- 1Department of Public Health, Goba Referral Hospital, Madda Walabu University, Goba, Ethiopia
- 2Department of Public Health, Madda Walabu University, Shashemene, Ethiopia
- 3Department of Public Health, College of Medicine and Health Science, Wolkite University, Wolkite, Ethiopia
- 4Department of Public Health, College of Medicine and Health Science, Wolayta Sodo University, Sodo, Ethiopia
Regular breast self-examination is the most cost-effective method for early detection of breast cancer, especially in resource-limited countries. However, breast self-examination practice was low among reproductive-age women.
Objective: This study aims to evaluate breast self-examination practice and associated factors among women of reproductive age in southeast Ethiopia.
Methods: A convergent parallel mixed-methods study design was conducted on 836 women of reproductive age. An interviewer-administered questionnaire was used for the quantitative part of the study and supplemented by focus group discussions. A database was created using Epi-info version 3.5.3, and analyzed using SPSS version 20. Bivariate and multivariable logistic regressions were done to examine the effect of explanatory variables. Variables with p-value <0.05 during multivariable logistic regressions were considered as significantly associated with the dependent variable. Thematic data analysis was carried out for the qualitative study.
Result: Out of 836 total participants, only 20.7% had ever heard about breast self-examination practice. Also, only 13.2% of the mothers had practiced breast self-examinations. Even though the majority of the participants during focused group discussions had knowledge about breast cancer screening, most of them stated that breast self-examination was not practiced among them. Maternal age, mother’s level of education, and previous history of breast examination by health professionals were significant predictors of breast self-examination practices.
Conclusion: This study reported a low prevalence of breast self-examination practice. Therefore, enhancing women’s education and encouraging breast examination by health professionals are essential to increase the proportion of women performing breast self-examination.
Introduction
Breast cancer (BC) is typically asymptomatic when the tumor is small and easily treated. Therefore, it is very essential for women to follow suggested screening rules in detecting BC in the early stage (1). Before BC develops to a size that can be felt, the most common physical sign is a painless lump or swelling until the original breast tumor itself is large enough to be felt (2–4). Other common signs and symptoms include breast pain or heaviness, persistent changes in the breast (swelling, thickening, or redness of the breast’s skin), nipple abnormalities (spontaneous bloody discharge), erosion, inversion, and tenderness (1, 5).
Age is the most important factor for BC risk in women. It will affect women in their most productive years of life. More breast cancer cases are identified in developing countries than those in developed countries among women of reproductive age (15–49 years) (6). The other risk factors for BC are inherited mutations in susceptible genes; a personal or family history of BC; high breast tissue densities; high dose radiations to the chest resulting from medical procedures (7); reproductive factors that increase risks (early start of menstrual periods and/or end later in life); not ever having children; prolonged use of oral contraceptives; and having a child after the age of 30. Some other factors that increase risk include being overweight or obese after menopause, use of menopausal hormone therapy (combined), physical inactivity, and consumption of alcohol (8).
The most imperative strategies in achieving early detection of BC are mammography and physical examination of the breasts by qualified health workers, or clinical breast examination (CBE) and breast self-examination (BSE) (6, 9, 10). BSE has been broadly recommended as a comparatively simple, non-offensive, non-harmful, and cost-free screening technique when comparing to other types of screening approaches for breast cancer (11, 12). It is a technique established for the purpose of assessing cancer; a woman uses her hands to systematically examine her breasts and the immediate areas for unfamiliar lumps and shape changes. Usually done on a fixed monthly basis, the same technique is used each time, ensuring that all areas of the breast are sensed and checked thoroughly.
In 2018, breast cancer represents approximately 24.2% of all new cancer cases and 15% of 4.2 million deaths due to cancer globally, of which sub-Saharan Africa accounts for 8.1% of breast cancer cases and 11.8% of breast cancer deaths. It is the most prevalent cancer in developing countries (6, 9, 13). In Ethiopia, BC is typically a fatal disease among women with a 24.4% prevalence rate (6, 14). Early detection makes the disease easier to treat. Some authors suggest that BSE does not significantly reduce the breast cancer mortality, but the awareness among women about their breasts provides them with knowledge to seek medical help early in order to improve the prognosis (15, 16). BSE is a recommended diagnostic method and an important technique in the prevention of breast cancer, especially in resource-limited countries (6, 14, 15). However, stigma towards cancer; poor knowledge of BC related to signs, symptoms, and its treatability; and system overload continue to account for delays in reaching care (17). Ethiopian women are usually alerted in the late stage of the disease (10, 18). In Ethiopia, reproductive-age women know little about BSE (6). Therefore, this study was designed to identify the prevalence of BSE and associated factors among reproductive-age women in Bale Zone, southeast Ethiopia.
Materials and methods
Study design, area, and period
A convergent parallel mixed-methods study design was conducted from 1 March 2017 to 30 May 2017 in Bale Zone. Robe town is the capital city of Bale Zone, which is 430 km from Addis Ababa, the capital city of Ethiopia. The Bale Zone has 20 districts with farming communities predominating. The study was conducted in Ginnir, Sinana, and Madda Walabu districts, which are located at 560 km, 430 km, and 630 km southeast of Addis Ababa, respectively. According to the last census survey (2007) projection in 2017, the estimated population of Ginnir, Sinana, and Madda Walabu districts were 159,766, 154,170, and 127,426, respectively. Women of childbearing age numbered 35,357 for the Ginnir district, 34,118 for the Sinana district, and 28,200 for the Madda Walabu district (19). The Ginnir district has 33 kebeles (kebele refers to the smallest administrative unit), of which 30 are rural and 3 are urban; the Sinana district has 29 kebeles, of which 27 are rural and 2 are urban; and the Madda Walabu district has 22 kebeles, of which 20 are rural and 2 are urban. The Ginnir district has eight health centers and 32 health posts, the Sinana district has six health centers and 26 health posts, and the Madda Walabu district has six health centers and 24 health posts. Each district has one hospital in their capital town that serves as referral centers. These hospitals do not provide breast cancer treatment, so women have to travel to Addis Ababa for treatment.
Patient and public involvement
In the selected household, adult participants responded to the questionnaire.
Inclusion criteria
All selected women of childbearing age (15–49 years) living in the study area and residing for more than 6 months in the selected district and interest in participating in the study were included in both qualitative and quantitative sections.
Exclusion criteria
Non-Ethiopians, pregnant women, women with known breast cancer, seriously ill women during data collection, and women not willing to participate in the study were excluded in both quantitative and qualitative studies. Participants in the quantitative study were also excluded from the qualitative study.
Sample size determination
A single population proportion formula was used to determine the sample size for the quantitative data. A sample size of 841 was calculated based on an estimated proportion of BSE practice of 53.6% (20); the desired precision was 5% with 95% confidence level and a design effect of 2, including a 10% non-response rate.
Six focus group discussions (FGDs) were conducted for the qualitative part, which was supplementary to the quantitative study, with two FGDs in each district. A total of 59 discussants participated (21). Five FGDs had 10 participants in each discussion, whereas 9 participants were involved in one FGD. The inclusion criteria for this study was women aged 15 to 49 years old, with no known breast cancer, and not having other severe illnesses that could have prevented them from responding.
Sampling procedure
A multi-stage sampling technique was used to select the study participants. In the first stage, three districts were selected randomly. The kebeles in the selected districts were identified and stratified into urban and rural kebeles. The selected urban and rural districts were selected by using a lottery method. The selection of kebeles was dependent on their distance from the capital town of the district, taking the hospital as a center. For the three districts, the furthest kebeles on average were 45 km from the center. Three kebeles closest to the town (at approximately 15 km), three kebeles from the middle region (at the second 15 km), and three kebeles furthest from the town (at the third 15 km) were selected randomly. A list of all households with eligible mothers was identified; finally, we used a sampling frame to pick the study participants using the simple random sampling method.
For the qualitative data, purposive sampling technique was used to select participants. From each selected district, two groups of childbearing-age women not included in the quantitative study were asked to participate in the FGD.
Data collection and data quality assurance
For quantitative data collection, a standardized questionnaire was initially developed in the English language after reviewing different literature reflecting the purpose of the study (22–24), then translated to the local language (Afan Oromo), and back translated to English. Data were also collected using face-to-face interviews.
Twelve diploma nurses collected interview data guided by three supervisors. The training of data collectors and supervisors mainly focused on issues such as data collection tools, field methods, inclusion–exclusion criteria, and record keeping. The investigators coordinated the interview process and reviewed completed questionnaires on a daily basis to ensure completeness and consistency of the data. The questionnaire was pre-tested on 5% of the sample outside the selected district for this study.
The FGDs were held in the community meeting room and in health posts at the participant’s districts. The participants were women of childbearing age (15–49 years old) not included in the quantitative study and recruited purposively. An interview guide was used to conduct the FGD and a tape recorder was used to capture the conversation. The interview guide was originally prepared in English, then translated to the local language (Afan Oromo), and translated back to English to check the consistency. Each FGD was conducted by two trained female degree holder nurses; one moderated the discussion while the other took notes and recorded the tape. One gatekeeper (non-health professional) for each FGD was assigned.
Data analysis
The quantitative data was entered into a database using Epi-info, version 3.5.3, and it was exported to SPSS version 20 for data analysis. First, descriptive statistics were used to describe the data. Then, simple logistic regression analysis was carried out; those variables that were significant at p ≤ 0.25 were retained for subsequent multivariable logistic regression. Strength of association was tested using adjusted odds ratio (AOR) and 95% confidence interval (CI). The significance level considered for multivariable logistic regressions was p ≤ 0.05.
For qualitative data, tape recordings were transcribed, organized in narrative forms congruent with the respondents’ own words, and analyzed under selected themes based on the question guide and summarized manually; i.e., thematic type of data analysis was carried out for the qualitative study.
Results
Socio-demographic characteristics
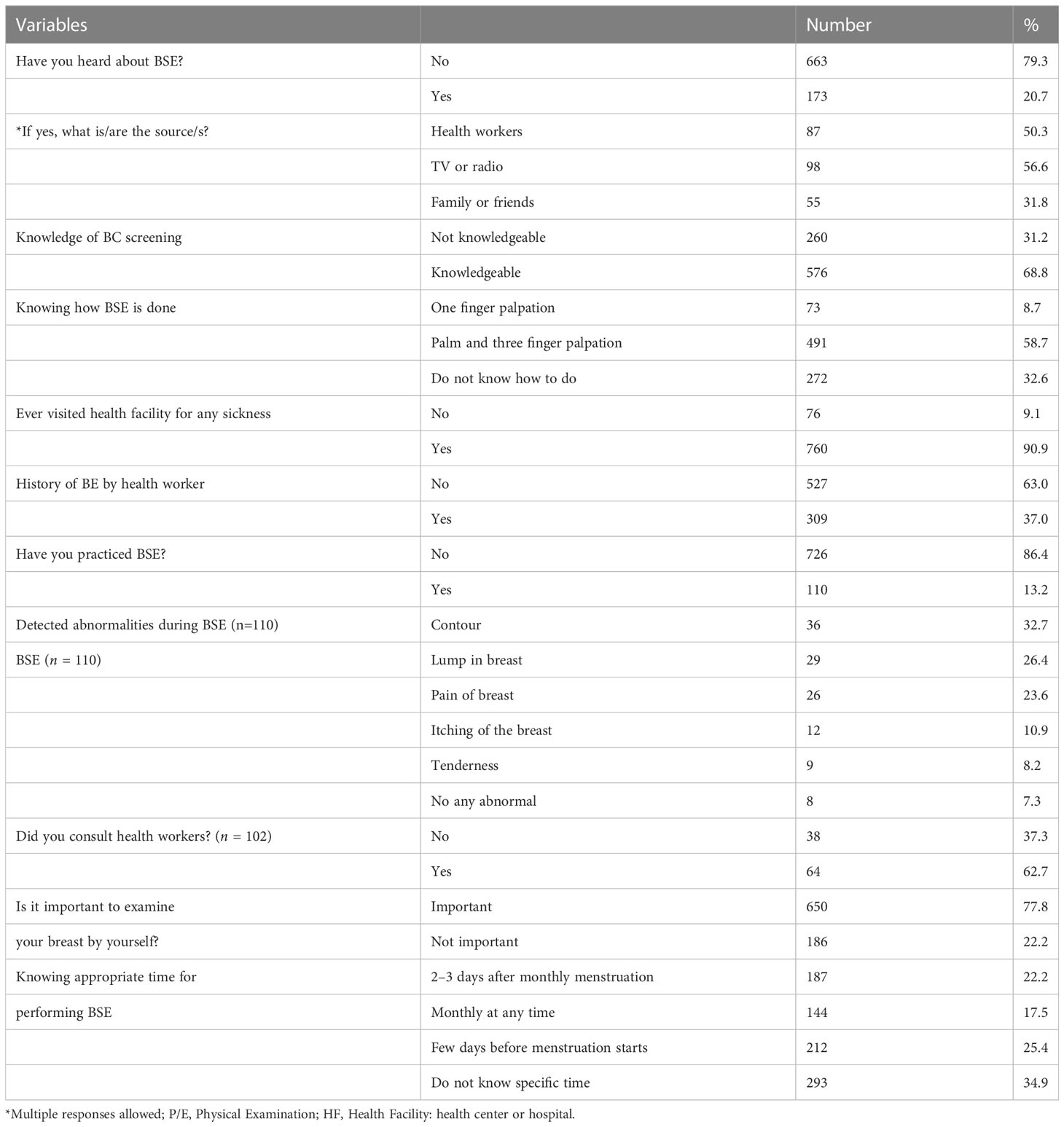
A total of 836 mothers completed the questionnaire for a response rate of 99.4%. The mothers had a mean ( ± SD) age of 31.09 ± 7.34 years. Forty-five percent of the study participants were illiterate. The majority [744 (89.0%)] of the study participants were married. Ninety percent of women were housewives. Regarding the husband’s level of education, more than half [439 (52.5%)] had finished primary school. The majority [463 (55.4%)] of respondents had a monthly income below the poverty line (less than 1,311 EB or $1.90 per month). The majority [475 (56.8%)] of the study participants had a television or radio. The majority [210 (74.9%)] were rural dwellers. Health centers or hospitals were very close to 667 (79.8%) of the study participants (approximately 5 km or less, maximum journey of 2 h on foot) (Table 1).
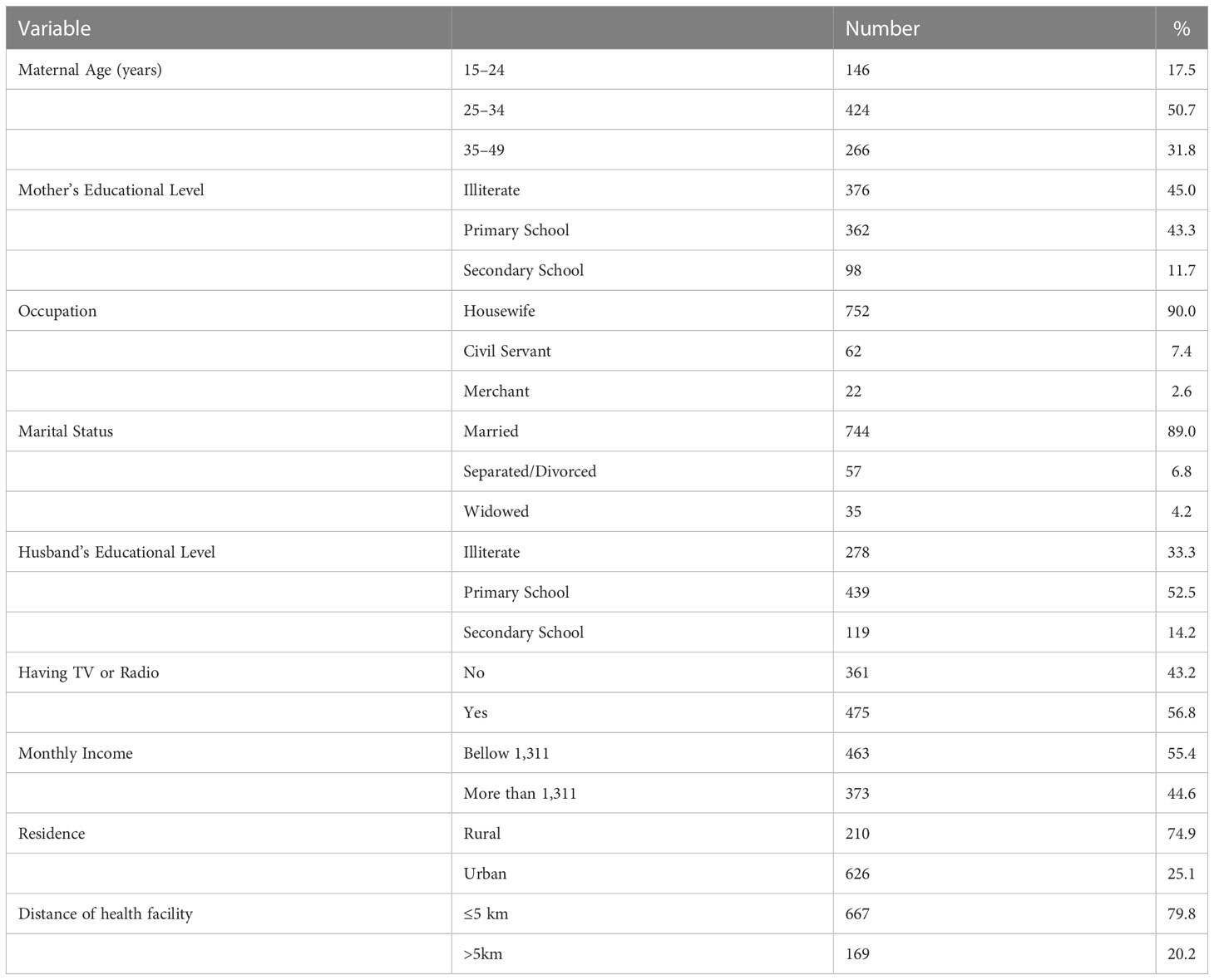
Table 1 Socio-demographic characteristics of the respondents in Bale zone, southeast Ethiopia, 2017.
Breast self-examination practice
The majority [576 (68.8%)] of the respondents had sufficient knowledge about breast cancer screening. Regarding sources of information, television and radio were the main sources [98 (56.6%)]. This finding was supported by comments from a 19-year-old merchant mother who reported, “…in our place there is no awareness creating activities or education by doctors on breast problem: presence of the disease, its consequences, its sign and symptoms, and its risk factors, and an option for treatment. We heard information from the television and radio. Some of us even heard the presence of its management today from this discussion.”
A middle-aged adult civil servant also stated that, “…I heard my neighbor complaining of a breast disease; I heard also that the disease was cancer. Many women have suffered with disease of the breast, yet I haven’t seen any breast disease on my body…. When I was a child, I heard a neighbor who died due to breast disease. Her breast was wounded, and she was referred and taken far out of this area to receive better treatment in referral hospitals. Even though she had visited many hospitals, she died as the consequence of the disease.”
Only 187 (22.2%) participants knew the appropriate timing to perform BSE. The knowledge of how BSE is performed was known to 491 (58.7%) of the study participants. The majority [650 (77.8%)] of the mothers responded that performing BSE is important. Above 90% of respondents had visited health facilities at some time for sickness. However, only 37% of the mothers had a CBE by health workers during the visit (Table 2).
During another FGD, a housewife in her early 20s reported, “…this breast disease is certainly present in its massive form; I have not experienced this disease on myself; it has hurt many women; and some people say it became “hola” on a woman; some say cancer, and some others say another thing. Even at the moment, there is a woman with breast problem, she gave birth recently, her breast has not produced milk, and she has severe breast ache. The problem is existed among us, however; we don’t know the right time to perform BSE…”
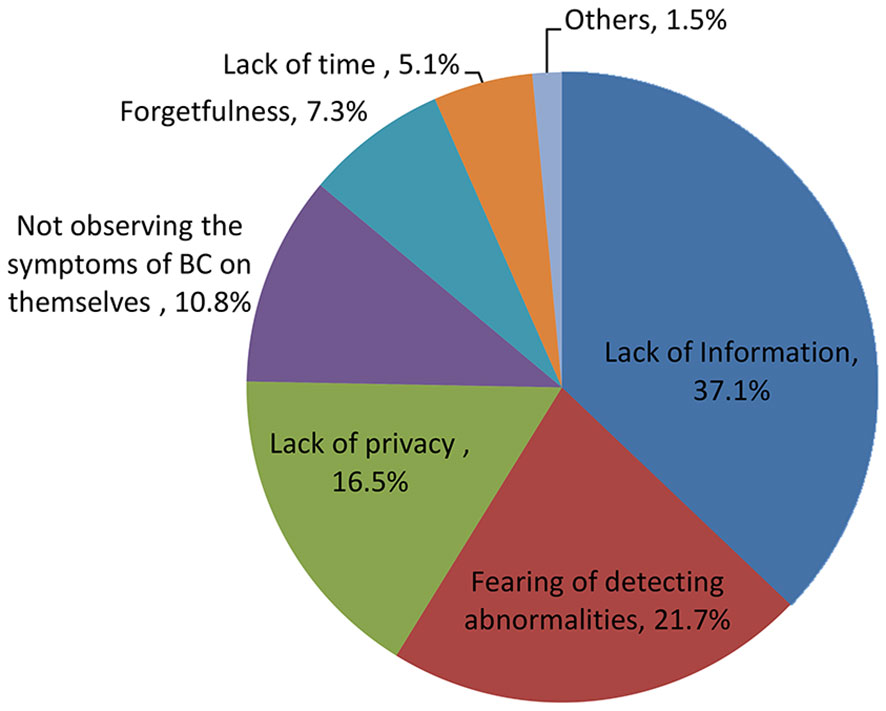
In this study, only 110 (13.2%) mothers performed BSE. The main reasons given by the mothers were lack of information [269 (37.1%)], fear of detecting abnormalities [158 (21.7%)], and lack of privacy [138 (16.5%)] (Figure 1).
During an FGD about BSE, six mothers stated that BSE was not practiced among them. For example, a civil servant in her early 20s reported that, “…I don’t need to touch and examine my breast if I don’t suspect the problem. If it develops a problem, symptoms force us to touch and examine the breast. It is important to see some internally felt discomfort or externally observed signs and symptoms of disease. We don’t know of breast cancer. Therefore, we don’t give focus to our breast. If we have a previous problem, we check the improvement of that problem from time to time. Unless and otherwise, we don’t examine our breast…”
Those mothers who performed BSE had detected abnormalities in their breasts such as changes in contour [36 (32.7%)] and lump in the breast [29 (26.4%)]. The majority [64 (62.7%)] of the respondents who detected abnormalities in their breasts did consult health workers (Table 2).
A middle-aged adult housewife also stated, “… for example, when I have pain of the breast, if all things, even children touch me, I feel pain on both breasts specially at the tip of it, before this time I haven’t ever see such things. For this reason, I have started to touch and look at my breast. If somebody has such problem that woman should touch and examine their own breast, otherwise there is no need to touch…”
During another FDG, a middle-aged adult health extension worker stated that, “…women know their breasts or their bodies especially during a change. Breast pain is not simple, its pain is more severe than other disease; therefore, it is easy to know breast problem on ourselves. However, women have seen this problem traditionally and some of them mostly seek traditional treatment because, they will not permit to expose their breast to health professionals if the disease is not severe. This makes the disease too fatal among our community…”
Factors associated with breast self-examination practice
Women in the age range of young adults and middle age adults were more likely to practice BSE compared to those women in their early 20s, AOR = 3.61 (95% CI: 1.13, 11.58) and AOR = 9.35 (95% CI: 2.31, 37.85), respectively. Participants who have finished primary education, AOR = 3.88 (95% CI: 1.26, 11.98), and secondary and above, AOR = 11.14 (95% CI: 2.48, 49.96), were more likely to practice BSE than illiterate mothers. In addition, participants who have ever had breast examination previously by health workers were more likely to practice BSE compared to those mothers who have never had CBE, AOR = 3.62 (95% CI: 1.15, 11.45) (Table 3).
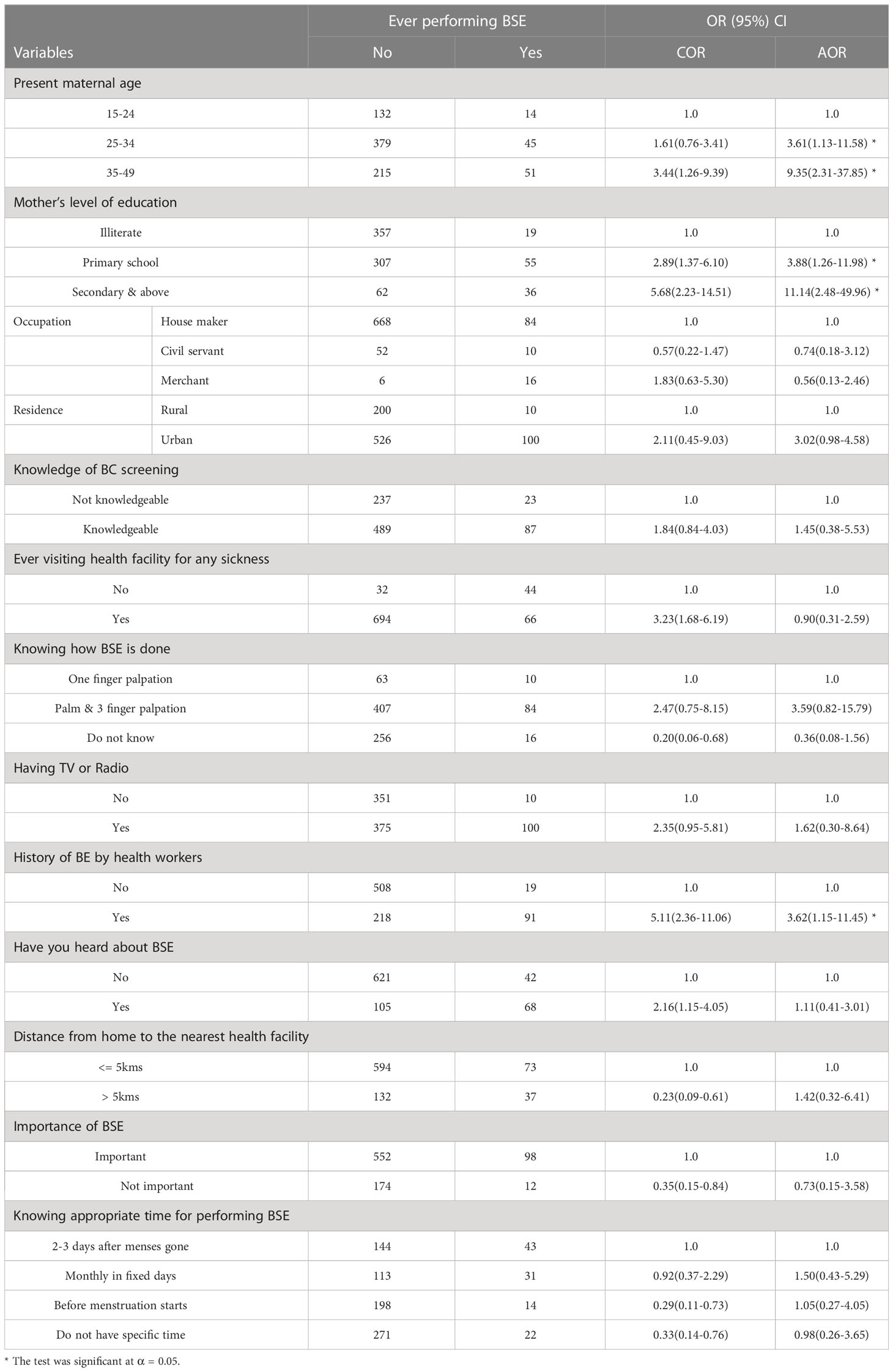
Table 3 Factors associated with breast self-examination practice in Bale zone, southeast Ethiopia, 2017.
Discussion
BSE is an important and inexpensive method for the screening and early detection of breast cancer (16, 25). This study showed that 20.7% of the participants responded that they have heard of BSE. This result was very low compared to a study conducted in Malaysia and Libya (26, 27). The mentioned sources of information on BSE for 56.6% of the study participants were the television and radio, altogether. These findings are consistent with a study conducted in Libya (27). Only 13.2% of those polled had used BSE, according to the findings. This result showed that the information was more frequently practiced than studies conducted in Zambia (5%) and south India (2.4%) (28, 29), but less than found in Malaysia (48%), Nigeria (43.5%), and Ethiopia (53.6%) (20, 27, 30). This idea was corroborated by the finding of the qualitative study. The lower BSE practice could be related to the participant’s lack of knowledge, fear of detection of abnormalities, and lack of privacy. This finding was similar to a study conducted in Iran (31).
This study showed that as a mother’s age increases, especially a female in her early 20s, the practice of BSE increases. This is similar to a study conducted in north Ethiopia (20) and two studies conducted in Nigeria by Oladimeji et al. (2015) and Balogun and Owoaje (2003), which revealed that women in their early 20s and middle-aged adult women practiced BSE. This may be due to the fact that at such ages, women are paying more attention to their reproductive activity, resulting in being aware of and caring for their breasts, due to increased contact with health facilities and health professionals than any other period in their lives. These opportunities may expose mothers to information that can be obtained from health professionals to help them to practice BSE.
Different studies showed that practice of BSE was determined by educational level of mothers. A study done in Libya (26) and another study done in Nigeria (30) reported that higher levels of education were significantly associated with BSE practice. Consistent with these previous studies, our study revealed that BSE was related to mother’s level of education. FGD participants reported that they do not know that the right time to perform BSE was one of the major barriers to BSE practice. This is because educated mothers have a greater awareness of the existence of healthcare and benefited from it by using such services. As education empowers women, they have greater confidence and capability of making decisions to use modern healthcare services (14).
In this study, a previous history of breast examination by a health professional was also another predictor for BSE practice. This result was consistent with a study conducted in northwest Ethiopia, which indicated that health extension workers who had previously had their breasts examined by health professionals were a significant predictor of BSE practice. Participants in the FGD noted that there are no effort from health professionals to raise awareness about BSE practice while they are visiting medical facilities. This could be due to the fact that if mothers came to know how breast examination is done, the probability of continuing examination by themselves seems high (22).
Strengths of the study
We have collected both quantitative and qualitative data, and the questionnaires were produced from standardized sources. The sample size of the study was large enough to establish generalizability to a large population. From the perspective of representativeness, the study included women from three different communities in the rural areas (lowland, temperate, and highland) of Bale Zone.
Limitations of the study
As a cross-sectional study, a cause-and-effect relationship cannot be established to identify the actual predictor. The study focused only on reproductive-age women and did not include older women, for whom concerns about breast cancer may be greater.
Conclusion
The study revealed low BSE practice among reproductive-age women, compared with the other studies conducted in Ethiopia. The proportion of the respondents who had ever heard of BSE was also low. Present maternal age, mother’s level of education, and previous history of breast examination by a health professional were found to have significant associations with BSE practices. Thus, increasing maternal education and coverage of breast examination by health professionals is crucial to increase BSE practice.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
Administrative approval was obtained before conducting the study and an ethical clearance letter was obtained from Madda Walabu University ethical clearance committee with approval number MU-14/51/78. An official letter of collaboration was written to Bale Zone administration and Ginnir, Sinana and Madda Walabu district administrations to get formal permission. Informed consent was obtained from each interviewee. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
AH, MK, JB, AL and SN developed the concept, developed methods, collected data and analyzed them, and drafted and edited the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by Madda Walabu University, Ethiopia. The University has supported this study financially and technically during the design of the study, collection, analysis, interpretation of data, and the writing the manuscript. N/A for award or grant number.
Acknowledgments
The authors are grateful to Madda Walabu University for supporting this study. We are also very grateful to Dr. David Allison for his English language and technical support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
BC, Breast Cancer; BSE, Breast Self-Examination; CBE, Clinical Breast Examination; AOR, Adjusted Odds Ratio; COR, Crude Odds Ratio; FGD, Focus Group Discussion; LMIC, Low- and Middle-Income Countries; OR, Odds Ratio; SPSS, Statistical Package for Social Studies; SSA, Sub-Saharan African Countries; WHO, World Health Organization.
References
2. American Cancer Society. Breast cancer facts and figures (2008). Available at: http://www.cancer.org/downloads/STT/CAFF2005BrFacspdf;2005.pdf (Accessed 20 December 2016).
4. World Health Organization. Global strategy for women's, children's and adolescents' health WHO. (2015). pp. 2016–30.
5. National Breast Cancer Foundation. What is cancer? (2015). 2600 Network Blvd. Suite 300, Frisco, TX 75034 (Accessed 09/08/2017).
6. Birhane K, Alemayehu M, Anawte B, Gebremariyam G, Daniel R, Addis S, et al. Practices of breast self-examination and associated factors among female debre berhan university students. Int J Breast Cancer (2017) 8026297. doi: 10.1155/2017/8026297
7. Worsham MJ, Raju U, Lu M. Risk factors for breast cancer from benign breast disease in a diverse population. Breast Cancer Res Treat (2009) 118(1):1–7. doi: 10.1007/s10549-008-0198-8
8. Ma H, Hill CK, Bernstein L, Ursine G. Low-dose medical radiation exposure and breast cancer risk in women under age 50 years overall and by estrogen and progesterone receptor status: results from a case-control and a case-case comparison. Breast Cancer Res Treat (2008) 109(1):77–90. doi: 10.1007/s10549-007-9625-5
9. Forouzanfar MH, Foreman KJ, Delossantosetal AM. Breast and cervical cancer in 187 countries between 1980 and 2010. Lancet (2011) 378(9801):1461–84. doi: 10.1016/S0140-6736(11)61351-2
10. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer, GLOBOCAN. Int J Cancer (2010) 127:2893–917. doi: 10.1002/ijc.25516
11. Kayode FO, Akande TM, Osagbemi G. Knowledge, attitude and practice of breast self- examination among female secondary school teachers in ilorin, Nigeria. Eurepan J Scientiic Res (2005) 10(3).
13. Tolessa L, Sendo EG, Dinegde NG, Dessalew A. Risk factors associated with breast cancer among women in Addis Ababa, Ethiopia: unmatched case–control study. Int J Women’s Health (2021) 13:101–10. doi: 10.2147/IJWH.S292588
14. Coleman MP, Quaresma M, Berrino F. Cancer survival in five continents: a worldwide population-based study (CONCORD). Lancet Oncol (2008) 9(8):730–56. doi: 10.1016/S1470-2045(08)70179-7
15. Thomas DB, Gao DL, Ray RM, Wang WW, Allison CJ, Chen FL, et al. Randomized trial of breast self-examination in shanghai: final results. J Natl Cancer Institute (2000) 94(19):1445–57. doi: 10.1093/jnci/94.19.1445
16. Hackshaw AK, Paul EA. Breast self-examination and death from breast cancer: a meta-analysis. British J Cancer (2003) 88(7):1047–53. doi: 10.1038/sj.bjc.6600847
17. De Ver Dye T, Bogale S, Hobden C. A mixed-method assessment of beliefs and practice around breast cancer in Ethiopia: implications for public health programming and international journal of breast cancer 5 cancer control. Global Public Health (2011) 6(7):719–31. doi: 10.1080/17441692.2010.510479
18. Andersen RS, Vedsted P, Olesen F, Bro F, Sondergaard J. Patient delay in cancer studies: a discussion of methods and measures. BMC Health Serv Res (2009) 9(189). doi: 10.1186/1472-6963-9-189
19. Central Statistical Authority (CSA). Summary and statistical report of the 2007 population and housing census results, Addis Ababa, Ethiopia: Central statistical agency. (2007).
20. Befikadu L, Teferi G. Knowledge on breast cancer and its prevention among women household heads in northern Ethiopia. Open J Prev Med (2014) 4(1):32–40. doi: 10.4236/ojpm.2014.41006
21. Nyumba TO, Wilson K, Derrick CJ, Mukherjee N. The use of focus group discussion methodology: insights from two decades of application in conservation. Methods Ecol Evol (2018) 9:21–32. doi: 10.1111/2041-210X.12860
22. Muluken A, Gedefaw A, Alemtsehay M. Assessment of factors associated with breast self-examination among health extension workers in West gojjam zone, Northwest Ethiopia. Int J Breast Cancer (2013) 814395. doi: 10.1155/2013/81439515
23. Tesfay H, Hailemariam B, Desta H, Haftu B. Knowledge of breast cancer and its early detection measures among female students in mekelle university, tigray region, Ethiopia. Sci J Clin Med (2014) 3(4):57–64. doi: 10.11648/j.sjcm.20140304.11
24. Rizwan A, Saleem Z, Sadeeqa S. Effect of family income on knowledge, attitude and practices regarding breast cancer and its screening methods amongst women of Lahore, Pakistan. J Appl Pharm Science (2017) 7(08):028–33. doi: 10.7324/JAPS.2017.70805
25. Tavafian SS, Hasani L, Aghamolaei T, Zare S, Gregory D. Prediction of breast self- examination in a sample of Iranian women an application of the Health belief model: BMC womens health. (2009).
26. Fatma YMZ, Ahmed AT, Tahani RH, Fayek S. El-KFemales' knowledge attitude and practices about breast self-examination (BSE) and risk f actors of breast cancer at Benghazi- Libya (2013) (Accessed April 28/2017).
27. Sami AR, Kurubaran G, Aied MA, Mohd RAM, Sharea I, Saba K. Exploration of barriers to breast-self examination among urban women in shah alam, Malaysia. Asian Pacific J Cancer Prev (2012) 13:1627–32. doi: 10.7314/APJCP.2012.13.4.1627
28. Mukupo FC, Mubita-Ngoma CA. Breast cancer knowledge and breast self-examination practice among rural and urban women in Zambia. Afr J Nurs midwifery (2007) 9(1):50–8.
29. Anantha LSDK, Surendranath B, Vani MK. Awareness and practice of breast self- examination among women in south India. Inernational J Curr Microbiol Appl Sci (2014) 3(1):391–4.
30. Oladimeji KE, Tsoka-Gwegweni JM, Igbodekwe FC, Twomey M, Akolo C, Balarabe HS. 2015, knowledge and beliefs of breast self-examination and breast cancer among market women in ibadan, south West, Nigeria. PLoS ONE (2015) 10(11):e0140904. doi: 10.1371/journal.pone.0140904
Keywords: reproductive age group, breast self-examination, breast cancer screening, Ethiopia, gurage zone
Citation: Hussen A, Kumbi M, Bedewi J, Lette A and Nuriye S (2023) Breast self-examination practice and associated factors among women of reproductive age in southeast Ethiopia. Front. Oncol. 13:1176022. doi: 10.3389/fonc.2023.1176022
Received: 28 February 2023; Accepted: 23 May 2023;
Published: 08 June 2023.
Edited by:
Brijesh Sathian, Hamad Medical Corporation, QatarReviewed by:
Ranjit Kumar Dehury, University of Hyderabad, IndiaRedhwan Ahmed Al-Naggar, National University of Malaysia, Malaysia
Copyright © 2023 Hussen, Kumbi, Bedewi, Lette and Nuriye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jemal Bedewi, amVtYWxiZWRld2lAZ21haWwuY29t
 Abduljewad Hussen1
Abduljewad Hussen1 Jemal Bedewi
Jemal Bedewi