
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol., 29 November 2023
Sec. Surgical Oncology
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.1268190
This article is part of the Research TopicSurgical Oncology in the Elderly: The State of the Art and Future Challenges - Vol. IIView all 5 articles
 Alberto Friziero1
Alberto Friziero1 Cosimo Sperti2*
Cosimo Sperti2* Federica Riccio1
Federica Riccio1 Irene Sole Zuin1
Irene Sole Zuin1 Lorenzo Vallese1
Lorenzo Vallese1 Simone Serafini1
Simone Serafini1 Alessandra Amico1
Alessandra Amico1 Valeria Valli1
Valeria Valli1 Chiara Da Re1
Chiara Da Re1 Nicola Baldan1
Nicola Baldan1 Michele Valmasoni1
Michele Valmasoni1 Gianfranco Da Dalt1
Gianfranco Da Dalt1Background: Surgical oncological emergencies represent a frequent challenge in acute settings, with postoperative courses characterized by high morbidity and mortality. An accurate selection of patients who could benefit from surgery is essential to avoid unnecessary invasive treatment. In this study, we tried to determine if advanced age (>80 years) represents a risk factor for negative short-term outcome in patients undergoing emergency surgery for acute abdominal oncological illness.
Methods: We retrospectively analyzed the records of patients who underwent emergency oncological surgery at the Department of Acute Care Surgery of Padua General Hospital from January 2018 to December 2022. One hundred two cancer patients were included in the study. Among them, 42 were aged ≥80 years (41%). Multiple preoperative and postoperative parameters were recorded, and the follow-up period was at least 90 days. Multivariate logistic regression analyses were used to identify factors associated with short-term postoperative outcomes.
Results: In the octogenarian group, 30-day mortality was 11% vs. 9.5% in the younger group [p = not significant (ns)] and 90-day mortality was 17.6% in the octogenarian group vs. 20.5% in the younger group (p = ns). Postoperative morbidity and hospital length of stay were not significantly different in the two groups. Low albumin levels [odds ratio (OR) 30.6, 9.51–87.07] and elevated lactate dehydrogenase (LDH) levels (OR 26.4, 9.18–75.83) were predictive for short-term mortality in surgical oncological emergencies.
Conclusion: Advanced age is not a risk factor for negative outcomes in surgical oncological emergencies. Therefore, surgical options should be considered in octogenarians with oncological emergencies and acceptable clinical conditions. Serum albumin levels and LDH can help predict the postoperative outcome after surgery for oncological emergencies.
An oncologic emergency may be defined as an acute life-threatening condition that has developed directly or indirectly as a result of cancer or cancer treatment (1). Perforation, occlusion, and gastrointestinal bleeding are the most common abdominal surgical emergencies in cancer patients (2). Decisions regarding treatment in emergencies are often not easy to make. In the absence of specific guidelines, the optimal method for objective evaluation and decision-making would be discussed in a multidisciplinary cancer conference. This makes surgical oncological emergency one of the most critical scenarios for acute care surgeons (3). It is essential to define the prognosis of both emergency and the cancer stage and to consider the patient’s performance score when deciding on the treatment.
The octogenarian population is expanding in industrialized countries, and at this point, the acute care surgery segment is growing. Emergency general surgery operations in elderly patients are overall associated with significant morbidity and mortality owing to underlying frailty, comorbidities, and reduced physiological reserve. It is known that older patients, in particular octogenarians, have poorer outcomes, with up to 44% mortality reported (4, 5).
In contrast, the only few studies focused on surgical oncological emergencies did not report chronological age as a predictive factor for negative surgical outcomes (6, 7).
The purpose of this retrospective study was first to investigate the outcome of octogenarian patients who underwent emergency operations for oncological acute illnesses in our institution and second to identify preoperative patient-related factors predicting postoperative mortality. As the geriatric population increases, we think that it is important to analyze if this parameter has a relevant influence on postoperative outcomes in older surgical patients presenting with acute malignancy-related symptoms.
Between January 2018 and December 2022, 102 patients underwent emergent surgery at our institution for abdominal oncologic emergencies. Patients were divided into two groups: the octogenarian group (OG) (n = 42), consisting of patients aged 80 or older, and the younger group (YG) (n = 60), consisting of patients under 80 years of age (Figure 1).
Inclusion criteria for the study were as follows: (i) age ≥18 years old; surgery for abdominal oncologic emergency for (ii) symptoms caused by any type of solid malignant disease (including primary onset) or for (iii) symptoms caused by current or previous cancer treatment (previous surgery, radiation therapy, chemotherapy, or drug-targeted therapy). Patients requiring emergency surgery for causes that could not be related directly to malignant disease or cancer treatment were excluded from the analysis (i.e., adherences or incisional hernias due to previous surgery). Finally, immunocompromised or hematological patients were excluded.
The two groups were compared in terms of (i) demographic characteristics, (ii) preexisting comorbidity, (iii) patient’s performance and functional status, (iv) cancer history, (v) preoperative laboratory tests, (vi) surgical procedure, and (vii) postoperative outcomes.
Comorbidity status before the emergency consultation was determined by Charlson Comorbidity Index (CCI) (8, 9). Performance status was assessed by the Eastern Cooperative Oncology Group performance score (ECOG-PS) (10), and functional status was determined by the American Society of Anesthesiologists (ASA) and divided in different physical status classes 1, 2, 3, or 4 (11). Cancer histology, chemotherapy treatments before surgery, and last oncological status based on RECIST criteria (12) were recorded for each patient.
The following biochemical lab tests and inflammatory markers were analyzed: serum leukocyte count, C-reactive protein (CRP), hemoglobin, creatinine, albumin, and lactate dehydrogenase (LDH). Systemic inflammatory response syndrome (SIRS) criteria were obtained (13, 14).
The indications for surgery were classified into the three most common surgical oncological emergencies (obstruction, visceral perforation, and gastrointestinal bleeding) (6). The intent of surgical treatment was differentiated into curative resection, defined as a tumor’s resection with pathologically confirmed negative margins and no macroscopic tumor residues, or palliative when a complete oncological resection has not been achieved.
The standardized Clavien–Dindo classification of surgical complications (15) is applied as a single and widely used tool to assess and report postoperative morbidity, and 90-day mortality was analyzed for each patient. Median follow-up was 4 months, ranging from 0 to 49 months.
Clinicopathological characteristics were expressed as medians with interquartile ranges (IQRs) as appropriate and compared using chi-square or Fisher exact test for categorical variables; the Mann–Whitney test was used for continuous variables. Cutoff scores for ECOG (10), ASA (11), and CCI (8) were obtained from previous established experiences, whereas for biochemical variables, they were calculated from the receiver operating characteristic (ROC) curve analysis. The optimal cutoff was identified as the point of intersection nearest the top left-hand corner between the ROC curve and a diagonal line drawn from the top right-hand corner to the bottom left-hand corner of the graph. Survival curves were constructed with the Kaplan–Meier method, and differences in survival curves were compared by log-rank test. Multivariate logistic regression analysis was performed to identify factors associated with 90-day mortality. This model was constructed by incorporating all of the preoperative variables that were statistically significant in the univariate analysis.
All data were processed using GraphPad Prism 9 (GraphPad Software Inc., CA, USA), and a p < 0.05 was considered significant.
This study was approved by the local institutional review board and followed local protocols in accordance with the Declaration of Helsinki.
During the study period, 102 patients were included: 47 were men (46%) and 55 were women (54%). Women were the most predominant gender in the octogenarian group (76.2%). Nearly 41% (n = 42) of the patients were aged 80 or older: 33 patients were between the ages of 80 and 89 years, and nine patients were aged 90 or older. The oldest patient was 98 years old, and the median age of the whole cohort was 75 (range 39–98).
The clinicopathological and operative features of the study population and a comparison between octogenarian and younger groups are reported in Tables 1, 2.
The most prominent type of cancer was colorectal carcinoma (77%), followed by urological (5%) and gynecological cancer (5%). Seventy patients (69%) received their first diagnosis of cancer during the first onset, and 49 (48%) had metastatic disease (Stage IV according to TNM classification) (16). Seventeen patients (16.6%) were on systemic chemotherapy at admission. Obstruction was the most frequent surgical oncological emergency, with no difference between the two groups.
The median ECOG-PS in the octogenarian group was 1 (IQR 1–1) compared with 0 (IQR 0–3) in the younger group, and this difference was statistically significant (p < 0.02). By comparing the ASA functional status in the two groups, the elderly group presented a significantly higher number of patients with ASA class 3 (IQR 3–3) compared to that in the younger group (p = 0.002). In contrast, there was no statistically significant difference concerning the CCI.
By analyzing clinical and laboratory data upon first presentation, we found that approximately 20% of all patients met SIRS criteria, with no significant differences between elderly and non-elderly patients.
Indications for surgery, type of operation, and outcome are reported in Tables 2, 3. The most frequently performed procedure was left hemicolectomy (30%), and laparoscopy was performed in only 31 patients, most of them in the younger group (p = 0.03). Curative resections were achieved in approximately half of the patients, with no statistically significant difference between octogenarian and younger patients.
The overall morbidity was the same in the two groups (40% vs. 46%), mostly represented by postoperative ileus and wound infections. The most frequent major morbidity (Clavien–Dindo ≥3b) was anastomotic leak, with a similar rate in the two groups (19% vs. 26%). Even if not statistically significant (p=0.09), it is to underline that the complication and major morbidity rates were higher in the younger group.
Median overall survival was 17 (IQR 6.8–25) months, with 30-day mortality and 90-day mortality rates of 21% and 38%, respectively. There were no statistically significant differences between the two groups (Figure 2).
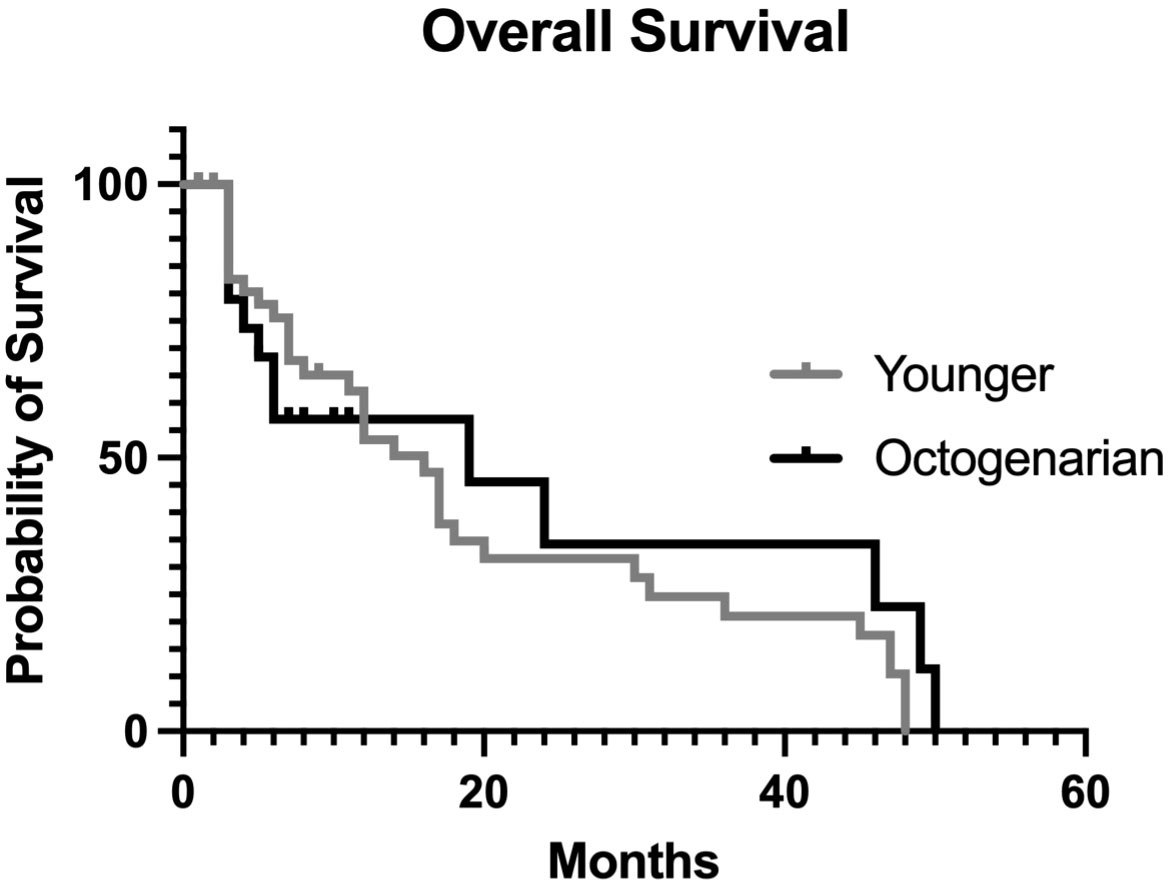
Figure 2 Overall actuarial survival curves comparing patients under 80 years to patients aged >80 years.
From our analysis, the most prominent cause of death was cancer progression, followed by postoperative surgical complications. Death due to medical complications (cardiovascular, pulmonary, renal, or infectious) associated with 30- and 90-day mortality was lower than 10% of the total, without any statistical difference between the younger and the octogenarian group (Table 4).
Two biomarkers were examined, and ROC curve analysis was set to identify the optimal cutoff values for albumin and LDH. The optimal cutoff values were as follows: 27.5 for albumin (AUC 0.88, sensitivity 92%, specificity 84%) and 202 for LDH (AUC 0.90, sensitivity 86%, specificity 84%) (Figures 3, 4).
The univariate and multivariate analyses of 90-day mortality are shown in Table 5. There was a statistically significant association between mortality and ECOG-PS >0 (p = 0.0001), CCI >6 (p = 0.008), creatinine level >78 µmol/L (p = 0.005), albumin <27.5 g/L (p < 0.0001), LDH >202 U/L (p < 0.0001), CRP >23.5 mg/L (p = 0.0002), presence of SIRS syndrome (p = 0.0003), cancer progression (p < 0.0001), metastatic disease (p = 0.0002), and past chemotherapy treatment (p = 0.002). All of these variables were included in the multivariate analysis. Albumin level <27.5 g/L and raised LDH >202 U/L remained as independent predictors of 90-day mortality.
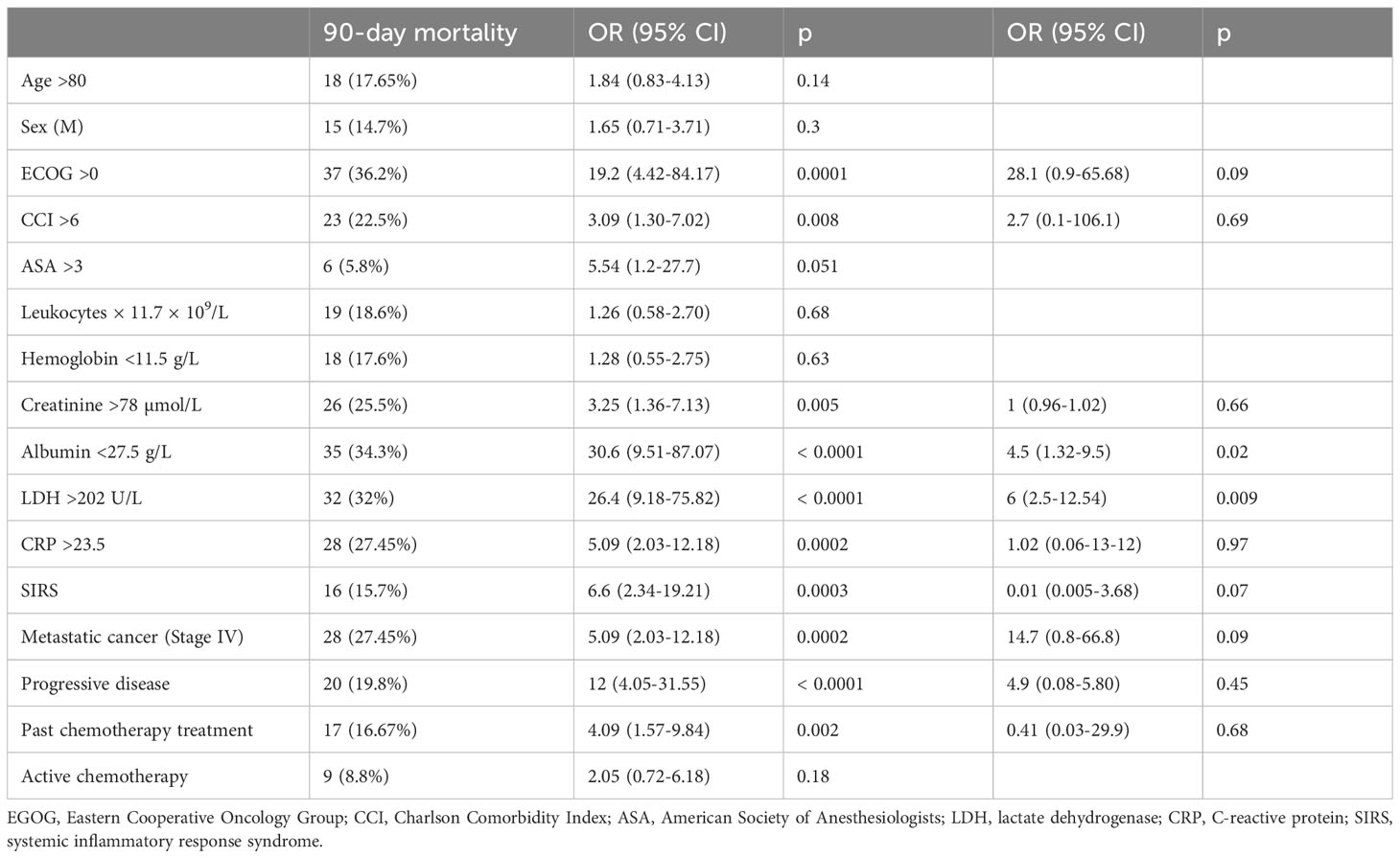
Table 5 Univariate and multivariate analyses of preoperative factors associated with 90-day mortality.
The present study aimed to evaluate the outcome after surgery for oncological emergencies in 102 patients, 42 of whom (41%) were octogenarians. Despite the octogenarians presenting more comorbidities and worse performance status, which were consistent with significantly higher ASA scores and lower ECOG-PS, no significant differences were observed in terms of survival and postoperative complications. These results suggest that the prognosis of surgical oncological emergencies is probably determined by other factors as compared to other non-oncological emergencies where the physiological status plays a key role in postoperative outcomes. A proof of this concept was derived from the results of our multivariate analysis where high LDH and low albumin levels were the only predictors of short-term survival.
The main goal of surgeons when dealing with acute oncological illness is to offer the most appropriate treatment with clinical benefit and the improvement of the residual quality of life. For this, an appropriate patient selection is mandatory. Octogenarians are a particular interest group; they are frequently frail or with multiple comorbidities (17). Also, they are exposed to a higher rate of complications when compared to younger patients (18, 19). In a systematic review and meta-analysis of Kennedy et al. (20), there is strong evidence to suggest that frailty in the older population predicts postoperative mortality, morbidity, prolonged length of hospital stay, and the loss of independence.
In the report by St-Louis et al. (9), focused on emergency surgery, chronological age together with CCI, ECOG-PS, and ASA score impacted the postoperative outcome in terms of a higher rate of postoperative morbidity and mortality, but with the limit of not distinguishing between oncological and non-oncological causes. In another series, age alone is recognized as an independent risk factor for morbidity and mortality in acute care general surgery (21).
In our experience, classical markers of poor prognosis, such as metastatic disease and cancer progression, appear associated with 90-day mortality in univariate analysis, but they do not reach statistical significance as independent predictive factors. This is probably related to an adequate preoperative patient selection and an appropriate surgical procedure. Indeed, approximately half of the patients received palliative treatment finalized to solve the acute problem, avoiding overtreatment.
Similar results concern typical markers of acute inflammatory response, notoriously correlated with poor prognosis in acute care surgery (22), as CRP and SIRS, that were significantly associated with 90-day mortality in univariate but not in multivariate analysis. High serum LDH and low albumin levels are historically considered as negative predictors in cancer patients, first for their role as biomarkers of cancer metabolism and second for their relationship with cancer cachexia. However, this concept has been challenged in the last decade, redefining their role as inflammation biomarkers in cancer patients independently of malnutrition or cancer metabolism (23). Low serum albumin seems to be directly related to elevated levels of circulating pro-inflammatory cytokines (as interleukin 6) that inhibit hepatocyte synthesis (24). Moreover, inflammation increases capillary permeability, promoting the escape of serum albumin, leading to an indirect decrease of serum levels. In a Taiwanese study of 3,800 colon cancer patients, hypoalbuminemia predicted a higher rate of 30-day mortality and was associated with more common wound healing and anastomotic complications, as well as pulmonary and urinary morbidities (24). LDH tends to be positively correlated with the systemic inflammatory response in various solid malignancies (25). LDH levels increase with tumor hypoxia and necrosis and are positively correlated with abnormal activation of hypoxia-inducible factor-1 (HIF-1), an oxygen-sensitive factor, upregulated in low-oxygen tumor microenvironments. HIF-1 has been shown to exacerbate certain sepsis infection models through induction of pro-inflammatory cytokines and chemokines (26).
This evidence could explain the great relevance of LDH and albumin levels in oncological emergencies as biomarkers of cancer progression and simultaneously systemic inflammatory response. For this, the measurement of LDH and albumin levels in emergency settings could serve as objective prognostic parameters to assess the clinical outcome and define the most appropriate surgical treatment. The importance to check albumin and LDH levels as objective prognostic parameters in the emergency setting has been previously emphasized (6): in a series of 207 patients presenting surgical oncologic emergencies, raised LDH (p < 0.001) and low albumin levels (p = 0.002) were associated with 30-day and 90-day mortality, respectively.
The retrospective nature and the relatively small population sample are the main limitations of this study. Furthermore, the heterogeneous characteristics of oncological presentations do not allow to create any solid prediction model. However, we believe that this study could represent a first tread to develop a prognostic model to predict survival in patients undergoing surgical oncological emergencies.
In conclusion, oncological emergencies are becoming increasingly common. It is important that acute care surgeons consider a patient’s nutritional and functional status as well as cancer stage and future treatment options. Chronological age is important but not so crucial. Preoperative assessment of LDH and albumin levels could help to predict short-term outcomes when facing patients with oncological emergencies. Finally, the presence of a specific acute care surgery department has led to an awareness of these pathologies with the aim to improve the residual quality of life of the patients.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Department of Surgery, Oncology and Gastroenterology (Discog). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
AF: Conceptualization, Data curation, Formal Analysis, Project administration, Supervision, Writing – original draft. CS: Funding acquisition, Supervision, Writing – review & editing. FR: Conceptualization, Data curation, Formal Analysis, Writing – original draft. IZ: Writing – review & editing. LV: Conceptualization, Formal Analysis, Writing – review & editing. SS: Writing – review & editing. AA: Data curation, Validation, Writing – review & editing. VV: Validation, Writing – review & editing. CR: Investigation, Writing – review & editing. NB: Project administration, Visualization, Writing – review & editing. MV: Project administration, Supervision, Writing – review & editing. GD: Project administration, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor LS declared a past co-authorship with the authors AF, CS, and SS.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Cervantes A, Chirivella I. Oncological emergencies. Ann Oncol (2004) 15Suppl 4:iv299–306. doi: 10.1093/annonc/mdh943
2. Prenen K, Prenen H. Oncological emergencies associated with gastrointestinal tumors. Ann Gastroenterol (2015) 28(4):426–30.
3. Dumont F, Goéré D, Honoré C, Elias D. Abdominal surgical emergencies in patients with advanced cancer. J Visc Surg (2015) 152(6 Suppl):S91–6. doi: 10.1016/j.jviscsurg.2015.09.014
4. Green G, Shaikh I, Fernandes R, Wegstapel H. Emergency laparotomy in octogenarians: A 5-year study of morbidity and mortality. World J Gastrointest Surg (2013) 5(7):216–21. doi: 10.4240/wjgs.v5.i7.216
5. St-Louis E, Sudarshan M, Al-Habboubi M, El-Husseini Hassan M, Deckelbaum DL, Razek TS, et al. The outcomes of the elderly in acute care general surgery. Eur J Trauma Emerg Surg (2016) 42(1):107–13. doi: 10.1007/s00068-015-0517-9
6. Bosscher MR, Bastiaannet E, van Leeuwen BL, Hoekstra HJ. Factors associated with short-term mortality after surgical oncologic emergencies. Ann Surg Oncol (2016) 23(6):1803–14. doi: 10.1245/s10434-015-4939-8
7. Lee JS, Kwon OY, Choi HS, Hong HP, Ko YG. Serum C-reactive protein level is a predictive factor for 14-day mortality of patients with advanced cancer who present to the emergency department with acute symptoms. Acad Emerg Med (2011) 18(4):440–2. doi: 10.1111/j.1553-2712.2011.01034.x
8. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis (1987) 40(5):373–83. doi: 10.1016/0021-9681(87)90171-8
9. St-Louis E, Iqbal S, Feldman LS, Sudarshan M, Deckelbaum DL, Razek TS, et al. Using the age-adjusted Charlson comorbidity index to predict outcomes in emergency general surgery. J Trauma Acute Care Surg (2015) 78(2):318–23. doi: 10.1097/TA.0000000000000457
10. Christodolulou C, Rizos M, Galani E, Rellos K, Skarlis DV, Michalopoulos A. Performance status (PS) a simple predictor of short-term outcome of cancer patients with solid tumors admittedto the intensive unit (ICU). Anticancer Res (2007) 27(4C):2945–48.
11. Hackett NJ, De Oliveira GS, Jain UK, Kim JY. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg (2015) 18:184–90. doi: 10.1016/j.ijsu.2015.04.079
12. Schwartz LH, Litière S, de Vries E, Ford R, Gwyther S, Mandrekar S, et al. RECIST 1.1-Update and clarification: From the RECIST committee. Eur J Cancer (2016) 62:132–7. doi: 10.1016/j.ejca.2016.03.081
13. Members of the American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference committee American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference. Definition for sepsis and organ failure and guidelines for the use innovative therapies in sepsis. Crit Care Med (1992) 20:864–74. doi: 10.1097/00003246-199206000-00025
14. Gando S, Shiraishi A, Abe T, Kushimoto S, Mayumi T, Fujishima S, et al. The SIRS criteria have better performance for predicting infection than qSOFA scores in the emergency department. Sci Rep (2020) 10(1):8095. doi: 10.1038/s41598-020-64314-8
15. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg (2004) 240(2):205–13. doi: 10.1097/01.sla.0000133083.54934.ae
16. Rosen RD, Sapra A. TNM classification. [Updated 2023 feb 13]. In: StatPearls [Internet]. Treasure Island (FL: StatPearls Publishing (2023).
17. Lin HS, Watts JN, Peel NM, Hubbard RE. Frailty and postoperative outcomes in older surgical patients: a systematic review. BMC Geriatrics (2016) 16:157. doi: 10.1186/s12877-016-0329-8
18. Hajibandeh S, Hajibandeh S, Antoniou GA, Antoniou SA. Meta-analysis of mortality risk in octogenarians undergoing emergency general surgery operations. Surgery. (2021) 169(6):1407–16. doi: 10.1016/j.surg.2020.11.027
19. Fabbian F, De Giorgi A, Ferro S, Lacavalla D, Andreotti D, Ascanelli S, et al. Post-operative all-cause mortality in elderly patients undergoing abdominal emergency surgery: role of charlson comorbidity index. Healthcare (Basel). (2021) 9(7):805. doi: 10.3390/healthcare9070805
20. Kennedy CA, Shipway D, Barry K. Frailty and emergency abdominal surgery: A systematic review and meta-analysis. Surgeon (2022) 20:e307–14. doi: 10.1016/j.surge.2021.11.009
21. Mallol M, Sabaté A, Dalmau A, Koo M. Risk factors and mortality after elective and emergent laparatomies for oncological procedures in 899 patients in the intensive care unit: a retrospective observational cohort study. Patient Saf Surg (2013) 7(1):29. doi: 10.1186/1754-9493-7-29
22. Nazha B, Moussaly E, Zaarour M, Weerasinghe C, Azab B. Hypoalbuminemia in colorectal cancer prognosis: Nutritional marker or inflammatory surrogate? World J Gastrointest Surg (2015) 7(12):370–7. doi: 10.4240/wjgs.v7.i12.370
23. Fearon KC, Falconer JS, Slater C, McMillan DC, Ross JA, Preston T. Albumin synthesis rates are not decreased in hypoalbuminemic cachectic cancer patients with an ongoing acute-phase protein response. Ann Surg (1998) 227(2):249–54. doi: 10.1097/00000658-199802000-00015
24. Lai CC, You JF, Yeh CY, Chen JS, Tang R, Wang JY, et al. Low preoperative serum albumin in colon cancer: a risk factor for poor outcome. Int J Colorectal Dis (2011) 26:473–81. doi: 10.1007/s00384-010-1113-4
25. Yu SL, Xu LT, Qi Q, Geng YW, Chen H, Meng ZQ, et al. Serum lactate dehydrogenase predicts prognosis and correlates with systemic inflammatory response in patients with advanced pancreatic cancer after gemcitabine-based chemotherapy. Sci Rep (2017) 7:45194. doi: 10.1038/srep45194
Keywords: age, colectomy, colon cancer, emergency, octogenarians, surgical oncology
Citation: Friziero A, Sperti C, Riccio F, Zuin IS, Vallese L, Serafini S, Amico A, Valli V, Da Re C, Baldan N, Valmasoni M and Da Dalt G (2023) Surgical oncological emergencies in octogenarian patients. Front. Oncol. 13:1268190. doi: 10.3389/fonc.2023.1268190
Received: 27 July 2023; Accepted: 08 November 2023;
Published: 29 November 2023.
Edited by:
Luca Saadeh, University Hospital of Padua, ItalyReviewed by:
Vincenzo Schiavone, Federico II University Hospital, ItalyCopyright © 2023 Friziero, Sperti, Riccio, Zuin, Vallese, Serafini, Amico, Valli, Da Re, Baldan, Valmasoni and Da Dalt. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cosimo Sperti, Y3NwZXJ0aUBsaWJlcm8uaXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.