- 1Department of Clinical Nutrition, Chongqing University Cancer Hospital, School of Medicine, Chongqing University, Chongqing, China
- 2Department of Geriatric Oncology and Department of Palliative Care, Chongqing University Cancer Hospital, School of Medicine, Chongqing University, Chongqing, China
Purpose: More effective approaches are needed to improve the prognosis of non-small-cell lung cancer (NSCLC) patients. Thus, we used the E-warm model to assess how early integration of interdisciplinary palliative care was related to the quality of life (QoL), psychological functioning, pain management, and nutrition factors of NSCLC patients.
Methods: This randomized controlled trial enrolled 280 newly diagnosed NSCLC patients, which were randomly divided (1:1) into combined early palliative care (CEPC) and standard oncological care (SC) groups. At baseline and after 24 weeks, the Functional Assessment of Cancer Therapy-Lung (FACT-L) scale, Hospital Anxiety and Depression Scale (HADS), and the Patient Health Questionnaire-9 (PHQ-9) were used to assess QoL and psychological function, respectively. The Numerical Rating Scale (NRS) and Patient-Generated Subjective Global Assessment (PG-SGA) were used to assess cancer patients’ pain and nutrition levels. The primary outcome was overall survival (OS). Secondary outcomes comprised changes in the QoL, psychological functioning, pain, and nutrition state. The intention-to-treat method was applied for analysis. This study was registered at www.chictr.org.cn (ChiCTR2200062617).
Results: Of the 140 patients enrolled in the CEPC and SC groups, 102 and 82 completed the research. The CEPC group presented higher QoL than the SC group (p < 0.05). Additionally, fewer patients presented depressive symptoms in the CEPC group than in the SC group (p < 0.05), as well as better nutritional status (p = 0.007) and pain management (p = 0.003). Compared to the SC group, CEPC patients had significantly longer OS (20.4 vs. 24.6 months, p = 0.042; HR: 0.19; 95% CI: 0.04-0.85, p = 0.029).
Conclusion: With combined early palliative care, NSCLC patients lived longer, had better QoL, were psychologically stable, were in less pain, and were more nutritionally satisfied.
Introduction
About 85% of lung cancers are non-small-cell lung cancers (NSCLC), which leads to a poor quality of life (QoL) and high symptom burdens (1–4). It is common for NSCLC patients to be diagnosed at an advanced stage and, therefore, lose the opportunity to undergo radical resection (5–7). Moreover, NSCLC patients are often malnourished, in pain, and psychologically distressed, contributing to poor QoL and short survival (8, 9). Thus, NSCLC patients need high-quality, low-medical-burden interventions to improve their QoL, nutrition, psychological well-being, and survival.
Palliative care focused on managing symptoms and providing psychosocial support can improve a patient’s quality of life and care (10, 11). For advanced cancer patients, palliative care has accumulated substantial evidence supporting its integration into oncology practice (12–15). There has been a rapid expansion in palliative care services worldwide, but China is experiencing a fundamentally different situation. Several factors contribute to the problem, including limited healthcare resources, policies, low awareness, and local cultural norms (16–19). Palliative care in China is still in its infancy (20, 21). In the greater China region, models of palliative care that delivered specialist palliative care services in various settings were reported (21), including hospitals (22), inpatient hospice units (23, 24), nursing home (25), and home-based care (26–28). Furthermore, few studies have focused on the collaborative experience of various specialists in early palliative care models, as well as the impact of China’s unique population characteristics and different regional cultural customs on palliative care. Therefore, in our endeavor to promote and develop a palliative care model tailored to the Chinese context, it is crucial to address the following aspects. In order to maintain the integrity and organization of the palliative care system, it is imperative to establish a comprehensive framework consisting of co-built wards, palliative communities, palliative homes, and hospices (29). Special emphasis should be placed on providing comprehensive support to patients and their families, ensuring their comfort, and offering ongoing assistance to survivors in their mourning process (29). Additionally, it is crucial to consider the influence of China’s distinct population characteristics and cultural customs across various regions on the implementation of palliative care. Consequently, developing an appropriate palliative care pattern for Chinese circumstances is urgently needed.
E-warm pattern interventions are interdisciplinary palliative care technologies considering Chinese culture and circumstances (30). The E-warm model is defined as Early, Whole, Assessment, Re-evaluation, and MDT Management by acknowledging and incorporating local culture and traditions into practices (30). By implementing the E-warm model, our primary objective is to establish a comprehensive palliative care system and procedure that embodies Chinese attributes, encompassing diverse professional teams and intervention cycles, in order to deliver comprehensive, holistic, family-centered, and continuous care to patients and their families. Herein, we investigated the effectiveness of the combined early palliative care for NSCLC patients on the QoL, psychological well-being, pain, and nutrition state.
Methods
Study design and patients
An open, randomized, controlled trial was conducted from October 7, 2019, to October 25, 2021, in newly diagnosed NSCLC patients at the Chongqing University Cancer Hospital in Chongqing, China. The inclusion criteria considered inpatients and outpatient, and patients could be followed up in an outpatient or inpatient setting after being recruited. The study was open to patients who had Stage IIIB to IV advanced NSCLC within eight weeks of enrollment, treatment naïve or have not received disease-directed treatments, were 18 years or older, had a baseline Eastern Cooperative Oncology Group (ECOG) from 0 to 2, had expected survival time at least 24 weeks and had sufficient reading and cognitive skills. Patients who have already received palliative care services were not eligible.
The Chongqing University University Cancer Hospital’s Ethics Committee approved this study (CZLS2019177), registered at http://www.chictr.org.cn/ (ChiCTR2200062617). The study design was not revised after it began.
Procedures
A flowchart of the combined early palliative care (CEPC) team process is shown in Supplementary Figure S1. The medical oncologists made medical decisions following the NCCN Guidelines and patient preferences (31). The E-warm model, which encompasses the principles of Early, Whole, Assessment, Re-evaluation, and MDT Management, is proposed (30). The term “Early” denotes the importance of early intervention, particularly in the context of advanced tumor patients, where early palliative care should be integrated into their anti-cancer treatment. The concept of “Whole” emphasizes the need for palliative care to be integrated throughout the entire cancer treatment process. “Evaluation” highlights the significance of dynamic assessment, allowing for continuous improvement of intervention strategies based on clinical feedback. Lastly, “MDT Management” underscores the necessity of Multi-Disciplinary Treatment being consistently applied throughout cancer treatment. In order to maintain the integrity and organization of the palliative care system, it is imperative to establish a comprehensive framework consisting of co-built wards, palliative communities, palliative homes, and hospices. Special emphasis should be placed on providing comprehensive support to patients and their families, ensuring their comfort, and offering ongoing assistance to survivors in their mourning process. Additionally, it is crucial to consider the influence of China’s distinct population characteristics and cultural customs across various regions on the implementation of palliative care. Currently, the E-warm model represents an initial palliative care approach that aligns with the aforementioned Chinese cultural customs and characteristics. The E-warm model focuses on establishing a palliative care system and procedure that incorporates Chinese characteristics, encompassing diverse professional teams and intervention cycles, in order to provide patients and their families with comprehensive, holistic, family-centered, and continuous care. For further details, please refer to the Supplementary Appendix.
A 1:1 randomization without stratification was used to assign eligible patients to either of the two groups within eight weeks of diagnosis. Professionals working for Palliative Care Services provided support and care for inpatients and outpatients. For 24 weeks, beginning within the first week of enrollment and continuing every month, patients met with a medical oncologist, an oncology nurse specialist, a dietitian, and a psychologist in the CEPC group. It was up to the patient, oncologist, or CEPC team to schedule additional palliative care visits. Randomly assigned SC patients did not have nutrition, pain, or psychology assessments except because of patient or oncologist requests. A single patient from the SC group did not cross over to the CEPC group if they received nutritional, psychological, or cancer pain consultations. Oncologic care was routinely provided to all study participants.
The early palliative care in the CEPC group focused on four basic elements: QoL, nutrition level, pain management, and psychological support (1). The QoL was evaluated by oncologists using the FACT-L scale, including the lung-cancer subscale (LCS) and Trial Outcome Index (TOI), which appraise the multidimensionality of the health-related QoL (function and symptom) (30) (2). Besides PG-SGA, dietitians assessed each patient’s nutritional intake, physical exams, and hematology tests. A nutritional intervention was initiated following the assessment results (3). Oncologists used an NRS to assess pain, and pain treatment was provided to the patient when necessary (4). The HADS, which evaluates anxiety (HADS-A) and depression (HADS-D) symptoms, and the Patient Health Questionnaire-9 (PHQ-9) were used by psychologists for psychological evaluations (8, 32). Psychologists provided psychotherapy to each patient and administered psychotropic medications when necessary.
The primary outcome was overall survival (OS). Secondary outcomes included changes in the QoL, nutrition state, pain, and psychological functioning. After enrollment, both groups were assessed every four weeks for QoL, nutritional level, pain status, and psychological factors. During CEPC weekly meetings, members discussed trial-related issues and potential solutions to improve the process to ensure all patients received coordinated interventions.
Statistical analysis
SPSS 22.0 was used to analyze the data. Descriptive statistics were used to estimate frequency distributions, means, and standard deviations. For categorical variables, Fisher’s exact and χ2 tests were used to assess differences between groups for baseline characteristics and clinical outcomes. Independent-sample Student’s t-tests were used for continuous variables. Kaplan-Meier plots and log-rank tests were performed to determine whether combining early palliative care with other forms of treatment led to better OS. Data were analyzed based on the intention-to-treat method. Patients were randomly assigned, including those who died or were not followed up. An intention-to-treat analysis was performed using the last observation as the outcome. A per-protocol analysis of participants who fulfilled the protocol’s eligibility requirements was performed (see Supplementary Table S1). Statistical significance was defined as p < 0.05.
Results
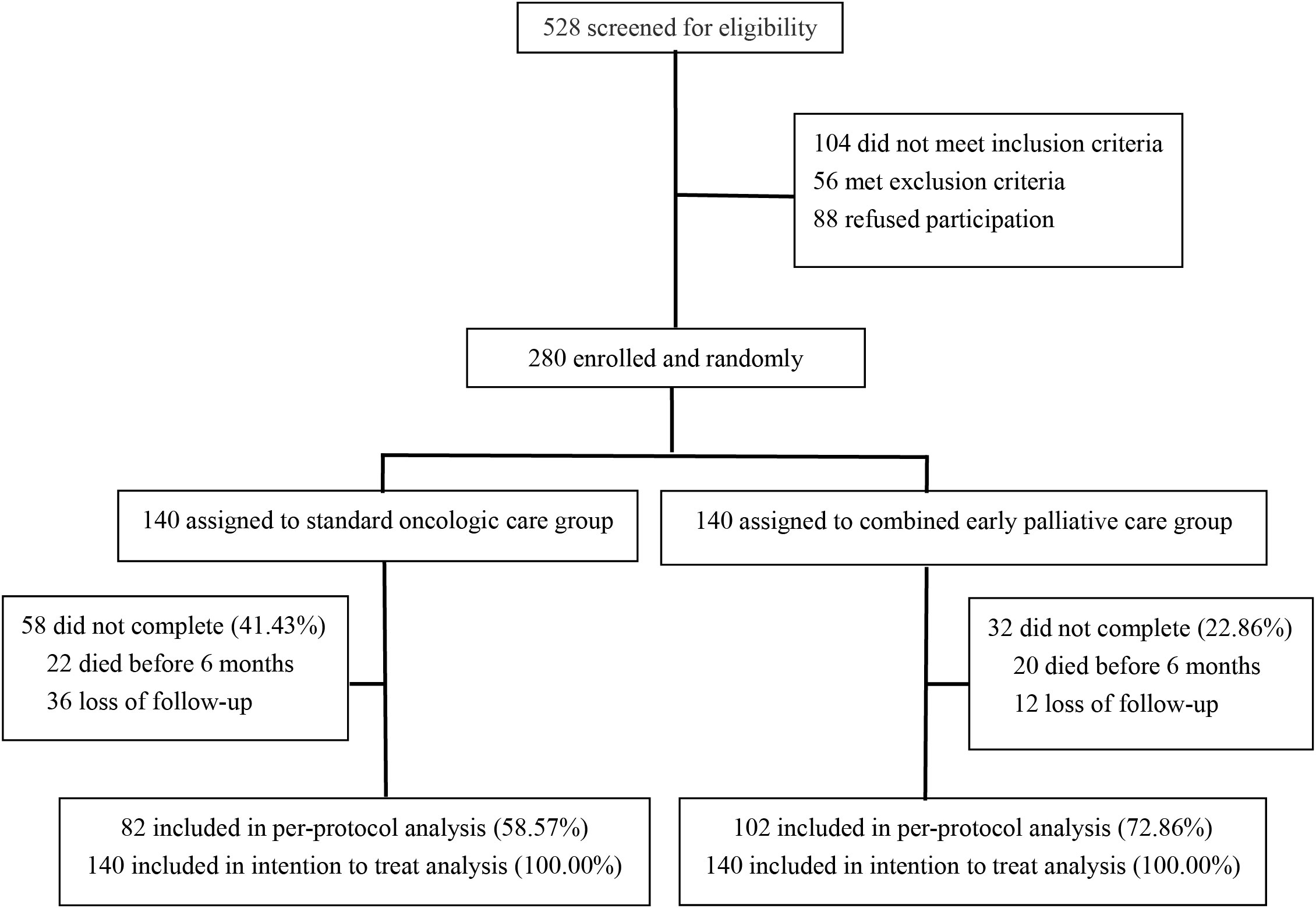
A total of 528 NSCLC patients were assessed for participation. Finally, 280 were enrolled and randomly (1:1) assigned to CEPC or standard oncologic care (Figure 1). Ultimately, all 280 patients were included in the intention-to-treat analysis, and 184 patients were analyzed per protocol, 102 in the CEPC group and 82 in the SC group. The compliance at 24 weeks was 72.86 and 58.57% in the CEPC and SC groups. Both groups had similar demographics and baseline clinical characteristics (Table 1). Between the SC and CEPC groups, 24.29% (34/140) vs. 60.71% (85/140) received nutritional consultations, 20.00% (28/140) vs. 22.14% (31/140) received psychological consultations, and 27.14% (38/140) vs. 40.00% (56/140) received pain medications over the 24 weeks. Additionally, 41.43% (58/140) of patients in the SC group and 22.86% (32/140) in the CEPC group were no longer being followed up or died at the cutoff date (April 25, 2022).
Baseline characteristics
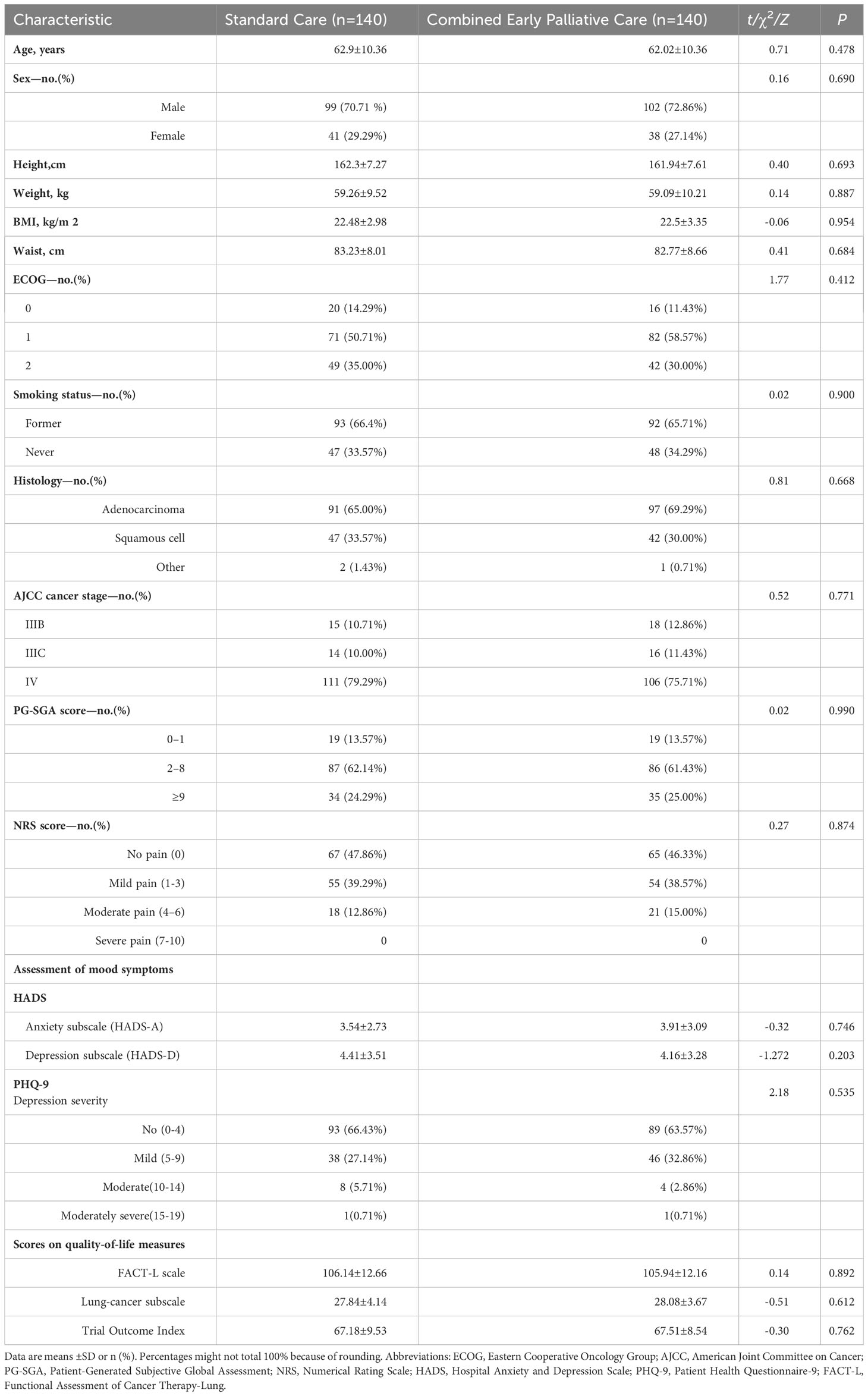
The baseline characteristics were similar for both groups (Table 1). Patients were matched on age, sex, height, weight, BMI, ECOG, smoking state, histology, and neoplasm staging. The groups did not differ regarding the baseline nutritional assessment, pain evaluation, emotional symptoms, or QoL (Table 1).
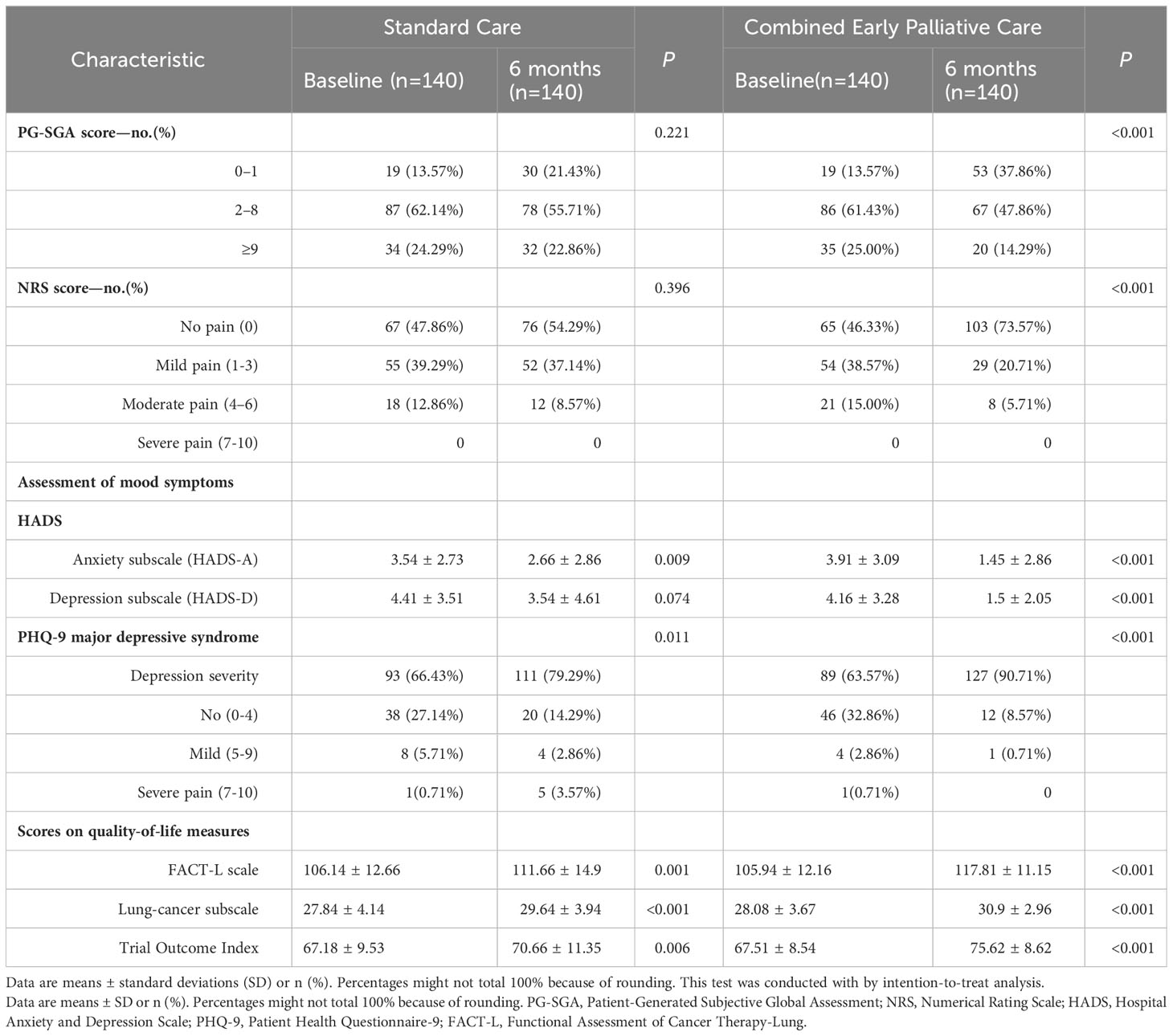
Key characteristics at baseline and 24 weeks
In the SC group, the baseline nutrition assessment and pain level did not significantly differ at baseline and after 24 weeks (Table 2). In contrast, the level of PG-SGA, NRS, HADS, PHQ-9, and QoL of the CEPC group markedly improved after 24 weeks (p < 0.05, Table 2). Subsequent analysis of participants who completed the 24-week intervention revealed no statistical differences in factors such as age, gender, and cancer stage between the SC group and CEPC group (see Supplementary Table S1).
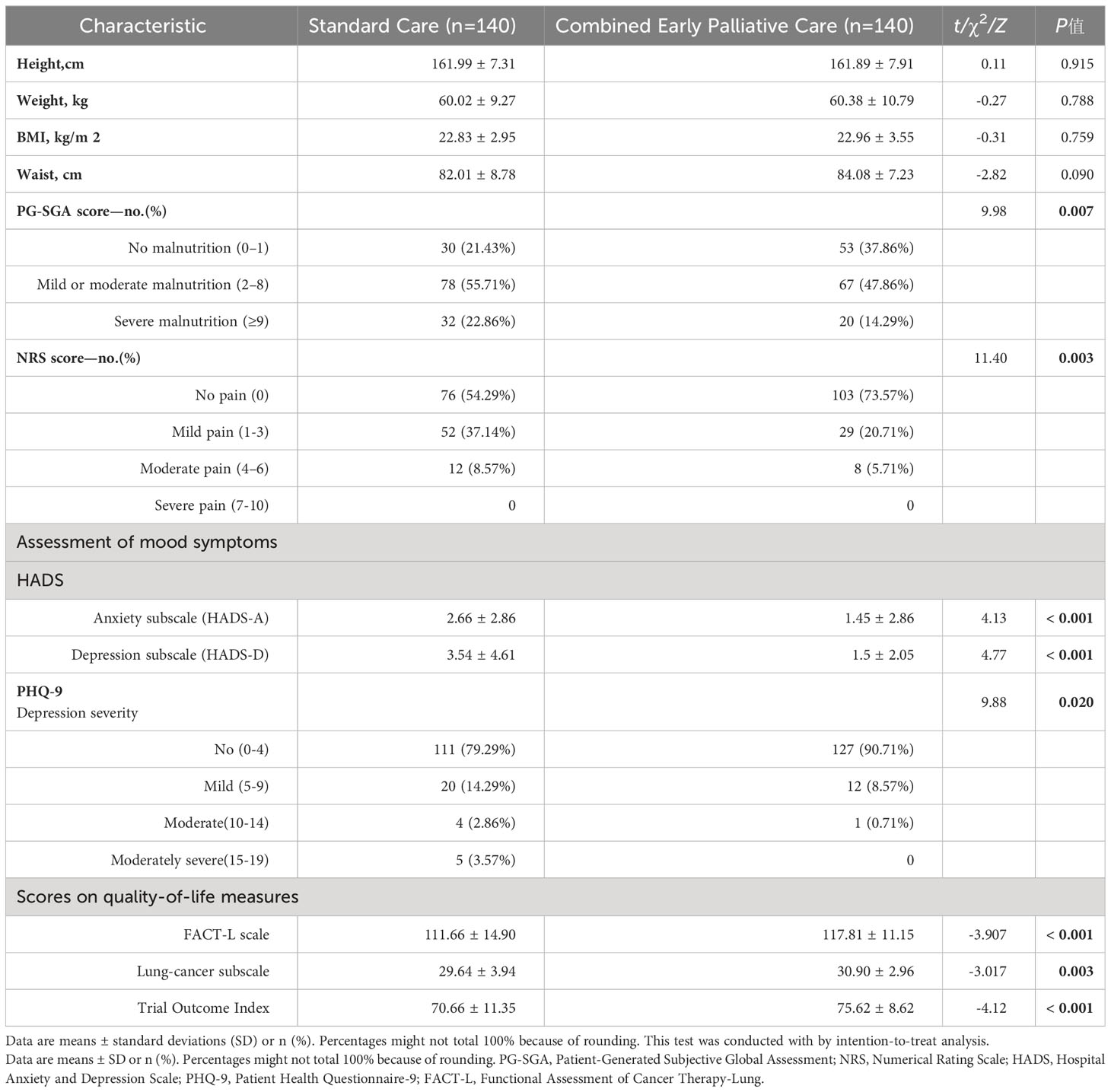
Nutrition, pain, mood symptoms, health-related QoL, and survival analysis
CEPC and SC patients were assessed by PG-SGA at baseline, and after 24 weeks, all participants were re-assessed. Additionally, the CEPC group (14.29 vs. 22.86%, severe malnutrition; 47.86 vs. 55.71%, moderate or mild malnutrition; and 37.86 vs. 22.86%, no malnutrition) had a better nutrition level than the SC group (p = 0.007) (Table 3). Moreover, the CEPC group had a much lower NRS score than the SC group after 24 weeks (p = 0.003) (Table 3).
Furthermore, the CEPC group had significantly lower levels of anxiety and depression at 24 weeks when assessed by both HADS and PHQ-9 (p < 0.05) than SC group patients. Nonetheless, the proportion of patients prescribed antidepressant drugs was similar (about 20%, p = 1.000). In the PHQ-9 depression severity test, the groups significantly differed, considering depression severity scores (p = 0.020). The per-protocol analyses showed similar results for HADS mood symptoms (Supplementary Table S1).
In the present study, a total of 15 patients (10.71%) in the SC group received palliative care consultations upon request, either by the patient or the oncologist, within the initial 24-week period. The primary purpose of these consultations was to address symptom management. Among these patients, 11 received a single visit, while 4 received two visits.
The combined early palliative care treatment significantly affected the QoL, improving not only the FACT-L scale (117.81 ± 11.15 vs. 111.66 ± 14.90; p < 0.001) but also the LCS (30.90 ± 2.96 vs. 29.64 ± 3.94; p = 0.003) and TOI (75.62 ± 8.62 vs. 70.66 ± 11.35; p < 0.001) than the SC group after 24 weeks (Table 3). From baseline to the 24th week, CEPC patients increased their mean FACT-L score by 11.77 points and SC patients by only 5.51 points (p < 0.001) (Figure 2). CEPC patients had significantly better survival than SC patients (median OS, 24.6 vs. 20.4 months, p = 0.042; HR, 0.19; 95% CI, 0.04 to 0.85, p = 0.029, Figure 3).
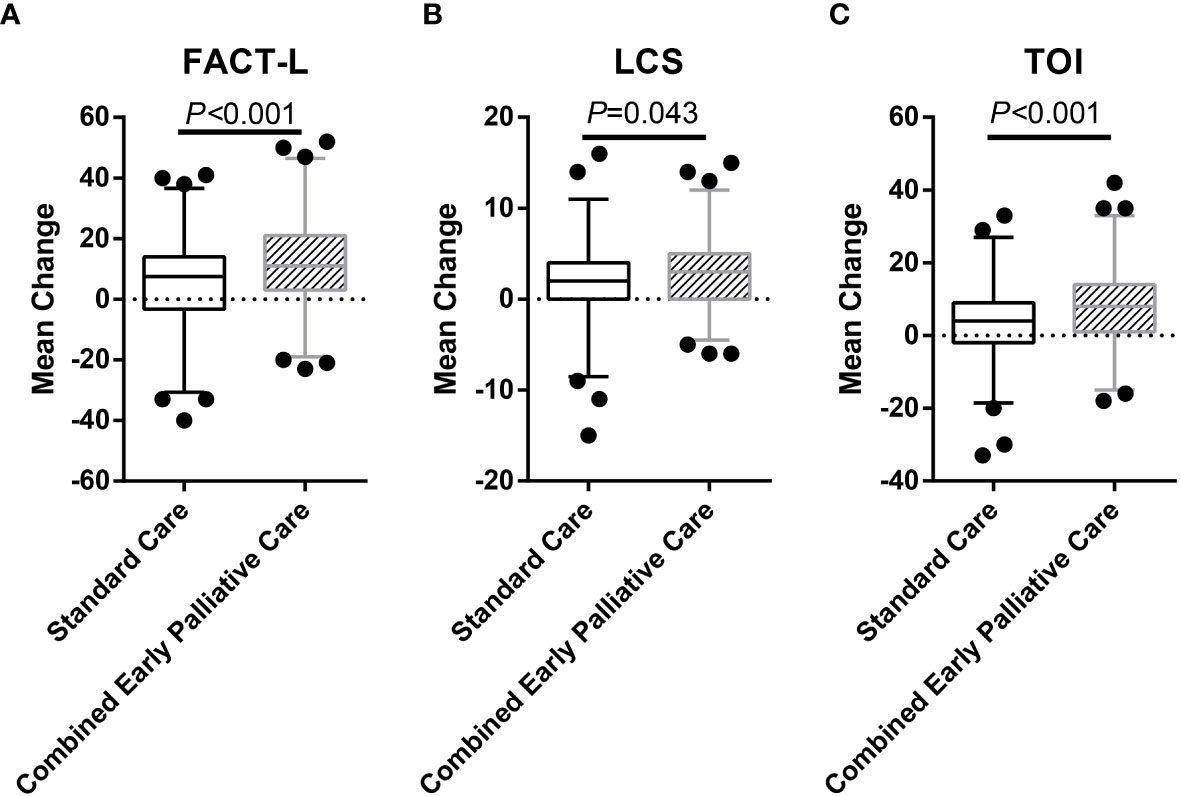
Figure 2 Mean Change in Quality-of-Life Scores from Baseline to 24 Weeks in the Two Study Groups. The study group was the independent variable, and the two-sided independent-sample Student’s t-tests showed a trend toward a significant between-group difference in the mean ( ± SD) change in scores from baseline to 24 weeks on the FACT-L scale (5.51 ± 14.04 in the SC group vs. 11.77 ± 14.89 in the CEPC group; differences between groups, 6.26; 95% confidence interval (CI), 2.83 to 9.68; p < 0.001) (A). A significant between-group difference was detected in the mean change in scores on the LCS (1.80 ± 4.33 and 2.80 ± 3.81 in the two groups, respectively; the difference between groups, 0.99; 95% CI, 0.03 to 1.96; p = 0.043) (B), as well as a significant between-group difference in the mean change in TOI scores(3.45 ± 10.41 vs. 8.03 ± 10.83; the difference between groups, 4.58; 95% CI, 2.07 to 7.09; p < 0.001) (C). Data from 140 patients in the SC group and 140 patients in the CEPC group by intention-to-treat analysis. I bars indicate 95% confidence intervals.
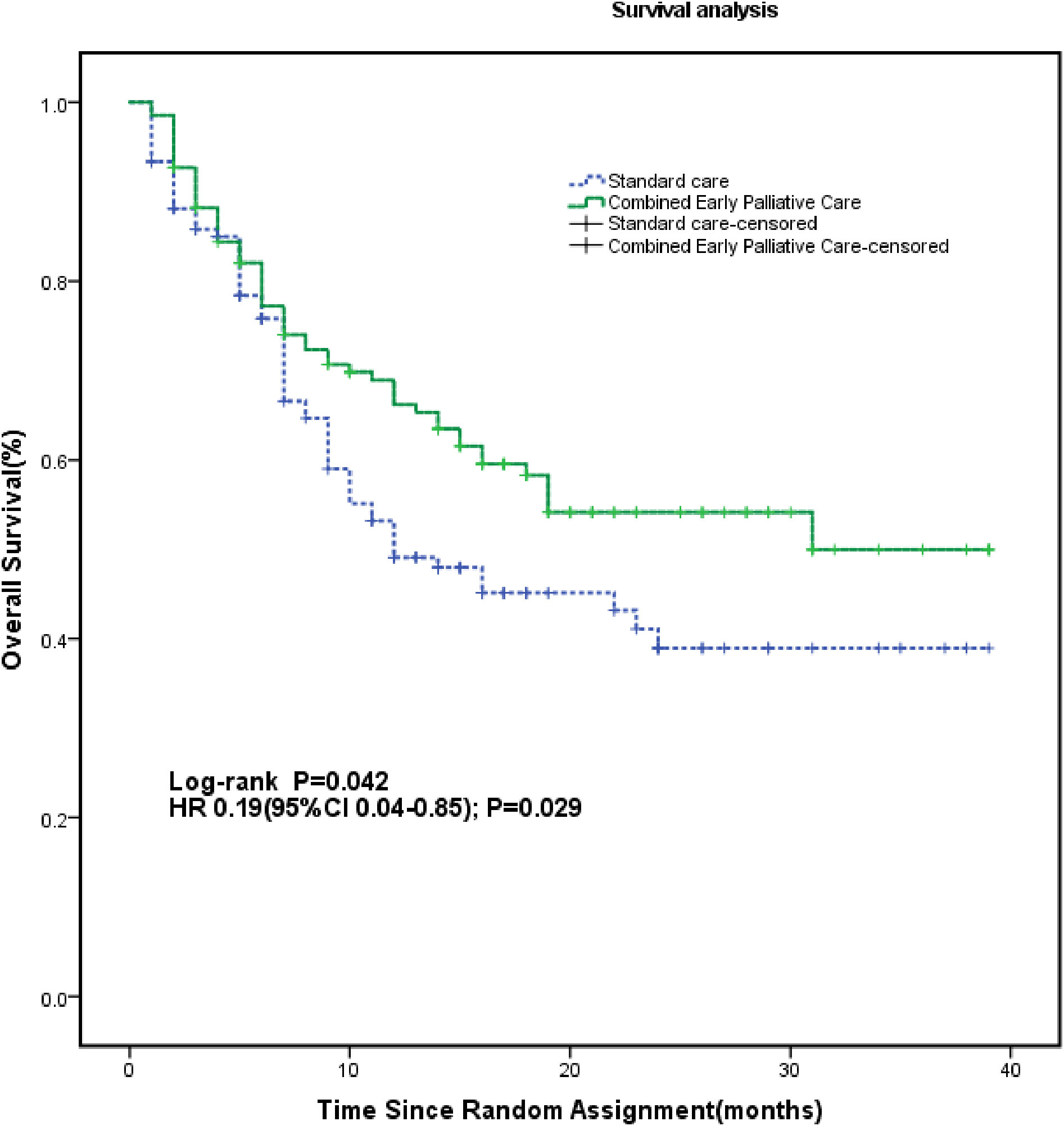
Figure 3 Kaplan-Meier Survival Estimates According to Study Group. The survival rate was calculated from enrollment through the time of death if it occurred during the study period or until January 1, 2023, when the data were censored. The median OS was 24.6 months (95% CI, 21.8 to 27.5) for patients assigned to the CEPC group (n = 140 patients) compared to 20.4 months (95% CI, 17.4 to 23.4) for patients in the SC group (n = 140 patients) (HR, 0.19; 95% CI, 0.04 to 0.85; p = 0.029). HR, hazard ratio.
Discussion
This study examined the effects of combined early palliative care (according to the E-warm concept) for NSCLC patients. When palliative care was integrated early into standard oncology care, NSCLC patients presented a clinically meaningful improvement in QoL, nutritional state, pain management, psychological level, and survival benefit. NSCLC patients have shorter survival when depressed, a poor nutritional level, and lower QoL (31). Further, when Early Palliative Care is integrated with Standard Oncologic Care, anticancer therapy can be optimally and appropriately administered, especially in the final stages of the illness (8, 32, 33). By receiving early referrals to palliative care, patients might manage their symptoms better, improving their condition and having a longer life expectancy (9, 34). Nevertheless, future studies are required to confirm these hypotheses.
Considering the progressive nature of NSCLC, improving patients’ quality of life, nutrition level, pain management, and psychological status is a major challenge (7). Our previous study has shown that early palliative care improved patients’ QoL in the FACT-L (30), consistent with this study and previous reports on metastatic NSCL patients in the New England Journal of Medicine (10). Palliative care integration in oncology care has been shown to improve quality of life in three previous trials at 12 weeks (8, 35, 36), and in three other trials at later time points (37–39). At 24 weeks, the intervention proposed in our trial significantly improved quality of life.
As a result of our findings, early and planned palliative care consultations are critical for patients to discuss all aspects of palliative care at their own pace. These approach contrasts with the usual care group, in which palliative care consultations were only arranged on demand and often. In the era of rapid development of targeted therapy and immunotherapy, comparing patients assigned to CEPC and those assigned to SC is of great interest. The CEPC group had better survival benefits and QoL. Besides, the depression scores significantly differed between the two groups. Thus, this did not result from a difference in antidepressant use between the groups.
Previous studies have demonstrated the benefits of supportive care in terms of QoL, symptom control, and mood management (30, 40, 41). Similar to previous studies (8, 38), we observed an improvement in overall survival. Despite the lack of a clear mechanism behind a better overall survival in this setting, more aggressive early palliative care treatment regimens have been suggested as an explanation (8, 38). There is evidence that the improved nutritional and psychological status of the CEPC group may contribute to the prolonged OS. Anxiety and depression have been linked to a significant increase in cancer-specific mortality (42). Furthermore, individualized nutritional interventions have been shown to reduce 30-day mortality (43). Impacts of nutrition and psychological status may play a significant role in immune response (41, 44–46), which improves long-term prognosis. There have, however, been few studies specifically investigating the effectiveness of multiple support systems in cancer patients.
In a recent study, nutrition and psychology interdisciplinary palliative care enhanced the OS in advanced esophagogastric cancer patients by alleviating symptoms (32). Our findings are similar to those from other researchers in which CEPC improved the QoL of advanced cancer patients (35, 47, 48). Our intervention might have had an effect on aggressive treatment choices of patients because the role of the effect of combined early palliative care group in our trial was large.
This randomized controlled trial has several advantages. First, palliative care interventions were provided for 24 weeks, and many studies have shorter intervention times (8, 35, 47, 49). Furthermore, no model of palliative care is suitable for Chinese conditions. Moreover, our study provided a Chinese-oriented model for palliative care.
However, our current study also has some limitations. First, it was conducted at a single institution, with only Chinese patients. Thus, its generalizability to people from different races and settings might be limited. An additional optimization is needed to customize this palliative care model to meet the needs of different cultures and resources. Second, a potential bias was introduced because participants and investigators were not masked in the group assignment. Finally, the intention-to-treat analysis is conservative if all missing data are carried forward from the last observation. This would suggest that the treatment effect of combined early palliative care might be greater than what we reported here.
In summary, we examined combined early palliative care (based on the E-warm concept) among NSCLC patients. Early palliative care may benefit survival rates, quality of life, psychological well-being, pain management, and nutrition. It would be beneficial to optimize and standardize further.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The Ethics Committee of the Chongqing University Cancer Hospital approved this study (CZLS201917). Informed consent was obtained from all patients before they participated in the study.
Author contributions
MC and HuY initiated the project, designed and performed experiments, analysed the data and drafted the manuscript. LY, HoY, HC, LL, LM, SL, LT, SW enrolled and followed up the patients. HuY and MC designed the project, obtained funding, helped with the writing of the paper, and finalized the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by Chongqing Talents Innovation Leading Talents Program (cstc2021ycjh-bgzxm0256), Natural Science Foundation of Chongqing of China (cstc2021jcyj-msxmX0400), Chongqing medicinal biotech association of scientific research projects(cmba2022kyym-zkxmQ0011), Chongqing Scientific Research Institutions Performance Incentive and guidance Project (cstc2022jxjl0221), Chongqing Municipal Education Commission of Science and Technology Research Project (KJQN202300120), and Technology innovation and application development projects of Shapingba district, Chongqing, China (202394).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2023.1184961/full#supplementary-material
Abbreviations
CEPC, combined early palliative care; ECOG, Eastern Cooperative Oncology Group; FACT-L, Functional Assessment of Cancer Therapy-Lung; HADS, Hospital Anxiety and Depression Scale; LCS, lung-cancer subscale; MDT, Multi disciplinary team; NRS, Numerical Rating Scale; NSCLC, non-small-cell lung cancer; PG-SGA, Patient-Generated Subjective Global Assessment; PHQ-9, Patient Health Questionnaire-9; QoL, quality of life; OS, overall survival; SC, standard oncological care; TOI, Trial Outcome Index.
References
1. Xia C, Dong X, Li H, Cao M, Sun D, He S, et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J (2022) 135(5):584–90. doi: 10.1097/CM9.0000000000002108
2. Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. Ca-Cancer J Clin (2023) 73(1):17–48. doi: 10.3322/caac.21763
3. Chen S, Cao Z, Prettner K, Kuhn M, Yang J, Jiao L, et al. Estimates and projections of the global economic cost of 29 cancers in 204 countries and territories from 2020 to 2050. JAMA Oncol (2023) 9(4):465–72. doi: 10.1001/jamaoncol.2022.7826
4. Luo G, Zhang Y, Etxeberria J, Arnold M, Cai X, Hao Y, et al. Projections of lung cancer incidence by 2035 in 40 countries worldwide: population-based study. JMIR Public Health Surveillance (2023) 9:e43651. doi: 10.2196/43651
5. Daly ME, Singh N, Ismaila N, Antonoff MB, Arenberg DA, Bradley J, et al. Management of stage III non-small-cell lung cancer: ASCO guideline. J Clin Oncol (2022) 40(12):1356–84. doi: 10.1200/JCO.21.02528
6. Donington J, Schumacher L, Yanagawa J. Surgical issues for operable early-stage non-small-cell lung cancer. J Clin Oncol (2022) 40(6):530–8. doi: 10.1200/JCO.21.01592
7. Chaft JE, Rimner A, Weder W, Azzoli CG, Kris MG, Cascone T. Evolution of systemic therapy for stages I-III non-metastatic non-small-cell lung cancer. Nat Rev Clin Oncol (2021) 18(9):547–57. doi: 10.1038/s41571-021-00501-4
8. Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. New Engl J Med (2010) 363(8):733–42. doi: 10.1056/NEJMoa1000678
9. Sullivan DR, Chan B, Lapidus JA, Ganzini L, Hansen L, Carney PA, et al. Association of early palliative care use with survival and place of death among patients with advanced lung cancer receiving care in the veterans health administration. JAMA Oncol (2019) 5(12):1702–9. doi: 10.1001/jamaoncol.2019.3105
10. Strang P. Palliative oncology and palliative care. Mol Oncol (2022) 16(19):3399–409. doi: 10.1002/1878-0261.13278
11. Schenker Y, Althouse AD, Rosenzweig M, White DB, Chu E, Smith KJ, et al. Effect of an oncology nurse-led primary palliative care intervention on patients with advanced cancer: the CONNECT cluster randomized clinical trial. JAMA Internal Med (2021) 181(11):1451–60. doi: 10.1001/jamainternmed.2021.5185
12. Barnato AE, Khayal IS. The power of specialty palliative care: moving towards a systems perspective. Lancet Haematol (2021) 8(5):e376–e81. doi: 10.1016/S2352-3026(21)00099-5
13. Kamal AH, Bausewein C, Casarett DJ, Currow DC, Dudgeon DJ, Higginson IJ. Standards, guidelines, and quality measures for successful specialty palliative care integration into oncology: current approaches and future directions. J Clin Oncol (2020) 38(9):987–94. doi: 10.1200/JCO.18.02440
14. Kaasa S, Loge JH, Aapro M, Albreht T, Anderson R, Bruera E, et al. Integration of oncology and palliative care: a Lancet Oncology Commission. Lancet Oncol (2018) 19(11):e588–653. doi: 10.1016/S1470-2045(18)30415-7
15. Fahy BN. Current guidelines for integration of palliative care in oncology. Surg Oncol Clinics North America (2021) 30(3):431–47. doi: 10.1016/j.soc.2021.02.002
16. Yan Y, Zhang H, Gao W, Liu D, Endo M, Deshpande GA, et al. Current awareness of palliative care in China. Lancet Global Health (2020) 8(3):e333–e5. doi: 10.1016/S2214-109X(20)30006-1
17. Willemsen AM, Mason S, Zhang S, Elsner F. Status of palliative care education in Mainland China: A systematic review. Palliative Supportive Care (2021) 19(2):235–45. doi: 10.1017/S1478951520000814
18. Ye G, Mao J, Hu J, Chen J, Hesketh T. Palliative care medical student education: a cross-sectional medical school survey in mainland China. BMJ Supportive Palliative Care (2022) 12(e4):e493–e6. doi: 10.1136/bmjspcare-2019-002044
19. Hu K, Feng D. Barriers in palliative care in China. Lancet (2016) 387(10025):1272. doi: 10.1016/S0140-6736(16)30017-4
20. Clark D, Baur N, Clelland D, Garralda E, Lopez-Fidalgo J, Connor S, et al. Mapping levels of palliative care development in 198 countries: the situation in 2017. J Pain Symptom Management (2020) 59(4):794–807 e4. doi: 10.1016/j.jpainsymman.2019.11.009
21. Chung H, Harding R, Guo P. Palliative care in the greater China region: A systematic review of needs, models, and outcomes. J Pain Symptom Management (2021) 61(3):585–612. doi: 10.1016/j.jpainsymman.2020.08.040
22. Yang KP, Yin TJ, Lee LC, Hsu N, Huang JM. Holistic outcome measurement for terminally ill cancer patients in medical centers in Taiwan. J Nurs Res JNR (2001) 9(3):43–56. doi: 10.1097/01.jnr.0000347562.92187.17
23. Hwang SJ, Chang HT, Hwang IH, Wu CY, Yang WH, Li CP. Hospice offers more palliative care but costs less than usual care for terminal geriatric hepatocellular carcinoma patients: A nationwide study. J Palliat Med (2013) 16(7):780–5. doi: 10.1089/jpm.2012.0482
24. Tai SY, Lee CY, Wu CY, Hsieh HY, Huang JJ, Huang CT, et al. Symptom severity of patients with advanced cancer in palliative care unit: longitudinal assessments of symptoms improvement. BMC Palliat Care (2016) 15:32. doi: 10.1186/s12904-016-0105-8
25. Ho AH, Dai AA, Lam SH, Wong SW, Tsui AL, Tang JC, et al. Development and pilot evaluation of a novel dignity-conserving end-of-life (EoL) care model for nursing homes in chinese societies. Gerontol (2016) 56(3):578–89. doi: 10.1093/geront/gnv037
26. Fan X, Huang H, Luo Q, Zhou J, Tan G, Yong N. Quality of life in Chinese home-based advanced cancer patients: does awareness of cancer diagnosis matter? J Palliat Med (2011) 14(10):1104–8. doi: 10.1089/jpm.2011.0111
27. Chan CW, Chui YY, Chair SY, Sham MM, Lo RS, Ng CS, et al. The evaluation of a palliative care programme for people suffering from life-limiting diseases. J Clin Nurs (2014) 23(1-2):113–23. doi: 10.1111/jocn.12094
28. Chiang JK, Kao YH. Impact of home hospice care on patients with advanced lung cancer: A longitudinal population-based study in Taiwan. J Palliat Med (2016) 19(4):380–6. doi: 10.1089/jpm.2015.0278
29. Wei L, Ping G. Exploring the challenges of implementing palliative care in China. Eur J Palliative Care (2017) 24(1):12–7.
30. Chen M, Yang L, Yu H, Yu H, Wang S, Tian L, et al. Early palliative care in patients with non-small-cell lung cancer: A randomized controlled trial in southwest China. Am J Hospice Palliative Care (2022) 39(11):1304–11. doi: 10.1177/10499091211072502
31. Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman JR, Bharat A, et al. NCCN guidelines insights: non-small cell lung cancer, version 2.2021. J Natl Compr Cancer Network JNCCN (2021) 19(3):254–66. doi: 10.6004/jnccn.2021.0013
32. Lu Z, Fang Y, Liu C, Zhang X, Xin X, He Y, et al. Early interdisciplinary supportive care in patients with previously untreated metastatic esophagogastric cancer: A phase III randomized controlled trial. J Clin Oncol (2021) 39(7):748–56. doi: 10.1200/JCO.20.01254
33. Temel JS, Petrillo LA, Greer JA. Patient-centered palliative care for patients with advanced lung cancer. J Clin Oncol (2022) 40(6):626–34. doi: 10.1200/JCO.21.01710
34. Yoong J, Park ER, Greer JA, Jackson VA, Gallagher ER, Pirl WF, et al. Early palliative care in advanced lung cancer: a qualitative study. JAMA Internal Med (2013) 173(4):283–90. doi: 10.1001/jamainternmed.2013.1874
35. Vanbutsele G, Pardon K, Van Belle S, Surmont V, De Laat M, Colman R, et al. Effect of early and systematic integration of palliative care in patients with advanced cancer: a randomised controlled trial. Lancet Oncol (2018) 19(3):394–404. doi: 10.1016/S1470-2045(18)30060-3
36. Maltoni M, Scarpi E, Dall'Agata M, Zagonel V, Berte R, Ferrari D, et al. Systematic versus on-demand early palliative care: results from a multicentre, randomised clinical trial. Eur J Cancer (2016) 65:61–8. doi: 10.1016/j.ejca.2016.06.007
37. Temel JS, Greer JA, El-Jawahri A, Pirl WF, Park ER, Jackson VA, et al. Effects of early integrated palliative care in patients with lung and GI cancer: A randomized clinical trial. J Clin Oncol (2017) 35(8):834–41. doi: 10.1200/JCO.2016.70.5046
38. Bakitas MA, Tosteson TD, Li Z, Lyons KD, Hull JG, Li Z, et al. Early versus delayed initiation of concurrent palliative oncology care: patient outcomes in the ENABLE III randomized controlled trial. J Clin Oncol (2015) 33(13):1438–45. doi: 10.1200/JCO.2014.58.6362
39. Zimmermann C, Swami N, Krzyzanowska M, Hannon B, Leighl N, Oza A, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet (9930) 2014:383. doi: 10.1016/S0140-6736(13)62416-2
40. Basch E, Deal AM, Kris MG, Scher HI, Hudis CA, Sabbatini P, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. J Clin Oncol (2016) 34(6):557–65. doi: 10.1200/JCO.2015.63.0830
41. Chen M, Ma L, Yu H, Huang S, Zhang J, Gong J, et al. JK5G postbiotics attenuate immune-related adverse events in NSCLC patients by regulating gut microbiota: a randomized controlled trial in China. Front Oncol (2023) 13:1155592. doi: 10.3389/fonc.2023.1155592
42. Wang YH, Li JQ, Shi JF, Que JY, Liu JJ, Lappin JM, et al. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry (2020) 25(7):1487–99. doi: 10.1038/s41380-019-0595-x
43. Schuetz P, Fehr R, Baechli V, Geiser M, Deiss M, Gomes F, et al. Individualised nutritional support in medical inpatients at nutritional risk: a randomised clinical trial. Lancet (2019) 393(10188):2312–21. doi: 10.1016/S0140-6736(18)32776-4
44. Chen MT, Hou PF, Zhou M, Ren QB, Wang XL, Huang L, et al. Resveratrol attenuates high-fat diet-induced non-alcoholic steatohepatitis by maintaining gut barrier integrity and inhibiting gut inflammation through regulation of the endocannabinoid system. Clin Nutr (2020) 39(4):1264–75. doi: 10.1016/j.clnu.2019.05.020
45. Yang H, Xia L, Chen J, Zhang S, Martin V, Li Q, et al. Stress-glucocorticoid-TSC22D3 axis compromises therapy-induced antitumor immunity. Nat Med (2019) 25(9):1428–41. doi: 10.1038/s41591-019-0566-4
46. Zitvogel L, Pietrocola F, Kroemer G. Nutrition, inflammation and cancer. Nat Immunol (2017) 18(8):843–50. doi: 10.1038/ni.3754
47. Ferrell B, Sun V, Hurria A, Cristea M, Raz DJ, Kim JY, et al. Interdisciplinary palliative care for patients with lung cancer. J Pain Symptom Management (2015) 50(6):758–67. doi: 10.1016/j.jpainsymman.2015.07.005
48. Vanbutsele G, Van Belle S, Surmont V, De Laat M, Colman R, Eecloo K, et al. The effect of early and systematic integration of palliative care in oncology on quality of life and health care use near the end of life: A randomised controlled trial. Eur J Cancer (2020) 124:186–93. doi: 10.1016/j.ejca.2019.11.009
Keywords: combined early palliative care, non-small-cell lung cancer (NLSCLC), overall survival (OS), pain management (MeSH), psychological status, nutritional level
Citation: Chen M, Yu H, Yang L, Yang H, Cao H, Lei L, Ma L, Liu S, Tian L and Wang S (2023) Combined early palliative care for non-small-cell lung cancer patients: a randomized controlled trial in Chongqing, China. Front. Oncol. 13:1184961. doi: 10.3389/fonc.2023.1184961
Received: 13 March 2023; Accepted: 23 August 2023;
Published: 14 September 2023.
Edited by:
Gabriela Salim de Castro, University of São Paulo, BrazilReviewed by:
Prashant Kaushik, Yokohama Ueki, JapanAynur Aktas, Levine Cancer Institute, United States
Copyright © 2023 Chen, Yu, Yang, Yang, Cao, Lei, Ma, Liu, Tian and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huiqing Yu, eWhxZHl4QGNxdS5lZHUuY24=
 Mengting Chen
Mengting Chen Huiqing Yu
Huiqing Yu Liejun Yang2
Liejun Yang2 Liling Ma
Liling Ma Ling Tian
Ling Tian