- 1Department of Ultrasound, Henan University People’s Hospital, Henan Provincial People’s Hospital, Zhengzhou University People’s Hospital, Zhengzhou, China
- 2Henan Engineering Technology Research Center of Ultrasonic Molecular Imaging and Nanotechnology, Henan Provincial People's Hospital, Zhengzhou, China
- 3Department of Ultrasound, First Affiliated Hospital of Zhengzhou University, Zhengzhou, China
- 4Department of Ultrasound, Henan Provincial Cancer Hospital, Zhengzhou, China
- 5Department of Health Management, Henan University People’s Hospital, Henan Provincial People’s Hospital, Zhengzhou University People’s Hospital, Zhengzhou, China
Objective: The purpose of this study was to investigate the preoperative prediction of Cytokeratin (CK) 19 expression in patients with hepatocellular carcinoma (HCC) by machine learning-based ultrasomics.
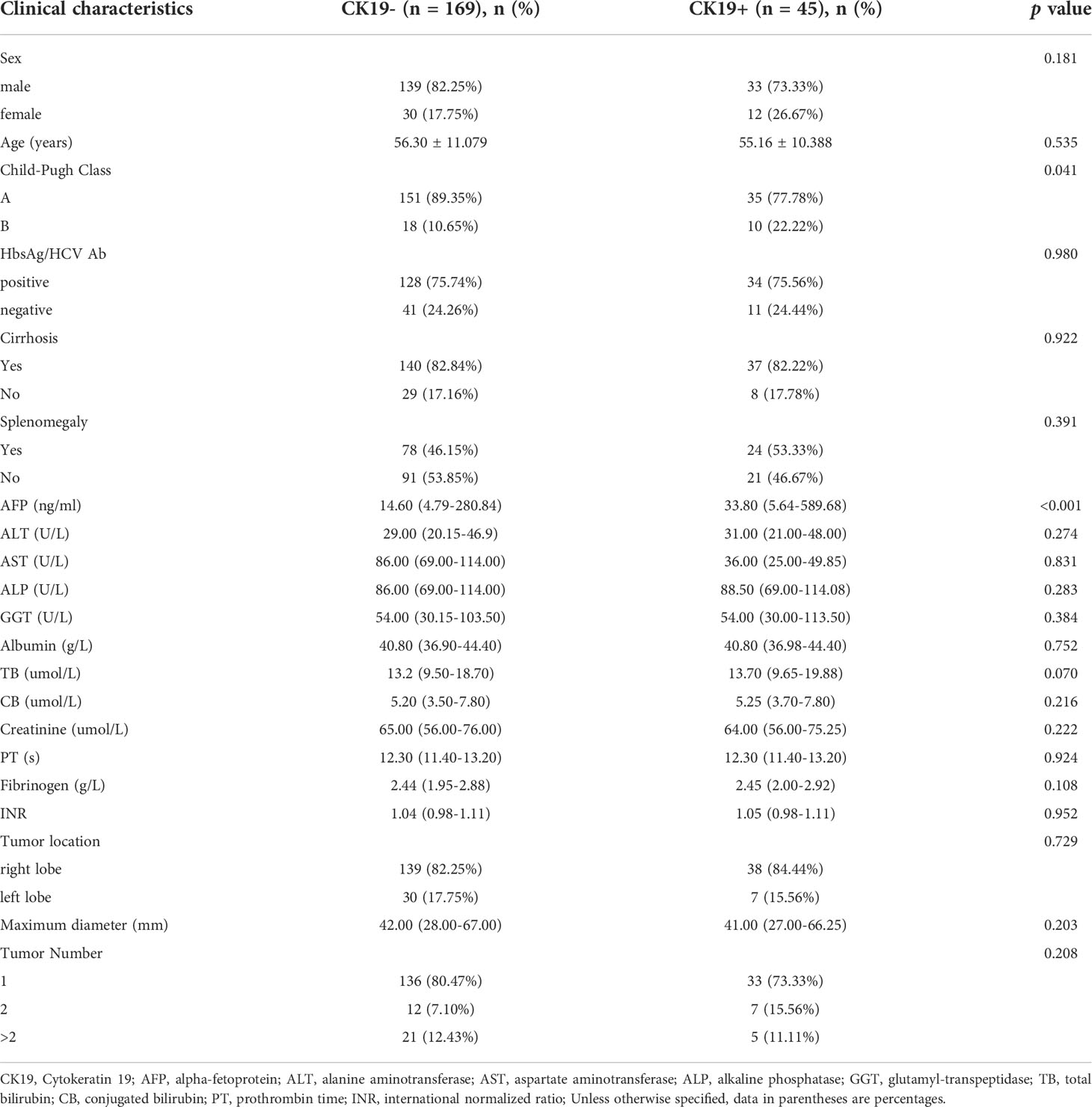
Methods: We retrospectively analyzed 214 patients with pathologically confirmed HCC who received CK19 immunohistochemical staining. Through random stratified sampling (ratio, 8:2), patients from institutions I and II were divided into training dataset (n = 143) and test dataset (n = 36), and patients from institution III served as external validation dataset (n = 35). All gray-scale ultrasound images were preprocessed, and then the regions of interest were then manually segmented by two sonographers. A total of 1409 ultrasomics features were extracted from the original and derived images. Next, the intraclass correlation coefficient, variance threshold, mutual information, and embedded method were applied to feature dimension reduction. Finally, the clinical model, ultrasonics model, and combined model were constructed by eXtreme Gradient Boosting algorithm. Model performance was assessed by area under the receiver operating characteristic curve (AUC), sensitivity, specificity, and accuracy.
Results: A total of 12 ultrasomics signatures were used to construct the ultrasomics models. In addition, 21 clinical features were used to construct the clinical model, including gender, age, Child-Pugh classification, hepatitis B surface antigen/hepatitis C virus antibody (positive/negative), cirrhosis (yes/no), splenomegaly (yes/no), tumor location, tumor maximum diameter, tumor number, alpha-fetoprotein, alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, glutamyl-transpeptidase, albumin, total bilirubin, conjugated bilirubin, creatinine, prothrombin time, fibrinogen, and international normalized ratio. The AUC of the ultrasomics model was 0.789 (0.621 – 0.907) and 0.787 (0.616 – 0.907) in the test and validation datasets, respectively. However, the performance of the combined model covering clinical features and ultrasomics signatures improved significantly. Additionally, the AUC (95% CI), sensitivity, specificity, and accuracy were 0.867 (0.712 – 0.957), 0.750, 0.875, 0.861, and 0.862 (0.703 – 0.955), 0.833, 0.862, and 0.857 in the test dataset and external validation dataset, respectively.
Conclusion: Ultrasomics signatures could be used to predict the expression of CK19 in HCC patients. The combination of clinical features and ultrasomics signatures showed excellent effects, which significantly improved prediction accuracy and robustness.
Introduction
Hepatocellular carcinoma (HCC) is the leading primary liver cancer, which is one of the major global health challenges (1). In 2020, liver cancer ranked sixth and third in incidence rate and mortality among all malignant tumors in the world, and there were approximately 905,000 new cases and 830,000 deaths (2). With a 5-year survival rate of 18%, liver cancer has become the second most fatal tumor, just secondary to pancreatic cancer (3). Although many treatment strategies are available in clinical practice, the recurrence rate of HCC remains high, and the prognosis is generally poor (4–6). Accumulating evidence suggests that HCC is a heterogeneous tumor with a multimolecular phenotype (7, 8), and that inter- and intratumoral heterogeneity is often highly resistant to clinical interventions, leading to treatment failure (9, 10). The key factors associated with the prognosis of HCC include microvascular invasion, tumor grade, Ki67 expression, etc. (11–13). Compared with these factors, CK19 is not only a prognostic marker of HCC (14), but also a stemness-related marker (15). Tumor hepatocytes are capable of self-renewal, differentiation and proliferation, with stronger tumorigenicity and chemoresistance (16, 17). Transarterial chemoembolization and systemic chemotherapy play an important role in the treatment of HCC (4, 6). However, CK19-positive HCC patients are more likely to develop resistance to chemotherapeutic drugs, resulting in treatment failure (18). Therefore, one manifestation of HCC heterogeneity is the expression of Cytokeratin (CK) 19.
Cytokeratins are important structural components in the epithelial cell skeleton (19). In adult liver, CK8 and CK18 are expressed in mature hepatocytes, while CK7 and CK19 are expressed in cholangiocytes and hepatic progenitor cells (20). CK19 has been shown to be expressed in 4-28% of HCC patients (21–23). In vitro studies have confirmed that CK19-positive HCC cells are closely related to invasiveness, epithelial-mesenchymal transition, and angiogenesis (23, 24). Compared with CK19-negative HCC patients, CK19-positive patients have a poorer prognosis, their clinical manifestations are not only more prone to resistance to chemotherapeutic drugs, but also have a higher incidence of extrahepatic metastasis and vascular invasion (14, 18, 23). Due to its high invasiveness, this molecular subtype has been considered as a new subtype of HCC (16, 25). It has been found that some liver transplant patients without CK19 expression and CK19-related gene expression have a good prognosis, even if they do not meet the Milan criteria (18, 24). It has been suggested that preoperative assessment of CK19 expression may help to determine judge whether patients beyond the Milan criteria meet the condition of liver transplantation, potentially expanding the criteria for liver transplantation (26). Therefore, preoperative assessment of CK19 expression in HCC patients is critical for the effective development of individualized treatment strategies.
Immunohistochemical analysis of biopsy tissues is a reliable method for the clinical preoperative assessment of CK19 expression in HCC patients (27). However, tissue biopsy is expensive, and the invasive procedure may bring a series of complications, such as intra-abdominal or subcapsular bleeding, needle-path metastasis and intra-abdominal metastasis (28, 29). In addition, the sample size of biopsy tissues is small which can easily leading to missed diagnosis (30). In addition, the biopsy is not recommended as a routine test for diagnosis of HCC by the current guidelines (6, 31). Therefore, the current preoperative detection of CK19 is somewhat limited. Radiomics is a powerful tool for modern precision medicine (32). It captures high-throughput radiomics features from medical images combined with clinically relevant information to further improve the accuracy of diagnosis and prognosis prediction, since these features can provide additional information, such as tumor phenotypes and immune microenvironment (33). As one field of radiomics, ultrasomics plays an important role in the diagnosis and treatment of liver cancer (34). Mao et al. successfully classified primary and metastatic liver cancer using k-nearest neighbor, logistic regression, multilayer perceptron, random forest, and SVM algorithms based on grayscale ultrasound images (35). Based on ultrasound original radio frequency signals of HCC, Dong et al. effectively predicted MVI using sparse representation algorithm and machine learning algorithm combined with signal analysis and processing techniques (36). Ma et al. developed a radiomics model based on dynamic contrast-enhanced ultrasound (CEUS) (37). They found that the model performed well in predicting early HCC recurrence after ablation, while combining CEUS, US radiomics and clinical Combination models of factors can stratify high risk of late recurrence. The above studies demonstrate that multiple modalities of ultrasomics can successfully predict diagnosis and differential diagnosis of HCC, early recurrence and key prognostic factors. At present, some studies have successfully constructed radiomics models for predicting CK19 status based on Magnetic resonance imaging (MRI) images with good performance (38–40). However, MRI cannot be applied to some special populations, such as those with claustrophobia or metal-containing implants in their bodies. Furthermore, MRI is time-consuming and expensive, which limits its clinical application (41). Ultrasound has become one of the most common examination methods for the liver because of its non-invasive and non-radiative properties, more applicable population, repeated observation and relatively low cost (42). As a branch of radiomics, ultrasomics has been successfully applied to the accurate diagnosis of various malignant tumors, such as liver cancer, thyroid cancer and breast cancer, with good results (43–47). However, there are few reports about the prediction of CK19 expression in HCC patients based on ultrasomics method.
Therefore, this study aims to explore the value of machine learning-based ultrasomics for non-invasive prediction of CK19 expression in HCC patients, and to further evaluate the generalization ability of the prediction model using an independent external validation dataset.
Materials and methods
Study population
This retrospective study was approved by the ethics review boards of three medical institutions, Henan Provincial People’s Hospital (Institution I), the First Affiliated Hospital of Zhengzhou University (Institution II), and Henan Cancer Hospital (Institution III), and the patients’ informed consent was waived. From May 2019 to December 2021, clinical, pathological and imaging data of 1535 hospitalized patients from the above three medical institutions were collected, and the population was screened according to the following criteria. Inclusion criteria: (1) pathologically confirmed HCC with CK19 results; (2) performed liver ultrasound with two weeks before the surgery; (3) clinical and imaging data integrity. Exclusion criteria: (1) recurrent HCC; (2) history of radiotherapy, chemotherapy, radiofrequency ablation, or other anti-tumor therapies; (3) abdominal ultrasonography performed at other hospitals; (4) preoperative imaging and clinical examinations showing obvious metastases or concurrent malignant tumors of other natures; (5) low quality image. A total of 214 patients were finally included in this study, of which 179 patients from institution I and II were divided into training dataset (n = 143) and test dataset (n = 36) by random stratified sampling (ratio, 8:2), and 35 patients from institution III served as an independent external validation dataset. The screening and grouping flow chart of the study population is shown in Figure 1.
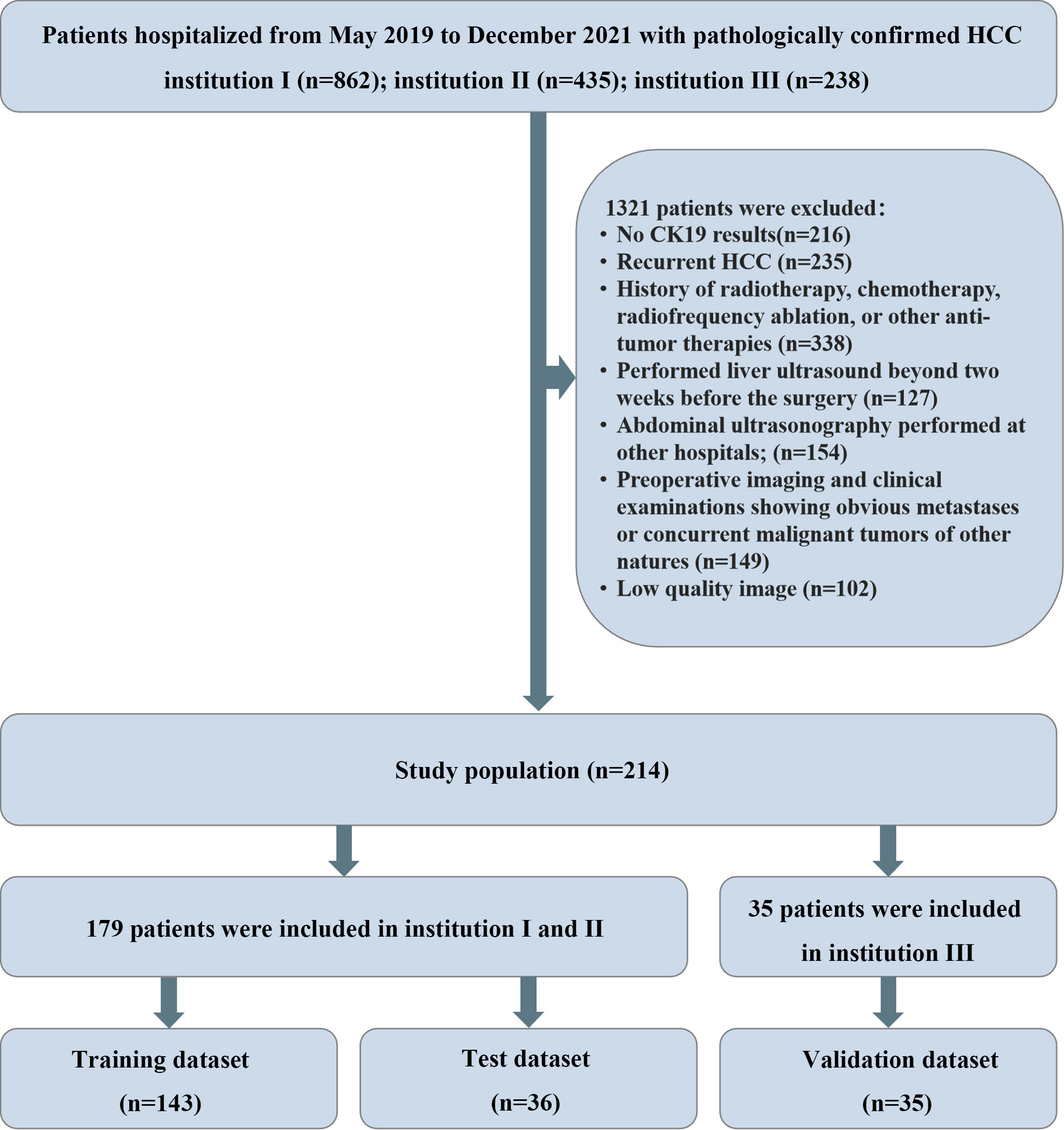
Figure 1 Flowchart: Cases were screened and enrolled according to the established exclusion criteria.
The indicators of the patients mainly included gender, age, hepatitis B surface antigen (HbsAg)/hepatitis C virus antibody (HCV-Ab), serum liver and kidney function indicators, coagulation function indicators, liver cirrhosis, splenomegaly, tumor location, maximum tumor diameter and tumor number. HCC specimens from all patients were pathologically examined and diagnosed according to World Health Organization criteria. In this study, all patients were divided into CK19-positive and CK19-negative groups, where CK19 positive is defined as the presence of membranous or cytoplasmic immunoreactivity in ≥5% of tumor cells (21).
Image acquisition, preprocessing and ROI segmentation
All patients fasted for more than 8 hours before abdominal ultrasonography. Preoperative ultrasonography was performed by sonographers with more than 10 years of experience in liver ultrasonography, and the echogenicity, lesion size, and blood flow signals of the lesions were also assessed and recorded. At least one original ultrasound image clearly showing the maximum lesion diameter and one original ultrasound image containing the measured parameters in the same section should be stored in Digital Imaging and Medicine Communication (DICOM) format, respectively. The models of ultrasound equipment used were: GE Logiq E20, GE Vivid E9, HIVISION Ascendus, HIALOK ProSound A5, Philips EPIQ 7 or Philips EPIQ 5, etc. All ultrasound probes were C75, with the frequency of 1 – 5 MHZ.
In order to eliminate differences caused by different ultrasound equipment and different operators and to ensure the comparability of the features, researchers with 6 years of experience carried out image preprocessing. To ensure the distribution of baseline features, we first used stratified sampling to divide the training dataset and test dataset for patients in institutions I and II in a ratio of 8:2. Then, we used b-spline for ultrasound images reconstructed with different voxel sizes. The images were resampled to a pixel size of 1 mm x1 mm, and gray-level discretized in the histogram with the bin width set to a fixed 25.
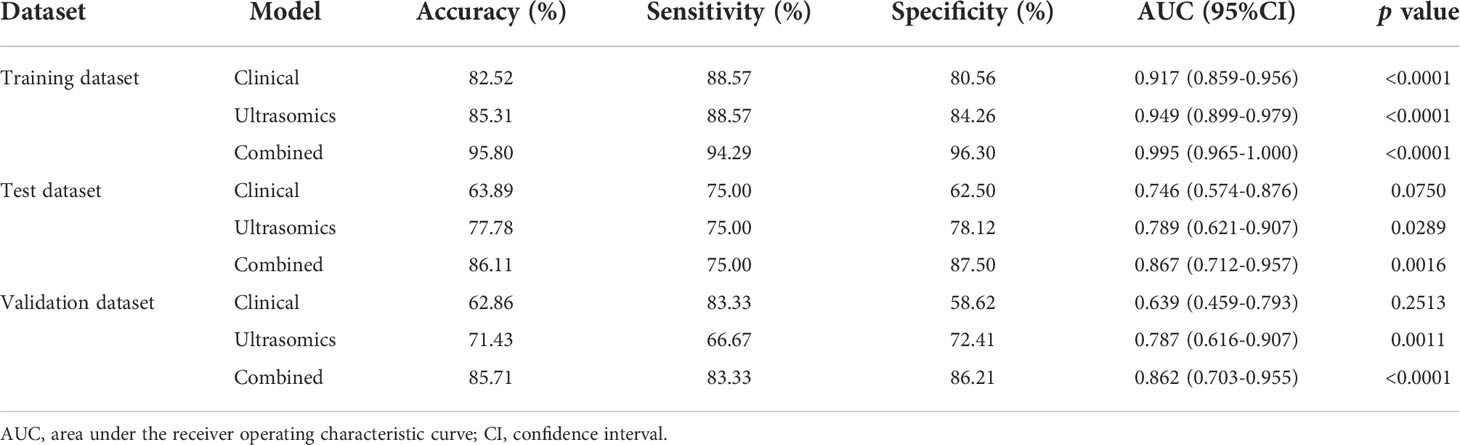
Region of interest (ROI) segmentation for this study was performed by a sonographer with 30 years of experience in abdominal ultrasound diagnosis (sonographer 1), and a sonographer with 10 years of experience in abdominal ultrasound diagnosis (sonographer 2). First, under the guidance of sonographer 1, sonographer 2 used ITK-SNAP software (http://www.itksnap.org) to manually segment each patient’s ultrasound image along the lesion margin on the largest transverse section of the tumor. To assess the reproducibility of features, 50 cases of the ultrasound images were randomly selected for segmentation by the sonographer 2. Both sonographers were blinded to the clinical and pathological data of all patients. The flowchart of this research is shown in Figure 2. The representative lesion segmentation images are shown in Figure 3.
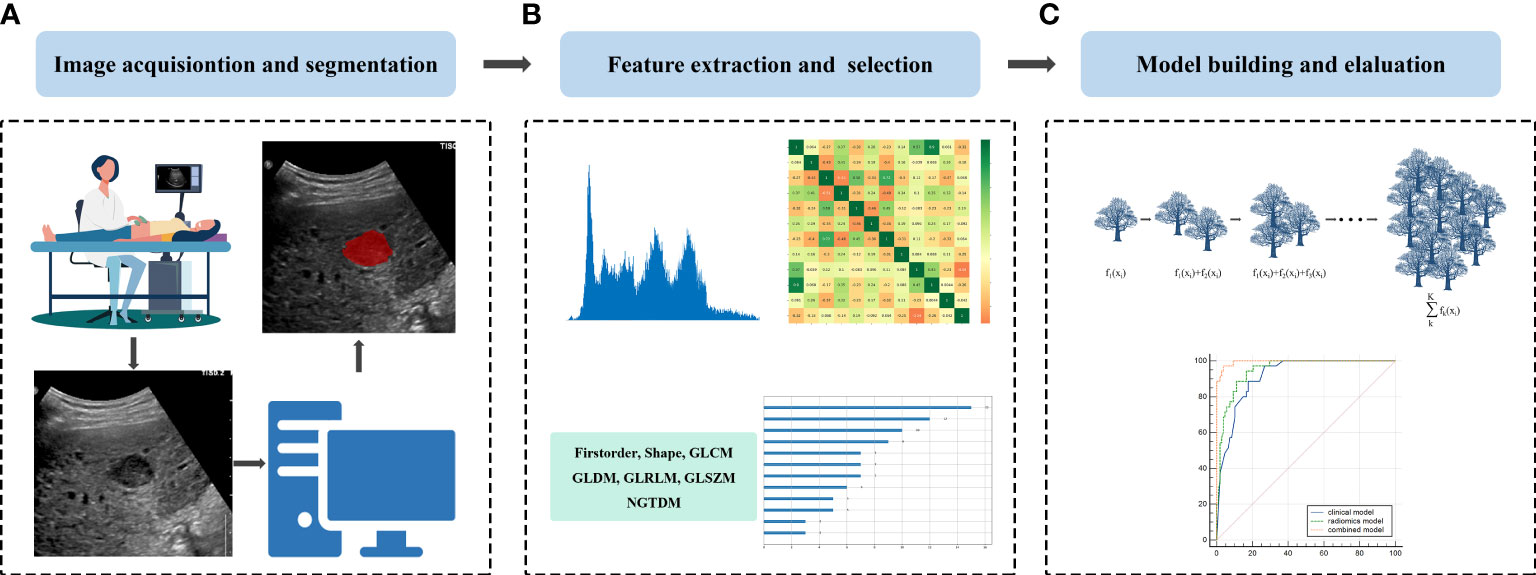
Figure 2 Schematic diagram of the overall study: (A) Image acquisition and lesion segmentation; (B) Feature extraction and feature selection, and (C) Model construction and evaluation.
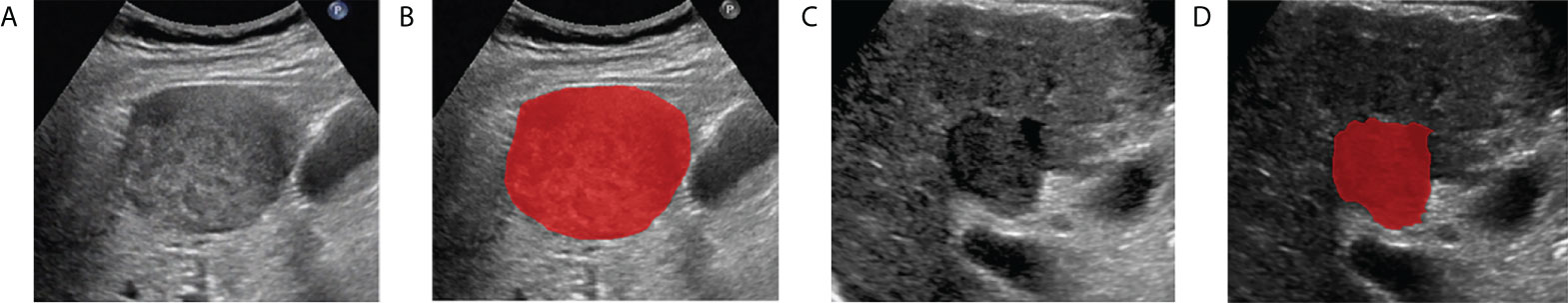
Figure 3 Examples of delineating regions of interest (ROI) on a grayscale ultrasound image. (A, B) are the CK19-positive HCC patient, (C, D) are the CK19-negative HCC patient.
Ultrasomics feature extraction and screening
First, 14 filters were used to process the original image of each patient to obtain the corresponding derived images, and then the open-source software package pyradiomics 2.1.2 was used to extract the information in all original images and derived images in high-throughput and converted them into quantitative features. Seven major radiomics features below were obtained: first order, shape, gray level co-occurrence matrix (GLCM), gray level run length matrix (GLRLM), gray level size zone matrix (GLSZM), neighboring gray tone difference matrix (NGTDM) and gray level dependence matrix (GLDM). After extracting all feature values, the missing value of each feature was filled with the median. Finally, the data were normalized (Z-score normalization) according to the mean and standard deviation to make the data conformed to a normal distribution. Details of the feature extraction methods and the filters used are provided in the Supplementary Material 1.
The optimal feature subset was selected by feature dimensionality reduction as follows: firstly, the reproducibility of the extracted features was evaluated by the intraclass correlation coefficient (ICC), where the features with ICC > 0.8 were considered to be reproducible (48); secondly, the features with variance of 0 (i.e., features that did not contribute anything to the classification) were excluded by the variance threshold; thirdly, the linear or nonlinear information relationships between each feature and the label were captured by mutual information, and the features with maximal information coefficient (MIC) of 0 were filtered. Finally, dimensionality reduction was further performed using the embedding method in combination with eXtreme Gradient Boosting (XG Boost).
Model construction and evaluation
The ultrasomics model, the clinical model and the combined model were constructed using the eXtreme Gradient Boosting (XGBoost) algorithm in combination with the learning curve and the grid search for tuning parameter, respectively. XGBoost, an efficient and widely used machine learning algorithm, incorporated regularization and parallel processing, which could reduce both overfitting and computation (49).
Firstly, the ultrasomics model was constructed using the optimal ultrasomics signatures selected above. Secondly, the clinical model was constructed by 21 clinical features, including gender, age, Child-Pugh classification, HbsAg/HBC Ab (positive/negative), cirrhosis (yes/no), splenomegaly (yes/no), tumor location, tumor maximum diameter, tumor number, and serum biochemical parameters, including alpha-fetoprotein (AFP), alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), glutamyl-transpeptidase (GGT), albumin, total bilirubin (TB), conjugated bilirubin (CB), creatinine, prothrombin time (PT), fibrinogen, international normalized ratio (INR). Finally, the combined model was constructed based on all the above clinical features and ultrasomics signatures to explore whether the combination of the two can show better performance. Supplementary Material 2 includes details of parameter tuning for model building.
The performance of the three prediction models was assessed in the test dataset and the external validation dataset, and expressed as four indicators: area under the receiver operating characteristic curve (AUC) with 95% confidence interval (CI), accuracy, sensitivity and specificity. Model construction and evaluation were performed in the Python environment using the scikit-learn 0.23.2 package.
Statistical analysis
Statistical analysis was performed by IBM SPSS Statistics 23.0 software. The distribution of continuous variables was first determined by the Shapiro – Wilk test, expressed as mean ± standard deviation or median (25th to 75th percentile) for continuous variables. Categorical variables were expressed as frequency and relative frequency. Statistical differences between the two groups of CK19-positive and CK19-negative patients were then analyzed as described above using t-test or Mann-Whitney U test for continuous variables and chi-square test or Fisher’s exact probability test for categorical variables. A value of p < 0.05 was considered statistically significant.
Results
Baseline characteristics of the study population
A total of 214 HCC patients were finally included in this study. Patients from institution I and II were mixed and divided into training dataset (n = 143) and test dataset (n = 36) by random stratified sampling (ratio, 8:2), and patients from institution III separately served as external validation dataset (n = 35). In the whole study cohort, CK19 negative and positive patients accounted for 78.97% (169/214) and 21.03% (45/214), respectively, and male and female patients accounted for 80.37% (172/214) and 19.63% (42/214), respectively. The baseline clinical and pathological characteristics of all patients are shown in Table 1.
Feature extraction and screening
A total of 1,409 features were extracted from the original and derived images, including first order, shape, GLCM, GLRLM, GLSZM, NGTDM and GLDM of 18, 14, 24, 16, 16, 5 and 14, respectively. All but 14 shape features were obtained from the original and derived images. Details of the features were provided in the Supplementary Material 3.
Firstly, a total of 992 features were retained according to the ICC of features. Secondly, 16 features with zero variance and 487 features with zero MIC were excluded using variance threshold and mutual information. Finally, 12 most valuable signatures were selected using the embedding method combined with XGBoost for further dimension reduction. Supplementary Figures 1, 2 showed the importance of the 12 signatures.
The performance Of ultrasomics, clinical and combined models
Three prediction models, that’s ultrasomics model, clinical model and combined model, were constructed using XGBoost algorithm, respectively. The results showed that the ultrasomics signatures showed satisfactory performance in predicting CK19 expression in HCC patients, and the AUCs of the test dataset and the external validation dataset were 0.789 (95% CI, 0.621 – 0.907) and 0.787 (95% CI, 0.616 – 0.907), respectively. The AUC of the clinical model constructed based on the relevant clinical characteristics was 0.746 (95% CI, 0.574 – 0.876) and 0.638 (95% CI, 0.459 – 0.793) in the test and validation datasets, respectively. However, when the clinical features and ultrasomics features were combined, the combined model achieved an excellent performance in predicting CK19 expression, and the AUC increased to 0.867 (95% CI, 0.712 – 0.957) and 0.862 (95% CI, 0.703 – 0.955), respectively. The ROC curves of all models in the three datasets are presented in Figure 4, and the detailed indicators of performance evaluation are presented in Table 2.
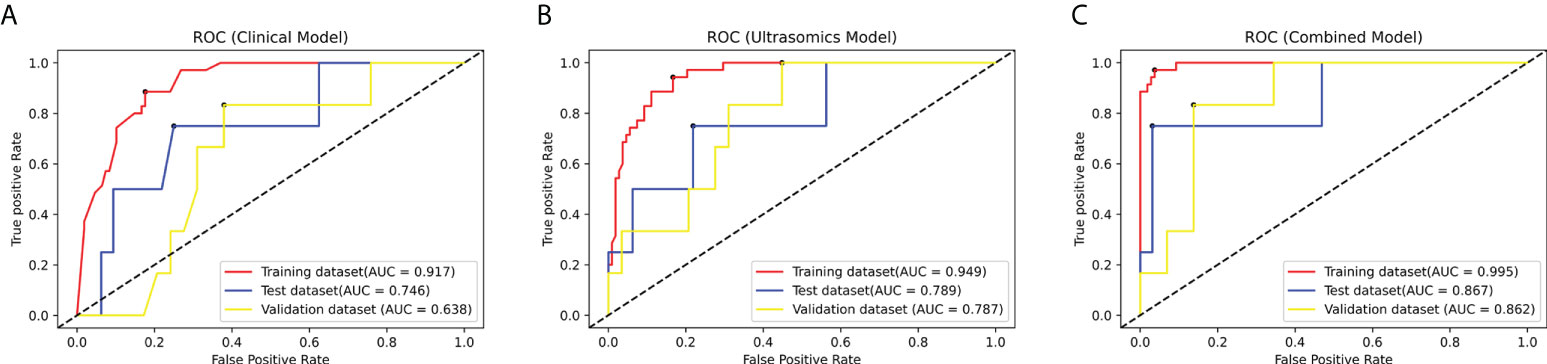
Figure 4 The ROC curves of the modes in the training dataset, test dataset and validation dataset: (A) The clinical model. (B) The ultrasomics model. (C) The combined model.
Discussion
HCC with positive CK19 expression is a new subtype of primary liver cancer (16, 25). In HCC, positive CK19 expression is one of the independent risk factors for prognosis, and is significantly correlated with invasion, chemotherapy drug resistance, and lymph node metastasis (14, 15, 18, 22). It has been reported that recurrence-free survival was significantly reduced in CK19-positive patients after surgical resection compared with CK19-negative HCC patients, with 26.1% decrease in 1-year survival, 16% decrease in 2-year survival, and 16.4% decrease in 3-year survival, which seriously affected prognosis of the patients (50). Therefore, preoperative assessment of CK19 expression in HCC patients is critical for the development of individualized treatment strategies, and improving the prognosis of patients. Preoperative immunohistochemistry is the main choice for clinical detection of CK19 (27). However, preoperative tissue biopsy may increase the risk of unwanted complications, such as abdominal or subcapsular hemorrhage, as well as needle tract metastasis (28, 29). Meanwhile, in current guidelines, biopsy is not a routine test for HCC diagnosis (6, 31). Therefore, the current preoperative detection of CK19 is somewhat limited.
Radiomics could extract a large number of macro unrecognizable, high- dimensional features through advanced data mining technology to help clinicians to further improve the accuracy of diagnosis and prognosis prediction (32). As a field of radiomics, ultrasomics plays an important role in the diagnosis and treatment of liver cancer (34). In this multicenter study, we fully mined the high-throughput information in gray-scale ultrasound images, and constructed and validated three models to predict CK19 expression in HCC patients. Firstly, we extracted a total of 1,409 ultrasomics features from the original and derived images. In order to avoid curse of dimensionality, we used ICC, variance threshold, and embedding method combined with XGBoost to reduce the dimensionality of the features, resulting in 12 optimal signatures. Then, the XGBoost algorithm combined with the learning curve and the grid search parameter adjustment method was used to train three prediction models: the ultrasound omics model, the clinical model and the combined model. The results showed that ultrasomics signatures based on machine-learning could predict and classify the expression of CK19 in HCC.As can be seen from Table 2, the combined model incorporating ultrasomics signatures and clinical factors performed excellently, with AUC improving to 0.867 (95% CI, 0.712 – 0.957) and 0.862 (95% CI, 0.703 – 0.955), respectively. In addition, in external validation dataset, the combined model not only reached an AUC of more than 0.85, but also reached an accuracy, sensitivity, and specificity of more than 80% (85.71%, 83.33%, and 86.21%, respectively), which indicated that the combined model had a more stable performance. Notably, the reproducibility of the results is one of the main limitations of radiomics in clinical application, but the current radiomics prediction studies of HCC are mostly based on a single center. On one hand, the heterogeneity of the images collected by the single center is relatively low, and the model had not been verified externally, which might be an overfitting phenomenon. On the other hand, the cases selected from multiple centers have a wide range of disease distribution and other aspects compared to a single center study. These were the reasons why we conducted a multicenter study. The results showed that model performance on the test dataset were comparable to the performance on the external validation dataset, especially the AUCs of the combined model were as high as 0.86. Therefore, the models had a reliable generalization ability.
To date, only a few scholars explored the correlation between HCC radiomics signatures and CK19 expression, mostly based on MRI (38–40). Wang et al. identified HCC patients with positive CK19 expression based on texture features of conventional MRI image sequences (38). They manually segmented lesions and extracted texture features in diffusion-weighted imaging (DWI) sequences, and then analyzed 7 conventional sequence MRI appearances, clinicopathological characteristics, and 2,415 texture features using univariate and multivariate analysis methods. Finally, serum AFP level ≥ 400 ng/mg, arterial rim enhancement, and StdSeparation 3D texture features were identified as predictive variables associated with CK19 positivity in HCC patients, and then a logistic regression prediction model was constructed using the above variables. The AUCs predicted by each of the three factors was 0.650 (95% CI, 0.533 – 0.754), 0.635 (95% CI, 0.518 – 0.741), and 0.765 (95% CI, 0.655 – 0.853), respectively. While combining the three characteristics, the prediction model performed optimally, with an AUC of 0.844 (95% CI, 0.744 – 0.916). Wang et al. developed a nomogram for the prediction of CK19 expression, which incorporates both clinico-radiological features and fused radiomics features (39). They extracted 647 radiomics features from enhanced MRI multi-sequence images based on a machine learning algorithm, and then used the least absolute shrinkage and selection operator regression and decision tree for feature screening and model construction. Finally, in the validation dataset, the AUC of the radiomics model fused with 17 optimal signatures was 0.822 (95% CI, 0.716 – 0.928), and the AUC of the combined model incorporating clinical factors, conventional imaging features, and radiomics signatures reached 0.846 (95% CI, 0.730 – 0.963). Yang et al. developed four CK19 expression classifiers based on HCC-enhanced MRI images from three centers and compared their performance (40). They constructed predictive classifiers using four machine learning algorithms: multiple logistic regression, support vector machine, random forest, and artificial neural network algorithm (ANN), respectively, and evaluated the generality of the optimal classifier in two validation datasets. The results showed that the ANN classifier constructed from the 12 optimal features exhibited the best diagnostic performance. The AUC was 0.857, 0.726, and 0.790 in the training, validation 1, and validation 2 datasets, respectively. In this study, the AUC of the ultrasomics model and the combined model reached 0.789 (95% CI, 0.621 – 0.907) and 0.867 (95% CI, 0.712 – 0.957) in the test dataset, respectively. In addition, the two models also achieved similar performance in the external validation dataset, with AUC of 0.787 (95% CI, 0.616 – 0.907) and 0.862 (95% CI, 0.703 – 0.955), respectively. The results showed that although the gray-scale ultrasound images used in this study were not as rich as the image sequences contained in MRI, our ultrasomics model achieved similar prediction performance with the prediction model constructed by integrating multiple sequence radiomics features of MRI. This fully demonstrated that gray-scale ultrasound images included a variety of information and also had a great potential in predicting the level of tumor heterogeneity. In addition, our prediction model also showed excellent prediction performance in the independent external validation dataset, and the ultrasonography is relatively cheap, which makes the ultrasomics method a better choice for popularization.
However, this study also had some limitations. Firstly, this was a retrospective study and there might be selection bias. And the data came from three medical institutions, especially with relatively few positive samples. In the future, we hope to expand the research scope and increase the sample size. Secondly, the images used in this study were acquired by multiple ultrasound devices. Although feature extraction was preprocessed before, there might still be some device-related differences which were not eliminated. Again, this study extracted features from the largest section of the tumor only, and will include more sections in the future for in-depth study. Finally, only gray-scale ultrasound images were collected, but we hope to collect more ultrasound images with multiple parameters and modalities to further investigate CK19 expression prediction in HCC patients by ultrasomics.
In conclusion, ultrasomics signatures could be used for noninvasive prediction of CK19 expression in HCC, and the combined prediction of clinical features and optimal ultrasomics feature subset showed an excellent performance, which improved the prediction of CK19 expression in HCC significantly. Therefore, machine learning-based ultrasomics methods may be used to predict tumor heterogeneity and facilitate the development of precision medicine.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by 1. Medical Ethics Committee of Henan Provincial People’s Hospital (Affiliated to Henan Provincial People’s Hospital) 2. Ethics Review Committee of Scientific Research Projects of the First Affiliated Hospital of Zhengzhou University (Affiliated to the First Affiliated Hospital of Zhengzhou University) 3. Medical Ethics Committee of Henan Provincial Cancer Hospital (Affiliated to Henan Provincial Cancer Hospital. The ethics committee waived the requirement of written informed consent for participation. Written informed consent was not obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LLZ: data collection, study design, statistical analysis and interpretation, manuscript writing. QQ, QL, XL, YW, LY: data collection and management. SR: study design and manuscript review. SL, BM: data analysis, software processing. LL, YL: study design support. SD: data collection, study design, manuscript review and funding. LZZ: manuscript review and editing, study design and supervision, project management, and funding. All authors contributed to the article and approved the submitted version.
Funding
This study was sponsored by the National Key Research and Development Program of China (Grant No. 2018YFC0114606) and Henan Nature Science Foundation (Grant No. 212300410389), and Medical Science and Technology Breakthrough Plan Project of Henan Province (Grant No. LHGJ20210020).
Acknowledgments
I am appreciative to LZZ and the Henan Engineering Technology Research Center of Ultrasonic Molecular Imaging and Nanotechnology s for providing the assistance and facilities to accomplish the whole research. I also want to express my thanks to Long Yang, Ye Zhang, Shuaiyang Wang, Guoxin Deng, Simeng Wang, Xiaoxia Xu and Qiwei Cheng for their assistance in data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.994456/full#supplementary-material
Abbreviations
HCC, hepatocellular carcinoma; CK19, Cytokeratin 19; MRI, Magnetic resonance imaging; MRI, magnetic resonance imaging; HBsAg, hepatitis B surface antigen; HCV Ab, hepatitis C virus antibody; AFP, alpha-fetoprotein; DICOM, digital imaging and communications in medicine; ROI, region of interest; GLCM, gray-level cooccurrence matrix; GLSZM, gray-level size-zone matrix; GLRLM, gray-level run length matrix; GLDM, gray-level dependence matrix; NGTDM, neighboring gray-tone-difference matrix; ICC intra-class correlation coefficient; ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; GGT, glutamyl-transpeptidase; TB, total bilirubin; CB, conjugated bilirubin; PT, prothrombin time; INR, international normalized ratio, AUC, area under the receiver operating characteristic curve; CI, confidence interval.
References
1. Villanueva A. Hepatocellular carcinoma. N Engl J Med (2019) 380(15):1450–62. doi: 10.1056/NEJMra1713263
2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2021) 71(3):209–49. doi: 10.3322/caac.21660
3. Jemal A, Ward EM, Johnson CJ, Cronin KA, Ma J, Ryerson B, et al. Annual report to the nation on the status of cancer, 1975-2014, featuring survival. J Natl Cancer Inst (2017) 109(9):djx030. doi: 10.1093/jnci/djx030
4. Heimbach JK, Kulik LM, Finn RS, Sirlin CB, Abecassis MM, Roberts LR, et al. Aasld guidelines for the treatment of hepatocellular carcinoma. Hepatology (2018) 67(1):358–80. doi: 10.1002/hep.29086
5. European Association For The Study Of The Liver, European Organisation For R, and Treatment Of C. Easl-eortc clinical practice guidelines: Management of hepatocellular carcinoma. J Hepatol (2012) 56(4):908–43. doi: 10.1016/j.jhep.2011.12.001
6. Easl clinical practice guidelines: Management of hepatocellular carcinoma. J Hepatol (2018) 69(1):182–236. doi: 10.1016/j.jhep.2018.03.019
7. Dagogo-Jack I, Shaw AT. Tumour heterogeneity and resistance to cancer therapies. Nat Rev Clin Oncol (2018) 15(2):81–94. doi: 10.1038/nrclinonc.2017.166
8. Zhang Q, Lou Y, Yang J, Wang J, Feng J, Zhao Y, et al. Integrated multiomic analysis reveals comprehensive tumour heterogeneity and novel immunophenotypic classification in hepatocellular carcinomas. Gut (2019) 68(11):2019–31. doi: 10.1136/gutjnl-2019-318912
9. Nault JC, Galle PR, Marquardt JU. The role of molecular enrichment on future therapies in hepatocellular carcinoma. J Hepatol (2018) 69(1):237–47. doi: 10.1016/j.jhep.2018.02.016
10. Wang XW, Thorgeirsson SS. The biological and clinical challenge of liver cancer heterogeneity. Hepat Oncol (2014) 1(4):349–53. doi: 10.2217/hep.14.18
11. Erstad DJ, Tanabe KK. Prognostic and therapeutic implications of microvascular invasion in hepatocellular carcinoma. Ann Surg Oncol (2019) 26(5):1474–93. doi: 10.1245/s10434-019-07227-9
12. Martins-Filho SN, Paiva C, Azevedo RS, Alves VAF. Histological grading of hepatocellular carcinoma-a systematic review of literature. Front Med (Lausanne) (2017) 4:193. doi: 10.3389/fmed.2017.00193
13. Luo Y, Ren F, Liu Y, Shi Z, Tan Z, Xiong H, et al. Clinicopathological and prognostic significance of high ki-67 labeling index in hepatocellular carcinoma patients a meta-analysis. Int J Clin Exp Med (2015) 8(7):10235–47.
14. Uenishi T, Kubo S, Yamamoto T, Shuto T, Ogawa M, Tanaka H, et al. Cytokeratin 19 expression in hepatocellular carcinoma predicts early postoperative recurrence. Cancer Sci (2003) 94(10):851–7. doi: 10.1111/j.1349-7006.2003.tb01366.x
15. Kim H, Choi GH, Na DC, Ahn EY, Kim GI, Lee JE, et al. Human hepatocellular carcinomas with "Stemness"-related marker expression: Keratin 19 expression and a poor prognosis. Hepatology (2011) 54(5):1707–17. doi: 10.1002/hep.24559
16. Mishra L, Banker T, Murray J, Byers S, Thenappan A, He AR, et al. Liver stem cells and hepatocellular carcinoma. Hepatology (2009) 49(1):318–29. doi: 10.1002/hep.22704
17. Yin S, Li J, Hu C, Chen X, Yao M, Yan M, et al. Cd133 positive hepatocellular carcinoma cells possess high capacity for tumorigenicity. Int J Cancer (2007) 120(7):1444–50. doi: 10.1002/ijc.22476
18. Rhee H, Nahm JH, Kim H, Choi GH, Yoo JE, Lee HS, et al. Poor outcome of hepatocellular carcinoma with stemness marker under hypoxia: Resistance to transarterial chemoembolization. Mod Pathol (2016) 29(9):1038–49. doi: 10.1038/modpathol.2016.111
19. Moll R, Divo M, Langbein L. The human keratins: Biology and pathology. Histochem Cell Biol (2008) 129(6):705–33. doi: 10.1007/s00418-008-0435-6
20. Roskams T. Liver stem cells and their implication in hepatocellular and cholangiocarcinoma. Oncogene (2006) 25(27):3818–22. doi: 10.1038/sj.onc.1209558
21. Durnez A, Verslype C, Nevens F, Fevery J, Aerts R, Pirenne J, et al. The clinicopathological and prognostic relevance of cytokeratin 7 and 19 expression in hepatocellular carcinoma. A possible progenitor cell origin. Histopathology (2006) 49(2):138–51. doi: 10.1111/j.1365-2559.2006.02468.x
22. Tsuchiya K, Komuta M, Yasui Y, Tamaki N, Hosokawa T, Ueda K, et al. Expression of keratin 19 is related to high recurrence of hepatocellular carcinoma after radiofrequency ablation. Oncology (2011) 80(3-4):278–88. doi: 10.1159/000328448
23. Govaere O, Komuta M, Berkers J, Spee B, Janssen C, de Luca F, et al. Keratin 19: A key role player in the invasion of human hepatocellular carcinomas. Gut (2014) 63(4):674–85. doi: 10.1136/gutjnl-2012-304351
24. Kawai T, Yasuchika K, Ishii T, Katayama H, Yoshitoshi EY, Ogiso S, et al. Keratin 19, a cancer stem cell marker in human hepatocellular carcinoma. Clin Cancer Res (2015) 21(13):3081–91. doi: 10.1158/1078-0432.Ccr-14-1936
25. Zhuo JY, Lu D, Tan WY, Zheng SS, Shen YQ, Xu X. Ck19-positive hepatocellular carcinoma is a characteristic subtype. J Cancer (2020) 11(17):5069–77. doi: 10.7150/jca.44697
26. Miltiadous O, Sia D, Hoshida Y, Fiel MI, Harrington AN, Thung SN, et al. Progenitor cell markers predict outcome of patients with hepatocellular carcinoma beyond Milan criteria undergoing liver transplantation. J Hepatol (2015) 63(6):1368–77. doi: 10.1016/j.jhep.2015.07.025
27. Takahashi Y, Dungubat E, Kusano H, Ganbat D, Tomita Y, Odgerel S, et al. Application of immunohistochemistry in the pathological diagnosis of liver tumors. Int J Mol Sci (2021) 22(11):5780. doi: 10.3390/ijms22115780
28. Filingeri V, Sforza D, Tisone G. Complications and risk factors of a Large series of percutaneous liver biopsies in patients with liver transplantation or liver disease. Eur Rev Med Pharmacol Sci (2015) 19(9):1621–9.
29. Silva MA, Hegab B, Hyde C, Guo B, Buckels JA, Mirza DF. Needle track seeding following biopsy of liver lesions in the diagnosis of hepatocellular cancer: A systematic review and meta-analysis. Gut (2008) 57(11):1592–6. doi: 10.1136/gut.2008.149062
30. Robert M, Sofair AN, Thomas A, Bell B, Bialek S, Corless C, et al. A comparison of hepatopathologists' and community pathologists' review of liver biopsy specimens from patients with hepatitis c. Clin Gastroenterol Hepatol (2009) 7(3):335–8. doi: 10.1016/j.cgh.2008.11.029
31. Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American association for the study of liver diseases. Hepatology (2018) 68(2):723–50. doi: 10.1002/hep.29913
32. Lambin P, Rios-Velazquez E, Leijenaar R, Carvalho S, Stiphout RGPMV, Granton P, et al. Radiomics: Extracting more information from medical images using advanced feature analysis. Eur J Cancer (2012) 48(4):441–6. doi: 10.1016/j.ejca.2011.11.036
33. Lambin P, Leijenaar RTH, Deist TM, Peerlings J, de Jong EEC, van Timmeren J, et al. Radiomics: The bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol (2017) 14(12):749–62. doi: 10.1038/nrclinonc.2017.141
34. Yin R, Jiang M, Lv WZ, Jiang F, Li J, Hu B, et al. Study processes and applications of ultrasomics in precision medicine. Front Oncol (2020) 10:1736. doi: 10.3389/fonc.2020.01736
35. Mao B, Ma J, Duan S, Xia Y, Tao Y, Zhang L. Preoperative classification of primary and metastatic liver cancer Via machine learning-based ultrasound radiomics. Eur Radiol (2021) 31(7):4576–86. doi: 10.1007/s00330-020-07562-6
36. Dong Y, Wang QM, Li Q, Li LY, Zhang Q, Yao Z, et al. Preoperative prediction of microvascular invasion of hepatocellular carcinoma: Radiomics algorithm based on ultrasound original radio frequency signals. Front Oncol (2019) 9:1203. doi: 10.3389/fonc.2019.01203
37. Ma QP, He XL, Li K, Wang JF, Zeng QJ, Xu EJ, et al. Dynamic contrast-enhanced ultrasound radiomics for hepatocellular carcinoma recurrence prediction after thermal ablation. Mol Imaging Biol (2021) 23(4):572–85. doi: 10.1007/s11307-021-01578-0
38. Wang HQ, Yang C, Zeng MS, Rao SX, Ji Y, Weng X, et al. Magnetic resonance texture analysis for the identification of cytokeratin 19-positive hepatocellular carcinoma. Eur J Radiol (2019) 117:164–70. doi: 10.1016/j.ejrad.2019.06.016
39. Wang W, Gu D, Wei J, Ding Y, Yang L, Zhu K, et al. A radiomics-based biomarker for cytokeratin 19 status of hepatocellular carcinoma with gadoxetic acid-enhanced mri. Eur Radiol (2020) 30(5):3004–14. doi: 10.1007/s00330-019-06585-y
40. Yang F, Wan Y, Xu L, Wu Y, Shen X, Wang J, et al. Mri-radiomics prediction for cytokeratin 19-positive hepatocellular carcinoma: A multicenter study. Front Oncol (2021) 11:672126. doi: 10.3389/fonc.2021.672126
41. Dyer RK Jr., Nakmali D, Dormer KJ. Magnetic resonance imaging compatibility and safety of the soundtec direct system. Laryngoscope (2006) 116(8):1321–33. doi: 10.1097/01.mlg.0000230479.39551.4a
42. Kim T-H, Kim SY, Tang A, Lee JM. Comparison of international guidelines for noninvasive diagnosis of hepatocellular carcinoma: 2018 update. Clin Mol Hepatol (2019) 25(3):245–63. doi: 10.3350/cmh.2018.0090
43. Mao B, Zhang L, Ning P, Ding F, Wu F, Lu G, et al. Preoperative prediction for pathological grade of hepatocellular carcinoma Via machine learning-based radiomics. Eur Radiol (2020) 30(12):6924–32. doi: 10.1007/s00330-020-07056-5
44. Ren S, Li Q, Liu S, Qi Q, Duan S, Mao B, et al. Clinical value of machine learning-based ultrasomics in preoperative differentiation between hepatocellular carcinoma and intrahepatic cholangiocarcinoma: A multicenter study. Front Oncol (2021) 11:749137. doi: 10.3389/fonc.2021.749137
45. Ren S, Qi Q, Liu S, Duan S, Mao B, Chang Z, et al. Preoperative prediction of pathological grading of hepatocellular carcinoma using machine learning-based ultrasomics: A multicenter study. Eur J Radiol (2021) 143:109891. doi: 10.1016/j.ejrad.2021.109891
46. Ma J, Duan S, Zhang Y, Wang J, Wang Z, Li R, et al. Efficient deep learning architecture for detection and recognition of thyroid nodules. Comput Intell Neurosci (2020) 2020:1242781. doi: 10.1155/2020/1242781
47. Conti A, Duggento A, Indovina I, Guerrisi M, Toschi N. Radiomics in breast cancer classification and prediction. Semin Cancer Biol (2021) 72:238–50. doi: 10.1016/j.semcancer.2020.04.002
48. Bektas CT, Kocak B, Yardimci AH, Turkcanoglu MH, Yucetas U, Koca SB, et al. Clear cell renal cell carcinoma: Machine learning-based quantitative computed tomography texture analysis for prediction of fuhrman nuclear grade. Eur Radiol (2019) 29(3):1153–63. doi: 10.1007/s00330-018-5698-2
49. Chen T, Guestrin C. (2016). Xgboost: A scalable tree boosting system, in: Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, (San Francisco, California, USA: Computing Machinery). doi: 10.1145/2939672.2939785
50. Choi SY, Kim SH, Park CK, Min JH, Lee JE, Choi YH, et al. Imaging features of gadoxetic acid-enhanced and diffusion-weighted Mr imaging for identifying cytokeratin 19-positive hepatocellular carcinoma: A retrospective observational study. Radiology (2018) 286(3):897–908. doi: 10.1148/radiol.2017162846
Keywords: hepatocellular carcinoma, machine learning, radiomics, cytokeratin 19 (CK19), ultrasonography
Citation: Zhang L, Qi Q, Li Q, Ren S, Liu S, Mao B, Li X, Wu Y, Yang L, Liu L, Li Y, Duan S and Zhang L (2022) Ultrasomics prediction for cytokeratin 19 expression in hepatocellular carcinoma: A multicenter study. Front. Oncol. 12:994456. doi: 10.3389/fonc.2022.994456
Received: 14 July 2022; Accepted: 10 August 2022;
Published: 02 September 2022.
Edited by:
Xin-Wu Cui, Huazhong University of Science and Technology, ChinaCopyright © 2022 Zhang, Qi, Li, Ren, Liu, Mao, Li, Wu, Yang, Liu, Li, Duan and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lianzhong Zhang, emx6ODc3N0B6enUuZWR1LmNu; Shaobo Duan, ZHVzdGluMjY2MkAxNjMuY29t
 Linlin Zhang
Linlin Zhang Qinghua Qi3
Qinghua Qi3 Shanshan Ren
Shanshan Ren