- 1Department of Public Health, University of Medicine and Pharmacy Carol Davila, Bucharest, Romania
- 2Ovidius Clinical Hospital, Constanta, Romania
- 3Department of Surgery, Ovidius Clinical Hospital, Constanta, Romania
- 4Faculty of Medicine, Ovidius University, Constanta, Romania
- 5Department of Imagistic, Ovidius Clinical Hospital, Constanta, Romania
- 6Department of Pharmacoeconomics, University of Medicine and Pharmacy, Craiova, Romania
- 7Department of Oncology, Ovidius Clinical Hospital, Constanta, Romania
Introduction: Digital health services and technology are rapidly developing following the COVID-19 pandemic. This study aimed to reveal the differences between users of digital health technology (DHT) and the general population with regard to cancer prevention.
Materials and Methods: This was an observational study on a conventional sample of 270 DHT users with completed data, performed in September 2021.
Results: A significant difference was observed in the proportion of DHT users and the general population reporting the screening test results, which was 2–6 times higher in the DHT group. Digital technologies applied to the “self-care” model were more suitable for internet-literate populations.
Discussion: Including digital technologies in a self-care model may be more suitable for internet-literate individuals. Thus, in a preventative health organizational framework, DHT should be integrated and used at the primary care level in the general population to improve disparities in the preventative health domain.
1 Introduction
Digital healthcare refers to technologies and services that use digital information and communication tools to improve the prevention, diagnosis, treatment, monitoring, and management of health-related issues and monitor and manage lifestyle habits that affect health. Digital health technologies (DHT) for preventive healthcare include wearables, sensors, telemedicine tools, and software applications that can evaluate health risks based on questionnaires and measurements. They can also recommend healthy lifestyle habits, record targeted health measurements (such as weight, glycemia, and cholesterol), and perform screening tests (1, 2).
As the COVID pandemic spread, several individuals chose online health services owing to fear of infection from traditional healthcare settings and convenience as these new technologies have recently become widely available. Consequently, we have witnessed a major rise in the development of digital technologies in the last few years and an increase in healthcare delivery through online settings (3). However, the literature on the topic is scarce, sparse, and immature, and knowledge is building up (4).
However, the rapid pace of development and adoption generates skepticism from the government, policymakers, and health system managers regarding the impact of digital self-care information and services on quality, safety, cost, and inequalities. For example, these services may be able to address some inequalities regarding access to health services. However, they may create other inequalities, such as disparities in the resources or skills needed to take advantage of these new technologies (5–7).
In oncology, applications are included in current recommended therapies (8). Nevertheless, health prevention is essential, and the studies exploring the DHT, particularly telephone reminders or messages, for cancer screening participation found that they do have effect (9, 10). Further research is needed to reveal also the effects on education and other aspects taken into consideration by different stakeholders. In this study, we aimed to build knowledge regarding DHT use for cancer prevention with a view on possible disparities.
The study’s objective was to compare the user profiles and the proportion of cancer preventive measures reported by DHT users using data from the general population in Romania.
2 Materials and methods
This was an observational descriptive study on a conventional sample of users of a DHT application, Alprevia© (Panmedica, Romania), over one month (September) in 2021, defined as the “DHT sample.” The application estimates risk, collects previous screening data, and recommends examinations, tests, consultations, and lifestyle changes for cardiovascular diseases, cancer, diabetes, and depression. The application collects no personal identification data.
The indicator used for comparison was: Proportion of women/men (aged “x -y”) reporting the test “z” in the past years: “z” is the recommended test (such as mammography and colonoscopy), and “x-y” is the age interval for that test according to the disease-specific guidelines.
The target age groups for specific screening and appropriate screening tests were considered based on European cancer screening/detection guides, as follows:
2.1 Women
a) Cervical cancer:
- Pap screening: 20–69 years, (11)
- HPV-DNA screening: 30–69 years, (11)
b) Breast cancer:
- Mammogram: 50–69 years, (10)
- Clinical examination of the breast: 50–69 years, (12)
- Breast ultrasound: 50–69 years, (10)
- Breast self-examination education: 50–69 years, (12)
c) Colorectal cancer
- Colonoscopy: 50–74 years, (11)
- Fecal occult blood test (FOBT): 50–74 years, (13)
- Fecal immunochemical test (FIT): 50–74 years (13).
2.2 Men
a) Prostate cancer:
- Prostate-specific antigen (PSA) screening: 55–69 years (14),
- Clinical examination of the prostate: 55–69 years (14),
b) Colorectal cancer
- Colonoscopy: 50–74 years (13),
- FOBT: 50–74 years (13),
- FIT: 50–74 years (13).
The application (for September) recorded the data of 270 participants (men and women) who had assessed their cancer risk. Access was free, with no username, password, or registration required. The general population was invited to use the application through web and Facebook advertisements. No specific groups were invited. We analyzed 261 applications with complete data and calculated the percentage of individuals within the target group that used each screening method.
Descriptive analysis was performed using GraphPad Prism 9.4.1. (GraphPad Software, San Diego, CA, USA). Chi-square or Fisher’s exact two-sided test was used in contingency analysis, with statistical significance defined as p <0.05.
3 Results
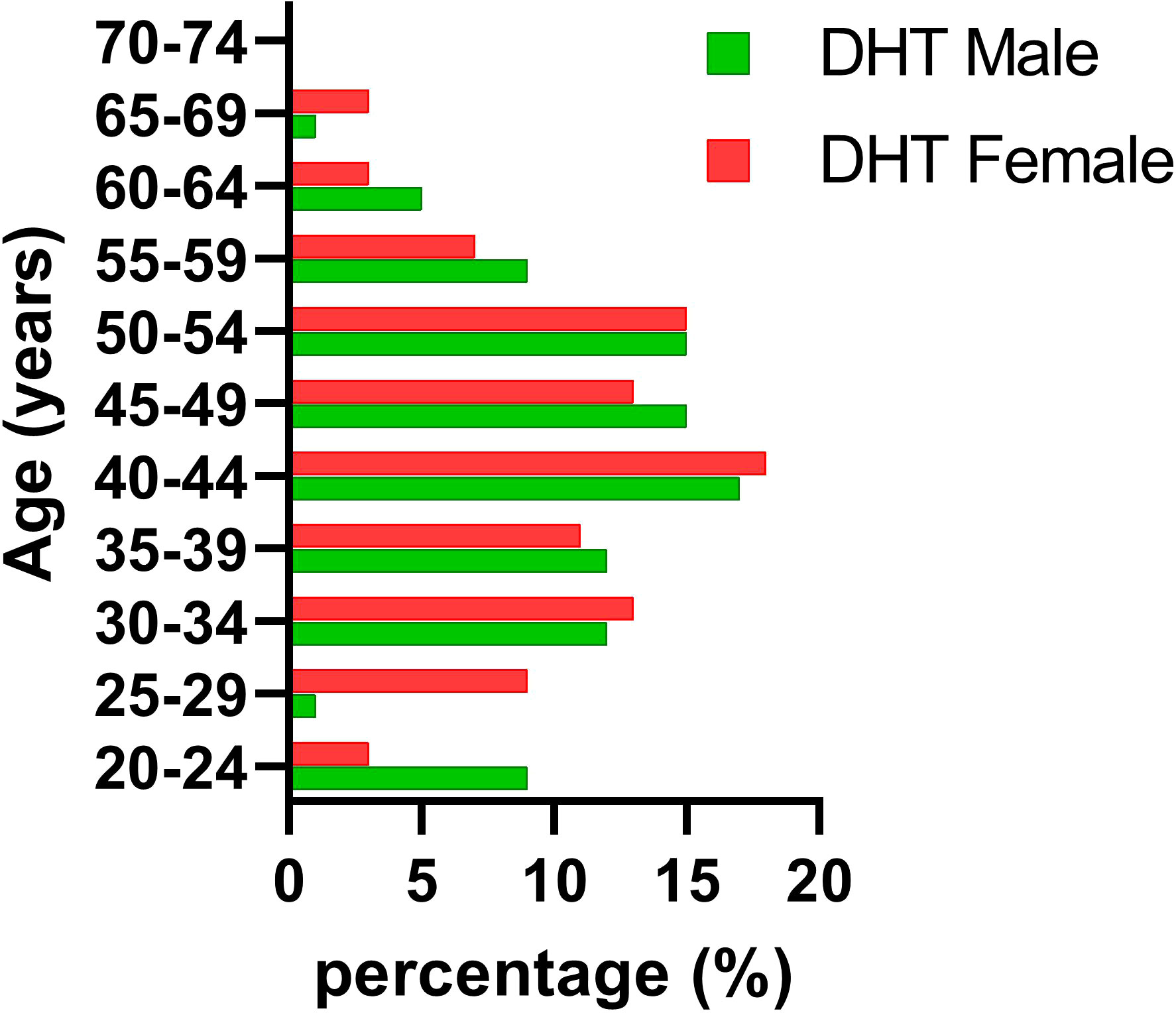
The DHT conventional sample had the following sex distribution: 28% men and 72% women. Approximately 97% of the group were aged 20–69, and 70% were 35–54 years old. The average age was 43, with a Gaussian distribution of 19–71 years.
The DHT conventional sample differed from the general population, with statistically significant differences in the 25–29 and 65–74 age groups, as presented in Table 1.
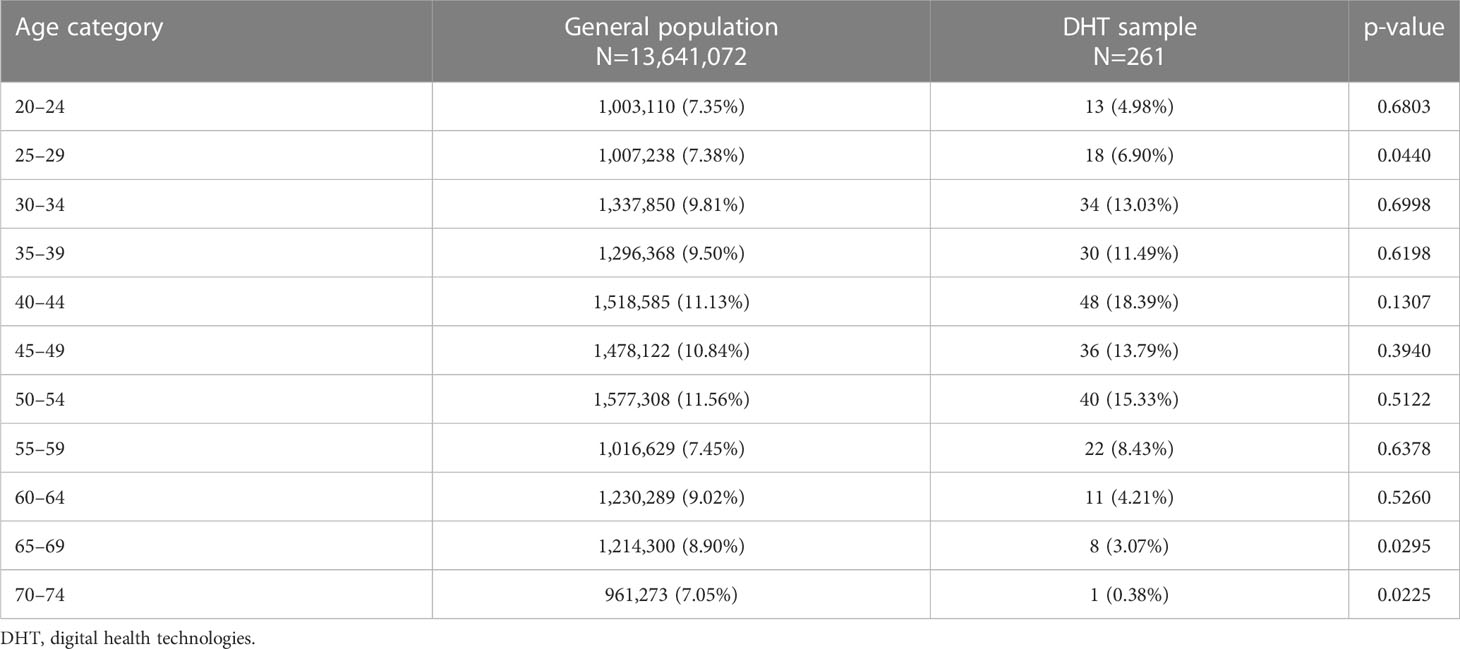
Table 1 Age distribution categories and statistical differences in the general population and DHT sample.
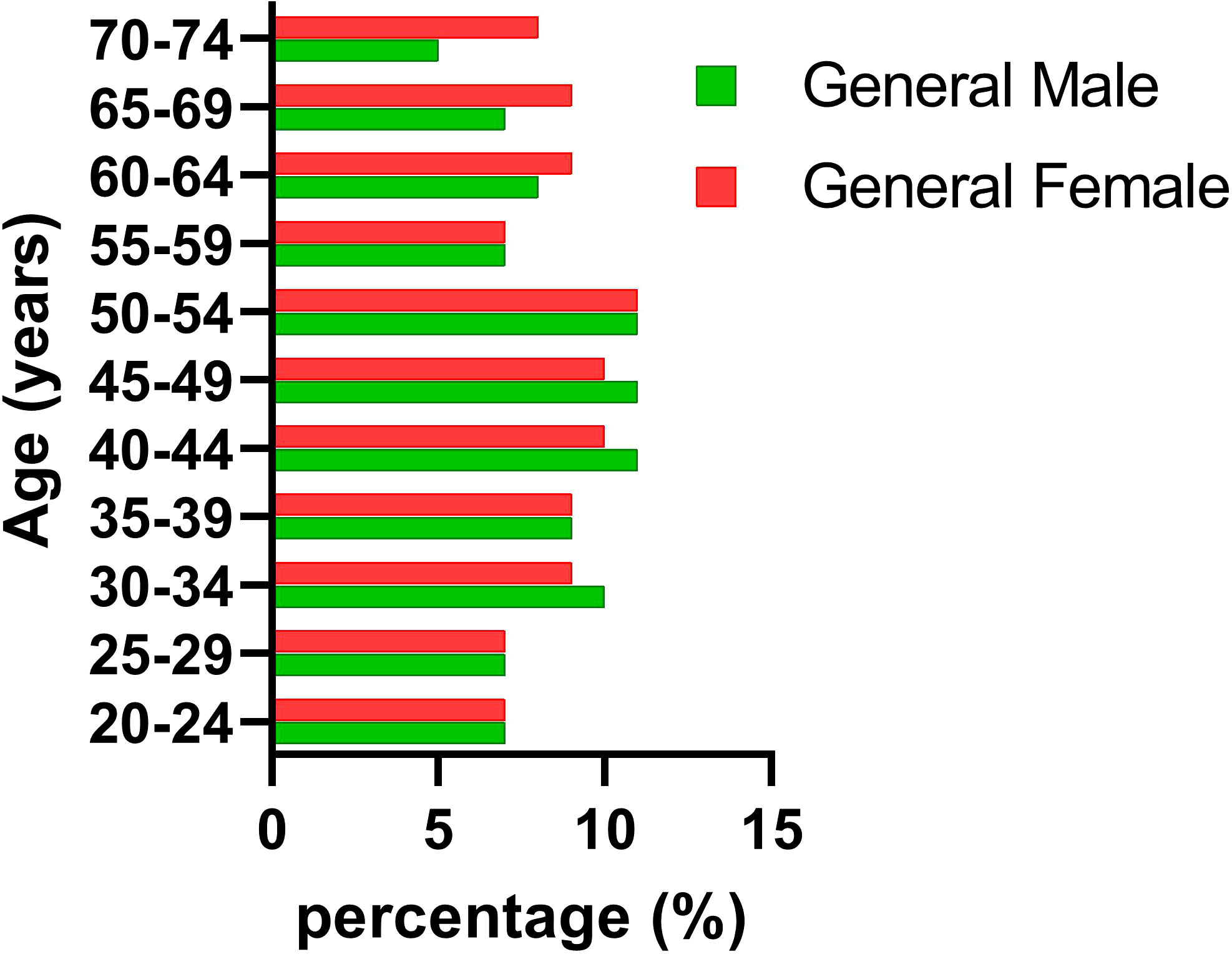
Figures 1, 2 reveal notable differences between men and women; however, these differences were not statistically significant (p = 0.6563 and p = 0.6914, respectively). Our findings also indicated that the DHT group comprised mostly women (72%) aged 30–54 years, which differed from the demographics of the general population, where we observed almost the same percentage of women as men (51%).
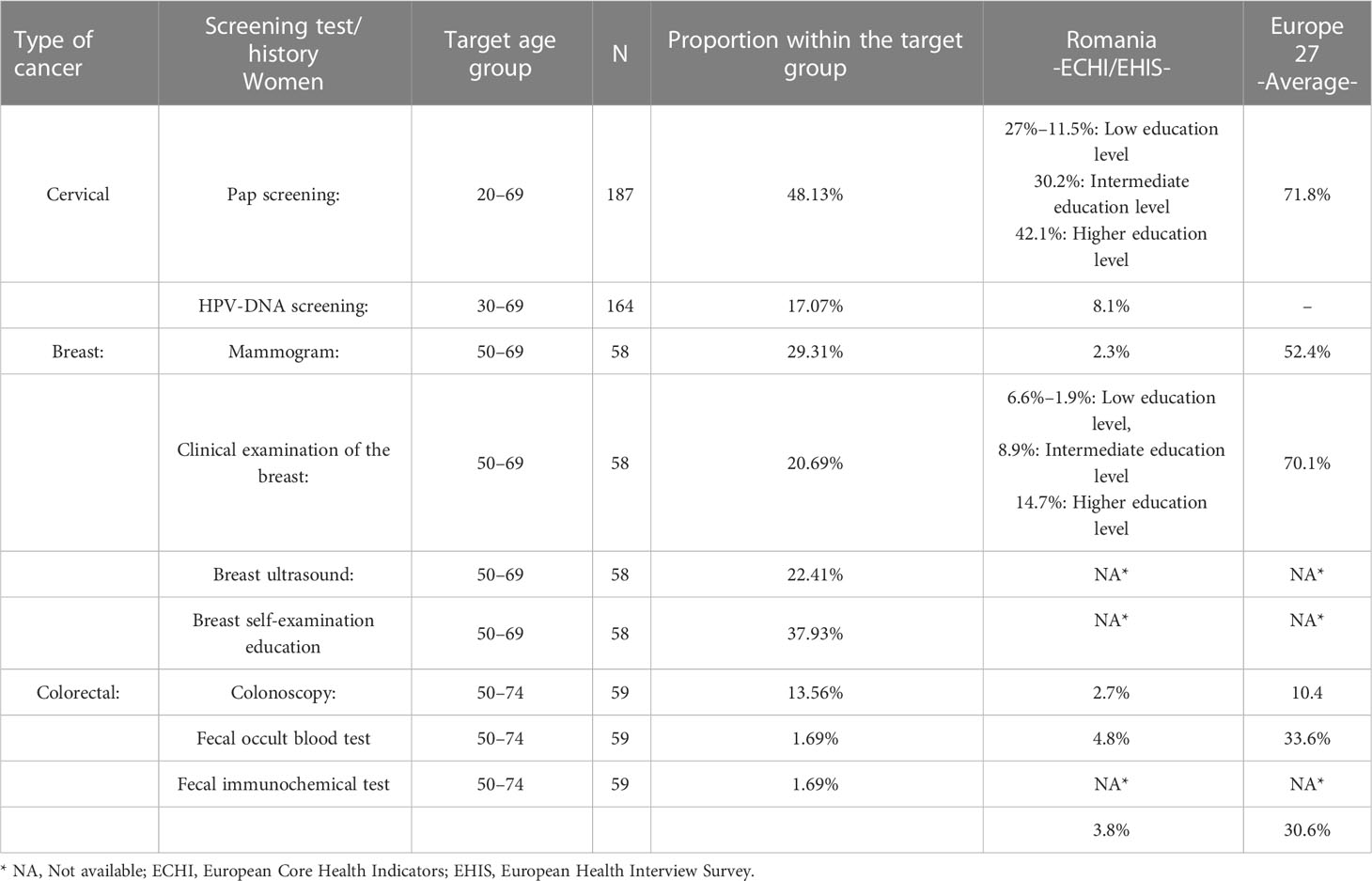
We analyzed the proportions of the preventive screening tests recommended for the DHT users (men and women) in each target age group. We compared these with the European Core Health Indicators (ECHI) (15) and European Health Interview Survey (EHIS) (16) data, where available. These comparisons are presented in Tables 1–3. The numbers of the target group are displayed in the target group column for each screening test.
3.1 Women
The cervical cancer tests involved Pap smears every three years and HPV-DNA testing every five years. The proportion of women (20–69 years) who reported having had a Pap test was 48% in DHT users, compared to 27% in Romania and 71.8% in European Union average (includes 27 member states; EU 27) as reported by the ECHI. According to the most recent EHIS performed in Romania in 2019, 37.5% of women reported having had Pap smear screening in the preceding two years, compared to 70.8% in the EU 27.
The proportion of women in our DHT group who reported having been tested for HPV-DNA was 17%, which was much lower than that for Pap, at 48,13%, reflecting the general trend in Romania with regard to HPV testing, at 8.1% (17).
The primary breast cancer standard screening test investigated was mammography; It was recommended at 50 years for women with no family history of breast cancer to be performed every two years until age 69 (12). The proportion of women (aged 50–69 years) who reported having had a mammogram within the preceding two years in the DHT group was 29.3%, compared to 2.3% in Romania and 52.4% in EU 27 (16). The values for other tests recommended or used for breast cancer screening were lower than those in EU 27 (20.6% reported having clinical examinations versus the EU 27 average of 70%). In the target group, 22% of the women underwent breast echography, which has some specific indications but is not considered a general screening method.
Of the women in the DHT group, 13.56% reported having undergone colorectal cancer tests (sigmoidoscopy or colonoscopy). Only 1.69% had undergone FOBTs, and 1.69% had undergone FITs. This was far below the EU 27 average of 30.6% but was four times higher than the percentage reported for the general Romanian population.
3.2 Men
PSA testing is a general recommendation for prostate cancer screening, alongside the clinical examination of the prostate. Of the DHT group men, 50% had undergone PSA screening, and 16.7% had undergone clinical examination of the prostate. The data for comparing prostate screening results with those in the EHIS and ECHI databases were unavailable (15, 16).
For colorectal cancer in the DHT group, 21.7% of the men reported having had sigmoidoscopy or colonoscopy, 4.3% had undergone FOBT, and 1.69% had undergone FITs. These figures were comparable to the EU 27 average of 30.2%. However, they were six times higher than those of the general population in Romania.
4 Discussion
In Romania, 80% of the population has internet access (18) from a highly developed and competitive infrastructure. Romania ranks tenth out of 180 countries in the average fixed broadband speed, with a speed of 174.26 Mbps reported in April 2023, which is twice the global 80.12 Mbps average. On mobile device the average upload speed it was 49.03 Mbps average, ranking 44 out of 138 global positions list, above global performance of 42.07 Mbps (19) One in every two Romanians owns a smartphone (20). Therefore, devices and internet connections are not barriers to accessing DHT in Romania.
For all cancer screening tests we investigated, the proportion of users who reported having undergone screening tests was two to six times higher in the DHT group than in the general Romanian population but closely mirrored the European average. Additionally, the age distribution reveals a large proportion of users <40 years, indicating that DHT can help detect cancers early in these age groups in the future, which can be considered a strength of DHT in oncology.
Challenges and barriers exist in balancing digital self-care utilization and general accessibility. Primary care centers are usually the first point of contact in prevention, and whether digital health will change this arrangement is questionable (21).
Herein, we revealed that it is not technical barriers but rather educational ones that influence the use of DHT for cancer prevention.
5 Conclusions
A significant difference existed between DHT users and the general Romanian population in terms of accessing cancer prevention screening tests. The DHT users in our cohort were mostly women (72%) aged 30–54 years. Regarding the utilization of preventive cancer screening tests, the DHT group reported two to six times higher rates compared to the general Romanian population. This led us to conclude that digital technologies in the “self-care” model were more amenable for internet-literate individuals with higher levels of education. This group also had the highest rate of utilizing screening tests in the general European population, according to the ECHI and EHIS. Consequently, implications in terms of the healthcare prevention organizational framework are that DHT should be integrated and used at the primary care level to have a stronger impact on the general population—older and younger—with different levels of education and internet literacy and to address health disparities in the preventive health domain.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://osf.io/tjuqe/files/osfstorage/63e1edd93db09501351ced85.
Ethics statement
The studies involving human participants were reviewed and approved by Ovidius Clinical Hospital Medical Ethics and Research Comity with Decision No. 5.1./15.08.2021. Written informed consent from the participants was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
BP, NC, and CC contributed to the study’s conception, methodology, original draft preparation, and design. These authors contributed equally to this work and share the first authorship. AT-S performed the statistical analysis. FF and LM reviewed the draft of the manuscript. All authors contributed to the manuscript revision and read and approved the final version.
Acknowledgments
Dr. Lavinia Lopatica and Dr. Otilia Frumusachi, public health resident doctors at the time of the study, are thanked for their contribution in data sorting.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Van Velthoven MH, Smith J, Wells G, Brindley D. Digital health app development standards: a systematic review protocol. BMJ Open (2018) 8:e022969. doi: 10.1136/bmjopen-2018-022969
2. Cosoli G, Spinsante S, Scalise L. Wearable devices and diagnostic apps: beyond the borders of traditional medicine, but what about their accuracy and reliability? IEEE Instrumentation Measurement Magazine (2021) 24(6):89–94. doi: 10.1109/MIM.2021.9513636
3. Patel NA, Butte AJ. Characteristics and challenges of the clinical pipeline of digital therapeutics. Digit Med (2020) 3:159. doi: 10.1038/s41746-020-00370-8
4. Choukou MA, Sanchez-Ramirez DC, Pol M, Uddin M, Monnin C, Syed-Abdul S. COVID-19 infodemic and digital health literacy in vulnerable populations: a scoping review. Digit Health (2022) 8:20552076221076927. doi: 10.1177/20552076221076927
5. Cunard Chaney S, Mechael P. HealthEnabled, in collaboration with the Self-Care Trailblazer Group, Digital Self-Care. A framework for Design, Implementation & Evaluation. Population Services International (2020). Available at: https://media.psi.org (Accessed September 2022).
6. Fahy N, et al. COVID-19 health system response monitor network. use of digital health technologys in Europe: before, during and after COVID-19 (2021). European Observatory on Health Systems and Policies. Available at: https://eurohealthobservatory.who.int/publications/i/use-of-digital-health-technologys-in-europe-before-during-and-after-covid-19 (Accessed September 2022).
7. Maddula R, MacLeod J, McLeish T, Painter S, Steward A, Berman G, et al. The role of digital health in the cardiovascular learning healthcare system. Front Cardiovasc Med (2022) 9:1008575. doi: 10.3389/fcvm.2022.1008575
8. Scholz S, Teetz L. Smart health via mHealth? potentials of mobile health apps for improving prevention and adherence of breast cancer patients. Digit Health (2022) 8:20552076221074127. doi: 10.1177/20552076221074127
9. Ruco A, Dossa F, Tinmouth J, Llovet D, Jacobson J, Kishibe T, et al. Social media and mHealth technology for cancer screening: systematic review and meta-analysis. J Med Internet Res (2021) 23(7):e26759. doi: 10.2196/26759
10. Zhang D, Advani S, Waller Jo, Cupertino A-P, Hurtado-de-Mendoza A, Chicaiza A, et al. Mobile technologies and cervical cancer screening in low- and middle-income countries: a systematic review. JCO Global Oncol (2020) 6:617–27. doi: 10.1200/JGO.19.00201
11. World Health Organisation. WHO guideline for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention (2021). 2nd edAvailable at: https://www.who.int/publications/i/item/9789240030824 (Accessed September 2022)
12. European Guidelines on breast cancer screening and diagnosis (2022). European Commission. Available at: https://healthcare-quality.jrc.ec.europa.eu/ecibc/european-breast-cancer-guidelines (Accessed September 2022).
13. European Guidelines for quality assurance in colorectal cancer screening and diagnosis (2010). European Commission. Available at: https://op.europa.eu/en/publication-detail/-/publication/e1ef52d8-8786-4ac4-9f91-4da2261ee535 (Accessed September 2022).
14. Policy paper on PSA screening for prostate cancer (2020). Europa Uomo. Available at: https://www.europa-uomo.org/wp-content/uploads/2020/03/71706_EAU_policy-briefing_PSA.pdf (Accessed September 2022).
15. ECHI. European Commission. Available at: https://health.ec.europa.eu/indicators-and-data/european-core-health-indicators-echi_en (Accessed September 2022).
16. EHIS. European Commission. Available at: https://ec.europa.eu/eurostat/cache/metadata/en/hlth_det_esms.htm (Accessed September 2022).
17. Bruni L, Albero G, Serrano B, Mena M, Collado JJ, Gómez D, et al. ICO/IARC information centre on HPV and cancer (HPV information centre). human papillomavirus and related diseases in romania. summary report. Available at: https://hpvcentre.net/statistics/reports/ROU.pdf (Accessed 10.01.2023).
18. World Bank. Available at: https://data.worldbank.org/indicator/IT.NET.USER.ZS?locations=RO (Accessed September 2022).
19. Speed test Global Index. Available at: https://www.speedtest.net/global-index#mobile (Accessed May 2023).
20. ANCOMNational authority for management and regulation in communications of Romania, annual report (2021). Available at: https://www.ancom.ro.
Keywords: digital health technologies, prevention, self-care, screening, cancer
Citation: Pana BC, Ciufu N, Ciufu C, Furtunescu FL, Turcu-Stiolica A and Mazilu L (2023) Digital technology for health shows disparities in cancer prevention between digital health technology users and the general population in Romania. Front. Oncol. 13:1171699. doi: 10.3389/fonc.2023.1171699
Received: 15 March 2023; Accepted: 15 June 2023;
Published: 06 July 2023.
Edited by:
Arvind Rao, University of Michigan, United StatesReviewed by:
Souptik Barua, New York University, United StatesGloria Cosoli, Marche Polytechnic University, Italy
Copyright © 2023 Pana, Ciufu, Ciufu, Furtunescu, Turcu-Stiolica and Mazilu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bogdan C. Pana, Ym9nZGFuLnBhbmFAdW1mY2Qucm8=
†These authors have contributed equally to this work and share first authorship
 Bogdan C. Pana
Bogdan C. Pana Nicolae Ciufu3,4†
Nicolae Ciufu3,4† Adina Turcu-Stiolica
Adina Turcu-Stiolica