- 1Department of Stomatology, The Affiliated First Hospital of Zhengzhou University, Zhengzhou University, Zhengzhou, China
- 2Department of Radiology, The Affiliated Cancer Hospital of Zhengzhou University & Henan Cancer Hospital, Zhengzhou, China
Objectives: To explore the possible risk factors of orocutaneous fistula (OCF) development in free flap reconstruction of the tongue/floor of the mouth (TFOM).
Methods: Data of patients who underwent free flap reconstruction of the TFOM were retrospectively analyzed. The association between clinicopathologic variables and OCF occurrence was analyzed using univariate and multivariate analyses.
Results: Altogether, 469 patients were enrolled. OCF occurred in 43 patients with a rate of 9.2%. The univariate analysis revealed the negative effects of smoking, preoperative albumin level, cachexia, T4 stage, neck dissection, entire resection of the floor of the mouth (FOM), segmental mandibulectomy, and surgical site infection on OCF occurrence. The multivariate analysis confirmed the independence of cachexia (p<0.001, 4.386[1.883–9.472]), tumor stage (p<0.001, 2.738[1.482–6.629]), entire FOM resection (p<0.001, 6.332[2.110–14.432]), and surgical site infection (p<0.001, 5.376[1.998–11.218]) in affecting the OCF development.
Conclusions: OCF development following free flap reconstruction of the TFOM was relatively uncommon, but significantly associated with presence of cachexia, T4 stage, entire FOM resection, and surgical site infection.
Introduction
Squamous cell carcinoma (SCC) in the tongue/floor of the mouth (TFOM), whose features include lymph node metastasis and local invasion, is the most common malignancy in the oral cavity. At the initial diagnosis, the majority of these tumors have an advanced stage (1, 2). Extensive soft or bone tissue resection is required, and free flap reconstruction is generally the preferred method (3); however, postoperative complications may develop frequently (4). One complication is orocutaneous fistula (OCF), which could cause significantly negative effects such as delays in adjuvant therapy initiation and oral feeding and voice rehabilitation, as well as increase in treatment costs, length of hospital stay, and risk of carotid blowout (5–7). Nowadays, methods for treating OCF include conventional wound care, negative pressure wound therapy, and surgical management (8–11).
A previous study has reported patient-related, tumor-related, and treatment-related factors in predicting fistula development after a larynx/hypopharynx surgery (12). However, considering the fact that there is larger and more dead space after a TFOM operation, there might be unique predictors for OCF occurrence in TFOM surgery.
However, studies regarding the predictors of OCF formation in oral surgery are rare (13–15). Dawson et al. (13) may be the first to analyze this issue and have reported an overall incidence of OCF occurrence of 11% in patients with different etiologies, such as cancer, ameloblastoma, osteoradionecrosis, and trauma. Moreover, previous chemoradiotherapy was the only significant factor increasing the possibility of OCF formation. Additionally, Girkar et al. (14) have reported a rate of 9% and identified that patients with surgical site infection (SSI) and bilateral neck dissection are at the maximum risk for developing OCF. No other similar literature is available for analyzing.
Therefore, this study aimed to explore the possible risk factors of OCF development in free flap reconstruction for TFOM SCC.
Patients and methods
Ethical considerations
The study was approved by The First Affiliated Hospital of Zhengzhou University institutional research committee, and all participants provided written informed consent. All methods and procedures were performed in accordance with the 1964 Helsinki Declaration.
Patient selection
Medical records of adult patients with surgically treated oral SCC between January 2010 and January 2022 were retrospectively reviewed in a Tertiary Level Teaching Hospital. Patients with primary TFOM SCC and those with defects repaired with a free flap were included. Those with a history of other malignant diseases or prior chemoradiotherapy were excluded. Data on demographics; body mass index (BMI); systemic diseases (hypertension, diabetes mellitus, and cardiovascular and cerebrovascular diseases); thyroid stimulating hormone (TSH) levels; cachexia; tumor, nodes, metastases stage according to the 8th American Joint Committee on Cancer classification; complications; and treatment were extracted and analyzed.
Definitions of variables
The normal range of whole blood hemoglobin was 115–150 g/L for women and 130–145 g/L for men. The normal range of venous albumin was 35–55 g/L. The normal range of blood serum TSH was 0.35–5.5 IU/ml. Based on the official standards by the World Health Organization for Asians (16), obesity, overweight, normal weight, and underweight were defined as BMI ≥ 25 kg/m2, 23 kg/m2 ≤ BMI < 25 kg/m2, 18.5 kg/m2 ≤ BMI < 23 kg/m2, and BMI < 18.5 kg/m2, respectively. To simplify the analysis, the patients were classified into three groups with two BMI cutoffs of 23 kg/m2 and 18.5 kg/m2.
SSI was regarded as the occurrence of purulent drainage or an incision that spontaneously dehisces in a patient with fever and/or localized pain or tenderness or deep site infection detected by radiographic examination within 30 days after surgery (2).
Cachexia was regarded as the occurrence of weight loss > 2% in an individual already showing depletion or weight loss > 5% relative to the current body weight and height or skeletal muscle mass (17).
Treatment
Resection with a margin of at least 1 cm with lower lip splitting was attempted in all tumors. Excision methods of primary focus included hemi, total, or subtotal glossectomy combined with resection of the floor of the mouth (FOM). Segmental mandibulectomy was performed if apparent mandible involvement was detected intraoperatively or preoperatively. Neck dissection was performed for all patients, level I to III/IV dissection was for a cN0 neck, and level I to V dissection for a cN+ neck. The type of free flap was considered mostly based on the defect size and range.
For the first 24 h postoperatively, the flap was monitored hourly and then every 4 h for the next 72 h. Cephalosporin was administered intravenously 30 min before incision, and continued for at least 3–5 days postoperatively. Before patients were able to feed orally, nasogastric nutrition was administered routinely (18).
OCF
OCF was generally verified by a swallow study or dye test when there was combined clinical detection of a visible breach in the intraoral suture line, a foul odor emanating from the oral cavity, congestion and/or edema of the neck flap, collection in the neck, fever, turbid drain, and leukocytosis (13, 14).
In our cancer center (a Tertiary Level Teaching Hospital), the preferred method of treating an OCF was commonly conventional wound care consisting of wound flushing with saline and hydrogen peroxide as well as compressive dressings. If the fistula was enormous determined by experience or the closure time was excessively long, negative pressure wound therapy and secondary surgery were selectively performed.
Statistical analysis
The relationship between OCF occurrence and clinicopathologic variables was firstly analyzed using the Chi-square test (univariate analysis). Then, the significant factors in the univariate analyses were included in the multivariate analysis (binomial logistic regression). All statistical analyses were performed using SPSS 20.0, and a p<0.05 was considered significant.
Results
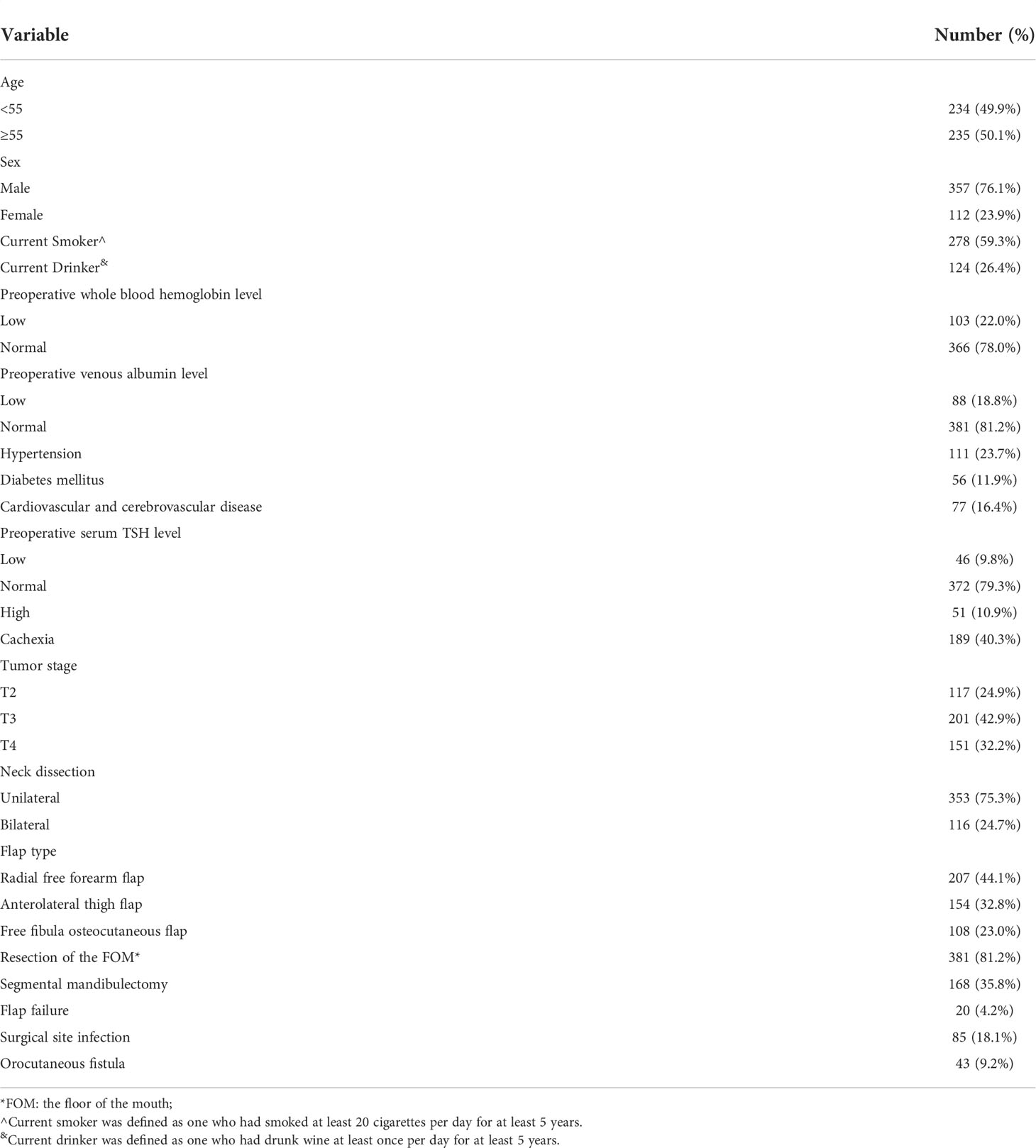
Overall, 469 patients, comprising 357 men and 112 women, were included for analysis. The median age was 55 (range: 36–76) years. Smoking and drinking were recorded in 278 and 124 patients, respectively. Hypertension, diabetes mellitus, and cardiovascular and cerebrovascular diseases occurred in 111, 56, and 77 patients, respectively. Low hemoglobin and albumin levels were present in 103 and 88 patients, respectively. Low, normal, and high TSH levels were recorded in 46, 372, and 51 patients, respectively. Cachexia was noted in 189 patients.
Tumor stages were distributed as T2 in 117 patients, T3 in 201 patients, and T4 in 151 patients. Neck stages were distributed as N0 in 276 patients and N+ in 193 patients. Hemi, subtotal, and total glossectomies were performed in 234, 156, and 79 patients, respectively. Partial and entire resections of the FOM were performed in 252 and 129 patients, respectively. Segmental mandibulectomy was performed in 168 patients. Unilateral and bilateral neck dissections were performed in 353 and 116 patients, respectively. Radial forearm free (RFF) flap, anterolateral thigh flap, and free fibula osteocutaneous (FFO) flap reconstructions were performed in 207, 154, and 108 patients, respectively.
SSI occurred in 85 patients. Vascular crisis developed in 45 flaps, and exploratory operation successfully salvaged 25 flaps. In the remaining 20 cases, a local flap was used for 10 patients, and a major pectoralis myocutaneous flap was used for ten patients (Table 1).
OCF occurrence
OCF occurred in 43 patients with a rate of 9.2%. The mean size of OCF was 2.8 ± 1.3 cm. The incidence of OCF development in patients with low and normal preoperative albumin levels was 15.9% and 7.6%, respectively, with a significant difference (p=0.015). Smokers had a rate of OCF formation of 11.9%, it was significantly higher than 5.2% in non-smokers (p=0.014). Patients with cachexia had a significantly higher OCF formation rate than those without cachexia (12.2% vs 5.3%, p=0.003). Patients with T4 tumors had a significantly higher OCF incidence than patients with T2/3 tumors (16.6% vs 5.7%, p<0.001). The bilateral neck dissection group had a significantly higher OCF development rate than the unilateral neck dissection group (13.8% vs 7.6%, p=0.047). Patients who underwent an entire FOM resection had a significantly higher OCF occurrence rate than patients who underwent no or partial FOM resection (23.2% vs 3.8%, p<0.001). Segmental mandibulectomy indicated an OCF occurrence rate of 13.1%, which was significantly higher than 7.0% in non-segmental mandibulectomy group (p=0.028). A significant difference was observed in the rate of OCF development in the SSI group and the non-SSI group at 20.0% and 6.8%, respectively (p<0.001). No other significant factors were associated with OCF development (Table 2).
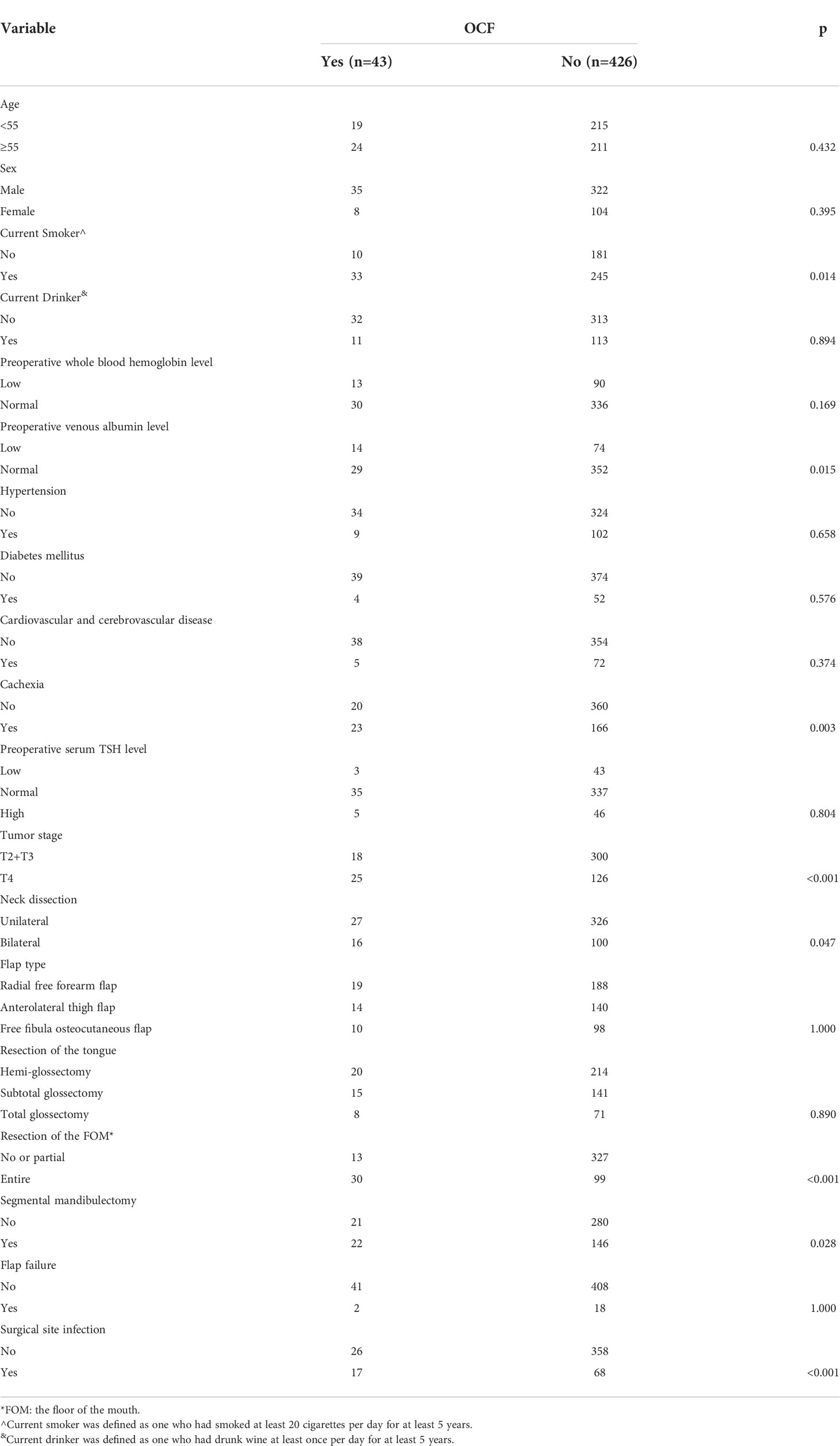
Table 2 Univariate analysis of the association between clinicopathologic variables and orocutaneous fistula (OCF) development.
In the subsequent multivariate analyses, cachexia (p<0.001, 4.386[1.883–9.472]), tumor stage (p<0.001, 2.738[1.482–6.629]), entire FOM resection (p<0.001, 6.332[2.110–14.432]), and SSI (p<0.001, 5.376[1.998–11.218]) were independently associated with increased risk of the occurrence of OCF (Table 3).
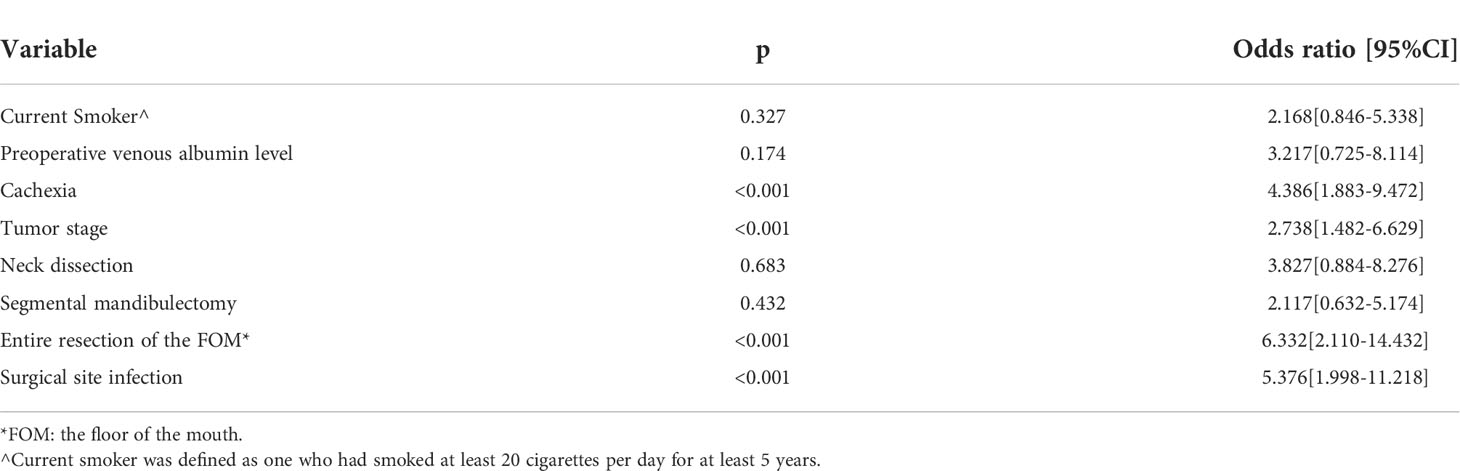
Table 3 Multivariate analysis of the association between clinicopathologic variables and orocutaneous fistula (OCF) development.
OCF treatment
All OCFs were initially treated by wound washing with normal saline and hydrogen peroxide solution, and a gauze with iodine dressing was placed within the fistula to stimulate the development of fresh granulation tissue. Oral feeding was prohibited but was replaced by nasal feeding nutrition until total recovery of the fistula. Thirty OCFs achieved total recovery by the single use of conventional wound care, and the median duration for total recovery was 20 days with a range from 4 days to 47 days. The remaining thirteen OCFs were treated successfully by local flaps including seven sliding advancement flaps and six rotation flaps, and no secondary OCF formation was observed.
Discussion
The most important finding in this study was that OCF development following free flap reconstruction for TFOM was relatively uncommon, but was significantly associated with the presence of cachexia, T4 stage, entire FOM resection, and SSI. Although conventional wound care alone could treat most OCFs, it was time-consuming.
Cachexia is associated with inadequate food intake, metabolic derangement, inactivity, loss of muscle mass, and weight loss in patients with advanced malignant tumors (17). More toxicities, treatment gaps, and postoperative complications as well as poorer disease-free survival are generally contributed by cachexia (19). Fukuta et al. (20) prospectively enrolled 98 patients with gastric or colorectal cancer, and 22.4% of those were diagnosed with cachexia; they discovered that the cachexia group had a significantly longer postoperative length of stay than the non-cachexia group. Similarly, Mason et al. (21) analyzed the short-term effect of cachexia on postoperative complications, and have reported that adverse events tended to occur in 64.3% of patients with cachexia, a rate that was significantly higher than that in those without cachexia. A study focusing on clinical impact of cachexia in patients with head and neck cancer undergoing chemoradiotherapy by Hayashi et al. (22) described that cachexia could play a negative role in all adverse events. Regarding grade 3/4 adverse events, a significant difference in the incidence of anemia, neutropenia, and leukopenia was observed between patients with and without cachexia. To the best of our knowledge, this study may be the first to report the importance of cachexia in causing OCF development, which could be explained by the impairing would healing capacity in patients with cachexia, it might be reflected by that cachexia patients were at higher risk of low preoperative venous blood albumin levels. This finding provides a reliable theoretical basis for decreasing OCF occurrence by improving patients’ nutritional status.
Tumor stage and entire FOM resection were both predictors and are also significantly associated with OCF occurrence. A T4 TFOM tumor generally indicated entire FOM resection with the help of lower lip splitting for complete disease clearance (23), then a large dead space could be expected; the importance of its obliteration had been emphasized by Al Deek et al. (6). The authors commented that the dead space between the hyoid bone and the mandible should be reconstructed with viable tissue to prevent OCF occurrence, which was occupied by suprahyoid muscles originally. Importantly, after establishing perfusion, reliability of the part of the flap inserted in the dead space should be re-checked, especially when there was an excess muscle resected or an orientation change during the flap inset. The viewpoint would also be supported by our results. Similarly, in a report by Girkar et al. (14), the rate of OCF development in patients with TFOM SCC and other subsites SCC was 15% and 7% independent of the used flap type, respectively, and the difference was significant. In our opinion, during the recovery period, motion of the reconstructed TFOM still occurred owing to the stimulation of saliva despite prohibition of oral intake. Therefore, in cases of an imperfect flap design, these movements could impair the water-tight closure directly, which caused accumulation of saliva at the TFOM. Thus, to minimize the possibility of suture dehiscence and tearing, tension must be distributed by multilayer mattress sutures that should be used to reduce tension.
Negative effects of SSI were also apparent, although they were common following free flap reconstruction and could develop in approximately 30% of patients (24). Both patient-related and treatment-related factors were related to SSI, including poor oral hygiene, poor nutritional status, prolonged operative time, type of reconstruction, faulty surgical techniques, and resection range. Šifrer et al. (25) recently described in their study of 48 patients with SSI that 38 patients suffered from pharyngocutaneous fistula, although in the patients without SSI, the rate of pharyngocutaneous fistula was only 18.2%. Moreover, the authors emphasize the importance of SSI timing, which should be started on the 5th postoperative day in the fistula group and on the 7th postoperative day in the control group. Andrades et al. (26) have reported that fistulas occurred in 28.8% of 104 patients undergoing RFF flap for hypopharyngeal reconstruction, although the incidence significantly increased in patients with SSI. Our results were also consistent with the finding. Generally, fistula and infections coexist, resulting in a vicious cycle where one may lead to the other (15). A fistula almost always presents as an infection initially, timely anti-infection treatment is essential for decreasing the OCF development. In the other hand, early detection of an OCF could be achieved by a swallow study or dye test from infected sites.
Negative effects of previous chemoradiotherapy and bilateral neck dissection have been reported in other literature (13, 14). On one hand, indication for bilateral neck dissection midline across the primary tumor or pathologically proven lymph nodes in the contralateral neck is related to an advanced stage disease, requiring extensive soft or bone tissue resection; increased surgery duration and intraoperative bleeding are expected. On the other hand, tissue fibrosis easily results from previous chemoradiotherapy and conversely causes poor wound healing (27). These aspects might help to predict the likelihood of OCF development in patients with the two features. However, this study failed to identify a positive association, and this might be due to the different study design and enrollment criteria. It could be noted that current OCF formulation rate is a little higher than that (7.7%) reported by Tassone et al. (27) who also enrolled patients with previous irradiation, there are at least three aspects contributing to the difference, first, all patients in current study received a lip split, second, the two studies have different inclusion criteria, third, previously radiated patients may not have had extensive neck surgery at the time of their salvage resections.
Segmental mandibulectomy is a reliable method for treating cases involving the mandible. Free flap reconstruction is commonly performed to maintain better appearance and functional results. However, short-term and long-term complications of this procedure, such as SSI and pathologic fracture/exposure of the mandible, have been previously reported (28, 29). However, in this study, we failed to identify the effects of segmental mandibulectomy on OCF occurrence. At least two aspects can explain this: firstly, the dead space between the mandible and hyoid disappeared after segmental mandibulectomy; secondly, no flap necrosis was observed in patients undergoing a FFO flap.
Smoking and drinking were the main risk factors for head and neck SCC, current study did not find the relationship between smoking and OCF development, but we still should emphasize the harmful effect of tobacco on postoperative complication (30). It was interesting to note that alcohol intake status did not appear to have a significant influence on OCF development in this study. Two aspects must be considered, on the one hand, even though East Asian patients consumed alcohol, but they were at a much lower risk for heavy alcoholism than people with functional aldehyde dehydrogenase (ALDH) genes which encodes one of the two enzymes primarily involved in alcohol metabolism (31). On the other hand, because of the high prevalence of ALDH2*2 allele among East Asian populations, East Asians may be more susceptible to the carcinogenic effect of alcohol, with most evidence coming from studies of esophageal cancer and head and neck cancer (32), however, perhaps, a more comprehensive study assessing the influence of alcohol intake on the postoperative TFOM reconstructive surgery complications in both Asian and non-Asian populations would be needed in the future.
Treating OCF requires longer time, which may take 1 month or longer (5). Conventional wound care, negative pressure wound therapy, and surgical treatment are the major treatment methods for OCF (6–11). Tian et al. (8), Inatomi et al. (10), and Khoo et al. (5) have verified the reliability of negative pressure wound therapy with a high success rate and shorter treatment time. This study might support the feasibility of conventional wound care with a high response rate, which was consistent with the finding of Andrades et al. (26).
Limitations in current study must be acknowledged, first, there was inherent bias within the retrospective study; second, both smoking and drinking status was not stratified based on the frequency and severity, it might cover up some interesting findings.
In summary, OCF development following free flap reconstruction for TFOM was relatively uncommon, although it was significantly associated with cachexia, T4 stage, entire FOM resection, and SSI. Although conventional wound care alone could cure most OCFs, it was time-consuming.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by The First Affiliated Hospital of Zhengzhou University institutional research committee. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All the authors made the contribution in study design, manuscript writing, studies selecting, data analysis, study quality evaluating, and manuscript revising. All authors have read and approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.947643/full#supplementary-material
References
1. Fang Q, Li P, Qi J, Luo R, Chen D, Zhang X. Value of lingual lymph node metastasis in patients with squamous cell carcinoma of the tongue. Laryngoscope (2019) 129:2527–30. doi: 10.1002/lary.27927
2. Karthik K, Dhiwakar M. Predictors of surgical site infection and pneumonia following oral cavity tumor surgery. Head Neck (2021) 43:3106–15. doi: 10.1002/hed.26799
3. Olinde LM, Farber NI, Kain JJ. Head and neck free-flap salvage. Curr Opin Otolaryngol Head Neck Surg (2021) 29:429–36. doi: 10.1097/MOO.0000000000000739
4. Garip M, Van Dessel J, Grosjean L, Politis C, Bila M. The impact of smoking on surgical complications after head and neck reconstructive surgery with a free vascularised tissue flap: a systematic review and meta-analysis. Br J Oral Maxillofac Surg (2021) 59:e79–98. doi: 10.1016/j.bjoms.2020.07.020
5. Khoo MJW, Ooi ASH. Management of postreconstructive head and neck salivary fistulae: A review of current practices. J Plast Reconstr Aesthet Surg (2021) 74:2120–32. doi: 10.1016/j.bjps.2020.12.096
6. Al Deek NF, Wei FC, Tsao CK. Fistulae after successful free tissue transfer to head and neck: its prevention and treatment. Clin Plast Surg (2016) 43:739–45. doi: 10.1016/j.cps.2016.05.010
7. Chang HP, Hong JW, Lee WJ, Kim YS, Koh YW, Kim SH, et al. Incorporating a continuous suction system as a preventive measure against fistula-related complications in head and neck reconstructive surgery. Arch Plast Surg (2018) 45:449–57. doi: 10.5999/aps.2018.00094
8. Tian B, Khoo D, Tay AC, Soo KC, Tan NC, Tan HK, et al. Management of orocutaneous fistulas using a vacuum-assisted closure system. Head Neck (2014) 36:873–81. doi: 10.1002/hed.23393
9. Kiong KL, Tan NC, Skanthakumar T, Teo CEH, Soo KC, Tan HK, et al. Salivary fistula: Blue dye testing as part of an algorithm for early diagnosis. Laryngoscope Investig Otolaryngol (2017) 2:363–8. doi: 10.1002/lio2.112
10. Inatomi Y, Kadota H, Yoshida S, Kamizono K, Shimamoto R, Fukushima S, et al. Utility of negative-pressure wound therapy for orocutaneous and pharyngocutaneous fistula following head and neck surgery. Head Neck (2020) 42:103–10. doi: 10.1002/hed.25989
11. Sanchez A, Frank E, Inman J, Wang W, Namin A, Ducic Y. Fistula management in head and neck cancer. Semin Plast Surg (2020) 34:299–304. doi: 10.1055/s-0040-1721825
12. Wang M, Xun Y, Wang K, Lu L, Yu A, Guan B, et al. Risk factors of pharyngocutaneous fistula after total laryngectomy: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol (2020) 277:585–99. doi: 10.1007/s00405-019-05718-9
13. Dawson C, Gadiwalla Y, Martin T, Praveen P, Parmar S. Factors affecting orocutaneous fistula formation following head and neck reconstructive surgery. Br J Oral Maxillofac Surg (2017) 55:132–5. doi: 10.1016/j.bjoms.2016.07.021
14. Girkar F, Thiagarajan S, Malik A, Sawhney S, Deshmukh A, Chaukar D, et al. Factors predisposing to the development of orocutaneous fistula following surgery for oral cancer: Experience from a tertiary cancer center. Head Neck (2019) 41:4121–7. doi: 10.1002/hed.25951
15. Fang Q, Yuan J, Du W, Dai L, Zhang X, Luo R. Orocutaneous fistula formation in free flap reconstruction for oral squamous cell carcinoma. Front Oncol (2022) 12:887118. doi: 10.3389/fonc.2022.887118
16. Wang L, Zhou B, Zhao Z, Yang L, Zhang M, Jiang Y, et al. Body-mass index and obesity in urban and rural China: findings from consecutive nationally representative surveys during 2004-18. Lancet (2021) 398:53–63. doi: 10.1016/S0140-6736(21)00798-4
17. Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol (2011) 12:489–95. doi: 10.1016/S1470-2045(10)70218-7
18. Feng A, Zhang J, Lu X, Fang Q. Effect of blood transfusion on short- and long-term outcomes in oral squamous cell carcinoma patients undergoing free flap reconstruction. Front Surg (2021) 8:666768. doi: 10.3389/fsurg.2021.666768
19. Nagpal P, Pruthi DS, Pandey M, Yadav A, Singh H. Impact of sarcopenia in locally advanced head and neck cancer treated with chemoradiation: An Indian tertiary care hospital experience. Oral Oncol (2021) 121:105483. doi: 10.1016/j.oraloncology.2021.105483
20. Fukuta A, Saito T, Murata S, Makiura D, Inoue J, Okumura M, et al. Impact of preoperative cachexia on postoperative length of stay in elderly patients with gastrointestinal cancer. Nutrition (2019) 58:65–8. doi: 10.1016/j.nut.2018.06.022
21. Mason MC, Garcia JM, Sansgiry S, Walder A, Berger DH, Anaya DA. Preoperative cancer cachexia and short-term outcomes following surgery. J Surg Res (2016) 205:398–406. doi: 10.1016/j.jss.2016.06.076
22. Hayashi N, Sato Y, Fujiwara Y, Fukuda N, Wang X, Nakano K, et al. Clinical impact of cachexia in head and neck cancer patients who received chemoradiotherapy. Cancer Manag Res (2021) 13:8377–85. doi: 10.2147/CMAR.S329581
23. Cheng SJ, Ko HH, Lee JJ, Kok SH. Comparison of long-term outcomes between pull-through resection and mandibular lip-split surgery for T4a tongue/floor of mouth cancers. Head Neck (2018) 40:144–53. doi: 10.1002/hed.24994
24. Lin SC, Chang TS, Yang KC, Lin YS, Lin YH. Factors contributing to surgical site infection in patients with oral cancer undergoing microvascular free flap reconstruction. Eur Arch Otorhinolaryngol (2018) 275:2101–8. doi: 10.1007/s00405-018-5035-z
25. Šifrer R, Aničin A, Pohar MP, Žargi M, Pukl P, Soklič T, et al. Pharyngocutaneous fistula: the incidence and the risk factors. Eur Arch Otorhinolaryngol (2016) 273:3393–9. doi: 10.1007/s00405-016-3963-z
26. Andrades P, Pehler SF, Baranano CF, Magnuson JS, Carroll WR, Rosenthal EL. Fistula analysis after radial forearm free flap reconstruction of hypopharyngeal defects. Laryngoscope (2008) 118:1157–63. doi: 10.1097/MLG.0b013e31816f695a
27. Tassone P, Galloway T, Dooley L, Zitsch R 3rd. Orocutaneous fistula after oral cavity resection and reconstruction: systematic review and meta-analysis. Ann Otol Rhinol Laryngol (2021) 34894211047463. doi: 10.1177/00034894211047463
28. Bowe C, Butler D, Dhanda J, Gulati A, Norris P, Bisase B. Lateral segmental mandibulectomy reconstruction with bridging reconstruction plate and anterolateral thigh free flap: a case series of 30 consecutive patients. Br J Oral Maxillofac Surg (2021) 59:91–6. doi: 10.1016/j.bjoms.2020.08.054
29. Blackwell KE, Buchbinder D, Urken ML. Lateral mandibular reconstruction using soft-tissue free flaps and plates. Arch Otolaryngol Head Neck Surg (1996) 122:672–8. doi: 10.1001/archotol.1996.01890180078018
30. Wang CY, Dudzinski J, Nguyen D, Armbrecht E, Maher IA. Association of smoking and other factors with the outcome of mohs reconstruction using flaps or grafts. JAMA Facial Plast Surg (2019) 21:407–13. doi: 10.1001/jamafacial.2019.0243
31. Wall TL, Ehlers CL. Genetic influences affecting alcohol use among asians. Alcohol Health Res World (1995) 19:184–9.
Keywords: free flap, tongue, floor of the mouth, orocutaneous fistula, cachexia, system design
Citation: Li W, Wu S, Yuan J, Meng F, Xu C and Li H (2022) Predictors predisposing to orocutaneous fistula occurrence following free flap reconstruction. Front. Oncol. 12:947643. doi: 10.3389/fonc.2022.947643
Received: 19 May 2022; Accepted: 27 June 2022;
Published: 18 July 2022.
Edited by:
Gyorgy B Halmos, University Medical Center Groningen, NetherlandsReviewed by:
Sebastiaan De Visscher, University Medical Center Groningen, NetherlandsMartin Stenekes, University Medical Center Groningen, Netherlands
Copyright © 2022 Li, Wu, Yuan, Meng, Xu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenlu Li, bHdsZG9jdG9yQDE2My5jb20=
 Wenlu Li1*
Wenlu Li1* Junhui Yuan
Junhui Yuan