
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol. , 03 May 2023
Sec. Pediatric Oncology
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.1122355
This article is part of the Research Topic Critical Complications In Pediatric Oncology and Hematopoietic Cell Transplant, volume II View all 22 articles
 Farris Abutineh1
Farris Abutineh1 Dylan E. Graetz1
Dylan E. Graetz1 Hilmarie Muniz-Talavera1
Hilmarie Muniz-Talavera1 Gia Ferrara1
Gia Ferrara1 Maria Puerto-Torres1
Maria Puerto-Torres1 Yichen Chen1
Yichen Chen1 Srinithya R. Gillipelli2
Srinithya R. Gillipelli2 Paul Elish3
Paul Elish3 Alejandra Gonzalez-Ruiz4
Alejandra Gonzalez-Ruiz4 Yvania Alfonso Carreras5
Yvania Alfonso Carreras5 Shillel Alvarez6
Shillel Alvarez6 Daniela Arce Cabrera7
Daniela Arce Cabrera7 Deiby Arguello Vargas8
Deiby Arguello Vargas8 Miriam Armenta Cruz9
Miriam Armenta Cruz9 Camila Barra10
Camila Barra10 Patricia Calderon Sotelo11
Patricia Calderon Sotelo11 Zulma Carpio12
Zulma Carpio12 Mayra Chavez Rios13
Mayra Chavez Rios13 Daniela Covarrubias14
Daniela Covarrubias14 Lucy de Leon Vasquez15
Lucy de Leon Vasquez15 Rosdali Diaz Coronado12
Rosdali Diaz Coronado12 Ever Amilcar Fing Soto16
Ever Amilcar Fing Soto16 Wendy Gomez-Garcia17
Wendy Gomez-Garcia17 Cinthia Hernandez18
Cinthia Hernandez18 María Susana Juarez Tobias19
María Susana Juarez Tobias19 Esmeralda Leon20
Esmeralda Leon20 Jose de Jesus Loeza Oliva21
Jose de Jesus Loeza Oliva21 Alejandra Mendez1
Alejandra Mendez1 Kenia Miller22
Kenia Miller22 Erika Montalvo Cozar23
Erika Montalvo Cozar23 Natalia del Carmen Negroe Ocampo24
Natalia del Carmen Negroe Ocampo24 Eulalia Penafiel25
Eulalia Penafiel25 Estuardo Pineda26
Estuardo Pineda26 Ligia Rios27
Ligia Rios27 Esperanza Rodriguez Ordonez28
Esperanza Rodriguez Ordonez28 Veronica Soto Chavez29
Veronica Soto Chavez29 Meenakshi Devidas1
Meenakshi Devidas1 Asya Agulnik1*
Asya Agulnik1*Background: Pediatric Early Warning Systems (PEWS) aid in identification of deterioration in hospitalized children with cancer but are underutilized in resource-limited settings. Proyecto EVAT is a multicenter quality improvement (QI) collaborative in Latin America to implement PEWS. This study investigates the relationship between hospital characteristics and time required for PEWS implementation.
Methods: This convergent mixed-methods study included 23 Proyecto EVAT childhood cancer centers; 5 hospitals representing quick and slow implementers were selected for qualitative analysis. Semi-structured interviews were conducted with 71 stakeholders involved in PEWS implementation. Interviews were recorded, transcribed and translated to English, then coded using a priori and novel codes. Thematic content analysis explored the impact of hospital characteristics and QI experience on time required for PEWS implementation and was supplemented by quantitative analysis exploring the relationship between hospital characteristics and implementation time.
Results: In both quantitative and qualitative analysis, material and human resources to support PEWS significantly impacted time to implementation. Lack of resources produced various obstacles that extended time necessary for centers to achieve successful implementation. Hospital characteristics, such as funding structure and type, influenced PEWS implementation time by determining their resource-availability. Prior hospital or implementation leader experience with QI, however, helped facilitate implementation by assisting implementers predict and overcome resource-related challenges.
Conclusions: Hospital characteristics impact time required to implement PEWS in resource-limited childhood cancer centers; however, prior QI experience helps anticipate and adapt to resource challenges and more quickly implement PEWS. QI training should be a component of strategies to scale-up use of evidence-based interventions like PEWS in resource-limited settings.
With modern advancements in treatments and supportive care, survival of children with cancer in high-income countries has risen to over 80% (1, 2). However, survival in low-middle-income countries (LMICs), where roughly 90% of children with cancer reside (1), remains low, between 10% and 50% (1, 3). Treatment-related toxicity (3) and infections (4) contribute to cancer mortality in resource-limited settings, where hospitals face limitations in staff and equipment needed for supportive care (5–10). There is an urgent need for evidence-based practices that reduce preventable mortality and improve global childhood cancer survival.
Pediatric Early Warning Systems (PEWS) are evidence-based interventions that allow for early detection of clinical deterioration in hospitalized children with cancer (11–13). PEWS produce multi-level advantages beyond the patient (14), such as improving interdisciplinary (15) and family communication (16), reducing hospital costs (17), and empowering providers (18). Resource-limited hospitals, however, face additional challenges implementing PEWS (19). More work is needed to understand how to address implementation challenges and support PEWS adoption in these settings.
The Consolidated Framework for Implementation Research (CFIR) describes factors influencing implementation of evidence-based interventions across five domains: inner setting, characteristics of individuals, outer setting, intervention characteristics, and implementation process (20–22), with modifications suggested for LMICs (22). CFIR constructs like culture (23), individual need (23), and teaming (23) characterize different aspects of the implementation process and their impact on its outcomes, e.g. time (24). The inner setting domain, including characteristics like resource availability and infrastructure, has been identified as particularly relevant to implementation of evidence-based interventions in resource-limited hospitals (22, 25, 26). Our prior work similarly suggested the importance of hospital characteristics on PEWS implementation (5); however, it remains unclear how these characteristics influence time required to implement PEWS, or what strategies can mitigate these effects. In this study, we evaluate the impact of hospital characteristics on PEWS implementation time in resource-limited pediatric oncology centers.
Proyecto Escala de Valoración de Alerta Temprana (EVAT) is a multicenter quality improvement (QI) collaborative in Latin America to implement PEWS (12). At participating centers, local implementation teams work with regional PEWS experts to plan, pilot, implement, and assess impact of PEWS (5, 27).
This mixed-methods study included 23 Proyecto EVAT centers across 11 Latin American countries completing PEWS implementation prior to March 2020. Time required for PEWS implementation was calculated from the start of the PEWS pilot to implementation completion.
Qualitative data collection has been described previously (5). Briefly, we selected 5 centers representing extremes of implementation time for in-depth analysis, including 3 high-performing centers (3-4 months for PEWS implementation) and 2 low-performing centers (10-11 months). At each center, two researchers conducted semi-structured interviews with 10 to 15 stakeholders involved in PEWS implementation, including hospital directors, PEWS implementation leaders, or other staff (see Supplementary Table 1 for participant demographics). Interviews were conducted virtually using WebEx, recorded, transcribed, and translated to English for analysis.
Quantitative data included measures of various center features. Initially collected on enrollment in Proyecto EVAT, site leads confirmed hospital data at the start of this study.
Consistent with Proyecto EVAT criteria, “implementation completion” was defined as having at least 2 months with high-quality PEWS use (5, 27). Centers are considered to have high-quality PEWS use when they have less than 15% in the three types of PEWS use errors: errors in PEWS scoring, PEWS algorithm non-adherence, and PEWS omissions (documented vital signs without using PEWS) (27). Implementation time was defined as time from the PEWS pilot start to implementation completion.
For analysis, research team members a priori identified hospital attributes hypothesized to be related to PEWS implementation time; these were supplemented with data from quantitative findings during analysis. Their definitions can also be found in Supplementary Table 2.
Hospital material resources included pediatric intensive care unit (PICU) capacity, physical pediatric hematology-oncology (PHO) ward space, and available finances. PICU capacity described available space in the ICU where pediatric patients were treated or the total number of PICU beds. Physical space was described by the number of beds per shared room on the PHO ward. Available finances describe available hospital economic resources for equipment and supplies needed for PEWS.
Human resources included the PHO ward nurse-to-patient ratio, number of PICU physicians, and staff turnover (how often hospital staff are replaced by new staff). In quantitative analysis, the nurse-to-patient ratio was interpreted according to the International Society of Paediatric Oncology (SIOP) nursing standards for LMICs, which recommend a ratio of one nurse to five or fewer pediatric oncology patients (28, 29). The number of PICU physicians included pediatric intensivists, fellows, and other critical care providers with expertise treating critically ill children with cancer.
Hospital characteristics encompassed funding structure (public or private), type (academic or not, specialized or general), relative PHO patient prioritization, and PHO service complexity. Specialized hospitals consisted of oncology or pediatric multidisciplinary centers while general hospitals included both general and women children’s hospitals. PHO patient prioritization conveyed the relative importance placed on PHO patient care and was quantitatively described by number of PHO beds and PHO ward structure (separate PHO ward or general pediatric ward). Service complexity was measured by the number of wards requiring PEWS implementation and number of staff requiring PEWS training.
Finally, we characterized hospitals by the participants’ self-reported prior individual or institutional experience with QI initiatives.
This study used a convergent mixed method design to investigate hospital characteristics that impact PEWS implementation time. For qualitative data, the study team developed a codebook a priori from the CFIR (20, 21) and supplemented by novel codes from iterative transcript review. Two researchers coded transcripts using the 2020 edition of MAXQDA software (VERBI Software GmbH), achieving a kappa of 0.8 to 0.9.
We used thematic content analysis focusing on the impact of hospital characteristics and QI experience on time required for PEWS implementation (Supplementary Table 3 for code definitions) Constant comparative analysis was used to explore perceived characteristics related to PEWS implementation across different hospitals and participant roles.
Quantitative analyses evaluated the relationship between hospital characteristics and PEWS implementation time. Association of PEWS implementation time with categorical and continuous covariates were analyzed using Wilcoxon rank sum test and univariate non-parametric regression analysis (Theil-Sen median estimators), respectively. P-values < 0.05 were considered statistically significant. Analyses were conducted using R 4.2.0 (https://www.r-project.org/).
We iteratively compared quantitative and qualitative results to synthesize common themes and statistical trends of how hospital characteristics related to PEWS implementation time.
Mixed methods analysis identified multiple factors associated with time required to implement PEWS, including material and human resources, hospital characteristics, and QI experience (Figure 1).
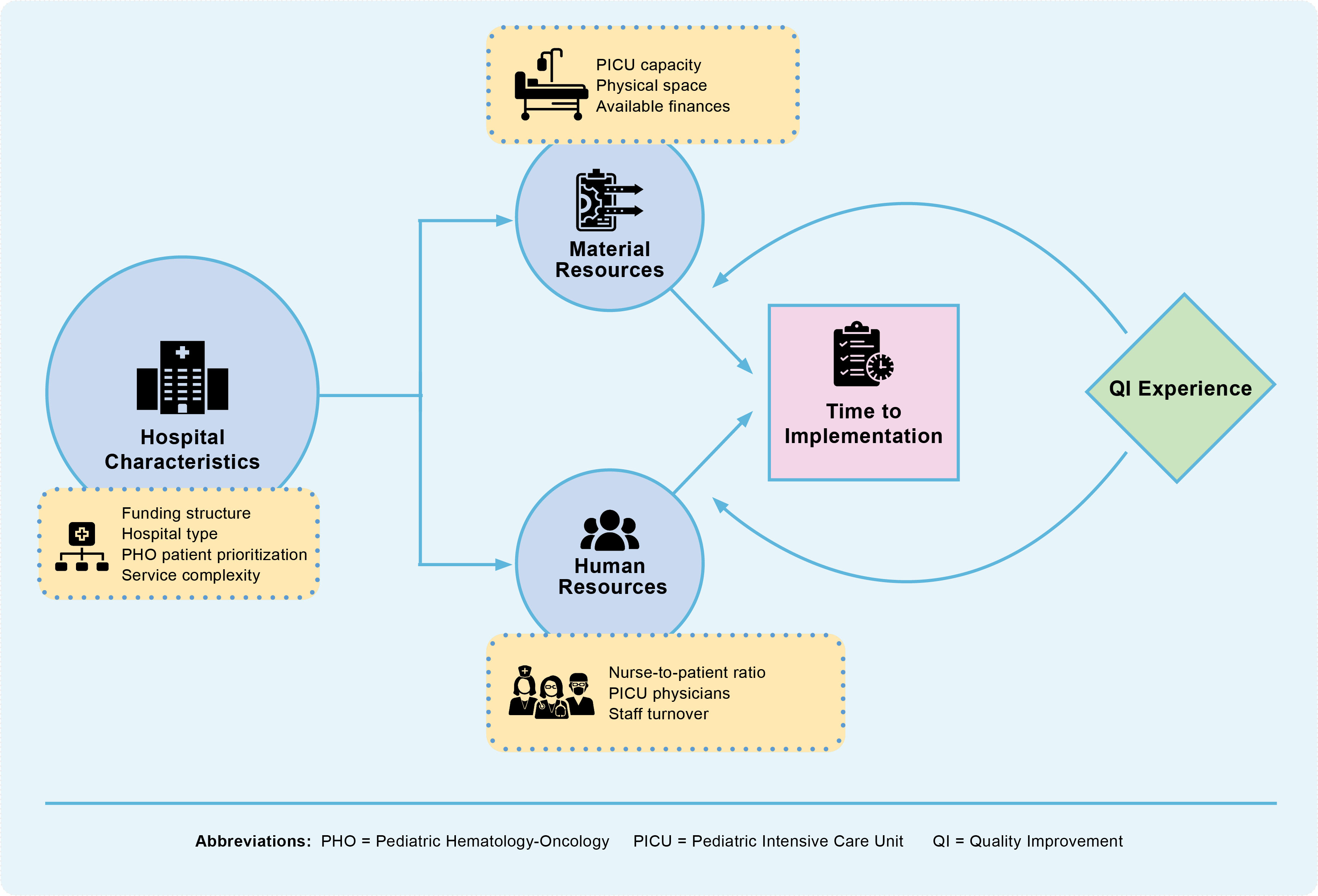
Figure 1 During implementation of Pediatric Early Warning Systems (PEWS), hospital characteristics such as funding structure and type impact resource availability, which in turn influences time required to implement PEWS. A hospital’s experience with Quality Improvement (QI) can alter this relationship between its resource availability and time to implementation, supporting faster PEWS implementation by enabling implementers to proactively identify and address PEWS barriers.
In qualitative analysis, participants described various material resource limitations that impacted time for PEWS implementation, including PICU capacity, physical space, and available finances (Table 1).
Participants at hospitals with limited PICU capacity had challenges implementing PEWS due to limited ability to transfer a patient with deterioration to a higher level-of-care: “There are few beds in the [P]ICU, so when the patient needed to be transferred because he was getting worse, there was no free space” (physician director, San Louis Potosi [SLP]). In hospitals without a dedicated PICU, pediatric patients were admitted to adult ICUs, further stretching limited resources: “it’s a multi-use ICU … we had to manage bed limitation to admit both adult patients and pediatric patients … we don’t have the necessary number of beds to treat all patients” (physician director, Lima).
Similarly, hospitals’ physical space limitation obstructed implementation of PEWS: “reduced space where we cannot monitor the child 24/7…made it difficult to find the way to the patient and move him to a space for higher supervision” (implementation leader, SLP). Additionally, financial limitations increased time required for PEWS implementation as hospitals struggled to obtain necessary medical equipment: “I wanted to do things well, but I didn’t have the equipment, and I ended up doing nothing” (implementation leader, Xalapa).
Quantitative data supported these findings (Table 2); hospitals with more PICU beds required less time for PEWS implementation (p = 0.045) and those with fewer beds per shared room implemented faster (p = < 0.0001).
In qualitative analysis, participants also identified human resource limitations that impacted PEWS implementation time, including nurse-to-patient ratios, availability of PICU physicians, and staff turnover (Table 1).
A low ratio of clinical staff to patient volume increased workload and threatened the quality of patient care, including ability to use PEWS. Nurses especially voiced this concern: “we’ve tried to have one nurse per child … taking care of one child implies a bigger effort and that couldn’t be shared if there was an extra adult or child” (nurse director, Lima). Nurses across all hospitals considered high nurse-to-patient ratios a significant barrier to PEWS use: “we have a big workload, one nurse for 8 or 9 patients, sometimes 11…the human factor is a big barrier for us … we cannot manage that” (implementation leader, El Salvador).
Similarly, hospitals lacking physicians specialized in PICU management struggled with timely evaluation and transfer of deteriorating patients, negatively affecting both patient outcomes and PEWS implementation: “We only work with one on-call intensivist … when they call saying this patient is having a cardiac arrest, even though I’d do everything in my power, I won’t be able to get there in time” (implementation leader, Cuenca). Even in settings with adequate physician staffing, a lack of specialists trained in management of critically ill children with cancer was felt to increase implementation time: “pediatrics is not our chosen specialty … Even though we have all the knowledge and experience from the courses, the health care staff don’t have the vocation or the affinity to work with children” (physician director, Lima).
In some hospitals, staff turnover, through both absenteeism and rotations, prolonged implementation as it was necessary to retrain staff in PEWS, and new staff without prior training struggled to consistently use PEWS correctly: “the new [resident] comes in … without good training, so some things may happen regarding the management that are incorrect” (physician director, SLP).
This perceived relationship between human resources and time to PEWS implementation was not observed in the quantitative analysis; neither the number of PICU physicians, nor the nurse-to-patient ratio significantly impacted implementation time (p = 0.18, Table 2 and p = 0.85, Table 3, respectively). The relationship between nurse-to-patient ratio and implementation time can be visualized with Supplementary Figure 1.
Across all hospitals, hospital characteristics such as funding structure, type, and PHO patient prioritization were seen by participants to impact PEWS implementation time by determining the relative availability of material and human resources for PEWS (Table 4).
Public hospitals rely on government resources, and participants from these settings described their centers as frequently underfunded, reducing available material and human resources necessary to quickly implement PEWS: “Our country is a poor country, our hospital is a public hospital, we lack many resources and it’s difficult to request them” (implementation leader, Lima). Conversely, participants viewed private hospitals as having greater access to human and material resources and fewer administrative barriers when requesting resources for new projects: “our hospital is a hospital that has its own resources. We were able to quickly approve it and prove that this was a sustainable project which helped the implementation go faster” (research director, Cuenca).
Similarly, academic teaching hospitals were perceived as having less resources and thus required more time for PEWS adoption. Academic hospitals faced more implementation barriers due to the prioritization of training healthcare staff, thus reducing time for initiatives like PEWS: “[Non-academic hospitals] can dedicate all the time to assisting patients. In academic hospitals, you have the excuse of preparing human resources, so it’s not feasible to develop certain types of initiatives” (quality director, SLP). In some teaching facilities, trainees with limited experience managing pediatric emergencies increased implementation time: “We don’t prepare residents in pediatric emergencies … so the hospitals that prepare residents in pediatric intensive care would have an earlier adoption than us” (quality director, SLP). Additionally, academic hospitals experienced more rotations among trainees, contributing to issues with PEWS use: “[in an academic hospital] they complete their training period, and they leave … So, it’s very variable to capture the critical state of a patient” (physician director, SLP).
Finally, participants across all centers reported that specialized hospitals, such as pediatric multidisciplinary or oncology hospitals, encountered fewer implementation barriers due to staff experience with and institutional prioritization of pediatric and/or oncology patients: “Since we are an oncology hospital … we try to be updated and have good reception for those programs that strengthen our patient’s safety” (nurse director, Xalapa). General hospitals were felt to have other competing priorities and less experience with pediatric oncology, resulting in fewer resources for projects like PEWS: “This generated some rejection because our [general] hospital has limited resources and we would need oximeters for children” (implementation leader, Lima).
Of the 23 participating hospitals, only 2 were private and 3 were mixed private/public; in quantitative analysis, we did not find an association between funding structure and implementation time (p = 0.94, Table 3). Similarly, only 1 hospital was non-academic, preventing analysis of the relationship between academic status and implementation time. Aligned with qualitative findings, however, quantitative analysis demonstrated that specialized hospitals implemented faster than general hospitals (p = 0.025, Table 3). Hospital prioritization of PHO patients was also significantly related to PEWS implementation time; hospitals with more PHO inpatient beds implemented faster (p = 0.039, Table 2), and those with a dedicated PHO ward trended towards shorter implementation times (p = 0.071, Table 3).
In quantitative analysis, service complexity emerged as an additional barrier to PEWS implementation. Hospitals with more than one PHO ward requiring PEWS implementation and those with more nurses and physicians requiring PEWS training required more time for PEWS implementation (p = 0.013, Table 3 and p = 0.0014, Table 2, respectively). Further conceptualization of various hospital characteristics impact on implementation time are available in Supplementary Figures 2A–D respectively.
Prior QI experience, both at the hospital and among implementation team members, was seen by participants to facilitate PEWS implementation by allowing centers to more easily overcome existing resource limitations (Table 4). Examples of these experiences included involvement with initiatives related to central venous catheters, decreasing hospitalization times, and shortening time to antibiotic administration in febrile neutropenia.
Past experience with QI was seen to facilitate PEWS implementation by allowing centers to anticipate and proactively address potential implementation barriers: “I think the knowledge exchange allows you to identify the difficulties you have in your center and learn from the experience of other centers” (physician director, Lima). Nurses also felt empowered by QI experience to participate in PEWS implementation as members of the multidisciplinary team: “since I’m a nurse I know how to take care of a patient, that [and to learn about quality] facilitated my support to conducting that project [PEWS] and to my colleagues” (nurse director, El Salvador).
Conversely, hospitals without QI experience struggled with implementation and were initially intimidated by the PEWS project: “it was something big … maybe we wouldn’t be able to accomplish it … maybe most of us felt the same way about not being able to accomplish it” (implementation leader, Cuenca). Despite most hospitals lacking prior QI experience, all eventually achieved successful PEWS implementation, often applying QI methodology learned in Proyecto EVAT: “At the beginning, it was kind of a barrier because we were afraid of the unknown, but then we were very successful” (implementation leader, Cuenca). Successfully implementing PEWS also empowered hospitals to apply their experience to future improvement initiatives: “A lot of us have started to get involved in other quality improvement projects that maybe didn’t exist before PEWS, it has helped us and pushed us to work” (implementation leader, Lima).
Most hospitals lacked QI experience prior to PEWS implementation (n = 17, 74%, Table 3). Supporting qualitative findings, quantitative analysis demonstrated hospitals without QI experience trended towards longer PEWS implementation times (6.5 months vs. 4.5 months, p = 0.13, Table 3). This relationship is also displayed in Supplementary Figure 3.
This study analyzed the relationship between hospital characteristics and PEWS implementation time in resource-limited settings. Fixed hospital characteristics, like funding structure and type, determined the relative availability of resources for PEWS and impacted time needed for implementation. Previous QI experience, however, either at the center or among members of the implementation team, mitigated these barriers by empowering centers to proactively anticipate and overcome implementation challenges. In centers without prior QI experience, implementation leaders leveraged training obtained through Proyecto EVAT to successfully implement PEWS.
Our findings are consistent with prior work in LMICs demonstrating the impact of resource availability on QI and intervention implementation (7, 8), including the barriers of staff turnover (26, 30), large organization size (31), and poor infrastructure (25). Similarly, the importance of hospital and staff specialization have been identified as important to the quality and capacity of pediatric onco-critical care (10, 32). Additionally, a systematic review evaluating the use of the CFIR in LMICs proposed a new domain, “Characteristics of Systems,” that affects organizational policies to produce changes to the inner setting (hospital) domain (22). This relationship reflects the impact of hospital characteristics (e.g., funding structure) on resource-availability we observed in this study.
Although data on the impact of QI collaboratives in LMICs is conflicting (33), our work supports findings that including QI training, as is done in Proyecto EVAT, can improve collaborative effectiveness (33, 34). In this study, few centers or implementation team members reported previous experience with QI, highlighting the importance of incorporating QI training into programs to scale-up interventions in resource-limited hospitals. Our findings suggest that QI training also provides additional benefits, including team empowerment and motivation to introduce other improvement projects, potentially resulting in more broad impact on patient outcomes.
Centers in our study more quickly completed implementation when they adapted the PEWS implementation process to the specific characteristics of their institution and resource-level. These findings provide actionable recommendations for clinicians, hospital leadership, and researchers wishing to implement PEWS or other QI interventions in resource-limited clinical settings. For clinicians, we recommend an iterative implementation strategy that includes aspects of successful methodologies from other resource-constrained sites and tailoring them to the needs of their center. This can include formal QI methods such as plan-do-study-act (PDSA) cycles, stakeholder analyses, and process mapping, among others. Hospital leadership looking to foster a culture of QI in their hospital should support local QI efforts and promote QI training options within the center to grow institutional and clinician capacity for QI. For researchers and public health experts leading collaborative efforts to scale-up evidence-based interventions, we recommend including training in QI methodology to better enable clinicians to leverage their knowledge to support improvement initiatives.
This study has several limitations. The relatively small sample size (23 centers) and low frequency of some variables (e.g., private funding structure) limited the power of our quantitative analysis to identify true relationships between some variables and PEWS implementation time. Our mixed methods design, however, supplemented this quantitative data with in-depth qualitative analysis from a diverse group of stakeholders. The synthesis between quantitative and qualitative findings strengthened our study and enriched the analysis of the relationship between hospital characteristics and PEWS implementation. At the time of this study, all Proyecto EVAT centers had successfully implemented PEWS (27). As a result, we used time needed for implementation, rather than implementation success or failure, as the implementation outcome. Implementation time is a relatively newly described implementation outcome (24), and this study further contributes to this emerging literature. Finally, this study focused on implementation of one intervention in pediatric oncology centers, potentially limiting generalizability of our findings to other interventions and settings. Future work should more broadly evaluate the impact of hospital characteristics on implementation of other interventions to improve childhood cancer care and explore the impact of external factors (e.g., the COVID pandemic) on intervention implementation and sustainability in resource-limited settings (35). This includes evaluation of the impact of changes in resources to promote intervention use over time and study of associated intervention costs and cost-benefits and their impact on sustainability.
This study describes how hospital characteristics impact time required for successful PEWS implementation in resource-limited pediatric oncology centers, with past hospital or individual QI experience mitigating implementation challenges by empowering implementation teams to proactively overcome identified barriers. Importantly, lack of prior QI experience can be addressed through teaching QI methods as part of the implementation process. These findings can be used by clinicians and researchers to conduct pre-implementation assessments to anticipate implementation challenges and guide future collaborative initiatives to scale up interventions that improve outcomes of children with cancer in hospitals of all resource-levels.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was approved by the institutional review board of St. Jude Children’s Research Hospital as an exempt, minimal-risk study. Additional approvals were obtained by participating centers as needed. As an exempt study, written participant consent was waived; verbal consent was provided at the start of each interview.
AA, DG developed the idea. MP-T, SG, PE, HM-T, AG-R, MA, CB, ZC, CH, MJ, JJL, AM, EM, EPe, EPi collected the data. AA provided supervision. FA and AA conducted the data analyses. FA, AA, DG drafted manuscript and prepared the tables and figures. All authors contributed to the interpretation of the findings, the editing of the article, and the approval of the final submitted version.
This study was funded by the American Lebanese-Syrian Associated Charities (ALSAC). AA was funded by the Conquer Cancer Foundation Global Oncology Young Investigator Award for this work. FA was funded through the St. Jude Children’s Research Hospital Pediatric Oncology Education Program via grant R25CA23944 from the National Cancer Institute. These funders were not involved in the design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
We thank the PEWS implementation teams at all Proyecto EVAT centers, including those who participated in this study, Marcela Hill for the figure design, and the Proyecto EVAT Steering Committee for oversight of this work
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2023.1122355/full#supplementary-material
1. Bhakta N, Force LM, Allemani C, Atun R, Bray F, Coleman MP, et al. Childhood cancer burden: A review of global estimates. Lancet Oncol (2019) 20(1):e42–53. doi: 10.1016/S1470-2045(18)30761-7
2. Rodriguez-Galindo C, Friedrich P, Alcasabas P, Antillon F, Banavali S, Castillo L, et al. Toward the cure of all children with cancer through collaborative efforts: Pediatric oncology as a global challenge. J Clin Oncol Off J Am Soc Clin Oncol (2015) 33(27):3065–73. doi: 10.1200/JCO.2014.60.6376
3. Agulnik A, Cárdenas A, Carrillo AK, Bulsara P, Garza M, Alfonso Carreras Y, et al. Clinical and organizational risk factors for mortality during deterioration events among pediatric oncology patients in Latin America: A multicenter prospective cohort. Cancer (2021) 127(10):1668–78. doi: 10.1002/cncr.33411
4. Shah SC, Kayamba V, Peek RM, Heimburger D. Cancer control in low- and middle-income countries: Is it time to consider screening? J Glob Oncol (2019) 5:JGO.18.00200. doi: 10.1200/JGO.18.00200
5. Agulnik A, Ferrara G, Puerto-Torres M, Gillipelli SR, Elish P, Muniz-Talavera H, et al. Assessment of barriers and enablers to implementation of a pediatric early warning system in resource-limited settings. JAMA Netw Open (2022) 5(3):e221547. doi: 10.1001/jamanetworkopen.2022.1547
6. Muttalib F, González-Dambrauskas S, Lee JH, Steere M, Agulnik A, Murthy S, et al. Pediatric emergency and critical care resources and infrastructure in resource-limited settings: A multicountry survey. Crit Care Med (2021) 49(4):671–81. doi: 10.1097/CCM.0000000000004769
7. Agyeman-Duah JNA, Theurer A, Munthali C, Alide N, Neuhann F. Understanding the barriers to setting up a healthcare quality improvement process in resource-limited settings: A situational analysis at the medical department of kamuzu central hospital in Lilongwe, Malawi. BMC Health Serv Res (2014) 14:1. doi: 10.1186/1472-6963-14-1
8. Kakyo TA, Xiao LD. Nurse managers’ experiences in continuous quality improvement in resource-poor healthcare settings. Nurs Health Sci (2017) 19(2):244–9. doi: 10.1111/nhs.12338
9. Maru DSR, Andrews J, Schwarz D, Schwarz R, Acharya B, Ramaiya A, et al. Crossing the quality chasm in resource-limited settings. Glob Health (2012) 8:41. doi: 10.1186/1744-8603-8-41
10. Arias AV, Sakaan FM, Puerto-Torres M, Al Zebin Z, Bhattacharyya P, Cardenas A, et al. Development and pilot testing of PROACTIVE: A pediatric onco-critical care capacity and quality assessment tool for resource-limited settings. Cancer Med (2022). doi: 10.1002/cam4.5395
11. Agulnik A, Forbes PW, Stenquist N, Rodriguez-Galindo C, Kleinman M. Validation of a pediatric early warning score in hospitalized pediatric oncology and hematopoietic stem cell transplant patients. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc (2016) 17(4):e146–153. doi: 10.1097/PCC.0000000000000662
12. Agulnik A, Méndez Aceituno A, Mora Robles LN, Forbes PW, Soberanis Vasquez DJ, Mack R, et al. Validation of a pediatric early warning system for hospitalized pediatric oncology patients in a resource-limited setting. Cancer (2017) 123(24):4903–13. doi: 10.1002/cncr.30951
13. Brown SR, Martinez Garcia D, Agulnik A. Scoping review of pediatric early warning systems (PEWS) in resource-limited and humanitarian settings. Front Pediatr (2018) 6:410. doi: 10.3389/fped.2018.00410
14. Agulnik A, Mora Robles LN, Forbes PW, Soberanis Vasquez DJ, Mack R, Antillon-Klussmann F, et al. Improved outcomes after successful implementation of a pediatric early warning system (PEWS) in a resource-limited pediatric oncology hospital. Cancer (2017) 123(15):2965–74. doi: 10.1002/cncr.30664
15. Graetz D, Kaye EC, Garza M, Ferrara G, Rodriguez M, Soberanis Vásquez DJ, et al. Qualitative study of pediatric early warning systems’ impact on interdisciplinary communication in two pediatric oncology hospitals with varying resources. JCO Glob Oncol (2020) 6:1079–86. doi: 10.1200/GO.20.00163
16. Gillipelli SR, Kaye EC, Garza M, Ferrara G, Rodriguez M, Soberanis Vasquez DJ, et al. Pediatric early warning systems (PEWS) improve provider-family communication from the provider perspective in pediatric cancer patients experiencing clinical deterioration. Cancer Med (2022). doi: 10.1002/cam4.5210
17. Agulnik A, Antillon-Klussmann F, Soberanis Vasquez DJ, Arango R, Moran E, Lopez V, et al. Cost-benefit analysis of implementing a pediatric early warning system at a pediatric oncology hospital in a low-middle income country. Cancer (2019) 125(22):4052–8. doi: 10.1002/cncr.32436
18. Graetz DE, Giannars E, Kaye EC, Garza M, Ferrara G, Rodriguez M, et al. Clinician emotions surrounding pediatric oncology patient deterioration. Front Oncol (2021) 11:626457. doi: 10.3389/fonc.2021.626457
19. van der Fluit KS, Boom MC, Brandão MB, Lopes GD, Barreto PG, Leite DCF, et al. How to implement a PEWS in a resource-limited setting: A quantitative analysis of the bedside-PEWS implementation in a hospital in northeast Brazil. Trop Med Int Health (2021) 26(10):1240–7. doi: 10.1111/tmi.13646
20. The consolidated framework for implementation research – technical assistance for users of the CFIR framework (2022). Available at: https://cfirguide.org/.
21. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement Sci (2009) 4(1):50. doi: 10.1186/1748-5908-4-50
22. Means AR, Kemp CG, Gwayi-Chore MC, Gimbel S, Soi C, Sherr K, et al. Evaluating and optimizing the consolidated framework for implementation research (CFIR) for use in low- and middle-income countries: A systematic review. Implement Sci IS (2020) 15(1):17. doi: 10.1186/s13012-020-0977-0
23. Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated consolidated framework for implementation research based on user feedback. Implement Sci (2022) 17(1):75. doi: 10.1186/s13012-021-01181-5
24. Proctor E, Ramsey AT, Saldana L, Maddox TM, Chambers DA, Brownson RC. FAST: A framework to assess speed of translation of health innovations to practice and policy. Glob Implement Res Appl (2022) 2(2):107–19. doi: 10.1007/s43477-022-00045-4
25. Gimbel S, Rustagi AS, Robinson J, Kouyate S, Coutinho J, Nduati R, et al. Evaluation of a systems analysis and improvement approach to optimize prevention of mother-To-Child transmission of HIV using the consolidated framework for implementation research. J Acquir Immune Defic Syndr (2016) 72 Suppl 2:S108–116. doi: 10.1097/QAI.0000000000001055
26. Wu S, Tannous E, Haldane V, Ellen ME, Wei X. Barriers and facilitators of implementing interventions to improve appropriate antibiotic use in low- and middle-income countries: A systematic review based on the consolidated framework for implementation research. Implement Sci IS (2022) 17:30. doi: 10.1186/s13012-022-01209-4
27. Agulnik A, Gonzalez Ruiz A, Muniz-Talavera H, Carrillo AK, Cárdenas A, Puerto-Torres MF, et al. Model for regional collaboration: Successful strategy to implement a pediatric early warning system in 36 pediatric oncology centers in Latin America. Cancer (2022) 128(22):4004–16. doi: 10.1002/cncr.34427
28. Baseline nursing standards | SIOP (2022). Available at: https://siop-online.org/baseline-nursing-standards/.
29. Sullivan CE, Morrissey L, Day SW, Chen Y, Shirey M, Landier W. Predictors of hospitals’ nonachievement of baseline nursing standards for pediatric oncology. Cancer Nurs (2020) 43(4):E197–206. doi: 10.1097/NCC.0000000000000688
30. Edmondson AC, Bohmer RM, Pisano GP. Disrupted routines: Team learning and new technology implementation in hospitals. Adm Sci Q (2001) 46(4):685–716. doi: 10.2307/3094828
31. Walston SL, Kimberly JR, Burns LR. Institutional and economic influences on the adoption and extensiveness of managerial innovation in hospitals: The case of reengineering. Med Care Res Rev MCRR (2001) 58(2):194–228. doi: 10.1177/107755870105800203
32. Arias AV, Garza M, Murthy S, Cardenas A, Diaz F, Montalvo E, et al. Quality and capacity indicators for hospitalized pediatric oncology patients with critical illness: A modified delphi consensus. Cancer Med (2020) 9(19):6984–95. doi: 10.1002/cam4.3351
33. Zamboni K, Baker U, Tyagi M, Schellenberg J, Hill Z, Hanson C. How and under what circumstances do quality improvement collaboratives lead to better outcomes? a systematic review. Implement Sci (2020) 15(1):27. doi: 10.1186/s13012-020-0978-z
34. Garcia-Elorrio E, Rowe SY, Teijeiro ME, Ciapponi A, Rowe AK. The effectiveness of the quality improvement collaborative strategy in low- and middle-income countries: A systematic review and meta-analysis. PloS One (2019) 14(10):e0221919. doi: 10.1371/journal.pone.0221919
35. Agulnik A, Malone S, Puerto-Torres M, Gonzalez-Ruiz A, Vedaraju Y, Wang H, et al. Reliability and validity of a Spanish-language measure assessing clinical capacity to sustain paediatric early warning systems (PEWS) in resource-limited hospitals. BMJ Open (2021) 11(10):e053116. doi: 10.1136/bmjopen-2021-053116
Keywords: Pediatric Early Warning Systems (PEWS), quality improvement collaborative (QIC), implementation science, pediatric oncology, resource-limited settings, global health
Citation: Abutineh F, Graetz DE, Muniz-Talavera H, Ferrara G, Puerto-Torres M, Chen Y, Gillipelli SR, Elish P, Gonzalez-Ruiz A, Alfonso Carreras Y, Alvarez S, Arce Cabrera D, Arguello Vargas D, Armenta Cruz M, Barra C, Calderon Sotelo P, Carpio Z, Chavez Rios M, Covarrubias D, de Leon Vasquez L, Diaz Coronado R, Fing Soto EA, Gomez-Garcia W, Hernandez C, Juarez Tobias MS, Leon E, Loeza Oliva JdJ, Mendez A, Miller K, Montalvo Cozar E, Negroe Ocampo NdC, Penafiel E, Pineda E, Rios L, Rodriguez Ordonez E, Soto Chavez V, Devidas M and Agulnik A (2023) Impact of hospital characteristics on implementation of a Pediatric Early Warning System in resource-limited cancer hospitals. Front. Oncol. 13:1122355. doi: 10.3389/fonc.2023.1122355
Received: 12 December 2022; Accepted: 17 April 2023;
Published: 03 May 2023.
Edited by:
Monica Kleinman, Boston Children’s Hospital and Harvard Medical School, United StatesReviewed by:
Hasan Yusefzadeh, Urmia University of Medical Sciences, IranCopyright © 2023 Abutineh, Graetz, Muniz-Talavera, Ferrara, Puerto-Torres, Chen, Gillipelli, Elish, Gonzalez-Ruiz, Alfonso Carreras, Alvarez, Arce Cabrera, Arguello Vargas, Armenta Cruz, Barra, Calderon Sotelo, Carpio, Chavez Rios, Covarrubias, de Leon Vasquez, Diaz Coronado, Fing Soto, Gomez-Garcia, Hernandez, Juarez Tobias, Leon, Loeza Oliva, Mendez, Miller, Montalvo Cozar, Negroe Ocampo, Penafiel, Pineda, Rios, Rodriguez Ordonez, Soto Chavez, Devidas and Agulnik. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Asya Agulnik, YXN5YS5hZ3VsbmlrQHN0anVkZS5vcmc=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.