
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Oncol. , 27 September 2023
Sec. Surgical Oncology
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.1259508
This article is part of the Research Topic Translational Research in Surgical Applications and Spinal Tumors View all 9 articles
 Wen-Bin Xu1
Wen-Bin Xu1 Nai-Kun Sun1,2*†
Nai-Kun Sun1,2*† Di-Xin Cai1,2
Di-Xin Cai1,2 Ding-Qiang Chen2
Ding-Qiang Chen2 Yuan Niu3
Yuan Niu3 Fang Jia1
Fang Jia1 Guang-Xun Lin1,2*†
Guang-Xun Lin1,2*† Gang Rui1,2*†
Gang Rui1,2*†Background: Spinal meningioma is a common intraspinal tumor, which mainly occurs in the thoracic spine. Ossified meningioma (OSM) is an extremely rare histological variant. Our article reports a rare patient with dorsal complete OSM and reviews this subject.
Case presentation: A 68-year-old woman presented with a one-year history of progressive weakness in both lower limbs with gait disturbance. Physical examination revealed hypoesthesia with a sensory level below T10. Babinski and pathological signs on both sides were weakly positive. Magnetic resonance imaging (MRI) showed a mass at the T10 to T11 level causing severe compression of the spinal cord. Computed tomography (CT) showed complete ossification of the mass. 18F-Fluoro-deoxy-glucose positron emission tomography CT (18F-FDG PET/CT) scan combined with MRI revealed that the mass was an intradural extramedullary high-density ossified nodule. The patient underwent a gross total resection of the mass and pathologic examination indicated that the mass was a meningioma with diffused psammomatous bodies.
Conclusion: We identified a rare case of dorsal complete OSM occurring in a 68-year-old woman. After complete surgical resection, although there were complications such as cerebral fluid leakage and fever, the patient finally recovered with a satisfactory result.
Spinal meningioma accounts for about one-quarter of total primary intraspinal tumors, which is the second commonest intraspinal tumor following neurilemmoma (1). Spinal meningioma can occur in the extramedullary intradural and epidural areas, but the vast majority are intradural tumors (2). Although spinal meningioma is common clinically, calcification or ossification of spinal meningioma is uncommon, accounting for 1% to 5% of all spinal meningioma (3). Complete ossified meningioma (OSM) is extremely rare and is considered to be a rare histological variant. At present, spinal meningioma is not sensitive to radiotherapy and chemotherapy, and safe gross total resection remains the standard of care (3).
Here, a case of dorsal complete OSM is reported and the relevant subject is reviewed.
A 68-year-old woman presented with a one-year history of progressive weakness in both lower limbs with gait disturbance. Physical examination revealed normal muscle force of both lower limbs and hypoesthesia with a sensory level below T10. Babinski and pathological signs on both sides were weakly positive.
Magnetic resonance imaging (MRI) demonstrated a mass between the T10 and T11 levels causing severe compression of the spinal cord (Figure 1). Computed tomography (CT) scan revealed complete ossification of the mass (Figure 2). 18F-Fluoro-deoxy-glucose positron emission tomography CT (18F-FDG PET/CT) scan combined with MRI revealed that the mass was an intradural extramedullary high-density ossified nodule (spinal meningioma)? (Figure 3).

Figure 1 MRI demonstrated a mass between the T10 and T11 levels. (A) Axial T2-weighted image; (B) Sagittal T2-weighted image; (C) Sagittal T2-weighted image with fat-suppression.
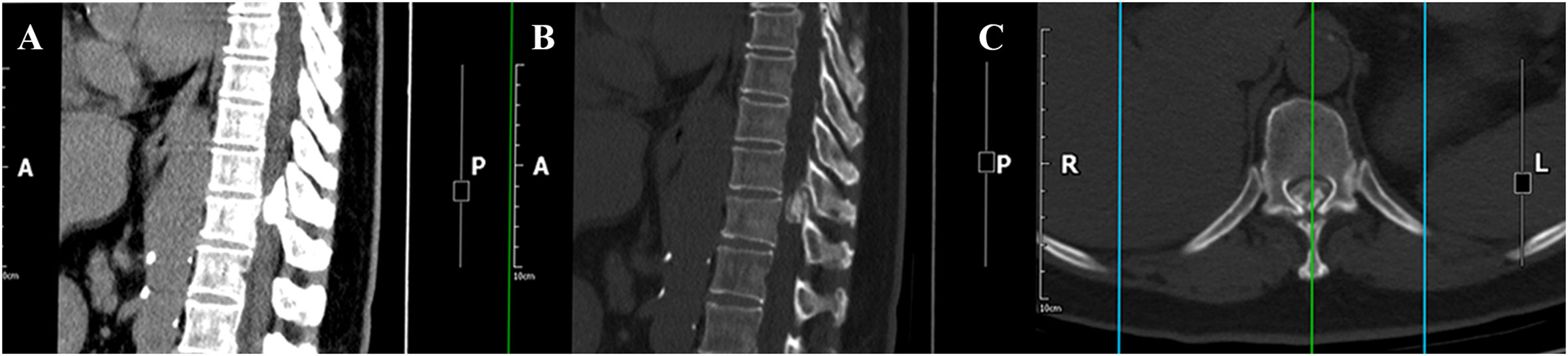
Figure 2 CT revealed complete ossification of the mass. (A) Sagittal CT image on bone window; (B) Sagittal CT image on soft-tissue window; (C) Axial CT image.
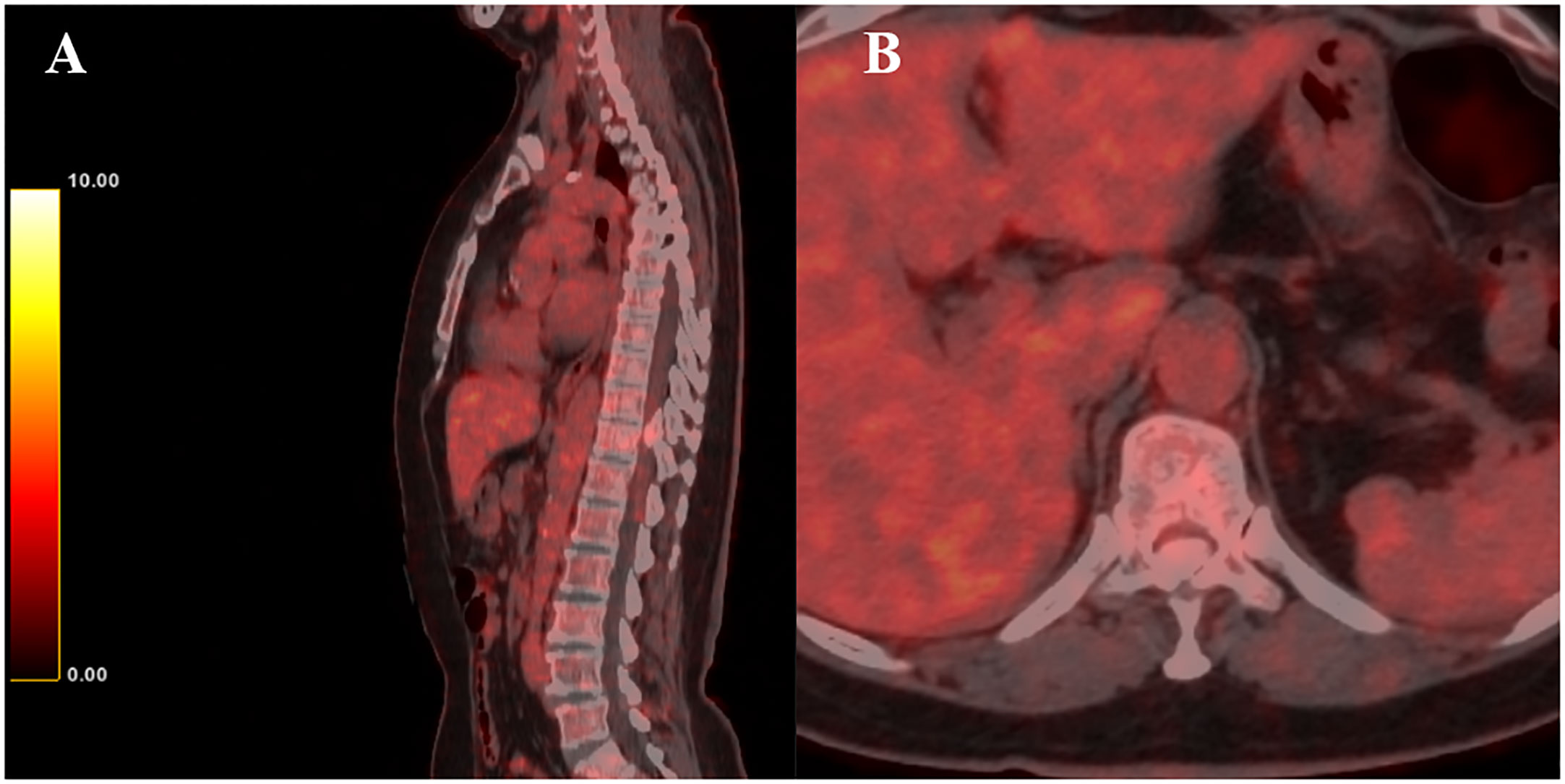
Figure 3 18F-FDG PET/CT revealed that the mass was an intradural extramedullary high-density ossified nodule. (A) Sagittal 18F-FDG PET/CT image; (B) Axial 18F-FDG PET/CT image.
Under general anesthesia, T9 to T12 transpedicular screw fixation was performed. Subsequently, the complete T10 to T11 spinous process and bilateral lamina of vertebra, and part of the spinous process and bilateral lamina of vertebra at the lower margin of T9 were removed under intraoperative neuromonitoring. Dorsal complete ossification of the intradural mass was revealed after full exposure of the dura of the corresponding segment (Figure 4). Then, the dura was cut along the edge of the mass and the mass was found to be heavily adhered to the arachnoid and spinal cord. After the careful separation between the tumor base and the adherent arachnoid, the mass was removed intact and then the dura mater was closed with a dural patch. Histopathological examination of the resected tissue revealed that the mass was a meningioma with diffused psammomatous bodies (Figure 5).
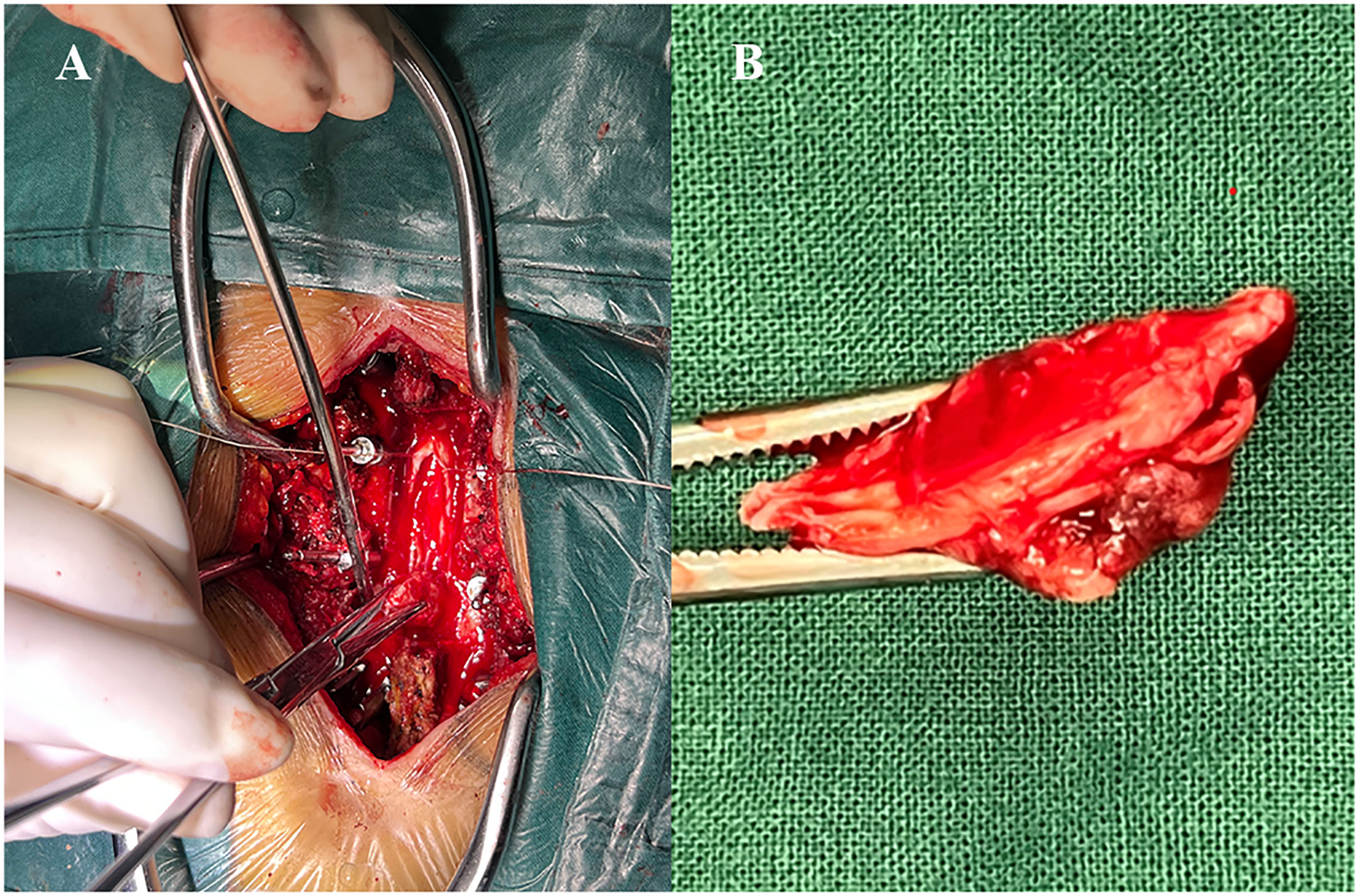
Figure 4 (A) Intraoperatively the mass was exposed by a dura incision; (B) The mass was completely resected.
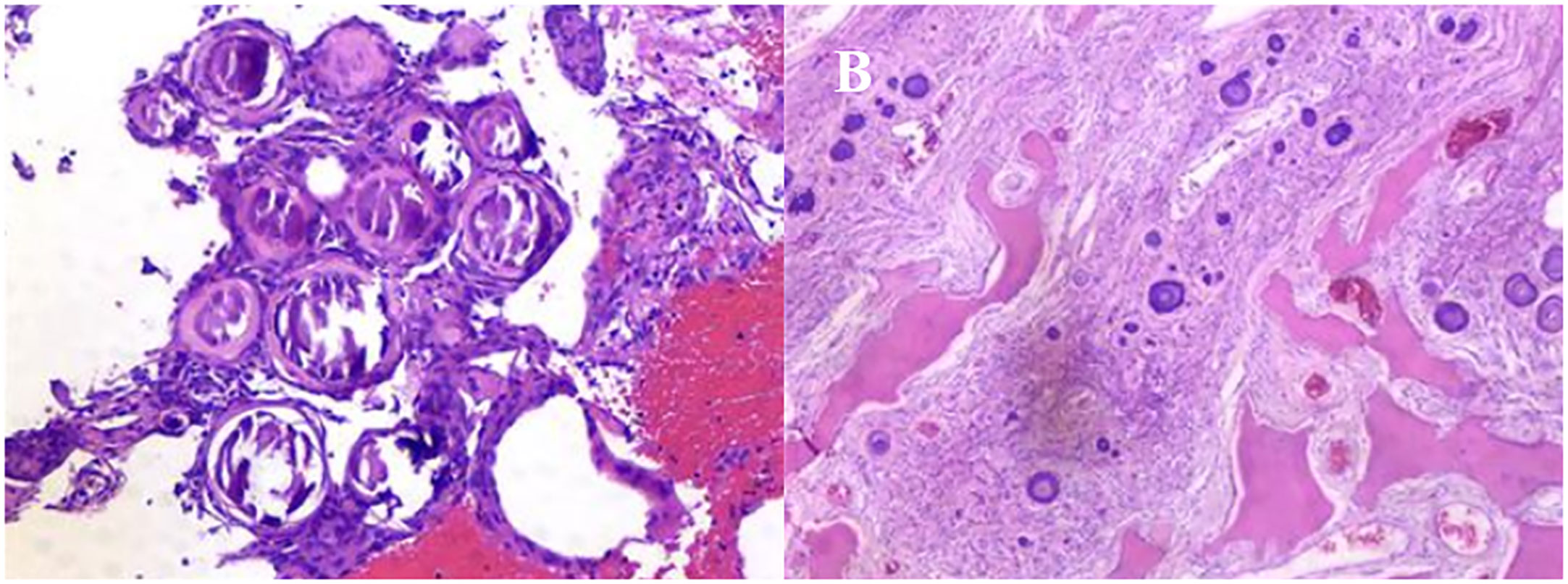
Figure 5 Histopathological examination of the resected tissue revealed that the mass was a meningioma with diffused psammomatous bodies.
The postoperative examination reported no residual mass compressing the spinal cord (Figure 6). The weakness in both lower limbs improved immediately. However, the patient was hospitalized for five weeks because of complications. This patient developed cerebral fluid leakage within three days after the operation (Day 1:300ml, Day 2: 500ml and Day 3: 450ml) because of the inevitable incision of the dura during the operation. In addition, on the 4th postoperative day, the patient began to have an unexplained low-grade fever, so the patient was treated with antibiotics (ceftriaxone sodium, vancomycin, and meropenem). Finally, the patient was discharged five weeks after the operation with a normal temperature.
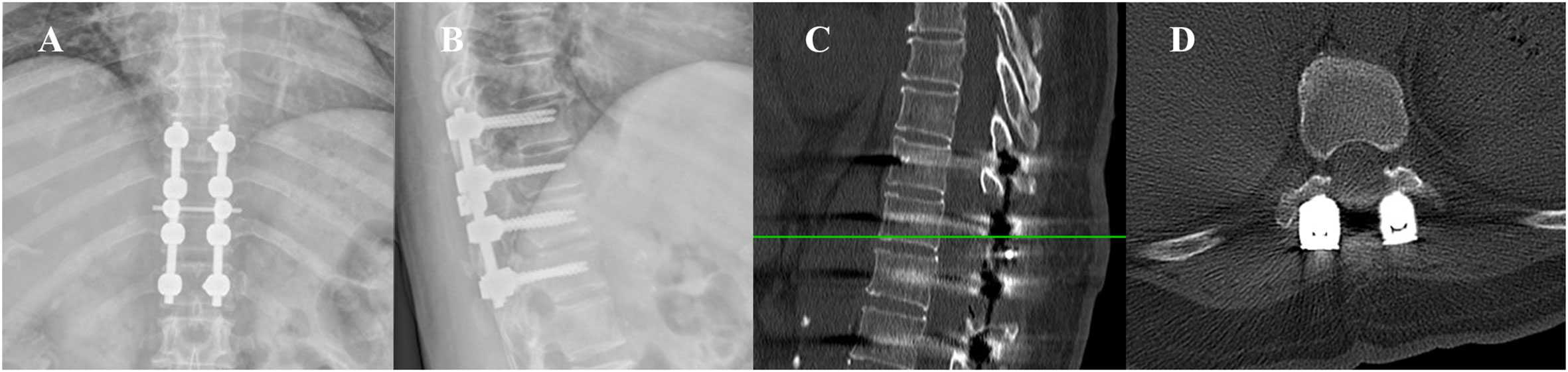
Figure 6 The postoperative examination of the patient. (A, B) DR revealed appropriate internal fixation; (C, D) CT images demonstrated no residual mass compressing the spinal cord.
According to PubMed, including the current case, altogether 34 articles (4–36) involving 43 cases have been published till 2022 (Table 1). This review indicated that the majority of OSM occur in women (female: 38, male: 5). The average age was 57.5 years (range from 15 to 90 years). Most patients with OSMs occurred in the thoracic spine (38 cases, 88.4%), followed by the cervical spine (4 cases, 9.3%) and lumbar spine (1, 2.3%). In terms of treatment, the tumors were removed in 38 cases by gross total resection (GTR), tumors in 3 cases were removed via subtotal resection (STR), and the extent of resection was not clearly described in the remaining 2 cases. The vast majority of patients improved gradually after the operation, and no recurrence (21 cases) was reported (the remaining not described).
Spinal meningioma may originate from the arachnoid cap cells originating from the outer layer of the arachnoid mater and villi (18). According to the latest WHO classification, spinal meningioma can be divided into 15 different histological subtypes, with psammomatous, meningothelial and transitional being the most common histologic variants, but the calcification or ossification of spinal meningioma is uncommon (37). The specific pathogenesis of OSM remains controversial. One theory suggests that ossification is caused by the accumulation of hydroxyapatite crystals in psammoma bodies (38). However, some articles have reported that ossification can also occur without psammoma bodies, which may not support the theory (7, 19, 28). Therefore, most of the current reports believe that ossification begins with the metaplasia of arachnoid cells, which induces the synergistic effect of osteoblast, fibroblast, and angiogenesis components in bone tissue formation, thereby promoting ossification in spinal meningioma (7, 8, 19). Another study suggested that ossification of spinal meningioma can be induced by biochemical activation of the ossification cascade or by exposure to osteoblast transformation factors such as SOX9 and Runx-2 (16).
As demonstrated in Table 1, the incidence of OSM in females is significantly higher than in males. This phenomenon may be due to estrogen deficiency which increases the risk of calcification in regions containing necrotic fibroblasts (18). However, no evidence has been found that this phenomenon is related to sex hormones (39). In addition, the incidence of OSM is higher in the elderly, and OSM in children and young adults may not be as rare as in the general population.
The most OSMs have symptomatic but nonspecific clinical manifestations. The clinical features of these tumors include motor, sensory, and sphincter dysfunction, with different phenotypes depending on tumor location and nerve compression. Interestingly, all 43 cases of OSM demonstrated progressive myelopathy and worsened with time, but most patients did not report a history of symptoms within 2 years and some cases remained asymptomatic until events such as falls occurred. Depending on the peak age of onset, the mass considered asymptomatic or mild for a long time. The mass becomes unsteady after stimulation and may cause bleeding and displacement, which displace and cause nerve compression and worsen neurological symptoms.
In terms of diagnosis, OSM can sometimes be detected in a digital radiograph (DR), small calcification or ossification can be further observed in a CT scan, and the size or extent of OSM can be determined by MRI. However, since imaging cannot distinguish ossification or calcification, the ultimate diagnosis should be determined by histopathological findings (40). In addition, 18F-FDG PET/CT is not a routine examination for the diagnosis of OSM. However, recent studies have shown that new specific tracers, such as 68Ga-DOTA-SSTR and 68Ga-DOTATOC, can improve the diagnostic accuracy of meningiomas and assist radiosurgical or surgical planning (41, 42).
Once spinal meningioma is diagnosed, surgical resection is the primary treatment, which can relieve spinal cord compression, restore limb motor function, and reduce the pain of patients. Most intradural meningiomas are epiarachnoid masses, and the arachnoid mater becomes a barrier to separate the tumor from surrounding normal tissues during surgery. However, the unique differentiation form of OSM causes calcification or ossification of the arachnoid mater, which leads to the disappearance of this natural barrier. Moreover, compared with general spinal meningioma, OSM often sticks to the surrounding nerve tissue, which may be due to its scant cellularity consisting of acellular concretions (23). Therefore, patients with OSM often lack a clear anatomical view, which increases the risk and difficulties of surgery. At present, gross total resection (GTR) of OSM is considered to be most associated with significant neurological improvement. However, some researchers believe that when trying to remove a tumor with heavy adhesion may cause spinal cord injury, subtotal resection (STR) can be selected to retain part of the mass to ensure normal spinal cord function after surgery (43). With the development of medical technology, intraoperative neurophysiological monitoring (IONM) has been applied to determine the extent of resection during intradural extramedullary tumors (44). IONM can alert the operator to prevent spinal cord or nerve root injury by the condition of sustained electromyoelectric response. In conclusion, complete surgical removal of OSM is not easy, especially in OSM with complete ossification, but it remains the best choice available.
We presented a rare patient with a dorsal complete OSM in the thoracic spine. In the current report, only 1% to 5% of spinal meningiomas present with ossification, and the majority are in women. The diagnosis of OSM can usually be correctly diagnosed by observing the neuroradiological appearances. Surgical resection is the main therapeutic method for OSM, but it is somewhat challenging because tumor adhesion can prevent complete resection. In summary, treatment with GTR or STR often leads to clinical improvement with a low risk of late recurrence.
Please contact the corresponding author if data is required.
W-BX: Conceptualization, Data curation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. N-KS: Conceptualization, Supervision, Writing – review & editing. D-XC: Validation, Visualization, Writing – original draft. D-QC: Formal Analysis, Visualization, Writing – original draft. YN: Investigation, Writing – original draft. FJ: Validation, Writing – original draft. G-XL: Conceptualization, Funding acquisition, Writing – review & editing. GR: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Writing – review & editing.
The authors declare financial support was received for the research, authorship, and/or publication of this article. This research was funded by the Natural Science Foundation of Fujian Province (No. 2020J011244) and the "Xiamen Health System Discipline Leaders and their Backup Candi-dates, Senior Management Talent Training Candidates Training Program (2021)".
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Albanese V, Platania N. Spinal intradural extramedullary tumors. Personal experience. J Neurosurg Sci (2002) 46(1):18–24.
2. Buetow MP, Buetow PC, Smirniotopoulos JG. Typical, atypical, and misleading features in meningioma. Radiographics (1991) 11(6):1087–106. doi: 10.1148/radiographics.11.6.1749851
3. Shah DS, Reddy RV, Doğruel Y, Asfour MZ, Pour-Rashidi A, Haider AS, et al. Calcified spinal meningiomas: a systematic review of clinical characteristics, treatment strategies, and outcomes. J Neurooncol (2023) 162(2):295–305. doi: 10.1007/s11060-023-04291-w
4. Rogers L. A. A spinal meningioma containing bone. Br J Surg. (1928) 15:675–7. doi: 10.1002/bjs.1800156015
5. Freidberg SR. Removal of an ossified ventral thoracic meningioma. Case report. J Neurosurg (1972) 37(6):728–30. doi: 10.3171/jns.1972.37.6.0728
6. Kandel E, Sungurov E, Morgunov V. Cerebral and two spinal meningiomas removed from the same patient. Neurosurgery (1989) 25:447–50. doi: 10.1097/00006123-198909000-00021
7. Niijima K, Huang YP, Malis LI, Sachdev VP. Ossified spinal meningioma en plaque. Spine (Phila Pa 1976) (1993) 18(15):2340–3. doi: 10.1097/00007632-199311000-00036
8. Kitagawa M, Nakamura T, Aida T, Iwasaki Y, Abe H, Nagashima K. Clinicopathologic analysis of ossification in spinal meningioma. Noshuyo Byori (1994) 11(1):115–9.
9. Nakayama N, Isu T, Asaoka K, Harata T, Hayashi S, Aoki T, et al. Two cases of ossified spinal meningioma. No Shinkei Geka (1996) 24(4):351–5.
10. Huang TY, Kochi M, Kuratsu J, Ushio Y. Intraspinal osteogenic meningioma: report of a case. J Formos Med Assoc (1999) 98(3):218–21.
11. Saito T, Arizono T, Maeda T, Terada K, Iwamoto Y. A novel technique for surgical resection of spinal meningioma. Spine (Phila Pa 1976) (2001) 26(16):1805–8. doi: 10.1097/00007632-200108150-00017
12. Naderi S, Yilmaz M, Canda T, Acar U. Ossified thoracic spinal meningioma in childhood: a case report and review of the literature. Clin Neurol Neurosurg (2001) 103(4):247–9. doi: 10.1016/S0303-8467(01)00157-3
13. Liu CL, Lai PL, Jung SM, Liao CC. Thoracic ossified meningioma and osteoporotic burst fracture: treatment with combined vertebroplasty and laminectomy without instrumentation: case report. J Neurosurg Spine (2006) 4(3):256–9. doi: 10.3171/spi.2006.4.3.256
14. Hirabayashi H, Takahashi J, Kato H, Ebara S, Takahashi H. Surgical resection without dural reconstruction of a lumbar meningioma in an elderly woman. Eur Spine J (2009) 18 Suppl 2(Suppl 2):232–5. doi: 10.1007/s00586-009-0895-y
15. Tahir M, Usmani N, Ahmad FU, Salmani S, Sharma MS. Spinal meningioma containing bone. a case report and review of literature. BMJ Case Rep (2009) 2009. doi: 10.1136/bcr.11.2008.1186
16. Uchida K, Nakajima H, Yayama T, Sato R, Kobayashi S, Mwaka ES, et al. Immunohistochemical findings of multiple ossified en plaque meningiomas in the thoracic spine. J Clin Neurosci (2009) 16(12):1660–2. doi: 10.1016/j.jocn.2009.03.013
17. Licci S, Limiti MR, Callovini GM, Bolognini A, Gammone V, Di Stefano D. Ossified spinal tumour in a 58-year-old woman with increasing paraparesis. Neuropathology (2010) 30(2):194–6. doi: 10.1111/j.1440-1789.2009.01076.x
18. Chotai SP, Mrak RE, Mutgi SA, Medhkour A. Ossification in an extra-intradural spinal meningioma-pathologic and surgical vistas. Spine J (2013) 13(12):e21–26. doi: 10.1016/j.spinee.2013.06.102
19. Ju CI, Hida K, Yamauchi T, Houkin K. Totally ossified metaplastic spinal meningioma. J Korean Neurosurg Soc (2013) 54(3):257–60. doi: 10.3340/jkns.2013.54.3.257
20. Taneoka A. Ossified thoracic spinal meningioma with hematopoiesis. A case report and review of the literature. Case Rep Clin Med (2013) 02:24–8. doi: 10.4236/crcm.2013.21007
21. Yamane K, Tanaka M, Sugimoto Y, Ichimura K, Ozaki T. Spinal metaplastic meningioma with osseous differentiation in the ventral thoracic spinal canal. Acta Med Okayama (2014) 68(5):313–6. doi: 10.18926/AMO/52901
22. Chan T-T, Lau VW-H, Chau TK-F, Lee Y-L. Ossified thoracic spinal meningioma with lamellar bone formation presented with paraparesis. J Orthopaedics Trauma Rehabil (2014) 18(2):106–9. doi: 10.1016/j.jotr.2013.06.001
23. Alafaci C, Grasso G, Granata F, Salpietro FM, Tomasello F. Ossified spinal meningiomas: Clinical and surgical features. Clin Neurol Neurosurg (2016) 142:93–7. doi: 10.1016/j.clineuro.2016.01.026
24. Demir MK, Yapıcıer Ö, Toktaş ZO, Akakın A, Yılmaz B, Konya D. Ossified-calcified intradural and extradural thoracic spinal meningioma with neural foraminal extension. Spine J (2016) 16(1):e35–37. doi: 10.1016/j.spinee.2015.08.053
25. Cochran EJ, Schlauderaff A, Rand SD, Eckardt GW, Kurpad S. Spinal osteoblastic meningioma with hematopoiesis: radiologic-pathologic correlation and review of the literature. Ann Diagn Pathol (2016) 24:30–4. doi: 10.1016/j.anndiagpath.2016.07.002
26. Xia T, Tian JW. Entirely ossified subdural meningioma in thoracic vertebral canal. Spine J (2016) 16(2):e11. doi: 10.1016/j.spinee.2015.09.005
27. Prakash A, Mishra S, Tyagi R, Attri PC, Bhatnagar A, Kansal S. Thoracic psammomatous spinal meningioma with osseous metaplasia: A very rare case report. Asian J Neurosurg (2017) 12(2):270–2. doi: 10.4103/1793-5482.150222
28. Sakamoto K, Tsutsumi S, Nonaka S, Suzuki T, Ishii H, Ito M, et al. Ossified extradural en-plaque meningioma of the cervical spine. J Clin Neurosci (2018) 50:124–6. doi: 10.1016/j.jocn.2018.01.058
29. Murakami T, Tanishima S, Takeda C, Kato S, Nagashima H. Ossified metaplastic spinal meningioma without psammomatous calcification: A case report. Yonago Acta Med (2019) 62(2):232–5. doi: 10.33160/yam.2019.06.008
30. Taha MM, Alawamry A, Abdel-Aziz HR. Ossified spinal meningioma: A case report and a review of the literature. Surg J (N Y) (2019) 5(4):e137–41. doi: 10.1055/s-0039-1697634
31. Wang C, Chen Y, Zhang L, Ma X, Chen B, Li S. Thoracic psammomatous meningioma with osseous metaplasia: a controversial diagnosis of a case report and literature review. World J Surg Oncol (2019) 17(1):150. doi: 10.1186/s12957-019-1694-5
32. Xu F, Tian Z, Qu Z, Yao L, Zou C, Han W, et al. Completely ossified thoracic intradural meningioma in an elderly patient: A case report and literature review. Med (Baltimore) (2020) 99(25):e20814. doi: 10.1097/MD.0000000000020814
33. Buchanan D, Martirosyan NL, Yang W, Buchanan RI. Thoracic meningioma with ossification: Case report. Surg Neurol Int (2021) 12:505. doi: 10.25259/SNI_643_2021
34. Wong YP, Tan GC, Mukari SAM, Palaniandy K. Heterotopic ossification in psammomatous spinal meningioma: a diagnostic controversy. Int J Clin Exp Pathol (2021) 14(5):627–32.
35. Thakur J, Ulrich CT, Schär RT, Seidel K, Raabe A, Jesse CM. The surgical challenge of ossified ventrolateral spinal meningiomas: tricks and pearls for managing large ossified meningiomas of the thoracic spine. J Neurosurg Spine (2021) 35(4):516–26. doi: 10.3171/2020.12.SPINE201526
36. Dong C, Liu Y, Zhu Y, Wei H, Ma Y. Multiple ossified spinal meningiomas in the thoracic spine: A case report and literature review. Front Surg (2022) 9:965815. doi: 10.3389/fsurg.2022.965815
37. Adogwa O, Fessler RG. Intradural extramedullary spinal tumors. In: Berhouma M, Krolak-Salmon P, editors. Brain and spine surgery in the elderly. Cham: Springer International Publishing (2017). p. 289–304.
38. Kubota T, Sato K, Yamamoto S, Hirano A. Ultrastructural study of the formation of psammoma bodies in fibroblastic meningioma. J Neurosurg (1984) 60(3):512–7. doi: 10.3171/jns.1984.60.3.0512
39. Marosi C, Hassler M, Roessler K, Reni M, Sant M, Mazza E, et al. Meningioma. Crit Rev Oncol Hematol (2008) 67(2):153–71. doi: 10.1016/j.critrevonc.2008.01.010
40. Ruggeri AG, Fazzolari B, Colistra D, Cappelletti M, Marotta N, Delfini R. Calcified spinal meningiomas. World Neurosurg (2017) 102:406–12. doi: 10.1016/j.wneu.2017.03.045
41. Umana GE, Ferini G, Harikar MM, Venkataram T, Costanzo R, Scalia G, et al. Detection of "Incidentalomas" on brain and body (68)Ga-DOTATOC-PET scans: A retrospective study and case illustration. Anticancer Res (2022) 42(12):5867–73. doi: 10.21873/anticanres.16095
42. Palmisciano P, Watanabe G, Conching A, Ogasawara C, Ferini G, Bin-Alamer O, et al. The role of [(68)Ga]Ga-DOTA-SSTR PET radiotracers in brain tumors: A systematic review of the literature and ongoing clinical trials. Cancers (Basel) (2022) 14(12). doi: 10.3390/cancers14122925
43. Sala F, Palandri G, Basso E, Lanteri P, Deletis V, Faccioli F, et al. Motor evoked potential monitoring improves outcome after surgery for intramedullary spinal cord tumors: a historical control study. Neurosurgery (2006) 58(6):1129–43. doi: 10.1227/01.NEU.0000215948.97195.58
Keywords: dorsal completely ossified meningioma, spinal meningioma, ossification, thoracic spine tumor, literature review
Citation: Xu W-B, Sun N-K, Cai D-X, Chen D-Q, Niu Y, Jia F, Lin G-X and Rui G (2023) An unusual presentation of ossified spinal meningioma: case report and literature review. Front. Oncol. 13:1259508. doi: 10.3389/fonc.2023.1259508
Received: 16 July 2023; Accepted: 06 September 2023;
Published: 27 September 2023.
Edited by:
Patricia Sullivan, Rhode Island Hospital, United StatesCopyright © 2023 Xu, Sun, Cai, Chen, Niu, Jia, Lin and Rui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gang Rui, cmVpZ2FuZ0AxNjMuY29t; Guang-Xun Lin, bGluZ3Vhbmd4dW5AaG90bWFpbC5jb20=; Nai-Kun Sun, c3Vud2VuemU2QDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.