
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol., 03 May 2023
Sec. Skin Cancer
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.1174542
 Alina Miriam Mueller1,2
Alina Miriam Mueller1,2 Elisabeth Victoria Goessinger1,2
Elisabeth Victoria Goessinger1,2 Sara Elisa Cerminara1,2
Sara Elisa Cerminara1,2 Lisa Kostner1,2
Lisa Kostner1,2 Margarida Amaral1
Margarida Amaral1 Stephanie Marie Huber1
Stephanie Marie Huber1 Lea Pauline Passweg2
Lea Pauline Passweg2 Laura Garcia Moreno2
Laura Garcia Moreno2 Daniel Bodenmann2
Daniel Bodenmann2 Michael Kunz1
Michael Kunz1 Mitchell Paul Levesque3,4
Mitchell Paul Levesque3,4 Julia-Tatjana Maul3,4
Julia-Tatjana Maul3,4 Phil Fang Cheng3
Phil Fang Cheng3 Alexander Andreas Navarini1,2
Alexander Andreas Navarini1,2 Lara Valeska Maul1,2*
Lara Valeska Maul1,2*Introduction: The worldwide incidence of melanoma has been increasing rapidly in recent decades with Switzerland having one of the highest rates in Europe. Ultraviolet (UV) radiation is one of the main risk factors for skin cancer. Our objective was to investigate UV protective behavior and melanoma awareness in a high-risk cohort for melanoma.
Methods: In this prospective monocentric study, we assessed general melanoma awareness and UV protection habits in at-risk patients (≥100 nevi, ≥5 dysplastic nevi, known CDKN2A mutation, and/or positive family history) and melanoma patients using questionnaires.
Results: Between 01/2021 and 03/ 2022, a total of 269 patients (53.5% at-risk patients, 46.5% melanoma patients) were included. We observed a significant trend toward using a higher sun protection factor (SPF) in melanoma patients compared with at-risk patients (SPF 50+: 48% [n=60] vs. 26% [n=37]; p=0.0016). Those with a college or university degree used a high SPF significantly more often than patients with lower education levels (p=0.0007). However, higher educational levels correlated with increased annual sun exposure (p=0.041). Neither a positive family history for melanoma, nor gender or Fitzpatrick skin type influenced sun protection behavior. An age of ≥ 50 years presented as a significant risk factor for melanoma development with an odd’s ratio of 2.32. Study participation resulted in improved sun protection behavior with 51% reporting more frequent sunscreen use after study inclusion.
Discussion: UV protection remains a critical factor in melanoma prevention. We suggest that melanoma awareness should continue to be raised through public skin cancer prevention campaigns with a particular focus on individuals with low levels of education.
Worldwide, the incidence and mortality of melanoma have increased over the last decades (1). In 2020, more than 320,000 melanomas were diagnosed and about 57,000 people died from melanoma (2). Switzerland has one of the highest melanoma incidences in Europe (3). An increased exposure to ultraviolet (UV) radiation due to lifestyle changes has been recognized as a relevant factor for these trends. Besides the number of melanocytic nevi, a positive family history for melanoma and a genetic predisposition, excessive sun exposure with sunburns and the use of sunbeds significantly increases the risk of developing cutaneous melanoma (4, 5). UV radiation is thought to be responsible for 60-70% of the melanoma cases (6, 7). Both UVA (320-400 nm) and UVB (280-320 nm) play a role in photocarcinogenesis by causing direct and/or indirect DNA damage (7–10). Previous sunscreens were developed to protect against UVB, with novel products additionally incorporating UVA spectrum wavelengths (11).
Since these risk factors can be modified by sun-protective behavior, there are numerous campaigns to raise awareness among the public (12–15). Limited sun exposure during peak hours, staying in the shade, sunscreen use, wearing protective clothing and avoiding sunbeds are recommended (16). Despite these efforts, sun-protective measures are still not practiced enough in the general population and even melanoma-survivors seem to display suboptimal UV protection behavior (17, 18) despite their increased risk of developing a second melanoma or nonmelanoma skin cancer (19, 20). Skin cancer awareness seems to be linked to gender (21, 22), socio-economic class, education level (21, 23, 24) and family history of skin cancer (24).
The aim of this study was to investigate the awareness of the potential risk of UV radiation and the role of protective measures in a high-risk population for melanoma in Switzerland. We intended to identify typical characteristics that distinguish UV protective behavior in high-risk patients for melanoma that might help to further raise melanoma and sun protection awareness.
This prospective monocentric study was conducted at the Department of Dermatology of the University Hospital in Basel, Switzerland between January 2021 and March 2022. While comparing 2D- and 3D-imaging with deep-learning based risk assessments and routine skin cancer screenings conducted by dermatologists for early detection of melanoma, we assessed general melanoma awareness and UV protection habits in high-risk patients for melanoma and melanoma patients using newly created questionnaires. Patients with ≥ 100 nevi, ≥ 5 atypical nevi, a diagnosis of dysplastic nevus syndrome or a known CDKN2A mutation or a positive family history for melanoma were included in this high-risk group whereas the other group consisted of patients who had a prior diagnosis of melanoma. This division was chosen because of previously described differences in sun-protective behaviors after a melanoma diagnosis (25). Participants were recruited from ongoing consultations at our Department of Dermatology as well as referred by external primary care physicians and dermatologists. Melanoma staging was based on the 8th edition of the American Joint Committee on Cancer’s (AJCC) Cancer Staging Manual (26). Exclusion criteria were Fitzpatrick skin type IV-VI due to the current lack of compatible artificial intelligence (AI)-based risk assessment algorithm for these skin types, acute psychiatric illness, acute crisis or lack of informed consent for study participation. Written informed consent was obtained from all participants.
Based on literature research, we generated a new questionnaire consisting of 8 questions about habits regarding annual sun exposure, use of sunscreen, outdoor hobbies and sunbed use as well as the number of blistering sunburns during childhood and/or adulthood (Supplemental Material 1), and additionally sociodemographic data. All participants completed the survey after the standard skin cancer screening by a dermatologist and the additional 2D and 3D total body photography and AI-based risk assessments. According to the standard recommendations in skin cancer screenings, we encouraged all participants to use adequate UV protection with SPF 50+. During the 6-month and 1-year follow-up visits, participants were asked about any changes in the frequency of sunscreen application and sun protection factor (SPF). An SPF of 6-10 or 15-25 was defined as “low SPF” and 30-50 or 50+ as “high SPF”. The questionnaire consisted of multiple-choice questions with three to seven response options and binary questions (yes/no). All answers were optional.
Data was analyzed using GraphPad Prism Version 9 (Graphpad Software, Inc) and RStudio (RStudio PBC). Two-sided Fisher’s exact test and chi2 test were used to determine associations between categorical variables. Multiple logistic regression was used to analyze the relationship between various independent variables and the occurrence of melanoma. Statistical significance was determined at an alpha level of 0.05. Missing values were listed as “unknown” in the demographics.
The study was approved by the local ethics committee (22020-02482) and registered with ClinicalTrials.gov (NCT04605822). It was conducted in compliance with the Declaration of Helsinki and Good Clinical Practice rules.
A total of 269 participants were included, of which 144 were at-risk patients and 125 were melanoma patients (Table 1). The mean age of the participants was 53.9 (+/- 14.2) years with the at-risk group being slightly younger than the melanoma group (50.9 +/- 14.5 vs. 57.3 +/- 13 years). There was an even gender distribution (52% male, 48% female). Most patients had Fitzpatrick skin type II, followed by III and I. In total, around 40% of the participants had a university degree and around 29% of both groups had a college degree. About one third of the participants (29.7%) went to secondary school or did an apprenticeship (23.6% of the at-risk patients and 36.8% of the melanoma patients). With around 50% of the cases, the most common melanoma type was superficial spreading melanoma (Supplemental Material 2). Melanomas on the lower extremities were most common in our population (n = 33, 26%), followed by the trunk, back and upper extremities. Most patients (44%) suspected the suspicious skin lesion themselves which has led to a medical consultation and diagnosis of a melanoma. In 32% of the cases, the presumptive diagnosis was made by a dermatologist.
Regarding the amount of UV exposure, sunburns, and UV protection measures, we observed that more than half of the patients (56%) reported blistering sunburns as a child whereas the majority of the participants (68%) never had blistering sunburns in adulthood (Supplemental Material 3). Around 27% of the melanoma patients and 32% of the at-risk patients reported using indoor tanning devices. In total, more than 90% of the participants reported applying sunscreen with a SPF of 30 or higher (Supplemental Material 3). We detected a significant trend for melanoma patients to use a higher SPF than at-risk patients (Figure 1; (SPF 50+: 48% vs. 26%, χ2 = 15.33, df = 3, p = 0.0016).
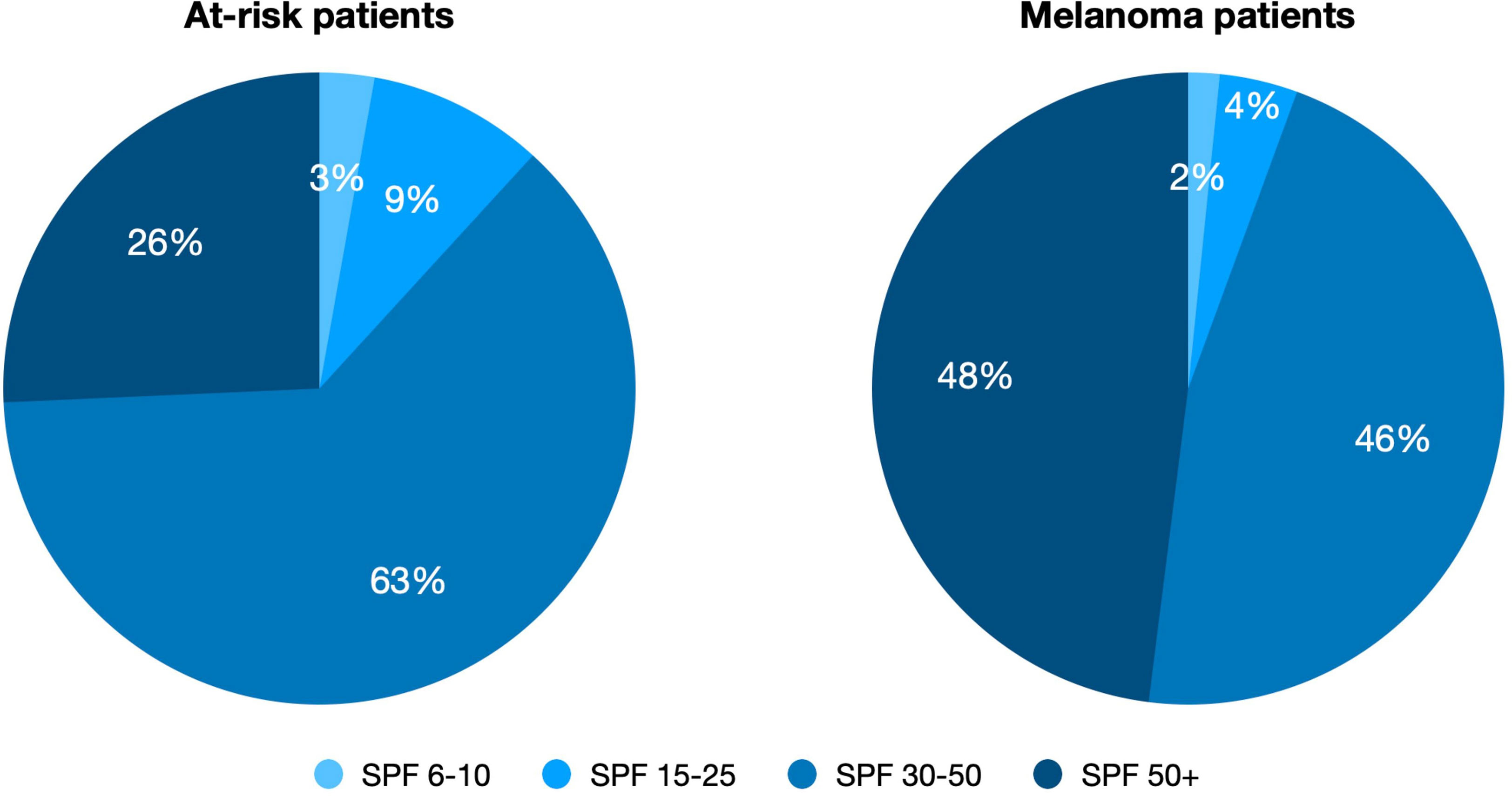
Figure 1 SPF use of at-risk patients vs. melanoma patients. Significant trend for melanoma patients to use higher SPF than at-risk patients (SPF 50+: 48% [n = 60] vs. 26% [n = 37], χ2 = 15.33, df = 3, p = 0.0016). SPF is color-coded.
By investigating a possible association between education level and sun protection habits, we observed that patients who had attended college or university were significantly more likely to use a high SPF than those who only attended secondary school or did an apprenticeship (Figure 2A, OR 4.54; 95% CI 1.92-10.83; p = 0.0007). An opposite observation was found for annual sun exposure: Subjects with a higher education level spent significantly more time in the sun than those with a lower level (Figure 2B, OR 2.23, 95% CI 1.07-4.89; p = 0.041). We also performed a sub-analysis for the at-risk and melanoma patients (Figures 2C, D).

Figure 2 (A) Correlation of education level and choice of SPF. OR 4.54; 95% CI 1.92-10.83; p = 0.0007; (B) Correlation of education level and sun exposure per year. OR 2.23, 95% CI 1.07-4.89; p = 0.041. (C) Correlation of education level and choice of SPF with comparison of the at-risk cohort and melanoma patients. At-risk patients: p = 0.007; melanoma patients: p = 0.011. (D) Correlation of education level and sun exposure per year with comparison of the at-risk cohort and melanoma patients. at-risk patients: p = 0.2; melanoma patients: p = 0.059. Low SPF = 6-10 or 15-25, High SPF = 30-50 or 50+. Light blue = secondary school or apprenticeship, dark blue = college or university.
Further, we detected a difference regarding different age groups and their yearly amount of sun exposure (Figure 3). Significantly more participants over the age of 40 years reported spending more than 5 weeks per year in the sun compared to the younger participants (Figure 3, OR 4.17, 95% CI 1.34-13.24; p = 0.0136). There was no statistically significant difference between different age groups and their choice of SPF.
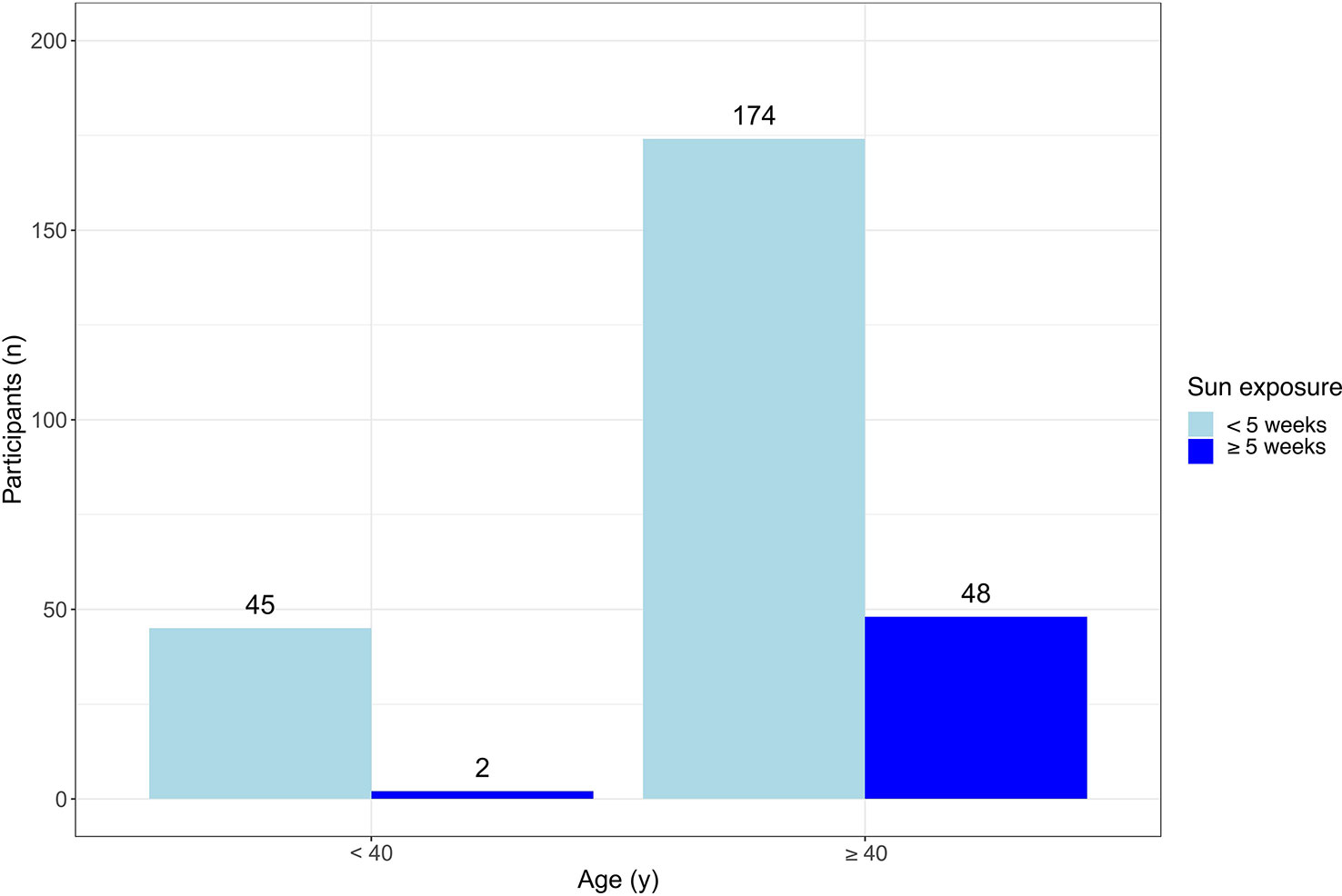
Figure 3 Correlation of age and sun exposure per year. Significantly more participants ≥ 40 years had a sun exposure of ≥ 5 weeks per year (OR 4.17, 95% CI 1.34-13.24; p = 0.0136). Light blue = sun exposure of not more than 5 weeks per year, dark blue = sun exposure of more than 5 weeks per year. OR 4.17, 95% CI 1.34-13.24; p = 0.0136.
Neither a positive family history for melanoma nor gender, Fitzpatrick skin type, melanoma subtype or stage nor the anatomic location of the melanoma on the body influenced sun protection behavior in terms of SPF used or amount of sun exposure.
At the time of this preliminary data analysis, 59 melanoma patients and 10 at-risk patients had come to their first follow-up visit. Due to the low number of cases, the results of the latter group were excluded from the current data analysis. More than half of the patients of the melanoma follow-up group (51%) reported a more frequent use of sunscreen since study participation (Table 2). Also, the use of sunscreen with the recommended SPF of 50+ increased within this group (Table 2, 47.5% vs. 57.6%).
To determine whether certain characteristics or behaviors were associated with cutaneous melanoma, we analyzed the data from the melanoma patient cohort and calculated the odds ratios for different variables with the endpoint of melanoma (Figure 4). Only an age of ≥ 50 years was significantly associated with an odds ratio of 2.32 (Figure 4, 95% CI 1.34-4.13, p = 0.003). Neither the occurrence of blistering sunburns during childhood or adulthood, nor sex, being exposed to the sun at work or outdoor hobbies such as trekking, skiing, swimming or gardening showed a significant association with melanoma in our cohort.
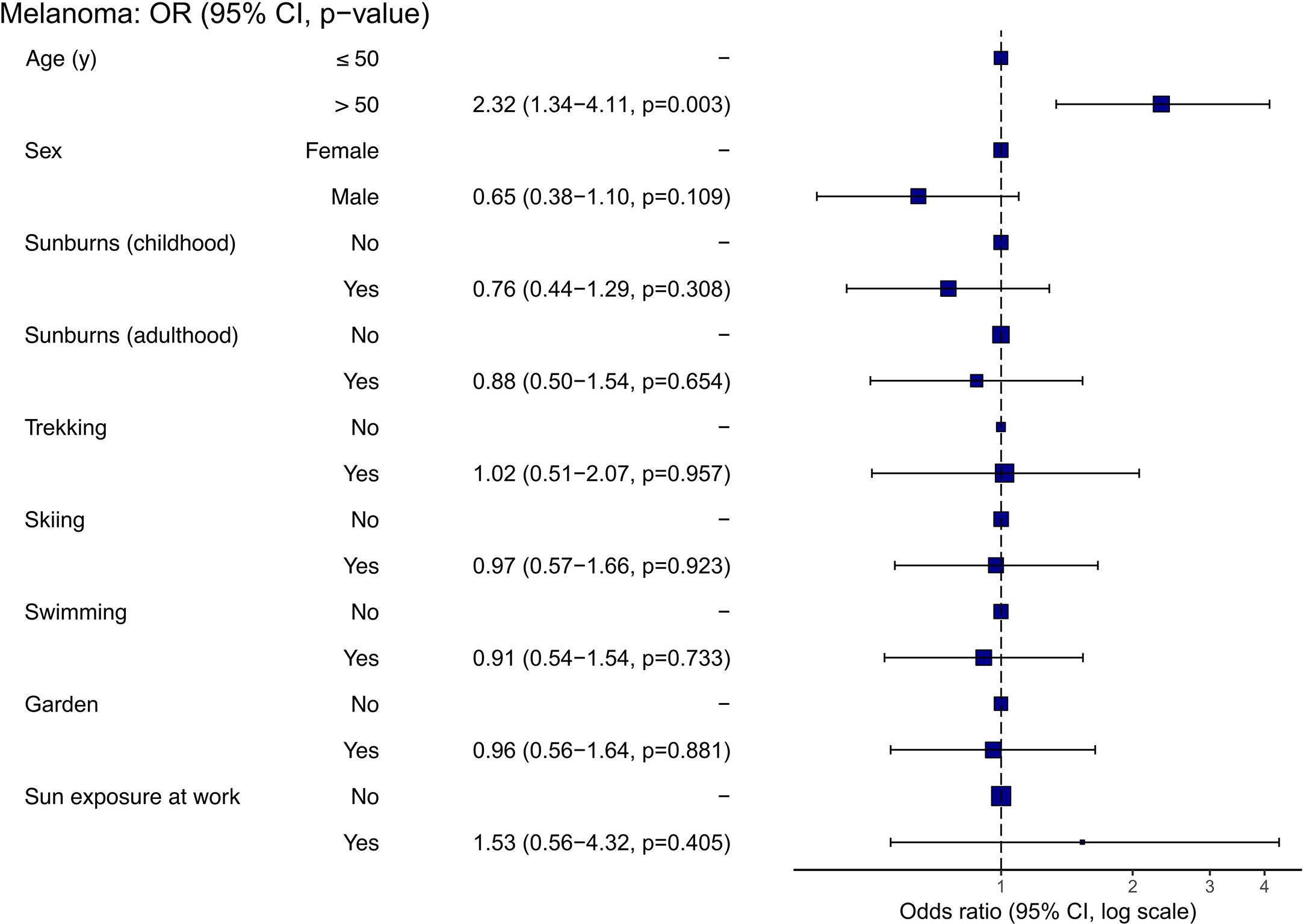
Figure 4 Correlations between demographics and hobbies and melanoma (data derived from melanoma patients, n = 125). An odds ratio close to 1.0 indicates that the odds are the same between the two compared groups.
In this prospective study, we found suboptimal sun protection behavior in both at-risk and melanoma patients. Nevertheless, we observed a trend for melanoma patients to use sunscreen with a higher SPF compared to at-risk patients. Significantly more participants with a high education level used sunscreen with a high SPF (≥ 30) than those with a lower education level, but also reported significantly more sun exposure.
At-risk and melanoma patients did not differ significantly from each other in terms of amount of sun exposure and sunburns in the past. Almost a third of the participants of both groups reported having blistering sunburns as adults despite their higher risk for melanoma occurrence. This is in line with previous studies (27, 28), displaying that a melanoma diagnosis only leads to adjusted risk behaviors in some patients. A Danish group investigated the UV exposure of melanoma patients during the first three summers after diagnosis (29) and found that after the second year, they had even more UV exposure than the healthy control group, suggesting that melanoma patients do not maintain a cautious behavior. Already in 1999, Euromelanoma was created with the aim to encourage all European countries to start skin cancer screening campaigns and to educate the population about preventive measures and treatment options (30). Despite these efforts, we still observe that even high-risk groups do not adequately implement the recommendations and skin cancer incidences continue to increase.
The observed more frequent use of sunscreen with an SPF ≥ 30 among patients with a high education level is in agreement with previously published data (21, 23, 24, 27). It could be due to a greater awareness of the possible consequences of melanoma (31) and also affects their children’s behavior (32). The knowledge about skin cancer and sun protection in childhood can already be educated in school (33, 34),
Interestingly, we observed an inverse correlation for annual sun exposure, as patients with higher education levels spent significantly more time in the sun. Researchers found that melanoma rates were 80% higher for young women living in California neighborhoods with the highest socio-economic status and UV exposure compared to the lowest (35) because of different cultural norms and/or more time to tan. Another group also found that knowledge and education level did not automatically lead to a reduction of melanoma-prone behavior, even among healthcare professionals (36). Our finding concerning increased sun exposure in older patients could have similar reasons, as they might have more resources to tan or travel. In addition, melanoma awareness campaigns have only gained momentum in the last 20 years (30), which is why they mainly impact the younger population rather than previously acquired skin damage in the elderly generation (37). We chose an age limit of 40 years for our calculations following a previous publication investigating the sun exposure profile of a French population, although interestingly, they made an opposite observation concerning sun exposure (38). In general, the correlation between age and sun protection behavior remains unclear in the literature (39).
More than one quarter of the study participants reported using sunbeds in the past. Modern sunbeds mainly emit in UVA range with a small fraction (<5%) of UVB. They can emit UV radiation 10-15 times stronger than the midday sunlight on the Mediterranean Sea (5) and are associated with a significant increase in melanoma risk (5). A recent study found that a ban on sunbeds along with a public information campaign could prevent 1206 melanoma cases, 207 melanoma deaths and 3987 non-melanoma skin cancers in the lifetime of all 18-year-olds (n=618 873) living in England in 2019 (40). Since the risk increases especially when the initial usage happens at a young age (5), Switzerland placed a ban on the use of solariums for minors in 2019 (41). In Australia and Brazil tanning salons are already prohibited completely (40, 42, 43) and recently, German and Swiss cancer leagues have been suggesting a general ban as well (44).
In contrast to previous findings (21, 22, 24, 45), we did not observe a correlation between gender, Fitzpatrick skin type or a positive family history for melanoma and sun protective behavior. We assume that a comparison of our cohorts is generally difficult, since all were patients with an increased melanoma risk who voluntarily participated in the melanoma early detection study and might have had an increased awareness primarily.
The average age of melanoma diagnosis is 57 years (46), consistent with positive correlation of melanoma and the age of ≥ 50 years in our cohort. Surprisingly, sex showed no correlation with melanoma, although according to the literature, men have a 1.5 times higher risk to develop melanoma (47). Interestingly, a history of blistering sunburns was not associated with melanoma in our study population despite data suggesting otherwise (4, 48). Workplace sun exposure also showed no correlation, which is in line with previous findings (49).
Despite observing suboptimal sun protection behavior in both at-risk and melanoma patients (21, 23–25, 27, 29, 45),, we found that compared to the general population (17), our study participants had already better sun protective behaviors before study enrollment. Nevertheless, we demonstrated that verbal education about sun protection during standard skin cancer screening by a dermatologist further improved sunscreen application frequency and SPF. The positive effects of education about sun protection by physicians, especially in high-risk populations, have been observed before (50–52). Therefore, we urge all dermatologists to instruct their patients on adequate UV protection with SPF 50+, avoidance of midday sun and wearing UV protective clothing.
The strengths of this study are a big sample size, a prospective study design in one of the European countries with the highest melanoma incidence as well as two comparative arms.
However, due to some limitations the generalizability of the results should be considered with caution. Since the questionnaires were not collected anonymously, it cannot be excluded that patients intended their answers to meet the expectations of the investigator, leading to a possible bias. Further, we were not able to obtain all the cancer characteristics due to missing data. This study focused on sun protection behavior in terms of sunscreen use. Other recommended prevention methods such as wearing protective clothing or limiting sun exposure during peak hours or staying in the shade (16) were not addressed. As only 10 participants in the at-risk group had completed their follow-up visits, they were excluded from the subanalysis concerning potential change of sun protective behavior since study participation. We plan to compare the two cohorts in this regard in a subsequent analysis after completion of the ongoing three-year prospective study. Also, future studies focusing on differences in serum vitamin D levels and oral vitamin D supplementation among different melanoma risk groups are of great interest.
UV protection remains one of the crucial factors in primary melanoma prevention. With Switzerland reporting among the highest incidence rates for melanoma in Europe, we strongly suggest to further raise melanoma awareness in public skin cancer prevention campaigns with a focus on individuals with low education levels. We propose to address the latter through campaigns on television and radio as target-oriented and promising media for this population. In addition, we suggest integrating the topic into the curriculum of schools. Further, we urge all dermatologists to instruct their patients at every examination on adequate UV protection with SPF 50+, avoidance of midday sun and wearing UV protective clothing.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The study was approved by the local ethics committee (22020- 02482) and registered with ClinicalTrials.gov (NCT04605822). The patients/participants provided their written informed consent to participate in this study.
Conceptualization, LM and AM; Data curation, AM, EG, SC, LK, MA, SH, MK, LP, LG, DB, and LM; Formal analysis, AM, PC, and LM; Investigation, AM, EG, SC, LK, MA, SH, MK, and LM; Methodology, LM, J-TM, and PC; Resources, LM and AN; Writing—original draft preparation, AM and LM; Writing—review and editing, AM, EG, SC, LK, MA, SH, LP, LG, DB, MK, ML, J-TM, PC, AN, and LM; Visualization, AM, PC, and LM; Supervision, LM; Project administration, LM; Funding acquisition, LM and AN. All authors contributed to the article and approved the submitted version.
This research project was fully funded by the Department of Dermatology, as well as to a minor part by the Research Foundation for Young Researchers Grant of the University of Basel, Switzerland and by the Voluntary Academic Society Grant, Basel, Switzerland.
Special thanks go to all participants who voluntarily participated in this study and made successful implementation of this study possible. LM gratefully acknowledges support from the Research Foundation for Young Researchers Grant of the University of Basel, Switzerland and from the Voluntary Academic Society Grant, Basel, Switzerland.
AM has received support for conference attendance from ALK, Bencard and Galderma. LK has received speaking fees in a presentation sponsored by Boehringer Ingelheim. ML has project-specific research funding from Roche, Novartis, Molecular Partners, and Oncobit AG and has received speaking fees from Danaher. J-TM is and has served as advisor and/or received speaking fees and/ or participated in clinical trials sponsored by AbbVie, Almirall, Amgen, BMS, Celgene, Eli Lilly, LEO Pharma, Janssen-Cilag, MSD, Novartis, Pfizer, Pierre Fabre, Roche, Sanofi, UCB. AN declares being a consultant and advisor and/or receiving speaking fees and/or grants and/or served as an investigator in clinical trials for AbbVie, Almirall, Amgen, Biomed, Bristol Myers Squibb, Boehringer Ingelheim, Celgene, Eli Lilly, Galderma, GlaxoSmithKline, LEO Pharma, Janssen-Cilag, MSD, Novartis, Pfizer, Pierre Fabre Pharma, Regeneron, Sandoz, Sanofi, and UCB. LM has served as advisor and/or received speaking fees and/or participated in clinical trials sponsored by Almirall, Amgen, BMS, Celgene, Eli Lilly, MSD, Novartis, Pierre Fabre, Roche and Sanofi.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2023.1174542/full#supplementary-material
1. Garbe C, Keim U, Gandini S, Amaral T, Katalinic A, Hollezcek B, et al. Epidemiology of cutaneous melanoma and keratinocyte cancer in white populations 1943-2036. Eur J Cancer (2021) 152:18–25. doi: 10.1016/j.ejca.2021.04.029
2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2021) 71(3):209–49. doi: 10.3322/caac.21660
3. Forsea AM, Del Marmol V, de Vries E, Bailey EE, Geller AC. Melanoma incidence and mortality in Europe: new estimates, persistent disparities. Br J Dermatol (2012) 167(5):1124–30. doi: 10.1111/j.1365-2133.2012.11125.x
4. Gandini S, Sera F, Cattaruzza MS, Pasquini P, Picconi O, Boyle P, et al. Meta-analysis of risk factors for cutaneous melanoma: II. sun exposure. Eur J Cancer (2005) 41(1):45–60. doi: 10.1016/j.ejca.2004.10.016
5. Boniol M, Autier P, Boyle P, Gandini S. Cutaneous melanoma attributable to sunbed use: systematic review and meta-analysis. Bmj (2012) 345:e4757. doi: 10.1136/bmj.e4757
6. Diepgen TL, Mahler V. The epidemiology of skin cancer. Br J Dermatol (2002) 146 Suppl 61:1–6. doi: 10.1046/j.1365-2133.146.s61.2.x
7. Kozma B, Eide MJ. Photocarcinogenesis: an epidemiologic perspective on ultraviolet light and skin cancer. Dermatol Clin (2014) 32(3):301–13, viii. doi: 10.1016/j.det.2014.03.004
8. Jin S-G, Padron F, Pfeifer GP. UVA Radiation, DNA damage, and melanoma. ACS Omega (2022) 7(37):32936–48. doi: 10.1021/acsomega.2c04424
9. Pfeifer GP. Mechanisms of UV-induced mutations and skin cancer. Genome Instab Dis (2020) 1(3):99–113. doi: 10.1007/s42764-020-00009-8
10. Sample A, He YY. Mechanisms and prevention of UV-induced melanoma. Photodermatol Photoimmunol Photomed (2018) 34(1):13–24. doi: 10.1111/phpp.12329
11. Serpone N. Sunscreens and their usefulness: have we made any progress in the last two decades? Photochem Photobiol Sci (2021) 20(2):189–244. doi: 10.1007/s43630-021-00013-1
12. Marks R. Two decades of the public health approach to skin cancer control in Australia: why, how and where are we now? Australas J Dermatol (1999) 40(1):1–5. doi: 10.1046/j.1440-0960.1999.00307.x
13. Youl PH, Youlden DR, Baade PD. Changes in the site distribution of common melanoma subtypes in Queensland, Australia over time: implications for public health campaigns. Br J Dermatol (2013) 168(1):136–44. doi: 10.1111/j.1365-2133.2012.11064.x
14. Seidenari S, Benati E, Ponti G, Borsari S, Ferrari C, Albertini G, et al. Italian Euromelanoma day screening campaign (2005-2007) and the planning of melanoma screening strategies. Eur J Cancer Prev (2012) 21(1):89–95. doi: 10.1097/CEJ.0b013e3283498e14
15. van der Leest RJ, de Vries E, Bulliard JL, Paoli J, Peris K, Stratigos AJ, et al. The euromelanoma skin cancer prevention campaign in Europe: characteristics and results of 2009 and 2010. J Eur Acad Dermatol Venereol (2011) 25(12):1455–65. doi: 10.1111/j.1468-3083.2011.04228.x
17. Vogel RI, Strayer LG, Engelman L, Nelson HH, Blaes AH, Anderson KE, et al. Sun exposure and protection behaviors among long-term melanoma survivors and population controls. Cancer Epidemiol Biomarkers Prev (2017) 26(4):607–13. doi: 10.1158/1055-9965.EPI-16-0854
18. Nahar VK, Allison Ford M, Brodell RT, Boyas JF, Jacks SK, Biviji-Sharma R, et al. Skin cancer prevention practices among malignant melanoma survivors: a systematic review. J Cancer Res Clin Oncol (2016) 142(6):1273–83. doi: 10.1007/s00432-015-2086-z
19. Caini S, Boniol M, Botteri E, Tosti G, Bazolli B, Russell-Edu W, et al. The risk of developing a second primary cancer in melanoma patients: a comprehensive review of the literature and meta-analysis. J Dermatol Sci (2014) 75(1):3–9. doi: 10.1016/j.jdermsci.2014.02.007
20. Bradford PT, Freedman DM, Goldstein AM, Tucker MA. Increased risk of second primary cancers after a diagnosis of melanoma. Arch Dermatol (2010) 146(3):265–72. doi: 10.1001/archdermatol.2010.2
21. Seité S, Del Marmol V, Moyal D, Friedman AJ. Public primary and secondary skin cancer prevention, perceptions and knowledge: an international cross-sectional survey. J Eur Acad Dermatol Venereol (2017) 31(5):815–20. doi: 10.1111/jdv.14104
22. Manne S, Lessin S. Prevalence and correlates of sun protection and skin self-examination practices among cutaneous malignant melanoma survivors. J Behav Med (2006) 29(5):419–34. doi: 10.1007/s10865-006-9064-5
23. Tas F, Cinar FE, Erturk K. Awareness on malignant melanoma and its prevention measures among Turkish cutaneous malignant melanoma patients: a tertiary cancer center experience. Dermatol Ther (2020) 33(6):e14425. doi: 10.1111/dth.14425
24. Villani A, Fabbrocini G, Costa C, Scalvenzi M. Awareness on sun protection behavior among melanoma and nonmelanoma skin cancer patients: an Italian tertiary cancer center experience. Dermatol Ther (2021) 34(2):e14728. doi: 10.1111/dth.14728
25. Mayer D, Layman A, Carlson J. Sun-protection behaviors of melanoma survivors. J Am Acad Dermatol (2012) 66(1):e9–10. doi: 10.1016/j.jaad.2010.10.002
26. Keung EZ, Gershenwald JE. The eighth edition American Joint Committee on Cancer (AJCC) melanoma staging system: implications for melanoma treatment and care. Expert Rev Anticancer Ther. (2018). 18(8):775–84. doi: 10.1080/14737140.2018.1489246.
27. Heckman CJ, Manne SL, Kashy DA, Bhurosy T, Ritterband L, Coups EJ. Correlates of sun protection behaviors among melanoma survivors. BMC Public Health (2021) 21(1):882. doi: 10.1186/s12889-021-10951-1
28. Patel SP, Chien AL. Sun protective clothing and sun avoidance: the most critical components of photoprotection in patients with melanoma. Dermatol Surg (2021) 47(3):333–7. doi: 10.1097/DSS.0000000000002794
29. Idorn LW, Datta P, Heydenreich J, Philipsen PA, Wulf HC. A 3-year follow-up of sun behavior in patients with cutaneous malignant melanoma. JAMA Dermatol (2014) 150(2):163–8. doi: 10.1001/jamadermatol.2013.5098
30. Del Marmol V. Prevention and screening of melanoma in Europe: 20 years of the euromelanoma campaign. J Eur Acad Dermatol Venereol (2022) 36 Suppl 6:5–11. doi: 10.1111/jdv.18195
31. Sanchez DP, Maymone MBC, McLean EO, Kennedy KF, Sahni D, Secemsky EA, et al. Racial and ethnic disparities in melanoma awareness: a cross-sectional survey. J Am Acad Dermatol (2020) 83(4):1098–103. doi: 10.1016/j.jaad.2020.04.137
32. Reinau D, Meier C, Gerber N, Hofbauer GF, Surber C. Sun protective behaviour of primary and secondary school students in north-Western Switzerland. Swiss Med Wkly (2012) 142:w13520. doi: 10.4414/smw.2012.13520
33. Geller AC, Rutsch L, Kenausis K, Selzer P, Zhang Z. Can an hour or two of sun protection education keep the sunburn away? evaluation of the environmental protection agency’s sunwise school program. Environ Health (2003) 2(1):13. doi: 10.1186/1476-069X-2-13
34. Reinau D, Meier CR, Gerber N, Surber C. Evaluation of a sun safety education programme for primary school students in Switzerland. Eur J Cancer Prev (2014) 23(4):303–9. doi: 10.1097/CEJ.0000000000000040
35. Hausauer AK, Swetter SM, Cockburn MG, Clarke CA. Increases in melanoma among adolescent girls and young women in California: trends by socioeconomic status and UV radiation exposure. Arch Dermatol (2011) 147(7):783–9. doi: 10.1001/archdermatol.2011.44
36. Guile K, Nicholson S. Does knowledge influence melanoma-prone behavior? awareness, exposure, and sun protection among five social groups. Oncol Nurs Forum. (2004) 31(3):641–6. doi: 10.1188/04.ONF.641-646
37. Hajdarevic S, Hvidberg L, Lin Y, Donnelly C, Gavin A, Lagerlund M, et al. Awareness of sunburn in childhood, use of sunbeds and change of moles in Denmark, northern Ireland, Norway and Sweden. Eur J Public Health (2016) 26(1):29–35. doi: 10.1093/eurpub/ckv112
38. Sassolas B, Grange F, Touboul C, Lebbe C, Saiag P, Mortier L, et al. Sun exposure profile in the French population. results of the EDIFICE melanoma survey. J Eur Acad Dermatol Venereol (2015) 29 Suppl 2:6–10. doi: 10.1111/jdv.12895
39. Kasparian NA, McLoone JK, Meiser B. Skin cancer-related prevention and screening behaviors: a review of the literature. J Behav Med (2009) 32(5):406–28. doi: 10.1007/s10865-009-9219-2
40. Eden M, Hainsworth R, Gordon LG, Epton T, Lorigan P, Rhodes LE, et al. Cost-effectiveness of a policy-based intervention to reduce melanoma and other skin cancers associated with indoor tanning. Br J Dermatol (2022) 187(1):105–14. doi: 10.1111/bjd.21046
41. BAG. Solarium (2022). Available at: https://www.bag.admin.ch/bag/de/home/gesund-leben/umwelt-und-gesundheit/strahlung-radioaktivitaet-schall/elektromagnetische-felder-emf-uv-laser-licht/solarium.html.
42. Sinclair C, Cleaves N, Dunstone K, Makin J, Zouzounis S. Impact of an outright ban on the availability of commercial tanning services in Victoria, Australia. Br J Dermatol (2016) 175(2):387–90. doi: 10.1111/bjd.14549
43. Organization WH. Legislation of artificial tanning sunbeds - existence of sunbed regulations . Available at: https://apps.who.int/gho/data/node.main.SUNBEDSEXISTENCE?lang=en.
44. SRF. Deutsche krebshilfe will solariumverbot – und die schweiz? (2020). Available at: https://www.srf.ch/news/schweiz/debatte-neu-entfacht-deutsche-krebshilfe-will-solariumverbot-und-die-schweiz.
45. Karlsson O, Hagberg O, Nielsen K, Paoli J, Ingvar Å. Difference in sun exposure habits between individuals with high and low risk of skin cancer. Dermatol Pract Concept (2021) 11(4):e2021090. doi: 10.5826/dpc.1104a90
46. Rastrelli M, Tropea S, Rossi CR, Alaibac M. Melanoma: epidemiology, risk factors, pathogenesis, diagnosis and classification. In Vivo (2014) 28(6):1005–11.
47. Markovic SN, Erickson LA, Rao RD, Weenig RH, Pockaj BA, Bardia A, et al. Malignant melanoma in the 21st century, part 1: epidemiology, risk factors, screening, prevention, and diagnosis. Mayo Clin Proc (2007) 82(3):364–80. doi: 10.1016/S0025-6196(11)61033-1
48. Wu S, Cho E, Li WQ, Weinstock MA, Han J, Qureshi AA. History of severe sunburn and risk of skin cancer among women and men in 2 prospective cohort studies. Am J Epidemiol (2016) 183(9):824–33. doi: 10.1093/aje/kwv282
49. Modenese A, Korpinen L, Gobba F. Solar radiation exposure and outdoor work: an underestimated occupational risk. Int J Environ Res Public Health (2018) 15(10):2063. doi: 10.3390/ijerph15102063
50. Freiman A, Yu J, Loutfi A, Wang B. Impact of melanoma diagnosis on sun-awareness and protection: efficacy of education campaigns in a high-risk population. J Cutan Med Surg (2004) 8(5):303–9. doi: 10.1177/120347540400800501
51. Robinson JK. Behavior modification obtained by sun protection education coupled with removal of a skin cancer. Arch Dermatol (1990) 126(4):477–81. doi: 10.1001/archderm.1990.01670280061010
Keywords: melanoma, awareness, prevention, sunscreen, education
Citation: Mueller AM, Goessinger EV, Cerminara SE, Kostner L, Amaral M, Huber SM, Passweg LP, Moreno LG, Bodenmann D, Kunz M, Levesque MP, Maul J-T, Cheng PF, Navarini AA and Maul LV (2023) Educational level-dependent melanoma awareness in a high-risk population in Switzerland. Front. Oncol. 13:1174542. doi: 10.3389/fonc.2023.1174542
Received: 26 February 2023; Accepted: 13 April 2023;
Published: 03 May 2023.
Edited by:
Giuseppe Palmieri, University of Sassari, ItalyReviewed by:
Reto Huggenberger, AstraZeneca, United KingdomCopyright © 2023 Mueller, Goessinger, Cerminara, Kostner, Amaral, Huber, Passweg, Moreno, Bodenmann, Kunz, Levesque, Maul, Cheng, Navarini and Maul. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lara Valeska Maul, bGFyYXZhbGVza2EubWF1bEB1c2IuY2g=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.