- Department of Urology, Hunan Provincial People’s Hospital, The First Affiliated Hospital of Hunan Normal University, Changsha, Hunan, China
Ectopic hepatocellular carcinoma (EHCC) originates from the ectopic liver, which refers to a liver organ or tissue unrelated to surrounding tissues. EHCC is a rare disease that lacks specific clinical signs, and preoperative diagnosis is often difficult. In a 61-year-old male patient with positive hepatitis B virus antibody, abdominal contrast-enhanced computed tomography scan showed a large heterogenously enhancing mass both on arterial and portal venous phase imaging arising from the right adrenal gland. Similar enhancement features were seen on magnetic resonance imaging. Serum potassium, aldosterone, cortisol, and plasma metanephrines were normal. The tumor markers of serum alpha-fetoprotein and alpha-fetoprotein-L3% were increased to 23.69 ng/mL and 82.1%, respectively. Exploratory laparotomy was performed and operative findings showed that the retroperitoneal tumor was disconnected from the right kidney and the liver, but invaded the right adrenal gland. Immunohistochemical examination showed that Arginase-1 was positive expression, and the retroperitoneal tumor was finally diagnosed as EHCC. We report a rare EHCC with adrenal infiltration that is difficult to diagnose preoperatively and mimics a retroperitoneal tumor or adrenal tumor, and we present a review of the literature on EHCC case reports.
Introduction
Ectopic hepatocellular carcinoma (EHCC) is defined as hepatocellular carcinoma arising from the hepatic parenchyma located in an extrahepatic organ or tissue (1). It is reported that the incidence of ectopic liver during laparoscopy or autopsy ranges from 0.24% to 0.47% (2). Ectopic liver can be located in various organs or tissues near the liver, such as gallbladder, adrenal gland, pancreas, peritoneum and thorax (3–6). Due to the variable location, the clinical signs of EHCC are still not fully elucidated. Thus, EHCC is a very rare tumor disease with variable location and lack of specific clinical signs, which increases the difficulty of accurate preoperative diagnosis. Here, we report a case of EHCC with adrenal infiltration mimicking a retroperitoneal tumor or adrenal tumor and review the literature concerning EHCC.
Case presentation
The case was a 61-year-old male patient with positive hepatitis B virus antibody (HBV-DNA was 2.174 × 102), and he presented with abdominal distention and hyporexia for one week. Due to abdominal distension and hyporexia, the patient went to a nearby outpatient clinic, and abdominal ultrasound examination showed a large solid mass with mixed echogenicity. The patient had no history of hypertension, diabetes, cardiovascular and cerebrovascular diseases, and no history of surgery. His abdomen was soft and flat. There was mild tenderness in the right upper quadrant, but Murphy’s sign was negative. The liver was palpable 2 cm below the costal margin due to the push of the mass. The patient lost 5 kg in weight last month. (Eastern Cooperative Oncology Group: 0).
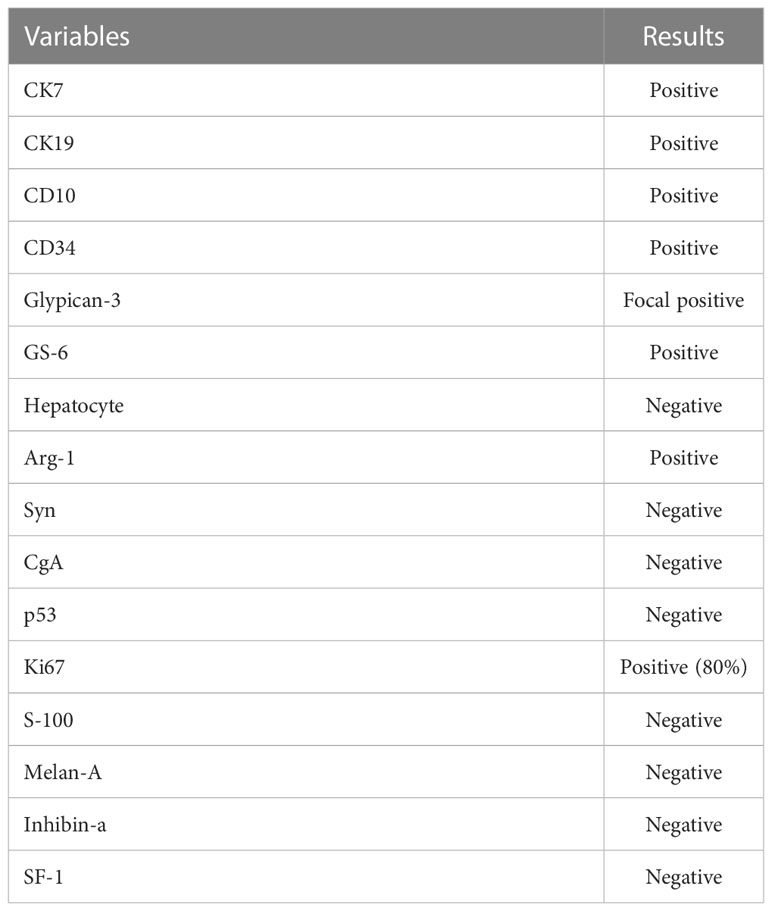
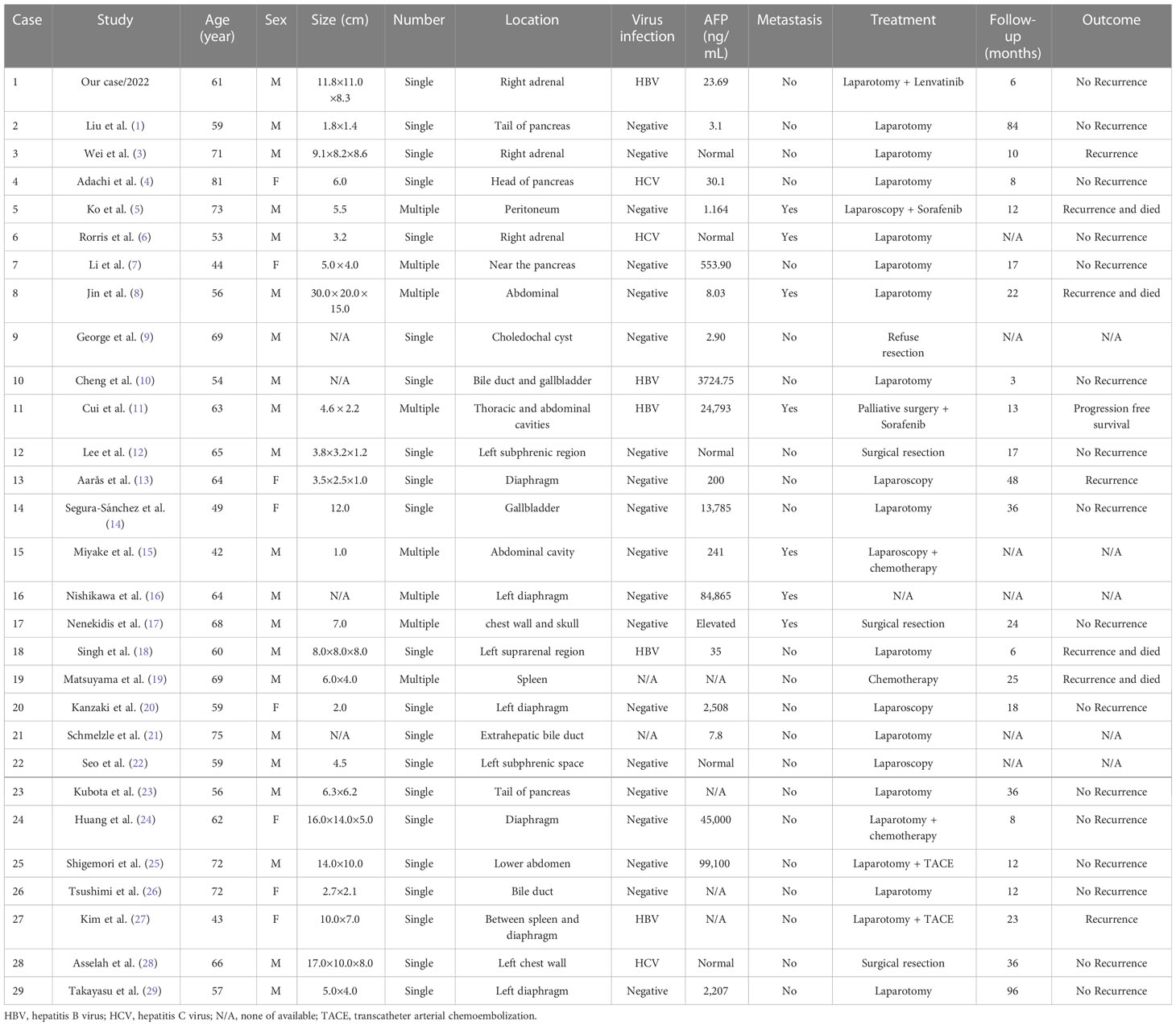
Abdominal contrast-enhanced computed tomography (CT) scan showed that the retroperitoneal tumor (11.8 × 11.0 × 8.3 cm) located in the right adrenal region, with obvious enhancement in arterial phase and continuous enhancement in venous phase (Figures 1A, B). Magnetic resonance imaging (MRI) displayed uneven enhancement in arterial phase and no abnormal signal focus in hepatobiliary phase (Figures 1C, D). On the laboratory tests, because the tumor was located in the adrenal region, serum potassium, aldosterone, cortisol, and plasma metanephrines were tested, and the results were normal. Serum alpha-fetoprotein (AFP) and AFP-L3% were 23.69 ng/mL and 82.1%, respectively.
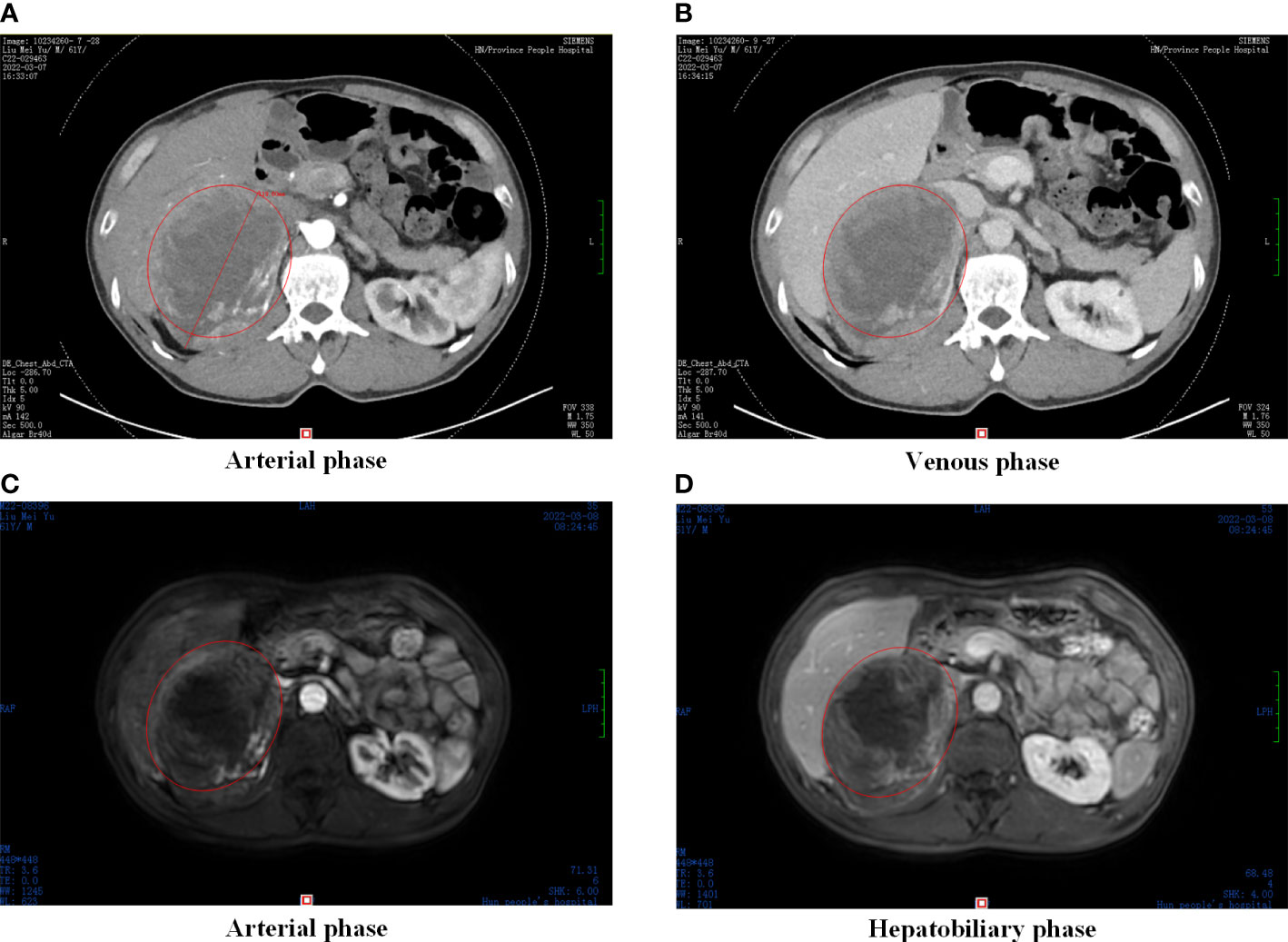
Figure 1 Preoperative abdominal CT and MRI. (A) CT scan in arterial phase, (B) CT scan in venous phase; (C) MRI scan in arterial phase, (D) MRI scan in hepatobiliary phase. Abdominal CT and MRI images showed an oval and smoothly mass located in the liver-kidney space (red circle).
The patient underwent an exploratory laparotomy to remove the tumor from an unknown primary organ in the adrenal region. On exploration, there was a large encapsulated oval solid tumor occupying the right retroperitoneal cavity, adjacent to the liver and right kidney, and infiltrating the adrenal tissue. The blood supply of the tumor is supplied by small branches of the right renal artery and abdominal aorta, and the adjacent liver, right kidney, and inferior vena cava are compressed and displaced by the tumor. The gross size of the resected specimen was about 16.0 × 14.0 × 10.0 cm and encapsulated in membrane, and the cut surface was reddish-yellow with intratumoral hemorrhage. Histopathological examination of tumor specimen showed that there were a large number of hepatoma cells arranged in beam, cord and nest shapes (Figure 2). Golden yellow adrenal tissue can be seen on the surface of the mass, and the pathological results suggest that cancer cells invade the adrenal gland. Pathological examination of the tumor specimen did not reveal any significant histological structure of the biliary tract. Therefore, it is speculated that ectopic hepatocytes may not have normal bile secretion functions, and this variation contributes to the degeneration or even canceration of hepatocytes. On immunohistochemical staining of the tumor specimen, Hepatocyte and Glypican-3 were negative and focal positive, respectively, but Arginase-1 (Arg-1) was positive. Moreover, GS-6 was positive, Ki67 was partly positive, Inhibin-a was negative, S-100 was negative, p53 was negative, and Melan-A was negative (Table 1). On postoperative laboratory tests, the levels of AFP and AFP-L3% had decreased to 5.98 ng/mL and 35.4%, respectively. Finally, we diagnosed the retroperitoneal tumor as EHCC. After the diagnosis of EHCC by histopathological examination, the patient received adjuvant treatment with the PD-1 blocker sintilimab and lenvatinib. Twelve months after operation, abdominal contrast-enhanced CT scan showed postoperative changes, and no tumor recurrence was found (Figure 3). Currently, twelve months have passed, the patient is still alive without recurrence.
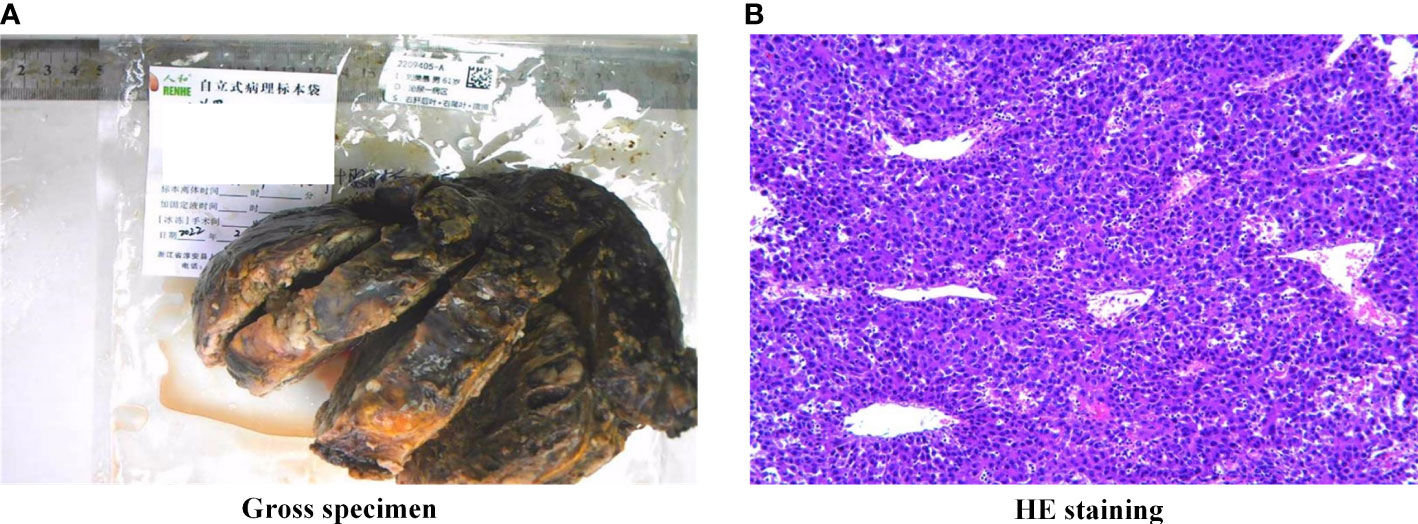
Figure 2 Gross specimen and HE staining. (A) Macroscopic features of the excised hepatocellular carcinoma demonstrating a solid tumor with a fibrous capsule and intratumoral hemorrhage, (B) HE staining of the tumor confirmed poorly differentiated carcinoma morphologically, magnification × 100. The hepatoma cells were large, polygonal, rich in cytoplasm and red staining, and were diagnosed as massive beam and cord liver cancer.

Figure 3 Postoperative abdominal CT. (A) CT scan in plain scanning, (B) CT scan in arterial phase. Postoperative abdominal CT images showed no new mass in the liver-kidney space (red circle).
Discussion
EHCC is a rare carcinomas defined as an HCC arising from ectopic liver organ or tissue. The incidence rate of ectopic liver is about 0.24% to 0.47%. When we searched for “ectopic hepatocellular carcinoma” as a “Text Word” in PubMed, only 28 full-text case reports written in English were obtained (Table 2) (1, 3–29). Ectopic liver tissue can occur in the adrenal gland, pancreas, peritoneum, gallbladder, bile duct, thoracic cavity, abdominal cavity, diaphragm, spleen, and chest wall, of which the diaphragm is the most common site (12, 13, 16, 20, 24, 27, 29).
Of the 29 patients including this case, 26 patients underwent surgery treatment (1, 3–8, 10–15, 17, 18, 20–29) and two patients did not undergo surgery due to serious complications (9, 19). Traditional laparotomy and laparoscopy can be performed as the surgical methods, and seven patients received adjuvant therapy after surgery (5, 11, 15, 24, 25, 27). For unresectable hepatocellular carcinoma, lenvatinib or sorafenib can be used as targeted drugs for adjuvant therapy in EHCC (30). After surgical resection alone or combined with adjuvant therapy, EHCC patients have a relatively good oncological prognosis, with 7/23 (30.4%) patients experiencing tumor recurrence. Therefore, if the patient does not have surgical contraindications, surgery should be recommended first. During follow-up, the clinical features of the tumors in the dead patients were multiple or relatively large in size. Thus, for patients with multiple or large tumors, a more rigorous follow-up plan should be developed to detect tumor recurrence early.
In previous case reports, three out of 28 tumors were located in the adrenal gland, but only one of them was located in the left adrenal gland region, while this case was located in the right adrenal gland region (3, 6, 18). Because the tumor is located in the adrenal region, it is difficult to diagnose EHCC before surgery, and it is easy to be misdiagnosed as an adrenal tumor. The tumor in this case invaded the adrenal tissue, which increased the difficulty of preoperative diagnosis. For EHCC located in the adrenal region, preoperative adrenal-related hormone testing is needed to determine whether the tumor has endocrine function. Except for one patient who did not undergo endocrine evaluation due to hemodynamic compromise and type I respiratory failure requiring emergency surgery, the other three patients underwent adrenal endocrine function evaluation. According to the test results, serum potassium, aldosterone, cortisol, and plasma metanephrines were normal, and the adrenal gland had no abnormal endocrine function (3, 6, 18).
Conclusion
Preoperative diagnosis of EHCC is usually very difficult. The tumor located in the adrenal region further increase the difficulty of diagnosis, and it is easy to be misdiagnosed as an adrenal tumor. Adrenal-related hormone testing can be performed to evaluate tumor endocrine function if radiographic studies reveal a tumor in the adrenal region. Early surgical treatment of EHCC will provide good long-term outcomes.
Patient perspective
His family is pleased that the patient is alive, and that the patient’s liver and kidney are protected during the operation. Both the patient and his families feel that if this exploratory laparotomy could ensure complete tumor resection and minimize damage to surrounding organs, they would like to choose such a surgical treatment strategy.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Hunan Provincial People’s Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
Author contributions
Manuscript writing: YY and YL; Clinical case diagnosis and treatment: YY, QL, and YL; Data collection and literature resarch: YY, ZL, and CW; Manuscript review and revision: YY and QL. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by by the Natural Science Foundation of Hunan Province (No.2021JJ40513), Hunan Provincial Inclusive Policy and Innovative Environment Construction Plan (2020SK50902), Excellent Youth Project of Hunan Provincial Department of Education (22B0099), and Doctoral Foundation of Hunan Provincial People’s Hospital (No.BSJJ202116).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Liu Q, Li J, Pan Y, Zheng X, Gao B. Challenge in diagnosis and treatment of ectopic hepatocellular carcinoma: a case report and literature review. Front Surg (2022) 9:827006. doi: 10.3389/fsurg.2022.827006
2. Martinez CA, de Resende HC Jr, Rodrigues MR, Sato DT, Brunialti CV, Palma RT. Gallbladder-associated ectopic liver: a rare finding during a laparoscopic cholecystectomy. Int J Surg Case Rep (2013) 4(3):312–5. doi: 10.1016/j.ijscr.2013.01.006
3. Wei N, Wong V, Matz A, Vemulakonda LA, Wang X, Phillips J. Ectopic hepatocellular carcinoma presenting as a right adrenal mass with IVC thrombus: case report and review of the literature. Urol Case Rep (2021) 40:101900. doi: 10.1016/j.eucr.2021.101900
4. Adachi Y, Hayashi H, Yusa T, Takematsu T, Matsumura K, Higashi T, et al. Ectopic hepatocellular carcinoma mimicking a retroperitoneal tumor: a case report. World J Gastroenterol (2020) 26(18):2268–75. doi: 10.3748/wjg.v26.i18.2268
5. Ko YL, Takata K, Tanaka T, Ohishi J, Takeshita M, Yamauchi R, et al. Unresectable ectopic hepatocellular carcinoma treated with sorafenib. Case Rep Gastroenterol (2020) 14(1):226–33. doi: 10.1159/000506929
6. Rorris FP, Tyrovolas K, Theodosis A, Tsamatsoulis M, Charitos C. Ectopic hepatocellular carcinoma in the adrenal gland with inferior vena cava thrombosis and right atrial extension. J Card Surg (2020) 35(6):1380–2. doi: 10.1111/jocs.14594
7. Li Z, Wu X, Wen T, Li C, Peng W. Multiple ectopic hepatocellular carcinomas in the pancreas: a case report. Med (Baltimore) (2017) 96(30):e6747. doi: 10.1097/MD.0000000000006747
8. Jin R, Yu Q, Liang X. Ectopic hepatocellular carcinoma manifesting multiple abdominal masses: a case report. Med (Baltimore) (2017) 96(48):e8968. doi: 10.1097/MD.0000000000008968
9. George NE, Raghavapuram S, Banerjee D, Al-Shoha M, Fedda F, Tharian B. Ectopic hepatocellular carcinoma within a choledochal cyst diagnosed using single-operator digital cholangioscopy. Am J Gastroenterol (2017) 112(8):1347–8. doi: 10.1038/ajg.2017.143
10. Cheng MQ, Zeng D, Huang H, Tang XF, Xu ZF. Ectopic hepatocellular carcinoma occurring in the bile duct and extending to the gallbladder. Ultrasound Q (2017) 33(1):58–61. doi: 10.1097/RUQ.0000000000000232
11. Cui T, Diao X, Chen X, Huang S, Sun J. A case report: delayed high fever and maculopapules during sorafenib treatment of ectopic hepatocellular carcinoma. BMC Cancer (2016) 16:543. doi: 10.1186/s12885-016-2590-9
12. Lee JY, Kim KH, Kang MS, Kim KH. Ectopic hepatocellular carcinoma arising from the peritoneum in a patient with a history of oropharyngeal cancer: a case report. Case Rep Oncol (2015) 8(3):456–60. doi: 10.1159/000441020
13. Aarås AM, Reitan-Gjersøe TA, Waage A, Mala T, Edwin B, Løberg EM, et al. Laparoscopic resection of recurrent ectopic hepatocellular carcinoma: a case report with review of the literature and guidelines for follow-up. Int J Surg Case Rep (2015) 17:92–5. doi: 10.1016/j.ijscr.2015.10.014
14. Segura-Sánchez J, Torres-Domínguez Y, Ruiz-García E. Ectopic hepatocellular carcinoma in the gallbladder. Rev Esp Enferm Dig (2014) 106(2):149–50. doi: 10.4321/s1130-01082014000200015
15. Miyake T, Hoshino S, Yoshida Y, Aisu N, Tanimura S, Hisano S, et al. Multiple ectopic hepatocellular carcinomas arising in the abdominal cavity. Case Rep Gastroenterol (2012) 6(3):629–34. doi: 10.1159/000343433
16. Nishikawa K, Watanabe K, Hisamatsu Y, Shirao K. Ectopic hepatocellular carcinoma of the left sub-diaphragm with metastasis. Intern Med (2011) 50(14):1505–6. doi: 10.2169/internalmedicine.50.5499
17. Nenekidis I, Anagnostakou V, Paralikas I, Kokkori A, Dedeilias P, Zisis C. Ectopic hepatocellular carcinomas developed in the chest wall and skull. Asian Cardiovasc Thorac Ann (2011) 19(5):360–2. doi: 10.1177/0218492311419460
18. Singh V, Sinha RJ, Sankhwar SN, Kumar S, Mehrotra B, Puri M, et al. Primary hepatocellular carcinoma in ectopic liver masquerading as left adrenal carcinoma: a rare occurrence. Rare Tumors (2010) 2(2):e35. doi: 10.4081/rt.2010.e35
19. Matsuyama M, Sugiura S, Kakita A, Sato Y, Kuroda M. Hepatocellular carcinoma arising from ectopic liver tissue in the spleen producing insulin-like growth factor II. Pathol Res Pract (2011) 207(2):124–6. doi: 10.1016/j.prp.2010.09.003
20. Kanzaki R, Yamada T, Gotoh K, Takahashi H, Ohigashi H, Ishikawa O. Ectopic hepatocellular carcinoma arising in the left triangular ligament of the liver. Case Rep Gastroenterol (2010) 4(2):138–43. doi: 10.1159/000314042
21. Schmelzle M, Matthaei H, Lehwald N, Raffel A, Tustas RY, Pomjanski N, et al. Extrahepatic intraductal ectopic hepatocellular carcinoma: bile duct filling defect. Hepatobiliary Pancreat Dis Int (2009) 8(6):650–2.
22. Seo UH, Lee HJ, Ryu WS, Kwak JM, Shin BK, Kim WB, et al. Laparoscopic resection of a hepatocellular carcinoma arising from an ectopic liver. Surg Laparosc Endosc Percutan Tech (2008) 18(5):508–10. doi: 10.1097/SLE.0b013e31817e920f
23. Kubota K, Kita J, Rokkaku K, Iwasaki Y, Sawada T, Imura J, et al. Ectopic hepatocellular carcinoma arising from pancreas: a case report and review of the literature. World J Gastroenterol (2007) 13(31):4270–3. doi: 10.3748/wjg.v13.i31.4270
24. Huang TW, Chan DC, Lee HS, Yao NS, Lee SC, Cheng YL. Ectopic hepatocellular carcinoma of the diaphragm. Dig Dis Sci (2007) 52(4):1118–20. doi: 10.1007/s10620-006-9329-4
25. Shigemori M, Kondo M, Azechi H, Inoue F, Tamura J, Kobayashi H, et al. A case of ectopic hepatocellular carcinoma in the jejunum. J Gastroenterol (2006) 41(9):913–8. doi: 10.1007/s00535-006-1872-4
26. Tsushimi T, Enoki T, Harada E, Orita M, Noshima S, Masuda M, et al. Ectopic hepatocellular carcinoma arising in the bile duct. J Hepatobiliary Pancreat Surg (2005) 12(3):266–8. doi: 10.1007/s00534-004-0963-y
27. Kim KA, Park CM, Kim CH, Choi SY, Park SW, Hong SJ, et al. Hepatocellular carcinoma in an ectopic liver: CT findings. Eur Radiol (2003) 13(Suppl 4):L45–7. doi: 10.1007/s00330-003-1908-6
28. Asselah T, Condat B, Cazals-Hatem D, Hassani Z, Bernuau J, Groussard O, et al. Ectopic hepatocellular carcinoma arising in the left chest wall: a long-term follow-up. Eur J Gastroenterol Hepatol (2001) 13(7):873–5. doi: 10.1097/00042737-200107000-00018
29. Takayasu K, Itabashi M, Moriyama N. Case report: ectopic hepatocellular carcinoma arising from the left diaphragm. Clin Radiol (1994) 49(8):579–81. doi: 10.1016/s0009-9260(05)82944-7
Keywords: ectopic hepatocellular carcinoma, retroperitoneal tumor, adrenal infiltration, endocrine function, case report
Citation: Yang Y, Lu Q, Li Z, Wang C and Li Y (2023) A large ectopic hepatocellular carcinoma with adrenal infiltration: a rare case report. Front. Oncol. 13:1116684. doi: 10.3389/fonc.2023.1116684
Received: 05 December 2022; Accepted: 05 April 2023;
Published: 24 April 2023.
Edited by:
Ulrich Ronellenfitsch, Medical Faculty of the Martin-Luther-University Halle-Wittenberg, GermanyReviewed by:
Praveen Peddu, Kings Health Partners, United KingdomAlastair Young, St James’s University Hospital, United Kingdom
Copyright © 2023 Yang, Lu, Li, Wang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuanwei Li, MTUxMzUxNDg5MTJAMTYzLmNvbQ==
 Yongjun Yang
Yongjun Yang Qiang Lu
Qiang Lu