
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol., 10 November 2023
Sec. Cancer Epidemiology and Prevention
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.1247006
This article is part of the Research TopicSex Differences in Cancer Incidence, Mortality, and Survival: Methodological PerspectivesView all 15 articles
 Zhenfeng Zhu1†
Zhenfeng Zhu1† Wenjing Ye2†
Wenjing Ye2† Li Zhang3†
Li Zhang3† Wenchang Jia4,5
Wenchang Jia4,5 Binghong Chen4,5
Binghong Chen4,5 Qizhe Wang5
Qizhe Wang5 Xuelin Cheng5
Xuelin Cheng5 Shijia Yang5
Shijia Yang5 Zhaoyu Zhang5
Zhaoyu Zhang5 Yibo Ding6
Yibo Ding6 Xiaopan Li5*
Xiaopan Li5*Objectives: Due to the increase in life expectancy and the aging of the global population, the “Belt and Road” (“B&R”) countries are faced with varying degrees of lung cancer threat. The purpose of this study is to analyze the differences in the burden and trend of lung cancer disability in the “B&R” countries from 1990 to 2019 so as to provide an analytical strategic basis to build a healthy “B&R”.
Methods: Data were derived from the Global Burden of Disease 2019 (GBD 2019). Incidence, mortality, prevalence, the years lived with disability (YLDs), and disability-adjusted life years (DALYs) of lung cancer and those attributable to different risk factors were measured from 1990 to 2019. Trends of disease burden were estimated by using the average annual percent change (AAPC), and the 95% uncertainty interval (UI) was reported.
Results: China, India, and the Russian Federation were the three countries with the highest burden of lung cancer in 2019. From 1990 to 2019, the AAPC of incidence, prevalence, mortality, and DALYs generally showed a downward trend in Central Asia (except Georgia) and Eastern Europe, while in China, South Asia (except Bangladesh), most countries in North Africa, and the Middle East, the trend was mainly upward. The AAPC of age-standardized incidence was 1.33% (1.15%–1.50%); the AAPC of prevalence, mortality, and DALYs from lung cancer in China increased by 24% (2.10%–2.38%), 0.94% (0.74%–1.14%), and 0.42% (0.25%–0.59%), respectively. A downward trend of the AAPC values of age-standardized YLD rate in men was shown in the vast majority of “B&R” countries, but for women, most countries had an upward trend. For adults aged 75 years or older, the age-standardized YLD rate showed an increasing trend in most of the “B&R” countries. Except for the DALY rate of lung cancer attributable to metabolic risks, a downward trend of the DALY rate attributable to all risk factors, behavioral risks, and environmental/occupational risks was shown in the vast majority of “B&R” countries.
Conclusion: The burden of lung cancer in “B&R” countries varied significantly between regions, genders, and risk factors. Strengthening health cooperation among the “B&R” countries will help to jointly build a community with a shared future for mankind.
The “Belt and Road” (“B&R”) Initiative refers to the “Silk Road Economic Belt” and the “21st Century Maritime Silk Road”, which was first proposed by China in 2013. “B&R” countries run through Eurasia, connecting the Asia Pacific Economic Circle in the east and the European Economic Circle in the west (1). “B&R” Initiative can fully rely on the existing bilateral and multilateral mechanisms between China and relevant countries and leverage existing and effective regional cooperation platforms. Health crises are cross-border issues that require collective action to address (2, 3). In 2017, the Chinese government proposed the “Health Silk Road” (HSR) initiative to strengthen global health cooperation. “B&R” health exchange and cooperation helps to share successful experiences in the medical and health field. HSR initiative can promote cooperation in health, build a strong and resilient health system for transnational cooperation, and jointly build a “community of human health” in order to deal with disease epidemics.
Lung cancer is one of the main causes of new cancer cases and cancer-related deaths worldwide (4). In the past two decades, significant improvements have been made in understanding the biology and targeted therapy in lung cancer and the application of immune checkpoint inhibitors (ICIs), which have changed the prognosis of many patients (5). In terms of disability-adjusted life years (DALYs), the disease burden is evolving to be dominated by the years lived with disability (YLDs) (6). YLDs measure the amount of time that people lose to illnesses and injuries that do not cause death but reduce health. These areas are becoming hot topics for measuring and improving health outcomes due to transitions in aging populations and mortality in different countries.
Currently, “B&R” member countries are facing varying degrees of lung cancer threat. It is crucial to have comparable and comprehensive analysis and assessment of lung cancer incidence, mortality, disease burden, and long-term trends in China and its partner countries in order to improve public health and the success of the organizations. However, little is known about the status and extent of lung cancer in the 66 countries under the “B&R” Initiative. Our objective is to estimate the burden and trends of lung cancer from 1990 to 2019 through this study, providing a basis for formulating disease prevention and control policies and building a “community of human health” by strengthening health industry cooperation among the “B&R” countries.
This study was conducted using the Global Burden of Disease 2019 (GBD 2019) study obtained from the Institute for Health Metrics and Evaluation (IHME) website. All data for this study were obtained from the Institute for Health Metrics and Evaluation (IHME) website (https://www.healthdata.org/data-tools-practices/data-sources). Detailed methodology has been published elsewhere (7, 8).
Incidence, mortality, prevalence, YLDs, and DALYs were used in this study. Age-standardized rates for incidence, mortality, prevalence, YLDs, and DALYs were calculated according to a global age structure from 2019. YLDs were estimated by multiplying lung cancer prevalence with the corresponding disability weight. DALYs assess comprehensively premature death and the disease burden of disability. DALYs are equal to YLDs plus years of life lost (YLLs). YLLs are calculated as the product of counts of deaths caused by lung cancer and a standard remaining life expectancy at the age of death. The age-standardized rates were corrected by the direct method and the world standard population to account for differences in the population age structure. Our study follows the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) to ensure transparency and replicability (Table 1) (9).
The 66 members of “B&R” countries are as follows: 1) East Asia: China; 2) Central Asia: Armenia, Azerbaijan, Georgia, Kazakhstan, Kyrgyzstan, Mongolia, Tajikistan, Turkmenistan, and Uzbekistan; 3) South Asia: Bangladesh, Bhutan, India, Nepal, and Pakistan; 4) Southeast Asia: Cambodia, Indonesia, Laos, Malaysia, Maldives, Burma, the Philippines, Sri Lanka, Thailand, and Vietnam; 5) high-income Asia Pacific: Brunei and Singapore; 6) North Africa and the Middle East: Afghanistan, Bahrain, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Oman, Palestine, Qatar, Saudi Arabia, Syria, Turkey, the United Arab Emirates, and Yemen; 7) Central Europe: Albania, Bosnia and Herzegovina, Bulgaria, Croatia, Czechia, Hungary, Montenegro, North Macedonia, Poland, Romania, Serbia, Slovakia, and Slovenia; 8) Eastern Europe: Belarus, Estonia, Latvia, Lithuania, Republic of Moldova, Russia, and Ukraine; 9) Western Europe: Cyprus, Greece, and Israel. See Figure 1 for more details.
We calculated absolute numbers and age-standardized rates of incidence, mortality, YLDs, and DALYs to quantify the burden of lung cancer, grouped by gender and age in the “B&R” countries. Age-standardized estimates allow comparisons across time, countries, and subregions and are adjusted for differences in the age distribution of the population. Age was divided into three groups: 20–54 years, 55–74 years, and ≥75 years. The three risk factors (behavioral risks, environmental/occupational risks, and metabolic risks) were included in the present study. Data were stratified by region [high, high-middle, middle, low-middle, and low socio-demographic index (SDI)]. SDI is a composite indicator of a country’s lag-distributed income per capita, educational attainment, and the total fertility rate in women younger than 25 years. Methods of SDI development and computation are detailed elsewhere (10). Trends of disease burden from 1990 to 2019 were evaluated using average annual percent change (AAPC), which was calculated by the Joinpoint Regression Program (Version 4.9.0.0, March 2021) (11). Uncertainty intervals (UIs) of 95% were calculated with the 2.5th and 97.5th percentiles of 1,000 drawn by age, sex, location, and year (12). The map visualization of the “B&R” member states was performed using the “ggmap” package in R software (version 4.3.0, R Core Team). The “ggmap” package is an extension package, which obtains shapefiles from Google Maps. p < 0.05 was considered statistically significant.
Being involved in the Global Burden of Disease 2019 and other open databases rather than directly speaking to patients inspired this research. Although no patient was directly involved in this study, members of the public read our manuscript, and all agreed on the specific findings of this study.
The absolute number of incidence, mortality, YLDs, and DALYs in 2019 caused by lung cancer in each member country of the “B&R” are shown in Table 2. We noted that there were significant geographic differences in the number of lung cancer incidence, mortality, YLDs, and DALYs across countries, with China, India, and the Russian Federation being the three countries with the highest burden of lung cancer. In 2019, there were 832,922.16 (95% UI 700,293.15 to 981,631.63) lung cancer incidences, 757,171.25 (95% UI 638,741.18 to 887,751.81) deaths, 199,351.51 (95% UI 138,983.38 to 264,035.88) YLDs, and 17,128,584.02 (95% UI 14,340,490.76 to 20,231,342.32) DALYs due to lung cancer in China. The country with the lowest number of lung cancer incidences is the Maldives in Southeast Asia (26.49, 95% UI 21.86 to 31.61).
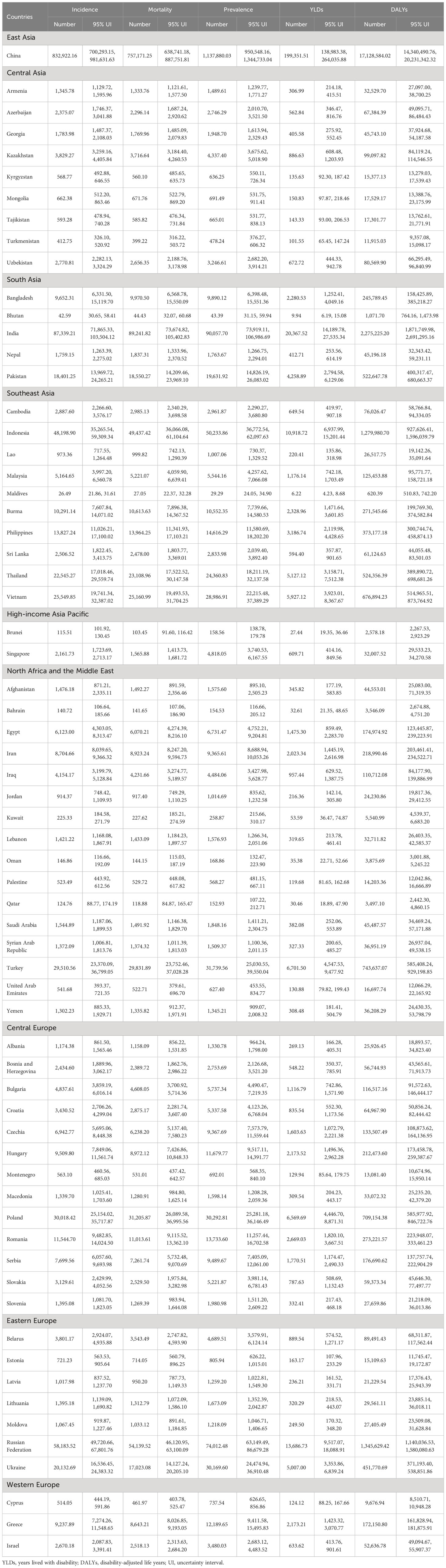
Table 2 The absolute number of incidence, mortality, prevalence, YLDs, and DALYs due to lung cancer in 2019.
Figure 2 shows the age-standardized rates of incidence, mortality, prevalence, YLDs, and DALYs due to lung cancer in 1990 and 2019 in member countries of the “Belt and Road” Initiative. From 1990 to 2019, the incidence, mortality, prevalence, YLDs, and DALYs of lung cancer in South and Southeast Asia were generally low. In 1990, the country with the highest incidence of YLDs and DALYs of lung cancer was Hungary (49.27 per 100,000, 11.25 per 100,000, and 1,295.93 per 100,000). Bhutan had the lowest rates of incidence, mortality, prevalence, YLDs, and DALYs (6.03 per 100,000, 6.37 per 100,000, 5.90 per 100,000, 1.43 per 100,000, and 157.30 per 100,000, respectively). In 2019, Montenegro had the highest incidence, mortality, prevalence, YLDs, and DALYs (56.72 per 100,000, 53.36 per 100,000, 70.60 per 100,000, 13.17 per 100,000, and 1,343.58 per 100,000, respectively). Bangladesh had the lowest rates of incidence, mortality, prevalence, YLDs, and DALYs (7.43 per 100,000, 7.81 per 100,000, 7.40 per 100,000, 1.74 per 100,000, and 181.71 per 100,000, respectively). Prevalence, YLDs, and DALYs due to lung cancer declined most rapidly in Kazakhstan, while incidence, prevalence, and YLDs increased the fastest in China from 1990 to 2019. See Supplementary Table 1 for more details.
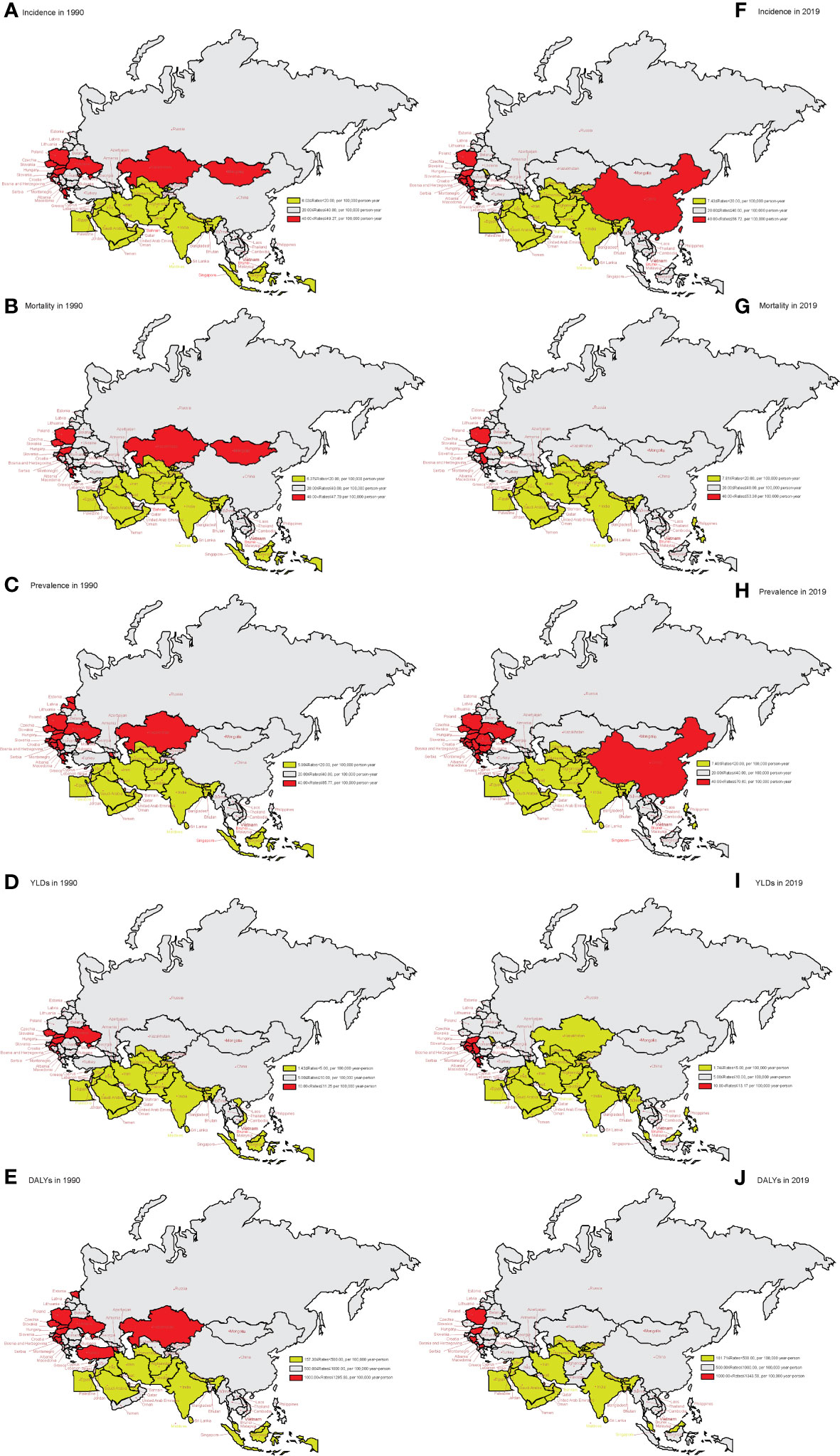
Figure 2 The age-standardized rates of incidence, mortality, prevalence, YLDs, and DALYs in 1990 and 2019 in “the Belt & Road” countries. (A) Age-standardized incidence rate in 1990. (B) Age-standardized mortality rate in 1990. (C) Age-standardized prevalence rate in 1990. (D) Age-standardized YLD rate in 1990. (E) Age-standardized DALY rate in 1990. (F) Age-standardized incidence rate in 2019. (G) Age-standardized mortality rate in 2019. (H) Age-standardized prevalence rate in 2019. (I) Age-standardized YLD rate in 2019. (J) Age-standardized DALY rate in 2019. YLDs, years lived with disability; DALYs, disability-adjusted life years.
From 1990 to 2019, the AAPC of age-standardized incidence, prevalence, mortality, and DALYs generally showed a downward trend in Central Asia (except Georgia) and Eastern Europe, while in China, South Asia (except Bangladesh), and most countries in North Africa and the Middle East, the trend was mainly upward (Figure 3). The AAPC of age-standardized incidence, prevalence, mortality, and DALYs from lung cancer in China increased by 1.33% (95%CI: 1.15% to 1.50%, p < 0.001), 2.24% (95%CI: 2.10% to 2.38%, p < 0.001), 0.94% (95%CI: 0.74% to 1.14%, p < 0.001), and 0.42% (95%CI: 0.25% to 0.59%, p < 0.001), respectively. See Supplementary Table 2 for more details.
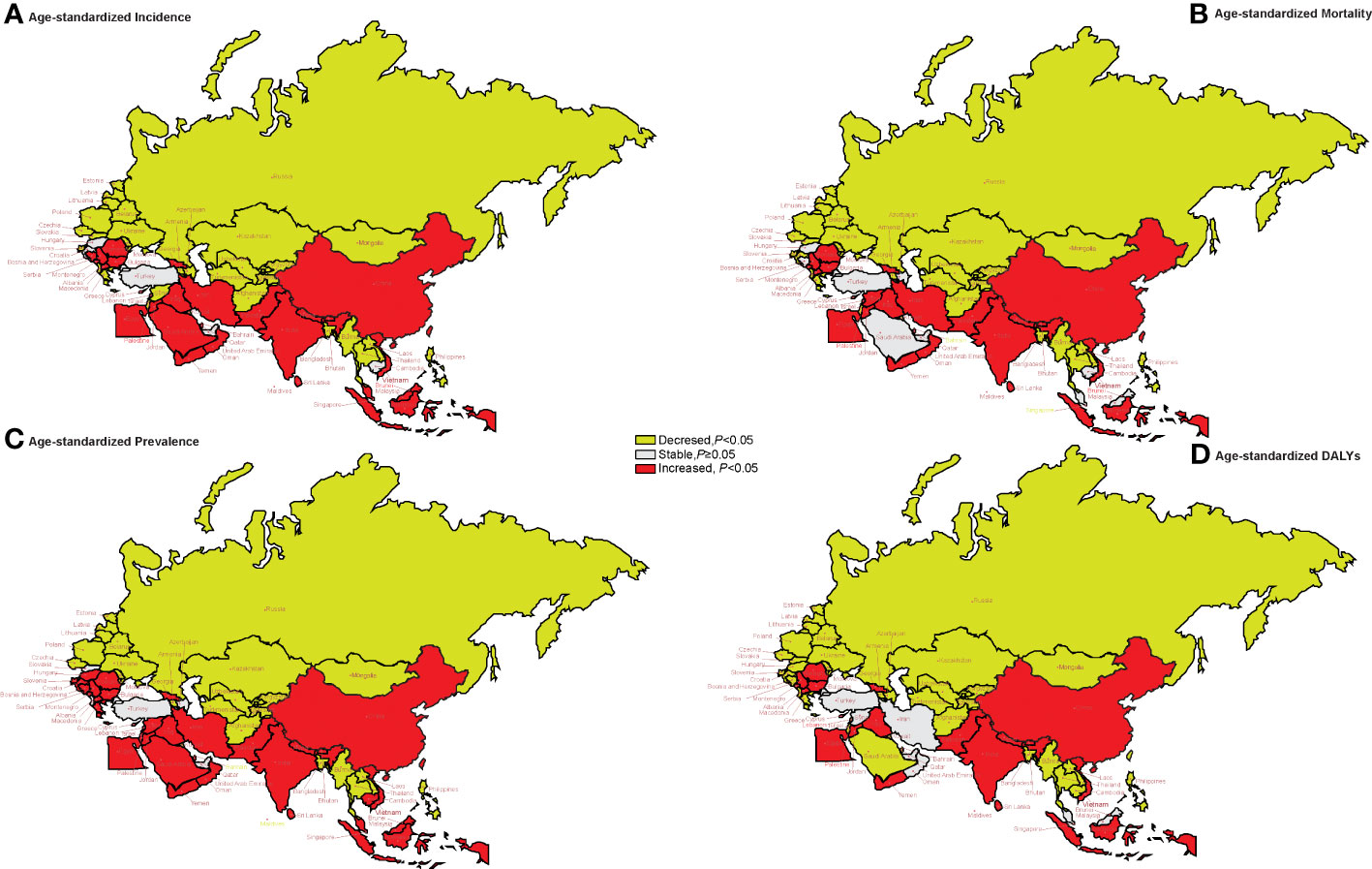
Figure 3 The trends of age-standardized rates of incidence, mortality, prevalence, and DALYs in 1990–2019 in “the Belt & Road” countries. (A) The AAPC of age-standardized incidence rate. (B) The AAPC of age-standardized mortality rate. (C) The AAPC of age-standardized prevalence rate. (D) The AAPC of age-standardized DALY rate. AAPC, average annual percent change; DALYs, disability-adjusted life years.
Figure 4 shows the AAPC values of age-standardized YLD rate in member countries. Turkmenistan, Uzbekistan, Lao, the Philippines, Albania, and Ukraine had an upward trend of age-standardized YLDs from 2010 to 2019 and a downward trend from 1990 to 2019. Pakistan, Malaysia, Sri Lanka, Jordan, Oman, Qatar, Saudi Arabia, Syrian Arab Republic, Yemen, Bosnia and Herzegovina, Bulgaria, Macedonia, and Serbia showed a downward trend in age-standardized YLDs from 2010 to 2019, while an upward trend was observed from 1990 to 2019 (p < 0.05) (Supplementary Table 3). There were also differences in the trend of changes in AAPC between men and women from 1990 to 2019. A downward trend of the AAPC values of age-standardized YLD rate in men was shown in the vast majority of “B&R” countries. For women, the change trend of YLDs was stable in Georgia and Russia, while the upward trend was observed in most other countries (Supplementary Table 4).
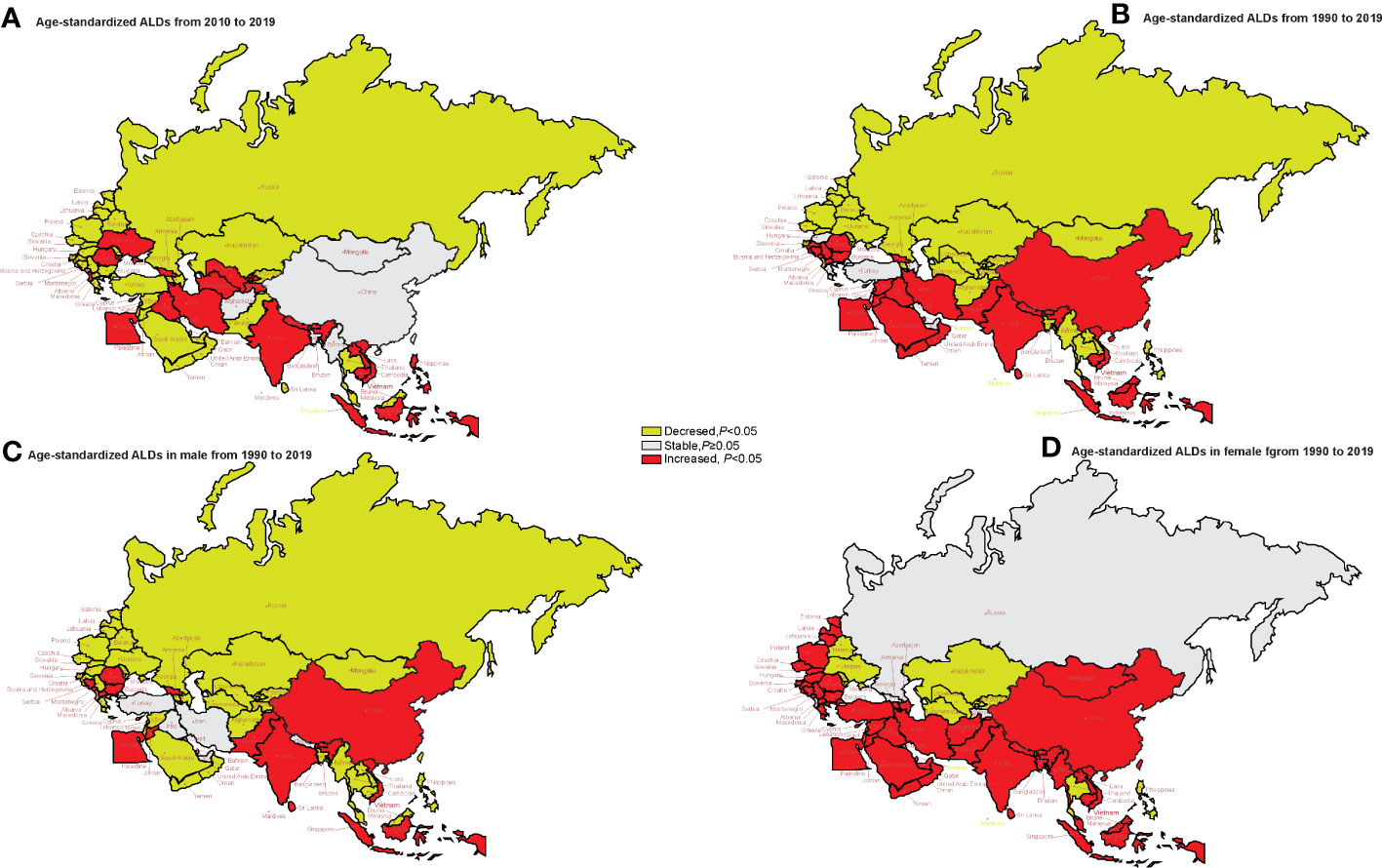
Figure 4 The trends of age-standardized rates of YLDs in genders in 2010–2019 and in 1990–2019 in “the Belt & Road” countries. (A) The AAPC of age-standardized rates of YLDs in 2010–2019. (B) The AAPC of age-standardized rates of YLDs in 1990–2019. (C) The AAPC of age-standardized rates of YLDs in men in 1990–2019. (D) The AAPC of age-standardized rates of YLDs in women in 1990–2019. AAPC, average annual percent change; YLDs, years lived with disability.
Figure 5 shows the long-term trends of age-standardized YLD rate due to lung cancer, stratified by age from 1990 to 2019 for the “B&R” countries. We found that in Maldives, the Philippines, Bahrain, Belarus, and Ukraine, the age-standardized YLDs of all ages showed a downward trend, while in China, Bhutan, India, Pakistan, Indonesia, Malaysia, Sri Lanka, Egypt, Iraq, Jordan, Lebanon, Bulgaria, Montenegro, Macedonia, Serbia, and Cyprus, the age-standardized YLDs of all ages showed an upward trend (p < 0.05). For adults aged 75 years or older, the age-standardized YLD rate from 1990 to 2019 showed an increasing trend in the “B&R” countries, except Kazakhstan, Kyrgyzstan, Turkmenistan, Mongolia, Bangladesh, Maldives, Afghanistan, Bahrain, the United Arab Emirates, Belarus, Moldova, Ukraine, Greece, and the Philippines. In China, age-standardized YLDs showed an increasing trend with the increase of age, and the highest AAPC value of age-standardized YLD rate from 1990 to 2019 was in adults aged 75 years or older: 2.87% (95%CI: 2.60%–3.14%, p < 0.001). See Supplementary Table 5 for more details.
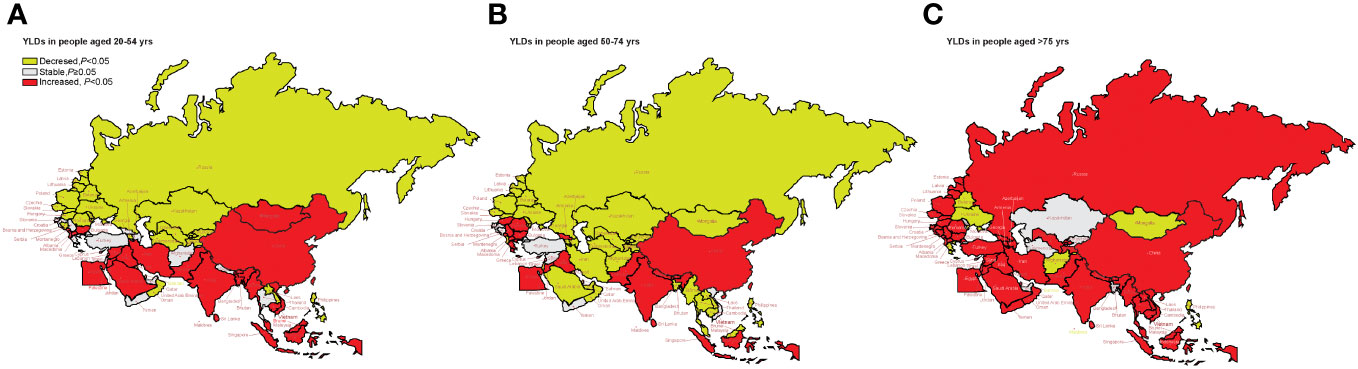
Figure 5 Visualization of the trends of age-standardized YLD rate stratified by age from 1990 to 2019 in “the Belt & Road” countries. (A) YLD rate in people aged 20–54 years. (B) YLD rate in people aged 55–74 years. (C) YLD rate in people aged ≥75 years. YLDs, years lived with disability.
Figure 6 shows the long-term trends of the age-standardized DALY rate due to lung cancer, stratified by risk factors from 1990 to 2019 for the “B&R” countries. We found that in middle SDI regions, China, Georgia, Bhutan, Indonesia, Sri Lanka, Vietnam, Egypt, Iraq, Jordan, Lebanon, Palestine, Yemen, Bulgaria, Montenegro, Macedonia, Serbia, and Cyprus, the age-standardized DALYs due to all risk factors showed an upward trend, while globally and in the other “B&R” countries, the age-standardized DALYs of all risk factors showed a downward trend (p < 0.05).
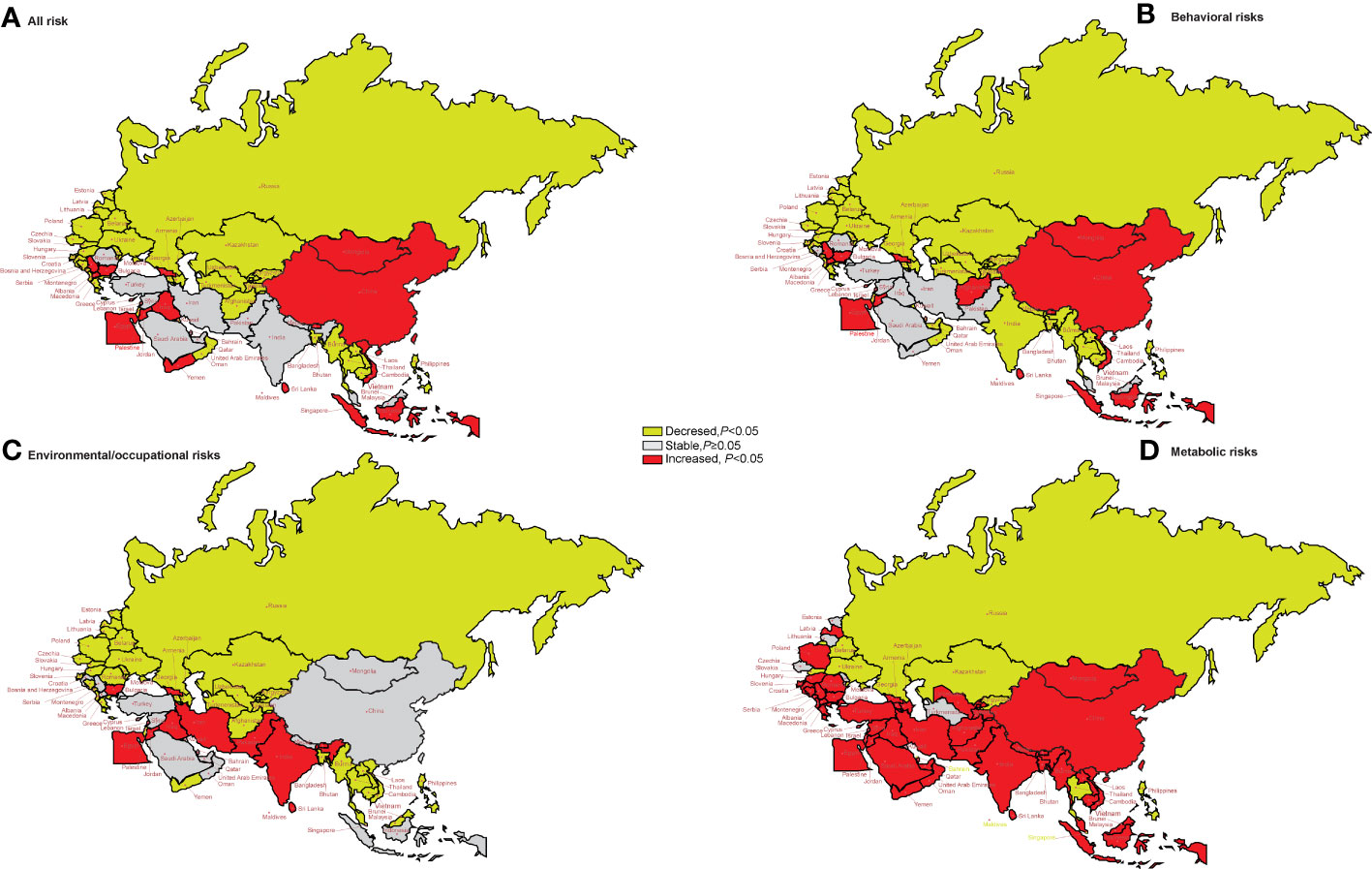
Figure 6 The temporal trend in the DALY rate of lung cancer attributed to risk factors for 1990–2019 in the “B&R” countries. (A) All risk factors. (B) Behavioral risks. (C) Environmental/occupational risks. (D) Metabolic risks. DALYs, disability-adjusted life years.
For DALYs of lung cancer attributable to behavioral risks, the age-standardized DALY rate of middle SDI regions, China, Georgia, Bhutan, Bhutan, Indonesia, Sri Lanka, Vietnam, Afghanistan, Egypt, Jordan, Lebanon, Palestine, Bulgaria, Montenegro, Macedonia, Serbia, and Cyprus showed an increasing trend in the “B&R” countries from 1990 to 2019 (all p < 0.05).
For DALYs of lung cancer due to environmental/occupational risks, the age-standardized DALY rate of Georgia, Bhutan, Pakistan, Sri Lanka, Egypt, Iran, Iraq, Jordan, Lebanon, and Bulgaria showed an increasing trend in the “B&R” countries from 1990 to 2019 (all p < 0.05).
For DALYs of lung cancer attributable to metabolic risks, the age-standardized DALY rate of Kazakhstan, Kyrgyzstan, Turkmenistan, Maldives, the Philippines, Thailand, Singapore, Bahrain, Slovakia, Belarus, and Ukraine showed a decreasing trend in the “B&R” countries from 1990 to 2019 (all p < 0.05). See Supplementary Table 6 for more details.
With an estimated 1.79 million deaths per year, lung cancer is one of the leading causes of cancer-related deaths (5). Smoking, poor diet, lack of exercise, genetic factors, air pollution, and occupational exposure are all risk factors for cancer (13). Smoking is an important risk factor for increasing cancer risk (14). Cigarettes contain polycyclic aromatic hydrocarbons and nitrosamines. Nicotine is an addictive substance, so it leads to frequent use among smokers, and therefore, lung cancer is more common among them (15, 16). In the last decade, the age-standardized incidence rate in high-socio-demographic index countries has been decreasing due to tobacco control (17). We found that the incidence, prevalence, and YLDs increased the fastest in China from 1990 to 2019, and the age-standardized incidence, prevalence, mortality, and DALYs showed an upward trend in China, South Asia, North Africa, and the Middle East, which may be related to a large number of smokers in these countries.
Our study found significant differences in the trend of age-standardized YLDs between genders. A downward trend of the AAPC values of age-standardized YLD rate in men was shown in the “B&R” countries. For women, the upward change trend of YLDs was observed in most countries. The global incidence of lung cancer in men is declining twice as fast as in women (5). The age-standardized incidence rates of lung cancer among women are predicted to increase before 2035 and are expected to peak after the 2020s, while those among men are expected to decrease in almost all countries (18). The mortality of cancers due to smoking has substantially increased among women in most countries of the North Africa and Middle East region (19). These studies all suggest that the “B&R” and even countries around the world need to strengthen the publicity and education of female smoking cessation and attach importance to physical examination and lung screening, which will help control the incidence rate and mortality of female lung cancer.
The increase in life expectancy has led to a greater global burden of diseases. Global population aging is the principal medical and social demographic problem worldwide. In the Non-Organisation for Economic Co-operation and Development countries, the fastest-aging countries are Saudi Arabia, Brazil, and China (20). Since 2000, China has gradually entered an aging society, the aging in China has not been alleviated but has gradually increased recently, and the burden of lung cancer on elderly patients is also increasing (21). In the “B&R” member countries, the age-standardized YLDs in most countries showed an upward trend with the increase of age, and the highest AAPC value of the age-standardized YLDs in 1990–2019 was in adults aged 75 years or older. A satisfactory and appropriate understanding of the health problems of older people caused by aging is a common challenge in the world. The goal vision is to establish a world where everyone has the chance to live a healthy and long life (20). This requires close cooperation between multiple sectors and departments in the “B&R” member countries to promote healthy aging.
In recent decades, countries within the Middle East have faced social, political, and financial instability brought about by war. These conflicts have directly led to a significant decline in the overall level of local medical services and a shortage of professional experts, seriously affecting the provision of cancer diagnosis services. The cancer patients in these areas cannot be diagnosed early and cannot receive effective healthcare (22, 23). In addition, the use of depleted uranium and white phosphorus bombs in wars may cause environmental pollution and even cancer (24). Therefore, many cancer patients must bear the cost of traveling to neighboring countries in order to receive medical services. Our study also found that from 1990 to 2019, the AAPC of age-standardized incidence rate, morbidity, mortality, and DALYs showed an upward trend in most countries in the Middle East. It is important to alleviate the shortage of medical services for these countries through the “B&R” Initiative.
With a deeper understanding of the biology of lung cancer, many advances have been made in the treatment of lung cancer, such as minimally invasive techniques, stereotactic ablative radiotherapy, targeted therapies, and ICIs (25). New therapies have benefited patients and reduced the burden of disease. However, due to various reasons such as economic development and healthcare systems, countries have varying opportunities to access drugs and healthcare (5). In low-income countries, new lung cancer cases and mortality continue to increase, which may be related to limited access to healthcare and outdated treatment methods in these countries (5). By implementing large-scale infrastructure construction and trade facilitation, poor and low-income countries can return to the mainstream of global development from a state of global marginalization, thereby providing bright prospects for comprehensive and long-term economic growth in the “B&R” member countries. In addition, the medical field should also be highly valued. The exchange of medical knowledge and experience among medical institutions in the “B&R” countries should be continuously promoted so that medical technology and health services will be extended from higher-level countries to lower-level ones, thus improving the medical level of each country and benefiting low-income people.
YLDs can reflect the amount of time lived in states of less than good health due to a specific disease or injury and are calculated as the prevalence of a sequela of any given cause multiplied by the average duration until death or remission and by the disability weight for that sequela. The YLDs are the sum of each of the sequelae associated with the disease or injury (26, 27). YLL refers to the loss of life caused by early death. Although YLDs and YLLs can reflect the burden on society, YLDs are more likely to be affected by diseases and injuries in their lives. Reducing the burden of disease involves not only prolonging the survival period of patients but also improving the quality of life of patients. The interventions required to reduce the causes of death may differ from those needed to reduce risk factors and disability rates for disease burden. This is why we chose to calculate YLDs in this study.
Globally, from 2010 to 2019, the number of lung cancer increased by 23.3%, and the age-standardized incidence rates decreased by 7.4% in men and increased by 0.9% in women (4). Compared to the USA and UK, China had lower incidence but higher cancer mortality and DALYs (28). All the age-standardized incidences had a decreasing trend in men and an increasing trend in women from 1990 to 2019 in the North Africa and Middle East region. Over 80% of DALYs could be decreased by controlling tobacco use (23). The number of new cases is predicted to increase by 50.19% from 2010 to 2035. When stratified by geographic region, the most rapid increases were predicted in Eastern Asia (79.00% for men and 140.05% for women) (18). We found that in the “B&R” countries, especially in middle SDI regions, DALYs due to all risk factors showed an upward trend, while globally, DALYs had a downward trend.
Unlike previous lung cancer burden studies based on GBD data, this study focuses on the “B&R” countries proposed by China, the world’s second-largest economy, under the global community of shared future strategy. It not only describes the changes in disease burden in a specific region or globally but also provides targeted data support for how countries with significant differences in social demographic indices but strong political and economic connections can formulate policies to reduce the burden of lung cancer. Preventive measures such as smoking control interventions and air quality management should be prioritized in low and middle SDI regions. Our research also suggested that we should pay more attention to female lung cancer patients. For women, the upward trend of YLDs was observed in the “B&R” countries, and it may continue to rise in the future (18). By studying the continuous transformation of epidemiology in the “B&R” countries, the necessity of resource redistribution and improvement of lung cancer control measures is highlighted.
This study also has several limitations. First, GBD 2019 has inherent limitations that are applicable to this study. Second, the GBD database lacks lung cancer’s pathological staging and classification. In the future, the “B&R” countries can use economic development as a link to drive the construction of information-based disease monitoring systems, providing sufficient support for the estimation of disease burden and policy adjustments.
In summary, the overall burden of lung cancer in the “B&R” countries is still huge, especially in China, South Asia, North Africa, and the Middle East. There are significant differences between genders and ages. The lung cancer prevention and treatment policies in women and adults aged 75 years or older need to be improved. With the background of the health “B&R” Initiative, multi-country cooperation and experience sharing will play an important role in jointly facing the challenges caused by lung cancer and promoting the positive development of healthcare in all member countries.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
XL conceived and designed the study. ZZhu, WY, LZ, WJ, BC,QW, XC, SY, and ZZhang analyzed the data. ZZhu, XL, and YD provided significant advice and consultation. WY and XL wrote the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by the National Natural Science Foundation of China (82104450 to ZZhu) and the Youth Science and Technology Project of Shanghai Pudong new area health commission (PW2018B-35). The funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report. All authors had full access to all data in the study and had responsibility for the decision to submit for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2023.1247006/full#supplementary-material
Supplementary Table 1 | The age-standardized rates of incidence, mortality, prevanlence, YLDs and DALYs in member countries of the “Belt and Road” initiative from 1990 to 2019. (YLDs, years lived with disability; DALYs, disability-adjusted life-years; UI, uncertainty interval).
Supplementary Table 2 | The average annual percentage change (AAPC) of age-standardized incidence, mortality, prevanlence and DALYs from 1990 to 2019 in the “Belt & Road” countries. (AAPC, average annual percent change; DALYs, disability-adjusted life-years).
Supplementary Table 3 | The average annual percentage change (AAPC) of age-standardized YLDs in 2010-2019 and 1990-2019 in the “Belt & Road” countries. (AAPC, average annual percent change; YLDs, years lived with disability).
Supplementary Table 4 | The average annual percentage change (AAPC) of age-standardized rates for YLDs in male and female from 1990 to 2019 in the “Belt & Road” countries. (AAPC,average annual percent change; YLDs, years lived with disability).
Supplementary Table 5 | The average annual percentage change (AAPC) of age-standardized rates for YLDs stratified by age from 1990 to 2019 in the “Belt & Road” countries. (AAPC,average annual percent change; YLDs, years lived with disability).
Supplementary Table 6 | The average annual percentage change (AAPC) of age-standardized rates for DALYs stratified by risk factors from 1990 to 2019 in the “Belt & Road” countries. (AAPC, average annual percent change; DALYs, disability-adjusted life-years).
1. Liu W, Hughes AC, Sachdeva G, Narain D, Zhou T, Wang Y, et al. The belt and road initiative and the sustainable development goals. One Earth (2020) 3(3):263–7. doi: 10.1016/j.oneear.2020.08.020
2. Tang K, Li Z, Li W, Chen L. China's Silk Road and global health. Lancet (2017) 390(10112):2595–601. doi: 10.1016/S0140-6736(17)32898-2
3. Hu R, Liu R, Hu N. China's Belt and Road Initiative from a global health perspective. Lancet Glob Health (2017) 5(8):e752–3. doi: 10.1016/S2214-109X(17)30250-4
4. GBD 2019 Respiratory Tract Cancers Collaborators. Global, regional, and national burden of respiratory tract cancers and associated risk factors from 1990 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Respir Med (2021) 9(9):1030–49. doi: 10.1016/S2213-2600(21)00164-8
5. Thai AA, Solomon BJ, Sequist LV, Gainor JF, Heist RS. Lung cancer. Lancet (2021) 398(10299):535–54. doi: 10.1016/S0140-6736(21)00312-3
6. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (2018) 392(10159):1789–858. doi: 10.1016/S0140-6736(18)32279-7
7. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (2020) 396(10258):1204–22. doi: 10.1016/S0140-6736(20)30925-9
8. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (2020) 396(10258):1223–49. doi: 10.1016/S0140-6736(20)30752-2
9. Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet (2016) 388(10062):e19–23. doi: 10.1016/S0140-6736(16)30388-9
10. GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet (2020) 396(10258):1160–203. doi: 10.1016/S0140-6736(20)30977-6
11. Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual per cent change in trend analysis. Stat Med (2009) 28(29):3670–82. doi: 10.1002/sim.3733
12. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol (2021) 20(10):795–820. doi: 10.1016/S1474-4422(21)00252-0
13. Malhotra J, Malvezzi M, Negri E, La Vecchia C, Boffetta P. Risk factors for lung cancer worldwide. Eur Respir J (2016) 48(3):889–902. doi: 10.1183/13993003.00359-2016
14. Chang CM, Corey CG, Rostron BL, Apelberg BJ. Systematic review of cigar smoking and all cause and smoking related mortality. BMC Public Health (2015) 15:390. doi: 10.1186/s12889-015-1617-5
15. GBD 2019 Cancer Risk Factors Collaborators. The global burden of cancer attributable to risk factors, 2010-19: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (2022) 400(10352):563–91. doi: 10.1016/S0140-6736(22)01438-6
16. Hecht SS. Lung carcinogenesis by tobacco smoke. Int J Cancer (2012) 131(12):2724–32. doi: 10.1002/ijc.27816
17. Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Akinyemiju TF, Al Lami FH, Alam T, Alizadeh-Navaei R, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2016: A systematic analysis for the global burden of disease study. JAMA Oncol (2018) 4(11):1553–68. doi: 10.1001/jamaoncol.2018.2706
18. Luo G, Zhang Y, Etxeberria J, Arnold M, Cai X, Hao Y, et al. Projections of lung cancer incidence by 2035 in 40 countries worldwide: population-based study. JMIR Public Health Surveill (2023) 9:e43651. doi: 10.2196/43651
19. Rezakhani L, Darbandi M, Khorrami Z, Rahmati S, Shadmani FK. Mortality and disability-adjusted life years for smoking-attributed cancers from 1990 to 2019 in the north Africa and middle east countries: a systematic analysis for the global burden of disease study 2019. BMC Cancer (2023) 23(1):80. doi: 10.1186/s12885-023-10563-5
20. Rudnicka E, Napierała P, Podfigurna A, Męczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas (2020) 139:6–11. doi: 10.1016/j.maturitas.2020.05.018
21. Wu F, Wang L, Zhou C. Lung cancer in China: current and prospect. Curr Opin Oncol (2021) 33(1):40–6. doi: 10.1016/j.maturitas.2020.05.018
22. Al-Ibraheem A, Abdlkadir AS, Mohamedkhair A, Mikhail-Lette M, Al-Qudah M, Paez D, et al. Cancer diagnosis in areas of conflict. Front Oncol (2022) 12:1087476. doi: 10.3389/fonc.2022.1087476
23. Khanmohammadi S, Saeedi Moghaddam S, Azadnajafabad S, Rezaei N, Esfahani Z, Rezaei N, et al. Burden of tracheal, bronchus, and lung cancer in North Africa and Middle East countries, 1990 to 2019: Results from the GBD study 2019. Front Oncol (2023) 12:1098218. doi: 10.3389/fonc.2022.1098218
24. Surdyk S, Itani M, Al-Lobaidy M, Kahale LA, Farha A, Dewachi O, et al. Weaponised uranium and adverse health outcomes in Iraq: a systematic review. BMJ Glob Health (2021) 6(2):e004166. doi: 10.1136/bmjgh-2020-004166
25. Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman JR, Bharat A, et al. Non-small cell lung cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw (2022) 20(5):497–530. doi: 10.6004/jnccn.2022.0025
26. Guthold R, White Johansson E, Mathers CD, Ross DA. Global and regional levels and trends of child and adolescent morbidity from 2000 to 2016: an analysis of years lost due to disability (YLDs). BMJ Glob Health (2021) 6(3):e004996. doi: 10.1136/bmjgh-2021-004996
27. Chen L, Wang L, Qian Y, Chen H. Changes and trend disparities in life expectancy and health-adjusted life expectancy attributed to disability and mortality from 1990 to 2019 in China. Front Public Health (2022) 10:925114. doi: 10.3389/fpubh.2022.925114
Keywords: “B&R” countries, lung cancer, burden of disease, risk factors, average annual percent change, years lived with disability (YLDs), disability-adjusted life years (DALYs)
Citation: Zhu Z, Ye W, Zhang L, Jia W, Chen B, Wang Q, Cheng X, Yang S, Zhang Z, Ding Y and Li X (2023) Diversities of disability caused by lung cancer in the 66 Belt and Road initiative countries: a secondary analysis from the Global Burden of Disease Study 2019. Front. Oncol. 13:1247006. doi: 10.3389/fonc.2023.1247006
Received: 25 June 2023; Accepted: 19 September 2023;
Published: 10 November 2023.
Edited by:
Syed Ahsan Raza, University of Pittsburgh, United StatesReviewed by:
Shirin Djalalinia, Ministry of Health and Medical Education, IranCopyright © 2023 Zhu, Ye, Zhang, Jia, Chen, Wang, Cheng, Yang, Zhang, Ding and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaopan Li, eGlhb3BhbmxpMDIyNEAxMjYuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.