
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Oncol. , 15 March 2024
Sec. Genitourinary Oncology
Volume 14 - 2024 | https://doi.org/10.3389/fonc.2024.1321919
Introduction: The most common sites of clear cell renal cell carcinoma(ccRCC) metastasis are the lung, bones, liver and brain; eyelid metastasis is a rare occurrence.
Case presentation: We report a case of ccRCC metastasis to the left eyelid after radical nephrectomy, and remission after sunitinib treatment.
Conclusions: Although the probability of eyelid metastasis rate is very low, tumor metastasis to the eyelid skin is possible after radical nephrectomy. Therefore, any rash like changes on the skin during the review procedure cannot be ignored by the physician.
Renal cell carcinoma (RCC) is the most common type of adult kidney cancer, and clear cell renal cell carcinoma (ccRCC) represents the most common renal cancer histology. About two-thirds of patients have no metastases when they are first diagnosed (1). Patients without metastatic ccRCC can be cured by nephrectomy. However, more than one third of patients with stage II-III ccRCC have a recurrence after radical nephrectomy (2), metastasis is common in lung, bone, liver, brain and so on (3). Metastatic sites of clear cell renal cell carcinoma are generally characterized by good blood supply and weak autoimmune function, such as lung and bone. The skin appears to be an exempt site for ccRCC metastasis. In this paper, we report a case of ccRCC metastasis to the left eyelid 5 years after radical nephrectomy and remission after targeted therapy with sunitinib.
A 59-year-old woman was admitted to the hospital with the chief complaint of a 2-month left eyelid mass with pain. Physical examination revealed a mass on to the left eyelid. 5 years ago, the patient accidentally discovered a mass on the right side of his abdomen. She had no symptoms of hematuria, frequent urination, or painful urination, nor was she accompanied by dysuria or low back pain. The patient had undergone laparoscopic radical nephrectomy of ccRCC in September 2018, and the TNM stage was T2N0M0. Pathological diagnosis: clear cell renal cell carcinoma, invasion of the renal capsule, WHO/ISUP grade III, no cancer cells found in the ureteral resection margin. Considering the patient’s medical history, we thought that the eyelid mass might be the result of ccRCC metastasis. MRI examination suggested the possibility of metastatic tumor (Figure 1A). After ruling out the remaining possibilities, we recommended that the patient undergo eyelid mass resection to remove the metastatic tumor. However, the patient and her family refused operation and biopsy. The patient decided not to use cabozantinib due to financial difficulties, we jointly decided to use sunitinib for antineoplastic therapy. She was medically treated after signing an informed consent form. After 1 months of treatment, the mass was significantly decreased compared with before (Figures 1B, C), and the pain disappeared.
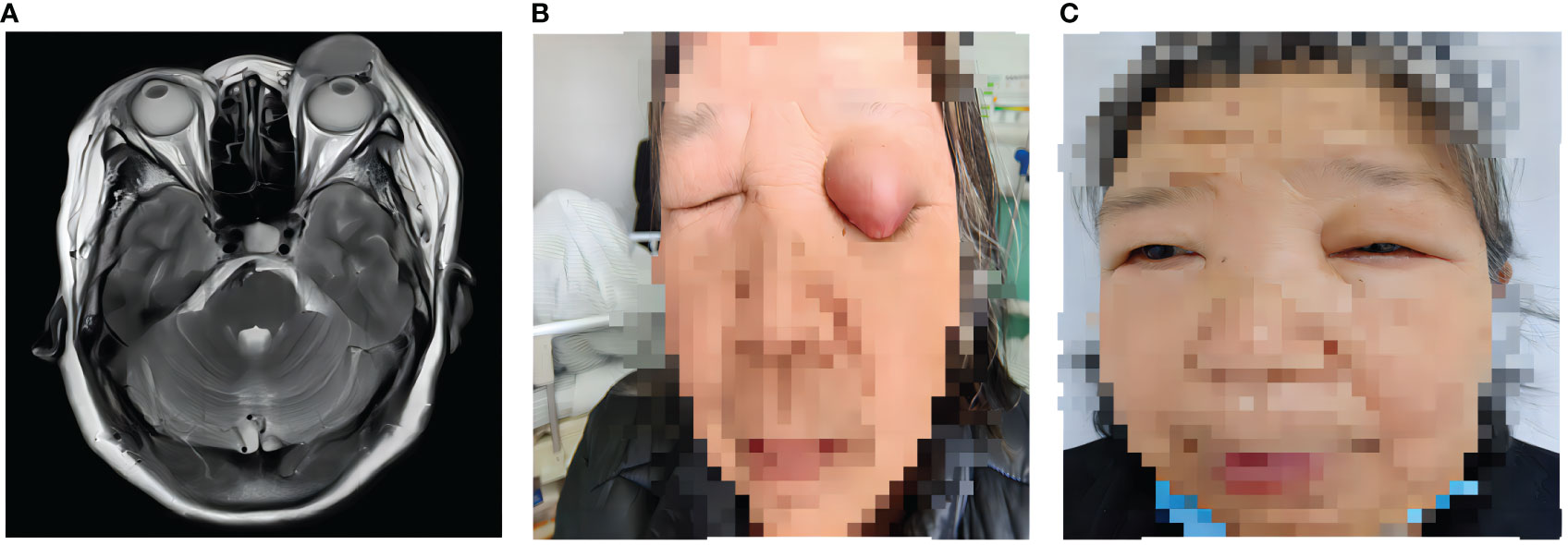
Figure 1 The change of ccRCC metastasis on the left eyelid. (A) MRI image of the mass on the left eyelid. (B) A painful mass on the left eyelid. (C) The mass was disappeared after 1 months of sunitinib treatment.
This case of eyelid metastasis 5 years after radical nephrectomy without accompanying metastasis in other locations proved that RCC can have unusual sites of metastasis. So far, there are few cases of ccRCC metastasis to the eyelid reported worldwide. In most cases, eyelid metastases usually occur later in the disease course as a manifestation of systemic metastatic cancer, and sometimes may be the first manifestation when the origin of the tumor is unknown (4). It has been reported that patients with RCC with isolated eyelid metastasis can obtain good prognosis after undergoing simultaneous resection of the primary and metastatic tumors. Nima Mikail et al. reported that simultaneous resection of the primary RCC and eyelid metastases did not result in tumor progression during a follow-up period of 2 years (5).
For metastatic ccRCC, targeted therapy alone or combined with immunotherapy has achieved efficacy and improved the overall survival time of patients (6). However, there is still a lack of consensus on the routine adjuvant therapy for patients with isolated eyelid metastasis after metastasis resection. In some reports, patients with eyelid metastasis were treated with resection, radiotherapy or interferon therapy, but some had poor prognosis (7, 8). According to some reports, the patient’s symptoms were relieved and the patient’s life quality was greatly improved after the use of sunitinib (9, 10).
Although eyelid metastasis from ccRCC is rare, cases of skin metastases have been reported. Our study reviewed the literature on skin metastases of renal cell carcinoma (Table 1). Therefore, postoperative patients with ccRCC should be regularly reexamined with chest CT, liver, gallbladder, pancreas, spleen and kidney color Doppler ultrasound. In addition, skin rashes or nodules on the surface of the skin, especially painless lesions should be dynamically monitored to early find metastasis. Some scholars have pointed out that RCC-Ma, a ccRCC marker, has specificity for ccRCC skin metastasis, which is also worthy of reference in our subsequent research and application (19).
After radical nephrectomy for ccRCC, there is the possibility of metastasis to the eyelid. In the follow-up process after surgery, some lesions or nodules of the body epidermis should not be ignored.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
YH: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Project administration, Software, Writing – review & editing. DZ: Writing – review & editing, Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft. ZJ: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft. MY: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft. ZS: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft. YT: Project administration, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Choueiri TK, Motzer RJ. Systemic therapy for metastatic renal-cell carcinoma. N Engl J Med. (2017) 376:354–66. doi: 10.1056/NEJMra1601333
2. Ciccarese C, Strusi A, Arduini D, Russo P, Palermo G, Foschi N, et al. Post nephrectomy management of localized renal cell carcinoma. From risk stratification to therapeutic evidence in an evolving clinical scenario. Cancer Treat Rev. (2023) 115:102528. doi: 10.1016/j.ctrv.2023.102528
3. McKay RR, Kroeger N, Xie W, Lee JL, Knox JJ, Bjarnason GA, et al. Impact of bone and liver metastases on patients with renal cell carcinoma treated with targeted therapy. Eur Urol. (2014) 65:577–84. doi: 10.1016/j.eururo.2013.08.012
4. Cabrera-Beyrouti R, Campos-Mollo E, Rico-Santos E, Jiménez-Rodríguez DN, Lledó-Riquelme M, Vierna-García J. Eyelid metastasis as first presentation of renal cell carcinoma. Arch Soc Esp Oftalmol. (2017) 92:547–51. doi: 10.1016/j.oftale.2017.05.002
5. Mikail N, Belew D, Ullah A, Payne-Jamaeu Y, Patel N, Kavuri S, et al. Renal cell carcinoma presenting as an isolated eyelid metastasis. J Endourol Case Rep. (2020) 6:322–4. doi: 10.1089/cren.2020.0107
6. Atkins MB, Tannir NM. Current and emerging therapies for first-line treatment of metastatic clear cell renal cell carcinoma. Cancer Treat Rev. (2018) 70:127–37. doi: 10.1016/j.ctrv.2018.07.009
7. Shome D, Honavar SG, Gupta P, Vemuganti GK, Reddy PV. Metastasis to the eye and orbit from renal cell carcinoma–a report of three cases and review of literature. Surv Ophthalmol. (2007) 52:213–23. doi: 10.1016/j.survophthal.2006.12.004
8. Kindermann WR, Shields JA, Eiferman RA, Stephens RF, Hirsch SE. Metastatic renal cell carcinoma to the eye and adnexae: a report of three cases and review of the literature. Ophthalmology. (1981) 88:1347–50. doi: 10.1016/S0161-6420(81)34854-4
9. Lee HJ, Lee A, Tan D, Du J, Wang Y, Tang PY, et al. Cutaneous metastasis of renal cell carcinoma. Lancet Oncol. (2020) 21:e292. doi: 10.1016/S1470-2045(20)30143-1
10. Kuroki H, Oyama N, Koike H. A case of an orbital metastasectomy in a renal cell carcinoma after sunitinib treatment : A case report. Hinyokika Kiyo. (2015) 61(8):335–9.
11. Escobar Gil T, Saldarriaga Santamaría S, Del Valle Saavedra JJ, Mejía Giraldo AM, Peña Zúñiga EB. An atypical cutaneous metastasis in a case of clear cell renal carcinoma. Cureus. (2022) 14:e30722. doi: 10.7759/cureus.30722
12. Gonzalez F, Abalo-Lojo JM, Suarez-Peñaranda JM, Caneiro-Gómez J. Eyelid metastasis as the initial presentation of a renal cell carcinoma. Urology. (2015) 85:e35–6. doi: 10.1016/j.urology.2015.01.039
13. Fang Q, Zeng J, Wu D. Eyelid metastasis as the initial presentation of renal cell carcinoma: Case report. J Fr Ophtalmol. (2022) 45:137–9. doi: 10.1016/j.jfo.2021.08.024
14. Lapp T, Mittelviefhaus H, Werner M, Auw-Hädrich C. Severe bleeding eyelid after trivial trauma: conjunctival metastasis of a renal cell carcinoma. Graefes Arch Clin Exp Ophthalmol. (2012) 250:1705–6. doi: 10.1007/s00417-011-1806-6
15. Greco F, Sabatino L, Sabatino F, Casale M, Quattrocchi CC, Zobel BB. Unilateral blepharoptosis from renal cell carcinoma. J Kidney Cancer VHL. (2016) 3:11–5. doi: 10.15586/jkcvhl.2016.61
16. Kurli M, Finger PT, Schneider S, Tena LB. Eyelid-sparing adjuvant radiation therapy for renal cell carcinoma. Ophthalmologica. (2006) 220:198–200. doi: 10.1159/000091766
17. Vozmediano-Serrano MT, Toledano-Fernández N, Fdez-Aceñero MJ, Gil-Díez JL, García-Saenz S. Lacrimal sac metastases from renal cell carcinoma. Orbit. (2006) 25:249–51. doi: 10.1080/01676830600575550
18. Rai R, Jakobiec FA, Fay A. Ocular metastatic renal carcinoma presenting with proptosis. Ophthalmic Plast Reconstr Surg. (2015) 31:e100–8. doi: 10.1097/IOP.0000000000000119
Keywords: renal cell carcinoma, eyelid metastasis, renal tumor, sunitinib, MRI
Citation: Yin H, Du Z, Zhang J, Ma Y, Zhao S and Yang T (2024) Case report: Isolated eyelid metastasis of ccRCC 5 years after receiving radical nephrectomy. Front. Oncol. 14:1321919. doi: 10.3389/fonc.2024.1321919
Received: 15 October 2023; Accepted: 01 March 2024;
Published: 15 March 2024.
Edited by:
Giovanni Rosti, San Matteo Hospital Foundation (IRCCS), ItalyReviewed by:
Giuseppe Schepisi, Scientific Institute of Romagna for the Study and Treatment of Tumors (IRCCS), ItalyCopyright © 2024 Yin, Du, Zhang, Ma, Zhao and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tiejun Yang, VGllanVueWFuZ0AxMjYuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.