
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Oncol., 20 October 2022
Sec. Surgical Oncology
Volume 12 - 2022 | https://doi.org/10.3389/fonc.2022.933777
This article is part of the Research TopicCase Reports in Surgical Oncology: 2022View all 56 articles
Background: Lymphangiomatosis is an extremely rare disease with potential soft tissue, bone, and spleen involvement, which can be characterized by lymphangioma. Only a few cases of colon and mesenteric lymphangiomatosis have been reported. We report a case presenting with fatigue, periumbilical pain, and intermittent bloody stools. This patient underwent a series of examinations. Exploratory laparoscopy, in particular, yielded very valuable images and videos for this disease, which can provide evidence for the diagnosis of this disease.
Case summary: The current patient had fatigue, periumbilical pain, and intermittent bloody stools. Colonoscopy indicated numerous variable-sized hyaline cysts in the colon. Submucosal puncture was performed during colonoscopy. The patient was readmitted to the hospital due to periumbilical pain. B-ultrasound and abdominal CT showed multiple hypoechoic nodules in the mesenteric area. Exploratory laparoscopy was performed, and histopathology revealed that D2-40 was positive. Based on auxiliary examination and laparoscopic biopsy, surgeons and pathologists reached the diagnosis of mesenteric lymphangiomatosis.
Conclusion: Clinicians need to comprehensively improve their knowledge of lymphangiomatosis, and the combination of clinical symptoms, histological characteristics, and colonoscopy biopsy findings should be considered to improve lymphangiomatosis diagnosis, thereby reducing misdiagnosis.
Core tip: Colon and mesenteric lymphangiomatosis is an extremely uncommon benign condition of unknown etiology and pathogenesis in adult patients. We report a case of mesenteric lymphangiomatosis in a 37-year-old woman who presented with fatigue, periumbilical pain, and intermittent bloody stools, as well as lesions in the kidney, spleen, and bones. This case provides new insights into the diagnosis and treatment of this disease.
Colon and mesenteric lymphangiomatosis is an extremely uncommon benign condition of unknown etiology and pathogenesis, which could lead to compression symptoms caused by mechanical pressure. Here, we report a case of abdominal lymphangiomatosis evaluated by laparoscopy, which has not been previously reported.
Colonoscopy indicated numerous variable-sized hyaline cysts, involving the ascending colon, transverse colon, and descending colon (Figure 1A), while no biopsy was carried out. Submucosal puncture was performed during colonoscopy. One year later, the patient returned with periumbilical pain. In abdominal ultrasound, multiple hypoechoic nodules with marked intranodular blood flow were observed in the spleen with a maximum size of 1.2 * 1.2 cm, with well-defined margins. In the inferior pole of the left kidney, a hypoechoic nodule was found, with an approximate diameter of 1.6 cm and no blood flow signal. Enlarged lymph nodes (1.9 * 1.1 cm2) were found in the retroperitoneum (Figures 2A–C). Abdominal CT revealed multiple diffuse low-density shadowing zones without enhancement distributed in the mesenteric area, which partly surrounded the small bowel and presented a doughnut shape. The boundaries were blurred (Figure 2D). Low-density shadowing zones were observed in the left kidney, spleen, ilium, and fifth lumbar vertebra on CT scan images (Figures 2E–H). Based on the images, lymphangiomatosis was highly suspected, which was further confirmed by laparoscopic biopsy (Figure 3A). Further exploratory laparoscopy showed numerous hyalines, smooth-walled, variable-sized cystic microstructures in the root of the mesentery, involving total mesenteric excision (Figure 3B). The liquid inclusions were clear and pale yellowish (Video S1). Histopathology revealed diffuse or multi-centric proliferation of thin-walled, dilated lymphatic vessels (Figure 4A). D2-40 (a monoclonal antibody), a highly sensitive and specific marker of lymphatic endothelium in the normal tissue and a subset of vascular lesions, confirmed mesenteric lymphangiomatosis by immunoreaction (Figure 4B). D2-40-positive lymphatic vessels were shown in mesentery (Figures 4C, D). The patient was treated with sirolimus (0.8 mg/m2, Bid) for 3 months, and follow-up colonoscopy was performed. Colonoscopy indicated decreased number and size of cysts compared with the condition observed 6 months before (Figure 1B).

Figure 1 (A) Colonoscopy indicated numerous cysts in the ascending colon, transverse colon, and descending colon. (B) The patient treated with sirolimus within 3 months, and colonoscopy indicated that the number and size of cysts decreased.
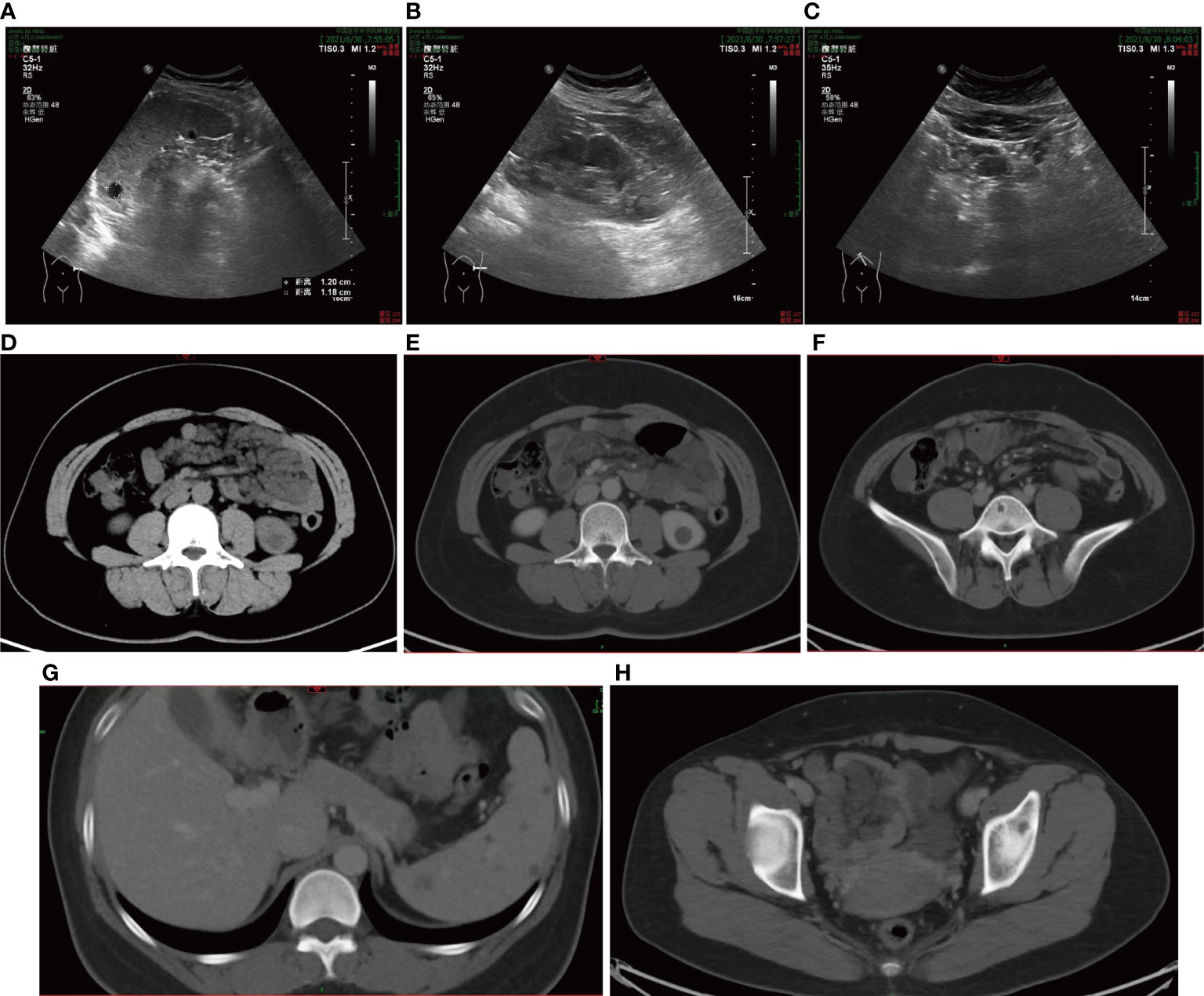
Figure 2 (A–C) Abdominal ultrasound observed multiple hypoechoic nodules in the spleen and the lower poles of the left kidney, and enlarged lymph nodes in the retroperitoneum. (D) Abdominal CT scan observed multiple diffuse low-density shadowing zones in the mesenteric area, which presented a doughnut shape. (E–H) Low-density shadowing zones can be observed in the left kidney, spleen, ilium, and the fifth lumbar vertebra in abdominal CT scan images.
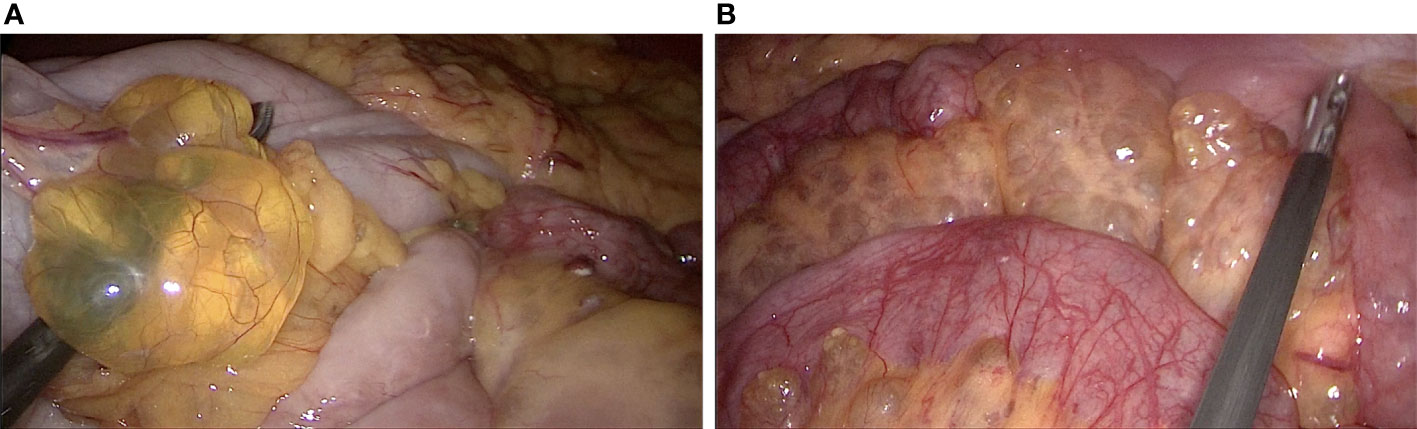
Figure 3 (A, B) Exploratory laparoscopy showed numerous hyalines, smooth-walled, variable-sized cystic microstructures in the root of the mesentery.
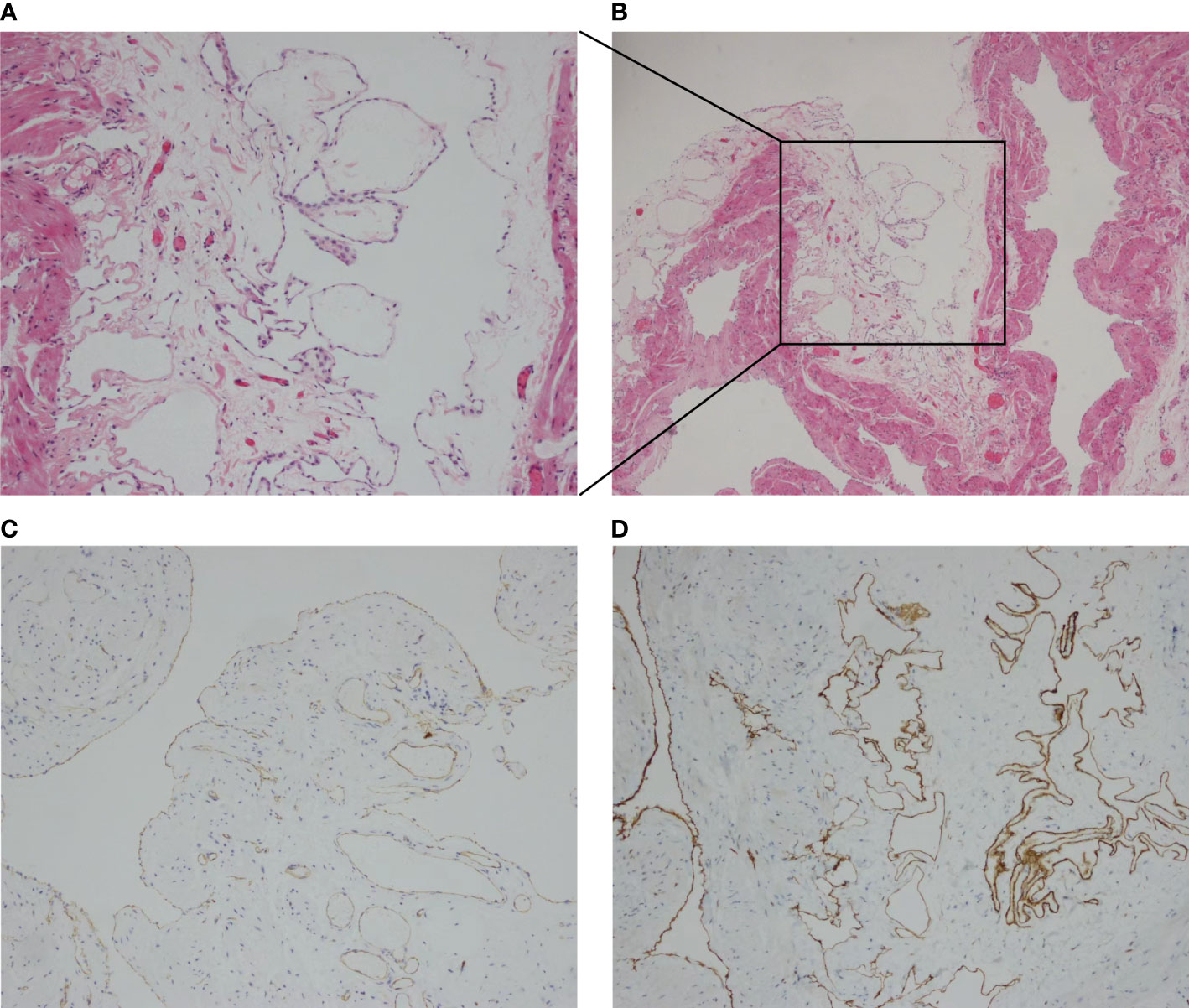
Figure 4 (A, B) Histological examination showed the positive D2-40 immunohistochemistry and confirmed mesenteric lymphangiomatosis. (C, D) Lymph vessels were identified imunohistochemically as D2-40-positive.
In 2014, generalized lymphatic anomaly (GLA) was proposed by the International Society for the Study of Vascular Anomalies (ISSVA) as a new term for lymphangiomatosis (1).
Mesenteric lymphangiomatosis is a benign cystic tumor of lymphatic vessels that occurs rarely in adults, while its etiology and pathogenesis remain elusive (2). It has variable clinical presentations and can involve different sites, including the mesentery, bone, spleen, mediastinum, lungs, and soft tissues (3). The clinical course and compression symptoms are directly correlated to the affected sites, mechanical pressure, and extent of the disease. In most cases, these lesions are multicystic and characterized by hypodense regions on CT images, without increased vascular flow on color Doppler ultrasound. We analyzed 11 previous cases of lymphangiomatosis involving the gastrointestinal tract and summarized them in Table 1. We listed the symptom and examination procedure of these cases so that colleagues can learn more about the disease. Reviews of the literature confirm that lymphangiomatosis progresses slowly and can be well controlled with appropriate treatment.
A case report of mesenteric lymphangiomatosis indicated that surgical resection of the mesentery could be an option in case of mechanical obstruction (15). However, the defect caused by the operation may lead to internal herniation, eventually resulting in bowel obstruction and intestinal volvulus. Repairing the defect with Permacol was performed with no complications after 4 years (14). Biomaterial implant may be an option for closing the mesenteric defect caused by surgery. Lymphorrhea after open or laparoscopic biopsy is one of the possible complications. Minor lymphatic leakage can be resolved by conservative management. Massive lymphatic leaks can be treated by embolization, but surgery may be necessary in some cases (16). Regarding the pharmacotherapy of lymphangiomatosis, sirolimus is an inhibitor of mammalian target of rapamycin (mTOR). Elisa Boscolo reached the conclusion that sirolimus suppresses the growth of lymphatic endothelial cells by inhibiting VEGF-A- and VEGF-C-driven proliferation and migration, thus impeding lymphangiogenesis (17). It is very effective in the treatment of multiple complicated vascular anomalies and has potential antitumor effects (18). Follow-up of the present case observed a significant decrease in number and size of cysts by colonoscopy.
Exploratory laparoscopy has not been utilized to evaluate mesenteric lymphangiomatosis so far, although a case report suggested that surgical resection of the mesentery could be an option in case of mechanical obstruction (14). The present case revealed the multi-systemic imaging manifestations of a rare systemic disease and highlighted the importance of exploratory laparoscopy in the diagnosis of mesenteric lymphangiomatosis.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
XW and YY contributed to the study concept and design. YY generated the literature strategy and filtered through the identified studies. YY evaluated study quality and wrote the manuscript. RW provided critical feedback on the manuscript. All authors contributed to the article and approved the submitted version.
National Natural Science Foundation of China, Grant Number: 82072732, 81572930; The National Key Research and Development Program of China, Grant Number: 2016YFC0905303; Beijing Science and Technology Plan, Grant Number: D171100002617004.
We thank Dr. Hulin Ma for data acquisition and clinical assessment and thank pathologist Quan Zhou for her contribution in the diagnosis of mesenteric lymphangiomatosis.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.933777/full#supplementary-material
Supplementary Video 1 | Laparoscopic presentation of lymphangiomatosis.
1. Dasgupta R, Fishman SJ. Issva classification. Semin Pediatr Surg (2014) 23(4):158–61. doi: 10.1053/j.sempedsurg.2014.06.016
2. Ozeki M, Fukao T, Kondo N. Propranolol for intractable diffuse lymphangiomatosis. New Engl J Med (2011) 364(14):1380–2. doi: 10.1056/NEJMc1013217
3. Pauzner R. Successful thalidomide treatment of persistent chylous pleural effusion. Ann Internal Med (2007) 146(1):75–6. doi: 10.7326/0003-4819-146-1-200701020-00022
4. Cao D, Wang J, Guo L. Gastrointestinal: Diffuse esophageal lymphangiomatosis manifesting as multiple submucosal masses. J Gastroenterol Hepatol (2020) 35(2):177. doi: 10.1111/jgh.14754
5. Lu G, Li H, Li Y. Lymphangiomatosis of the sigmoid colon - a rare cause of lower gastrointestinal bleeding: A case report and review of the literature. Oncol Lett (2017) 13(1):339–41. doi: 10.3892/ol.2016.5399
6. Mujagic Z, Masclee AAM, Keszthelyi D. Lymphangiomatosis of the colon. Clin Gastroenterol Hepatol (2022) 20(2):e14–e5. doi: 10.1016/j.cgh.2020.08.037
7. Giuliani A, Romano L, Coletti G, Walid AFM, Calvisi G, Maffione F, et al. Lymphangiomatosis of the ileum with perforation: A case report and review of the literature. Ann Med Surg (Lond) (2019) 41:6–10. doi: 10.1016/j.amsu.2019.03.010
8. Hwang SS, Park SY, Radiology DO, Hospital SV. Cavernous mesenteric lymphangiomatosis mimicking metastasis in a patient with rectal Cancer: A case report. World J Gastroenterol (2009) 15(31):3947–9. doi: 10.3748/wjg.15.3947
9. Rai P, Rao RN, Chakraborthy S. Case report: Caecal lymphangioma: A rare cause of gastrointestinal blood loss. (2013) 2013:bcr2013008866. doi: 10.1136/bcr-2013-008866
10. Liang X, Wei GG, Hou J, Di G, Xiao JC. Huge lymphangiomatosis of the esophagus. Ann Thorac Surg (2012) 93(6):2048-51. doi: 10.1016/j.athoracsur.2011.11.021
11. Alhasan AS, Daqqaq TS. Extensive abdominal lymphangiomatosis involving the small bowel mesentery: A case report. World J Clin Cases (2021) 9(32):7. doi: 10.12998/wjcc.v9.i32.9990
12. Meerhaeghe TV, Vandenbroucke F, Velkeniers B. Systemic generalised lymphangiomatosis: Unknown aetiology and a challenge to treat. BMJ Case Rep (2021) 14(1):e237331. doi: 10.1136/bcr-2020-237331
13. Amodeo I, Cavallaro G, Raffaeli G, Colombo L, Mosca F. Abdominal cystic lymphangioma in a term newborn: A case report and update of new treatments. Medicine (2017) 96(8):e5984. doi: 10.1097/MD.0000000000005984
14. Kim SH, Yoon KC, Lee W, Kim HY, Jung SE. Result of using a biologic collagen implant (Permacol) for mesenteric defect repair after excision of a huge mesenteric lymphangioma in a child. Ann Surg Treat Res (2015) 89(6):330–3. doi: 10.4174/astr.2015.89.6.330
15. de Vries JJ, Vogten JM, de Bruin PC, Boerma D, van de Pavoordt HD, Hagendoorn J. Mesenterical lymphangiomatosis causing volvulus and intestinal obstruction. Lymphat Res Biol (2007) 5(4):269–73. doi: 10.1089/lrb.2007.1010
16. Lv S, Wang Q, Zhao W, Han L, Wang Q, Batchu N, et al. A review of the postoperative lymphatic leakage. Oncotarget (2017) 8(40):69062–75. doi: 10.18632/oncotarget.17297
17. Boscolo E, Coma S, Luks VL, Greene AK, Klagsbrun M, Warman ML, et al. Akt hyper-phosphorylation associated with Pi3k mutations in lymphatic endothelial cells from a patient with lymphatic malformation. Angiogenesis (2015) 18(2):151–62. doi: 10.1007/s10456-014-9453-2
Keywords: lymphangiomatosis, exploratory, laparoscopy, colon, mesenteric
Citation: Yin Y, Wang R and Wang X (2022) Laparoscopy for evaluating mesenteric lymphangiomatosis: A case report. Front. Oncol. 12:933777. doi: 10.3389/fonc.2022.933777
Received: 01 May 2022; Accepted: 30 September 2022;
Published: 20 October 2022.
Edited by:
Airazat M. Kazaryan, Østfold Hospital, NorwayReviewed by:
Hai Zou, Fudan University, ChinaCopyright © 2022 Yin, Wang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xishan Wang, d3hzaGFuXzEyMDhAMTI2LmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.