- 1Department of Surgery, Ajou University School of Medicine, Suwon, Republic of Korea
- 2Department of Internal Medicine, Seoul National University Hospital, Seoul, Republic of Korea
- 3Cancer Research Institute, Seoul National University, Seoul, Republic of Korea
- 4Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea
- 5Department of Medical Oncology, Instituto Nacional de Enfermedades Neoplasicas, Lima, Peru
- 6Division of Hematology-Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
- 7Division of Medical Oncology, Department of Internal Medicine, Gachon University Gil Medical Center, Incheon, Republic of Korea
- 8Department of Surgery, Chosun University College of Medicine, Chosun University Hospital, Gwangju, Republic of Korea
- 9Division of Hematology/Oncology, Department of Internal Medicine, Korea University College of Medicine, Guro Hospital, Seoul, Republic of Korea
- 10Department of Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea
- 11Department of Surgery, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, Daegu, Republic of Korea
- 12Department of Clinical Epidemiology and Biostatistics, Asan Medical Center, Seoul, Republic of Korea
- 13Division of Breast Surgery, Department of Surgery, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Republic of Korea
Background: Fertility is an important issue for young women with breast cancer, but studies about physicians’ knowledge, attitudes, and practices toward fertility preservation (FP) are largely based on Western populations and do not reflect recent international guidelines for FP. In this international study, we aimed to assess the knowledge, attitudes, and practices of physicians from South Korea, other Asian countries, and Latin America toward FP in young women with breast cancer, and identify the related barriers.
Methods: The survey was conducted anonymously among physicians from South Korea, other Asian countries, and Latin America involved in breast cancer care between November 2020 and July 2021. Topics included knowledge, attitudes, and perceptions toward FP; practice behaviors; barriers; and participant demographics. We grouped related questions around two main themes—discussion with patients about FP, and consultation and referral to a reproductive endocrinologist. We analyzed the relationships between main questions and other survey items.
Results: A total of 151 physicians completed the survey. Most participants’ overall knowledge about FP was good. More than half of the participants answered that they discussed FP with their patients in most cases, but that personnel to facilitate discussions about FP and the provision of educational materials were limited. A major barrier was time constraints in the clinic (52.6%). Discussion, consultations, and referrals were more likely to be performed by surgeons who primarily treated patients with operable breast cancer (FP discussion odds ratio [OR]: 2.90; 95% confidence interval [CI]: 1.24–6.79; FP consultation and referral OR: 2.98; 95% CI: 1.14–7.74). Participants’ knowledge and attitudes about FP were significantly associated with discussion, consultations, and referrals.
Conclusion: Physicians from South Korea, other Asian countries, and Latin America are knowledgeable about FP and most perform practice behaviors toward FP well. Physicians’ knowledge and favorable attitudes are significantly related to discussion with patients, as well as consultation with and referral to reproductive endocrinologists. However, there are also barriers, such as limitations to human resources and materials, suggesting a need for a systematic approach to improve FP for young women with breast cancer.
Introduction
Breast cancer is the most common cancer and a leading cause of death among women (1). The incidence of invasive breast cancer in women of reproductive age is 73.2 cases per 100,000, which far exceeds the incidence of other cancers in young adults from 2011 to 2015 (2). However, advances in treatment have led to gradual improvements in survival rates over the past 20 years. As long-term survival is expected, survivorship issues, such as fertility and quality of life, are becoming more important (3, 4).
Despite the improvements in survival rates, women with breast cancer have a lower birth rate than those with other cancers, as well as the general population (5). Younger patients with breast cancer often have more biologically aggressive tumor characteristics than older patients, and tend to receive more chemotherapy, which can lead to premature ovarian failure (6). Chemotherapy-induced amenorrhea may be reversible, but in some cases, ovarian function is not restored for years (7). Furthermore, the ovarian reserve is reduced after the completion of chemotherapy (8). In addition, for patients with hormone receptor-positive tumors, standard endocrine therapy includes tamoxifen for at least five or even ten years, with or without two to five years of ovarian suppression (9). Owing to the long duration of treatment, patients age after treatment, and their fecundity decrease accordingly (10).
Fertility loss causes considerable distress and results in various psychosocial problems among cancer survivors (4). In particular, younger patients with breast cancer are more vulnerable to distress than older ones (11, 12). More than 50% of patients of childbearing age with breast cancer have concerns about treatment-related early menopause or infertility (13). These fertility concerns can also lead to problems with treatment adherence (14), and non-adherence is related to low survival rates (15). Therefore, counseling for fertility preservation (FP) is recommended to reduce dissatisfaction and concerns regarding loss of fertility in young patients (16).
Current international guidelines recommend advising patients about the potential risk to fertility as early as possible before treatment starts, to allow for the full range of options for FP (17). Several factors have been identified that can influence FP counseling or procedures for patients with cancer (18–21). Regarding physician factors, several survey studies have been conducted about FP in patients with cancer (19–25); most have focused on Western populations. However, there are differences in the patterns of breast cancer in Western and Asian countries, with a lower peak age in Asian countries (26). In Asia, more than 40% of patients with breast cancer are diagnosed under the age of 50, compared with about 20% in Western countries (27). Nevertheless, in a study of FP experts in Asian countries, it was reported that low recognition among medical staff is one of the major issues hampering FP for childhood and adolescent patients (28). In addition, previous studies on Asian physicians treating breast cancer are single-nation studies conducted prior to the American Society of Clinical Oncology guidelines update in 2016 (22, 25).
Therefore, we conducted a survey study to assess the knowledge, attitudes, and practices of physicians toward FP in young women with breast cancer, to identify barriers, and to elucidate which factors are associated with FP discussion and referral to infertility specialists among physicians in South Korea, other Asian countries, and Latin America.
Materials and methods
Survey instrument
Based on previous studies (20, 23), we developed a questionnaire consisting of 45 questions in 6 categories: knowledge about FP, practice behaviors, barriers to FP, attitudes toward FP, perceptions on FP, and participant demographics.
Questions were answered using a five-point Likert scale, except for demographics and one question regarding knowledge about FP. For some behaviors and barriers, participants could fill out their own answers. Regarding knowledge about FP, for statements A-1 and A-4, “strongly agree” and “agree” were considered correct answers. For statement A-5, “required” was considered a correct answer (Supplementary Table 1). The total score was calculated by assigning one point to each correct answer. We categorized participants into knowledgeable and not knowledgeable groups based on the score distribution.
Regarding attitudes toward FP, we calculated the total score by assigning one point to the response corresponding to the positive attitude. Subsequently, participants were divided into three groups based on the score distribution. The odds were estimated with three groups, but as zero and one showed a closer effect size; they were grouped together, and two was analyzed separately. As a result, we categorized the participants into two groups: those with favorable or unfavorable attitudes. Since preimplantation genetic diagnosis is prohibited by law in South Korea, the related attitudinal survey item was not included in the analysis. Perceptions of FP were also divided into two groups based on the sum of the survey responses.
Participants’ demographics included questions on medical training and practice information. The questionnaire was developed in English, and the translated Korean version, which did not contain a nationality question, was used in the group consisting only of South Koreans.
Procedures
The survey was conducted four times over nine months, each time with a different group. First, the survey sample included members of the Korean Breast Cancer Society (KBCS)— mainly surgeons who treat patients with breast cancer. A link to the Korean version of the survey was sent to KBCS members whose email addresses were secured in November 2020 (n = 150). Second, an English version of the survey link was distributed onsite to participants of the Asian Breast Cancer Network (ABCN) meeting held during the 2021 Global Breast Cancer Conference in Seoul, South Korea (n = 30). The ABCN meeting is a platform for the selection of joint research projects for breast cancer in the Asia-Pacific region, and for the discussion organized by the KBCS of the practical problems and solutions facing each participating country. Third, during a virtual conference about breast cancer in young women with Latin American physicians held on May 11, the survey link was released to attendees (n = about 80). Finally, a link to the Korean questionnaire was emailed to members of the Breast Committee of the Korean Cancer Study Group (n = 109), a clinical trial organization mainly composed of medical oncologists. This study was reviewed and approved by the Institutional Review Board of the Asan Medical Center (2020-1828, 2021-1463), which also waived the requirement for informed consent because of the anonymity of the survey.
Statistical analysis
We grouped related questions around two main topics and analyzed their associations with other survey items. The first main topic was discussions about FP with patients; example items include “I discuss fertility issues with patients regardless of pathologic staging of cancer,” and “I discuss the impact of cancer treatment on future fertility with my cancer patients.” The second was consultation and referral to an infertility specialist or reproductive endocrinologist; example items include “I consult an infertility specialist or reproductive endocrinologist with questions about potential fertility issues in my patients,” and “I refer patients who have questions about fertility to an infertility specialist or reproductive endocrinologist.” Owing to the correlations between items, the sum of the items was calculated and used as a covariate (five items for physicians’ knowledge, four items for attitudes, and two items for perceptions).
Logistic regression was used to assess the association between key questions and physicians’ knowledge, attitudes, and characteristics. Odds ratios (ORs) and their 95% confidence intervals (CIs) were estimated. The candidate variables with P < 0.2 in univariate analysis were evaluated in multivariable analysis using backward elimination. The data of two participants who did not respond to demographic items were excluded from the univariate and multivariate analyses. P-values < 0.05 were considered statistically significant. All statistical analyses were performed using SPSS version 21.0 (IBM Corp., Armonk, NY, USA).
Results
Participant characteristics
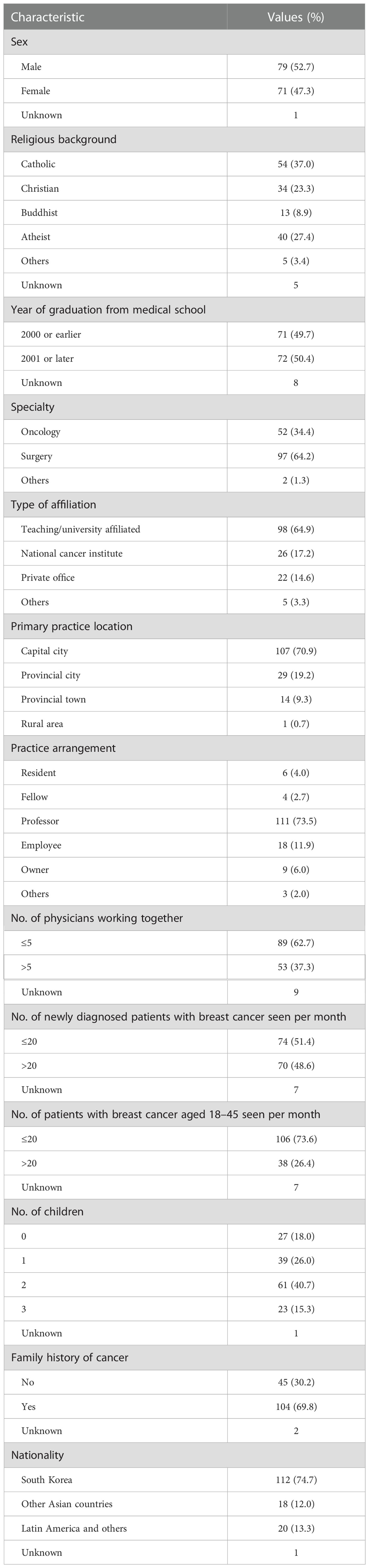
A total of 151 physicians responded to the survey. Participants’ demographic and other characteristics are listed in Table 1. Of the participants, 71 (47.3%) were women. Totally, 52 (34.4%) and 97 (64.2%) of the participants specialized in oncology and surgery, respectively. A total of 64.9% of the participants were affiliated with teaching/university hospitals. Less than half of the physicians responded that they see more than 20 patients with newly diagnosed breast cancer per month. On the contrary, 26.4% responded that they see over 20 breast cancer patients every month in the 18–45 age group. One hundred and twenty-three (82.0%) physicians had children. The majority of the participants were Korean (74.7%), followed by Peruvian (9.3%) and Japanese (7.3%).
Survey results
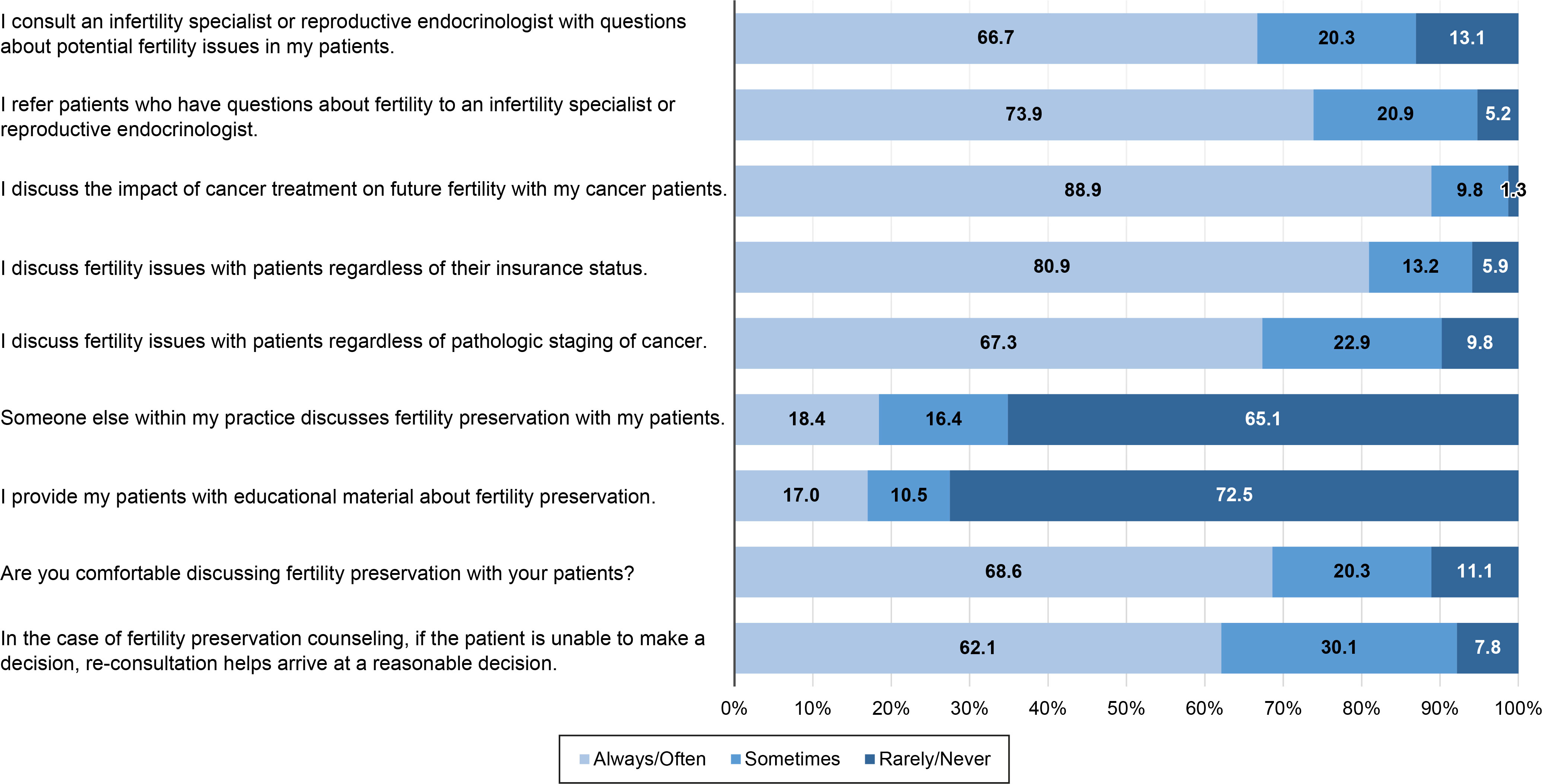
The survey results are shown in the Supplementary Tables. Most of the participants had adequate knowledge about FP (Supplementary Table 1). Regarding practice behaviors, more than half of the participants always/often consulted with and referred patients with fertility issues to an infertility specialist or reproductive endocrinologist, discussed FP with their patients, and felt comfortable discussing FP with their patients. On the contrary, more than half the participants said they rarely/never provided their patients with educational materials about FP, and reported that someone else within their practice rarely/never discussed FP with their patients (Figure 1, Supplementary Table 2). The mean time spent on discussions about FP was 13.2 ± 10.4 minutes.
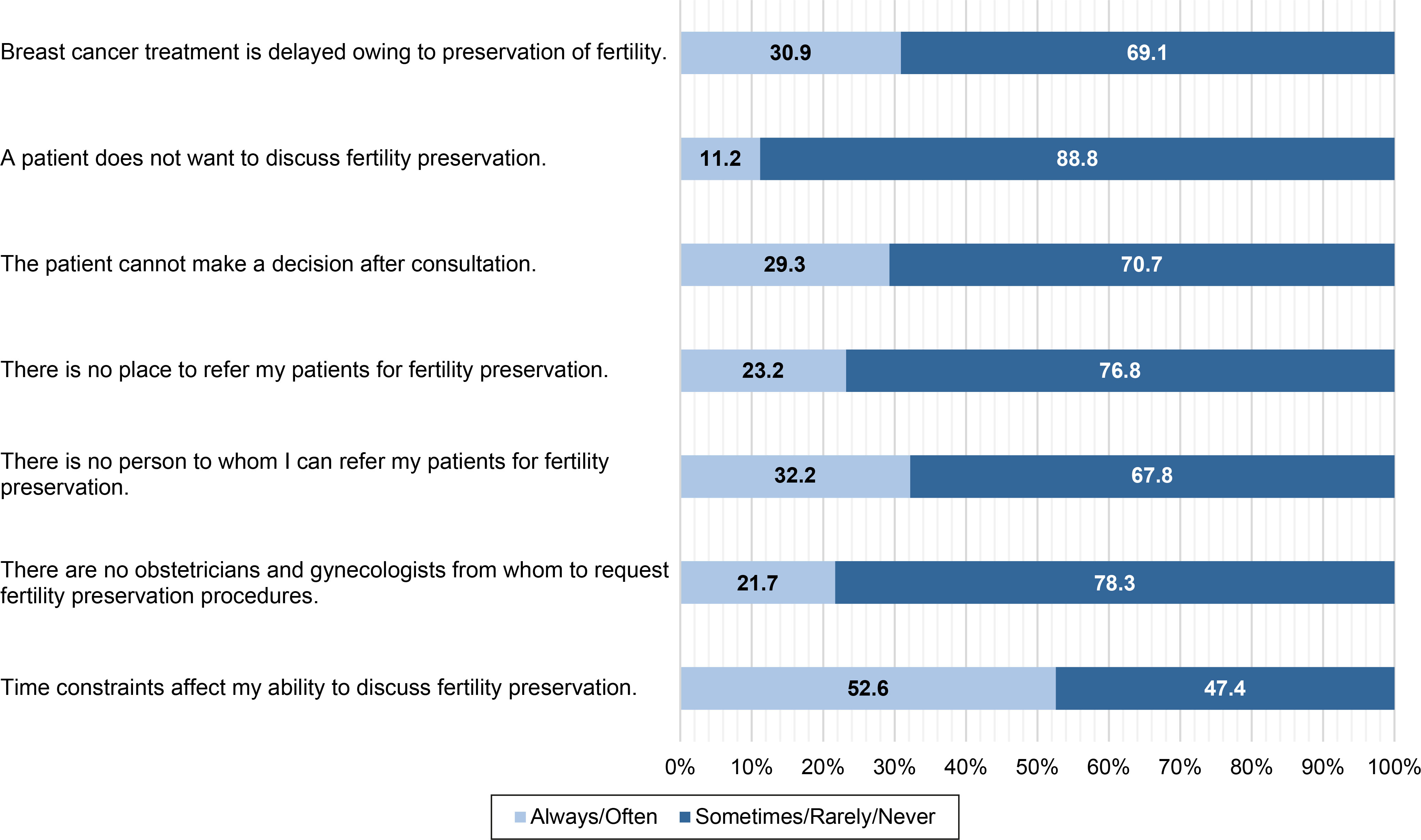
In terms of barriers, the most common response was time constraints in the clinical setting (52.6%), followed by lack of human resources to whom to refer patients for FP (32.2%) (Figure 2, Supplementary Table 3). Patients’ unwillingness to discuss FP was the least common barrier (11.2%). In addition to the questionnaire items, the participants indicated other barriers to FP counseling, such as fear of recurrence and financial problems.
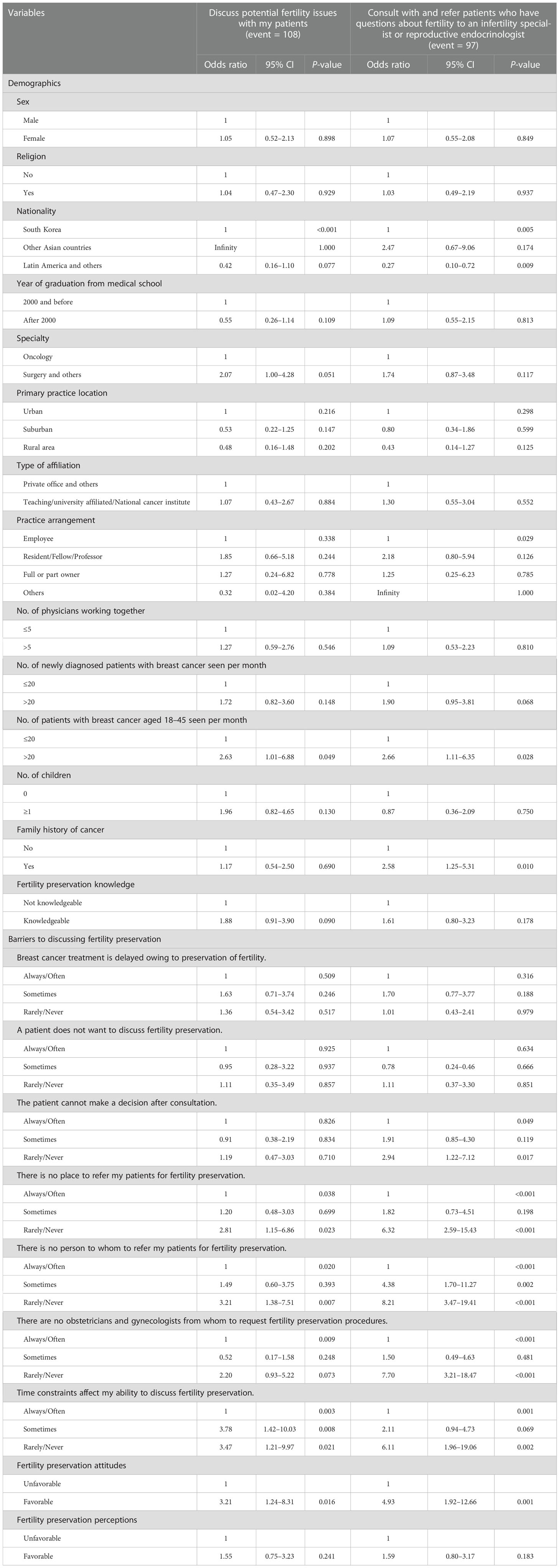
Univariate analysis
In terms of participants’ characteristics, factors significantly associated with discussion were nationality (P < 0.001) and the number of patients with breast cancer aged 18–45 seen per month (P = 0.049). Factors significantly associated with consultation and referral were nationality (P = 0.005), number of patients with breast cancer aged 18–45 seen per month (P = 0.028), and family history of cancer (P = 0.010). For barriers, except for two items, the rarer the barrier was, the more frequent discussions with patients or consultations and referrals were performed. The group that showed favorable attitudes toward FP had more discussions, consultations, and referrals than the group with unfavorable attitudes (Table 2).
Factors associated with discussions, consultations, and referrals
Table 3 shows the multivariate analysis of key questions and other variables. Surgeons, who primarily see patients with operable breast cancer, were more likely to engage in discussions with them (OR: 2.90; 95% CI: 1.24–6.79) and consult with and refer patients who had questions about fertility to an infertility specialist or reproductive endocrinologist than medical oncologists (OR: 2.98; 95% CI: 1.14–7.74). Physicians who saw more than 20 patients aged 18–45 were more likely to discuss fertility issues with patients (OR: 3.55; 95% CI: 1.23–10.27). Physicians with a family history of cancer were more likely to consult and refer patients who had questions about fertility to an infertility specialist or reproductive endocrinologist (OR: 4.90; 95% CI: 1.69–14.21).
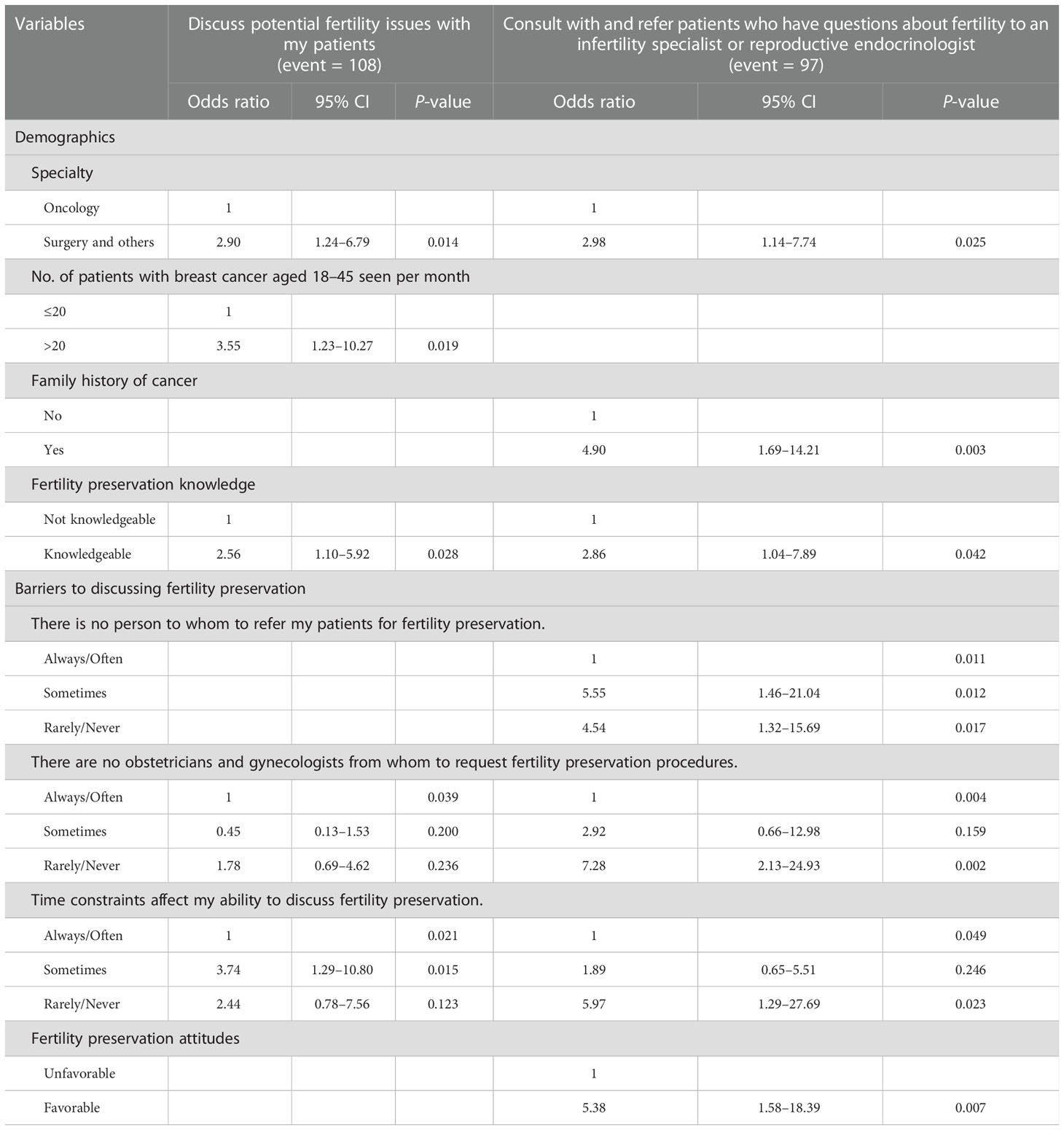
Table 3 Factors associated with discussion with patients and consultation and referral to specialists.
Participants who had better knowledge engaged in more discussions (OR: 2.56; 95% CI: 1.10–5.92) and consultations and referrals (OR: 2.86; 95% CI: 1.04–7.89) compared to those who did not. Physicians with favorable attitudes toward FP engaged in more consultations and referrals compared to those with unfavorable attitudes (OR: 5.38; 95% CI: 1.58–18.39).
In terms of barriers, the availability of infertility specialists to whom to make requests regarding FP procedures was associated with discussion (P = 0.039) and consultation and referral (P = 0.004). Time constraints were associated with discussion (P = 0.021) and consultation and referral (P = 0.049). In addition, participants who did not have personnel to whom to refer patients for FP engaged in significantly less consultation and referral (P = 0.011).
Discussion
Fertility information is a well-known unmet need among young adult cancer survivors (29). In addition to the lack of information, decisional conflicts about FP arise in complex decision-making processes (18). In a previous study, the prevalence of high-decisional conflict was significantly higher among participants not referred for FP counseling (30). Therefore, providing necessary information through appropriate referral to infertility specialists is important in survivorship care for patients of reproductive age.
In this study, we report the current knowledge, attitudes, and practices of physicians who treat young women with breast cancer, as well as the barriers they face in the clinical setting. We also identified factors associated with discussions with patients about FP and referral to infertility specialists. Multiple factors pertaining to participants’ characteristics have previously been reported in relation to referrals (20, 22, 25). Our study finds that specialty, number of patients with breast cancer aged 18–45 seen per month, and family history of cancer were related to discussion or consultation and referral. Quinn et al. (20) showed that the gender of oncologists is related to referral, with female oncologists making more referrals (P = 0.004). Shimizu et al. (22) also reported that female physicians and physicians aged under 50 are more likely to refer patients to a reproductive specialist. However, in our study, there were no significant differences between male and female physicians with regard to FP discussion and consultation and referral. These variations are likely due to differences in study populations and participants’ socio-demographics. Interestingly, in this study there was a significant difference in discussion, consultation, and referral depending on the participants’ specialty. The odds of FP discussion were about 2.90-fold higher among surgeons compared to medical oncologists, and the odds of consultation and referral to infertility specialists were 2.98-fold higher among surgeons. In South Korea, where most of the participants live, surgeons often diagnose and treat patients with operable breast cancer first, and then refer them to medical oncologists. Therefore, surgeons would have more opportunities to discuss FP with patients before treatment.
In our survey, physicians with higher knowledge scores tended to discuss more (OR: 2.56) and engage in more consultation and referral (OR: 2.86). In addition, physicians with favorable attitudes toward FP tended to consult and refer more (OR: 5.38). This result is comparable to previous studies (20, 22). On the contrary, Son et al. (25) reported that knowledge and attitudes about FP are not correlated with actual practice. Although we divided the sample into not knowledgeable and knowledgeable groups based on the response distribution, many participants responded correctly. Therefore, it is difficult to state that the not knowledgeable group actually lacked absolute knowledge about FP, and is a relative classification. Nevertheless, it is true that the group with higher knowledge scores engaged in more counseling and referral. These results suggest that more consultations and referrals will be possible if physicians’ knowledge and attitudes are improved with attention and effort.
Although our findings indicate that practices regarding FP were well performed by physicians, the provision of educational materials about FP to patients was not satisfactory. Only 17% of the participants provided educational materials about FP to patients. Sallem et al. (24) reported that 76% of oncologists responded that educational materials could be helpful in discussing fertility. We previously reported that about half of young patients with breast cancer were unaware of the effects of anticancer treatment on ovarian function and fertility, but after viewing educational videos provided by healthcare professionals, only 2% of patients answered that they had no knowledge (31). Several FP decision aids for patients with breast cancer have been developed and systemized, and their effectiveness has been proven (32, 33). Therefore, standardized educational materials and decision aids for FP should be developed and distributed to improve current practices.
This study also shows that several barriers still exist in clinical settings—and the most frequently reported barrier was time constraints. This problem has been previously reported in a South Korean study (25). In that study, patients’ lack of interest in FP was also reported as a significant barrier (25). However, the percentage of “patients did not want to discuss FP” was the lowest (11.2%) among the survey items regarding barriers in our study. Time constraints, a lack of people to consult with, and an absence of infertility specialists to request FP procedures are systematic barriers that cannot be resolved by individual physicians’ efforts. Kelvin et al. (33) reported that a hospital-level cancer and fertility program resulted in significant improvements in patient satisfaction and helpfulness of information about treatment-related fertility risks and FP options. Therefore, support and establishing programs at the hospital and national level will be needed to overcome obstacles and improve fertility-related practices.
Physician nationalities had little impact on key questions. The responses of physicians from South Korea, other Asian countries, and Latin America were mostly similar (data not shown)—with one exception. Participants from South Korea and Latin America tended to answer that time constraints affected their FP discussions “always/often” (58.9% and 55%, respectively), while only 16.7% of participants from other Asian countries responded similarly (Supplementary Figure 1). This is likely a selection bias regarding physicians from other Asian countries who were invited to the ABCN meeting, which is related to joint breast cancer research in the Asia-Pacific region. The number of participants from other countries was not large enough to evaluate differences among nationalities. A large multinational survey is required to reveal national differences related to FP environments and practices in the future.
This study has several limitations. First, we could not include all the relevant physicians from each country, restricting generalizability to all physicians from the studied countries or continents. Second, there may be a selection bias for physicians from other Asian countries who attended the ABCN meeting because only selected physicians from each country were invited. Third, physicians who are interested in FP are more likely to respond to the survey through e-mail or a survey link during the virtual conference. Therefore, the results that most of the practices pertaining to FP are well-performed may be biased. Finally, we did not collect data on the procedure and pathway of discussion, consultation, and referral as well as patients’ adherence to it. Further study is warranted to identify how fertility issues are discussed and through which pathways referrals and consultations are implemented in actual patient care. However, the results are meaningful in that the survey area was extended to other countries, not limited to Western countries or South Korea. In addition, this survey included physicians from a variety of specialties.
In conclusion, this survey demonstrates physicians’ current knowledge, attitudes, and practices toward FP for patients with breast cancer and reveals the obstacles to FP. Physicians’ knowledge about FP is generally high. Most of the practices pertaining to FP are well-performed among physicians in South Korea, other Asian countries, and Latin America. However, there is room for improvement regarding time constraints, a lack of personnel to consult, and poor collaboration with infertility specialists. Systematic approaches to overcome barriers are needed to improve the FP discussion and referral of patients with breast cancer.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Board of Asan Medical Center. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
Study design was contributed by HK. Data acquisition was contributed by K-HL, S-BK, HG, TV, YP, HA, YK, IP, SA, JL, JJ, and HK. Data analysis was contributed by SB and SK. Manuscript writing was contributed by SB and K-HL. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HC20C0135).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2023.1109694/full#supplementary-material
Abbreviations
FP, fertility preservation; KBCS, the Korean Breast Cancer Society; ABCN, Asian Breast Cancer Network.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2018) 68(6):394–424. doi: 10.3322/caac.21492
2. Ward EM, Sherman RL, Henley SJ, Jemal A, Siegel DA, Feuer EJ, et al. Annual report to the nation on the status of cancer, featuring cancer in men and women age 20–49 years. J Natl Cancer Inst (2019) 111(12):1279–97. doi: 10.1093/jnci/djz106
3. Ganz PA, Greendale GA, Petersen L, Kahn B, Bower JE. Breast cancer in younger women: reproductive and late health effects of treatment. J Clin Oncol (2003) 21(22):4184–93. doi: 10.1200/jco.2003.04.196
4. Gorman JR, Malcarne VL, Roesch SC, Madlensky L, Pierce JP. Depressive symptoms among young breast cancer survivors: the importance of reproductive concerns. Breast Cancer Res Treat (2010) 123(2):477–85. doi: 10.1007/s10549-010-0768-4
5. Stensheim H, Cvancarova M, Møller B, Fosså SD. Pregnancy after adolescent and adult cancer: a population-based matched cohort study. Int J Cancer (2011) 129(5):1225–36. doi: 10.1002/ijc.26045
6. Fredholm H, Eaker S, Frisell J, Holmberg L, Fredriksson I, Lindman H. Breast cancer in young women: poor survival despite intensive treatment. PloS One (2009) 4(11):e7695. doi: 10.1371/journal.pone.0007695
7. Sukumvanich P, Case LD, Van Zee K, Singletary SE, Paskett ED, Petrek JA, et al. Incidence and time course of bleeding after long-term amenorrhea after breast cancer treatment: a prospective study. Cancer (2010) 116(13):3102–11. doi: 10.1002/cncr.25106
8. Wenners A, Grambach J, Koss J, Maass N, Jonat W, Schmutzler A, et al. Reduced ovarian reserve in young early breast cancer patients: preliminary data from a prospective cohort trial. BMC Cancer (2017) 17(1):632. doi: 10.1186/s12885-017-3593-x
9. National Comprehensive Cancer Network (NCCN). NCCN clinical practice guidelines in oncology (NCCN guidelines®): Breast cancer (Version: 4.2022) (2022). Available at: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1419 (Accessed July 21, 2022).
10. Baird DT, Collins J, Egozcue J, Evers LH, Gianaroli L, Leridon H, et al. Fertility and ageing. Hum Reprod Update (2005) 11(3):261–76. doi: 10.1093/humupd/dmi006
11. Wenzel LB, Fairclough DL, Brady MJ, Cella D, Garrett KM, Kluhsman BC, et al. Age-related differences in the quality of life of breast carcinoma patients after treatment. Cancer (1999) 86(9):1768–74. doi: 10.1002/(SICI)1097-0142(19991101)86:9<1768::AID-CNCR19>3.0.CO;2-O
12. Politi MC, Enright TM, Weihs KL. The effects of age and emotional acceptance on distress among breast cancer patients. Support Care Cancer (2007) 15(1):73–9. doi: 10.1007/s00520-006-0098-6
13. Partridge AH, Gelber S, Peppercorn J, Sampson E, Knudsen K, Laufer M, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol (2004) 22(20):4174–83. doi: 10.1200/jco.2004.01.159
14. Llarena NC, Estevez SL, Tucker SL, Jeruss JS. Impact of fertility concerns on tamoxifen initiation and persistence. J Natl Cancer Inst (2015) 107(10):djv202. doi: 10.1093/jnci/djv202
15. Hershman DL, Shao T, Kushi LH, Buono D, Tsai WY, Fehrenbacher L, et al. Early discontinuation and non-adherence to adjuvant hormonal therapy are associated with increased mortality in women with breast cancer. Breast Cancer Res Treat (2011) 126(2):529–37. doi: 10.1007/s10549-010-1132-4
16. Deshpande NA, Braun IM, Meyer FL. Impact of fertility preservation counseling and treatment on psychological outcomes among women with cancer: a systematic review. Cancer (2015) 121(22):3938–47. doi: 10.1002/cncr.29637
17. Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol (2018) 36(19):1994–2001. doi: 10.1200/jco.2018.78.1914
18. Peate M, Meiser B, Friedlander M, Zorbas H, Rovelli S, Sansom-Daly U, et al. It's now or never: fertility-related knowledge, decision-making preferences, and treatment intentions in young women with breast cancer–an Australian fertility decision aid collaborative group study. J Clin Oncol (2011) 29(13):1670–7. doi: 10.1200/jco.2010.31.2462
19. Quinn GP, Vadaparampil ST, King L, Miree CA, Wilson C, Raj O, et al. Impact of physicians' personal discomfort and patient prognosis on discussion of fertility preservation with young cancer patients. Patient Educ Couns (2009) 77(3):338–43. doi: 10.1016/j.pec.2009.09.007
20. Quinn GP, Vadaparampil ST, Lee JH, Jacobsen PB, Bepler G, Lancaster J, et al. Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol (2009) 27(35):5952–7. doi: 10.1200/jco.2009.23.0250
21. Forman EJ, Anders CK, Behera MA. A nationwide survey of oncologists regarding treatment-related infertility and fertility preservation in female cancer patients. Fertil Steril (2010) 94(5):1652–6. doi: 10.1016/j.fertnstert.2009.10.008
22. Shimizu C, Bando H, Kato T, Mizota Y, Yamamoto S, Fujiwara Y. Physicians' knowledge, attitude, and behavior regarding fertility issues for young breast cancer patients: a national survey for breast care specialists. Breast Cancer (2013) 20(3):230–40. doi: 10.1007/s12282-011-0328-8
23. Rosenberg SM, Gelber S, Gelber RD, Krop E, Korde LA, Pagani O, et al. Oncology physicians' perspectives on practices and barriers to fertility preservation and the feasibility of a prospective study of pregnancy after breast cancer. J Adolesc Young Adult Oncol (2017) 6(3):429–34. doi: 10.1089/jayao.2017.0031
24. Sallem A, Shore J, Ray-Coquard I, Ferreux L, Bourdon M, Maignien C, et al. Fertility preservation in women with cancer: a national study about French oncologists awareness, experience, and feelings. J Assist Reprod Genet (2018) 35(10):1843–50. doi: 10.1007/s10815-018-1251-0
25. Son H, Lee HM, Yang YJ, Youn HJ, Lee JW, Lee J, et al. Current practices toward fertility issues for young breast cancer patients: a survey of the Korean breast cancer society; the SMARTSHIP study. J Breast Dis (2020) 8(2):100–7. doi: 10.14449/jbd.2020.8.2.100
26. Leong SP, Shen ZZ, Liu TJ, Agarwal G, Tajima T, Paik NS, et al. Is breast cancer the same disease in Asian and Western countries? World J Surg (2010) 34(10):2308–24. doi: 10.1007/s00268-010-0683-1
27. Youlden DR, Cramb SM, Yip CH, Baade PD. Incidence and mortality of female breast cancer in the Asia-pacific region. Cancer Biol Med (2014) 11(2):101–15. doi: 10.7497/j.issn.2095-3941.2014.02.005
28. Takae S, Lee JR, Mahajan N, Wiweko B, Sukcharoen N, Novero V, et al. Fertility preservation for child and adolescent cancer patients in Asian countries. Front Endocrinol (Lausanne) (2019) 10:655. doi: 10.3389/fendo.2019.00655
29. Benedict C, Thom B, Friedman DN, Diotallevi D, Pottenger EM, Raghunathan NJ, et al. Young adult female cancer survivors' unmet information needs and reproductive concerns contribute to decisional conflict regarding posttreatment fertility preservation. Cancer (2016) 122(13):2101–9. doi: 10.1002/cncr.29917
30. Mersereau JE, Goodman LR, Deal AM, Gorman JR, Whitcomb BW, Su HI. To preserve or not to preserve: how difficult is the decision about fertility preservation? Cancer (2013) 119(22):4044–50. doi: 10.1002/cncr.28317
31. Shin S, Kim J, Kim D, Kim H, Lee S, Kim SH, et al. The importance of education regarding the effects of anticancer treatment on fertility and ovarian function in the female patients with breast cancer. J Menopausal Med (2019) 25(3):142–8. doi: 10.6118/jmm.19010
32. Garvelink MM, ter Kuile MM, Fischer MJ, Louwé LA, Hilders CG, Kroep JR, et al. Development of a decision aid about fertility preservation for women with breast cancer in the Netherlands. J Psychosom Obstet Gynaecol (2013) 34(4):170–8. doi: 10.3109/0167482x.2013.851663
Keywords: breast cancer, young age, fertility preservation, consultation and referral, survivorship
Citation: Baek SY, Lee K-H, Kim S-B, Gomez H, Vidaurre T, Park YH, Ahn HK, Kim YS, Park IH, Ahn SG, Lee J, Jeong JH, Kim S and Kim HJ (2023) Knowledge, attitudes, and behaviors toward fertility preservation in patients with breast cancer: A cross-sectional survey of physicians. Front. Oncol. 13:1109694. doi: 10.3389/fonc.2023.1109694
Received: 28 November 2022; Accepted: 09 January 2023;
Published: 23 January 2023.
Edited by:
Giuliano Marchetti Bedoschi, Faculty of Medicine of Ribeirão Preto, University of São Paulo, BrazilReviewed by:
Valentina Magnani, University of Bologna, ItalyGiacomo Corrado, Agostino Gemelli University Polyclinic (IRCCS), Italy
Copyright © 2023 Baek, Lee, Kim, Gomez, Vidaurre, Park, Ahn, Kim, Park, Ahn, Lee, Jeong, Kim and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hee Jeong Kim, aGVlamVvbmdfa2ltQGFtYy5zZW91bC5rcg==
†These authors have contributed equally to this work and share first authorship
 Soo Yeon Baek
Soo Yeon Baek Kyung-Hun Lee
Kyung-Hun Lee Sung-Bae Kim4
Sung-Bae Kim4 Henry Gomez
Henry Gomez Yeon Hee Park
Yeon Hee Park In Hae Park
In Hae Park Sung Gwe Ahn
Sung Gwe Ahn Jeeyeon Lee
Jeeyeon Lee Jae Ho Jeong
Jae Ho Jeong Hee Jeong Kim
Hee Jeong Kim