
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Oncol. , 13 July 2023
Sec. Thoracic Oncology
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.1108798
 Na Wang1†‡
Na Wang1†‡ Nan Zhang1†‡
Nan Zhang1†‡ Xinyue Zhang1‡
Xinyue Zhang1‡ Yuanyuan Wang2‡
Yuanyuan Wang2‡ Yajie Fu3‡
Yajie Fu3‡ Lingfei Guo1‡
Lingfei Guo1‡ Changhu Liang1‡
Changhu Liang1‡ Mengru Yu4*‡
Mengru Yu4*‡Choriocarcinoma is a rare malignant germ cell neoplasm with high invasiveness, the majority of which are pregnancy-related, and the female genital tract is the most prevalent site of the disease. Although early-stage choriocarcinoma typically metastasizes to the lungs, primary pulmonary choriocarcinoma is extremely rare. Primary pulmonary choriocarcinoma is difficult to diagnose, and it progresses rapidly. Combined with the difficulty of treatment, the prognosis of patients is generally poor. In this article, we retrospectively analyzed a case of female primary pulmonary choriocarcinoma, combined with a review of literature, to understand and describe the diagnostic and treatment progress of PPC.
Choriocarcinoma is a highly invasive malignant tumor originating from the trophoblast epithelium of pregnancy. In rare cases, choriocarcinoma can originate in the external genital region, predominantly in midline structures such as the retroperitoneum, mediastinum, and pineal gland (1, 2). Tumor tissue is composed of cytotrophoblasts, syncytiotrophoblasts, and variable intermediate trophoblasts that secrete β-human chorionic gonadotropin (β-hCG) (3, 4). Primary choriocarcinoma of the lung is very rare and presents mainly as hemoptysis with pulmonary nodules (5); it primarily affects young adults and has a poor prognosis, with a 5-year survival rate of less than 5% (2, 6). In clinical practice, due to the atypical symptoms of primary pulmonary choriocarcinoma (PPC), it is particularly easy to misdiagnose or delay diagnosis. Here, we report the diagnosis and treatment of primary pulmonary choriocarcinoma in a 27-year-old woman.
A 27-year-old woman presented to the hospital with a cough, blood-stained sputum, and a fever for 1 month and chest pain for 10 days. The patient reported that she was married at an appropriate age, had regular menstruation, and had two pregnancies, 3.5 and 1.5 years before her admission to the hospital. There were no similar or hereditary disorders in her family. The physical examination, including the lungs, heart, peripheral lymph nodes, abdomen, and external anal genitalia, showed normal results, and no abnormalities were detected in other organs. A chest computerized tomography (CT) scan in a local hospital showed a space-occupied lesion in the lower lobe of the left lung. However, the anti-infective treatment was ineffective. A second chest CT scan showed an enlarged space occupying lesion in the lower lobe of the left lung (Figure 1), which was diagnosed as an infected-pulmonary cyst.
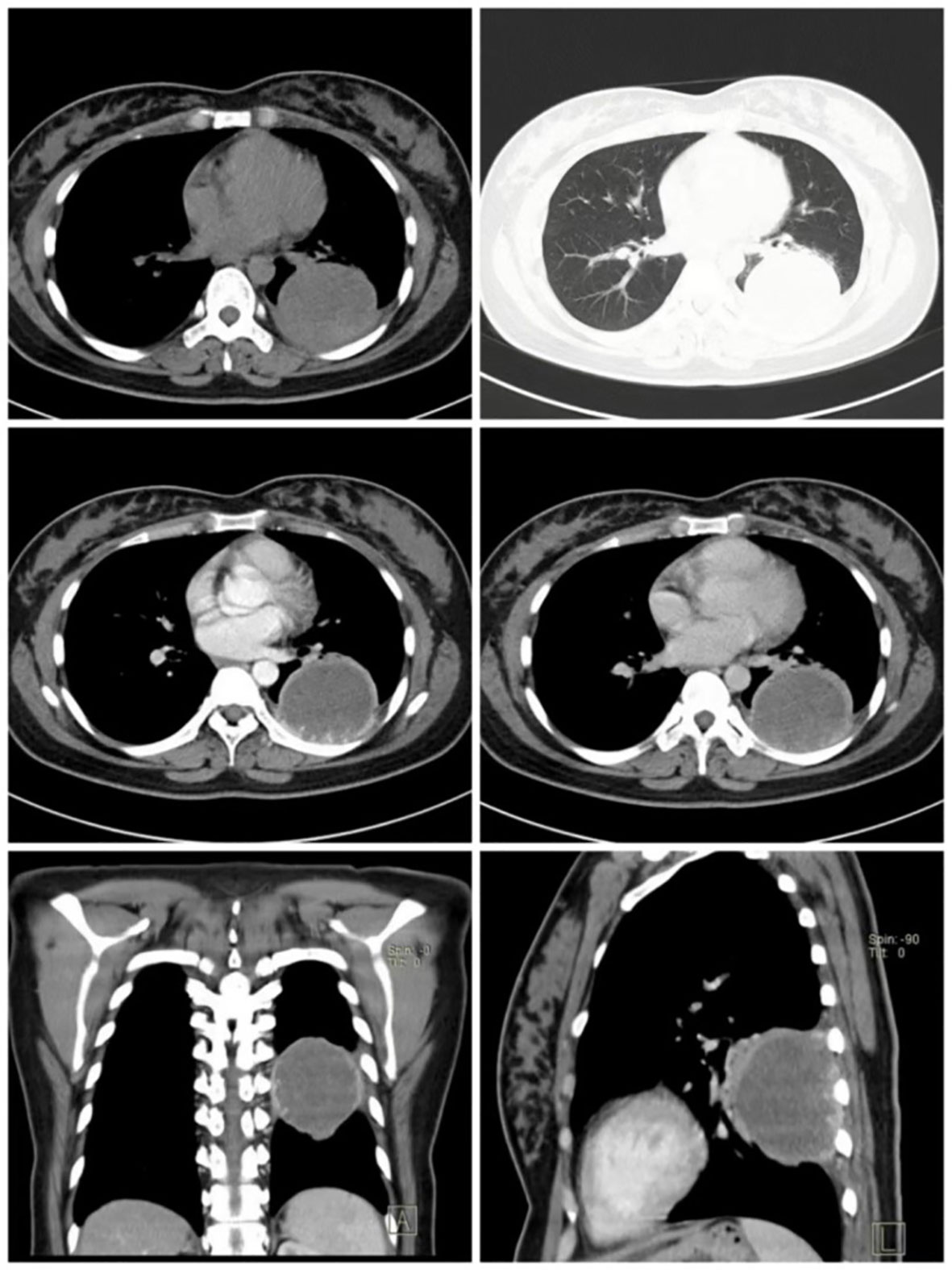
Figure 1 A chest CT scan revealed a large round lesion, approximately 6 cm in diameter, in the lower lobe of the left lung, with a well-defined border and homogeneous density. Following the enhancement scan, the edge of the lesion showed obvious ring enhancement, and villous tissue protruding inward.
Preliminary laboratory examination revealed that the level of non-small cell lung cancer (NSCLC)-associated antigen was 6.62 ng/ml and the level of neuron-specific enolase was 16.73 ng/ml, indicating a malignant lung tumor.
At first, the patient was diagnosed with pulmonary cyst associated with infection according to the fever symptoms and CT examination results, but after a period of antibiotic treatment, there was no obvious effect. After the second CT examination, the lesion in the left lower lobe of the lung became larger than before in a short time, and the values of neuron-specific enolase and NSCLC-associated antigen were relatively high. Although it was still uncertain whether the lesion was inflammation or tumor, considering the high possibility of lung cancer, the decision was made to perform surgical resection of the lung lesion of the lower left lobe. The patient had surgical indications, and there was no evidence of other lesion in the preoperative imaging examinations, including emission computed tomography (ECT), brain magnetic resonance imaging (MRI), and abdominal ultrasound. Meanwhile, the cardiopulmonary risk of surgical resection was within the acceptable range. Therefore, video-assisted thoracoscopic surgery was proposed to remove the lung lesion of the left lower lobe.
The tumor size was 7 × 6 × 6 cm. It invaded the chest wall, and the intraoperative frozen section showed a poorly differentiated malignant tumor with a reproductive system origin. Because the laparoscopic resection was difficult, it was converted to an axillary small incision, left lower lobectomy, and systematic lymph node dissection.
HE staining (Figure 2) showed a small number of tumor cells. Immunohistochemical examination of the diseased tissues of the patients revealed that tumor cells were strongly positive for CK 8/18, CD10, β-hCG, proliferating cell nuclear antigen Ki-67, human placental lactogen (HPL), and GATA-3 and were negative for P63 and P40. The patient was diagnosed with PPC based on the results of laboratory and pathological examinations.
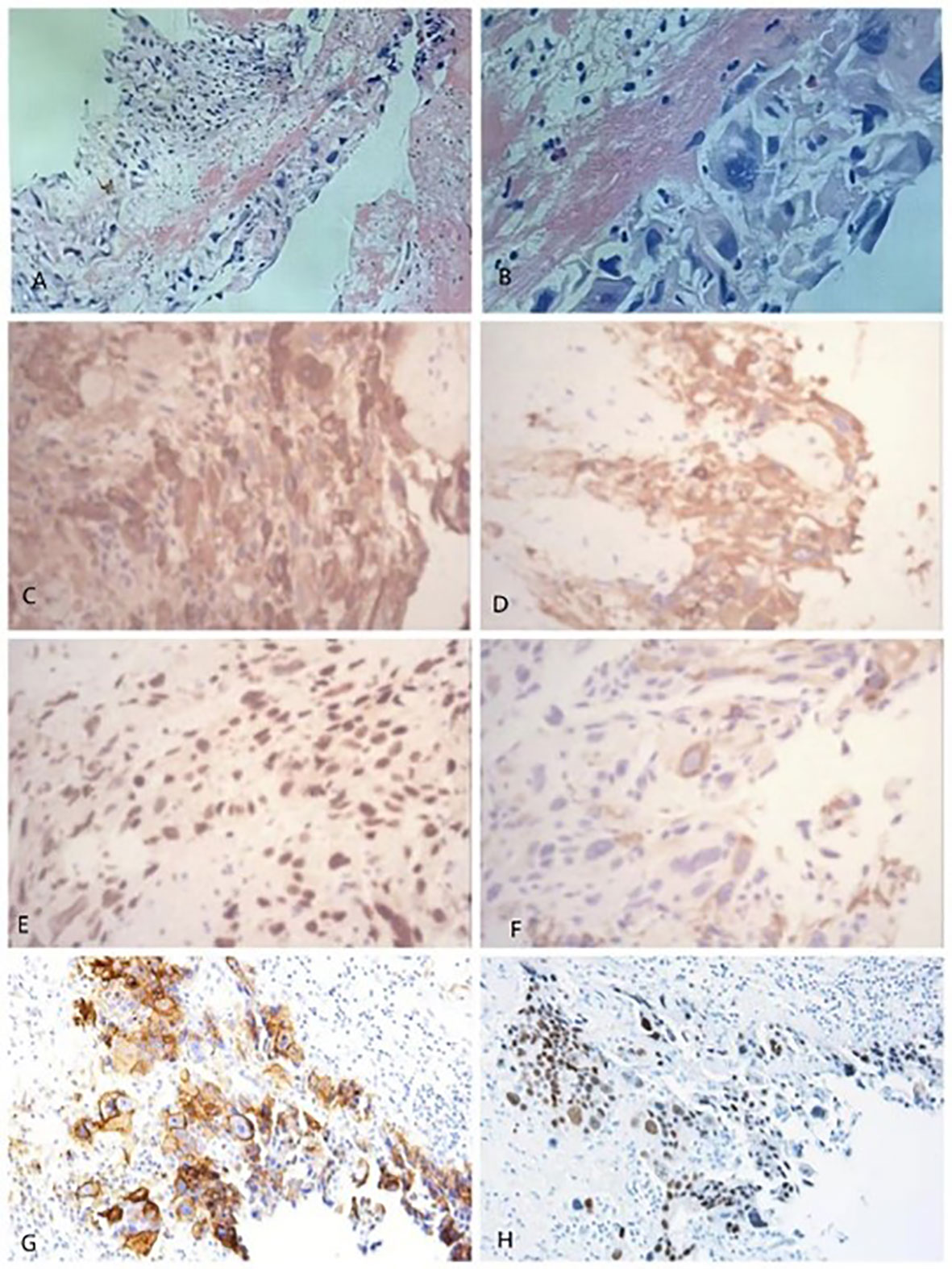
Figure 2 HE staining: Figure (B) is a partial enlargement of figure (A). (B): Fibrinous-like material is present in the upper left corner, and neoplastic trophoblasts are present in the lower right corner, with large hyperchromatic nuclei and no villi, as well as strongly positive immunohistochemical staining of the tumor at 40× magnification: (C) β-hCG; (D) CK 8/18; (E) Ki-67; and (F) HPL; and at 20× magnification: (G) CD10; (H) GATA-3. The pathological diagnosis was chorionic epithelial carcinoma of the left lower lobe of the lung, and the diameter of the lesion was approximately 10 cm. Most of the lesion was necrotic, and only a few tumor cells were visible.
The patient’s postoperative vital signs were normal, and no serious adverse reactions occurred. We advised the patient to review HCG and to undergo chemotherapy, but the patient refused due to economic and social factors. After a period of postoperative treatment, the patient recovered well and was discharged after completing a series of examinations, and it was recommended that the patient be reexamined regularly. A follow-up 5 years later showed that the patient had recovered well, with no recurrence or metastasis of the lung or other sites detected by chest CT and physical examinations.
Our report depicts a difficult situation in which the diagnosis of PPC was unexpected in women who were not pregnant but had elevated β-hCG levels (Figure 3). As can be seen in this case, no specific features contributed to the diagnosis of PPC, which was confirmed by postsurgical biopsy. Combined with other published cases of primary pulmonary choriocarcinoma (Table 1), the preoperative diagnosis of PPC is difficult unless β-hCG is determined for other reasons (12). In this case, the patient’s two CT examinations failed to diagnose the type of disease, demonstrating that CT examinations with high clinical diagnostic value for other common lung diseases are not helpful for the diagnosis in PPC. CT scans, on the other hand, can be used for the precise localization of lesions, as well as for searching for primary and metastatic lesions of tumors due to their convenience and high-density resolution.
Primary choriocarcinoma, also known as non-gestational choriocarcinoma, is different from gestational choriocarcinoma. The former is not related to pregnancy, originates from primordial germ cells, and can occur in both men and women. It generally occurs in the gonadal organs but also in the midline outside the gonads (such as brain-pineal gland, mediastinum, retroperitoneum), and even other organs (e.g., stomach, lung, pancreas) (7).
It is important to note that primary choriocarcinoma of the lung should be differentiated from giant cell carcinoma of the lung (13), as both diseases are associated with a lung mass and elevated β-hCG levels (11). However, the number and volume of multinucleated giant cells in giant cell carcinoma of the lung are lower than in PPC, and the level of β-hCG elevation is similarly lower. Furthermore, PPC must be differentiated from other types of pulmonary lesions (14). In this case, the patient exhibited a cough, sputum, fever, and other obvious symptoms, which are common manifestations of pulmonary infections, and this is why the patient was initially misdiagnosed with a pulmonary cyst complicated with infection. Pulmonary inflammatory pseudotumor (15) and organizing pneumonia (16) are also symptoms of pulmonary infection that must be differentiated during the diagnosis process. On CT images, organizing pneumonia presents as diffuse lesions in the lungs, whereas pulmonary inflammatory pseudotumors and PPCs appear as nodules or masses in the lungs. PPC, on the other hand, always has an unclear border and may be accompanied by villous bulges. When distinguishing between them is challenging, an enhanced CT (17) or lung biopsy should be performed to further clarify the nature of the disease.
The tumor in this case originated in the lung, which is unusual compared with the previously common choriocarcinoma (18). Although this is not the first case, the conception of the cellular origin and pathogenesis of PPC is still limited (19). Here are several popular theories. The first theory is that it originates from the ectopic position of primordial germ cells in the lungs during embryonic development. The second theory is that PPC is a high-level transformation of non-trophoblastic lung tumors. The third theory is that primary choriocarcinoma of the lung is the same as giant cell carcinoma of the lung (6, 20). Because the patient was not pregnant, the second theory is more likely to explain this occurrence.
Regarding the diagnosis of primary choriocarcinoma, there was no significant difference in the pathological morphology between gestational choriocarcinoma and non-gestational choriocarcinoma, and the immunohistochemical results could be CK (+) and HCG (+), but from the point of origin and tissue, they were significantly different. Gestational choriocarcinoma is a tumor transformed from allogeneic cells with male components, so it has strong immunogenicity or antigenicity, whereas non-gestational choriocarcinoma is a tumor transformed from autologous cells, which has low immunogenicity or antigenicity. The precise differentiation requires polymorphism analysis of the tumor genome. Therefore, it is necessary to check the presence of paternal gene in the tumor tissue to confirm the diagnosis of this patient (21). Short tandem repeat (STR) genotyping is currently the most suitable method for identity detection (22).
Due to the poor survival rate of patients with PPC, early accurate diagnosis and aggressive treatment are crucial. In this case, the follow-up after 5 years showed a good recovery, which again confirmed that the diagnosis was consistent with PPC. Previous studies have shown that patients who are actively treated have longer survival than those who are not treated, and the survival rate of the surgical group is higher than that of the non-surgical group according to the different treatment methods (7). Although PPC is a highly malignant tumor, there is no standard treatment for it due to its rarity. Treatment strategies for PPC in published cases have included complete excision, chemotherapy, radiation therapy, and supportive care, which are the same as those for gestational choriocarcinoma (3, 23). Surgical resection is an effective treatment for PPC, particularly for isolated lung lesions, when combined with postoperative chemotherapy to prevent tumor metastasis to other sites (5, 24). Etoposide, carboplatin, bleomycin, and methotrexate are examples of common chemotherapy drugs (3, 6). Furthermore, patients with choriocarcinoma who are resistant to chemotherapeutic drugs can be treated with a combination of toripalizumab and surgery (25).
In conclusion, primary pulmonary choriocarcinoma is very rare and difficult to diagnose, and elevated β-hCG levels are characteristic of the disease. According to current research, the combination of surgery and chemotherapy has a superior effect. Further research on appropriate treatment options and factors affecting survival is needed to improve the prognosis of patients with PPC.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Institutional Review Board of Shandong Provincial Hospital Affiliated to Shandong First Medical University Subcommittee on Human Studies. The patient provided written informed consent to participate in this study. Written informed consent was obtained from the individual for the publication of any potentially identifiable images or data included in this article.
NW and NZ wrote the main manuscript text and contributed equally. XZ and YW prepared figures. YF collected the clinical data and imaging data. LG, CL, and MY revised the manuscript text. All authors revised the manuscript and approved the submitted version.
This study was funded by the Project ZR2021QH180 supported by Shandong Provincial Natural Science Foundation.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ben Abdallah I, Mlika M, Berrazega Y, Mejri N, Rachdi H, El Benna H, et al. Amenorrhea and elevated betahuman chorionic gonadotropin of unknown origin: an unexpected location of choriocarcinoma. Gynecol Oncol Rep (2021) 36:100746. doi: 10.1016/j.gore.2021.100746
2. Wu PS. Primary choriocarcinoma of the lung: a case report and literature review. Int J Clin Exp Pathol (2020) 13(9):2352–5.
3. Dlewati MM, Gonzalez T, Razi SS, Hussain SF, Bennett J. Primary pulmonary choriocarcinoma treated with neoadjuvant chemotherapy and lobectomy: a case report. Cureus (2022) 14(2):e21931. doi: 10.7759/cureus.21931
4. Ji YS, Park SH. Clinical experience of Male primary choriocarcinoma at the Samsung medical center. Cancer Res Treat (2021) 53(3):874–80. doi: 10.4143/crt.2020.1066
5. Chen F, Tatsumi A, Numoto S. Combined choriocarcinoma and adenocarcinoma of the lung occurring in a man: case report and review of the literature. Cancer (2001) 91(1):123–9. doi: 10.1002/1097-0142(20010101)91:1<123::AID-CNCR16>3.0.CO;2-3
6. Rali P, Xie J, Rali G, Rali M, Silverman J, Malik K. A rare case of metastatic choriocarcinoma of lung origin. Case Rep Pulmonol (2017) 2017:4649813. doi: 10.1155/2017/4649813
7. Zhang X, Ding B, Chen L, Huang X, Zhang K, Wang Z, et al. Primary pulmonary choriocarcinoma in male: report a case with genetic testing and review of the literature. Transl Cancer Res (2022) 11(6):1844–9. doi: 10.21037/tcr-21-2627
8. Johnson AM, Johnson CM, Khalil Z, Stitzel M, Teoh D. Case report: treatment of primary pulmonary choriocarcinoma with lung lobectomy and adjuvant chemotherapy. Gynecol Oncol Rep (2022) 43:101064. doi: 10.1016/j.gore.2022.101064
9. Nguyen HTT, Hoang HH, Le ATV. A case report of primary pulmonary choriocarcinoma in a man: successful combination of surgery and chemotherapy. Case Rep Oncol (2020) 13(2):923–8. doi: 10.1159/000508744
10. Onishi I, Kirimura S, Wakejima R, Okubo K, Odai T, Kakuta R, et al. Primary pulmonary choriocarcinoma with a genomic sequence. Pathol Int (2022) 72(2):141–3. doi: 10.1111/pin.13193
11. Ikura Y, Inoue T, Tsukuda H, Yamamoto T, Ueda M, Kobayashi Y. Primary choriocarcinoma and human chorionic gonadotrophin-producing giant cell carcinoma of the lung: are they independent entities? Histopathology (2000) 36(1):17–25. doi: 10.1046/j.1365-2559.2000.00789.x
12. Kamata S, Sakurada A, Sato N, Noda M, Okada Y. A case of primary pulmonary choriocarcinoma successfully treated by surgery. Gen Thorac Cardiovasc Surg (2017) 65(6):361–4. doi: 10.1007/s11748-016-0666-8
13. Habib S, Leifer LE, Azam M, Siddiqui AH, Rajdev K, Chalhoub M. Giant cell carcinoma of the lung successfully treated with surgical resection and adjuvant vinorelbine and cisplatin. Respir Med Case Rep (2018) 25:300–2. doi: 10.1016/j.rmcr.2018.10.012
14. Kim JH, Cha MJ, Kim MK, Chung YJ, Lee EJ. Disseminated primary pulmonary choriocarcinoma successfully treated by chemotherapy: a case report and literature review. Cancer Invest (2020) 38(8-9):493–501. doi: 10.1080/07357907.2020.1804575
15. Kim JH, Cho JH, Park MS, Chung JH, Lee JG, Kim YS, et al. Pulmonary inflammatory pseudotumor–a report of 28 cases. Korean J Intern Med (2002) 17(4):252–8. doi: 10.3904/kjim.2002.17.4.252
16. Cherian SV, Patel D, Machnicki S, Naidich D, Stover D, Travis WD, et al. Algorithmic approach to the diagnosis of organizing pneumonia: a correlation of clinical, radiologic, and pathologic features. Chest (2022) 162(1):156–78. doi: 10.1016/j.chest.2021.12.659
17. Wang XL, Shan W. Application of dynamic CT to identify lung cancer, pulmonary tuberculosis, and pulmonary inflammatory pseudotumor. Eur Rev Med Pharmacol Sci (2017) 21(21):4804–9.
18. Jiao L, Ghorani E, Sebire NJ, Seckl MJ. Intraplacental choriocarcinoma: systematic review and management guidance. Gynecol Oncol (2016) 141(3):624–31. doi: 10.1016/j.ygyno.2016.03.026
19. Takahashi T, Kobayashi R. Choriocarcinoma syndrome after resection of primary pulmonary choriocarcinoma: report of a case. Surg Case Rep (2016) 2(1):122. doi: 10.1186/s40792-016-0227-5
20. Słodkowska J, Kamiński Z, Decker E, Broniek A, Radomski P. Are lung choriocarcinoma and giant cell carcinoma producing chorionic gonadotropins just variants of the same neoplasm? Pneumonol Alergol Pol (1996) 64(11-12):798–804.
21. Jia N, Chen Y, Tao X, Ou E, Lu X, Feng W. A gestational choriocarcinoma of the ovary diagnosed by DNA polymorphic analysis: a case report and systematic review of the literature. J Ovarian Res (2017) 10(1):46. doi: 10.1186/s13048-017-0334-3
22. da Silva FF, Barata R, Rolim I, Carvalheiro C, Gil N, Pantarotto M. Case report: using DNA short tandem repeats to confirm nongestational origin of pulmonary choriocarcinoma. Front Oncol (2022) 12:1001627. doi: 10.3389/fonc.2022.1001627
23. Yun J, Lee SW, Lim SH, Kim SH, Kim CK, Park SK. Successful treatment of a high-risk nonseminomatous germ cell tumor using etoposide, methotrexate, actinomycin d, cyclophosphamide, and vincristine: a case report. World J Clin Cases (2020) 8(21):5334–40. doi: 10.12998/wjcc.v8.i21.5334
24. Ngu SF, Ngan HYS. Surgery including fertility-sparing treatment of GTD. Best Pract Res Clin Obstet Gynaecol (2021) 74:97–108. doi: 10.1016/j.bpobgyn.2020.10.005
Keywords: primary pulmonary choriocarcinoma, β-human chorionic gonadotropin, differential diagnosis, computerized tomography, treatment
Citation: Wang N, Zhang N, Zhang X, Wang Y, Fu Y, Guo L, Liang C and Yu M (2023) The tumor or inflammation? a case report on primary pulmonary choriocarcinoma. Front. Oncol. 13:1108798. doi: 10.3389/fonc.2023.1108798
Received: 26 November 2022; Accepted: 27 June 2023;
Published: 13 July 2023.
Edited by:
Anthonie J Van Der Wekken, University Medical Center Groningen, NetherlandsReviewed by:
Etienne Marbaix, Université Catholique de Louvain, BelgiumCopyright © 2023 Wang, Zhang, Zhang, Wang, Fu, Guo, Liang and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mengru Yu, eXVtZW5ncnVAc2RmbXUuZWR1LmNu
†These authors have contributed equally to this work and share the first authorship
‡ORCID: Na Wang, orcid.org/0000-0001-6191-4760
Nan Zhang, orcid.org/0000-0002-6202-9349
Xinyue Zhang, orcid.org/0000-0003-1643-608X
Yuanyuan Wang, orcid.org/0000-0002-0641-8411
Yajie Fu, orcid.org/0000-0002-1195-5764
Lingfei Guo, orcid.org/0000-0002-4885-625X
Changhu Liang, orcid.org/0000-0003-3796-2978
Mengru Yu, orcid.org/0000-0002-9339-3477
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.