- 1Department of Geriatric Oncology, The Third Affiliated Hospital of Kunming Medical University - Yunnan Cancer Hospital, Kunming, China
- 2Department of Hematology, The Sixth Affiliated Hospital of Kunming Medical University-Yuxi People’s Hospital, Yuxi, China
- 3Department of Hematology, General Medical College of Kunming Medical University, Kunming, China
Objective: To develop a Thyroid Cancer Self-Perceived Discrimination Scale (TCSPDS) to identify patients at high risk for psychological problems and to test its reliability, validity and acceptability.
Methods: Using classical test theory, a total of 176 thyroid cancer patients from November 2021 to October 2022 were recruited to develop the TCSPDS. Item analysis was used to improve the preliminary TCSPDS. Exploratory factor analysis (EFA), confirmatory factor analysis (CFA) and structural equation model (SEM) were used to test the construct validity of the final TCSPDS. Pearson correlation coefficient was used to analyze the validity coefficient between TCSPDS and EORTC QLQ-C30 to test the criterion-related validity (CRV) of the final TCSPDS. The internal consistency coefficient (Cronbach’s alpha coefficient), split half reliability (Spearman-Brown coefficient) and test-retest reliability were used to verify the reliability of the final TCSPDS. The questionnaire completion time and effective response rate were used to validate the acceptability of the final TCSPDS.
Results: The TCSPDS consisted of 20 items and was divided into 3 subscales: 8 items for stigma, 6 items for self-deprecation, and 6 items for social avoidance. The TCSPDS had good validity (χ2/df=1.971, RMSEA=0.074, GFI=0.921, CFI= 0.930, IFI=0.932, TLI=0.901, Validity coefficient=0.767), reliability (Cronbach’s alpha=0.867, Spearman-Brown coefficient=0.828, test-retest reliability coefficient=0.981) and acceptability [average completion time (15.01 ± 1.348 minutes) and an effective response rate of 95.14%]. Patients with higher TCSPDS scores reported a lower quality of life (P<0.05).
Conclusion: The TCSPDS could be used for early identification and assessment of the level of self-perceived discrimination in patients with thyroid cancer, which may provide a scientific basis for health education, social support and psychosocial oncology services in the future, especially in Southwest China.
Introduction
Over the past 30 years, the incidence of thyroid cancer has continued to rise globally (1). Data from the National Cancer Center of China in 2022 showed that the incidence of thyroid cancer in China was the second most common cancer among people aged 15 to 44 years (2). Among malignant tumors in women, thyroid cancer is the third most common cancer after breast cancer and lung cancer, and it seriously threatens the physical and mental health and socio-economic development of the nation (2).
“Discrimination” is a kind of psychological reaction and behavior among different social groups, including stigmatization, negation, exclusion and other unequal treatment in speech and behavior (3). “Self-perceived discrimination” refers to the intermittent or persistent negative psychological state of a member of a special population after subjectively predicting or objectively experiencing negative, exclusionist and other unfair social behaviors of other social groups, which includes shame, stigma, fear, anxiety and depression (4, 5). However, most studies on disease-related self-perceived discrimination mainly focus on patients with infectious diseases, mental disorders and disabilities (6–8). There are few studies on cancer-related self-perceived discrimination, especially thyroid cancer (9, 10).
With improvements in the treatment effect and life expectancy of thyroid cancer patients, cancer-related psychological problems have gradually become the new focus and have received global attention. Although thyroid cancer, which is mainly treated with surgery, is regarded as a “good cancer”, the risk of treatment toxicity (include neck wounds, thyroid dysfunction, paresthesia, pain, etc.) and long-term recurrence, as well as the continuous negative effects on social and family relationships, result in widespread and nonnegligible self-perceived discrimination among patients and significantly affect their quality of life (QOL) (11–13).
Previous studies have shown that self-perceived discrimination of thyroid cancer patients may come from cancer phobia, treatment methods and economic burden. The public’s fear of cancer stems from the fact that cancer is a malignant disease that is difficult to cure and eventually leads to the patient’s death (14). Patients newly diagnosed with thyroid cancer still show obvious fear and anxiety about disease recurrence and death even after receiving health education with good prognosis (15). Second, patients often felt pain and helplessness related to the change in appearance after surgery, which was more obvious within 6 months; the appearance of injury in female patients may be particularly serious (16, 17). Furthermore, the continuous increase in treatment costs and the decline in work ability undoubtedly caused a heavy economic burden for patients. The objective economic burden usually developed into the self-perceived burden of patients, which may be more prominent in low-income patients (18, 19).
At present, there is no suitable tool specifically designed to assess self-perceived discrimination in thyroid cancer patients. Only the Shame and Stigma Scale (SSS), developed by DW Kissane et al. for patients with head and neck cancer, is currently available (20). The SSS contains four subscales: shame with appearance, regret, sense of stigma and speech/social concerns. Although the SSS had good validity and reliability, it focused on oral cancer and could only evaluate the patient’s perceived stigma, which is only one component of self-perceived discrimination. Moreover, although our previously developed Cancer Self-Perceived Discrimination Scale (CSPDS) could be used to preliminarily estimate the self-perceived discrimination of all cancer patients, it still lacks specificity for thyroid cancer (21).
Therefore, the purpose of our study was to develop and validate a specific Thyroid Cancer Self-Perceived Discrimination Scale (TCSPDS) to identify patients at high risk for psychological problems, and analyze the correlation between TCSPDS and QOL.
Methods
Study design and participants
Based on classical test theory, the steps were as follows:
(1) A preliminary TCSPDS was developed through a literature review, semi-structured interviews, expert consultations and cognitive interviews.
(2) A questionnaire was formed to investigate patients with thyroid cancer.
(3) The final TCSPDS was formed by the item analysis method.
(4) The final TCSPDS was validated.
(5) The independent influencing factor of TCSPDS was analyzed.
(6) The correlation between TCSPDS and QOL was analyzed.
Patients with thyroid cancer treated at Yunnan Cancer Hospital were selected as the research objects. Individuals who were patients from November to December 2021 were selected as the semi-structured interview objects, and those from March to October 2022 were selected as the questionnaire objects.
The inclusion criteria for patients included the following:
(1) had a diagnosis of thyroid cancer by histopathology and thyroidectomy was performed (tumor staging followed AJCC Version 8 criteria) (22),
(2) had good language expression capability and understanding ability,
(3) were aware of their diagnosis and volunteered to participate in the study, and
(4) were ≥18 years old.
The exclusion criteria for patients were as follows:
(1) had other primary cancers, or
(2) had infectious diseases, mental disorder, brain trauma history, physical disability or underwent emergency medical treatment.
This was a single-center study with all participants from the Yunnan Cancer Hospital, Yunnan Province, China. Ethical approval for this study was granted by the Ethics Committee of Yunnan Cancer Hospital (NO. KYLX2022063). All participants signed an informed consent form. We promised the participants that the data would only be used for this study, and that the participants may withdraw from the study at any time.
Development of the preliminary TCSPDS
Step 1
The random sampling method was used to select thyroid cancer patients who could reflect the target population of the research questions to the greatest extent for semi-structured interviews (from November 1 to December 20, 2021). Before the interview, qualitative research experts were consulted to help understand the necessary precautions for the interview process, and relevant training was conducted for researchers to ensure the reliability of the interview data. An interview outline was established by reviewing a large number of studies: (1)How did you feel psychologically after being diagnosed with thyroid cancer? (2) Did your disease affect your life? Was there any psychological burden? (3)Had you ever been treated unfairly? How was it handled? (4) Were you cared for by others? (5) How have your relationships with your family and friends changed? Were you willing to share your diagnosis with them? When necessary, the researchers asked additional follow-up questions based on the patient’s answers.
With the consent of the participants, the researchers introduced the research purpose, methods and privacy protection measures to them. Individual interviews were conducted in the inpatient talk room, and general information such as age, sex, marital status, education level, treatment methods, and disease duration were collected. Participants were informed that the interview content would be recorded in the form of an audio recording or notetaking during the interview, and they were assured that the interview content would only be used for this research study and would not be released. Each participant was interviewed for approximately 35 to 45 minutes, and their real names were replaced by numbers.
The study followed the principle of the “information saturation method”, so that the sample size of participants depended on whether further information was available in the semi-structured interview (23). The interview data were sorted out within 24 hours after the end of the interview. Based on the construction grounded theory, two researchers applied NVivo 12 PLUS software to conducted independent selective coding on the interview data to extract the theme and subtheme, and a third researcher made decisions when disagreements occurred.
Step 2
The literature related to self-perceived discrimination in cancer patients was reviewed, and an item pool was established through semi-structured interviews and literature reviews (20, 21, 24–28). The language design (grammar and sentence patterns) should refer to the literature review and conform to Chinese grammar (from November 18 to December 25, 2021). Items were expressed on a 5-point Likert scale, and for the forward-scored items, the options were as follows: 1=strongly disagree, 2=somewhat disagree, 3=not sure, 4=somewhat agree, and 5=strongly agree. For the reverse-scored items, the score was reversed. Therefore, a higher score indicated a higher level of self-perceived discrimination.
Step 3
The Delphi expert consultation method was used to invite 4 experts in medical oncology, 2 experts in head and neck surgery and 1 expert in linguistics to evaluate the content and applicability of the items in two rounds (from January 3 to February 8, 2022) (29). In the first round of expert consultation, the inappropriate descriptions were removed, and the expressions of the items were further revised. In the second round of expert consultation, a 4-point rating scale (1=uncorrelation, 2=weak correlation, 3=moderate correlation, 4=strong correlation) was used to independently review and assess each item by experts, and the item-level content validity index (I-CVI) was calculated. If any item had an I-CVI<0.80, we would repeat the above steps until the item had an I-CVI≥0.80, or it would be deleted.
Step 4
Ten patients with thyroid cancer were invited to give cognitive interviews on the content and meaning of each item to ensure that all items could be understood and accepted in the formal investigation (from February 10 to February 28, 2022). For each item, 10 participants answered the question “Can you understand and accept the content and meaning of the item?” Finally, the preliminary TCSPDS was formed.
Questionnaire development and distribution
The questionnaire consisted of three parts: (1) The general information questionnaire included age, sex, marital status, residential area, economic burden, education level, disease duration and operation method. (2) The preliminary TCSPDS was included. (3) The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ⁃C30) was included (30). The EORTC QLQ⁃C30 has been widely used to evaluate the QOL of cancer patients. It covered 15 domains with 30 items, including 5 functional domains, 9 symptom domains and one global health domain. Its Cronbach’s alpha was 0.884, which indicated good reliability and validity. Items 1 to 28 from EORTC QLQ⁃C30 were scored on a 4-point scale, with scores from 1 to 4 indicating no, somewhat, fairly or very much. Items 29 and 30 were rated from 1 to 7 based on patient responses, with higher scores indicating lower QOL.
For factor analysis, the common recommendation for sample size was N≥100, and the ratio between independent and dependent variables was at least 5 (31, 32). Before administration of the survey, the researchers were trained professionally. Questionnaires were distributed to patients with thyroid cancer who came to the hospital for treatment and were collected on site. In principle, the questionnaire should be completed by patients according to their own assumptions. However, it could be completed under the guidance of researchers, if necessary. The formal investigation was conducted from March 1 to October 20, 2022.
Validation of TCSPDS
Step 1: item analysis
The Pearson correlation coefficient was used to analyze the correlation between each item’s score and the total score of the scale. If the Pearson correlation coefficient of any item was less than 0.3 or was not significant (P>0.05), then it was deleted.
Step 2: validity analysis
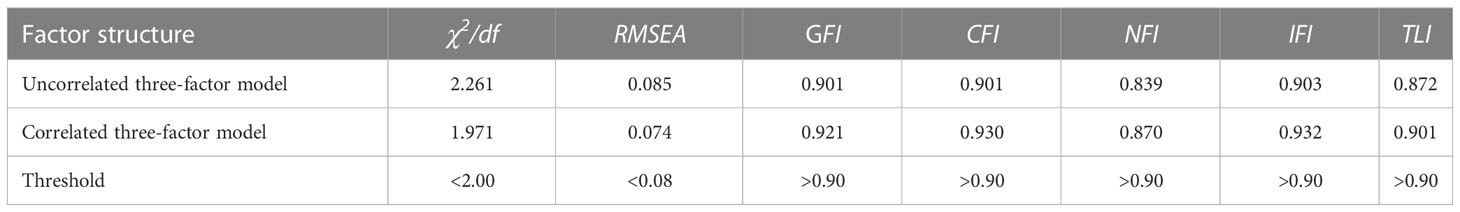
The I-CVI was used to verify the content validity of the TCSPDS. If the I-CVI>0.8, the content validity of the scale was considered to be good. Exploratory factor analysis (EFA), confirmatory factor analysis (CFA) and structural equation modeling (SEM) were used to verify the construct validity of the TCSPDS. First, EFA of SPSS 25.0 software was used to construct the theoretical model. If the Kaiser−Meyer−Olkin (KMO) was greater than 0.7 and the significance of Bartlett’s test was less than 0.001, the common factor was considered suitable to for extraction (33). Then, CFA and SEM of AMOS 24.0 software was applied to verify the theoretical model. If the criteria were met for the chi-square degree of freedom ratio (χ2/df<2), root mean square error of approximation (RMSEA<0.08), goodness-of-fit index (GFI>0.90), comparative fit index (CFI>0.90), normed fit index (NFI>0.90), incremental fit index (IFI>0.90) and Tucker−Lewis index (TLI>0.90), then the scale could be considered to have good construct validity (34). Pearson correlation coefficient was used to analyze the validity coefficient between TCSPDS and EORTC QLQ-C30 to test the criterion-related validity (CRV) of TCSPDS. If the validity coefficient r≥0.50 (P<0.05), the CRV was considered to be good (35).
Step 3: reliability analysis
The Cronbach’s alpha coefficient, Spearman-Brown coefficient and test-retest reliability were used to verify the reliability of the TCSPDS. If the Cronbach’s alpha and Spearman-Brown coefficients were at least 0.7, then it was considered to have good reliability (36). The intraclass correlation coefficient (ICC) was used to verify the test-retest reliability of the TCSPDS. If the ICC was at least 0.8, then it was considered to have good test-retest reliability (37).
Step 4: acceptability analysis
The acceptability of the questionnaire was verified by the effective response rate and average completion time. The questionnaire was considered to have good acceptability if the effective response rate was at least 90% and the average completion time was at most 20 minutes (38).
Application of TCSPDS
Step 1: influencing factors analysis
One-way ANOVA was used to compare the scores of TCSPDS among different participants, and multiple stepwise regression analysis was used to analyze the independent influencing factors of patients’ TCSPDS scores.
Step 2: QOL correlation analysis
The Pearson correlation coefficient was used to analyze the correlation between the scores of TCSPDS and QOL. If the correlation coefficient r<0.4 (P<0.05), it indicated that the correlation was weak; If 0.4≤r<0.7 (P<0.05), it indicated that the correlation was moderate; If r≥0.7 (P<0.05), it indicated that the correlation was strong (39).
SPSS 25.0, AMOS 24.0 and NVivo 12 PLUS were used for statistical analysis. Two-tailed P<0.05 was considered significant.
Results
Participant characteristics
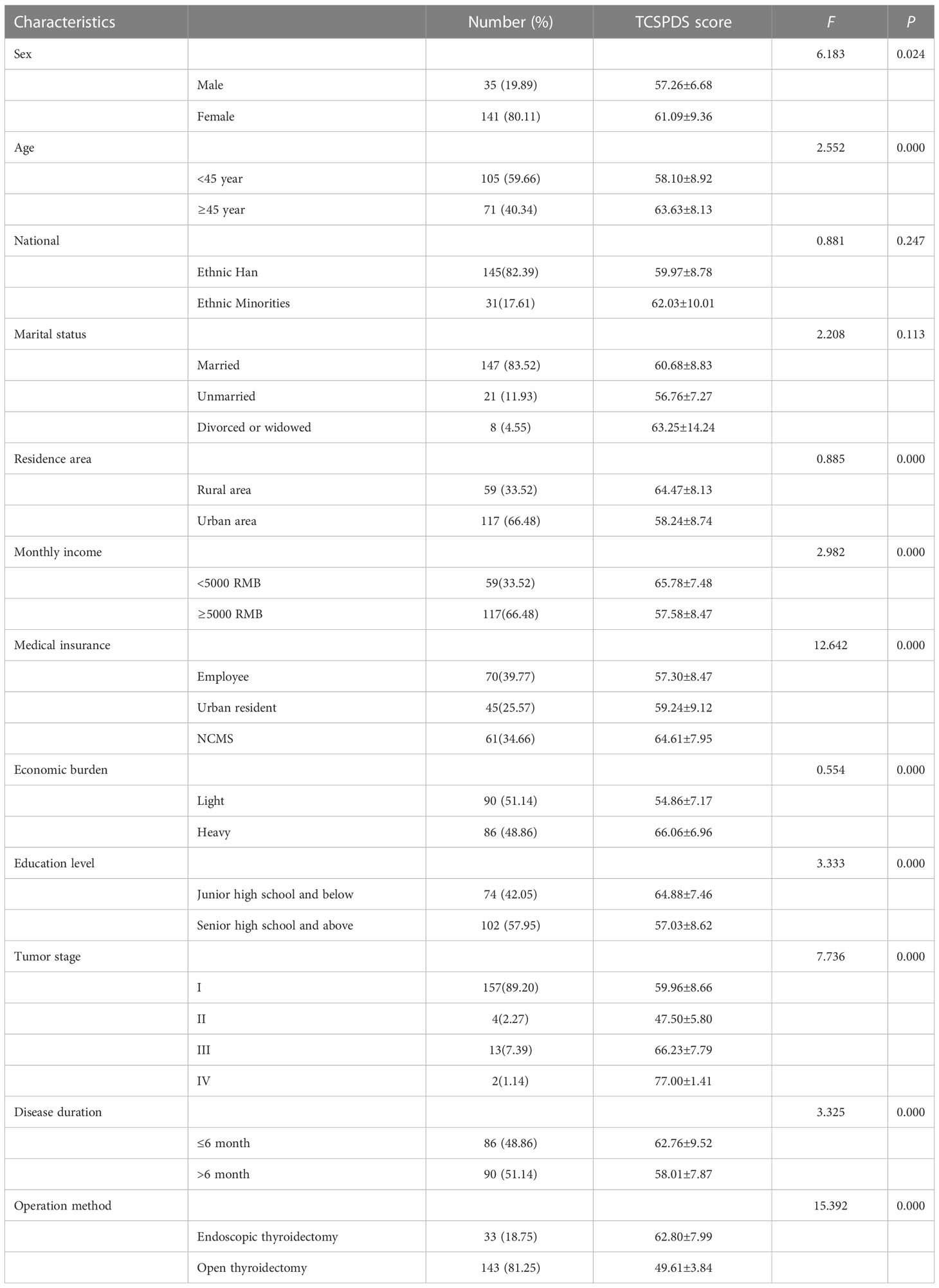
A total of 185 patients with thyroid cancer agreed to participate, and 176 patients completed the survey (effective response rate, 95.14%). Among the 176 participants, 141 were female and 35 were male; 105 were younger than 45 years old and 71 were older than or equal to 45 years old. Their disease duration was as follows: 86 had disease duration less than or equal to 6 months and 90 had disease duration more than 6 months. Detailed information about the participants’ characteristics is shown in Table 1.
Development of the preliminary TCSPDS
According to the in-depth semi-structured interviews, the three themes of stigma, self-deprecation and social avoidance were extracted from the self-perceived discrimination of 35 thyroid cancer patients. The stigma included cancer fear, wound and voice changes, irritable temper and medication labels. Self-deprecation included dysfunction, disfigurement and financial burden. Social avoidance included disease concealment, communication disorder and refusal of care.
Based on the qualitative research and literature review, a preliminary TCSPDS with 12 items was developed. In the first round of expert consultation, we revised three items. We revised item 3 “Some people believe that thyroid cancer is a genetic disease” to “Some people believe that thyroid cancer is inherited”. Item 11, “I hate seeing myself in the mirror”, was revised to “Sometimes I feel distressed about my neck wound”. Item 13, “Sometimes I feel responsible for my thyroid cancer”, was revised to “Sometimes I feel very guilty about my thyroid cancer”. In the second round of expert consultation, the I-CVIs of the 12 items were all greater than 0.80. After cognitive interviews with 10 thyroid cancer patients, no revision of the item content was needed.
Validation of TCSPDS
Item analysis
The Pearson correlation coefficient between the score of each item and the total score of the TCSPDS ranged from 0.343 to 0.722 (P<0.01). Therefore, there was no need to remove any item from the TCSPDS.
Content validity
After two rounds of expert consultation, the I-CVIs of all 12 items in the preliminary TCSPDS were greater than 0.80. Each item was strongly correlated with the total scale, and Pearson correlation coefficients ranged from 0.343 to 0.722 (P<0.01). Each item was strongly correlated with each subscale, and Pearson correlation coefficients ranged from 0.472 to 0.874 (P<0.01). Therefore, it was determined that the TCSPDS had good content validity.
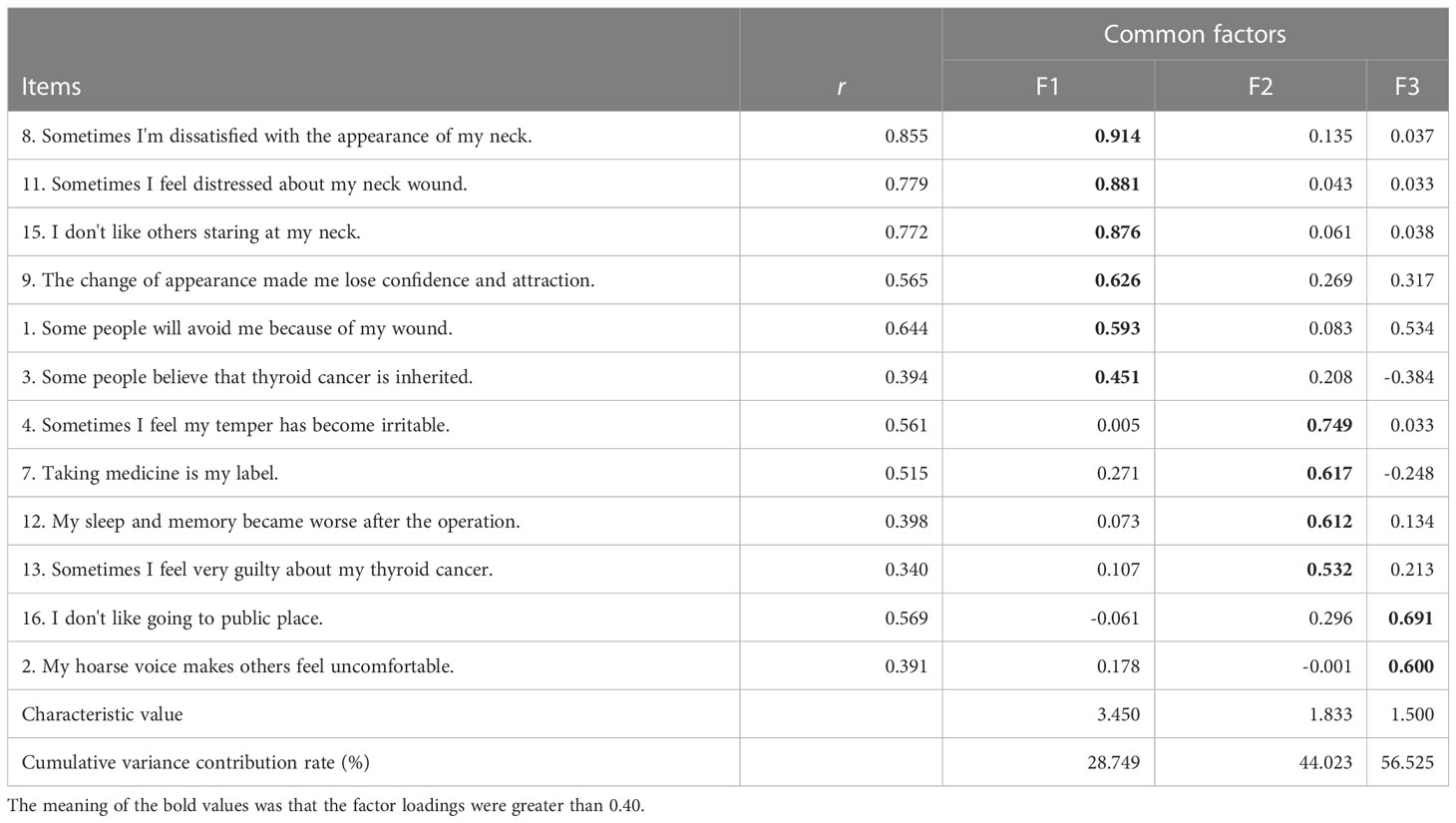
Construct validity
The EFA results showed that the KMO of the preliminary TCSPDS was 0.802, and Bartlett’s test was 695.088 (P<0.001), which indicated that it was suitable for factor analysis. Three common factors with characteristic roots greater than 1 were extracted by principal component analysis (PCA), and the cumulative variance contribution rate was 56.525%. The detailed factor loadings are shown in Table 2.
According to the qualitative research results, Factor 1 was named stigma, which mainly reflects the fact that thyroid cancer patients were treated unfairly because of their disease and disfigurement. Factor 2 was named self-deprecation, which mainly reflected the negative psychology of patients under multiple burdens, such as dysfunction, economic, social and psychological burdens. Factor 3 was named social avoidance, which mainly reflected the actual condition of disease concealment, communication disorder and refusal of care.
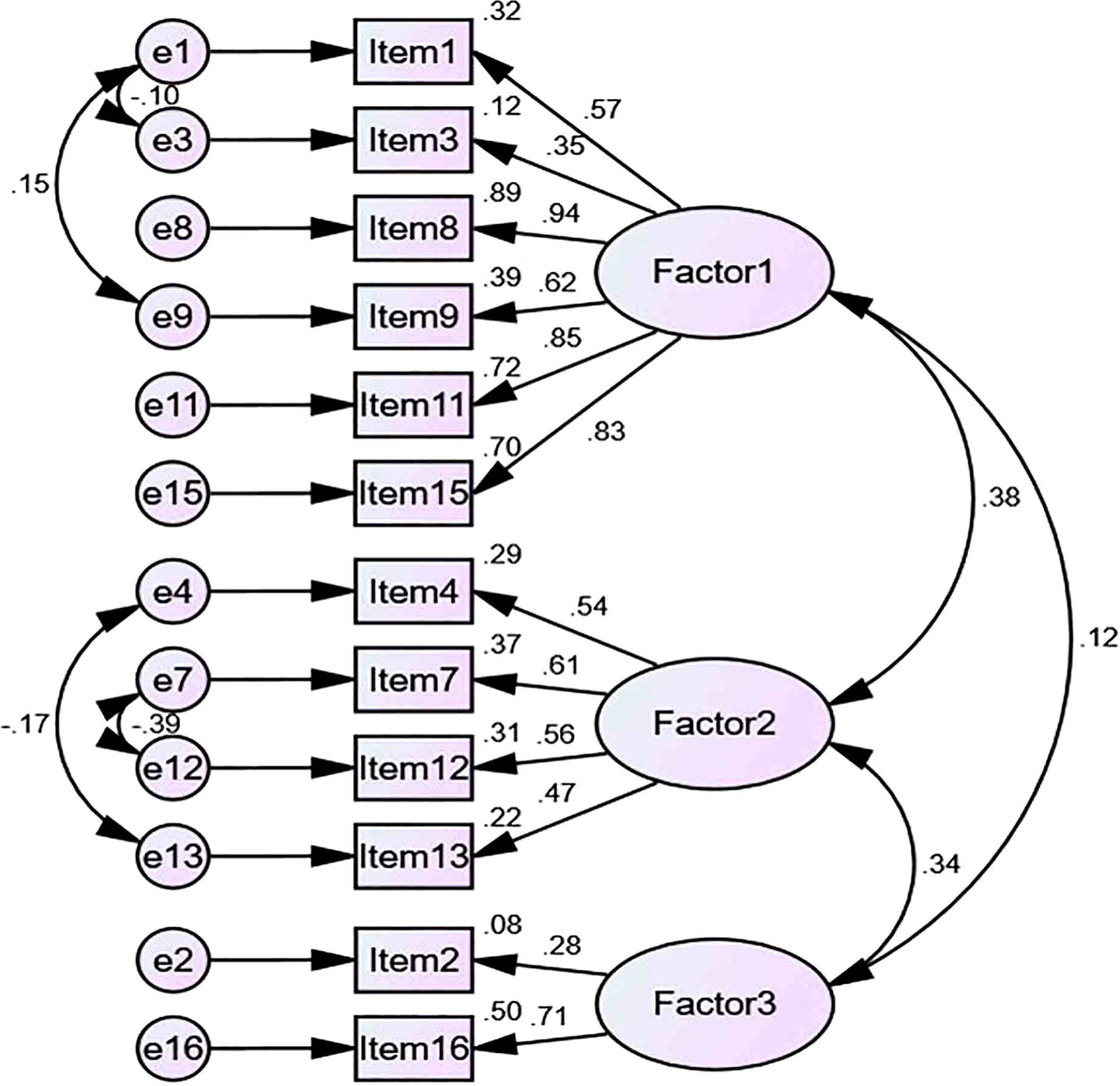
According to the theoretical model constructed by EFA, CFA and SEM were conducted on the distribution of each item of the scale. The results showed that the fitting degree of the correlated three-factor model was better than that of the uncorrelated three-factor model. However, the NFI was slightly lower than the threshold, and the other fitting index performed well, which indicated that the TCSPDS had good construct validity (Figure 1 and Table 3). The 8 items previously verified in the CSPDS were added to the corresponding subscale of the TCSPDS, and these 8 items were universal to all cancer patients (20). Finally, the final TCSPDS with 20 items was formed. Except for item 20, which was a reverse item, all the items were forward items (Table 4).
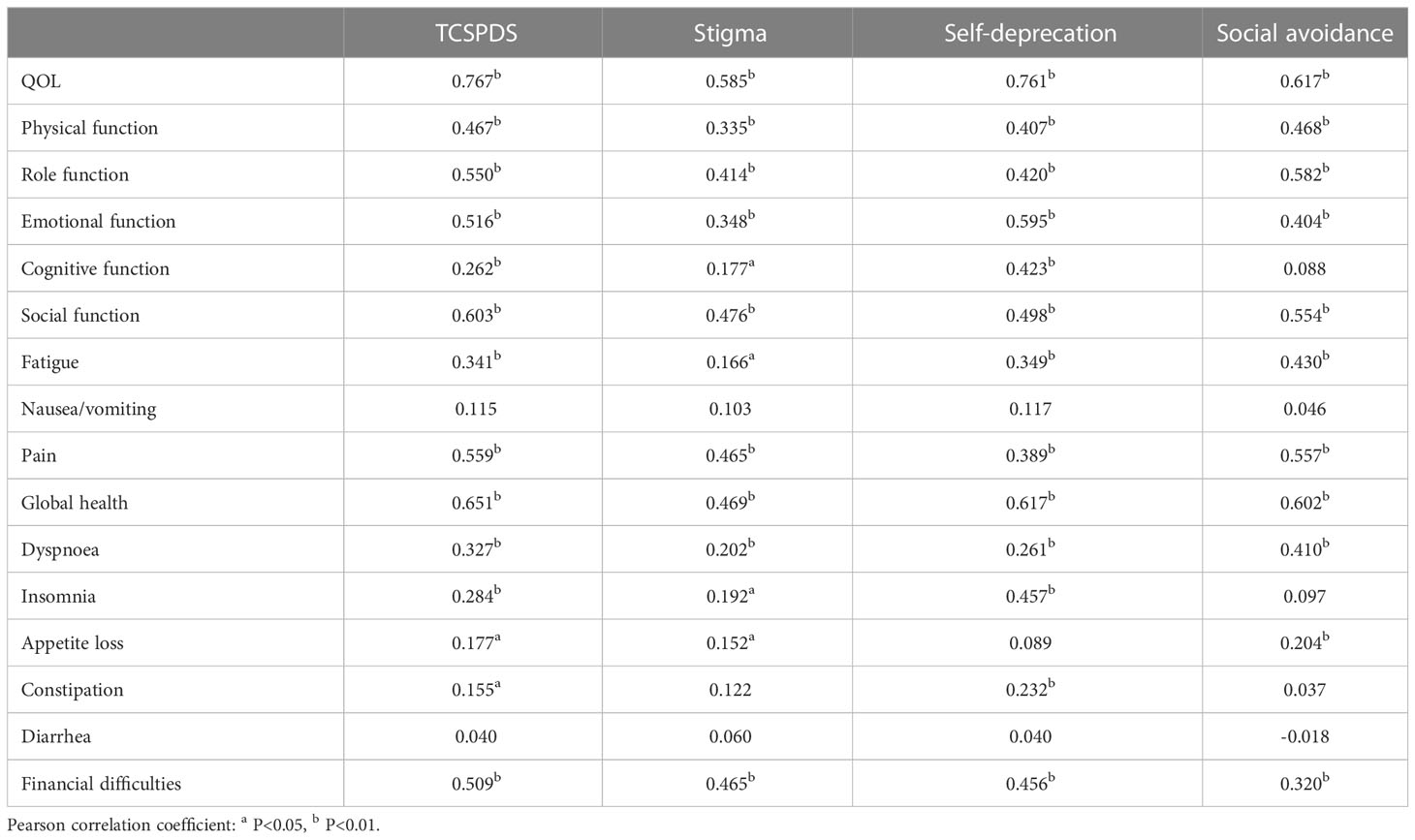
Criterion-related validity
The validity coefficients of TCSPDS, shame subscale, self-deprecation subscale and social avoidance subscale with EORTC QLQ-C30 were 0.767, 0.585, 0.761 and 0.617 respectively (r≥0.50, P<0.01), which indicated that the TCSPDS had good CRV (Table 5).
Reliability
The Cronbach’s alpha of the final TCSPDS was 0.867, and the Spearman-Brown coefficient was 0.828. The Cronbach’s alpha values of the three subscales were 0.850, 0.650 and 0.628, and the Spearman-Brown coefficients were 0.741, 0.671 and 0.641. These results indicated that the final TCSPDS had good internal reliability. Two weeks after the first questionnaire survey, 14 patients with thyroid cancer participated in the second survey. The test-retest results showed that the ICCs of the final TCSPDS and the three subscales were 0.981, 0.976, 0.861 and 0.967, which indicated that the final TCSPDS had good test-retest reliability.
Acceptability
The average completion time of the TCSPDS with 20 items was 15.01 ± 1.348 (range: 13 to 19) minutes. A total of 185 final TCSPDS questionnaires were distributed, and 176 valid questionnaires were recovered (effective response rate was 95.14%), which indicated that the final TCSPDS had good acceptability.
Application of TCSPDS
Influencing factors of TCSPDS
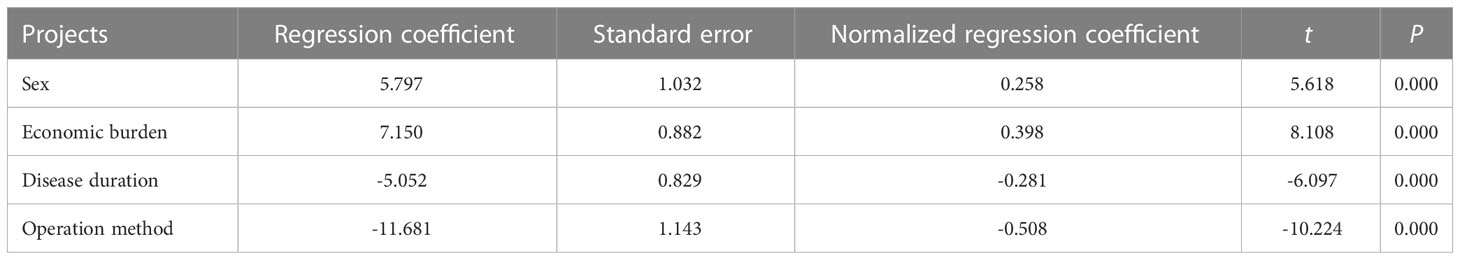
One-way ANOVA indicated, statistically significant differences in scores of sex, age, area of residence, monthly income, type of medical insurance, economic burden, education level, tumor stage, disease duration and operation method (P<0.05), as shown in Table 1. TCSPDS scores were used as dependent variables, and the above 10 statistically significant variables were used as independent variables. Through multiple stepwise regression analysis, the results showed that gender, economic burden, disease duration and operation method were independent influencing factors of patients’ self-perceived discrimination (P<0.05), as shown in Table 6.
QOL correlation analysis
The scores of TCSPDS were positively correlated with the scores of QOL, global health, 5 functional domains and 7 symptom domains (fatigue, pain, dyspnea, insomnia, appetite loss, constipation and financial difficulties) (P<0.05), and there was a strong correlation between TCSPDS and QOL (r=0.767, P<0.01). These results indicated that patients with higher TCSPDS scores reported a lower QOL, poorer global health and function, and more prominent symptoms (Table 5).
Discussion
Our study showed that the self-perceived discrimination of thyroid cancer patients was mainly manifested in three dimensions: stigma, self-deprecation and social avoidance. Although patients had objective stigma from others, patients’ subjective self-deprecation and social avoidance were more common. Therefore, we developed a 20-item TCSPDS based on classical test theory specifically to assess self-perceived discrimination in thyroid cancer patients. Exploratory factor analysis extracted three common factors: stigma, self-deprecation and social avoidance. The correlated three-factor model had a good fit with the initial theory (χ2/df=1.971, GFI=0.921, CFI=0.930, TLI=0.901). The I-CVI, the content correlation (Pearson correlation coefficients ranged from 0.343 to 0.722, P<0.01) and the validity coefficient (r=0.767, P<0.01) were satisfactory. These results proved that the TCSPDS had good content, construct and criterion-related validity. The Cronbach’s alpha of the TCSPDS was 0.867, the Spearman-Brown coefficient was 0.828, and the ICC was 0.981, which proved that the TCSPDS had good reliability. The completion time (15.01 ± 1.348 minutes) and effective response rate (95.14%) of the TCSPDS were satisfactory, which suggested that the TCSPDS had good acceptability. Thus, the TCSPDS can be used to estimate the self-perceived discrimination factors of stigma, self-deprecation, and social avoidance associated with thyroid cancer.
Compared with the CSPDS and SSS, the TCSPDS has higher reliability and comprehensiveness. The reliability of the TCSPDS was higher than that of the CSPDS (Cronbach’s alpha=0.829) (21). Although the TCSPDS had eight items that were similar to items on the CSPDS, we included 12 items that were more comprehensive in assessing self-perceived discrimination of thyroid cancer, such as disfigurement and glandular dysfunction. Furthermore, although the Cronbach’s alpha of the TCSPDS may be lower than that of the SSS (Cronbach’s alpha=0.930) (20), the TCSPDS had better construct validity and test-retest reliability, and we added a self-deprecation subscale. Most thyroid cancer patients said in the interview that self-deprecation was the main cause of self-perceived discrimination, so adding the self-deprecation subscale may make the evaluation content more comprehensive.
The specificity of TCSPDS is higher than that of CSPDS and SSS. The CSPDS is a universal scale for all cancer patients (21), which can only preliminarily evaluate the self-perceived discrimination shared by all cancer patients but cannot estimate the self-perceived discrimination specific to thyroid cancer, so it still lacks specificity. The SSS mainly focuses on the influence of the facial appearance of patients with oral cancer (20), while the biological characteristics, treatment methods and prognosis of thyroid cancer are different from those of oral cancer; in particular, the implementation of endoscopic thyroidectomy has greatly improved the appearance of the neck of patients with thyroid cancer. Therefore, the TCSPDS may be a more promising early screening tool for self-perceived discrimination in thyroid cancer.
In China, because of the lack of health knowledge, the public is afraid of “talking about cancer”. Some people believe in feudal superstitions and mistakenly believe that cancer is “retribution from heaven” and even think that being close to cancer patients will lead to “misfortune”, and thus deliberately avoid cancer patients. The change in appearance may reduce confidence for thyroid cancer patients, causing them to fear communicating with others face to face or going out in public, as they want to avoid others seeing their neck wound. Thyroid cancer patients can be very embarrassed if others pay attention to their neck wounds. Therefore, they usually try to avoid the sight of others by lowering their heads or pulling up their collars. However, owing to the lack of thyroid gland function after surgery, long-term oral administration of “levothyroxine sodium tablets” has undoubtedly become a characteristic label for patients with thyroid cancer. Moreover, patients usually need their families to accompany them to their medical treatments, yet they cannot provide help in return to their families. Due to the internal pressure of family responsibility, patients tend to think that they are a burden to their families. Consequently, our research provides more evidence for cancer-related discrimination.
Interestingly, our study found that financial burden, sex, disease duration and operation method were independent risk factors for patients’ self-perceived discrimination. Patients with heavy economic burdens have higher self-perceived discrimination, and continuously increasing costs of thyroid cancer treatment and long-term review, and a decline in physical fitness and work ability caused by the toxicity of the treatment is less conducive to their return to society, which undoubtedly brings a heavy economic burden to their entire families one that often aggravates their self-perception burden (18). In addition, patients with short disease duration and open thyroidectomy had stronger self-perceived discrimination, which may be related to postoperative toxicity, such as physiological and social dysfunction and image disfigurement, especially for female patients. Patients often have difficulty adapting to their sudden change in appearance after an open thyroidectomy, and a poor appearance is more likely to cause others’ rejection and aversion, undoubtedly having a heavy psychological blow on female patients (40). Although endoscopic thyroidectomy has certain advantages, a large proportion of patients still undergo open thyroidectomy for various reasons, such as the presence of lateral neck compartment lymph node metastasis, local invasive carcinoma, previous neck surgery or irradiation, and financial difficulties. Therefore, more attention needs to be paid to the mental health status of open thyroidectomy patients (41). However, as time passes, patients’ self-perceived discrimination may improve to some extent from the positive psychological adjustment effect, which can help them recover their original mental state (42). Therefore, in addition to paying attention to the treatment of primary diseases, medical staff should also pay more attention to patients’ psychological problems, and actively prevent and alleviate their self-perceived discrimination, to reduce the occurrence of mental diseases.
Notably, the TCSPDS is negatively correlated with QOL in patients with thyroid cancer, and there is a strong correlation between the two (r=0.767, P < 0.01). Patients with higher TCSPDS scores have lower QOL, worse global health and function, and more prominent symptoms. Although thyroid cancer has a good prognosis, long-term psychological distress, such as disease recurrence and fear of death and dysfunction, may make it difficult for patients to realize their own social values and maintain stable interpersonal relationships (11–13, 43). Self-perceived discrimination may aggravate the antagonism and contradiction between thyroid cancer patients and the general population, and the problems of disfigurement and long-term dysphonia further affect the normal social activities of patients (44, 45). Additionally, the insomnia, fatigue and paresthesia caused by treatment toxicity not only aggravate patients’ physical decline and feelings of inferiority but also significantly affect patients’ daily life and work (46–48). Therefore, the TCSPDS will help with early identification of these problems and will help the development and implementation of targeted health education, psychological counseling and social support. This may ultimately improve the QOL in patients with thyroid cancer.
As an exploratory study, this study had a limited sample size and was derived from a single center. The sample used in this study only included people from Southwest China, where economic development is relatively underdeveloped, so the results of this study only represent the situation of thyroid cancer patients in Southwest China. Future research should cover a larger sample size of multiple centers and multiple fields to analyze the correlation between self-perceived discrimination and other negative psychological factors (anxiety, depression, fear, etc.). Further exploration of the impact mechanism of self-perceived discrimination on the QOL will provide more powerful evidence to reduce the self-perceived discrimination of thyroid cancer patients and improve their QOL.
If any researcher needs to use this scale, we allow him or her to translate it into other languages or make modifications and confirm its validity and reliability.
Conclusion
Our study shows that the TCSPDS is effective and reliable in assessing self-perceived discrimination in thyroid cancer patients and can be used as a basis for health education, psychological counseling and social support in the future, especially in Southwest China.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Yunnan Cancer Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
Z-JL: Study design, data analysis and manuscript preparation. L-SF, FL, L-RY, W-QW, YH, Z-TM: Data collection. Y-FW: Study design, data interpretation and manuscript modification. All authors read and approved the final manuscript.
Funding
This study was supported by Program of Philosophy and Social Science Foundation of Yunnan Province (No. QN202214) and Yunnan Provincial Education Department Fund Project (No. JX0036).
Acknowledgments
We would like to extend our heartfelt gratitude to all thyroid cancer patients for their participation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
TCSPDS, Thyroid Cancer Self ⁃Perceived Discrimination Scale; QOL, Quality of life; EFA, Exploratory factor analysis; CFA, Confirmatory factor analysis; SEM, Structural equation modeling; I-CVI, Item-level content validity index; ICC, Intra-class correlation coefficient; χ2/df, Chi-square fit statistics/degree of freedom; RMSEA, Root mean square error of approximate; GFI, Goodness of fit index; CFI, Comparative fit index; NFI, Normed fit index; IFI, Incremental fit index; TLI, Tucker-lewis index; CRV, Criterion-related validity; ANOVA, Analysis of variance; CSPDS, Cancer Self ⁃Perceived Discrimination Scale; SSS, Shame and Stigma Scale; PCA, Principal component analysis.
References
1. Lin L, Li Z, Yan L, Liu Y, Yang H, Li H. Global, regional, and national cancer incidence and death for 29 cancer groups in 2019 and trends analysis of the global cancer burden, 1990-2019. J Hematol Oncol (2021) 14:197–220. doi: 10.1186/s13045-021-01213-z
2. Zheng R, Zhang S, Zeng H, Wang S, Sun K, Chen R, et al. Cancer incidence and mortality in China, 2016. Natl Cancer Cent (2022) 27:1–9. doi: 10.1016/j.jncc.2022.02.002
3. DeLamater J, Collett J. Social psychology. 9nd ed. New York: Taylor & Francis Press (2018) p. 197–233.
4. Krieger N. A glossary for social epidemiology. J Epidemiol Commun H (2001) 55:693–700. doi: 10.1136/jech.55.10.693
5. Stergiou-Kita M, Pritlove C, Kirsh B. The "Big c"-stigma, cancer, and workplace discrimination. J Cancer Surviv (2016) 10:1035–50. doi: 10.1007/s11764-016-0547-2
6. Batchelder AW, Burgess C, Perlson J, O'Cleirigh C. Age and year of HIV diagnosis are associated with perceptions of discrimination and internalized stigma among sexual minority men who use substances. AIDS Behav (2022) 26:125–37. doi: 10.1007/s10461-021-03333-6
7. Stickley A, Oh H, Sumiyoshi T, Narita Z, DeVylder JE, Jacob L, et al. Perceived discrimination and psychotic experiences in the English general population. Eur Psychiat (2019) 62:50–7. doi: 10.1016/j.eurpsy.2019.08.004
8. Chowdhury D, Lund EM, Carey CD, Li Q. Intersection of discriminations: experiences of women with disabilities with advanced degrees in professional sector in the United States. Rehabil Psychol (2022) 67:28–41. doi: 10.1037/rep0000419
9. Williamson TJ, Garon EB, Shapiro JR, Chavira DA, Goldman JW, Stanton AL. Facets of stigma, self-compassion, and health-related adjustment to lung cancer: a longitudinal study. Health Psychol (2022) 41:301–10. doi: 10.1037/hea0001156
10. Rose S, Boyes A, Kelly B, Cox M, Palazzi K, Paul C. Help-seeking behaviour in newly diagnosed lung cancer patients: assessing the role of perceived stigma. PSYCHO-ONCOLOGY (2018) 27:2141–7. doi: 10.1002/pon.4779
11. Hedman C, Strang P, Djärv T, Widberg I, Lundgren CI. Anxiety and fear of recurrence despite a good prognosis: an interview study with differentiated thyroid cancer patients. Thyroid (2017) 27:1417–23. doi: 10.1089/thy.2017.0346
12. Misra S, Meiyappan S, Heus L, Freeman J, Rotstein L, Brierley JD, et al. Patients' experiences following local-regional recurrence of thyroid cancer: a qualitative study. J Surg Oncol (2013) 108:47–51. doi: 10.1002/jso.23345
13. Dionisi-Vici M, Fantoni M, Botto R, Nervo A, Felicetti F, Rossetto R, et al. Distress, anxiety, depression and unmet needs in thyroid cancer survivors: a longitudinal study. Endocrine (2021) 74:603–10. doi: 10.1007/s12020-021-02786-y
14. Vrinten C, McGregor LM, Heinrich M, von Wagner C, Waller J, Wardle J, et al. What do people fear about cancer? a systematic review and meta-synthesis of cancer fears in the general population. Psycho-Oncology (2017) 26:1070–9. doi: 10.1002/pon.4287
15. Pitt SC, Saucke MC, Wendt EM, Schneider DF, Orne J, Macdonald CL, et al. Patients' reaction to diagnosis with thyroid cancer or an indeterminate thyroid nodule. Thyroid (2021) 31:580–8. doi: 10.1089/thy.2020.0233
16. Kurumety SK, Helenowski IB, Goswami S, Peipert BJ, Yount SE, Sturgeon C, et al. Post-thyroidectomy neck appearance and impact on quality of life in thyroid cancer survivors. Surgery (2019) 165:1217–21. doi: 10.1016/j.surg.2019.03.006
17. Liu YH, Xue LB, Zhang S, Yang YF, Li J. Appearance characteristics of incision, satisfaction with the aesthetic effect, and quality of life in of thyroid cancer patients after thyroidectomy. Int J Health Plan M (2021) 36:784–92. doi: 10.1002/hpm.3111
18. Mongelli Michael N, Sneha G, Peipert Benjamin J, Helenowski Irene B, Yount Susan E. Financial burden and quality of life among thyroid cancer survivors. Surgery (2020) 167:631–7. doi: 10.1016/j.surg.2019.11.014
19. Alhashemi A, Jones JM, Goldstein DP, Mina DS, Thabane L, Sabiston CM, et al. An exploratory study of fatigue and physical activity in Canadian thyroid cancer patients. Thyroid (2017) 27:1156–63. doi: 10.1089/thy.2016.0541
20. Kissane DW, Patel SG, Baser RE, Bell R, Farberov M, Ostroff JS, et al. Preliminary evaluation of the reliability and validity of the shame and stigma scale in head and neck cancer. Head Neck (2013) 35:172–83. doi: 10.1002/hed.22943
21. Feng LS, Li XY, Wang HR, Zhan JJ, Chen D, Wang YF. Development and validation of the cancer self-perceived discrimination scale for Chinese cancer patients. Health Qual Life Outcomes (2018) 16:165–73. doi: 10.1186/s12955-018-0984-x
22. Tam S, Boonsripitayanon M, Amit M, Fellman BM, Li Y, Busaidy NL, et al. Survival in differentiated thyroid cancer: comparing the AJCC cancer staging seventh and eighth editions. THYROID (2018) 28:1301–10. doi: 10.1089/thy.2017.0572
23. Hamilton AB, Finley EP. Qualitative methods in implementation research: an introduction. Psychiat Res (2019) 280:112516. doi: 10.1016/j.psychres.2019.112516
24. Fife BL, Wright ER. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Soc Behav (2000) 41:50–67. doi: 10.2307/2676360
25. Cataldo JK, Slaughter R, Jahan TM, Pongquan VL, Hwang WJ. Measuring stigma in people with lung cancer: psychometric testing of the cataldo lung cancer stigma scale. Oncol Nurs Forum (2011) 38:46–54. doi: 10.1188/11.ONF.E46-E54
26. Pirola WE, Paiva BSR, Barroso EM, Kissane DW, Serrano CVMP, Paiva CE. Translation and cultural adaptation of the shame and stigma scale (SSS) into Portuguese (Brazil) to evaluate patients with head and neck cancer. Braz J Otorhino-laryngol (2017) 83:697–704. doi: 10.1016/j.bjorl.2016.10.005
27. Pirola WE, Paiva BSR, de Oliveira CZ, Lucchetti G, Lucchetti ALG, Kissane D, et al. Validation of the Brazilian version of the shame and stigma scale (SSS-br) for patients with head and neck cancers. Palliat Support Care (2020) 18:186–92. doi: 10.1017/S1478951519000488
28. Tseng WT, Lee Y, Hung CF, Lin PY, Chien CY, Chuang HC, et al. Validation of the Chinese version of the shame and stigma scale in patients with head and neck cancer. Cancer Manage And Res (2019) 11:10297–305. doi: 10.2147/CMAR.S228843
29. He H, Zhou T, Zeng D, Ma Y. Development of the competency assessment scale for clinical nursing teachers: results of a Delphi study and validation. Nurs Educ Today (2021) 101:104876. doi: 10.1016/j.nedt.2021.104876
30. Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst (1993) 85:365–76. doi: 10.1093/jnci/85.5.365
31. Gagne P, Hancock GR. Measurement model quality, sample size, and solution propriety in confirmatory factor models. Multivar Behav Res (2006) 41:65–83. doi: 10.1207/s15327906mbr4101_5
32. Fu Y, Wen Z, Wang Y. A comparison of reliability estimation based on confirmatory factor analysis and exploratory structural equation models. Educ Psychol Meas (2022) 82:205–24. doi: 10.1177/00131644211008953
33. Montoya AK, Edwards MC. The poor fit of model fit for selecting number of factors in exploratory factor analysis for scale evaluation. Educ Psychol Meas (2021) 81:413–40. doi: 10.1177/0013164420942899
34. Schneider S, Yoon D, Mokros A, Schwarz MF, Baster A, Koehler D. The elemental psychopathy assessment (EPA): factor structure and construct validity across three German samples. Psychol Assess (2022) 34:717–30. doi: 10.1037/pas0001126
35. Fino E, Humphries M, Robertson J, Orosz G, Griffiths MD. Factor structure, reliability and criterion-related validity of the English version of the problematic series watching scale. BJPsych Open (2022) 8:1–9. doi: 10.1192/bjo.2022.561
36. Viladrich C, Angulo-Brunet A, Doval E. Un viaje alrededor de alfa y omega para estimar la fiabilidad de consistencia interna. Psicol-Spain (2022) 33:755–82. doi: 10.6018/analesps.33.3.268401
37. Barchard KA, Brouwers V. Internal consistency and power when comparing total scores from two groups. Multivar Behav Res (2016) 51:482–94. doi: 10.1080/00273171.2016.1166422
38. Wang WJ, Dong J, Ren ZP, Chen B, He W, Li WD, et al. Validity, reliability, and acceptability of the scale of knowledge, attitude, and behavior of lifestyle intervention in a diabetes high-risk population. Zhonghua Yu Fang Yi Xue Za Zhi (2016) 50:584–8. doi: 10.3760/cma.j.issn.0253-9624.2016.07.004
39. Heavner MS, Gorman EF, Linn DD, Yeung SYA, Miano TA. Systematic review and meta-analysis of the correlation between bispectral index (BIS) and clinical sedation scales: toward defining the role of BIS in critically ill patients. PHARMACOTHERAPY (2022) 42:667–76. doi: 10.1002/phar.2712
40. Bach K, Prince S, Pitt SC, Robbins S, Connor NP, Macdonald C, et al. Time heals most wounds-perceptions of thyroidectomy scars in patients with thyroid cancer. J Surg Res (2022) 270:437–43. doi: 10.1016/j.jss.2021.09.041
41. Rossi L, Materazzi G, Bakkar S, Miccoli P. Recent trends in surgical approach to thyroid cancer. Front Endocrinol (Lausanne) (2021) 12:699805. doi: 10.3389/fendo.2021.699805
42. Seok JH, Choi WJ, Lee YS, Park CS, Oh YJ, Kim JS, et al. Relationship between negative mental adjustment to cancer and distress in thyroid cancer patients. Yonsei Med J (2013) 54:658–64. doi: 10.3349/ymj.2013.54.3.658
43. Papaleontiou M, Reyes-Gastelum D, Gay BL, Ward KC, Hamilton AS, Hawley ST, et al. Worry in thyroid cancer survivors with a favorable prognosis. Thyroid (2019) 29:1080–8. doi: 10.1089/thy.2019.0163
44. Noto B, Asmus I, Schäfers M, Görlich D, Riemann B. Predictors of anxiety and depression in differentiated thyroid cancer survivors: results of a cross-sectional study. Thyroid (2022) 32:1077–85. doi: 10.1089/thy.2022.0067
45. Li C, Lopez B, Fligor S, Broekhuis JM, Maeda A, Duncan S, et al. Long-term voice changes after thyroidectomy: results from a validated survey. Surgery (2021) 170:1687–91. doi: 10.1016/j.surg.2021.04.060
46. Hughes DT, Reyes-Gastelum D, Kovatch KJ, Hamilton AS, Ward KC, Haymart MR, et al. Energy level and fatigue after surgery for thyroid cancer: a population-based study of patient-reported outcomes. Surgery (2020) 167:102–9. doi: 10.1016/j.surg.2019.04.068
47. Pitt SC, Haymart MR. Breaking down or waking up? psychological distress and sleep disturbance in patients with thyroid nodules and cancer. J Clin Endocr Metab (2021) 106:4278–80. doi: 10.1210/clinem/dgab319
Keywords: thyroid cancer, psychometrics, psycho-oncology, scale development, validation, quality of life
Citation: Liu Z-j, Feng L-s, Li F, Yang L-r, Wang W-q, He Y, Meng Z-t and Wang Y-f (2023) Development and validation of the thyroid cancer self-perceived discrimination scale to identify patients at high risk for psychological problems. Front. Oncol. 13:1182821. doi: 10.3389/fonc.2023.1182821
Received: 09 March 2023; Accepted: 03 July 2023;
Published: 18 July 2023.
Edited by:
Li-Ang Lee, Chang Gung University, TaiwanReviewed by:
Yu Lan, China Medical University, ChinaDante De Paz, Universidad Peruana Cayetano Heredia, Peru
Copyright © 2023 Liu, Feng, Li, Yang, Wang, He, Meng and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu-feng Wang, MTM1NzcwMzc1ODVAMTYzLmNvbQ==
 Zhi-jin Liu
Zhi-jin Liu Lin-sen Feng
Lin-sen Feng Feng Li1
Feng Li1