- 1Cancer Center, Department of Radiation Oncology, Zhejiang Provincial People’s Hospital, Affiliated People’s Hospital, Hangzhou Medical College, Hangzhou, Zhejiang, China
- 2Department of Tumor Radiochemotherapy, Second Affiliated Hospital of Wenzhou Medical University, Wenzhou, Zhejiang, China
Objective: To explore the advantages of dosimetry and the treatment efficiency of tangent-arc technology in deep inspiration breath-hold radiotherapy for breast cancer.
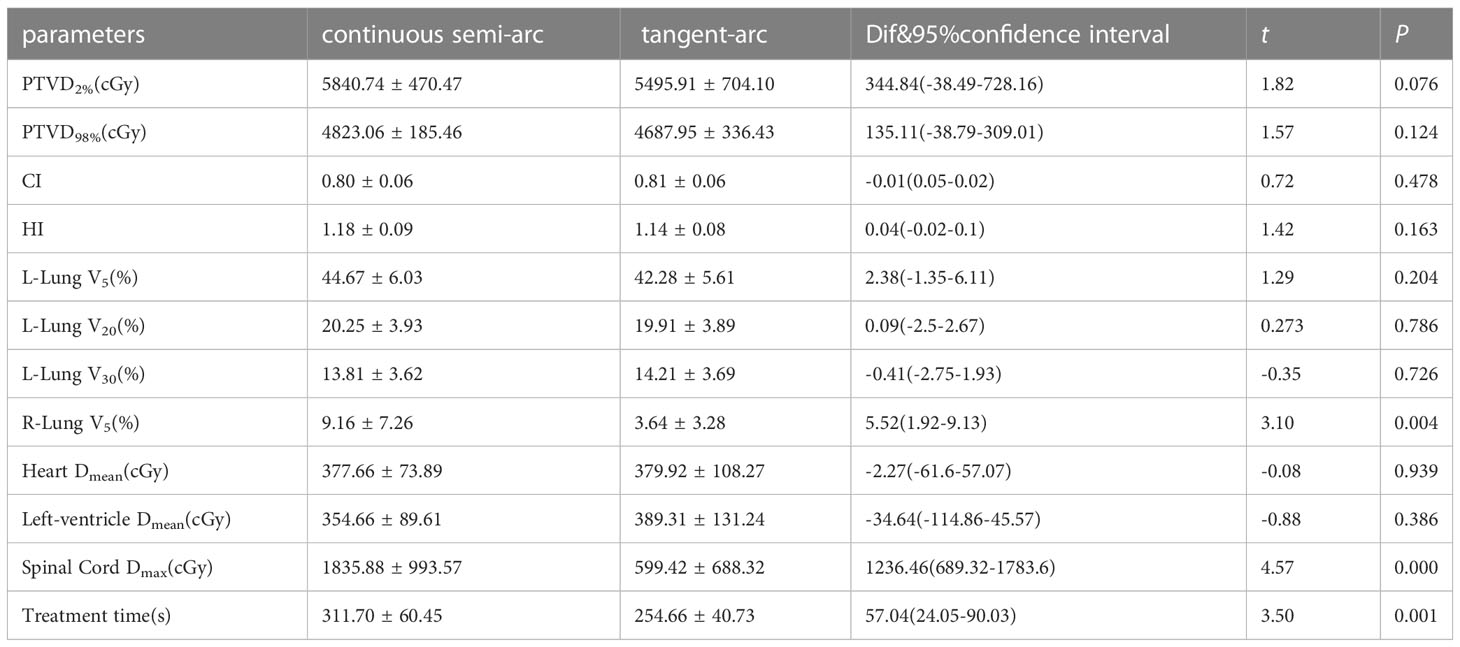
Methods: Forty patients with left-sided breast cancer who were treated in our hospital from May 2020 to June 2021 were randomly selected and divided into two groups. The first group’s plan was a continuous semi-arc that started at 145° ( ± 5°) and stopped at 325° ( ± 5°). The other group’s plan, defined as the tangent-arc plan, had two arcs: the first arc started at 145° ( ± 5°) and stopped at 85° ( ± 5°), and the second arc started at 25° ( ± 5°) and stopped at 325° ( ± 5°). We compared the target dose, dose in organs at risk (OARs), and treatment time between the two groups.
Results: The target dose was similar between the continuous semiarc and tangent-arc groups. The V5 of the right lung was significantly different between the two groups (Dif 5.52, 95% confidence interval 1.92-9.13, t=3.10, P=0.004), with the patients in the continuous semi-arc and tangent-arc groups having lung V5 values of (9.16 ± 1.62)%, and (3.64 ± 0.73)%, respectively. The maximum dose to the spinal cord was (1835.88 ± 222.17) cGy in the continuous semi-arc group and (599.42 ± 153.91) cGy in the tangent-arc group, yielding a significant difference between the two groups (Dif 1236.46, 95% confidence interval 689.32-1783.6, t=4.57, P<0.001). The treatment times was (311.70 ± 60.45) s for patients in the continuous semi-arc group and (254.66 ± 40.73) s for patients in the tangent-arc group, and there was a significant difference in the mean number of treatment times between the two groups (Dif 57.04, 95% confidence interval 24.05-90.03, t=3.5, P=0.001).
Conclusion: Both the continuous semi-arc and tangent-arc plans met the clinical prescription dose requirements. The OARs received less radiation with the tangent-arc plan than the continuous semi-arc plan, especially for the lung (measured as V5) and the spinal cord (measured as the maximum dose). Tangent-arc plan took significantly less time than the continuous semi-arc, which can greatly improve treatment efficiency. Therefore, tangent-arc plans are superior continuous semi-arc plans for all cases.
Introduction
In women, breast cancer is the most common malignant tumor and has the highest mortality and morbidity among all malignant tumors worldwide (1–4). Recently, radiation therapy coupled with breast-conserving surgery has become the standard treatment for many patients with breast cancer (5, 6). For patients with breast cancer on the left side, the radiation dose to the heart should be taken into account during radiation therapy because the tumor is relatively close to the heart. Although no studies have demonstrated that the minimum exposure dose causes radiation-induced cardiac injury, increased cardiac doses are associated with increased rates of cardiac and coronary events. Furthermore, cardiac damage is correlated with the mean cardiac dose, with an increase of 4%-16% in the rate of acute coronary events per 1 Gy (7–11). To reduce the dose to organs at risk (OARs) as much as possible, some scholars have proposed new improvements in imaging techniques and treatment planning systems and have introduced new irradiation techniques, such as deep inspiration breath hold (DIBH) and respiratory gating (RG) (12–16). The main techniques used in breast cancer radiotherapy are three-dimensional conformal radiation therapy (3D-CRT), intensity modulated radiation therapy (IMRT), and volumetric modulated arc therapy (VMAT). Compared to 3D-CRT, both IMRT and VMAT can improve the target volume’s conformity index (CI) and homogeneity index (HI) while reducing the dose to OARs (17–19). The difference between IMRT and VMAT is that, when treating patients, the IMRT gantry has a fixed angle during irradiation, whereas in VMAT, the gantry rotates while the beam is on. Therefore, VMAT technology can increase the CI of the target. In recent years, the application of VMAT combined with DIBH technology has further reduced the dose of OARs (20–22). The focus of medical physicists is the optimization of treatment efficiency and design of the X-ray angle in the radiotherapy plan such that the dose to the OARs can be reduced as much as possible while ensuring that the target volume receives a sufficient dose.
This study aims to explore a new tangent-arc irradiation technique based on DIBH. It is expected that this technique will allow patients with left-sided breast cancer to receive adequate doses of radiotherapy in the target region while further reducing the dose of OARs, especially the heart, lungs, and other organs that affect the quality of life of patients. It is also expected to reduce patients’ DIBH time which can effectively improve the efficiency of treatment time while improving patient cooperation. Thus, a high-quality and efficient plan design scheme is provided for patients with left breast cancer using the DIBH technique.
Methods and materials
Patient selection
Forty patients with left-sided breast cancer who were treated in our hospital from May 2020 to June 2021 were randomly enrolled in this study and divided into two groups, one continuous semi-arc plan group and the other tangent-arc plan group. The continuous semi-arc plan had only one arc that rotated counterclockwise from 145° ( ± 5°) to 325° ( ± 5°). The tangent-arc plan had two arcs: the first arc rotated counterclockwise with a start angle of 145° ( ± 5°) and a stop angle of 85° ( ± 5°), and the second arc rotated counterclockwise from 25 ( ± 5)°to 325° ( ± 5°). The angles of the two plans are shown in Figure 1. Among them, the mean age of the 20 patients treated with continuous semi-arc technology was 47.1 (range 33-58) years, and the mean age of the 20 patients treated with tangent-arc technology was 45.7 (range 29-60) years. The inclusion criteria were left-sided breast cancer, no contraindications to radiotherapy, KPS> 70, age younger than 60 years old, ability to fully understand the process of DIBH, and ability to breath-hold for more than 30 s. All patients completed simulated positioning and surface-guided radiation therapy (SGRT) using Catalyst Systems v5.4.2 SP3 (C-RAD Positioning AB, Uppsala, Sweden) with DIBH to reduce localization uncertainty during treatment delivery. The exclusion criteria were a breath-holding time of fewer than 30 s, communication disorders, and other underlying diseases affecting radiotherapy.
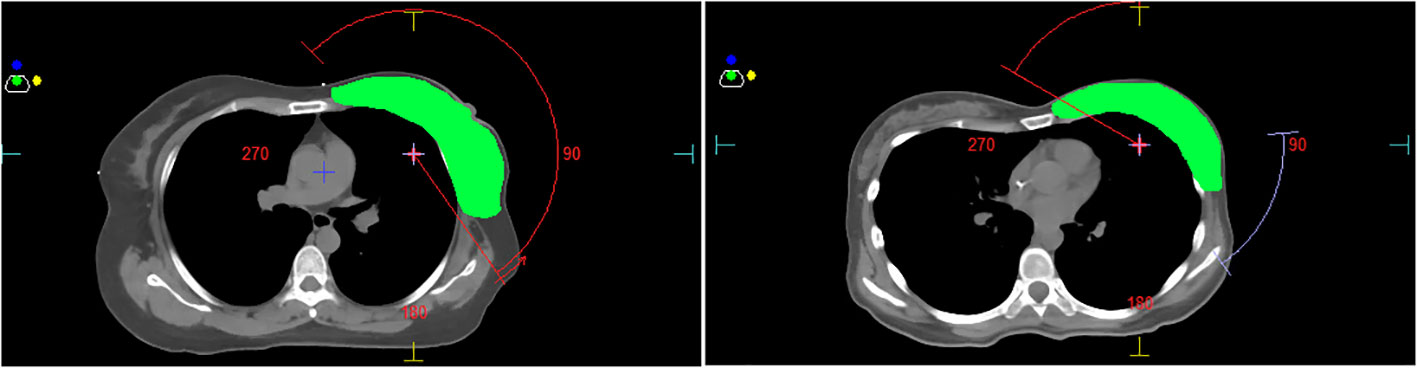
Figure 1 (The left is the continuous semi-arc, the right is the tangent-arc, and green represents PTV).
CT simulation positioning, target contour, planning design
All patients were laid in a supine position with both arms fully abducted and externally rotated on a vacuum cushion on the all-in-one board. Treatment planning CT scans at 5-mm intervals from the ear to 2 cm below the diaphragm were obtained for each patient with a CT simulator (Discovery CT590, GE, Wisconsin, USA). The target and OARs of this study were delineated following the Radiation Therapy Oncology Group (RTOG) and the International Commission Radiological Units (ICRU) (23, 24). The two groups of patients were treated with continuous semi-arc technology and tangent-arc technology. Both plans were generated using the MonacoV5.11 (Elekta AB, Stockholm, Sweden) three-dimensional treatment planning system by the same senior medical physicist. The “Dual Arc” function provided by the treatment planning system was used to generate clockwise and counterclockwise dual arcs for each plan. The doses were normalized such that the dose to 95% of the planning target volume (PTV) was the same for all plans.
Dose evaluation
All plans were compared and evaluated. The near maximum dose covering 2% of the PTV (D2%), near minimum dose covering 98% of the PTV (D98%), and mean dose (Dmean) to the PTV was determined. The volume of the left lung receiving dose greater than 5, 20, and 30 Gy (V5, V20, and V30, respectively) and the Dmean of the left lung were considered as well as the V5 and Dmean of the right lung, Dmean of the heart and left ventricle, maximum dose (Dmax) of the spinal cord, beam-on time, CI and HI. The CI was calculated from the formula: CI= (TV95/TV) × (TV95/V95), where V95 is the target volume receiving 95% of the prescription dose, TV is the target volume, and V95 is the volume receiving 95% of the prescription dose. HI was calculated according to HI=(D5%)/(D95%) where D5% and D95% represent doses received by 5% and 95% of PTV, respectively). The closer the CI and HI values are to 1, the better the quality of the plan. The treatment time of all patients was recorded by the catalyst software.
Statistical analysis
All patient data were statistically analyzed using SPSS software (version 20, SPSS Inc., Chicago, IL, USA). The independent sample t-test was used to analyze parameters with homogeneous variance and normal distribution; otherwise, the nonparametric Wilcoxon signed-rank test was used. Data with a normal distribution are expressed as x ± s and were analyzed with the independent sample t-test, while those with a nonnormal distribution are presented as M (Q1, Q3) and were analyzed with the Mann-Whitney U test. A value of P< 0.05 was considered statistically significant.
Results
Details of the dosimetry, treatment time, and beam-on-time comparisons are presented in Tables 1 and 2. The dose constraints were defined for OARs as follows: left lung: V5<50%, V20< 26%, V30< 20%; right lung: V5<12%; heart: Dmean<7 Gy; left ventricle: Dmean<7 Gy; spinal cord: Dmax< 40 Gy. The right lung V5 of the patients in the continuous semi-arc group and the tangent-arc group were (9.16 ± 1.62)% and (3.64 ± 0.73)%, respectively, with a significant difference between the two groups (Dif 5.52, 95% confidence interval 1.92-9.13, t=3.10, P=0.004). The maximum dose in the spinal cord was (1835.88 ± 222.17) cGy in the continuous semi-arc group and (599.42 ± 153.91) cGy in the tangent-arc group, and there was a significant difference between the two groups (Dif 1236.46, 95% confidence interval 689.32-1783.6, t=4.57, P<0.001). The treatment time was (311.70 ± 60.45) s for patients in the continuous semi-arc group and (254.66 ± 40.73) s for patients in the tangent-arc group, with a significant difference between the two groups (Dif 57.04, 95% confidence interval 24.05-90.03, t=3.5, P=0.001).
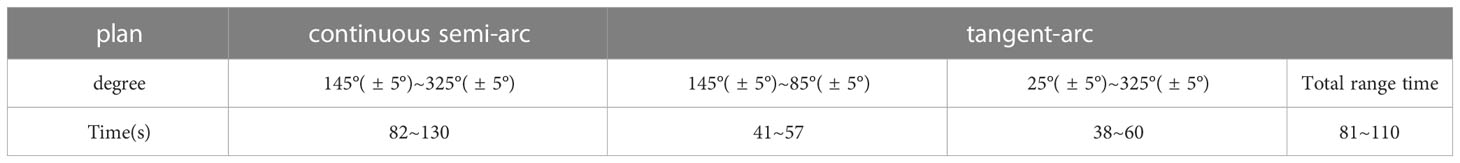
Table 2 Comparison of the beam-on-time between continuous semi-arc and tangent-arc plans with different field angles.
Discussion
Recently, with developments in radiotherapy physics and computing technologies, VMAT has become one of the mainstream technologies of radiotherapy. In particular, VMAT combined with DIBH can greatly reduce the dose of OARs while ensuring a sufficient dose to the target (20–22). Currently, the 5-year survival rate for stage I breast cancer is >85% worldwide and the majority of breast cancer patients can be cured with a combination of chemotherapy and radiotherapy (25–27). However, to our knowledge, there is no evidence proving that the minimum dose does not cause radiation-induced heart and lung injuries. Therefore, to improve the patient’s quality of life, medical physicists ensure that normal tissues are treated at as low a dose as possible while maintaining adequate target coverage. Comparing the time and dosimetry of two different VMAT techniques, This study showed that the tangent-arc technique was shown to reduce the dose to OARs and the treatment time compared to the continuous semi-arc plan.
The analysis showed that the maximum and minimum doses to the PTV increased by 5.9% and 2.8%, respectively, in the continuous semi-arc group compared with the tangent-arc group, but these increases were not statistically significant. The CI and HI of the two plans were also not significantly different. The reason for this lack of statistical difference may be that the dose of the target area was normalized to 95% for both the continuous semi-arc and tangent-arc plan designs.
Related studies have shown that V5, V20, and V30 of the lung, especially V20, play important roles in radiation-induced pulmonary injury and fibrosis. When lung V20>20%, the probability of radiation pneumonitis is 28.4%, and when V20 ≤ 20%, the incidence of radiation pneumonitis is 12.5% (28–31). Here, the average V20 of the left lung of the continuous semi-arc plan was 20.25%, and that of the tangent-arc plan was 19.91%. Therefore, the tangent-arc plan may reduce the incidence of radiation pneumonitis. Additionally, the low-dose volume effect of the bilateral lung must be taken seriously in the clinical practice of breast cancer radiotherapy. Novakova-Jiresova et al. (32) conducted radiation-induced lung injury animal experiments, and showed that animals receiving low-dose and large-volume irradiation showed had greater lung function damage. John et al. (33) believed that larger lung volumes receiving low-dose irradiation would cause more severe radiation-induced lung damage. With the development of radiotherapy technology, the long-term survival rate of breast cancer has improved significantly. Some scholars have shown that low-dose radiation increases the risk and toxicity of secondary cancer (34, 35). Our results showed that the mean V5 value of the left and right lungs was reduced by approximately 5.4% and 60.26%, respectively, in the tangent-arc group compared with the continuous semi-arc group. Therefore, the V5 lung benefited from the use of tangent-arc (Table 1).
The results of this study showed that the mean cardiac doses of 377.66 cGy (continuous semi-arc group) and 379.92 cGy (tangent-arc group) in patients with breast cancer were lower than the 403 cGy value reported by Karpf et al. (36). The difference may result from the sample size and the volumes of the tumors. The author believe that this small difference would not affect the clinical benefit. Regarding the spinal cord, the maximum dose in the continuous semi-arc plan was approximately three times that of the tangent arc plan, possibly because the tangent-arc plan does not contribute any dosage to the spinal cord at 85°~25°, which is exactly the direction of vertical irradiation of the spinal cord, causing the spinal cord dose to drop significantly. Although the spinal cord doses of the two plans met the clinical dose requirement, the tangent-arc technique is more in line with the principle of being as low as reasonably achievable (37, 38).
The tangent-arc plan had shorter treatment time and X-ray beam-on time than the continuous semi-arc plan, and that the patient’s breath-hold interval was an important factor in the efficiency of treatment in the delivery treatment process. During the CT simulation, the patient must hold breath longer than 30 s. Then, in the continuous semi-arc plan, the beam-on time is 82~130 s, during which the patients can suffer from too little rest time which restricts their breathing, ultimately affecting the efficiency of treatment. However, in the tangent-arc plan, two small arcs are designed, with respective beam-on time of each arc is 41~57s and 38~60s, so the patient can complete each therapeutic arc in 1-2 breath-hold cycles. During the gantry rotation of the LINAC in between the two treatment fields, all patients were able to rest enough to maintain a stable breath-hold during the subsequent treatment field.
Conclusions
Both continuous semi-arc and tangent-arc plans met the clinical prescription dose requirements. After comparing the radiation dose to OARs and the treatment time of patients, we believe that when left-sided breast cancer patients are treated with VMAT radiotherapy combined with DIBH, tangent-arc plans can be more effective. Tangent-arc plans can reduce the radiation dose to the patient’s OARs, such as the lung and spinal cord, and the treatment time can be faster. Therefore, the plan quality is superior for tangent-arc plans compared to continuous semi-arc plans for all cases. A limitation of this study is that there was no discussion of patient staging. The authors will further explore the advantages and disadvantages of using the two technical schemes in different stages.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The ethics institutional review board of Zhejiang Provincial People’s Hospital (Hangzhou, China) approved this study (project approval number QT2023020) and waived informed consent for this retrospective study.
Author contributions
Manuscript drafting, editing, and statistical analysis: YL. Design, supervision, data interpretation, and critical review: WC. Patient surveillance and data acquisition:WZ, YJ, HX, CF, BL, and LQ. Literature search: QL, HL, and YZ, JD. All authors read and approved the final manuscript. All authors contributed to the article.
Funding
This research was partially supported by the National Natural Science Foundation of China (82102814), this research was supported by Zhejiang Provincial Natural Science Foundation of China under Grant No. GF21H180053, and the Medical and Health Research Project of Zhejiang Province (2021PY002).
Acknowledgments
Our thanks to AJE American Journal Experts for help with language editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ferlay J, Colombet M, Soerjomataram I, Parkin DM, Piñeros M, Znaor A, et al. Cancer statistics for the year 2020: an overview. Int J Cancer (2021).
2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2020) 68(6):394–424. doi: 10.3322/caac.21492
3. Hegde P, Pande J, Adly HH, Shetty P, Jayakumari A. Breast Cancer Risk factor awareness and utilization of screening program: A cross-sectional study among women in the Northern Emirates. Gulf J Oncolog (2018) 1(27):24–30.
4. Patra S, Young V, Llewellyn L, Senapati JN, Mathew J. BRAF, KRAS and PIK3CA mutation and sensitivity to trastuzumab in breast cancer cell line model. Asian Pac J Cancer Prev (2017) 18(8):2209–13. doi: 10.22034/APJCP.2017.18.8.2209
5. Hu S, Xie D, Zhou P, Liu X, Yin X, Huang B, et al. LINCS gene expression signature analysis revealed bosutinib as a radiosensitizer of breast cancer cells by targeting eIF4G1. Int J Mol Med (2021) 47(5):72.
6. Nunez A, Jones V, Schulz-Costello K, Schmolze D. Accuracy of gross intraoperative margin assessment for breast cancer: experience since the SSO-ASTRO margin consensus guidelines. Sci Rep (2020) 10(1):17344.
7. Darby S, McGale P, Taylor C, Peto R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer. Prospective cohort study of about 300 000 women in US SEER cancer registries. LancetOncol (2005) 6(8):557–65.
8. Sardaro A, Petruzzelli MF, D'Errico MP, Grimaldi L, Pili G, Portaluri M. Radiation-induced cardiac damage in early left breast cancer patients. Risk factors, biological mechanisms, radiobiology, and dosimetric constraints. Radiother Oncol (2012) 103(2):133–42.
9. Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Brønnum D, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med (2013) 368(11):987–98.
10. Van den Bogaard VAB, Ta BDP, van der Schaaf A, Bouma AB, Middag AM, Bantema-Joppe EJ, et al. Validation and modification of a prediction model for acute cardiac events in patients with breast cancer treated with radiotherapy based on three-dimensional dose distributions to cardiac substructures. J Clin Oncol (2017) 35:1171–8.
11. Taylor C, Correa C, Duane FK, Aznar MC, Anderson SJ, Bergh J, et al. Estimating the risks of breast cancer radiotherapy: evidence from modern radiation doses to the lungs and heart and from previous randomized trials. J Clin Oncol (2017) 35:1641–9.
12. Waissi W, Amé JC, Mura C, Noël G, Burckel H. Gemcitabine-based chemoradiotherapy enhanced by a PARP inhibitor in pancreatic cancer cell lines. Int J Mol Sci (2021) 22(13):6825.
13. Bergom C, Currey A, Desai N, Tai A, Strauss JB. Deep inspiration breath hold: techniques and advantages for cardiac sparing during breast cancer irradiation. Front Oncol (2018) 8:87.
14. Reitz D, Carl G, Schönecker S, Pazos M, Freislederer P, Niyazi M, et al. Real-time intra-fraction motion management in breast cancer radiotherapy: analysis of 2028 treatment sessions. Radiat Oncol (2018) 13(1):128.
15. Falco M, Masojć B, Macała A, Łukowiak M, Woźniak P, Malicki J. Deep inspiration breath hold reduces the mean heart dose in left breast cancer radiotherapy. Radiol Oncol (2021) 55(2):212–20.
16. Pandeli C, Smyth LML, David S, See AW. Dose reduction to organs at risk with deep-inspiration breath-hold during right breast radiotherapy: a treatment planning study. Radiat Oncol (2019) 14(1):223.
17. Mansouri S, Naim A, Glaria L, Marsiglia H. Dosimetric evaluation of 3-D conformal and intensity-modulated radiotherapy for breast Cancer after conservative surgery. Asian Pac J Cancer Prev (2014) 15(11):4727–32.
18. Fong A, Bromley R, Beat M, Vien D, Dineley J, Morgan G. Dosimetric comparison of intensity modulated radiotherapy techniques and standard wedged tangents for whole breast radiotherapy. J Med Imaging Radiat Oncol (2009) 53(1):92–9.
19. Mo JC, Huang J, Gu WD, Gao M, Ning ZH, Mu JM, et al. A dosimetric comparison of double-arc volumetric arc therapy, step-shoot intensity-modulated radiotherapy and 3D-CRT for left-sided breast cancer radiotherapy after breast-conserving surgery. Technol Health Care (2017) 25(5):851–8. doi: 10.3233/THC-160746
20. Tang L, Ishikawa Y, Ito K, Yamamoto T, Umezawa R, Jingu K. Evaluation of DIBH and VMAT in hypofractionated radiotherapy for left-sided breast cancers after breast-conserving surgery: A planning study. Technol Cancer Res Treat (2021) 20:15330338211048706.
21. Corradini S, Ballhausen H, Weingandt H, Freislederer P, Schönecker S, Niyazi ., et al Left-sided breast cancer and risks of secondary lung cancer and ischemic heart disease: Effects of modern radiotherapy techniques. Strahlenther Onkol (2018) 194(3):196–205.
22. Jensen CA, Roa AMA, Johansen M, Lund JÅ, Frengen J. RobustnessofVMATand3DCRTplanstowardsetuperrorsinradiationtherapyoflocallyadvancedleft-sidedbreastcancerwithDIBH. Phys Med (2020) 45:198–204. doi: 10.3322/caac.21492
23. Oncology N R G. Breast Cancer Atlases, Templates, & Tools,NRG Protocol Radiation Therapy Template (Whole Breast Photon and Proton Therapy).[Internet]. Philadelphia: NRG Oncology. Available at: https://www.nrgoncology.org/ciro-breast.
24. Prescribing I. recording, and reporting photon-beam intensity-modulated radiation therapy (IMRT)[J]. ICRU Rep (2010) 83(10):27–40.
25. Bijker N, Meijnen P, Peterse JL, Bogaerts J, Van Hoorebeeck I, Julien JP, et al. Breast-conserving treatment with or without radiotherapy in ductal carcinoma-in-situ: Ten-year results of European Organization for research and treatment of cancer randomized phase III trial 10853-a study by the EORTC breast cancer cooperative group and EORTC radiotherapy group. J Clin Oncol (2006) 24:3381–7.
26. Early Breast Cancer Trialists' Collaborative Group (EBCTCG), Darby S, McGale P, Correa C, Taylor C, Arriagada R, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomized trials. Lancet (2011) 378:1707–16.
27. Salmon R, Garbey M, Moore LW, Bass BL. Interrogating a multifactorial model of breast conserving therapy with clinical data. PloS One (2015) 10:e0125006.
28. NSABP B-39. RTOG 0413: A Randomized Phase III Study of conventional whole breast irradiation versus partial breast irradiation for women with stage 0, I, or II breast cancer. Clin Adv Hematol Oncol (2006) 4(10):719–21.
29. Lind PA, Marks LB, Hardenbergh PH, Clough R, Fan M, Hollis D, et al. Technical factors associated with radiation pneumonitis after local +/- regional radiation therapy for breast cancer. Int J Radiat Oncol Biol Phys (2002) 52(1):137–43.
30. Jain AK, Vallow LA, Gale AA, Buskirk SJ. Does three-dimensional external beam partial breast irradiation spare lung tissue compared with standard whole breast irradiation? Int J Radiat Oncol Biol Phys (2009) 75(1):82–8. doi: 10.1016/j.ijrobp.2008.10.041
31. Blom Goldman U, Wennberg B, Svane G, Bylund H, Lind P. Reduction of radiation pneumonitis by V20-constraints in breast cancer. Radiat Oncol (2010) 5:99.
32. Novakova-Jiresova A, van Luijk P, van Goor H, Kampinga HH, Coppes RP. Changes in expression of injury after irradiation of increasing volumes in rat lung. Int J Radiat Oncol Biol Phys (2007) 67(5):1510–8.
33. Schallenkamp JM, Miller RC, Brinkmann DH, Foote T, Garces YI. Incidence of radiation pneumonitis after thoracic irradiation: Dose-volume correlates. Int J Radiat Oncol Biol Phys (2007) 67(2):410–6.
34. Hall EJ. Intensity modulated radiation therapy, protons and the risk of second cancers. Int J.Rad Oncol Biol Phys (2006) 65(1):1–7.3.
35. Hall EJ, Wuu C-S. Radiation-induced second cancers : the impact of 3D-CRT and IMRT. Int J.Rad Oncol Biol Phys (2003) 56:83–8.
36. Karpf D, Sakka M, Metzger M, Grabenbauer GG. Left breast irradiation with tangential intensity modulated radiotherapy (t-IMRT) versus tangential volumetric modulated arc therapy (t-VMAT): trade-offs between secondary cancer induction risk and optimal target coverage. Radiat Oncol (2019) 14(1):156.
37. Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, et al. American College of Cardiology Foundation/American Heart Association Task Force. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation (2012) 126(25):e354–471.
38. Wolk MJ, Bailey SR, Doherty JU, Douglas PS, Hendel RC, Kramer CM, et al. American College of Cardiology Foundation Appropriate Use Criteria Task Force. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol (2014) 63(4):380–406.
Keywords: deep inspiration breath-hold, left breast cancer, dosimetry, organ of risk, continuous semi-arc, tangent-arc
Citation: Li Y, Zhan W, Jia Y, Xiong H, Lin B, Li Q, Liu H, Qiu L, Zhang Y, Ding J, Fu C and Chen W (2023) Application of tangent-arc technology for deep inspiration breath-hold radiotherapy in left-sided breast cancer. Front. Oncol. 13:1145332. doi: 10.3389/fonc.2023.1145332
Received: 16 January 2023; Accepted: 31 July 2023;
Published: 18 August 2023.
Edited by:
Haibo Lin, New York Proton Center, United StatesReviewed by:
Ning Yue, The State University of New Jersey, United StatesJiajian Shen, Mayo Clinic Arizona, United States
Copyright © 2023 Li, Zhan, Jia, Xiong, Lin, Li, Liu, Qiu, Zhang, Ding, Fu and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weijun Chen, Y2hlbndlaWp1bkBobWMuZWR1LmNu
 Yucheng Li
Yucheng Li Wenming Zhan
Wenming Zhan Yongshi Jia1
Yongshi Jia1 Hanchu Xiong
Hanchu Xiong Qiang Li
Qiang Li Weijun Chen
Weijun Chen