
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Oncol., 28 November 2023
Sec. Surgical Oncology
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.1326032
This article is part of the Research TopicRobotic and Video-Assisted Surgery for Cancer TreatmentView all 10 articles
 Yihui Han1,2†
Yihui Han1,2† Wenming Yang3†
Wenming Yang3† Wenshu Dai4
Wenshu Dai4 Qin Ma3
Qin Ma3 Tao Yuan5
Tao Yuan5 Yun Yang1,6
Yun Yang1,6 Yanrong Lu4
Yanrong Lu4 Bo Zhang1,2*
Bo Zhang1,2* Mingming Zhang1,6*
Mingming Zhang1,6*Introduction: Intra-abdominal gossypiboma, a cotton-based retained foreign body after an abdominal surgery, is associated with various clinical manifestations and complications. Its infrequent occurrence and unpredictability make its early diagnosis particularly challenging. We herein present an atypical case of intra-abdominal gossypiboma mistaken for a jejunal tumor.
Case presentation: A 33-year-old female presented to the emergency room with an acute episode of progressive abdominal pain and distention, nausea, and vomiting for 20 hours. She had undergone an urgent cesarean section due to fetal tachycardia seven years prior. The initial diagnosis of small bowel obstruction (SBO) due to a jejunal tumor was established by computed tomography. Subsequent to successful medical management of the SBO, a laparoscopy-assisted resection of the mass and the adherent jejunal segment was conducted, culminating in a primary side-to-side jejunojejunostomy. Examination of the excised tissue revealed an approximately spherical fibrous mass, 6 × 6 × 5 cm in dimension, embedded in the jejunal wall, housing a 20 × 20-cm gauze. Postoperative recovery and routine follow-up ensued without complications.
Conclusion: In light of this case, the need for clinicians to maintain an elevated awareness and suspicion of gossypiboma should be accentuated when evaluating an intra-abdominal mass, especially in patients with a prior history of high-risk laparotomy. Laparoscopic surgery stands out as a technically proficient and minimally invasive strategy for diagnosing and treating intra-abdominal gossypiboma. Besides, it is imperative to emphasize the importance of meticulous surgical procedures and postoperative protocols to prevent such oversights, reaffirming the need for consistent intraoperative counts and checks of surgical items.
Gossypiboma, derived from “gossypium” (Latin for cotton) and “boma” (Swahili for place of concealment), was first documented by Wilson in 1884 (1). It represents a rare yet entirely preventable iatrogenic complication (2). By definition, a gossypiboma is a cotton-based mass within a body cavity that results from the body’s reaction to a sponge or gauze inadvertently retained post-surgery. In the United States, the incidence varied from 1 in 1,000 – 1,500 to 1 in 8,801 - 18,760 inpatient operations in the past decades (3). Due to malpractice claims and medicolegal consequences involved, the actual incidence of gossypiboma remains unknown and definitely underestimated (4). The gossypiboma formation are reported to be significantly associated with emergency surgery, unplanned changes in procedure, morbid obesity, and multiple major procedures done in a single operation or cases in which multiple surgical teams were involved (3, 5, 6).
The abdominopelvic cavity was the most frequent body cavity where the foreign body left (54%), followed by vagina (22%), thorax (7%), and others (17%; including the spinal canal, face, brain, and extremities) (3). Notably, while gossypibomas are less likely to occur in laparoscopic or robotic procedures, their prevalence is higher in laparotomy (7). Intra-abdominal gossypiboma patients can present to hospital with various clinical manifestations and even significant morbidity, such as ileus, perforation, abscess collection, fistula formation, and sepsis (8, 9). Due to rare and unanticipated, precise preoperative diagnosis of intra-abdominal gossypiboma is extremely challenging (10).
In alignment with the principles of the CAse REport (CARE) guidelines (11), we herein describe an unusual case of intra-abdominal gossypiboma complicated by ileus and masquerading as a jejunal tumor, which was treated successfully by laparoscopy-assisted resection. In light of this case, it is imperative to emphasize the importance of meticulous surgical procedures and postoperative protocols to prevent such oversights, reaffirming the need for consistent intraoperative counts and checks of surgical items.
In November 2022, a 33-year-old Han Chinese female patient was referred to our emergency room with progressive abdominal pain (colicky in nature; sudden onset, continuous, crushing in character) and distention, nausea, and vomiting for 20 hours. She had undergone an urgent cesarean section because of fetal tachycardia 7 years previously. There were no underlying comorbidities or family history of malignancies with her. On admission, she was subfebrile with slightly abnormal vital signs (Temperature, 37.5°C; Blood pressure, 108/72 mmHg; Heart rate, 102 beats per minute; Respiratory rate, 19 beats per minute). Physical examination showed abdominal distention, slight rebound tenderness in the periumbilical area, and a painless palpable mass in the lower quadrant with metallic bowel sounds. The result of digital rectal examination was unremarkable.
Blood tests indicated a systemic infection with an elevated total leukocyte count (13.2 ×10^9/L; reference range, 3.5 – 9.5 × 10^9/L), percentage of neutrophils (91%; reference range, 40 – 75%), and C-reaction protein (36 mg/L; reference range, <5 mg/L). Contrast-enhanced computed tomography (CT) of the abdomen and pelvis demonstrated dilated proximal bowel loops and multiple air-fluid levels due to a 6.1 × 5.7-cm, approximately spherical, well-delineated heterogeneous cystic and hyperdense jejunal mass and mild intestinal volvulus, without indicators of intestinal ischemia or necrosis (Figure 1). There were no metastases to the liver, greater omentum, or peritoneum detectable on radiologic imaging.
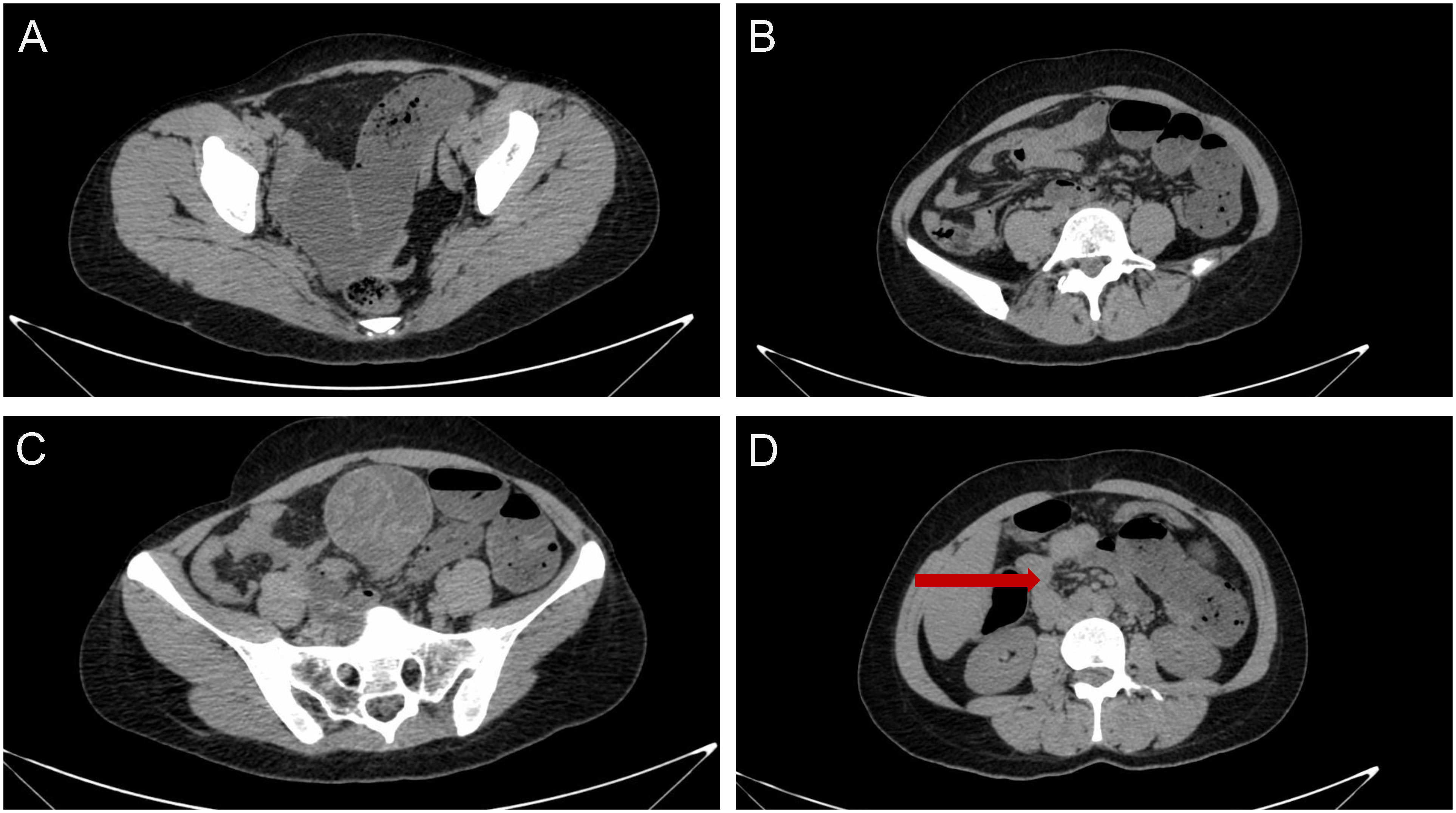
Figure 1 Computed tomography of the abdomen and pelvis indicated (A, B) dilated proximal bowel loops and multiple air-fluid levels due to (C) a 6.1 × 5.7-cm, approximately spherical, well-delineated heterogeneous cystic and hyperdense jejunal mass and (D) mild intestinal volvulus, without indicators of intestinal ischemia or necrosis.
The preliminary suspected diagnosis of SBO due to a jejunal tumor and mild intestinal volvulus was established by above clinical findings. The physical condition of the patient was optimized and elective laparoscopic exploration was then scheduled for her (12). Intraoperatively, a solitary jejunal mass was found to be the possible lead point of intestinal volvulus and subsequent SBO. Therefore, laparoscopy-assisted resection surgery was performed according to the following steps (13, 14): (1) adhesionlysis and complete mobilization of the intra-abdominal mass; (2) extracorporeal resection with wide surgical margin of the mass and segmental jejunum (15); (3) primary side-to-side jejunojejunostomy; (4) check for a safe anastomosis and no intestinal volvulus under laparoscopy (16); (5) peritoneal irrigation and drainage placement (Supplementary Material Figure S1; Supplementary Material Video S1). The procedure lasted 115 minutes, with estimated blood loss of 20 ml.
Gross examination of the resected specimen demonstrated a 6 × 6 × 5 cm in dimension, approximately spherical mass of fibrous hyperplasia adherent to the jejunal wall, which contained a 20 × 20-cm surgical gauze (Figure 2). Given potential medicolegal consequences, histopathologic examination was not conducted. Because of the possibility of negative result under effective antibiotics treatment preoperatively, the gauze was not sent to bacteriology examination. Postoperatively, the patient was transferred back to the general medical ward. Complying with the pathway of enhanced recovery after surgery, the course of postoperative rehabilitation was uneventful, with first flatus on postoperative day (POD) 1 and oral feeding beginning on POD 2. The patient was discharged on POD 6 without any complications. So far, the regular follow-up of 9 months has been unremarkable. The timeline with corresponding clinical data from the period of care is shown in Figure 3.
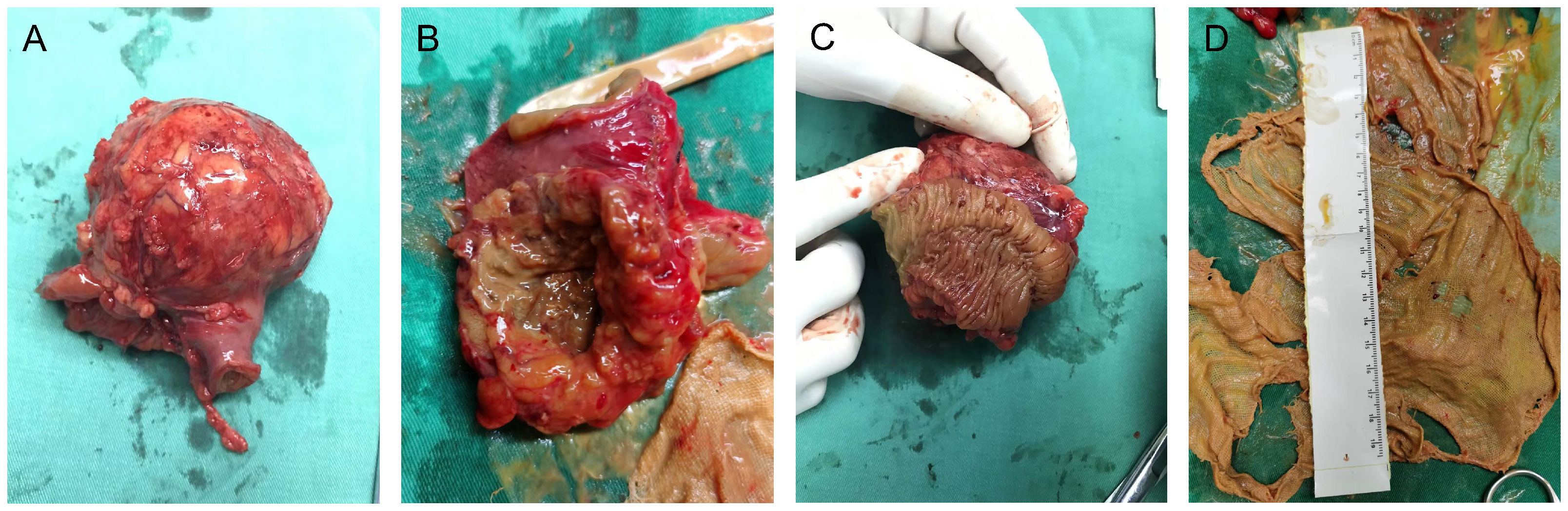
Figure 2 Gross examination of the surgical specimen demonstrated a 6 × 6 × 5-cm, approximately spherical mass of fibrous hyperplasia adherent to the jejunal wall (A–C), which contained a 20 × 20-cm gauze (D).
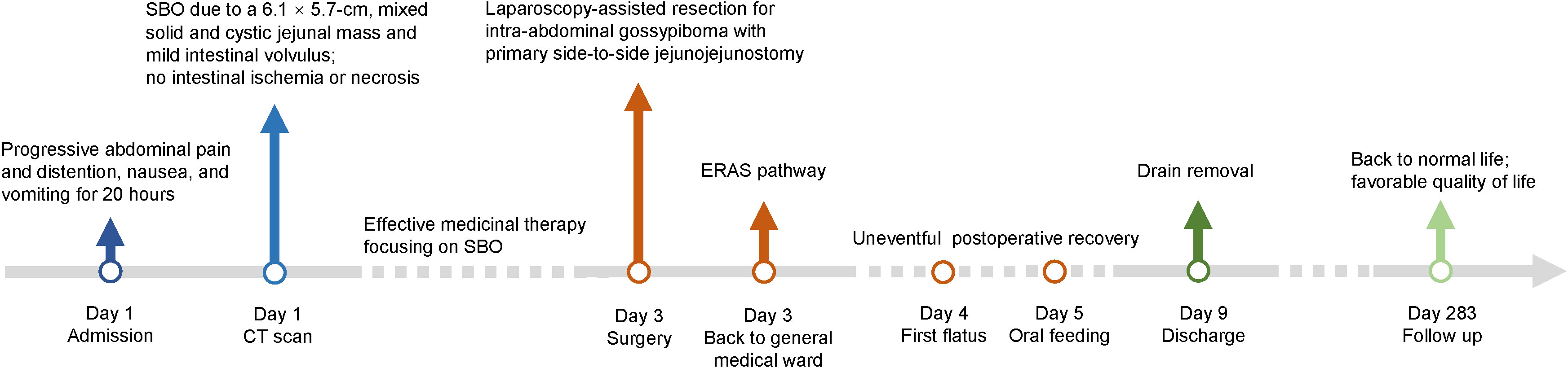
Figure 3 Timeline of the case presentation with relevant data from the episode of care. SBO, small bowel obstruction; CT, computed tomography; ERAS, enhanced recovery after surgery.
A systematic literature search was conducted in the PubMed database utilizing medical subject headings and text words related to “intra-abdominal gossypiboma” to acquire relevant case reports published till October 13, 2023. The search strategy and syntax for PubMed database are shown in Supplementary material Table S1. The studies with initial misdiagnosis as intra-abdominal tumor met the eligible criteria. Systematic reviews, case series with unavailable individual patient data, and articles with non-English languages or animal subjects were excluded. The general characteristics of the enrolled studies were extracted and entered into a preplanned electronic form (Table 1). The pooled data were summarized in a narrative and descriptive way.

Table 1 General characteristics of the included case reports regarding intra-abdominal gossypiboma with initially suspected diagnosis as tumor.
As a result, 233 articles were screened for further potential. Then, 20 cases with intra-abdominal gossypibomas which were initially misdiagnosed as tumors in 19 literature (between 1979 to 2023) met the inclusion criteria (17–35). Overall, the relevant case reports focusing on this special population emerged rapidly in the past decade. These events of initial misdiagnosis proved to occur mostly in Asian countries (15/19), especially Turkey. Despite the risk of publication bias, relatively insufficient healthcare resources in transitioning economies could definitely contribute to higher incurrence rate of intra-abdominal gossypiboma to some extent. Female patients accounted for 75% of the included cases (15/20). Previous obstetrics and gynecology surgery remained the leading cause of intra-abdominal gossypiboma (9/20), followed by open cholecystectomy (4/20), gastrectomy (4/20), urinary operations (2/20), and other laparotomies. The interval between the previous procedures to the present diagnosis of intra-abdominal gossypiboma ranged from 2 months to 40 years. The most common diagnostic tools were CT and ultrasonography (US). In terms of tumor, the predominant misdiagnosis for these patients as well as our reported case was gastrointestinal stromal tumor (GIST).
The optimal approach to dealing with this iatrogenic surgical complication is prevention. For surgeries associated with high risk of retained surgical sponge (RSS) as mentioned above, repeated sponge counting at the key time point (such as beginning and ending of the operation, handover of surgical team, closure of the peritoneum, and every 3 hours) should be advocated and emphasized (2). All the surgeons, assistants, and operating theater nurses should take a meticulous and responsible attitude towards the patient’s life and postoperative quality of life. On the other hand, the application of radiopaque marker and quick response code within the surgical sponge is highly advisable (36–38). However, routinely postoperative plain films to identify RSS is not recommended. Small sponges should be abandoned during laparotomy while surgical compresses should be employed only intraperitoneally and one by one. A thorough intraperitoneal exploration prior to closure of the peritoneum is also crucial to minimize the risk of RSS. In a word, the prevention of RSS requires a high sense of responsibility, standardized clinical practice, diversified knowledge, and shared information.
As mentioned above, intra-abdominal gossypibomas are associated with unpredictable clinical presentations and the possibility of a long interval between the previous surgery and current episode (9). It may be discovered most frequently by a different surgeon rather than the one who did the previous procedure. It is critical for clinicians to hold a high index of suspicion of intra-abdominal gossypiboma when evaluating the episode of new symptoms in these patients with a distant history of high-risk laparotomy. Radiologic examinations (including CT, US, and MRI) can help establish preliminary diagnosis (10). For intra-abdominal gossypiboma presenting as a mass, the common differential diagnoses include GIST, tumor of the small bowel and colon, retroperitoneal tumor, and intra-abdominal abscess. Noticeably, the gossypiboma and abscess can co-exist in the same patient. The role of percutaneous biopsy under the guidance of US or CT and histopathologic examination in the diagnosis of an intra-abdominal mass should be emphasized, once a malignancy tumor cannot be ruled out (27).
Furthermore, gastrointestinal endoscopy, as well as cystoscopy and ureteroscopy, can be applied to identify transmural migration and sometimes remove the RSS (32, 39). For a long time, redo exploratory laparotomy remains the frequent and vital method to finally confirm the diagnosis and treat this specific patient population. However, with minimal invasion and improved visualization, laparoscopic and robotic-assisted approaches have been placed high hopes in the management of intra-abdominal gossypiboma, especially with preoperatively ambiguous diagnosis (40, 41).
In conclusion, our case report accentuates the need for clinicians to maintain an elevated awareness and suspicion of gossypiboma when evaluating an intra-abdominal mass, especially in patients with a prior history of high-risk laparotomy. Laparoscopic surgery stands out as a technically proficient and minimally invasive strategy for diagnosing and treating intra-abdominal gossypiboma.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Biomedical Ethical Committee of West China Hospital, Sichuan University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
YH: Writing – original draft, Project administration. WY: Writing – original draft, Project administration. WD: Writing – original draft. QM: Writing – review & editing, Data curation, Investigation, Visualization. TY: Writing – review & editing, Formal Analysis, Software. YY: Writing – review & editing, Formal Analysis, Software. YL: Writing – review & editing, Supervision. BZ: Supervision, Writing – review & editing, Conceptualization, Funding acquisition, Methodology. MZ: Supervision, Writing – review & editing, Conceptualization, Funding acquisition, Methodology.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was funded by the 1·3·5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (Grant No. ZYJC18034 and ZYJC21021) and Sichuan Provincial Administration of Traditional Chinese Medicine (Grant No. 2023MS173).
We would like to thank all the staff from Department of Anesthesiology & Operation Room, West China Shangjin Hospital, Sichuan University for their professional and kind support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2023.1326032/full#supplementary-material
Supplementary Figure 1 | The flow diagram of the surgical procedure, extracorporeal resection of the mass and segmental jejunum with primary side-to-side jejunojejunostomy.
Supplementary Video 1 | Laparoscopy-assisted resection for intra-abdominal gossypiboma masquerading as a jejunal tumor.
2. Lauwers PR, Van Hee RH. Intraperitoneal gossypibomas: the need to count sponges. World J Surg (2000) 24:521–7. doi: 10.1007/s002689910084
3. Gawande AA, Studdert DM, Orav EJ, Brennan TA, Zinner MJ. Risk factors for retained instruments and sponges after surgery. N Engl J Med (2003) 348:229–35. doi: 10.1056/NEJMsa021721
4. Yakar A, Atacan SÇ, Yakar F, Ziyade N, Gündoğmuş ÜN. Medicolegal consequences of thoracic gossypiboma: a case report. J Forensic Leg Med (2016) 42:65–7. doi: 10.1016/j.jflm.2016.05.010
5. Bani-Hani KE, Gharaibeh KA, Yaghan RJ. Retained surgical sponges (gossypiboma). Asian J Surg (2005) 28:109–15. doi: 10.1016/s1015-9584(09)60273-6
6. Lincourt AE, Harrell A, Cristiano J, Sechrist C, Kercher K, Heniford BT. Retained foreign bodies after surgery. J Surg Res (2007) 138:170–4. doi: 10.1016/j.jss.2006.08.001
7. Gibbs VC. Retained surgical items and minimally invasive surgery. World J Surg (2011) 35:1532–9. doi: 10.1007/s00268-011-1060-4
8. Ryan G, Kawka M, Gnananandan J, Yip V. Presentation and surgical management of a gossypiboma presenting with small bowel obstruction. Clin J Gastroenterol (2021) 14:1067–70. doi: 10.1007/s12328-021-01400-y
9. Sozutek A, Colak T, Reyhan E, Turkmenoglu O, Akpınar E. Intra-abdominal gossypiboma revisited: Various clinical presentations and treatments of this potential complication. Indian J Surg (2015) 77:1295–300. doi: 10.1007/s12262-015-1280-1
10. Manzella A, Filho PB, Albuquerque E, Farias F, Kaercher J. Imaging of gossypibomas: pictorial review. AJR Am J Roentgenol (2009) 193:S94–101. doi: 10.2214/AJR.07.7132
11. Riley DS, Barber MS, Kienle GS, Aronson JK, von Schoen-Angerer T, Tugwell P, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol (2017) 89:218–35. doi: 10.1016/j.jclinepi.2017.04.026
12. Liu K, Chen X-Z, Zhang W-H, Zhang D-Y, Luo Y, Yu Y, et al. “Four-Step Procedure” of laparoscopic exploration for gastric cancer in West China Hospital: a retrospective observational analysis from a high-volume institution in China. Surg Endosc (2019) 33:1674–82. doi: 10.1007/s00464-018-6605-2
13. Hu J, Or BHN, Hu K, Wang ML. Comparison of the post-operative outcomes and survival of laparoscopic versus open resections for gastric gastrointestinal stromal tumors: A multi-center prospective cohort study. Int J Surg Lond Engl (2016) 33 Pt A:65–71. doi: 10.1016/j.ijsu.2016.07.064
14. Xiong Z, Wan W, Zeng X, Liu W, Wang T, Zhang R, et al. Laparoscopic versus open surgery for gastric gastrointestinal stromal tumors: A propensity score matching analysis. J Gastrointest Surg (2020) 24:1785–94. doi: 10.1007/s11605-019-04318-6
15. Åhlén J, Karlsson F, Wejde J, Nilsson I-L, Larsson C, Bränström R. Wide surgical margin improves the outcome for patients with gastrointestinal stromal tumors (GISTs). World J Surg (2018) 42:2512–21. doi: 10.1007/s00268-018-4498-9
16. Hwang RF, Swartz DE, Felix EL. Causes of small bowel obstruction after laparoscopic gastric bypass. Surg Endosc (2004) 18:1631–5. doi: 10.1007/s00464-004-8804-2
17. Jason RS, Chisolm A, Lubetsky HW. Retained surgical sponge simulating a pancreatic mass. J Natl Med Assoc (1979) 71:501–3.
18. Cheng T-C, Chou AS-B, Jeng C-M, Chang P-Y, Lee C-C. Computed tomography findings of gossypiboma. J Chin Med Assoc (2007) 70:565–9. doi: 10.1016/S1726-4901(08)70063-7
19. Yamamura N, Nakajima K, Takahashi T, Uemura M, Nishitani A, Souma Y, et al. Intra-abdominal textiloma. A retained surgical sponge mimicking a gastric gastrointestinal stromal tumor: report of a case. Surg Today (2008) 38:552–4. doi: 10.1007/s00595-007-3654-x
20. Akbulut S, Arikanoglu Z, Yagmur Y, Basbug M. Gossypibomas mimicking a splenic hydatid cyst and ileal tumor: a case report and literature review. J Gastrointest Surg (2011) 15:2101–7. doi: 10.1007/s11605-011-1592-9
21. Buluş H, Şımşek G, Coşkun A, Koyuncu A. Intraabdominal gossypiboma mimicking gastrointestinal stromal tumor: a case report. Turk J Gastroenterol (2011) 22:534–6. doi: 10.4318/tjg.2011.0269
22. Cheon JW, Kim EY, Kim KY, Park JB, Shin YK, Kim KY, et al. A case of gossypiboma masquerading as a gastrointestinal stromal tumor. Clin Endosc (2011) 44:51–4. doi: 10.5946/ce.2011.44.1.51
23. Kawamura Y, Ogasawara N, Yamamoto S, Sasaki M, Kawamura N, Izawa S, et al. Gossypiboma mimicking gastrointestinal stromal tumor causing intestinal obstruction: a case report. Case Rep Gastroenterol (2012) 6:232–7. doi: 10.1159/000338833
24. Shen H-P, Tseng C-J, Lin L-Y, Lin Y-H, Chen H-Y, Ying T-H, et al. Retroperitoneal gossypiboma 25 years after abdominal hysterectomy. Taiwan J Obstet Gynecol (2012) 51:460–2. doi: 10.1016/j.tjog.2012.07.030
25. George AJP, Mukha RP, Kekre NS. Gossypiboma mimicking a retroperitoneal tumor. Urology (2014) 84:e13–14. doi: 10.1016/j.urology.2014.06.018
26. Eken H, Soyturk M, Balci G, Firat D, Cimen O, Karakose O, et al. Gossypiboma mimicking a mesenchymal tumor: A report of a rare case. Am J Case Rep (2016) 17:27–30. doi: 10.12659/ajcr.896717
27. Singla N, Haddad AQ, Cefalu C, Margulis V. Gossypiboma manifesting as urachal mass. Rev Urol (2016) 18:239–41. doi: 10.3909/riu0703
28. Nishimura N, Mizuno M, Shimodate Y, Doi A, Mouri H, Matsueda K, et al. Gossypiboma with bleeding from fistula to the colon observed by colonoscopy. Clin J Gastroenterol (2017) 10:37–40. doi: 10.1007/s12328-016-0699-7
29. Zhang H, Jiang Y, Wang Q, Liu J. Lower abdominal gossypiboma mimics ovarian teratoma: a case report and review of the literature. World J Surg Oncol (2017) 15:6. doi: 10.1186/s12957-016-1082-3
30. Oran E, Yetkin G, Aygün N, Celayir F, Uludağ M. Intraabdominal gossypiboma: Report of two cases. Turk J Surg (2018) 34:77–9. doi: 10.5152/turkjsurg.2017.3147
31. Arıkan Y, Ozdemir O, Seker KG, Eksi M, Guner E, Kalfazade N, et al. Gossypiboma: A dramatic result of human error, case report and literature review. Prague Med Rep (2019) 120:144–9. doi: 10.14712/23362936.2019.20
32. Boghratian AH, Al-Taee AM. Gossypiboma masquerading as small bowel Malignancy. Middle East J Dig Dis (2020) 12:123–5. doi: 10.34172/mejdd.2020.172
33. Celik H, Akin IB, Altay C, Bisgin T, Obuz F. Giant gossypiboma presenting as a pelvic mass. Radiol Case Rep (2021) 16:3308–10. doi: 10.1016/j.radcr.2021.07.075
34. Hajri A, Touimi KB, El Berni Y, Erguibi D, Boufettal R, Rifki Jai S, et al. Abdominal textiloma mimicking as gastrointestinal stromal tumor: a case report. Ann Med Surg (2021) 70:102795. doi: 10.1016/j.amsu.2021.102795
35. Modrzejewski A, Kaźmierczak KM, Kowalik K, Grochal I. Surgical items retained in the abdominal cavity in diagnostic imaging tests: a series of 10 cases and literature review. Pol J Radiol (2023) 88:e264–9. doi: 10.5114/pjr.2023.127668
36. Fabian CE. Electronic tagging of surgical sponges to prevent their accidental retention. Surgery (2005) 137:298–301. doi: 10.1016/j.surg.2004.10.003
37. Greenberg CC, Diaz-Flores R, Lipsitz SR, Regenbogen SE, Mulholland L, Mearn F, et al. Bar-coding surgical sponges to improve safety: a randomized controlled trial. Ann Surg (2008) 247:612–6. doi: 10.1097/SLA.0b013e3181656cd5
38. Cima RR, Kollengode A, Clark J, Pool S, Weisbrod C, Amstutz GJ, et al. Using a data-matrix-coded sponge counting system across a surgical practice: impact after 18 months. Jt Comm J Qual Patient Saf (2011) 37:51–8. doi: 10.1016/s1553-7250(11)37007-9
39. Enebe JT, Ilo CA, Ofor IJ, Chukwubuike KE, Omeke CA, Udeozor NV, et al. Gossypiboma: Spontaneous trans-urethral migration of a forgotten surgical gauze sponge 5 years post hysterectomy in grand multiparous post-menopausal woman. Int J Surg Case Rep (2020) 71:168–71. doi: 10.1016/j.ijscr.2020.04.104
40. Târcoveanu E, Dimofte G, Georgescu S, Vasilescu A, Lupaşcu C, Bradea C, et al. Laparoscopic retrieval of gossypibomas–short series and review of literature. Acta Chir Belg (2011) 111:366–9. doi: 10.1080/00015458.2011.11680774
Keywords: intra-abdominal gossypiboma, tumor, iatrogenic complication, differential diagnosis, laparoscopic surgery
Citation: Han Y, Yang W, Dai W, Ma Q, Yuan T, Yang Y, Lu Y, Zhang B and Zhang M (2023) Case Report: Laparoscopy-assisted resection for intra-abdominal gossypiboma masquerading as a jejunal tumor (with video). Front. Oncol. 13:1326032. doi: 10.3389/fonc.2023.1326032
Received: 22 October 2023; Accepted: 10 November 2023;
Published: 28 November 2023.
Edited by:
Pasquale Cianci, Azienda Sanitaria Localedella Provincia di Barletta Andri Trani (ASL BT), ItalyReviewed by:
Jiaxin Li, People’s Hospital of Dafang County, ChinaCopyright © 2023 Han, Yang, Dai, Ma, Yuan, Yang, Lu, Zhang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingming Zhang, bW16aGFuZ21kQDE2My5jb20=; Bo Zhang, emhhbmdib19zY3VAc2N1LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.