
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol. , 16 March 2023
Sec. Surgical Oncology
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.1085634
This article is part of the Research Topic Video-Assisted Surgery in Oncology View all 13 articles
Objectives: Video-assisted thoracoscopic lobectomy has become the preferred surgical approach in experienced centers, and uniportal approaches are becoming increasingly used. But the uniportal approach is still not widely applied presumably due to the learning difficulties of this complex procedure. The use of surgical videos may be helpful to accelerate the learning of this new techniques as in other fields. In this study, we aimed to analyze the learning curve of uniportal video-assisted thoracoscopic lobectomy with the help of postoperative review of videos.
Methods: 114 patients with early-stage lung cancer who underwent uniportal video-assisted thoracoscopic lobectomy performed from 2020 to 2021 were reviewed in this study. We recorded the operation video for each patient and reviewed all the videos after surgery. The learning curves were assessed using cumulative sum analysis and the collected data of perioperative outcomes were assessed.
Results: The CUMSUM curve showed its inflection points were around case 38 and 53. It was less compared with previous studies, which about 57–140 cases are needed to attain the proficient phase. The perioperative outcomes were similar in each phase, which included intraoperative blood loss (79.00 ± 26.70 vs 70.67 ± 26.64 vs 70.56 ± 27.23, p=0.0119), the length of hospital stay (3.60 ± 1.52 days vs. 3.23 ± 0.90 days vs. 3.06 ± 0.88 days, p=0.053), the rate of prolonged air leak and conversion to open thoracotomy. There was also no significant difference in the numbers and station of lymph node dissection among the three phases.
Conclusions: Uniportal video-assisted thoracoscopic lobectomy is a safe and reliable approach. Recording and reviewing the operation video could help the surgeon to improve deficiencies and refine the procedure.
With the full implementation of screening and the development of high-resolution computed tomography, the detection rate of early stage lung cancer has significantly increased (1). Minimally invasive surgery, which includes video-assisted thoracoscopic surgery (VATS), has become the preferred approach for the curative treatment of early stage lung cancer (2, 3).
In the last decade, VATS lobectomy has become the preferred surgical approach in experienced centers, and is usually performed through 2–4 ports. Uniportal VATS (U-VATS) is based on the conventional VATS with reduced auxiliary operation ports. However, the U-VATS technique is still not widely applied in most medical centers, presumably due to the learning difficulties of this complex procedure (4–8).
Video review has been proved to be a useful tool for learning new skills in many fields such as athletics, modern drama and aviation. The use of surgical videos is also emerging as a powerful tool to facilitate the acquisition of new surgical skills and to accelerate the learning of new techniques (9, 10). However, these studies are usually limited to the study of multiportal laparoscopic technology and there is no research report on the uniportal thoracoscopy technology. In this study, we aimed to describe our experience in 114 consecutive cases and to analyze the learning curve of uniportal video-assisted thoracoscopic lobectomy with the help of video-assisted operative feedback.
This retrospective study was reviewed and approved by the ethics committee of the Shanghai Chest Hospital. All patients have signed the written informed consent before the operation. All operations were performed by the same surgeon (Dr. Xinghua Cheng) from Shanghai Chest Hospital, which had performed 88 cases of multiportal thoracoscopic lobectomy before. Totally 114 consecutive patients who underwent uniportal VATS lobectomy from May 2020 to August 2021 were reviewed in this study.
The patients were maintained in the lateral decubitus position and 1-lung ventilated with double-lumen endotracheal intubation, received general anesthesia. The surgeon was on the patient’s abdominal side, and the assistant was on the opposite side (the back of the patient). A 2.5 to 3 cm hole was made at the fifth intercostal space on the middle axillary line. Wound protectors were used at the incision to facilitate exposure and simplify instrumentation.
The camera was positioned on the posterior portion of the incision. The staplers were always introduced through the most anterior portion of the incision, below any other instrument, and fissures were always cut with energy sealing devices. The bronchus, vein and artery were divided anatomically, and dissected separately using endoscopic staplers or ligated by using hem-o-locks before dissection. 24 Fr chest tubes were inserted through the incision at the end of the operations, and we would remove the chest tube if the patient’s volume of drainage was less than 200ml per day and there was no air leakage.
We recorded the operation video for each patient and reviewed the videos after surgery. The video recording was started with the introduction of a dissector and concluded with the removal of the target lobe and lymph nodes. All videos were assessed from three domains of bimanual dexterity, efficiency and tissue handling based on the surgical performance. Besides, all the operation videos were analyzed for frequency of minor technical errors and adverse events after surgery. Minor errors included insufficient exposure, wrong pass angle of cutting stapler, dropping tissue or suture. Examples of adverse events included excessive blood loss, tears of lung or bronchus requiring repair. Meeting quarterly, we reviewed the ‘‘typical’’ and ‘‘challenging’’ operation videos with senior surgeons to share best practices and identify where the technique could be improved.
All patients were characterized by demographic and clinical variables, including sex, age, smoking history, body mass index (BMI), Charlson comorbidity index (CCI), forced expiratory volume in 1 s (FEV1), diffusion capacity of the lung for carbon monoxide (DLCO), pathology, tumor size, operation procedure, and lymph node (LN) status. Surgical outcomes included procedure time, intraoperative blood loss, postoperative hospital stay, complications, and lymph node retrieval. Procedure time was defined as the time from the first incision to complete closure of the skin. Prolonged air leakage was defined as air leakage lasting for >5 days postoperatively. Perioperative mortality included death during hospitalization or within the first 30 days after the operation.
Statistical analysis was performed using SPSS software (version 18.0; SPSS, Inc., Chicago, IL) and R (version 3.6.2). Data are shown as mean (standard deviation) or median (interquartile range) for continuous variables and as n (%) for categorical variables. Differences between groups were analyzed using one-way analysis of variance or the Kruskal-Wallis H test. Fisher’s exact test or chi-square test was used to classify variables. A two-sided P-value < 0.05 was considered statistically significant. The cumulative sum (CUSUM) analysis method was used to quantitatively assess the learning curve. CUSUM for operation time was calculated as follows: , where xi and u respectively represent an individual and the mean overall operative time (6). In addition, we established a polynomial trend line to show the change in the slope of the learning curve. According to the learning curve obtained from the analysis, we divided it into three stages: the ascending phase (Phase I), the transition phase (Phase II), and the maturity phase (Phase III).
Altogether, 114 patients who undergoing U-VATS lobectomy performed by a single surgeon between May 2020 and August 2021 were enrolled in this study. The baseline characteristics of the patients are shown in Table 1. Of the 114 patients, 50(43.86%) were men and 64(56.14%) were women. The median age of the patients was 61 years. Adenocarcinoma was the most frequent histologic type(87 patients, 76.3%), and the mean tumor diameter was 21.00 ± 12.80 mm. Detailed patient characteristics are presented in Table 1. When clinical demographics and characteristics were assessed for the three periods of the learning curve, there were no significant differences between patients in each learning period.
The raw operative time for all 114 patients is shown in Figure 1B. As the number of procedures increased, the operation time decreased and became stable eventually. The learning curve for operative time is shown in Figure 1A. According to the trend and inflection points of the curve, we obtained three well-differentiated phases: phase I (1–35 cases), phase II (36–53 cases), and phase III (54–114 cases). Phase I was the ascending slope of the curve, which represented the initial experience of the technique learning, and Phase II was the transition part of the curve, which represented further improvement in surgical skills. Phase III was the descending slope, which indicated that proficiency had been achieved.
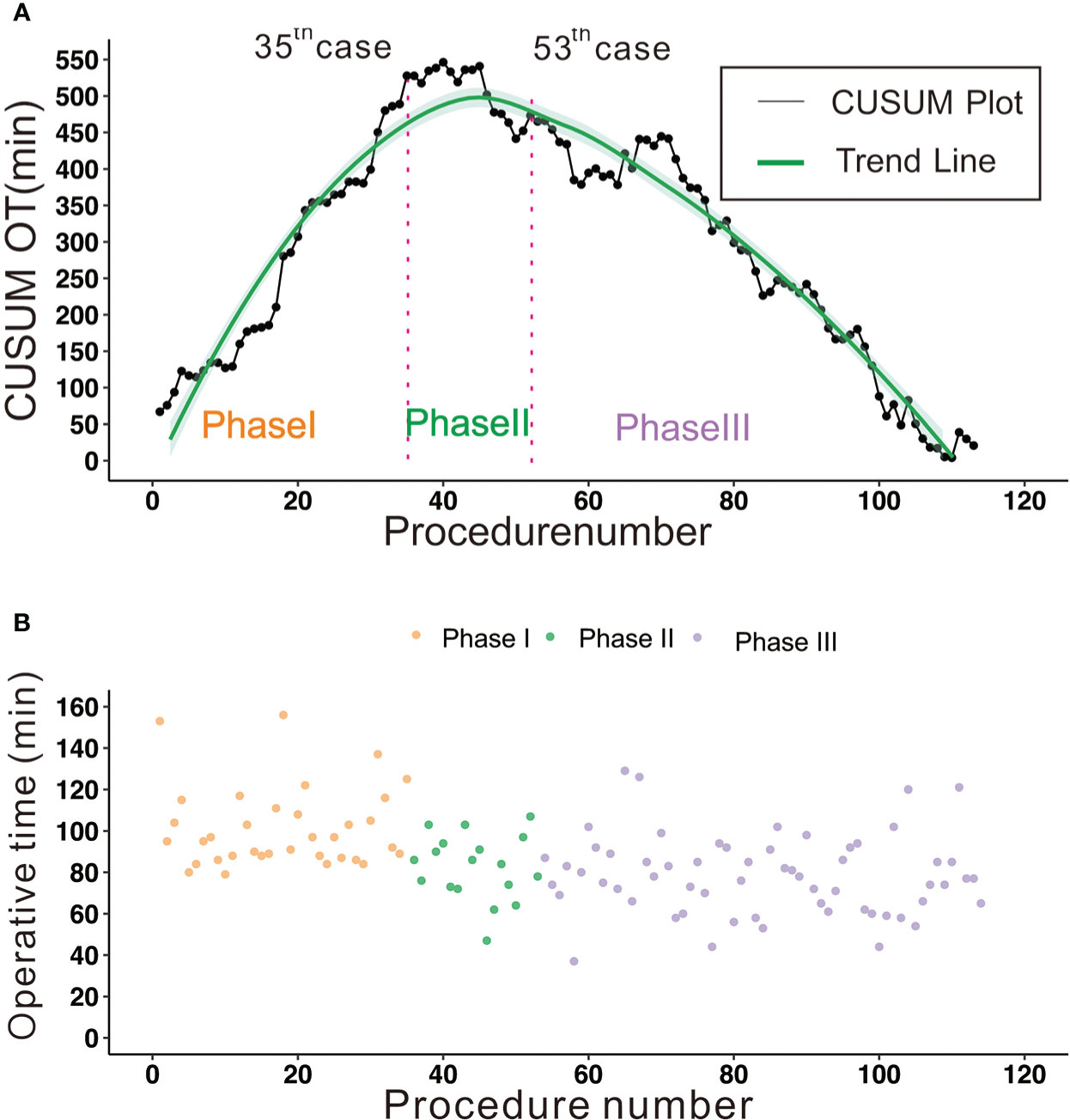
Figure 1 (A) The CUSUM curve of operative time; 35 cases were needed to lay the technical foundation and 53 cases were necessary to achieve proficiency. Phase I: 1-35 cases, learning phase. Phase II: 36-53 cases, transition phase. Phase III: 54-114 cases, proficiency phase. (B) The raw operative times were plotted in chronologic surgery order.
In the all patients, the mean operative time and length of stay were 86.09 ± 21.23 minutes and 3.25 ± 1.10 days (Table 1). No patient died perioperatively, and two cases were converted to open thoracotomy due to severe adhesions in thoracic cavity (1 case) and vascular accident (1 case). Only four patients (3.5%) experienced prolonged air leak after surgery.
In the subgroup analysis, the operative time improved from a mean of 99.40 ± 18.72 minutes to 78.78 ± 19.36 minutes, with a significant difference (p<0.001). Intraoperative blood loss tended to decrease, but there was no significant difference between the three phases (P = 0.119) (Figure 2A). The length of hospital stay was reduced (3.60 ± 1.52 days vs. 3.23 ± 0.90 days vs. 3.06 ± 0.88 days), but this was not statistically significant (P = 0.053) (Figure 2B). There was no significant difference in the stations (p=0.521) or numbers (p=0.086) of lymph node dissection among the three phases (Figure 3).
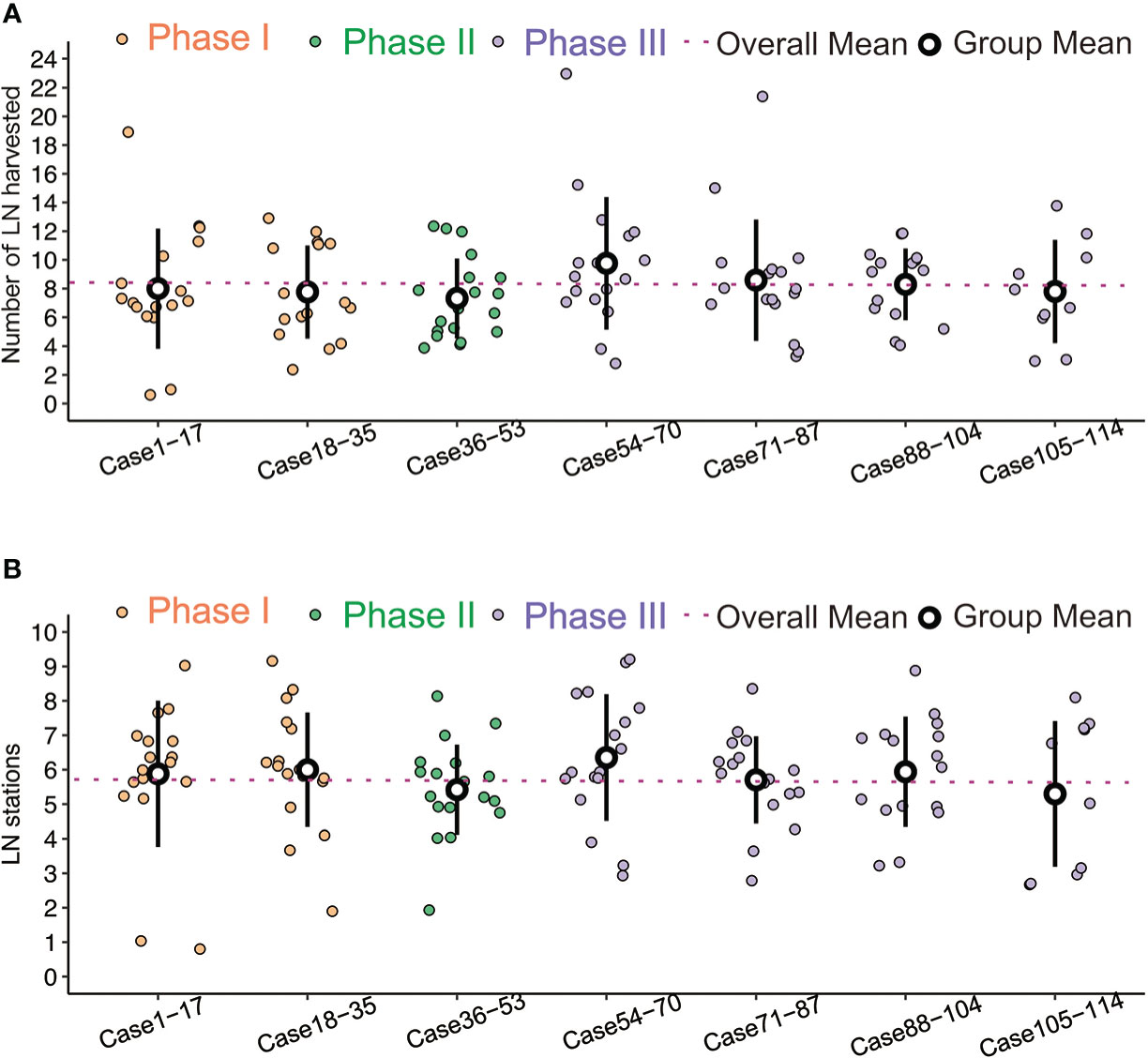
Figure 2 (A) Comparisons of blood loss, no significant difference between the three phases. (B) Comparisons of postoperative stay, no significant difference between the three phases.
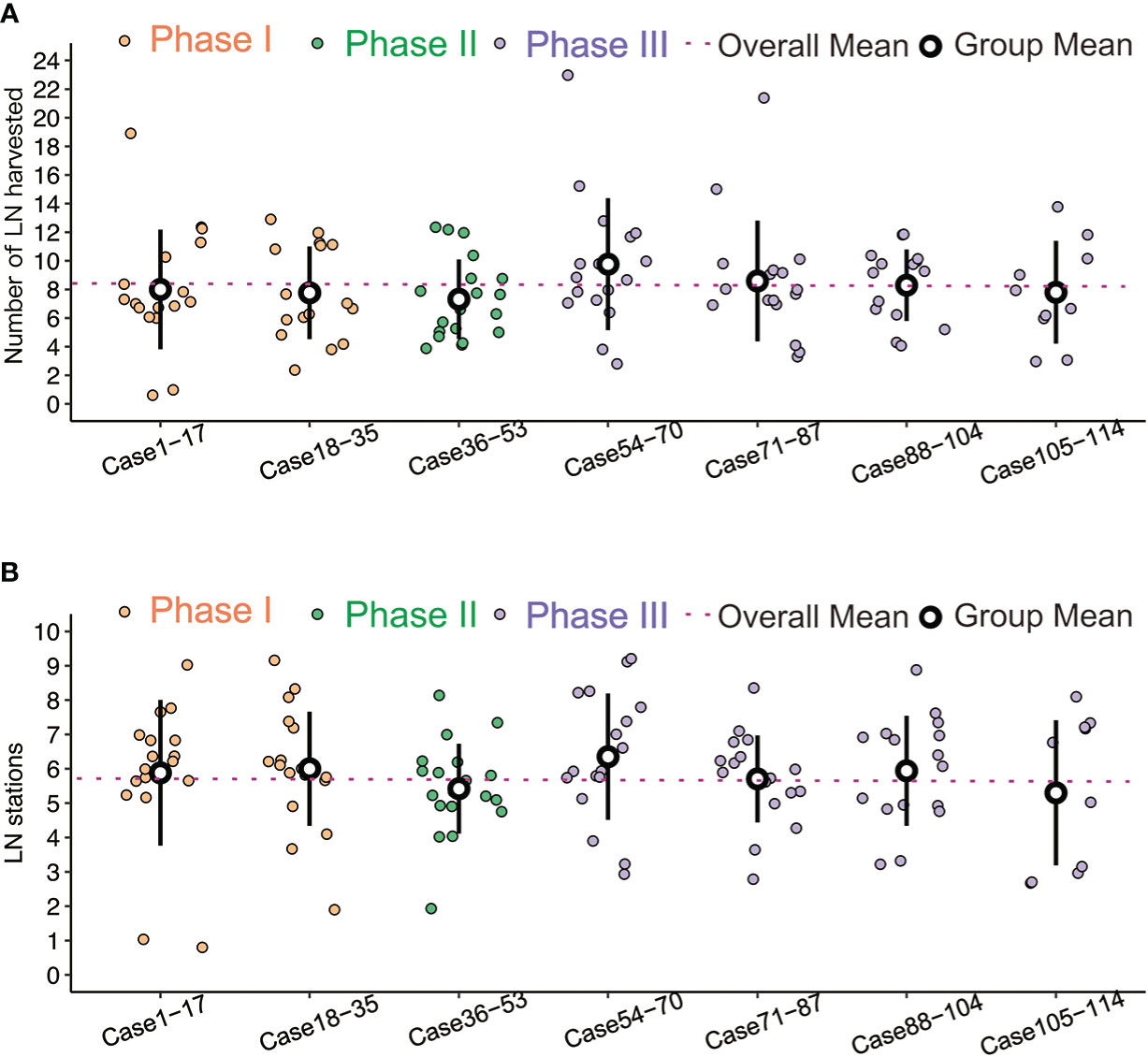
Figure 3 (A) Comparisons of LN harvested number, no significant difference between the three phases. (B) Comparisons of LN station, no significant difference between the three phases.
U-VATS lobectomy has been proven to be a safe and feasible surgical approach for early stage lung cancer (11–13). However, it is not widely applied in most medical centers because of technical difficulties. Currently, the use of surgical videos by surgeons facilitate the learning of new procedures and techniques (9, 10). Surgical videos could record the frequency of minor technical errors and adverse events. Surgeons can review these videos to continuously reduce and correct these errors, thereby reducing the incidence rate of potential patients’ morbidity. There is always a sharp contrast between what the surgeons think they did and what actually happened, postoperative review of videos would be helpful for operators to addresses important cognitive limitations (14–17). Besides, reviewing the ‘‘typical’’ and ‘‘challenging’’ operation videos with senior surgeons allows accurate assessment and identifying where the technique could be improved. All of the above can help improve surgical techniques, thus to accelerate the learning curve of surgeons and improve the surgical safety. Nevertheless, most of the research on video learning is limited to laparoscopic technology, there is few research focus on the thoracoscopy technology, especially on the uniportal thoracoscopy technology.
In the present study, we analyzed 114 cases of U-VATS lobectomy performed by a single surgeon using the CUSUM method to evaluate how video review promotes the learning curve. It took 35 consecutive cases of U-VATS lobectomy to complete the ascending phase and 18 additional cases to overcome the transition phase. In other words, efficacy was achieved after 35 cases and proficiency was achieved after 53 cases. No patient died preoperatively, regardless of the phase of the learning curve. There was no significant difference between the three phases in terms of both intraoperative blood loss and length of hospital stay. There was also no significant difference in the number and station of lymph node dissection among the three phases. These results indicate that U-VATS lobectomy is safe and reliable, even during the initial phase of learning the technique.
So far, studies have been carried out in large-volume centers to analyze the learning curve of U-VATS lobectomy regardless of video review (Table 2) (7, 18–20). According to the results of these study, about 57–140 cases are needed to attain the proficient phase. Compared with our results, this number is obviously higher than required, which may indicate that video review can accelerate the learning curve of surgeons. Moreover, almost all previous studies showed that the amount of blood loss and length of hospital stay showed a downward trend among the three distinct periods of the learning curve. In other words, the other surgeons’ operations were not sufficiently stable at the beginning of the learning curve. However, in our study, all the perioperative outcomes of patients in the three phases were comparable. This may be what was caused by the earlier mentioned video review that can help reduce intraoperative errors and improve surgical safety. Besides, in some of these previous studies (7), there was significant difference in the numbers or stations of lymph node removed because of performing lymph node dissection through the uniportal technique remains challenging. But there was no significant difference in the numbers and stations of lymph node dissection among the three phases of our study. The comparative analysis of these research results all suggest that video review can help surgeons learn uniportal thoracoscopy more quickly and safely.
Video review is associated with shortened learning curve and reduced intraoperative accidents such as bleeding probably implicates accelerated self-improvement of surgical skills. It is particularly important when new technique is to be implemented or to be transferred to new trainees. By recording surgical videos, surgeons can not only review by themselves but also compare the videos with the operations from more experienced surgeons, and ask for suggestion from senior peers. For intraoperative accidents, it is easier for the surgeon to re-think how to confound and avoid similar situations after the surgery. Besides, a surgical video database is important for surgical education and generate future artificial intelligence guided surgical programs (21, 22). Video review is very practical and eliminates many inconveniences and risks associated with on-site surgical guidance. It can also be of great help in the training and education of surgical residents (23). The emergence of complex thoracoscopic and robotic surgeries transfers surgical experience from junior residents to more advanced trainees. Intraoperative learning is further limited by increasing concerns for patient safety and the possibility that resident teaching may prolong surgery time. These challenges indicate a need for innovative educational strategies to maximize the learning of operative skills (24). The electronic transmission of video is well suited for remote viewing without the limitations of location and environment. Surgical residents can use fragmented time to conduct video review and analysis freely. In addition, they can share videos with peers or more experienced surgeons to obtain feedback. Nowadays, most thoracoscopic equipment comes with video recording capability, making video recording of surgeries very easy. With the fast development of imaging and AI technologies, video review methods will become an increasingly valuable tool to accelerate innovation and promote safer surgeries.
Despite our best efforts, this study has some limitations. First, this study was a retrospective study, in which the selection bias is inevitable. Second, the residents, fellows, and nursing teams were not the same for every procedure. There was no definite evidence to demonstrate whether these could have impacted the learning curve. Third, there was no clear definition of a ‘‘learning curve’’ for this procedure, and there were varying definitions of proficiency (25–27).
In conclusion, uniportal VATS lobectomy is a safe and reliable approach, and the surgeon with the help of postoperative review of videos is better able to improve deficiencies and can better refine the procedure. In the results of our study, with the help of video review, efficacy was reached after 35 cases, and proficiency was achieved after 53 cases.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the ethics committee of the Shanghai Chest Hospital. The patients/participants provided their written informed consent to participate in this study.
XC and QL conceived and designed the study. ZS and YY wrote the paper. CC performed data analysis. ZS and XC reviewed and edited the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by funding awarded to Dr. CC by the National Natural Science Foundation of China (82073191), the Shanghai Municipal Science & Technology Commission Research Project (18441901500), Shanghai Municipal Health Commission Research Project (no. 2019SY047), the Innovative Research Team of High-level Local Universities in Shanghai (SHSMU-ZLCX20212302), the Shanghai Chest Hospital Project of Collaborative Innovation (no. YJXT20190105) and Shanghai Chest Hospital Research Support Program 2019YNJCM15.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
VATS, video -assisted thoracoscopic surgery; BMI, Body mass index; ASA, American Society of Anesthesiology; CCI, Charlson comorbidity index; DLCO, Diffusion capacity of the lung for carbon monoxide; FEV1, Forced expiratory volume in 1 s; LN, Lymph node.
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2021) 71:209–49. doi: 10.3322/caac.21660
2. Thai AA, Solomon BJ, Sequist LV, Gainor JF, Heist RS. Lung cancer. Lancet (2021) 398:535–54. doi: 10.1016/S0140-6736(21)00312-3
3. Swanson SJ, Herndon JE 2nd, D’Amico TA, Demmy TL, McKenna RJ Jr, Green MR, et al. Video-assisted thoracic surgery lobectomy: Report of CALGB 39802–a prospective, multi-institution feasibility study. J Clin Oncol (2007) 25:4993–7. doi: 10.1200/JCO.2007.12.6649
4. Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: Comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg (2005) 28:43–6. doi: 10.1016/j.ejcts.2005.02.039
5. Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg (2004) 77:726–8. doi: 10.1016/S0003-4975(03)01219-0
6. Shen Y, Wang H, Feng M, Xi Y, Tan L, Wang Q. Single- versus multiple-port thoracoscopic lobectomy for lung cancer: A propensity-matched studydagger. Eur J Cardiothorac Surg (2016) 49 Suppl 1:i48–53. doi: 10.1093/ejcts/ezv358
7. Vieira A, Bourdages-Pageau E, Kennedy K, Ugalde PA. The learning curve on uniportal video-assisted thoracic surgery: An analysis of proficiency. J Thorac Cardiovasc Surg (2020) 159(6):2487–95.e2482. doi: 10.1016/j.jtcvs.2019.11.006
8. Drevet G, Ugalde Figueroa P. Uniportal video-assisted thoracoscopic surgery: safety, efficacy and learning curve during the first 250 cases in Quebec, Canada. Ann Cardiothorac Surg (2016) 5:100–6. doi: 10.21037/acs.2016.03.05
9. Coco D, Leanza S. Video-learning in surgical training: Is it a method to improve preparation of surgical residents? N Engl J Med (2021) 01:15588–91. doi: 10.24941/ijcr.40376.01.2021
10. Ibrahim AM, Varban OA, Dimick JB. Novel uses of video to accelerate the surgical learning curve. J Laparoendosc Adv Surg Tech A (2016) 26(4):240–2. doi: 10.1089/lap.2016.0100
11. Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: A retrospective comparative study of perioperative clinical outcomesdagger. Eur J Cardiothorac Surg (2016) 49 Suppl 1:i37–41. doi: 10.1093/ejcts/ezv320
12. Gonzalez-Rivas D, Sihoe ADL. Important technical details during uniportal video-assisted thoracoscopic major resections. Thorac Surg Clin (2017) 27:357–72. doi: 10.1016/j.thorsurg.2017.06.004
13. Moon Y. Initial experience with uniportal video-assisted thoracoscopic surgery for the treatment of lung cancer performed by a surgeon who did not have previous experience performing multiportal thoracoscopic surgery: A single center retrospective study. J Thorac Dis (2020) 12:1972–81. doi: 10.21037/jtd-20-242
14. Fischer J, Geurts J, Valderrabano V, Hugle T. Educational quality of youtube videos on knee arthrocentesis. J Clin Rheumatol (2013) 19(7):373–6. doi: 10.1097/RHU.0b013e3182a69fb2
15. Bezner SK, Hodgman EI, Diesen DL, Clayton JT, Minkes RK, Langer JC, et al. Pediatricsurgery on YouTubeTM: Is the truth out there? J Pediatr Surg (2014) 49(4):586–9. doi: 10.1016/j.jpedsurg.2013.08.004
16. Rössler B, Lahner D, Schebesta K, Chiari A, Plöchl W. Medical information on the Internet: quality assessment of lumbar puncture and neuroaxial block techniques on YouTube. Clin Neurol Neurosurg (2012) 114(6):655–8. doi: 10.1016/j.clineuro.2011.12.048
17. Larouche M, Geoffrion R, Lazare D, Clancy A, Lee T, Koenig NA, et al. Mid-urethral slings on YouTube: quality information on the internet? Int Urogynecol J (2016) 27(6):903–8. doi: 10.1007/s00192-015-2908-1
18. Liu X, Chen X, Shen Y, Wang H, Feng MX, Tan LJ, et al. Learning curve for uniportal video-assisted thoracoscopic surgery lobectomy-results from 120 consecutive patients. J Thorac Dis (2018) 10:5100–7. doi: 10.21037/jtd.2018.08.87
19. Chen L, Pan Y, Zhang Q, Shao F, Ma GD, Yang RS. Learning curve for uniportal thoracoscopic anatomical pulmonary segmentectomy. Surg Innov (2020) 27(4):378–83. doi: 10.1177/1553350620932430
20. Li S, Wu J, Wan Z, Chen YY, She YL, Xie D, et al. The learning curve for uniportal video-assisted thoracoscopic anatomical segmentectomy. J Surg Oncol (2021) 124(3):441–52. doi: 10.1002/jso.26517
21. Madani A, Namazi B, Altieri MS, Hashimoto DA, Rivera AM, Pucher PH, et al. Artificial intelligence for intraoperative guidance: Using semantic segmentation to identify surgical anatomy during laparoscopic cholecystectomy. Ann Surg (2022) 276(2):363–9. doi: 10.1097/SLA.0000000000004594
22. Takeuchi M, Kawakubo H, Saito K, Maeda Y, Matsuda S, Fukuda K, et al. Automated surgical-phase recognition for robot-assisted minimally invasive esophagectomy using artificial intelligence. Ann Surg Oncol (2022) 29(11):6847–55. doi: 10.1245/s10434-022-11996-1
23. Herrera-Almario GE, Kirk K, Guerrero VT, Jeong K, Kim S, Hamad GG, et al. The effect of video review of resident laparoscopic surgical skills measured by self- and external assessment. Am J Surg (2016) 211(2):315–20. doi: 10.1016/j.amjsurg.2015.05.039
24. Hu YY, Peyre SE, Arriaga AF, Osteen RT, Corso KA, Weiser TG, et al. Postgame analysis: using video-based coaching for continuous professional development. J Am Coll Surg (2012) 214(1):115–24. doi: 10.1016/j.jamcollsurg.2011.10.009
25. Chaput de Saintonge DM, Vere DW. Why don’t doctors use cusums? Lancet (1974) 1:120–1. doi: 10.1016/S0140-6736(74)92345-9
26. Maguire T, Mayne CJ, Terry T, Tincello DG. Analysis of the surgical learning curve using the cumulative sum (CUSUM) method. Neurourol Urodyn (2013) 32:964–7. doi: 10.1002/nau.22375
Keywords: uniportal video-assisted thoracoscopic lobectomy, learning curves, review of videos, efficacy, proficiency
Citation: Song Z, Yuan Y, Cheng C, Luo Q and Cheng X (2023) The learning curve on uniportal video-assisted thoracoscopic lobectomy with the help of postoperative review of videos. Front. Oncol. 13:1085634. doi: 10.3389/fonc.2023.1085634
Received: 01 November 2022; Accepted: 06 March 2023;
Published: 16 March 2023.
Edited by:
Long Jiang, First Affiliated Hospital of Guangzhou Medical University, ChinaReviewed by:
Pietro Bertoglio, IRCCS Azienda Ospedaliero Universitaria di Bologna, ItalyCopyright © 2023 Song, Yuan, Cheng, Luo and Cheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinghua Cheng, Y2hlbmd4aW5naHVhXzAwMUAxNjMuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.