
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Oncol., 04 June 2024
Sec. Surgical Oncology
Volume 14 - 2024 | https://doi.org/10.3389/fonc.2024.1337870
Background and objectives: Anastomotic leakage (AL) is one of the most serious complications after laparoscopic anus-preserving surgery for rectal cancer, which significantly prolongs the patient’s hospital stay, leads to dysfunction, and even increases the patient’s perioperative morbidity and mortality, and little is known about the effectiveness of anastomotic reinforcement sutures to prevent AL. Thus, this study was conducted to evaluate the efficacy of anastomotic reinforcement sutures as a means to prevent AL during laparoscopic surgery for rectal cancer.
Methods: A comprehensive and systematic search was performed in the literature database by combining subject and free terms up to 10 October 2023. The overall literature included was integrated and analyzed using Stata 12.0 software and Review Manager version 5.4 software to assess the effect of anastomotic reinforcement sutures on the incidence of AL.
Results: A total of 2,452 patients from 14 studies were included, and an integrated analysis showed that the use of anastomotic reinforcement sutures significantly reduced the incidence of AL [odds ratio (OR) = 0.26; 95% confidence interval (CI), 0.18–0.37; P < 0.00001; I2 = 0%]. However, the findings confirmed whether or not the anastomosis reinforced with sutures did not affect the incidence of anastomotic stenosis (OR = 0.69; 95% CI, 0.37–1.32; P = 0.27; I2 = 0%). We performed subgroup analyses of the results of the study, the randomized controlled studies (OR = 0.31; 95% CI, 0.15–0.65; P < 0.001) as well as retrospective studies (OR = 0.28; 95% CI, 0.19–0.41; P < 0.001), 3–0 sutures (OR = 0.28; 95% CI, 0.17–0.45; P < 0.001) versus 4–0 sutures (OR = 0.26; 95% CI, 0.13–0.53; P < 0.001), barbed wire sutures (OR = 0.26; 95% CI, 0.14–0.48; P < 0.001) versus non-barbed wire sutures (OR = 0.30; 95% CI, 0.20–0.46; P < 0.001), interrupted (OR = 0.30, 95% CI, 0.20–0.46; P < 0.001) versus continuous sutures (OR = 0.29, 95% CI, 0.16–0.51; P < 0.001) to the anastomosis, full-thickness suture (OR = 0.29; 95% CI, 0.16–0.51; P < 0.001) versus sutured with the seromuscular layer (OR = 0.27; 95% CI, 0.14–0.53; P < 0.001), anastomotic sutured in one (OR = 0.27; 95% CI, 0.14–0.53; P < 0.001) versus non-one circle (OR = 0.30; 95% CI, 0.20–0.44; P < 0.001), and reinforcing sutures to the dog-ear area (OR = 0.26; 95% CI, 0.14–0.50; P < 0.001) versus the non–dog-ear area (OR = 0.30; 95% CI, 0.20–0.45; P < 0.001), which have suggested that there is no significant difference between each other and that all of them reduce the incidence of AL.
Conclusions: This study provides evidence that performing reinforcement suturing of the anastomosis during laparoscopic rectal surgery significantly lowers the incidence of postoperative AL but has no significant effect on anastomotic stenosis. It is important to note that further randomized controlled studies are required to confirm this conclusion.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, identifier CRD42022368631.
Anastomotic leakage (AL) is the most serious complication of laparoscopic surgery for rectal cancer with a high mortality rate (1). In recent years, with the continuous improvement of the stapler and manual suturing techniques, preoperative evaluation of patients, and surgical techniques for rectal anastomosis, the incidence of AL still falls within the range of 2.8%–30%. Out of these cases, 75% occurs in rectal anastomosis, resulting in a mortality rate of 2%–16.4% and a morbidity rate of 20%–35% (2–4).
It has been shown that the risk factors for the occurrence of anastomotic leaks are closely related to the level of anastomosis, anastomotic blood supply, anastomotic tension, anastomotic technique, and the degree of anastomotic reinforcement (5, 6). Previous studies have reported that, in laparoscopic anterior rectal resection, the straight line formed by the linear cutting closure to dissect the rectum and the circular line of the tubular anastomosis inevitably form two intersecting corners (“dog-ear zone”). This brings about a high incidence of AL due to the structural weakness and lack of blood supply of the intersecting part of the pegs and is susceptible to inflammation and edema (7, 8). Therefore, surgeons tend to reinforce the anastomotic site, especially the “dog-ear” area, to minimize postoperative AL. However, there is still some controversy regarding the effectiveness of anastomotic reinforcement sutures in improving AL. Placer et al. (9), in a prospective randomized controlled study, showed that bioabsorbable suture reinforcement of colorectal anastomoses more than 5 cm away from the anal verge did not reduce the incidence of anastomotic complications (i.e., leakage, bleeding, or stenosis). Similarly, Senagore et al. (10) have concluded that reinforcement of colorectal anastomoses with bioabsorbable material did not affect the incidence of anastomotic leaks but may reduce anastomotic strictures. However, Lin et al. (11), in a study of anastomotic reinforcement with barbed sutures during laparoscopic low anterior resection of rectal cancer, found that the incidence of AL was 10% in the control group and 2.82% in the suture-reinforced group, suggesting that reinforcement of the anastomotic “dog’s ear” area with sutures is associated with a low incidence of AL. Similarly, Ban et al. (12) have demonstrated that reinforcement of the anastomosis with barbed sutures after laparoscopic rectal cancer resection significantly reduced the incidence of AL. Several retrospective clinical studies have confirmed that reinforcement suturing of the anastomosis reduces the incidence of AL. However, to date, few studies have compared the efficacy assessment of patients who underwent anastomotic reinforcement with those who did not. There is still some controversy as to whether anastomotic reinforcement suturing reduces the incidence of AL.
Our study aimed to evaluate if reinforcing anastomotic sutures during laparoscopic rectal resection reduces the incidence of AL. In this study, we analyzed the clinical studies published in recent years on reinforced versus unreinforced sutures in laparoscopic surgery for rectal resection. Moreover, this study provides guidance and evidence-based medicine for the prevention of AL in laparoscopic surgery for rectal resection.
This pooled analysis was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidance (13). The study protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO registration number: CRD42022368631).
Literature searches were conducted by two independent authors in PubMed, Embase, Cochrane Library, Web of Knowledge, and Clinical Trials.gov databases for medical subject terms and free words. From the time of database inception until 20 October 2023, the last database search was updated on 10 November 2022. There were no language restrictions. The search terms that we used were as follows: laparoscopic surgery for rectal cancer, anastomosis, AL, and reinforcement. The search strategy on PubMed is as follows: (Anastomotic) AND (((laparoscopic surgery) AND (rectal)) AND (Reinforcement)).
The clinical studies included in this integrative analysis met the following criteria: (1) All patients included in the study were required to undergo laparoscopic rectal resection. (2) The intervention group used reinforcing sutures to close the anastomosis without limiting the type of reinforcing sutures and the method of reinforcing sutures, and the control group did not use reinforcing sutures.
Exclusion criteria are as follows: single-arm clinical studies, observational studies, abstracts, as well as reviews.
Two researchers individually screened the titles or abstracts of the retrieved literature and, when necessary, the full text of the articles. They also reviewed the included literature with each other for accuracy and completeness of data, and a third researcher participated in or jointly discussed any disagreements that arose during the process. When an article does not contain information on a specific endpoint, an attempt was made to contact the authors to clarify details and/or request missing outcome data.
The primary endpoint was the occurrence of AL and the secondary endpoint was the occurrence of anastomotic stenosis.
Two investigators independently assessed the risk of bias using the latest version of the Cochrane Collaboration tool to guide the assessment of randomized controlled studies (14). The quality of the literature was rated as low, high, or unclear, and the results of the risk of bias assessment were used only to describe the quality of the literature and were not used as criteria for study selection. The quality of retrospective studies was assessed using the Newcastle-Ottawa scale (NOS) (15), which includes mainly the selection of study subjects, comparability between groups, and outcome or exposure assessment. A full score of 9 was assigned, where 1–3 was considered as low quality, 4–6 as moderate quality, and 7–9 as high quality.
Endpoints were expressed as odds ratios (OR) for dichotomous data and with 95% confidence interval (CI). Heterogeneity between studies was assessed with the I² statistic; when I² = 0, there was no heterogeneity; the larger the I² statistic, the greater the heterogeneity (I² < 25%, 25%–50%, and >50% indicate low, moderate, and high heterogeneity, respectively), and if I² > 50% indicates the presence of more pronounced heterogeneity, then the analysis was performed using a random-effects model, and vice versa, using a fixed-effects model. When heterogeneity was found in the main results, a separate sensitivity analysis was performed to find potential sources of heterogeneity. We used the software RevMan 5.4 and Stata 12.0 to perform statistical analyses. In addition, publication bias was assessed using funnel plots. The only way to control for publication bias is to collect as comprehensively as possible all studies that meet the inclusion criteria.
A subgroup analysis of the effect of AL was performed by the type of study in the literature (retrospective and randomized controlled studies), 3–0 versus 4–0 suture, barbed versus non-barbed suture, interrupted versus continuous suture, full-thickness versus seromuscular suture, one-circle versus non–one-circle suture, and closure of the dog’s ear versus non-dog’s ear.
Based on the search strategy, 193 relevant studies were initially identified. After removing 90 duplicates, a total of 103 potential studies were included. Sixty-two studies were excluded in the title and abstract screening, and 41 studies were considered eligible for full-text assessment. In addition, 27 full-text were excluded, 19 studies were excluded because they were single-arm studies, and eight studies did not provide data information because they were clinical guidelines. Fourteen studies met the inclusion criteria for this analysis (12 retrospective studies (11, 12, 16–25) versus two randomized controlled studies (26, 27)). A total of 14 studies (11, 12, 16–27) with 2,452 patients (reinforced suture group, n = 1196, and non-reinforced suture group, n = 1,256) were included. All patients included in the study underwent rectal resection. The flow chart of this study is shown in Figure 1.
Tables 1, 2 incorporate study details from 14 studies, which include patient demographics, procedure-related details, postoperative complications, and the type of suture used during anastomotic reinforcement suturing.
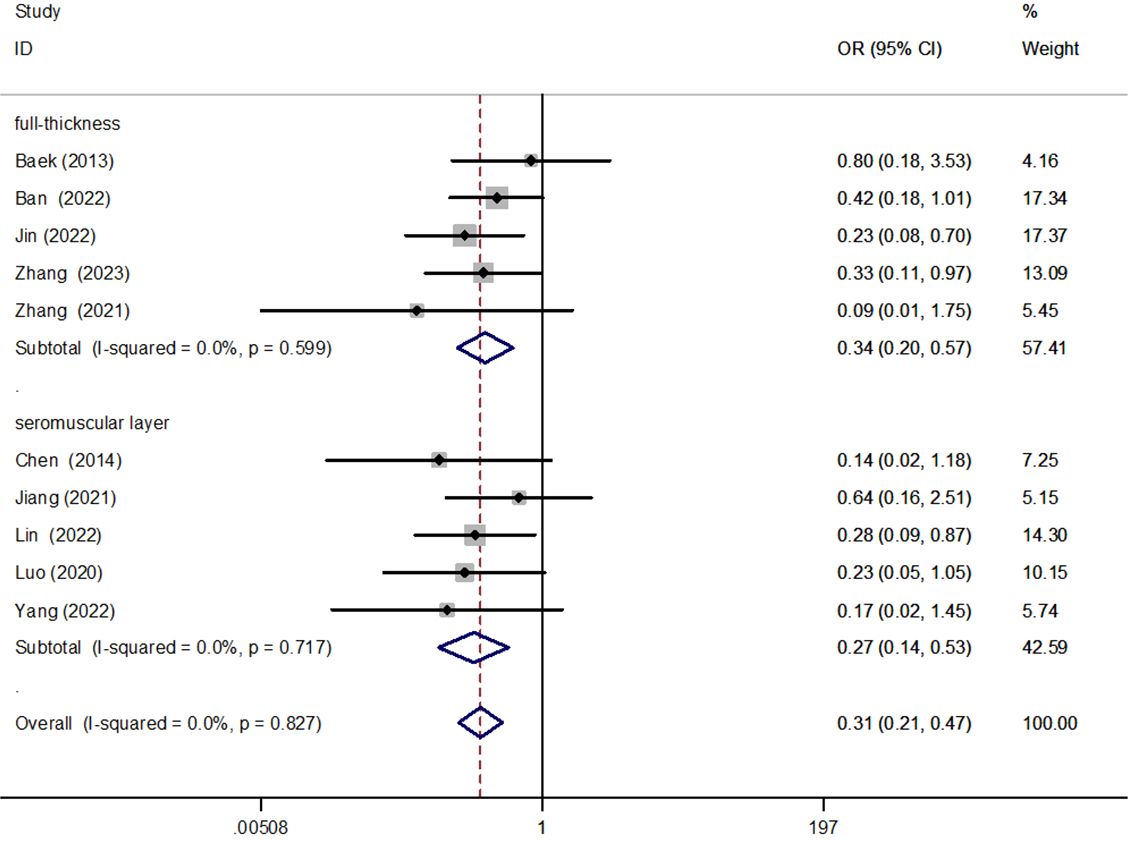
Figure 2 Forest plot of full-thickness versus seromuscular suture in the subgroup analysis of AL incidence.
The quality of the literature for randomized controlled studies was evaluated. All two randomized controlled studies were grouped using either the random number method or the sealed envelope random assignment method, and one study was blinded. All two studies reported complete data for each outcome indicator, but other sources of bias were not clear. All 12 retrospective cohort studies that were included in this analysis were rated as high quality. Out of the 12 studies, five had a score of 7, four had a score of 8, and three had a score of 9 out of a possible 9 on the NOS. This indicates a high level of quality for the included studies, with NOS scores mostly ranging between 7 and 9 (Table 3). The large number of high-quality studies used in this analysis helps to reduce bias and increase the credibility of the results. Therefore, the high quality of the studies included in this analysis makes the resulting meta-analysis more credible.
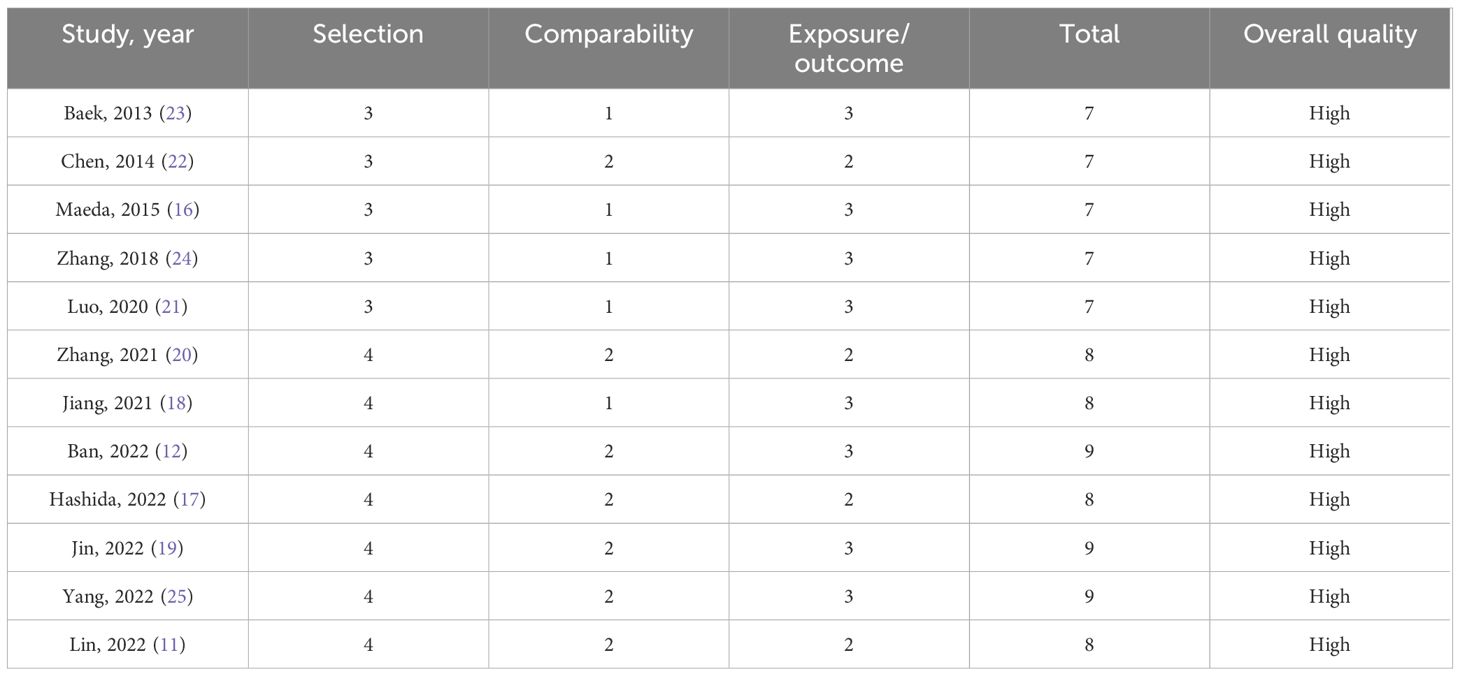
Table 3 Quality assessment of studies included in the final analysis according to the Newcastle-Ottawa scale (NOS).
Fourteen studies (11, 12, 16–27), which included 2,452 participants, were reported with data on AL after laparoscopic surgery for rectal resection. Pooled analysis showed that reinforced sutures to the anastomosis significantly reduced the risk of AL in patients undergoing laparoscopic surgery for rectal resection (OR = 0.26; 95% CI, 0.18–0.37; P < 0.00001; I2 = 0%; Figure 3).
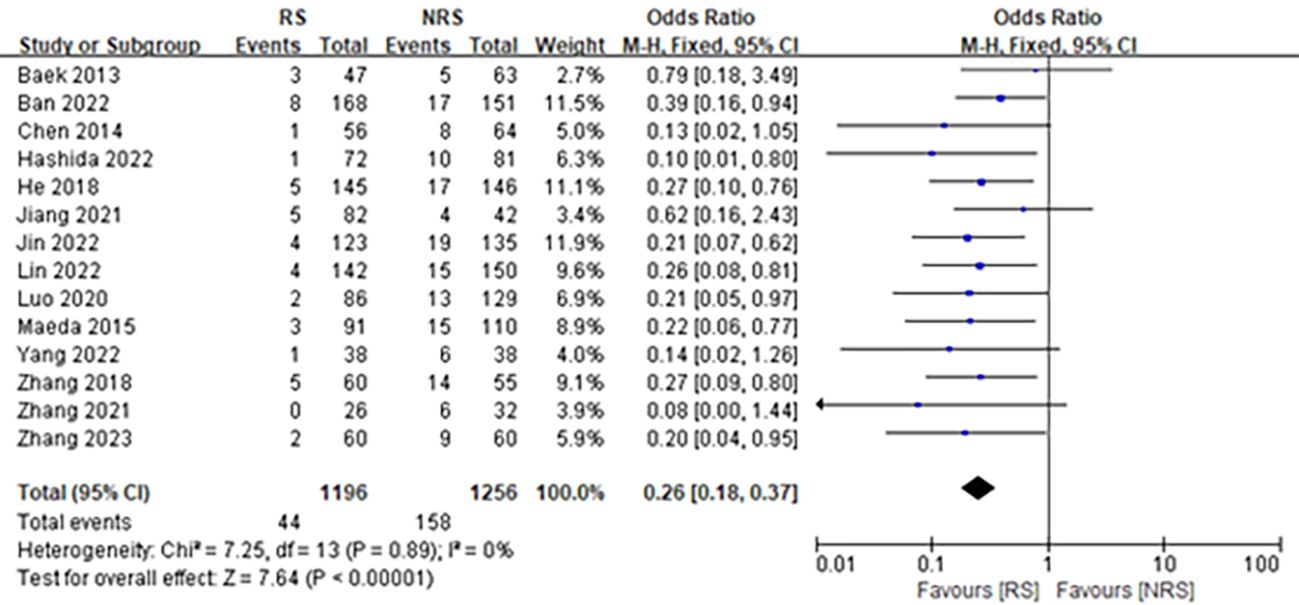
Figure 3 Forest plot comparing the incidence rate of AL in patients with anastomotic reinforcement suture (RS) versus non-reinforcement suture (NRS).
There were three studies (11, 12, 20), consisting of 669 participants, reporting data on anastomotic stenosis after laparoscopic surgery for rectal resection. The results revealed that anastomotic reinforcement sutures did not significantly affect anastomotic stenosis following laparoscopic surgery for rectal resection (OR = 0.69; 95% CI, 0.37–1.32; P = 0.27; I2 = 0%) (Figure 4).
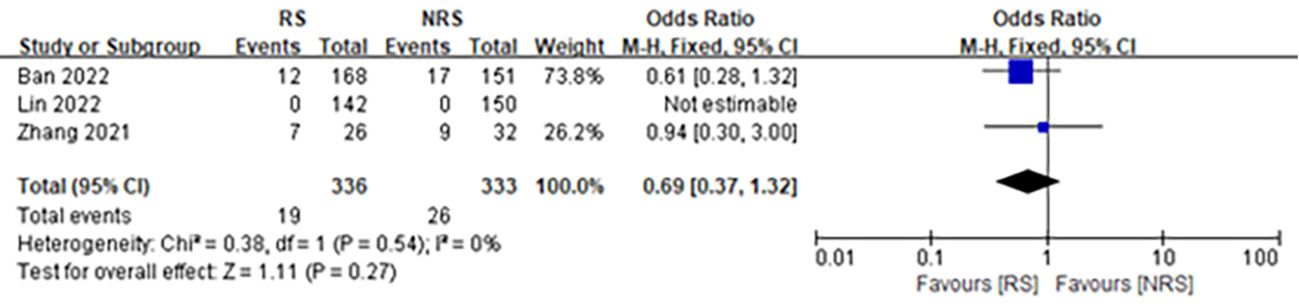
Figure 4 Forest plot comparing the incidence of anastomotic stenosis in patients with reinforced (RS) versus non-reinforced anastomotic sutures (NRS).
We analyzed the results of both retrospective [OR = 0.28, 95% CI (0.19, 0.41), P < 0.001] and randomized [OR = 0.31, 95% CI (0.15, 0.65), P < 0.001] controlled studies according to the type of study, showing that reinforced sutures to the anastomosis significantly reduced the incidence of AL (Figure 5).
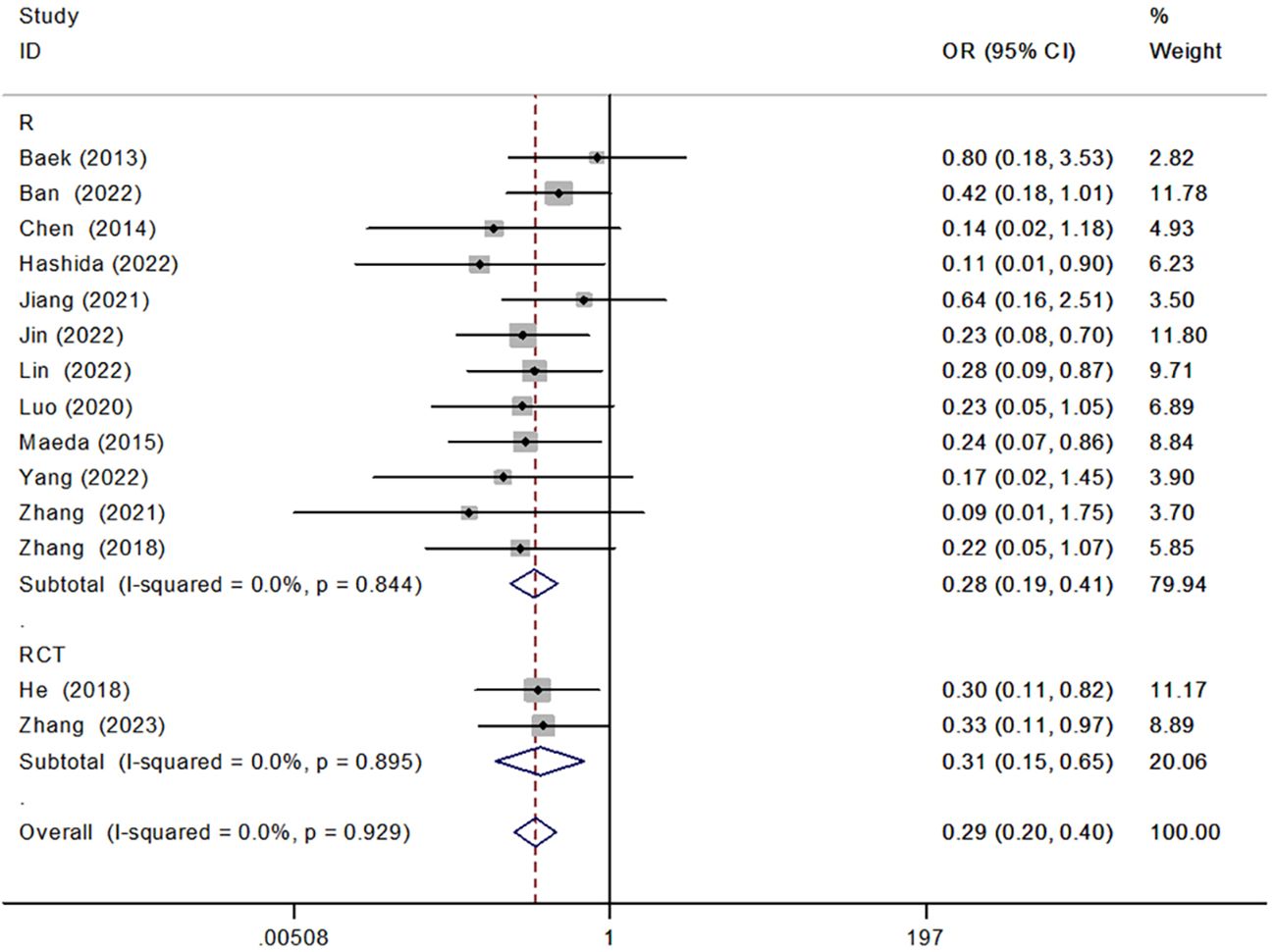
Figure 5 Forest plot of retrospective versus randomized controlled studies in the subgroup analysis of AL incidence.
We performed a subgroup analysis of anastomotic reinforcement sutures using 3–0 versus 4–0 sutures, and the results showed that both anastomotic reinforcement sutures using 3–0 [OR = 0.28, 95% CI (0.17, 0.45), P < 0.001] versus 4–0 [OR = 0.26, 95% CI (0.13, 0.53), P < 0.001] sutures reduced the incidence of AL, and there was no significant difference between the two (Figure 6).
We conducted a subgroup analysis to compare the use of barbed versus non-barbed sutures in anastomotic reinforcement sutures. The results indicated that anastomotic reinforcement sutures using barbed sutures [OR = 0.26, 95% CI (0.14, 0.48), P < 0.001] reduced the incidence of AL when compared to non-barbed sutures [OR = 0.30, 95% CI (0.20, 0.46), P < 0.001]. However, there was no significant difference between the two approaches (Figure 7).
We conducted a subgroup analysis comparing interrupted [OR = 0.31, 95% CI (0.18, 0.53), P < 0.001] and continuous sutures [OR = 0.29, 95% CI (0.16, 0.51), P < 0.001] for anastomotic reinforcement. Results indicated that both suture techniques reduced the incidence of AL (Figure 8).
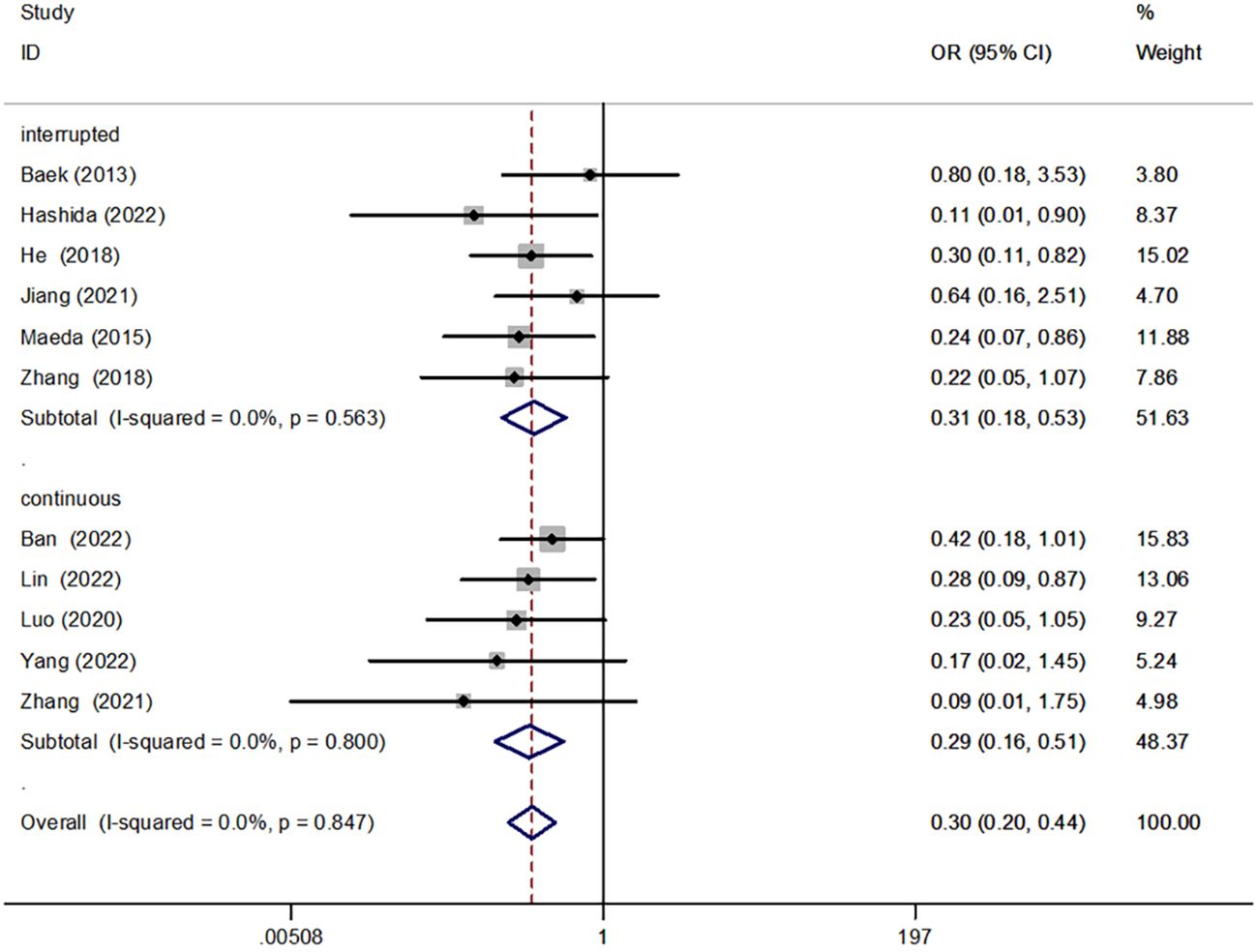
Figure 8 Forest plot of interrupted versus continuous suture in the subgroup analysis of AL incidence.
We performed a subgroup analysis of full-thickness suture and seromuscular suture for anastomotic reinforcement. The results showed that both full-thickness sutures [OR = 0.34, 95% CI (0.20, 0.57), P < 0.001] and seromuscular suture [OR = 0.27, 95% CI (0.14, 0.53), P < 0.001] could reduce the incidence of AL, but there was no significant difference between them (Figure 2).
We performed a subgroup analysis of anastomotic reinforcement sutures for anastomotic one-circle versus non–one-circle sutures. The results showed that both one-circle [OR = 0.25, 95% CI (0.12, 0.52), P < 0.001] versus non–one-circle sutures [OR = 0.30, 95% CI (0.20, 0.44), P < 0.001] for anastomotic reinforcement reduced the incidence of AL, with no significant difference between the two (Figure 9).
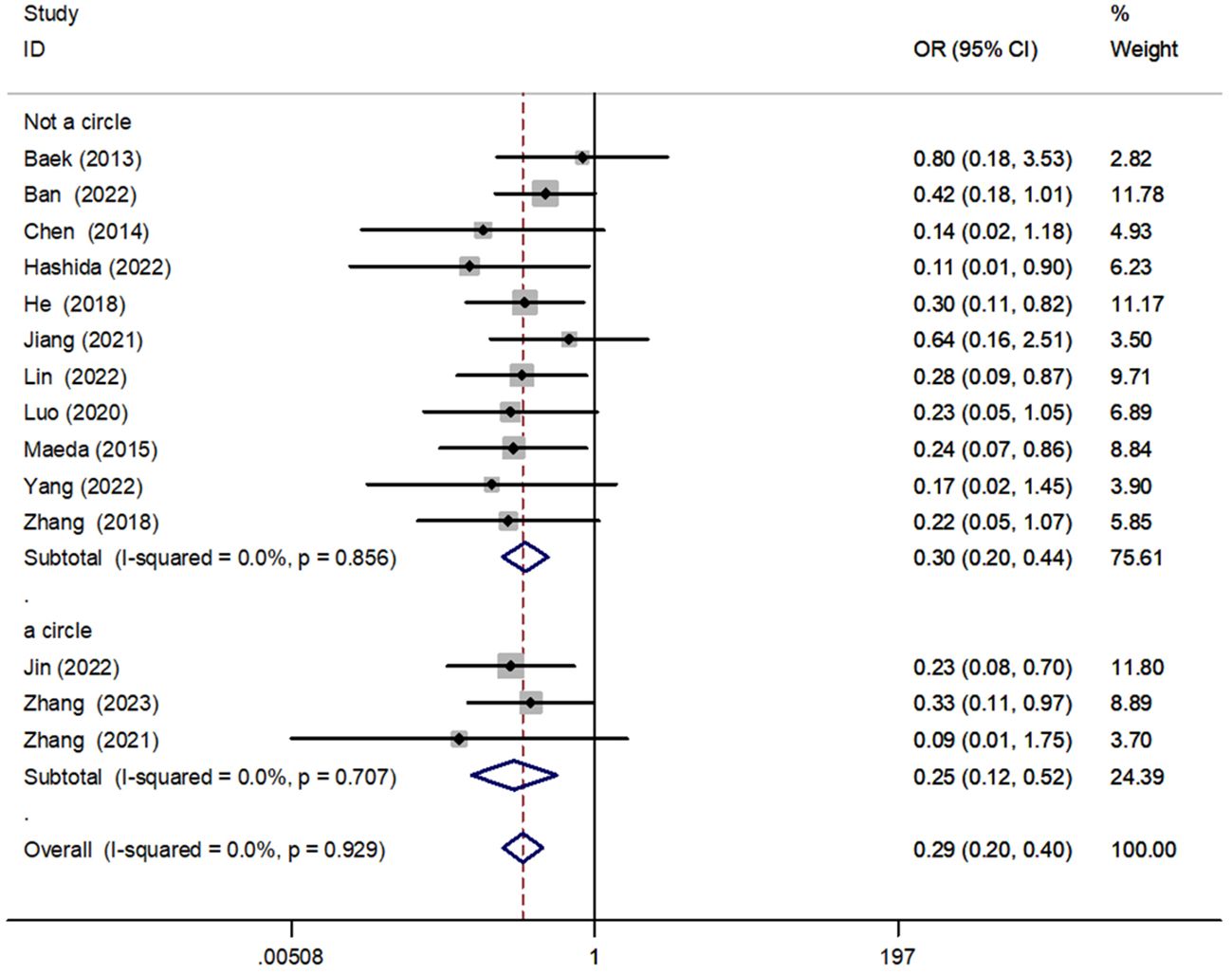
Figure 9 Forest plot of one-circle versus non–one-circle suture in the subgroup analysis of AL incidence.
We performed a subgroup analysis of anastomotic reinforcement sutures for the dog-ear region versus the non–dog-ear region. The results showed that the incidence of AL was reduced for both dog-ear [OR = 0.26, 95% CI (0.14, 0.50), P < 0.001] and non–dog-ear [OR = 0.30, 95% CI (0.20, 0.45), P < 0.001] regions, with no significant difference between the two (Figure 10).
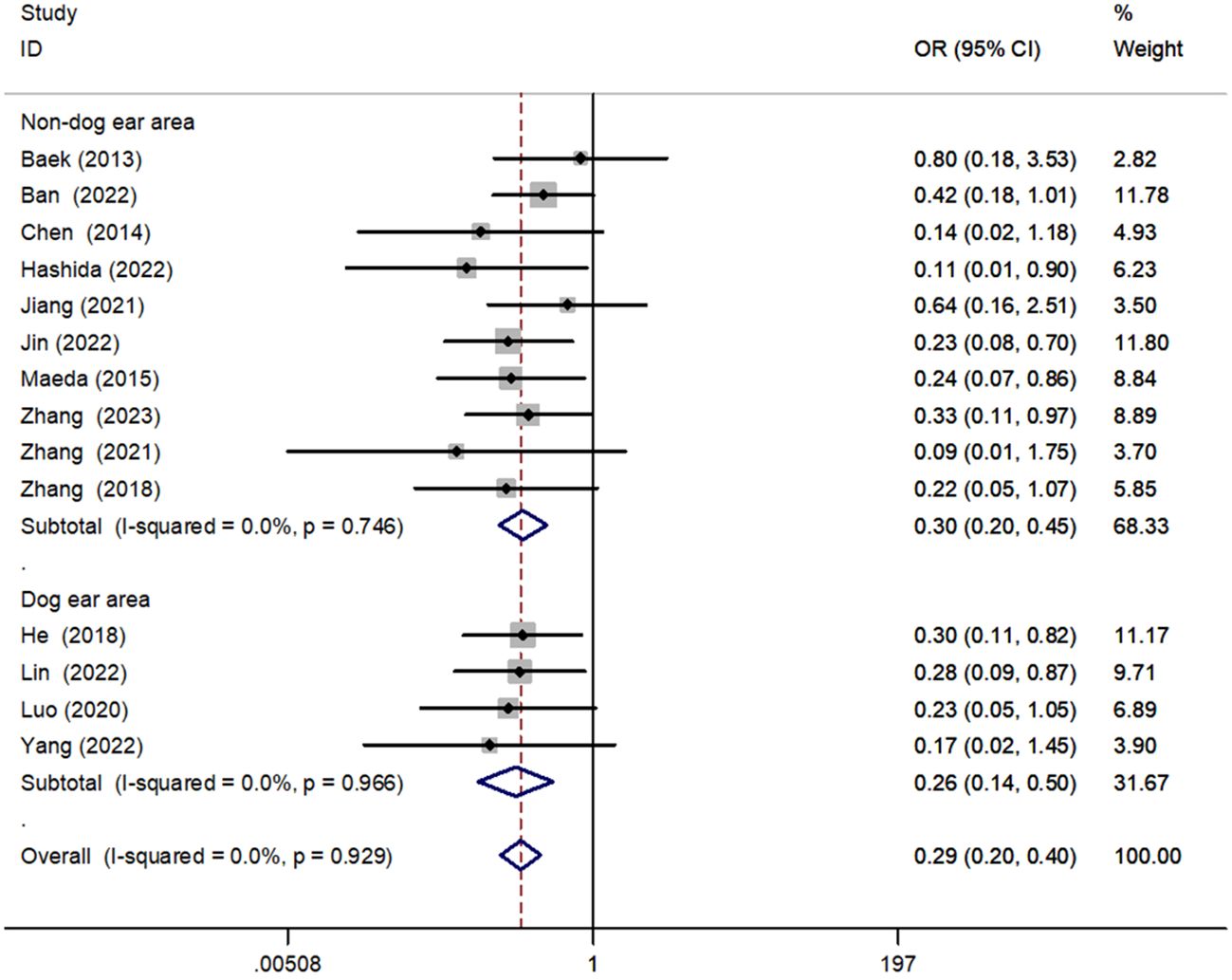
Figure 10 Forest plot of closure of the dog’s ear versus the non–dog’s ear in the subgroup analysis of AL incidence.
Analysis of publication bias is based on a funnel plot drawn to assess the effect of anastomotic reinforcement sutures on AL in patients undergoing rectal resection. This analysis revealed that the scatter of included studies was more evenly distributed, suggesting that the publication bias was not significant and that the results of this systematic analysis were reliable (Figure 11).
Our recent pooled analysis has confirmed that reinforcing the anastomotic suture during laparoscopic surgery for rectal cancer can significantly reduce the incidence of AL in patients who undergo laparoscopic surgery for rectal cancer. This study is the largest pooled and integration analysis of its kind, and its more reliable conclusions suggest that anastomotic reinforcement sutures significantly reduce AL.
AL is one of the most serious complications after laparoscopic surgery for rectal cancer, which induces intra-abdominal infection and pelvic abscess and seriously affects the patient’s postoperative quality of life and prognosis (28). The direct causes of AL include the blood supply of the anastomosis, the level of anastomosis technique, anastomotic tension, and intestinal luminal pressure. The current studies have confirmed that tumor size, distance from the tumor to the anal verge, and the use of reinforcement sutures to the anastomosis are independent risk factors for symptomatic AL (29). Lin et al. (11) conducted a retrospective study of 292 patients undergoing laparoscopic low anterior resection for rectal cancer. They found that the use of barbed sutures for anastomotic reinforcement was associated with a low incidence of AL. These results further suggest that the incidence of postoperative AL was 2.82% and 10%, respectively. These results further suggest that AL can be significantly reduced by reinforcing the anastomotic suture, strengthening the “dog-ear” region, and closing the rectal mesenteric space. As mentioned in our background section, the dog-ear region is a potential ischemic area for AL as the two suture angles of the rectal stump are created by rectal transection. In addition, when performing colorectal end-to-end anastomosis in rectal cancer surgery, a gap between the colonic and rectal mesentery tends to form, leading to delayed postoperative healing and increasing the risk of AL. Several studies have demonstrated that strengthening the “dog’s ear” area and closing the gap with sutures reduces anastomotic tension improve local blood supply and prevent anastomotic dehiscence (24, 26). Few previous studies have focused on the role of anastomotic reinforcement sutures in reducing the incidence of AL after laparoscopic surgery for rectal cancer. Earlier, Gadiot et al. (30) compared 76 cases that received attraction sutures with 77 cases that did not and found a significant decrease in the incidence of AL in the sutured group. Similarly, Maeda et al. (16). conducted a retrospective study on rectal cancer patients who underwent laparoscopic surgery. The study found that the distance between the tumor and the anal verge, the tumor size, and the use of reinforcing sutures were all independent risk factors for AL. The patients in this study were divided into two groups, a low-risk group (patients without any risk factors) and a high-risk group (patients with one or two risk factors), based on the site and size of their tumor. Among the high-risk group, patients who received reinforcing sutures had a significantly lower incidence of AL compared to patients who did not receive reinforcing sutures. However, no significant difference was observed in the low-risk group. In a study of laparoscopic endoluminal reinforcement sutures in laparoscopic rectal surgery, Hashida et al. (17). found that laparoscopic endoluminal reinforcement sutures significantly reduced the incidence of AL, whereas, in multivariate analysis, distance to the anal verge less than 6.5 cm, diabetes mellitus, and non-use of reinforcement sutures were shown to be the independent risk factors for AL.
Currently, most laparoscopic radical rectal cancer surgeries are performed with a double anastomosis device anastomosis, and clinical reports on further reducing AL through technical improvements are rare. In this study, we included all the clinical studies on the postoperative effects of anastomotic reinforcement sutures on patients after laparoscopic surgery for rectal resection, and the results confirmed that anastomotic reinforcement suture can significantly reduce the incidence of AL after laparoscopic surgery for rectal resection, and, therefore, we believe that anastomotic reinforcement suture is a clinical problem that surgeons need to pay great attention to and has a significant effect on reducing the incidence of postoperative complications after laparoscopic surgery for rectal resection. The incidence of complications after laparoscopic surgery for rectal resection is of great significance.
In this study, we conducted a pooled analysis of currently available randomized controlled and retrospective studies on anastomotic reinforcement suturing, 3–0 versus 4–0 suture, barbed versus non-barbed suture, interrupted versus continuous suture, full-thickness versus seromuscular suture, one-circle versus non–one-circle suture, and closure of the dog’s ear versus non–dog’s ear to further confirm that anastomotic reinforcement suturing significantly reduces the incidence of AL, which was similarly confirmed by subgroup analyses showing the results of randomized controlled studies. We also found that reinforcement suturing of the anastomosis could reduce the risk of anastomotic stenosis, but, due to the small number of included studies, the results may have some errors, so further validation is still needed in subsequent studies. Meanwhile, most of the studies included in this study were retrospective clinical studies with small sample sizes, and the methods of anastomotic reinforcement suturing varied from study to study, so there is a certain degree of variability, and we look forward to future multicenter prospective randomized controlled trials with large sample sizes to further validate the results. We have used this study to reinforce the anastomosis with sutures during laparoscopic rectal surgery.
Through our integrated analysis study, we have confirmed that reinforcing sutures in the anastomosis significantly reduces the incidence of AL. This finding can provide useful guidance for clinical surgeons and has great value in reducing postoperative complications after rectal surgery. However, the present study requires a large number of randomized controlled studies to further confirm the reliability of this finding.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
YY: Conceptualization, Data curation, Formal analysis, Software, Validation, Writing – original draft, Writing – review & editing. XLZ: Conceptualization, Data curation, Formal analysis, Software, Supervision, Writing – review & editing. YQ: Conceptualization, Data curation, Methodology, Project administration, Validation, Writing – review & editing. XZ: Formal analysis, Project administration, Software, Supervision, Validation, Writing – review & editing. FD: Conceptualization, Data curation, Formal analysis, Project administration, Resources, Validation, Visualization, Writing – review & editing. JL: Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing. BZ: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Resources, Supervision, Validation, Visualization, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2024.1337870/full#supplementary-material
1. Paun BC, Cassie S, MacLean AR, Dixon E, Buie WD. Postoperative complications following surgery for rectal cancer. Ann Surg. (2010) 251:807–18. doi: 10.1097/SLA.0b013e3181dae4ed
2. Brisinda G, Vanella S, Cadeddu F, Civello IM, Brandara F, Nigro C, et al. End-to-end versus end-to-side stapled anastomoses after anterior resection for rectal cancer. J Surg Oncol. (2009) 99:75–9. doi: 10.1002/jso.21182
3. Park JS, Huh JW, Park YA, Cho YB, Yun SH, Kim HC, et al. Risk factors of anastomotic leakage and long-term survival after colorectal surgery. Med (Baltimore). (2016) 95:e2890. doi: 10.1097/MD.0000000000002890
4. Gessler B, Eriksson O, Angenete E. Diagnosis, treatment, and consequences of anastomotic leakage in colorectal surgery. Int J Colorectal Dis. (2017) 32:549–56. doi: 10.1007/s00384–016-2744-x
5. Kim CW, Baek SJ, Hur H, Min BS, Baik SH, Kim NK. Anastomotic leakage after low anterior resection for rectal cancer is different between minimally invasive surgery and open surgery. Ann Surg. (2016) 263:130–7. doi: 10.1097/SLA.0000000000001157
6. Kawada K, Sakai Y. Preoperative, intraoperative and postoperative risk factors for anastomotic leakage after laparoscopic low anterior resection with double stapling technique anastomosis. World J Gastroenterol. (2016) 22:5718–27. doi: 10.3748/wjg.v22.i25.5718
7. Katory M, McLean R, Osman K, Ahmad M, Hughes T, Newby M, et al. The novel appearance of low rectal anastomosis on contrast enema following laparoscopic anterior resection: discriminating anastomotic leaks from "dog-ears" on water-soluble contrast enema and flexible sigmoidoscopy. Abdom Radiol (NY). (2017) 42:435–41. doi: 10.1007/s00261–016-0885–6
8. Hazama S, Oka M, Suzuki T. Modified technique for double stapling of colorectal anastomosis following low anterior resection. Br J Surg. (1996) 83:1110. doi: 10.1002/bjs.1800830824
9. Placer C, Enríquez-Navascués JM, Elorza G, Timoteo A, Mugica JA, Borda N, et al. Preventing complications in colorectal anastomosis: results of a randomized controlled trial using bioabsorbable staple line reinforcement for circular stapler. Dis Colon Rectum. (2014) 57:1195–201. doi: 10.1097/DCR.0000000000000207
10. Senagore A, Lane FR, Lee E, Wexner S, Dujovny N, Sklow B, et al. Bioabsorbable Staple Line Reinforcement Study Group. Bioabsorbable staple line reinforcement in restorative proctectomy and anterior resection: a randomized study. Dis Colon Rectum. (2014) 57:324–30. doi: 10.1097/DCR.0000000000000065
11. Lin H, Yu M, Ye G, Qin S, Fang H, Jing R, et al. Intracorporeal reinforcement with barbed suture is associated with low anastomotic leakage rates after laparoscopic low anterior resection for rectal cancer: a retrospective study. BMC Surg. (2022) 22:335. doi: 10.1186/s12893–022-01782-x
12. Ban B, Shang A, Shi J. Efficacy of staple line reinforcement by barbed suture for preventing anastomotic leakage in laparoscopic rectal cancer surgery. World J Gastrointest Surg. (2022) 14:821–32. doi: 10.4240/wjgs.v14.i8.821
13. Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. (2021) 372:n160. doi: 10.1136/bmj.n160
14. Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. (2019) 10:ED000142. doi: 10.1002/14651858.ED000142
15. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
16. Maeda K, Nagahara H, Shibutani M, Ohtani H, Sakurai K, Toyokawa T, et al. Efficacy of intracorporeal reinforcing sutures for anastomotic leakage after laparoscopic surgery for rectal cancer. Surg Endosc. (2015) 29:3535–42. doi: 10.1007/s00464–015-4104–2
17. Hashida H, Mizuno R, Iwaki K, Hanabata Y, Kita R, Oshima N, et al. Intracorporeal reinforcing sutures reduce anastomotic leakage in double-stapling anastomosis for laparoscopic rectal surgery. Wideochir Inne Tech Maloinwazyjne. (2022) 17:491–7. doi: 10.5114/wiitm.2022.115168
18. Jiang TY, Zang L, Dong F, Feng B, Zong YP, Sun J, et al. Effect of different reinforcement methods on anastomotic leakage prevention after laparoscopic double anastomosis. J Surg Oncol. (2021) 123 Suppl 1:S81–7. doi: 10.1002/jso.26333
19. Jin CW, Wang Y, Fu Z. Effect of anastomotic reinforcemect suture on the incidenceof anastomotic fistula after laparoscopic surgery for low and middle rectal cancer. J Xuzhou Med Univ. (2022) 42:110–4. doi: 10.3969/j.issn.2096-3882.2022.02.007
20. Zhang H, Chen S, Zhang J, Zhou Q, Xu SR. Effectiveness of transanal reinforced anastomosis in laparoscopic sphincter preserving operation for ultra-low rectal cancer. J Colorectal Anal Surg. (2021) 27:560–3. doi: 10.19668/j.cnki.issn1674-0491.2021.06.008
21. Luo Y, Yu MH, Chen JJ, Qin J, Qin SL, Huang YZ, et al. Application value of barbed suture in reinforcing anastomosis during laparoscopic radical resection of rectal cancer. Chin J Dig Surg. (2020) 19:1205–10. doi: 10.3760/cma.j.cn115610-20-201020-00664
22. Chen S, Wu Y, Han S, Mo Q, Ma Y, Song S, et al. [Modification and efficacy observation of laparoscopic dual anastomosis for mid-low rectal cancer]. Zhonghua Wei Chang Wai Ke Za Zhi. (2014) 17:1216–9. doi: 10.3760/cma.j.issn.1671-0274.2014.12.016
23. Baek SJ, Kim J, Kwak J, Kim SH. Can trans-anal reinforcing sutures after double stapling in lower anterior resection reduce the need for a temporary diverting ostomy? World J Gastroenterol. (2013) 19:5309–13. doi: 10.3748/wjg.v19.i32.5309
24. Zhang Y, Wang X. Effect of reinforcing ‘dog ear area’ to reduce the risk of anastomotic leakage after laparoscopic TME for rectal cancer. J Colorectal Anal Surg. (2018) 24:545–8. doi: 10.19668/j.cnki.issn1674-0491.2018.06.004
25. Yang XD. The application value of barbed suture in laparoscopic radical resection of rectal cancer to strengthen the anastomosis. system Med. (2022) 7:131–4. doi: 10.19368/j.cnki.issn2096-1782.2022.01.131
26. He Y, Zhu Z, Liu S, Liu L, Hu B, Wan X, et al. [Effect of anastomotic reinforcing sutures on the incidence of anastomotic leakage after laparoscopic radical resection of rectal cancer: a prospective randomized controlled trial]. Zhonghua Wei Chang Wai Ke Za Zhi. (2018) 21:431–6. doi: 10.3760/cma.j.issn.1671-0274.2018.04.014
27. Zhang HQ, Xu L, Wang ZL, Shao Y, Chen Y, Lu YF, et al. The effect of reinforcing sutures and trans-anal drainage tube on the outcome of laparoscopic resection for rectal cancer: propensity score-matched analysis. Langenbecks Arch Surg. (2023) 408:289. doi: 10.1007/s00423–023-03027–8
28. Chiarello MM, Fransvea P, Cariati M, Adams NJ, Bianchi V, Brisinda G. Anastomotic leakage in colorectal cancer surgery. Surg Oncol. (2022) 40:101708. doi: 10.1016/j.suronc.2022.101708
29. Tsalikidis C, Mitsala A, Mentonis VI, Romanidis K, Pappas-Gogos G, Tsaroucha AK, et al. Predictive factors for anastomotic leakage following colorectal cancer surgery: where are we and where are we going? Curr Oncol. (2023) 30:3111–37. doi: 10.3390/curroncol30030236
Keywords: anastomotic reinforcement sutures, anastomotic leakage, rectal cancer, laparoscopic surgery, pooled and integration analysis
Citation: Yue Y, Zhang X, Qu Y, Zhao X, Ding F, Li J and Zheng B (2024) Effectiveness of anastomotic reinforcement sutures in reducing anastomotic leakage risk after laparoscopic rectal cancer surgery: a pooled and integration analysis. Front. Oncol. 14:1337870. doi: 10.3389/fonc.2024.1337870
Received: 28 December 2023; Accepted: 16 May 2024;
Published: 04 June 2024.
Edited by:
Jacopo Andreuccetti, Civil Hospital of Brescia, ItalyReviewed by:
Tadahiko Masaki, Kyorin University, JapanCopyright © 2024 Yue, Zhang, Qu, Zhao, Ding, Li and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bobo Zheng, emhlbmdibzgxNkAxMjYuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.