- Department of Gynecology, Cancer Hospital of China Medical University, Liaoning Cancer Hospital and Institute, Shenyang, Liaoning, China
Gynecological malignancy remains a prevalent cause of mortality among women. Chronic cancer pain, as a severe complication of malignancy and its therapies, accounts for a substantial burden of physical and psychological distress in affected patients. Accordingly, early identification, assessment, and standardized management of such pain are crucial in the prevention or delay of its progression. In the present review, we provide a comprehensive overview of the pathological factors that contribute to pain in patients with gynecological malignancy while highlighting the underlying mechanisms of pain in this population. In addition, we summarize several treatment modalities targeting pain management in gynecologic cancer patients, including surgery, radiotherapy, and chemotherapy. These interventions are crucial for tumor elimination and patient survival. Chronic cancer pain exerts a significant impact on wellbeing and quality of life for patients with gynecologic cancer. Therefore, our review emphasizes the importance of addressing this pain and its psychological sequelae and advocates for a multidisciplinary approach that encompasses nursing and psychological support. In summary, this review offers valuable insights into the pathological factors underlying pain, reviews pain management modalities, and stresses the critical role of early intervention and comprehensive care in enhancing the quality of life of these patients.
1 Introduction
Gynecological malignancies are among the most prevalent types of female malignancies, with high incidence rates in the ovarian, cervix uteri, and uterine bodies (1). Among these, cervical cancer has the highest incidence rate, followed by endometrial and ovarian cancers. These malignancies are known to cause significant morbidity and mortality in females, with lung cancer being the only type of malignancy with higher incidence and mortality rates (2, 3). Treatments such as surgery, radiotherapy, and chemotherapy have been known to improve the survival time of gynecological malignancy patients by removing the tumor and regional lymph nodes. However, these treatments also lead to severe impacts on the patient’s quality of life (4–7). Cancer pain is among the critical factors affecting the patient’s quality of life. Around 70% of patients suffering from advanced gynecological malignant tumors reported experiencing varying degrees of cancerous pain (8). The pain is caused by the tumor, metastases, cancer embolus, and infiltration into the surrounding tissues (9). Cancer pain is universal and severe, and is often difficult to manage, leading to the need for continuous drug intervention. The incidence rate of cancer pain is 50.7% in all cancer stages and 66.4% in advanced stages (10).
Cancer-related pain is a highly prevalent subjective symptom observed in patients with gynecologic malignancies (11). The nature of pain experienced by patients is generally dull and of a moderate degree. The pain predominantly affects the pelvic cavity and adjacent tissues, including the hypogastrium, perineum, and waist. Additionally, several patients experience pain in more than two sites. Cancer-related pain is a burdensome issue for patients and may lead to various adverse outcomes, such as interference with daily activities, hindrance of social function, and impairment of cognitive function (12). The consequences of cancer-related pain can negatively impact patients’ quality of life, leading to pessimism, anxiety, fear, and depression, resulting in patients’ societal and economic dependence. Furthermore, pain may affect patients’ sleep quality, leading to adverse emotions and reduced disease resistance, which is potentially detrimental to tumor treatment and symptom relief. Therefore, healthcare professionals are advised to pay adequate attention to the management of cancer-related pain in patients with gynecologic malignancies, including an accurate and reasonable evaluation and intervention. In this review, we focused on pain nursing for gynecologic cancer patients, emphasizing the importance of early identification, evaluation, and standardized pain treatment. We summarized the pathological factors contributing to pain in this population and reviews the pain management regimen for gynecologic cancer patients. Regarding the search strategies, we utilized a systematic approach to identify relevant studies, including searching electronic databases (Pubmed, Cochrane Library and Web of science), reviewing reference lists, and consulting with experts in the field. We also established inclusion and exclusion criteria to select studies for review and used methods to analyze and synthesize the data.
2 Pathophysiology of chronic pain in gynecological cancer
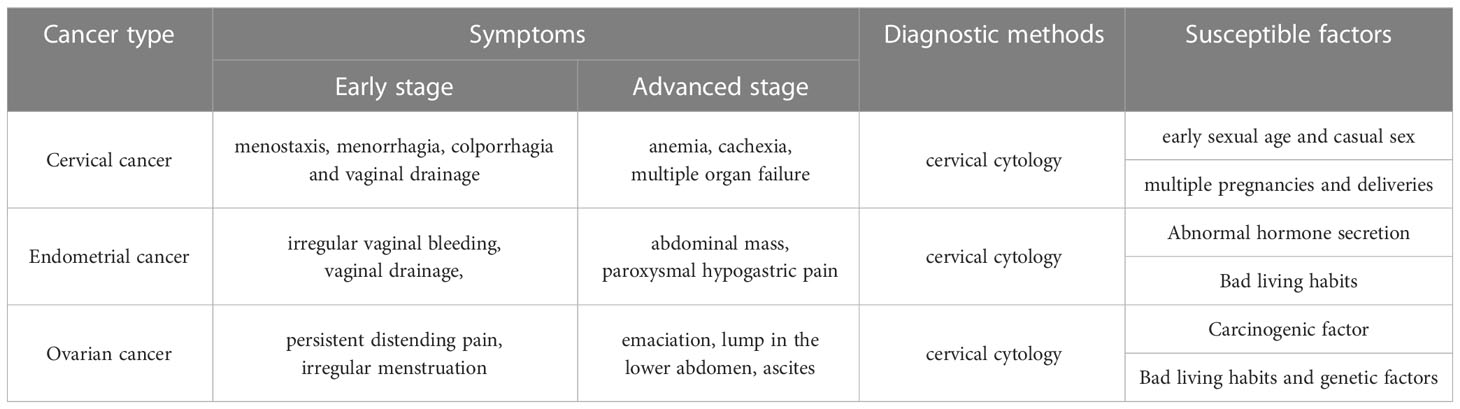
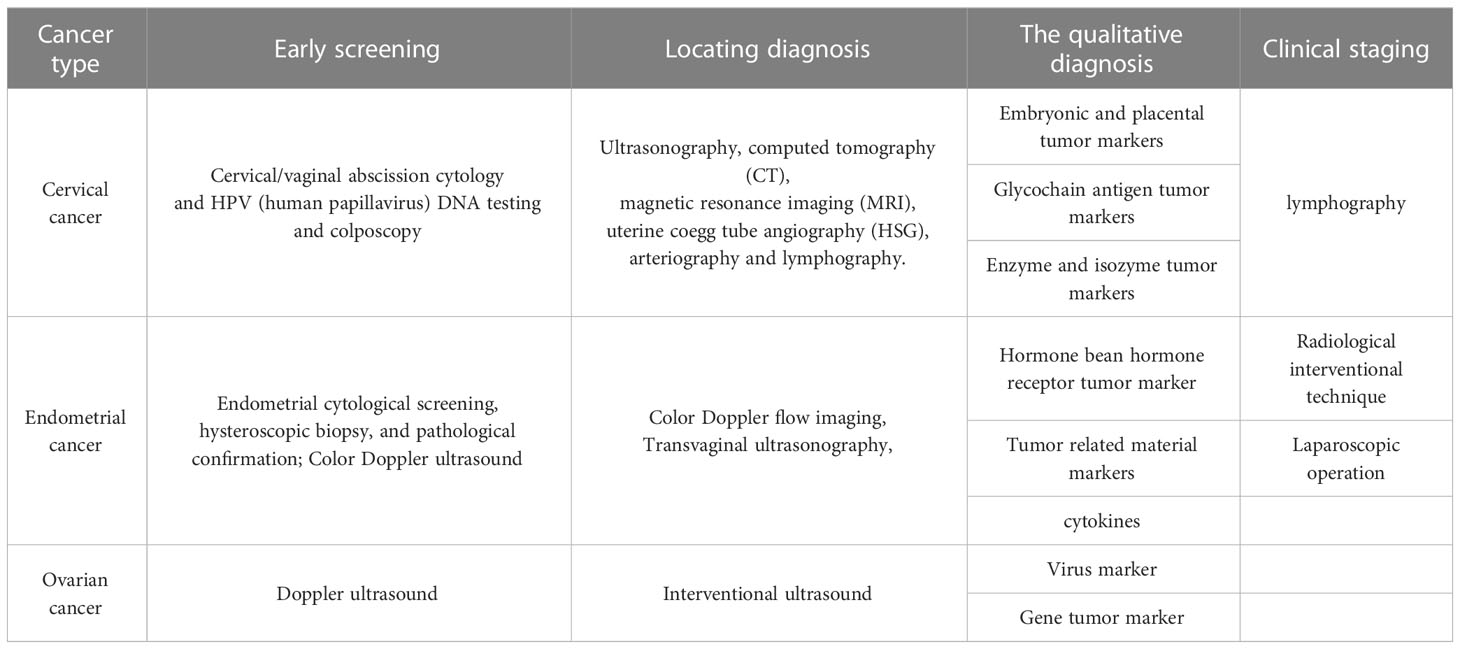
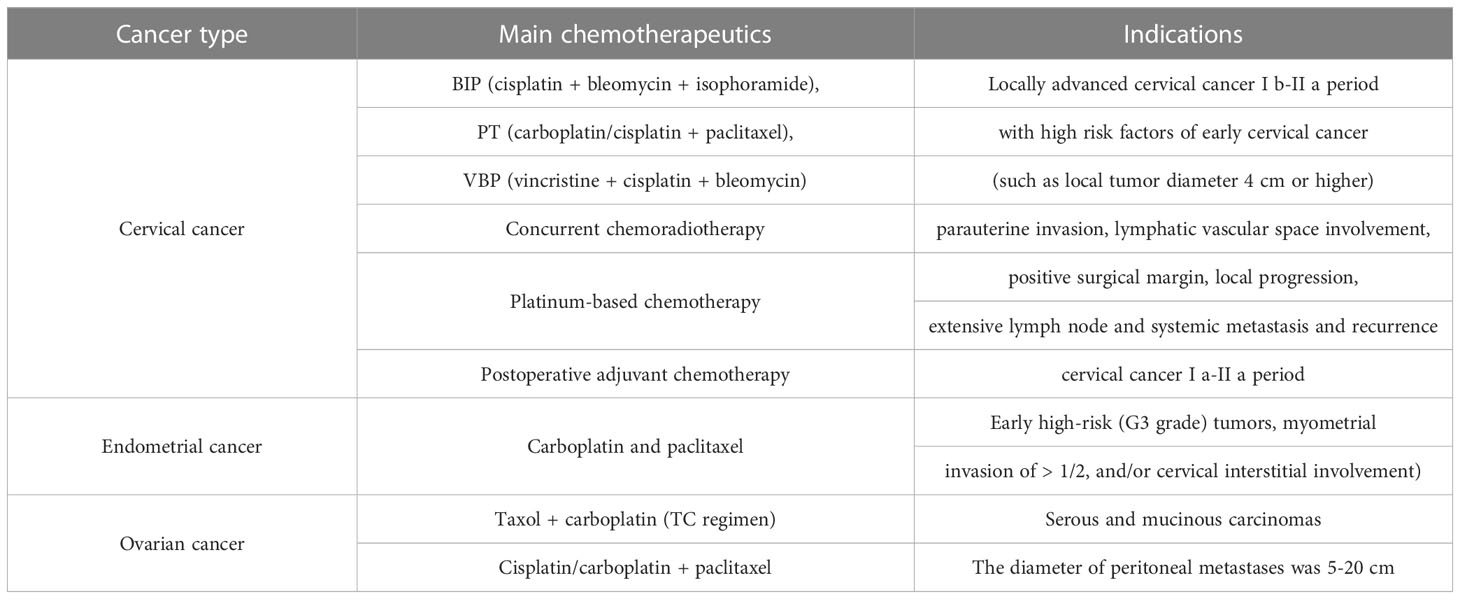
Gynecological malignancies encompass tumors that occur in various regions such as the cervix, endometrium, ovary, and other areas (Table 1). Among women, cervical cancer, endometrial cancer, and ovarian cancer are the most prevalent gynecological malignancies (13, 14). These malignancies are characterized by symptoms such as increased leucorrhea with an unpleasant odor, vaginal bleeding, the lump of hypogastrium, bearing-down pain, low fever, weight loss, and other indications, which can impede the health and well-being of patients (4). The pathogenesis of gynecological tumors remains widely unknown, and in most cases, these malignancies do not manifest apparent symptoms during the early stage. Distinguishing between benign and malignant malignancies preoperatively is difficult, and detection typically occurs during the moderate to late stages of the disease, significantly impacting the patient’s treatment and survival (2, 15). In recent years, various new concepts, new methods and new technologies have continuously emerged medicine (16, 17). Advancements in medicine continue to introduce novel concepts, methods, and technologies. Researchers believe that several factors, including reproductive history, menstrual history, sexual behavior, sexual age, endocrine function anomalies, lifestyle choices such as smoking, drinking, and infections, can increase the likelihood of developing gynecological malignancies (18, 19). Studies have shown that an unhealthy lifestyle, abnormal endocrine function, and sexual behaviors are high-risk factors for gynecological malignant tumors, which have close correlation with the incidence of cancer (20). The main therapeutic approaches and diagnostic markers are listed in Tables 2 and 3.
2.1 Cervical cancer and pathogenic factors
Cervical cancer is the most frequently occurring malignancy in the female genital tract (21, 22). During the early stages of the disease, no definite symptoms or signs are apparent. However, as the disease advances, various symptoms arise, such as menostaxis, menorrhagia, colporrhagia, and vaginal discharge. The extent of infiltration of the cancerous cells causes the emergence of secondary symptoms, and frequently observed symptoms in the advanced stages comprise cachexia, anemia, and multiple organ failure (23–25). Several factors influence the incidence of cervical cancer, including smoking, infection by high-risk strains of human papillomavirus (HPV), multiple sexual partners, an early onset of menstruation, a history of multiple pregnancies and deliveries, together with infections from pathogenic agents such as Chlamydia trachomatis, Herpes simplex, Type II Trichomonas vaginalis, and trichomonads. Cervical cancers in more than 90% of cases are associated with high-risk HPV infections (26, 27). A significantly higher incidence of cervical cancer was evident among females infected with strains such as 26, 53, 66 than uninfected individuals. Recent research findings indicate that commencing sexual activities at an early age, particularly under the age of twenty, can substantially heighten the risk of cervical cancer (28–30). During pregnancy, an increase in estrogen and progestational hormone levels is liable to trigger various adverse effects on the cervical environment, thus escalating the danger of cancer (31).
2.2 Endometrial cancer and pathogenic factors
Endometrial cancer is a malignant tumor that arises from the epithelial lining of the endometrium, which is the inner layer of the uterus. It ranks second among female reproductive malignancies and is the third most common cause of death in women (32, 33). The disease is frequently asymptomatic in the early stages, and incidental discovery during general or gynecological examination is common. As the disease progresses, patient may experience various symptoms, including irregular vaginal bleeding, vaginal discharge, abdominal mass, and paroxysmal hypogastric pain, which pose a significant risk to the patient’s health (34, 35). Endometrial cancer incidence is higher among perimenopausal and postmenopausal women. While the disease is primarily related to hormonal factors, menstrual and reproductive history, and lifestyle factors are also involved (35, 36). Dysregulation of the uterine endocrine system, such as progesterone deficiency and estrogen excess, can lead to continuous stimulation of the endometrium, resulting in endometrial hyperplasia, menstrual irregularities, and eventually, endometrial cancer (37). Epidemiological studies have demonstrated that unhealthy lifestyle behaviors such as overeating, smoking, and alcohol consumption are significantly associated with endometrial cancer. Patients with an unhealthy lifestyle exhibit lower estrone and estradiol levels while having a higher incidence of endometrial cancer (38–40). Moreover, recent studies suggest that certain reproductive factors, such as delayed menopause, nulliparity, and never have given birth, are related to endometrial cancer development. Delayed menopause prolongs the endometrial exposure to estrogen, consequently increasing the risk of developing the disease. Conversely, pregnancy protects the endometrium from estrogen stimulation and consequently reduces endometrial cancer risk (41, 42).
2.3 Ovarian cancer and pathogenic factors
Ovarian cancer is the third most common malignancy affecting the female reproductive system, with the highest mortality rate among all types of gynecological tumors (43, 44). The clinical manifestations of ovarian cancer include persistent distending pain, irregular menstruation, emaciation, a lump in the lower abdomen, and ascites (45). This type of cancer mainly occurs in perimenopausal women, and its etiology remains obscure due to the complex interactions between embryonic development and endocrine function. It is generally attributed to dietary and nutritional disorders, poor living habits, chemical, physical, and carcinogenic biological factors, endocrine, hereditary, and psychological factors (46, 47). Research studies have indicated that women who experience early menstruation and delayed menopause are more susceptible to ruptures on the ovarian surface during each ovulation. Abnormal repairs that occur during the subsequent repair process, owing to the decline in endocrine function, can increase the risk of ovarian cancer (48, 49). Furthermore, studies have demonstrated an association between ovarian cancer and adverse emotional states, such as anxiety and depression. These emotions may adversely affect the body’s endocrine system, leading to an imbalance in ovarian endocrine function and ultimately resulting in cancer (50, 51). In addition, research has shown that the use of hormone drugs is also associated with a higher incidence of ovarian cancer (52, 53).
3 Assessment and diagnosis of pain
Patients experiencing cancer pain often report it as a subjective feeling that is evaluated comprehensively based on its location, degree, and duration. Various assessment tools are commonly used in the clinic, such as McMillan’s Pain Assessment Form, Visual Analog Scale, and Wong-Banker Facial Expression Scale. The selection of an appropriate assessment method should depend on the patient’s physical condition, cultural background, and level of consciousness (54).
3.1 The mechanism of chronification process of pain
The chronification process of pain in gynecological cancer patients is complex and involves the interaction of various mechanisms. Firstly, ongoing tissue damage and inflammation can lead to the sensitization of peripheral nociceptors, resulting in increased pain sensitivity and decreased pain thresholds. This can lead to a self-perpetuating cycle of pain, as the continuous stimulation of nociceptors can lead to changes in their excitability and trigger the release of pro-inflammatory mediators, intensifying the pain response (55, 56). Secondly, the central nervous system (CNS) can undergo neuroplastic changes in response to chronic pain. These changes can lead to altered pain perception, making pain feel more intense and difficult to control. Neuroplastic changes can occur at various levels of the CNS, including the spinal cord and brain, and can involve altered activity in pain-processing regions and disrupted inhibitory pathways (57, 58). Thirdly, psychosocial factors such as anxiety, depression, and stress can also contribute to the chronification of pain in gynecological cancer patients. These factors can affect pain perception and increase pain sensitivity, as well as impair coping strategies and quality of life. The relationship between pain and psychosocial factors is bidirectional, with pain exacerbating psychosocial symptoms, and psychosocial symptoms exacerbating pain (59, 60). These mechanisms work together to contribute to the chronification of pain in gynecological cancer patients. Effective pain management strategies in these patients may involve a multifaceted approach that targets peripheral and central sensitization, as well as psychosocial factors (61).
3.2 Standardized management of pain
Pain is a pervasive phenomenon that can cause physical discomfort and psychological distress in patients, ultimately leading to a reduction in their overall quality of life. Effective pain control is, therefore, of paramount importance for ensuring the well-being of patients. Nurses play a crucial role in pain management and their care has been shown to yield significant benefits (62). In recent years, many hospitals have been implementing pain management measures to minimize negative outcomes in physical and psychological states. Pain management aims to optimize analgesic efficacy while minimizing adverse drug reactions and avoiding inappropriate drug administration (63, 64). There have been two significant shifts in the management of pain in cancer patients. Firstly, there was a transition from pain control to pain management. Secondly, there has been a gradual shift in the personnel involved in pain management, from the original anesthesiologist-based treatment model to the nurse-based care model (65). Nurses should be responsible for pain assessment, analgesic treatment, education, and promotion. Presently, cancer pain management faces many challenges due to the multifactorial and complex nature of cancer pain itself. As a result, clinical management of this particular type of pain primarily relies on drugs (66, 67). Acceptable treatment options for cancer pain in patients include over-the-counter analgesics, non-opioid prescription medications, interventions, complementary therapies, and systemic opioids. Although the World Health Organization (WHO) recommends the three-step analgesic method due to its effectiveness, some patients may seek non-pharmacological treatment due to an aversion to treatment-related adverse effects and a fear of developing addiction (68). Studies have explored the roles of various integrative medicine therapies, such as mind-body practices, acupuncture, massage therapy, and music therapy, in cancer pain management. Data from randomized controlled trials have provided support for the efficacy of hypnosis, acupuncture, and music therapy in reducing pain (69). Nonetheless, 60% of patients still suffer from pain that cannot be effectively managed due to the diverse symptoms they experience despite the development and study of multiple pain management strategies and approaches (70).
3.3 Standardized diagnosis and treatment system in pain clinic
Effective pain management is a critical aspect of cancer patients’ rehabilitation and palliative care. The pain clinic’s management plays an essential role in ensuring standardized pain diagnosis and treatment. It functions as a crucial link and bridge between inpatient and outpatient care. Standardized clinic treatment can enhance the efficacy of treatment while improving patient satisfaction with the quality of medical care (70). The development of pain clinics can facilitate pain control, thereby enhancing the quality of pain diagnosis and treatment services provided to outpatients. Therefore, outpatient management is of utmost importance in the standardized treatment of pain.
4 Management of pain
4.1 Integrative care of cancer pain treated with drugs
As per the treatment protocol for cancer pain recommended by the World Health Organization (WHO), non-opioid analgesics, weak opioids, and strong opioids are prescribed for patients with mild, moderate, and severe advanced cancer pain, respectively. The representative drugs for each category are aspirin, codeine, and morphine, respectively (71, 72). During medication, it is imperative to adhere to the prescribed dosage and follow the doctor’s instructions. Patient-specific pain evaluation is crucial to customize the treatment plan, and the selection of analgesic drugs should follow the principle of gradual escalation from weak to strong and from fewer to more potent medications. Whenever feasible, oral medications should be considered to minimize the risk of intravenous complications, ensure improved pain management, and adherence to medication (73). The treatment outcomes and adverse effects should be vigilantly documented, and the management of any associated symptoms should be addressed accordingly. If necessary, medication changes may be considered.
4.2 Integrative care for non-drug treatment of cancer pain
Non-pharmacological interventions are recommended for management of cancer pain, which include minimally invasive interventional therapy and physical therapy. Pain due to tumor infiltration and invasion of peripheral sensory nerves is characterized by acuteness, persistence, and progressive aggravation. Mild stimulation can cause severe pain, which can seriously affect patients’ psychological and physiological functions and reduce patient compliance with treatment, posing a barrier to comprehensive treatment of patients (74, 75). For such patients, minimally invasive interventional therapy is recommended. Various physical or chemical methods can be utilized to block the corresponding sensory nerves, under guidance of ultrasound, C-arm X-ray machine or computer tomography, to effectively eliminate malignant pain and manage clinical symptoms (76, 77). Nursing staff should actively collaborate with clinical doctors to provide adequate treatment and care for patients. Accurate judgment of the nature and location of the cancer pain is important to carry out preoperative preparation, implement thorough disinfection protocols, carefully record post-treatment pain relief, and provide timely feedback. Physical therapy methods for cancer pain management include microwave, infrared ray, electrical stimulation, heat treatment, etc., which have shown effectiveness in alleviating symptoms of cancer pain. Appropriate physiotherapy methods should be selected based on the location, severity, and other characteristics of the patient’s cancer pain, to achieve specific goals (78). Furthermore, traditional Chinese medicine therapy, guided imagery, music therapy and acupuncture therapy also provide relief in managing malignant pain amongst patients with gynecological malignant tumors.
4.3 Mental nursing
Patients with advanced gynecological malignancies often experience negative emotions such as pessimism, anxiety, fear, and depression, which can significantly reduce their quality of life and hinder the effectiveness of treatment (79–81). In order to address the psychological needs of these patients, it is recommended that positive psychological nursing interventions be implemented. These interventions may include establishing a supportive treatment environment, providing education on positive psychology and health, offering empathetic listening and psychological counseling, utilizing relaxation therapy, providing cognitive guidance, facilitating regular experience sharing, and engaging the support of family members (82). Research suggests that creating a comfortable treatment environment can promote emotional well-being, improve treatment outcomes, and enhance patients’ ability to manage cancer-related pain (83). Regular psychoeducation, health education, and cognitive-behavioral intervention are crucial for introducing patients to knowledge about their illness, alleviating anxiety and fear, enhancing treatment confidence, and improving treatment adherence (paragraph 1 modified). This process also enables the examination of the unique psychological characteristics of patients so that targeted interventions can be applied, providing guidance, inspiration, and social support to improve the treatment efficacy of pain in cancer patients. Employing active listening techniques, providing counseling, and promoting regular exchange of experiences can effectively mitigate the emotional burden experienced by patients, reduce their sense of fear and loneliness, facilitate access to social support, bolster confidence in treatment, establish a sense of hope, and increase treatment efficacy. However, the cooperation and understanding of family members are paramount to patients’ treatment and rehabilitation. Establishing an open communication channel and involving family members in the treatment can contribute to their improved understanding of patients’ condition, treatment approaches, and objectives (84). It can also guide them to cooperate with the diagnosis and treatment of the patients, provide more psychological support and care to the patients, thus contributing to improving the treatment effect of the patients’ cancerous pain (83).
4.4 Physical nursing
Patients who are at risk of developing pressure sores, respiratory, urinary tract, skin infections, muscle atrophy, and metastasis site symptoms, among others, should receive targeted nursing interventions (85, 86). Those who are confined to bed for prolonged periods or require a fixed position can benefit from an air cushion bed and a turn-over schedule. Regular repositioning should be provided, and skin integrity at compression sites should be monitored to prevent pressure ulcers and infections. Additionally, nursing staff should encourage or assist patients to mobilize their lower limbs effectively to prevent venous thrombosis and reduce the incidence of muscle atrophy (87). Moreover, ensuring optimal oral and perineal hygiene in patients is crucial in decreasing the risk of lung, skin, and pelvic infections. Patients who can move independently should be encouraged to engage in regular mobility by getting out of bed regularly, exposing themselves to fresh air, and moving their limbs appropriately to minimize complications such as infection, thrombosis, and pain-related discomfort (60).
4.5 Psychosocial interventions
Psychosocial interventions had meaningful effects on both pain severity and interference (88). Meanhiwle, psychosocial interventions, such as cognitive-behavioral therapy, relaxation and experience intervention, are associated with fewer side effects and should be part of multimodal pain management methods (89). As recommended in a recent Institute of Medicine (IOM) report and guidelines of the American Pain Society, the use of psychosocial interventions as part of a multimodal approach to the treatment of cancer-related pain and the inclusion of experts in psychosocial care should be included as members of the multidisciplinary treatment team (89). In short, psychosocial interventions, including skills instruction and education, can improve cancer pain management.
4.6 Continuous care for patients with pain
In recent years, significant advancements have been made in comprehending and treating pain globally. In various regions, extensive research involving continuous care for diverse chronic ailments such as diabetic chronic obstructive pulmonary disease has been conducted and yielded positive outcomes (90). Additionally, studies indicate that patients who underwent continuous care display remarkable enhancement in their ability to manage pain independently at home. Continuous care administration not only elevates the percentage of pain control, but also serves to remind patients to take medication promptly and rectify discrepancies in medication instructions, thereby standardizing the medication guide for patients following discharge from the hospital. Through collaborative interdisciplinary teamwork and pain patient symposia, pain patients are provided with a platform for mutual communication which facilitates their systematic, prompt, and continual treatment, allowing for more accurate self-evaluation of pain score. The above measures can effectively enhance medication compliance in pain patients, prevent and treat adverse reactions more effectively, promote the standardized treatment of pain, increase patient satisfaction, and ultimately improve the relief effect of pain and their quality of life.
5 Nursing role in pain management
5.1 Standardized pain management
5.1.1 Health care personnel
Pain management is an essential aspect of patient care, yet it often receives inadequate attention in the medical field. Given that pain is widely prevalent among patients, it is crucial to improve healthcare professionals’ knowledge and competence in this area. Various studies have shown that many nurses in level-1 or level-2 hospitals lack sufficient knowledge of pain assessment methods, particularly when managing cancer patients. As a result, effective pain management is often compromised. Moreover, the lack of time and resources, and the wide range of clinical duties, often limit healthcare professionals’ capacity to provide critical health education and resources to pain-suffering patients and their families.
5.1.2 Patient-level factors
The lack of knowledge about pain management among patients and their families often results in patients deliberately enduring pain, as they consider it as a normal experience, without promptly notifying their healthcare providers. This subsequently leads to a delay in receiving the necessary analgesic treatment. Further, several surveys have reported that patients hold a misconception regarding the use of analgesics leading to addiction. This impression causes many patients to discontinue the use of analgesics to avoid dependence and increased drug dosages. The cost of treatment also poses a significant concern for patients, which can result in not adhering to appropriate analgesic therapy.
5.1.3 Lack of medical humanistic thought
As society’s economic status has advanced, the medical profession has similarly progressed. Modern physicians possess exceptional diagnostic and therapeutic capabilities, as well as psychological counseling skills, which enable them to provide personalized treatment regimens tailored to individual patients. It is imperative to emphasize people-oriented thinking and implement standardized pain diagnosis and treatment approaches that prioritize psychological support for patients and their families. This approach aims to assist patients in properly comprehending pain and ultimately achieving effective pain control, thus improving their quality of life. Encouraging patients and caregivers to actively participate in the decision-making process is also recommended as a fundamental component of effective pain management.
5.2 Establishment of standardized diagnosis and treatment system in tumor pain clinic
Outpatient pain management is a crucial component in the standardized management of cancer pain diagnosis and treatment, which has yielded some favorable outcomes. Nonetheless, practical observations indicate that some patients continue to experience moderate to severe pain even after being discharged, and the primary reasons for this are as follows:
① Assessing pain in patients in real-time presents a notable challenge. Studies have demonstrated that pain is a subjective phenomenon and that the most reliable and efficacious way to assess it is through the patient’s self-report. Notwithstanding, it is often the case that logistical barriers prevent patients from seeking in-person medical attention, particularly in instances of protracted illness or advanced age. Under such circumstances, family members may be designated as proxies, attending pain clinics in lieu of the patient. Nevertheless, the accuracy of pain assessment and the efficacy of any resultant therapeutic interventions may be compromised by the inability of family members to provide a faithful account of the patient’s pain experience.
② The follow-up work was not satisfactory. At present, the follow-up work is only completed by the hospital alone, while most patients return to the local community or family after discharge from the hospital where there is no mature continuous service. It is difficult to guarantee the follow-up rate at 100%, resulting in a majority of patients still suffer pain at home. It is of great importance to establish medical association between community and tertiary hospitals. Additionally, there are problems that the researchers do not have enough awareness and attention of the continuous care, content of continuous nursing remains simple, health education is lack of individualization, research on continuous nursing is not advisable and the system is not perfect, which are issues in need of attention in the future.
③ Currently, there is a lack of established demonstration wards for standardized pain treatment, resulting in non-uniformity in clinical pain treatment practices and unresolved issues. Despite the emphasis on individualized treatment, the current state of pain treatment is plagued by several challenges, including primary-stage pain treatment in economically less-developed regions, common instances of inadequate pain treatment, and insufficient familiarity and practical experience with analgesics among clinical medical staff. Moreover, the absence of evidence-based medical evidence exacerbates the aforementioned challenges, rendering the standardization of pain treatment elusive. These challenges signal the imperative need for demonstration wards with standardized pain treatment protocols to facilitate effective clinical management, thereby promoting standardization, and mitigating pain occurrences.
④ Continuous care for patients with pain is not performed. In the standardized treatment of pain, nursing staffs play a very important role, for the reason that most cancerous pain is a chronic disease with a long span, and patients often experience aggravation or recurrence of pain due to lack of standard guidance after discharge from hospital. Reports have shown that standardized management of pain-suffered patients should extend beyond the hospital to better ease their suffering. In the future, nursing staffs are supposed to strengthen the continuous care for patients with pain to ensure that the treatment of pain can be effectively continued.
5 Conclusion
Gynecological malignancy is a prevalent form of cancer that affects the human body. The development and emergence of this disease is primarily linked to several factors, including reproductive history, sexual age, sexual behavior, menstrual history, endocrine function impairments, infections, smoking, excessive alcohol consumption, and other unhealthy habits (91). The medical field is continuously introducing innovative concepts, methodologies, and technologies, which in turn improves understanding of gynecological malignancies. It is rational to surmise that the disease’s prevention could be achievable in the future (92).
Patients diagnosed with advanced gynecological malignancies, including cervical cancer, endometrial cancer, and ovarian cancer, experience varying degrees of physical pain. This pain significantly impacts the psychological and physiological wellbeing of patients, ultimately compromising the efficacy of treatment. Consequently, the appropriate diagnosis and management of pain are of utmost importance to improve patient outcomes and reduce suffering (93). The management of cancer-related pain involves the implementation of targeted treatments that include drug and non-pharmacological interventions, as dictated by the underlying etiology of the primary disease. Optimal patient care also requires the provision of positive nursing measures to enhance patients’ psychological well-being and foster their confidence in managing pain associated with cancer (94). Implementing drug analgesia and minimally invasive interventional treatment individually can reduce infection, thrombosis and related pain caused by improper posture and hygiene habits. Nurses play a very important role in the pain management of patients with advanced gynecological malignant tumors, including assessing the degree of malignant pain, implementing pain relief measures, assisting clinicians, guiding patients and their families (95). It is imperative to recognize the crucial role of nursing interventions in the management of cancer-related pain in patients with advanced gynecological malignancies. Therefore, nursing staff must possess a profound understanding of advanced gynecological malignancies, including comprehensively assessing the patient and being familiar with pertinent evaluation methods. Additionally, nurses should possess expert knowledge regarding analgesic techniques and strategies, specifically related to the management of pain in the context of advanced gynecological malignant tumor. Nursing interventions should also emphasize the importance of effective communication, and psychological counseling to ensure an evidence-based approach to promote optimal patient outcomes. As a result, nursing staff should adapt to emerging medical models and strive to enhance their overall medical expertise. To improve the quality of life for patients with advanced gynecological malignant tumor, nursing staffs are required to accurately evaluate and record cancer pain incidence, selecting personalized treatment plan, engaging in psychological nursing, advocating health education and effective communication, as well as carrying out appropriate body nursing, all of which can contribute to reducing pain severity and enhancing pain tolerance in patients.
Author contributions
Original draft preparation, allocation: WW and XH, Manuscript revision, supplement and edition: SL, MJ, and YN. All authors contributed to the article and approved the submitted version.
Acknowledgments
We thank the generous support by Liaoning Cancer Hospital and Institute (Shenyang).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Dubbins PA, Subba B. Screening for gynecological malignancy. Semin Ultrasound CT MR (1999) 20(4):231–8. doi: 10.1016/S0887-2171(99)90068-9
2. Wang Q, Peng H, Qi X, Wu M, Zhao X. Targeted therapies in gynecological cancers: a comprehensive review of clinical evidence. Signal Transduct Target Ther (2020) 5(1):137. doi: 10.1038/s41392-020-0199-6
3. Nielsen B, Kleppe A, Hveem TS, Pradhan M, Syvertsen RA, Nesheim JA, et al. Association Between Proportion of Nuclei With High Chromatin Entropy and Prognosis in Gynecological Cancers. J Natl Cancer Inst (2018) 110(12):1400–8. doi: 10.1093/jnci/djy063
4. Yetkin-Arik B, Kastelein AW, Klaassen I, Jansen C, Latul YP, Vittori M, et al. Angiogenesis in gynecological cancers and the options for anti-angiogenesis therapy. Biochim Biophys Acta Rev Cancer (2021) 1875(1):188446. doi: 10.1016/j.bbcan.2020.188446
5. Bayala B, Zoure AA, Zohoncon TM, Tinguerie BL, Baron S, Bakri Y, et al. Effects of extracts and molecules derived from medicinal plants of West Africa in the prevention and treatment of gynecological cancers. A Review Am J Cancer Res (2020) 10(9):2730–41.
6. Saavalainen L, Lassus H, But A, Tiitinen A, Harkki P, Gissler M, et al. A Nationwide Cohort Study on the risk of non-gynecological cancers in women with surgically verified endometriosis. Int J Cancer (2018) 143(11):2725–31. doi: 10.1002/ijc.31721
7. Di Tucci C, Schiavi MC, Faiano P, D'Oria O, Prata G, Sciuga V, et al. Therapeutic vaccines and immune checkpoints inhibition options for gynecological cancers. Crit Rev Oncol Hematol (2018) 128:30–42. doi: 10.1016/j.critrevonc.2018.05.011
8. Plow EB, Pascual-Leone A, Machado A. Brain stimulation in the treatment of chronic neuropathic and non-cancerous pain. J Pain (2012) 13(5):411–24. doi: 10.1016/j.jpain.2012.02.001
9. Juganavar A, Joshi KS. Chronic Pelvic Pain: A Comprehensive Review. Cureus. (2022) 14(10):e30691. doi: 10.7759/cureus.30691
10. Song W, Eaton LH, Gordon DB, Hoyle C, Doorenbos AZ. Evaluation of Evidence-based Nursing Pain Management Practice. Pain Manag Nurs (2015) 16(4):456–63. doi: 10.1016/j.pmn.2014.09.001
11. Levytska K, Pena SR, Brown J, Yu Z, Wally MK, Hsu JR, et al. Opioid and benzodiazepine use in gynecologic oncology patients. Int J Gynecol Cancer (2023) 33(5):786–91. doi: 10.1136/ijgc-2022-003955
12. Rodriguez C, Ji M, Wang HL, Padhya T, McMillan SC. Cancer Pain and Quality of Life. J Hosp Palliat Nurs (2019) 21(2):116–23. doi: 10.1097/NJH.0000000000000507
13. Deshpande M, Romanski PA, Rosenwaks Z, Gerhardt J. Gynecological Cancers Caused by Deficient Mismatch Repair and Microsatellite Instability. Cancers (Basel) (2020) 12(11):3319. doi: 10.3390/cancers12113319
14. Pourhanifeh MH, Darvish M, Tabatabaeian J, Fard MR, Mottaghi R, Azadchehr MJ, et al. Therapeutic role of curcumin and its novel formulations in gynecological cancers. J Ovarian Res (2020) 13(1):130. doi: 10.1186/s13048-020-00731-7
15. Vizza E, Chiofalo B, Cutillo G, Mancini E, Baiocco E, Zampa A, et al. Robotic single site radical hysterectomy plus pelvic lymphadenectomy in gynecological cancers. J Gynecol Oncol (2018) 29(1):e2. doi: 10.3802/jgo.2018.29.e2
16. Polastro L, Closset C, Kerger J. Immunotherapy in gynecological cancers: where are we? Curr Opin Oncol (2020) 32(5):459–70. doi: 10.1097/CCO.0000000000000661
17. Matanes E, Gotlieb WH. Immunotherapy of gynecological cancers. Best Pract Res Clin Obstet Gynaecol (2019) 60:97–110. doi: 10.1016/j.bpobgyn.2019.03.005
18. Kwolek DG, Gerstberger S, Tait S, Qiu JM. Ovarian, Uterine, and Vulvovaginal Cancers: Screening, Treatment Overview, and Prognosis. Med Clin North Am (2023) 107(2):329–55. doi: 10.1016/j.mcna.2022.10.016
19. Keyvani V, Kheradmand N, Navaei ZN, Mollazadeh S, Esmaeili SA. Epidemiological trends and risk factors of gynecological cancers: an update. Med Oncol (2023) 40(3):93. doi: 10.1007/s12032-023-01957-3
20. Stasenko M, Tarney C, Seier K, Casablanca Y, Brown CL. Sexual harassment and gender discrimination in gynecologic oncology. Gynecol Oncol (2020) 159(2):317–21. doi: 10.1016/j.ygyno.2020.08.014
21. Somigliana E, Mangili G, Martinelli F, Noli S, Filippi F, Bergamini A, et al. Fertility preservation in women with cervical cancer. Crit Rev Oncol Hematol (2020) 154:103092. doi: 10.1016/j.critrevonc.2020.103092
22. Arbyn M, Xu L, Simoens C, Martin-Hirsch PP. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst Rev (2018) 5(5):CD009069. doi: 10.1002/14651858.CD009069.pub3
23. Ai Y, Zhu H, Xie C, Jin X. Radiomics in cervical cancer: Current applications and future potential. Crit Rev Oncol Hematol (2020) 152:102985. doi: 10.1016/j.critrevonc.2020.102985
24. Ayen A, Jimenez Martinez Y, Boulaiz H. Targeted Gene Delivery Therapies for Cervical Cancer. Cancers (Basel) (2020) 12(5):1301. doi: 10.3390/cancers12051301
25. Bogani G, Leone Roberti Maggiore U, Signorelli M, Martinelli F, Ditto A, Sabatucci I, et al. The role of human papillomavirus vaccines in cervical cancer: Prevention and treatment. Crit Rev Oncol Hematol (2018) 122:92–7. doi: 10.1016/j.critrevonc.2017.12.017
26. Park SH, Kim M, Lee S, Jung W, Kim B. Therapeutic Potential of Natural Products in Treatment of Cervical Cancer: A Review. Nutrients. (2021) 13(1):154. doi: 10.3390/nu13010154
27. Wendel Naumann R, Leath CA 3rd. Advances in immunotherapy for cervical cancer. Curr Opin Oncol (2020) 32(5):481–7. doi: 10.1097/CCO.0000000000000663
28. Adiga D, Eswaran S, Pandey D, Sharan K, Kabekkodu SP. Molecular landscape of recurrent cervical cancer. Crit Rev Oncol Hematol (2021) 157:103178. doi: 10.1016/j.critrevonc.2020.103178
29. Guo L, Hua K. Cervical Cancer: Emerging Immune Landscape and Treatment. Onco Targets Ther (2020) 13:8037–47. doi: 10.2147/OTT.S264312
30. Balmagambetova S, Tinelli A, Mynbaev OA, Koyshybaev A, Urazayev O, Kereyeva N, et al. Human Papillomavirus Selected Properties and Related Cervical Cancer Prevention Issues. Curr Pharm Des (2020) 26(18):2073–86. doi: 10.2174/1381612826666200422094205
31. Wenzel HHB, Smolders RGV, Beltman JJ, Lambrechts S, Trum HW, Yigit R, et al. Survival of patients with early-stage cervical cancer after abdominal or laparoscopic radical hysterectomy: a nationwide cohort study and literature review. Eur J Cancer (2020) 133:14–21. doi: 10.1016/j.ejca.2020.04.006
32. Berger AA, Dao F, Levine DA. Angiogenesis in endometrial carcinoma: Therapies and biomarkers, current options, and future perspectives. Gynecol Oncol (2021) 160(3):844–50. doi: 10.1016/j.ygyno.2020.12.016
33. Javadian P, Nezhat F. Endometrial Carcinoma and its Precursors. Adv Exp Med Biol (2020) 1242:59–72. doi: 10.1007/978-3-030-38474-6_4
34. Huvila J, Pors J, Thompson EF, Gilks CB. Endometrial carcinoma: molecular subtypes, precursors and the role of pathology in early diagnosis. J Pathol (2021) 253(4):355–65. doi: 10.1002/path.5608
35. Wortman BG, Nout RA, Bosse T, Creutzberg CL. Selecting Adjuvant Treatment for Endometrial Carcinoma Using Molecular Risk Factors. Curr Oncol Rep (2019) 21(9):83. doi: 10.1007/s11912-019-0825-z
36. Bell DW, Ellenson LH. Molecular Genetics of Endometrial Carcinoma. Annu Rev Pathol (2019) 14:339–67. doi: 10.1146/annurev-pathol-020117-043609
37. McAlpine J, Leon-Castillo A, Bosse T. The rise of a novel classification system for endometrial carcinoma; integration of molecular subclasses. J Pathol (2018) 244(5):538–49. doi: 10.1002/path.5034
38. Hussein YR, Soslow RA. Molecular insights into the classification of high-grade endometrial carcinoma. Pathology. (2018) 50(2):151–61. doi: 10.1016/j.pathol.2017.09.010
39. Bartosch C, Pires M, Jeronimo C, Lopes JM. The role of pathology in the management of patients with endometrial carcinoma. Future Oncol (2017) 13(11):1003–20. doi: 10.2217/fon-2016-0570
40. Palisoul M, Mutch DG. The clinical management of inoperable endometrial carcinoma. Expert Rev Anticancer Ther (2016) 16(5):515–21. doi: 10.1586/14737140.2016.1168699
41. Piulats JM, Guerra E, Gil-Martin M, Roman-Canal B, Gatius S, Sanz-Pamplona R, et al. Molecular approaches for classifying endometrial carcinoma. Gynecol Oncol (2017) 145(1):200–7. doi: 10.1016/j.ygyno.2016.12.015
42. Zhou JY, Zhang L, Wei LH, Wang JL. Endometrial carcinoma-related genetic factors: application to research and clinical practice in China. BJOG. (2016) 123 Suppl 3:90–6. doi: 10.1111/1471-0528.14007
43. Yang Q, Yang Y, Zhou N, Tang K, Lau WB, Lau B, et al. Epigenetics in ovarian cancer: premise, properties, and perspectives. Mol Cancer (2018) 17(1):109. doi: 10.1186/s12943-018-0855-4
44. Christie EL, Bowtell DDL. Acquired chemotherapy resistance in ovarian cancer. Ann Oncol (2017) 28(suppl_8):viii13–viii5. doi: 10.1093/annonc/mdx446
45. Ledermann JA. Front-line therapy of advanced ovarian cancer: new approaches. Ann Oncol (2017) 28(suppl_8):viii46–50. doi: 10.1093/annonc/mdx452
46. Marth C, Reimer D, Zeimet AG. Front-line therapy of advanced epithelial ovarian cancer: standard treatment. Ann Oncol (2017) 28(suppl_8):viii36–viii9. doi: 10.1093/annonc/mdx450
47. Odunsi K. Immunotherapy in ovarian cancer. Ann Oncol (2017) 28(suppl_8):viii1–7. doi: 10.1093/annonc/mdx444
48. Pignata S, CC S, Du Bois A, Harter P, Heitz F. Treatment of recurrent ovarian cancer. Ann Oncol (2017) 28(suppl_8):viii51–viii6. doi: 10.1093/annonc/mdx441
49. Pogge von Strandmann E, Reinartz S, Wager U, Muller R. Tumor-Host Cell Interactions in Ovarian Cancer: Pathways to Therapy Failure. Trends Cancer (2017) 3(2):137–48. doi: 10.1016/j.trecan.2016.12.005
50. Karam A, Ledermann JA, Kim JW, Sehouli J, Lu K, Gourley C, et al. Fifth Ovarian Cancer Consensus Conference of the Gynecologic Cancer InterGroup: first-line interventions. Ann Oncol (2017) 28(4):711–7. doi: 10.1093/annonc/mdx011
51. An Y, Yang Q. Tumor-associated macrophage-targeted therapeutics in ovarian cancer. Int J Cancer (2021) 149(1):21–30. doi: 10.1002/ijc.33408
52. Funston G, Hardy V, Abel G, Crosbie EJ, Emery J, Hamilton W, et al. Identifying Ovarian Cancer in Symptomatic Women: A Systematic Review of Clinical Tools. Cancers (Basel) (2020) 12(12):3686. doi: 10.3390/cancers12123686
53. Yang J, Stack MS. Lipid Regulatory Proteins as Potential Therapeutic Targets for Ovarian Cancer in Obese Women. Cancers (Basel) (2020) 12(11):3469. doi: 10.3390/cancers12113469
54. Boz I, Teskereci G. Experiences of gynecologic oncology nurses regarding caring behaviors: a hermeneutic phenomenological study. J Psychosom Obstet Gynaecol (2021) 42(1):29–39. doi: 10.1080/0167482X.2020.1726316
55. Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain (2009) 10(9):895–926. doi: 10.1016/j.jpain.2009.06.012
56. Hooten WM. Chronic Pain and Mental Health Disorders: Shared Neural Mechanisms, Epidemiology, and Treatment. Mayo Clin Proc (2016) 91(7):955–70. doi: 10.1016/j.mayocp.2016.04.029
57. Yang S, Chang MC. Chronic Pain: Structural and Functional Changes in Brain Structures and Associated Negative Affective States. Int J Mol Sci (2019) 20(13):3130. doi: 10.3390/ijms20133130
58. Ji RR, Nackley A, Huh Y, Terrando N, Maixner W. Neuroinflammation and Central Sensitization in Chronic and Widespread Pain. Anesthesiology. (2018) 129(2):343–66. doi: 10.1097/ALN.0000000000002130
59. Cillessen L, Johannsen M, Speckens AEM, Zachariae R. Mindfulness-based interventions for psychological and physical health outcomes in cancer patients and survivors: A systematic review and meta-analysis of randomized controlled trials. Psychooncology. (2019) 28(12):2257–69. doi: 10.1002/pon.5214
60. Campos ACP, Antunes GF, Matsumoto M, Pagano RL, Martinez RCR. Neuroinflammation, Pain and Depression: An Overview of the Main Findings. Front Psychol (2020) 11:1825. doi: 10.3389/fpsyg.2020.01825
61. Ji RR, Chamessian A, Zhang YQ. Pain regulation by non-neuronal cells and inflammation. Science. (2016) 354(6312):572–7. doi: 10.1126/science.aaf8924
62. Littell RD, Kumar A, Einstein MH, Karam A, Bevis K. Advanced communication: A critical component of high quality gynecologic cancer care: A Society of Gynecologic Oncology evidence based review and guide. Gynecol Oncol (2019) 155(1):161–9. doi: 10.1016/j.ygyno.2019.07.026
63. Li D, Gao L, Ren LY, Zeng X, Cui EP, Zhang LJ, et al. Knowledge and attitudes regarding cancer pain management among oncology nurses in China. J Int Med Res (2021) 49(1):300060520979448. doi: 10.1177/0300060520979448
64. Hagedorn JM, Pittelkow TP, Hunt CL, D'Souza RS, Lamer TJ. Current Perspectives on Spinal Cord Stimulation for the Treatment of Cancer Pain. J Pain Res (2020) 13:3295–305. doi: 10.2147/JPR.S263857
65. Hochberg U, Perez J, Borod M. New frontier: cancer pain management clinical fellowship. Support Care Cancer (2018) 26(7):2453–7. doi: 10.1007/s00520-018-4085-5
66. Kwon JH. Overcoming barriers in cancer pain management. J Clin Oncol (2014) 32(16):1727–33. doi: 10.1200/JCO.2013.52.4827
67. Paice JA, Portenoy R, Lacchetti C, Campbell T, Cheville A, Citron M, et al. Management of Chronic Pain in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol (2016) 34(27):3325–45. doi: 10.1200/JCO.2016.68.5206
69. Deng G. Integrative Medicine Therapies for Pain Management in Cancer Patients. Cancer J (2019) 25(5):343–8. doi: 10.1097/PPO.0000000000000399
70. Vitzthum LK, Riviere P, Murphy JD. Managing Cancer Pain During the Opioid Epidemic-Balancing Caution and Compassion. JAMA Oncol (2020) 6(7):1103–4. doi: 10.1001/jamaoncol.2020.0779
71. Staley SA, Tucker KR, Clark LH. The Role of Obesity in the Development and Management of Gynecologic Cancer. Obstet Gynecol Surv (2020) 75(5):308–16. doi: 10.1097/OGX.0000000000000779
72. Kim CH, Lefkowits C, Holschneider C, Bixel K, Pothuri B. Managing opioid use in the acute surgical setting: A society of gynecologic oncology clinical practice statement. Gynecol Oncol (2020) 157(3):563–9. doi: 10.1016/j.ygyno.2020.01.024
73. Mitchell MT. Dancing with Deterrents: Understanding the Role of Abuse-Deterrent Opioid Formulations and Naloxone in Managing Cancer Pain. Oncologist. (2019) 24(12):1505–9. doi: 10.1634/theoncologist.2019-0340
74. Knisely A, Huang Y, Melamed A, Tergas AI, St Clair CM, Hou JY, et al. Effect of regionalization of endometrial cancer care on site of care and patient travel. Am J Obstet Gynecol (2020) 222(1):58 e1– e10. doi: 10.1016/j.ajog.2019.07.026
75. Schmidt M, Ditrio L, Shute B, Luciano D. Surgical management and gynecologic care of the transgender patient. Curr Opin Obstet Gynecol (2019) 31(4):228–34. doi: 10.1097/GCO.0000000000000553
76. Kiss N, Loeliger J, Findlay M, Isenring E, Baguley BJ, Boltong A, et al. Clinical Oncology Society of Australia: Position statement on cancer-related malnutrition and sarcopenia. Nutr Diet (2020) 77(4):416–25. doi: 10.1111/1747-0080.12631
77. Coleman RL, Monk BJ, Sood AK, Herzog TJ. Latest research and treatment of advanced-stage epithelial ovarian cancer. Nat Rev Clin Oncol (2013) 10(4):211–24. doi: 10.1038/nrclinonc.2013.5
78. Nguyen NH, Hadgraft NT, Moore MM, Rosenberg DE, Lynch C, Reeves MM, et al. A qualitative evaluation of breast cancer survivors' acceptance of and preferences for consumer wearable technology activity trackers. Support Care Cancer (2017) 25(11):3375–84. doi: 10.1007/s00520-017-3756-y
79. Beesley VL, Price MA, Butow PN, Green AC, Olsen CM, Australian Ovarian Cancer Study G, et al. Physical activity in women with ovarian cancer and its association with decreased distress and improved quality of life. Psychooncology. (2011) 20(11):1161–9. doi: 10.1002/pon.1834
80. Roland KB, Rodriguez JL, Patterson JR, Trivers KF. A literature review of the social and psychological needs of ovarian cancer survivors. Psychooncology. (2013) 22(11):2408–18. doi: 10.1002/pon.3322
81. Lin KY, Edbrooke L, Granger CL, Denehy L, Frawley HC. The impact of gynaecological cancer treatment on physical activity levels: a systematic review of observational studies. Braz J Phys Ther (2019) 23(2):79–92. doi: 10.1016/j.bjpt.2018.11.007
82. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep (1985) 100(2):126–31.
83. Tucker K, Staley SA, Clark LH, Soper JT. Physical Activity: Impact on Survival in Gynecologic Cancer. Obstet Gynecol Surv (2019) 74(11):679–92. doi: 10.1097/OGX.0000000000000731
84. Sonalkar S, Chavez V, McClusky J, Hunter TA, Mollen CJ. Gynecologic Care for Women With Physical Disabilities: A Qualitative Study of Patients and Providers. Womens Health Issues (2020) 30(2):136–41. doi: 10.1016/j.whi.2019.10.002
85. Yue J, Sun W, Li S. Denosumab versus zoledronic acid in cases of surgically unsalvageable giant cell tumor of bone: A randomized clinical trial. J Bone Oncol (2022) 35:100441. doi: 10.1016/j.jbo.2022.100441
86. Yue J, Aobulikasimu A, Sun W, Liu S, Xie W, Sun W. Targeted regulation of FoxO1 in chondrocytes prevents age-related osteoarthritis via autophagy mechanism. J Cell Mol Med (2022) 26(11):3075–82. doi: 10.1111/jcmm.17319
87. Beck A, Vind Thaysen H, Hasselholt Soegaard C, Blaakaer J, Seibaek L. Prehabilitation in cancer care: patients' ability to prepare for major abdominal surgery. Scand J Caring Sci (2021) 35(1):143–55. doi: 10.1111/scs.12828
88. Sheinfeld Gorin S, Krebs P, Badr H, Janke EA, Jim HS, Spring B, et al. Meta-analysis of psychosocial interventions to reduce pain in patients with cancer. J Clin Oncol (2012) 30(5):539–47. doi: 10.1200/JCO.2011.37.0437
89. Syrjala KL, Donaldson GW, Davis MW, Kippes ME, Carr JE. Relaxation and imagery and cognitive-behavioral training reduce pain during cancer treatment: a controlled clinical trial. Pain. (1995) 63(2):189–98. doi: 10.1016/0304-3959(95)00039-U
90. Gordon DB, Dahl JL, Miaskowski C, McCarberg B, Todd KH, Paice JA, et al. American pain society recommendations for improving the quality of acute and cancer pain management: American Pain Society Quality of Care Task Force. Arch Intern Med (2005) 165(14):1574–80. doi: 10.1001/archinte.165.14.1574
91. Rayburn WF. Gynecologic Cancer Care: Innovative Progress. Obstet Gynecol Clin North Am (2019) 46(1):xiii–xiv. doi: 10.1016/j.ogc.2018.11.002
92. Pahlawanian AM, Norris VA, Jernigan AM, Morrell B, Morrell M, Nair N, et al. An Update on Screening and Prevention for Breast and Gynecological Cancers in Average and High Risk Individuals. Am J Med Sci (2020) 360(5):489–510. doi: 10.1016/j.amjms.2020.06.008
93. Rivera Dominguez A, Mora Jurado A, Garcia de la Oliva A, de Araujo Martins-Romeo D, Cueto Alvarez L. Gynecological pelvic pain as emergency pathology. Radiologia. (2017) 59(2):115–27. doi: 10.1016/j.rx.2016.09.010
94. Wang WY, Chu CM, Sung CS, Ho ST, Wu YS, Liang CY, et al. Using a New Measurement to Evaluate Pain Relief Among Cancer Inpatients with Clinically Significant Pain Based on a Nursing Information System: A Three-Year Hospital-Based Study. Pain Med (2016) 17(11):2067–75. doi: 10.1093/pm/pnw026
Keywords: gynecology, malignant tumor, cancer pain, nursing, psychology of pain
Citation: Wu W, He X, Li S, Jin M and Ni Y (2023) Pain nursing for gynecologic cancer patients. Front. Oncol. 13:1205553. doi: 10.3389/fonc.2023.1205553
Received: 14 April 2023; Accepted: 11 July 2023;
Published: 26 July 2023.
Edited by:
Carole Helissey, Hôpital d’Instruction des Armées Bégin, FranceReviewed by:
Raquel Chacon Ruiz Martinez, Hospital Sirio Libanes, BrazilCopyright © 2023 Wu, He, Li, Jin and Ni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaodan He, bWFnZ2llMzM3N0AxNjMuY29t
 Wei Wu
Wei Wu Xiaodan He
Xiaodan He