Writing – review & editing. HD: Data curation, Writing – review & editing. ZD: Supervision, Writing – review & editing, Project administration.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by grants from the Key Projects of the Sichuan Provincial Health Commission (21PJ042), the Incubation Project of West China Hospital of Sichuan University (2022HXFH004), and the Natural Science Foundation of Sichuan Province (22NSFSC2361).
Acknowledgments
We would like to thank all of our patients and researchers for participating in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2024.1366877/full#supplementary-material
References
1. Shin H. Current trends in and indications for endoscopy-assisted breast surgery for breast cancer. Adv Exp Med Biol. (2021) 1187:567–90. doi: 10.1007/978-981-32-9620-6_30
2. Lai HW, Chen ST, Tai CM, Lin SL, Lin YJ, Huang RH, et al. Robotic- versus endoscopic-assisted nipple-sparing mastectomy with immediate prosthesis breast reconstruction in the management of breast cancer: A case-control comparison study with analysis of clinical outcomes, learning curve, patient-reported aesthetic results, and medical cost. Ann Surg Oncol. (2020) 27:2255–68. doi: 10.1245/s10434-020-08223-0
3. Sakamoto N, Fukuma E, Higa K, Ozaki S, Sakamoto M, Abe S, et al. Early results of an endoscopic nipple-sparing mastectomy for breast cancer. Ann Surg Oncol. (2009) 16:3406–13. doi: 10.1245/s10434-009-0661-8
4. Shi F, Huang Z, Yu J, Zhang P, Deng J, Zou L, et al. Immediate liposuction could shorten the time for endoscopic axillary lymphadenectomy in breast cancer patients. World J Surg Oncol. (2017) 15:35. doi: 10.1186/s12957-017-1106-7
5. Wu QF, Yu YH, Zhu X, Cui Y, Mo QG, Wei CY, et al. Development of video-assisted breast cancer surgery: Initial experience with a novel method for creating working space without prior liposuction. Mol Clin Oncol. (2017) 7:32–8. doi: 10.3892/mco.2017.1279
6. Wang Y, Wu JX, Guan S. A technique of endoscopic nipple-sparing mastectomy for breast cancer. JSLS: J Soc Laparoendoscopic Surg. (2017) 21(2). doi: 10.4293/jsls.2017.00028
7. Margenthaler JA. Robotic mastectomy-program malfunction? JAMA Surg. (2020) 155:461–2. doi: 10.1001/jamasurg.2019.6361
8. Ingram D. Is it time for breast cancer surgeons to embrace endoscopic-assisted mastectomy? ANZ J Surg. (2008) 78:837–8. doi: 10.1111/j.1445-2197.2008.04676.x
9. Chanoit G, Pell CA, Bolotin G, Buckner GD, Williams JP, Crenshaw HC. Retraction mechanics of Finochietto-style self-retaining thoracic retractors. BioMed Eng Online. (2019) 18:45. doi: 10.1186/s12938-019-0664-z
10. Du J, Liang Q, Qi X, Ming J, Liu J, Zhong L, et al. Endoscopic nipple sparing mastectomy with immediate implant-based reconstruction versus breast conserving surgery: a long-term study. Sci Rep. (2017) 7:45636. doi: 10.1038/srep45636
11. Zhang S, Xie Y, Liang F, Wang Y, Lv Q, Du Z. Endoscopic-assisted nipple-sparing mastectomy with direct-to-implant subpectoral breast reconstruction in the management of breast cancer. Plast Reconstr Surg Glob Open. (2021) 9:e3978. doi: 10.1097/gox.0000000000003978
12. Zhang S, Xie Y, Liang F, Wang Y, Wen N, Zhou J, et al. Video-assisted transaxillary nipple-sparing mastectomy and immediate implant-based breast reconstruction: A novel and promising method. Aesthetic Plast Surg. (2022) 46:91–8. doi: 10.1007/s00266-021-02527-6
13. Yang H, Liang F, Xie Y, Qiu M, Du Z. Single axillary incision reverse-order endoscopic nipple/skin-sparing mastectomy followed by subpectoral implant-based breast reconstruction: Technique, clinical outcomes, and aesthetic results from 88 preliminary procedures. Surgery. (2023) 174:464–72. doi: 10.1016/j.surg.2023.05.037
14. Zhou J, Liu X, Feng Y, Li J, Qin X, Huang Y, et al. Breakthrough in breast reconstruction in the context of COVID-19: safety and efficiency of endoscopic breast reconstruction at a day surgery center. Gland Surg. (2021) 10:2477–89. doi: 10.21037/gs-21-405
15. Qiu M, Yang H, Zhou J, Feng Y, Liu X, Zhang Q, et al. Short-term safety and cosmetic outcomes of endoscopic direct-to-implant breast reconstruction and simultaneous contralateral breast augmentation for breast cancer: a prospective analysis of 33 patients. World J Surg Oncol. (2023) 21:201. doi: 10.1186/s12957-023-03089-4
16. Jiao Z, Xie Y, Liang F, Feng Y, Yang H, Qiu M, et al. A novel technique of reverse-sequence endoscopic nipple-sparing mastectomy with direct-to-implant breast reconstruction: medium-term oncological safety outcomes and feasibility of 24-hour discharge for breast cancer patients. Int J Surgery. (2024) 10:1097. doi: 10.1097/js9.0000000000001134
17. Feng Y, Xie Y, Liang F, Zhou J, Yang H, Qiu M, et al. Twenty-four-hour discharge of patients after endoscopic nipple-sparing mastectomy and direct-to-implant breast reconstruction: safety and aesthetic outcomes from a prospective cohort study. Br J Surg. (2023) 111(1):znad356. doi: 10.1093/bjs/znad356
18. Qiu J, Wen N, Xie Y, Feng Y, Liang F, Lv Q, et al. Novel technique for endoscopic-assisted nipple-sparing mastectomy and immediate breast reconstruction with endoscopic-assisted latissimus dorsi muscle flap harvest through a single axillary incision: a retrospective cohort study of comparing endoscopic and open surgery. Gland Surg. (2022) 11:1383–94. doi: 10.21037/gs-22-398
19. Feng Y, Wen N, Liang F, Zhou J, Qin X, Liu X, et al. Endoscopic nipple- or skin-sparing mastectomy and immediate breast reconstruction with endoscopic harvesting of the latissimus dorsi flap: A preliminary experience of an innovative technique. Breast J. (2022) 2022:1373899. doi: 10.1155/2022/1373899
20. Qiu M, Liang F, Xie Y, Yang H, Zhang Q, Zhong J, et al. Clinical outcomes of transaxillary reverse-sequence endoscopic nipple-sparing mastectomy and direct-to-implant prepectoral breast reconstruction: A prospective study of initial 68 procedures. Ann Surg Oncol. (2024), 1–9. doi: 10.1245/s10434-023-14687-7
21. Fitzal F, Krois W, Trischler H, Wutzel L, Riedl O, Kühbelböck U, et al. The use of a breast symmetry index for objective evaluation of breast cosmesis. Breast. (2007) 16:429–35. doi: 10.1016/j.breast.2007.01.013
22. Ueda S, Tamaki Y, Yano K, Okishiro N, Yanagisawa T, Imasato M, et al. Cosmetic outcome and patient satisfaction after skin-sparing mastectomy for breast cancer with immediate reconstruction of the breast. Surgery. (2008) 143:414–25. doi: 10.1016/j.surg.2007.10.006
23. Yang Y, Mu D, Xu B, Li W, Zhang X, Lin Y, et al. Endoscopic subcutaneous mastectomy plus liposuction via a single axillary incision for gynecomastia in Asian patients: A report of 45 cases. Surgery. (2021) 170:39–46. doi: 10.1016/j.surg.2021.01.046
24. Chang HP, Fan KL, Song SY, Lee DW. The traditional versus endoscopic-assisted latissimus dorsi harvest in oncoplastic surgery: A long term comparison of breast volume, aesthetics, and donor site outcomes. Asian J Surg. (2020) 43:1165–71. doi: 10.1016/j.asjsur.2020.03.002
25. Ryu JM, Lee J, Lee J, Ko B, Kim JH, Shin H, et al. Mastectomy with Reconstruction Including Robotic Endoscopic Surgery (MARRES): a prospective cohort study of the Korea Robot-Endoscopy Minimal Access Breast Surgery Study Group (KoREa-BSG) and Korean Breast Cancer Study Group (KBCSG). BMC Cancer. (2023) 23:571. doi: 10.1186/s12885-023-10978-0
26. Zhu L, Li S, Tan L, Zhang X, Wu J, Su F, et al. In pursuit of a flawless aphrodite: paving the way to scarless oncoplastic breast surgery. Cancer Commun (Lond). (2019) 39:82. doi: 10.1186/s40880-019-0422-4
27. Mallon P, Feron JG, Couturaud B, Fitoussi A, Lemasurier P, Guihard T, et al. The role of nipple-sparing mastectomy in breast cancer: a comprehensive review of the literature. Plast Reconstr Surg. (2013) 131:969–84. doi: 10.1097/PRS.0b013e3182865a3c
28. Lai HW, Chen ST, Lin YJ, Lin SL, Lin CM, Chen DR, et al. Minimal access (Endoscopic and robotic) breast surgery in the surgical treatment of early breast cancer-trend and clinical outcome from a single-surgeon experience over 10 years. Front Oncol. (2021) 11:739144. doi: 10.3389/fonc.2021.739144
29. Jimenez RB, Packowski K, Horick N, Rosado N, Chinta S, Koh DJ, et al. The timing of acute and late complications following mastectomy and implant-based reconstruction. Ann Surg. (2023) 278:e203–e8. doi: 10.1097/sla.0000000000005574
30. Gentile P, Bernini M, Orzalesi L, Sordi S, Meattini I, Lessi F, et al. Titanium-coated polypropylene mesh as innovative bioactive material in conservatives mastectomies and pre-pectoral breast reconstruction. Bioact Mater. (2021) 6:4640–53. doi: 10.1016/j.bioactmat.2021.05.002
31. Lai HW, Lee YY, Chen ST, Liao CY, Tsai TL, Chen DR, et al. Nipple-areolar complex (NAC) or skin flap ischemia necrosis post nipple-sparing mastectomy (NSM)-analysis of clinicopathologic factors and breast magnetic resonance imaging (MRI) features. World J Surg Oncol. (2023) 21:23. doi: 10.1186/s12957-023-02898-x
32. Wattoo G, Nayak S, Khan S, Morgan J, Hocking H, MacInnes E, et al. Long-term outcomes of latissimus dorsi flap breast reconstructions: a single-centre observational cohort study with up to 12 years of follow up. J Plastic Reconstructive Aesthetic Surgery. (2021) 74:2202–9. doi: 10.1016/j.bjps.2020.12.058
33. Alkaaki A, Al-Radi OO, Khoja A, Alnawawi A, Alnawawi A, Maghrabi A, et al. Surgical site infection following abdominal surgery: a prospective cohort study. Can J surgery. (2019) 62:111. doi: 10.1503/cjs.004818
34. Wan A, Liang Y, Chen L, Wang S, Shi Q, Yan W, et al. Association of long-term oncologic prognosis with minimal access breast surgery vs conventional breast surgery. JAMA Surg. (2022) 157:e224711. doi: 10.1001/jamasurg.2022.4711
35. Lai H-W, Chang Y-L, Chandrachamnong K, See M-H, Huang H-I, Lin S-L, et al. Factors associated with alteration of nipple or skin sensation and impact of duration of time following nipple-sparing mastectomy (NSM): an analysis of 460 cases with comparison of conventional versus endoscopic- or robotic-assisted NSM. World J Surg Oncol. (2023) 21:222. doi: 10.1186/s12957-023-03107-5
36. Lai HW, Chen ST, Mok CW, Lin YJ, Wu HK, Lin SL, et al. Robotic versus conventional nipple sparing mastectomy and immediate gel implant breast reconstruction in the management of breast cancer- A case control comparison study with analysis of clinical outcome, medical cost, and patient-reported cosmetic results. J Plast Reconstr Aesthet Surg. (2020) 73:1514–25. doi: 10.1016/j.bjps.2020.02.021
Keywords: C-E-NSM, R-E-NSM, operation time, complication, HUAXI hole 1
Citation: Chung K, Xie Y, Liang F, Qiu M, Yang H, Zhang Q, Dai H and Du Z (2024) Reverse-sequence endoscopic nipple-sparing mastectomy with immediate implant-based breast reconstruction: an improvement of conventional minimal access breast surgery. Front. Oncol. 14:1366877. doi: 10.3389/fonc.2024.1366877
Received: 07 January 2024; Accepted: 22 February 2024;
Published: 06 March 2024.
Edited by:
Haiyan Li, The Sixth Affiliated Hospital of Sun Yat-sen University, ChinaReviewed by:
Matteo Ghilli, Pisana University Hospital, ItalySi-Qi Qiu, Shantou Central Hospital, China
Copyright © 2024 Chung, Xie, Liang, Qiu, Yang, Zhang, Dai and Du. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhenggui Du, ZG9jZHV6Z0AxNjMuY29t
†These authors have contributed equally to this work and share first authorship
 Kawun Chung
Kawun Chung Yanyan Xie1,2†
Yanyan Xie1,2† Faqing Liang
Faqing Liang Huanzuo Yang
Huanzuo Yang Zhenggui Du
Zhenggui Du