
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Oncol. , 02 September 2022
Sec. Thoracic Oncology
Volume 12 - 2022 | https://doi.org/10.3389/fonc.2022.921151
This article is part of the Research Topic Reviews in Thoracic Oncology View all 17 articles
Purpose: This systematic review and meta-analysis aims to assess the effects of acupuncture on patient-reported outcomes (PROs) in adults with lung cancer.
Methods: Electronic databases including PubMed, Embase, Cochrane Library, Web of Science, China National Knowledge Infrastructure (CNKI), China Science and Technology Journal Database (CQVIP), Wanfang Data, SinoMed, and gray literatures were retrieved from inception to 1 July 2022 for randomized controlled trials (RCTs). Acupuncture was defined as an experimental intervention, and the patients of the control groups included either treatment including conventional therapy (usual care, sham/placebo acupuncture, pharmacotherapy including Western medicine and Chinese traditional medicine). PROs for this study were measured by seven scales of primary outcomes including the Karnofsky Performance Status (KPS), European Organization for Research and Treatment of Cancer Quality of Life Questionnaire, Functional Assessment of Cancer Therapy-Lung, Functional Assessment of Cancer Therapy Lung Cancer Subscale, Leicester Cough Questionnaire (LCQ score), the Medical Outcomes Study (MOS) item short form health survey (SF-36), and the St George’s Respiratory Questionnaire, and 12 scales of secondary outcomes. Cochrane Collaboration’s tool was used to assess the risks of bias. Data were combined and analyzed with RevMan 5.4 and Stata/SE 16.0.
Results: We retrieved 3,002 lung cancer patients from 33 trials. KPS included with 1,000 patients showed that acupuncture could significantly improve the quality of life (QOL) compared with the control group regardless of different tumor–node–metastasis stages or the different stages of disease. The study showed that acupuncture significantly improved lung cancer–related symptoms in the QOL, pain, nausea and vomiting, insomnia, anxiety and depression, fatigue, and constipation compared with the control group. Eight RCTs reported the occurrence of adverse events, whereas four reported none and four RCTs reported that the events in the observation group were significantly less than those in the control group.
Conclusion: Acupuncture proved to be a promising intervention, both postoperatively and after chemotherapy, and should be recommended as a beneficial alternative strategy to promote PROs in lung cancer patients at all stages of application. Considering the low quality, we suggest more rigorous clinical trials of acupuncture for lung cancer in the future and more emphasis on the effect of acupuncture in patients with lung cancer on their PROs, mainly in the aspect of the QOL.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?, identifier [CRD42021274122].
Lung cancer remains the most common cancer and the leading cause of cancer deaths (1). The overall 5-year survival rate for lung cancer diagnosed from 2010 to 2014 was in the range 10%–20% in most countries around the world, still being dismal (2). According to the latest global statistical analysis of International Agency for Research on Cancer, approximately 2.2 million new cases were diagnosed worldwide in 2020, with a mortality rate of 18% in the same year (3). Furthermore, the cost of drugs imposes a heavy social and economic burden on individuals, families, communities, and countries, thus posing substantial challenges (4). Studies have been conducted on patients after lung cancer surgery, commonly showing a significant decline in the quality of life (QOL) scores (5, 6).
Patient-reported outcomes (PROs) are the measurements of any aspect of a patient’s health obtained by a self-report, which means that there is no need for physician or any others to interpret the patient’s reactions (7). PROs are becoming increasingly important in the evaluation of cancer treatment modalities (8). PROs provide valuable insight into the patient experience and allow the measurement of preoperative and postoperative QOL (9). QOL is a critical outcome measure in lung cancer surgery and is of great significance, especially in treating patients with early-stage lung cancer (10). It has been reported that PRO-based active symptom monitoring intervention is feasible and demonstrates encouraging preliminary efficacy for reducing symptoms and the readmission risk (11), and more to the point, resulting in superior QOL (12).
Recent advances in clinical research show that acupuncture, as an effective, safe, and cost-effective treatment for cancer and cancer-related symptoms, may provide clinical benefits for oncology patients in symptom control and supportive care (13, 14). Acupuncture also alleviates side effects induced by chemotherapy or radiotherapy such as nausea and vomiting (15), cancer-related pain (16), fatigue (17), insomnia (18), and the QOL. Oncology acupuncture has become a new research field with great prospects (19). It is anticipated that as a growing number of evidence continues to emerge, oncology acupuncture will eventually be integrated into standard oncology practice (20).
Despite growing attention to acupuncture as an alternative medicine for lung cancer treatment, the evidence of its impact on the PROs of lung cancer patients is scanty (21). Moreover, there are no systematic reviews of acupuncture improving PROs in lung cancer patients. To fill this gap, we undertake systematic retrieval and analysis to summarize the existing evidence of acupuncture therapy in improving PROs among the lung cancer patients. Our study will provide more reliable evidence from the perspective of PROs and the implementation details of acupuncture therapies in the clinical practice of lung cancer, as well as contribute to optimizing a clinical acupuncture regimen and trial design in the future.
This study is performed according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines (22). The protocol of this study has been registered in International Prospective Register of Systematic Reviews (PROSPERO), and the registration number is CRD42021274122.
Electronic databases including PubMed, Embase, Cochrane Library, Web of science, CNKI, CQVIP, Wanfang Data, SinoMed, and gray literatures including ClinicalTrials.gov Database (www.clinicaltrials.gov), Chinese Clinical Trial Register (www.chictr.org.cn), and conference literatures were retrieved from inception to 1 July 2022. The language is limited to Chinese and English. In addition, the reference lists of eligible articles were also checked to identify additional studies. The searches were performed using the following mesh terms plus keywords, such as “acupuncture”, “lung cancer”, “PROs”, and “Randomized Controlled Trial”, including their synonyms. Supplementary Tables 1, 2 in the Supplementary Materials show the complete search strategy for English and Chinese databases above.
The eligible criteria included:
a. Adult patients (age ≥ 18 years) who were diagnosed with lung cancer through pathology with any tumor stage with no gender restrictions
b. Randomized controlled trials (RCTs) on acupuncture treatment among lung cancer patients with the outcomes of PROs
c. Acupuncture is a method to treat diseases by stimulating meridians and acupoints. It includes manual acupuncture, electroacupuncture (EA), moxibustion, transcutaneous electrical acupoint stimulation (TEAS), auriculotherapy, acupoint application, acupoint injection, fire needle, plum-blossom needle, and acupressure. Acupuncture used alone or in combination was defined as an experimental intervention.
d. The comparison groups included either treatment as follows: usual care, sham/placebo acupuncture, and pharmacotherapy including Western medicine (WM) and Chinese Traditional medicine (TCM).
The eligible criteria included:
a. Combined with other cancers
b. Quasi-randomized control trial, cohort studies, case–control studies, and articles that have not been peer-reviewed
c. The same acupuncture therapy was conducted in both groups.
It deserves to be mentioned that the acupuncture group has no restriction on the needle size, acupoint selection, stimulation frequency, retention time, and treatment course.
We divided the different PRO outcome indicators into two categories: QOL and patient-perceived symptoms. The primary outcome measures were QOL scales commonly used in the efficacy evaluation of lung cancer patients, such as the Karnofsky Performance Status (KPS) (23), European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C30) (24), Functional Assessment of Cancer Therapy-Lung (FACT-L) (25), Functional Assessment of Cancer Therapy Lung Cancer Subscale (FACT-LCS), Leicester Cough Questionnaire (LCQ score) (26), the MOS item short form health survey (SF-36) (27), and the St George’s Respiratory Questionnaire (SGRQ) (28).
Secondary outcomes were patient-perceived symptoms, including pain, nausea and vomiting, insomnia, fatigue, and constipation, as well as adverse events to be recorded. Pain intensity was measured by four measurement tools including the numerical rating scale (NRS) score (29), Visual Analog Scale (VAS) pain scales (30), pain score in EORTC QLQ-C30, and Brief Pain Inventory-Chinese Version (BPI-C) (31). Nausea and vomiting were measured by three measurement tools including the MASCC (Multinational Association of Supportive Care in Cancer) Antiemesis Tool (MAT) (32), Index of Nausea and Vomiting and Retching (INVR) (33), and nausea and vomiting score in EORTC QLQ-C30. Insomnia was measured by three measurement tools including the Pittsburgh Sleep Quality Index (PSQI) (34), Athens Insomnia Scale (AIS) (35), and sleep score in EORTC QLQ-C30. Fatigue was measured by the following four measurement tools: Revised Piper Fatigue Scale (PFS-R) (36), Brief Fatigue Inventory-Chinese Version (BFI-C) (37), and fatigue score in EORTC QLQ-C30. The secondary outcome anxiety and depression was measured by two measurement tools including the Self-Rating Anxiety Scale (SAS) (38) and Self-Rating Depression Scale (SDS) (39). Constipation was measured by following one measurement tool constipation score in EORTC QLQ-C30.
Two researchers (X.Q. W and Z.Q. X) independently extracted and managed data by Excel software (16.59, Microsoft excel for Mac). Any disagreement was resolved by discussion until a consensus was reached or by consulting a third researcher (K W). The data extraction elements included the authors, year, sex, age, stage, randomization, intervention details, main acupoint, course of treatment, results, follow-up, and outcomes. For RCTs with multiple time points to evaluate outcomes, the data at the end of treatment were extracted. The selection process was presented in a PRISMA flow diagram.
Methodological quality and reporting biases were evaluated by two reviewers independently. Cochrane Collaboration’ s tool was used to assess the risks of bias (40). We assessed from the following seven dimensions: random sequence generation, allocation concealment, the blinding of participants and patients, the blinding of outcome evaluators, incomplete outcome data, and selective reporting. Divergence would be conquered by the adjudication of the corresponding author.
Data were combined and analyzed with RevMan 5.4.1 (The Cochrane Collaboration) and Stata/SE 16.0. Dichotomous data were reported as the relative ratio (RR), whereas continuous data were reported as the mean difference (MD) or standardized mean difference (SMD), with 95% confidence interval (CI). The MD was used for PROs with the same measures; otherwise, the SMD was chosen. The fixed-effect model was employed when the study of heterogeneity (I2) was <50%; otherwise, a random-effect model was used. Sensitivity analysis was performed by excluding each RCT out sequentially to test the robustness of the result. Subgroup analysis was applied to explore the source of heterogeneity. Meta regression analysis was used to clarify the sources and value of heterogeneity and to further explain the influence of variables on the combined effect. A random-effect model was used for meta regression analysis. The funnel plot was conducted to detect publication bias.
A total of 499 trials were retrieved in the literature search. After a preliminary screening of the titles and abstracts of the articles, we used EndNoteX9 (X9.3.3, Thomson Reuters (Scientific) LLC Philadelphia, PA, USA) and manual checking to remove duplicate and non-standard studies and identified 96 studies from the database. We evaluated the full text of the 96 studies, and only 33 of them met our inclusion criteria. Figure 1 shows the process of the literature search and the screening process used in this study (22).
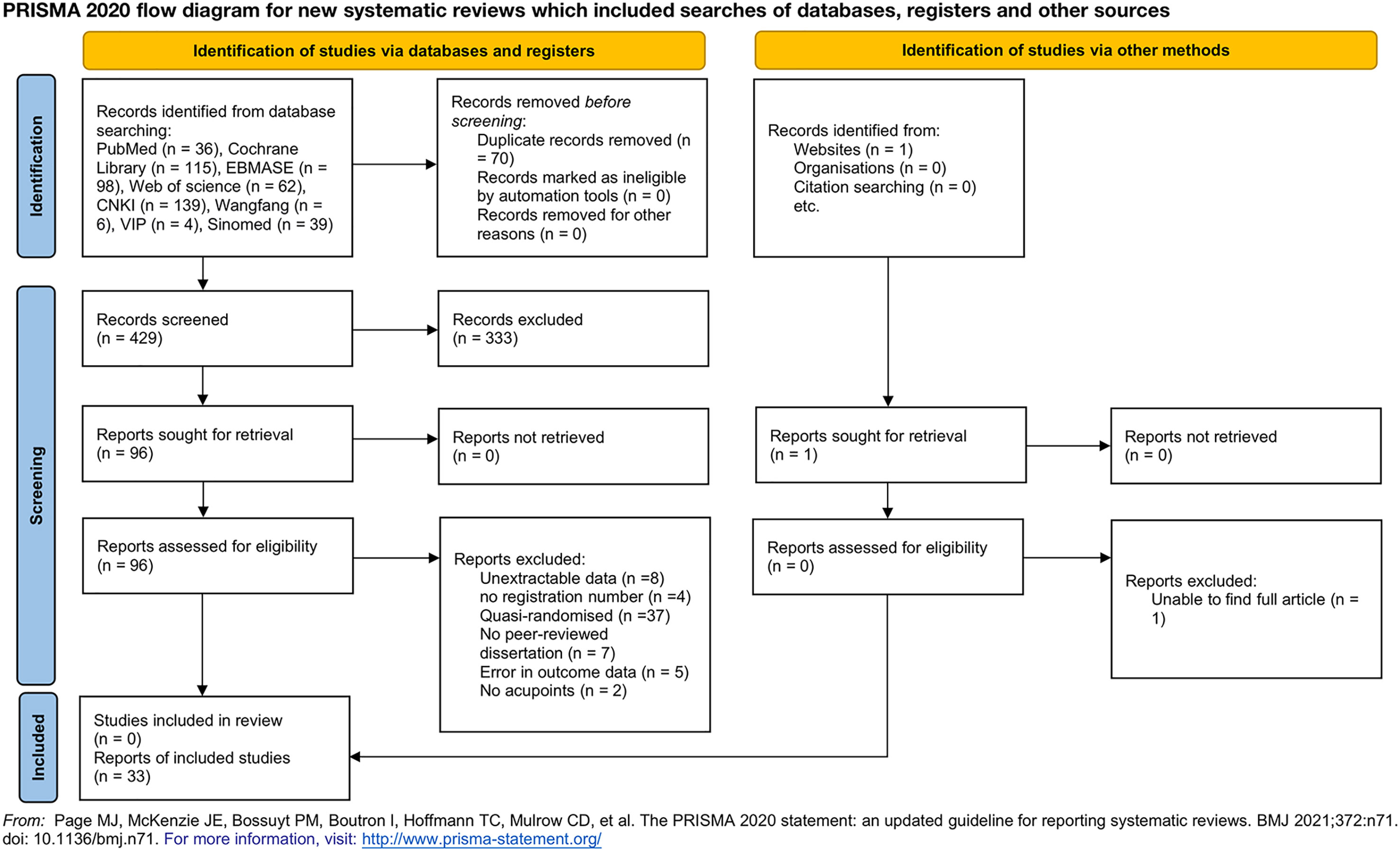
Figure 1 Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) 2020 flow diagram for new systematic reviews that included the searches of databases, registers, and other sources. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021;372:n71.doi:10.1136/bmj.n71. For more information, visit http://www.prisma-statement.org/.
Of all included 33 RCTs, 27 were published in Chinese and 6 were published in English. Seven trials used auricular acupoint (41–47), seven trials used acupoint application (45, 46, 48–52), six trials used manual acupuncture (41, 46, 53–56), four trials used moxibustion (43, 48, 57, 58), three trials used electroacupuncture (EA) (51, 59, 60), three trials used transcutaneous electrical acupoint stimulation (TEAS) (61–63), two trials used acupoint injection (49, 64), two trials used a fire needle (65, 66), two trials used acupressure (67, 68), and only one trial for each used plum-blossom needle tapping (69), low-frequency pulse (49), catgut-embedding therapy (70), thunder-fire moxibustion (71), thermal moxibustion (72), and Mongolian medicine warm acupuncture (73). All RCTs provided the details of the treatment acupoints. The auricular acupoint sessions ranged from 3 to 5 min. Plum-blossom needle tapping sessions ranged from 5 to 10 min. Acupressure sessions ranged from 10 to 18 min. Thunder⁃fire moxibustion sessions ranged from 20 to 30 min. Low-frequency pulse sessions ranged from 25 min. Moxibustion, EA, TEAS, manual acupuncture, and Mongolian medicine warm acupuncture sessions ranged from 30 min, and acupoint application sessions ranged from 4 to 6 h. Fire needle sessions were done three times at each point.
Twenty trials used Western medicine or traditional Chinese medicine (TCM) as a control intervention, 9 trials used usual care as a control intervention, and only 4 trials used sham or placebo acupuncture.
Nineteen trials covered the primary outcomes, 8 of which also included secondary outcomes. The remaining 14 trials only with secondary outcomes. The characteristics of the included studies and acupuncture details of included studies are shown in Supplementary Tables 3 and 4 in the Supplementary Materials.
All of the RCTs reported the generation of random sequences. Twenty-three trials used the random number table method, five trials used random number produced by computer, two trials used lottery, two trials used random number produced by SPSS (20.0 and 22.0) and the remaining one trial used regional random grouping method. The major sources of risk of bias correlated with allocation concealment, blinding of participants and personnel, and blinding of outcome assessment. twenty-nine trials were judged to have a high risk of bias with respect to the blinding of participants given that it was not possible to blind the acupuncturists and most patients in a study of acupuncture intervention. Other bias in two trials (67, 70) were identified as high risk because these two trials did not report baseline data for age comparison of patient in both control group and observation group. We judge that only two trials (60, 61) had a relatively low risk of bias. The individual risk of bias for each trial is presented in Figure 2.
Seventeen RCTs (41, 42, 45–50, 53, 54, 57, 58, 61, 64–66, 69) reported QOL scales, including KPS (42, 45–50, 53, 61, 64–66, 69), EORTC QLQ-C30 (41, 57), FACT-L (61, 65), FACT-LCS (54), SF-36 (58), LCQ (50), and SGRQ (68). Among these 17 trials, 7 trials used ST36; 4 trials used BL13, LI4, and TF4; 3 trials used PC6 and AH6a; and 2 trials used AT4. Higher scores were considered better in all PROs except SGRQ in which a higher score indicates a poorer QOL. In terms of the QOL measured by KPS, 11 of which used continuous variables and two original studies referred to the criteria of KPS and transformed it into a dichotomous variable. We combined these trials in two different ways: different tumor–node–metastasis (TNM) stage or different stage of disease. A study (74) has shown that KPS appeared to be a more reliable predictor of survival than the results of the QOL questionnaire. This again suggests that KPS is more informative when used to evaluate older and more impaired patients. It was found that the QOL of patients who received acupuncture-related treatment improved significantly compared with those who only received Western medicine treatment and usual care using continuous variables (MD 6.75, 95%CI, 5.82 to 7.68, P<0.00001, I2 = 0%) Two trials (46, 64) concluded that patients experienced a higher effect on QOL in the acupuncture-related group compared with those in the WM/TCM group using dichotomous variables (RR 1.24, 95%CI, 1.09 to 1.41, P=0.001 I2 = 0%). The pooled analysis results of the changes in the mean scores of each scale are listed in Tables 1 and 2.
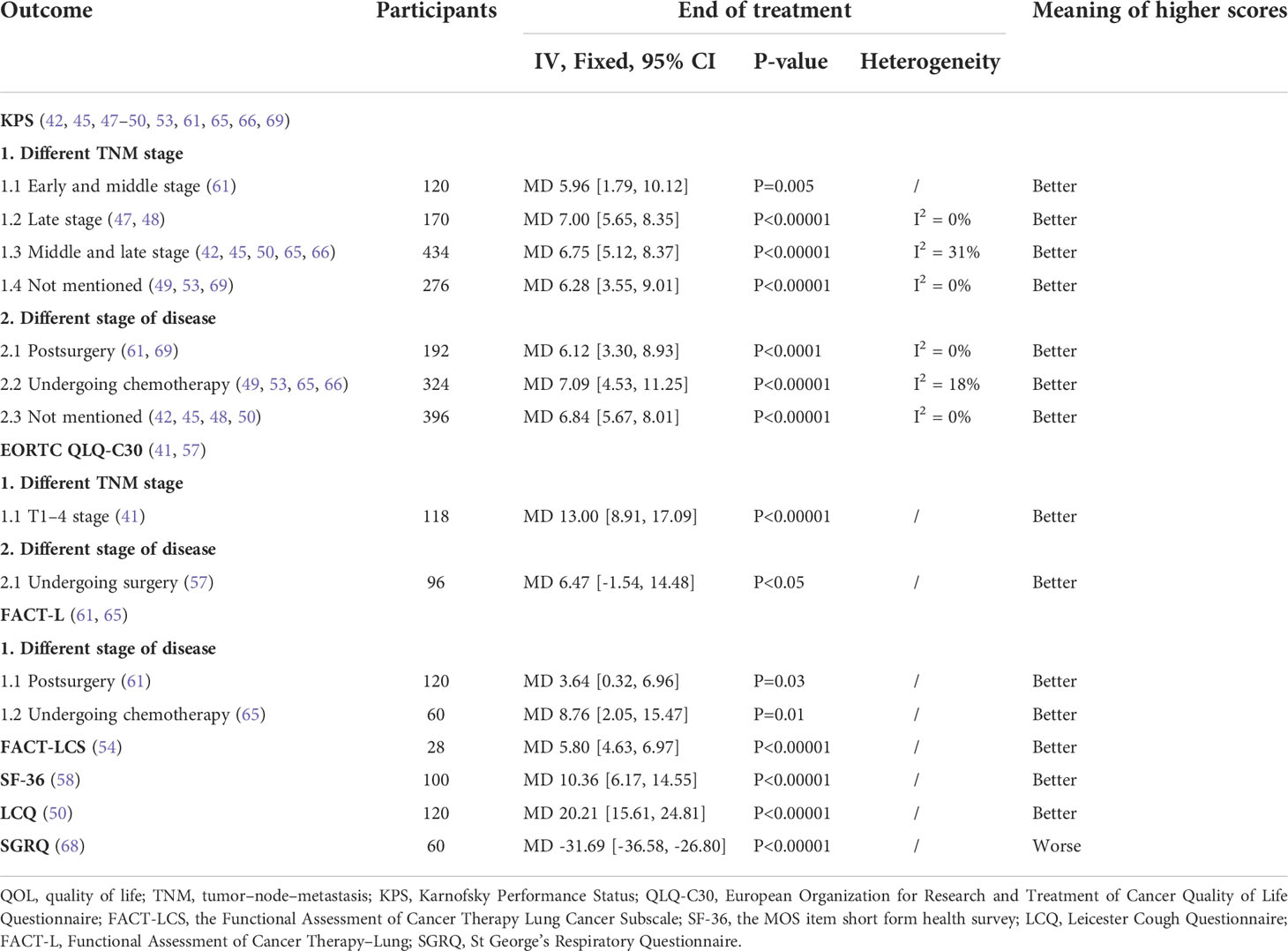
Table 1 The QOL of acupuncture with continuous variables versus comparators for lung cancer treatment–related symptoms.
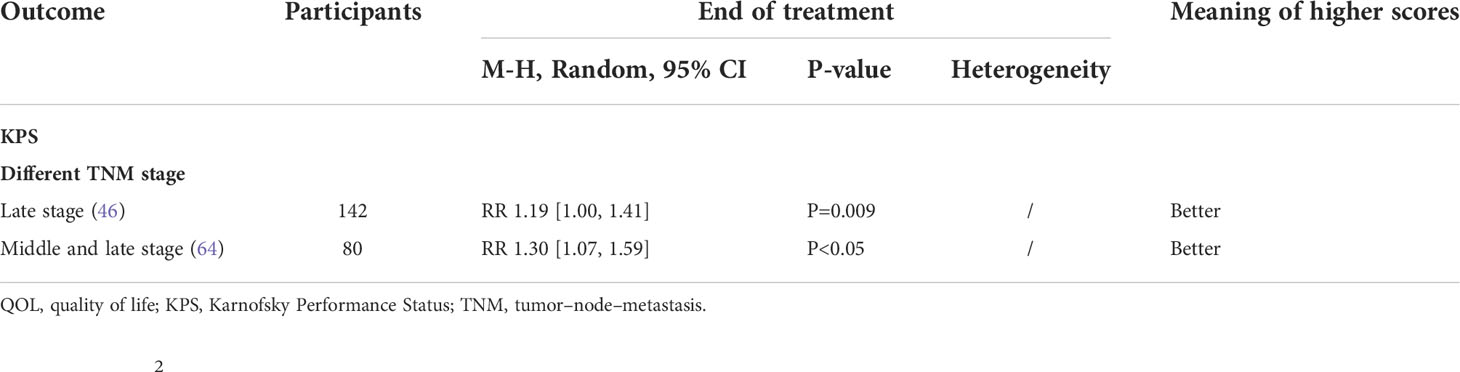
Table 2 The QOL of acupuncture with dichotomous variables versus comparators for lung cancer treatment–related symptoms.
Four RCTs (41, 51, 55, 57) reported on nausea and vomiting by patients and used three NA measures including the NV score in EORTC QLQ-C30 (41, 57), MAT (51) and INVR (55). Among these four trials, two trials used LI4 and ST36, one trial used TF4, AH6a, PC6, and AT4. Two (51, 55) of the trials were for nausea and vomiting after chemotherapy; one (57) was postoperative, and one (41) was not specified. Higher scores were considered worse in all these PROs. For NV measured by the NV score in EORTC QLQ-C30, Wang X et al. (41) and Wang LQ et al. (57) compared the NV scores of patients in the observation group after treatment with those in the control group; scores in the observation group were significantly lower than those in the control group for both postoperative and routine patients (MD -14.73, 95%CI, -23.88 to -5.59, P=0.002, I2 = 81%). In terms of INVR scores (55), there was no statistical difference between the POG and the control group on the first day of chemotherapy, but the prechemotherapy acupuncture group (PRG) differed significantly from the postchemotherapy acupuncture group (POG) and control group (P<0.05). On the second-to-seventh day of chemotherapy, the difference between the three groups was statistically significant (MD -1.18, 95%CI, -1.89 to -0.47, P=0.001).
One RCT (51) measured by MAT using dichotomous variables showed that the severity of acute vomiting in the observation group was significantly lower than that in the control group at the end of treatment (RR 0.59, 95%CI, 0.41 to 0.86, P=0.006) (Table 5).
Seven RCTs (41, 43, 44, 52, 59, 71, 73) reported on sleep disturbances by patients and used three sleep disturbance measures including the SL score in EORTC QLQ-C30 (41), PSQI (43, 52, 59, 71, 73), and AIS (44). Among these seven trials, three trials used TF4, AT4, and ST36; two trials used AH6a and LI4; and one trial used BL13. Three (43, 71, 73) of the trials were for sleep disturbances after chemotherapy, three (41, 52, 59) were cancer-related sleep disturbances, and one (44) was for radiotherapy. Higher scores were considered worse in this PRO. Five trials used PSQI to measure patients’ sleep quality, one of which (43) used four arms, so the results are not easy to be combined and will be analyzed separately. Guo et al. showed that there were statistically significant differences in the PSQI factor scores of the four groups, suggesting that the auricular acupoint combined with the moxibustion treatment group had the most obvious effect. The remaining four trials showed that the score of PSQI in the observation group was significantly lower than those in the control group and the total improvement rate of sleep quality was also superior to the patients in the control group for both chemotherapy-induced and cancer-related sleep disturbances (MD -3.73, 95%CI, -5.99 to -1.48, P=0.001, I2 = 97%) (Figure 4). For the SL score in EORTC QLQ-C30 (41), a comparison between groups after treatment showed that the SL scores in the observation group after acupuncture observation were lower than those in the control group (MD -14.16, 95%CI, -20.91 to -7.41, P<0.001). One RCT (44) using AIS showed that AIS scores in the observation group and the control group were not statistically significant (P>0.05) (MD -0.17, 95%CI, -1.93 to 1.59, P=0.85) (Table 5).
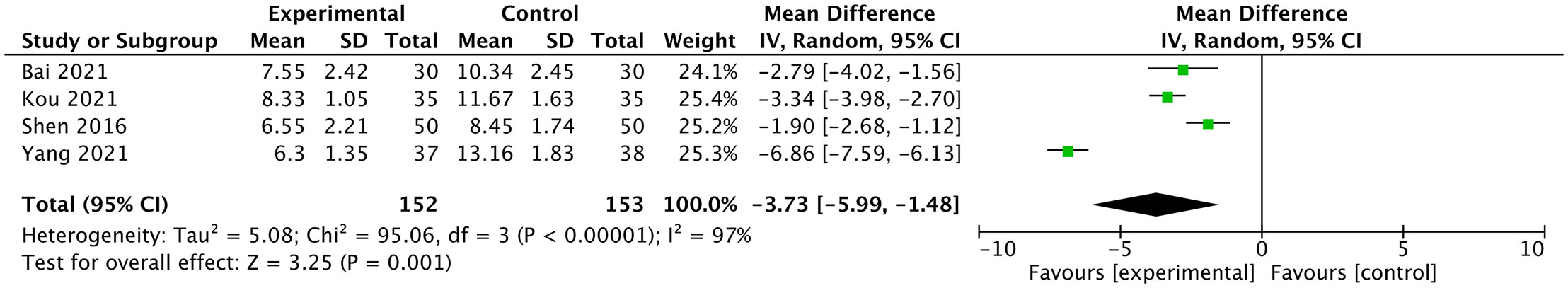
Figure 4 Forest plot of the sleep disturbances measured by Pittsburgh Sleep Quality Index in lung cancer patients treated with acupuncture and control.
Eight RCTs (41, 42, 54, 57, 63, 67, 71, 72) reported on fatigue by patients and used four fatigue measures including the FA score in EORTC QLQ-C30 (41, 57), PFS-R (42, 63, 71, 72), and BFI-C (54, 67). Among these eight trials, five trials used ST36; three trials used LI4; two trials used AT4, BL13, TF4 and AH6a; and one trial used PC6. Three (63, 67, 71) of the trials were for fatigue after chemotherapy and five (41, 42, 54, 57, 72) were cancer-related fatigue. Higher scores were considered worse in all these PROs. Four RCTs used PFS-R to measure fatigue, including two (63, 71) trials of chemotherapy-induced fatigue and two (42, 72) trials of cancer-related fatigue. After weeks of intervention, the PFS score of the two groups was significantly lower than those before the intervention, and the decrease in the observation group was more significant than that in the control group for both chemotherapy-induced and cancer-related fatigue (MD -1.18, 95%CI, -1.93 to -0.43, P<0.00001, I2 = 92%) (MD -0.94, 95%CI, -1.16 to -0.72, P = 0.34, I2 = 0%) (Figure 5).
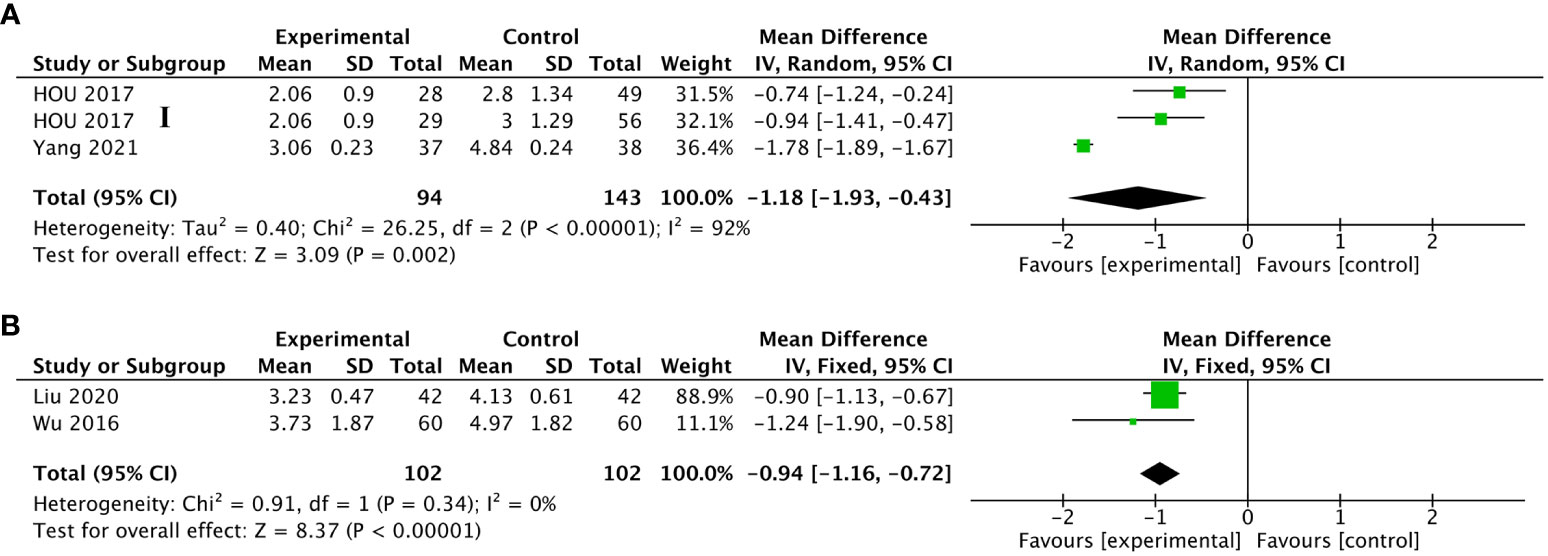
Figure 5 Forest plot of the fatigue in lung cancer patients treated with acupuncture and control. (A) The changes measured by the Revised Piper Fatigue Scale (PFS-R) in lung cancer patients undergoing chemotherapy treated with acupuncture-related intervention versus control from the baseline to the end of treatment; (B) the changes measured by PFS-R in lung cancer patients with cancer-related fatigue treated with acupuncture-related intervention versus control from the baseline to the end of treatment. IV, inverse variance; CI, confidence interval. The Roman numerals “I”, followed by the study ID, represented the comparison of acupuncture versus no intervention in the study that had three arms.
For FA measured by the FA score in EORTC QLQ-C30, Wang X et al. (41) and Wang LQ et al. (57) compared the FA scores of patients in the observation group after treatment with those in the control group; scores in the observation group were significantly lower than those in the control group (MD -12.81, 95%CI, -24.50 to -1.12, P=0.01, I2 = 84%). There were two trials measured by BFI-C using continuous variables and dichotomous variables, respectively. Cheng et al. (54) showed that patients who received active acupuncture had significantly lower BFI-C scores compared to those who received placebo (MD -1.40, 95%CI, -1.62 to -1.18, P<0.00001). Liu (67) showed that the degree of fatigue in the observation group was significantly lower than that of the control group (RR 0.84, 95%CI, 0.73 to 0.97, P=0.02) (Table 5).
Two RCTs (45, 59) reported on anxiety and depression by patients and used two AD measures including SAS (45, 59) and SDS (45, 59). Among these two trials, BL13, TF4, AH6a, LI4, and ST36 were all used only once. Higher scores were considered worse in all these PROs. Shen et al. and Zhang et al. showed that compared with the control group, both SAS scores in the observation group were lower than those in the control group after treatment (MD -4.74, 95%CI, -6.66 to -2.82, P=0.51, I2 = 0%) and so were SDS scores (MD -6.02, 95%CI, -8.11 to -3.94, P=0.58, I2 = 0%) (Figure 6).
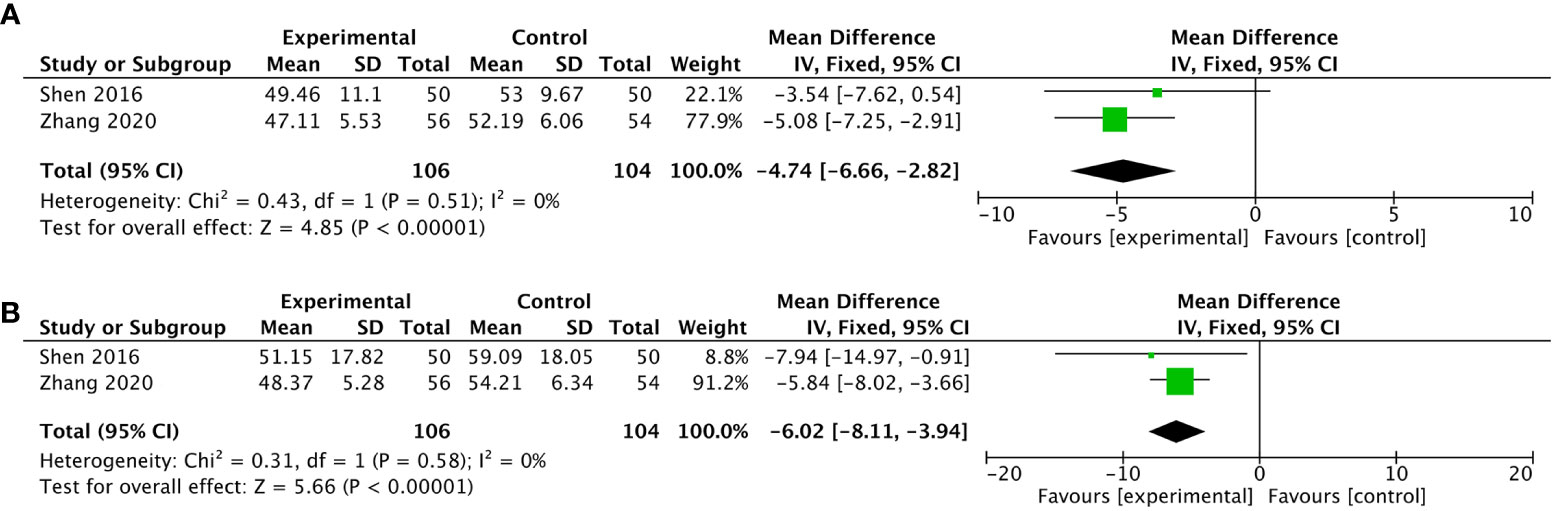
Figure 6 Forest plot of the fatigue in lung cancer patients treated with acupuncture and control. (A) the changes measured by the Self-Rating Anxiety Scale in lung cancer patients treated with acupuncture-related intervention versus control from the baseline to the end of treatment; (B) the changes measured by Self-Rating Depression Scale in lung cancer patients treated with acupuncture-related intervention versus control from the baseline to the end of treatment. IV, inverse variance; CI, confidence interval.
Only one RCT (41) reported on anxiety and depression by patients and used the CO score in EORTC QLQ-C30. This trial used acupoints including LI4, LR3, AT4, TF4, and AH6a. Higher scores were considered worse in all these PROs. Wang et al. showed that the CO score of patients in the study group after treatment was lower than that in the control group (Table 5).
Eight trials (42, 44, 46, 49, 50, 68, 70, 71) reported on side effects including dizziness, encephalalgia, fatigue, somnolence, gastrointestinal reaction, erythra, or respiratory depression. Three trials (46, 50, 71) reported no serious side effects in both groups. One trial (68) concluded that there were no serious side effects, but no data were available. Four trials reported that side effects in the observation group were lower than those in the control group and two (44, 70) of which had statistical significance (P<0.05), while the other two (42, 44) had no statistical significance (P>0.05). Since one patient could be associated with multiple side effects, and the author did not report in detail, the data were not convenient for statistics.
When we combined two secondary outcomes of pain, VAS and NRS, in the trials of cancer pain, the heterogeneity was up to 90%. Then, we compared the effects between subgroups according to the following methods: acupuncture technique, acupoint combination, frequency of treatment session, duration time, and TNM stage. The results are shown in Table 3.
On two EORTC QLQ-C30 measures of QOL (41, 57), patients receiving acupuncture-related treatment had remarkably higher mean scores than patients from the control group (MD 10.68, 95%CI, 4.56 to 16.81, P=0.0006, I2 = 51%). For the QOL measured by FACT-L, the TEAS and fire needle used by Sun Y et al. (61) and Pei WY et al. (65) worked better (MD 4.65, 95%CI, 1.67 to 7.63, P=0.002, I2 = 26%). For the QOL measured by FACT-LCS, a significant reduction in the FACT-LCS score was observed in the 14 participants who received active acupuncture compared with those receiving the placebo (MD 5.80, 95%CI, 4.63 to 6.97, P<0.00001). In terms of the QOL measured by LCQ, Ma HX et al. (50) concluded that the improvements in the LCQ score in the treatment group were better than the control group (MD 20.21, 95%CI, 15.61 to 24.81, P<0.00001). Based on the QOL measured by SF-36 (58), the scores of physiological function, physiological function, general health, social function, emotional intelligence, and mental health in the observation group were significantly higher than those in the control group (MD 10.36, 95%CI, 6.17 to 14.55, P<0.00001). For the QOL measured by SGRQ (68), the intervention group’s life quality scores significantly decreased (MD -31.58, 95%CI, -36.58 to -26.80, P<0.00001).
Eleven RCTs (41, 42, 45, 56–60, 62, 69, 70) reported on pain by patients, and used four pain measures including the NRS score (42, 56, 58, 59, 69, 70), VAS (45, 60, 62), and PA score in EORTC QLQ-C30 (41, 57) or BPI-R (41). Among these 11 trials, 6 trials used LI4, 4 trials used ST36, 3 trials used TF4 and AH6a, and 2 trials used BL13, PC6, and AT4. Higher scores were considered worse in all these PROs. We combined the data of two pain scales, VAS and NRS, and classified them according to different stages of the disease. We reached the conclusions that for patients of cancer pain (42, 45, 56, 59), compared with those receiving Western medicine treatment and usual care, patients receiving acupuncture-related treatment improved significantly (SMD -1.69, 95%CI, -2,49 to -0.90, P<0.0001, I2 = 90%). However, for patients of postoperative pain (60, 62, 69), the results showed no statistical significance (SMD -1.20, 95%CI, -2.26 to 0.22, P = 0.11, I2 = 92%). There were two trials (58, 70) measured by the NRS that used dichotomous variables with the patients of cancer pain, showing that the pain relief efficiency in the observation group was significantly higher than that of the control group (RR 0.50, 95%CI, 0.30 to 0.82, P=0.006, I2 = 0%) (Figure 3).
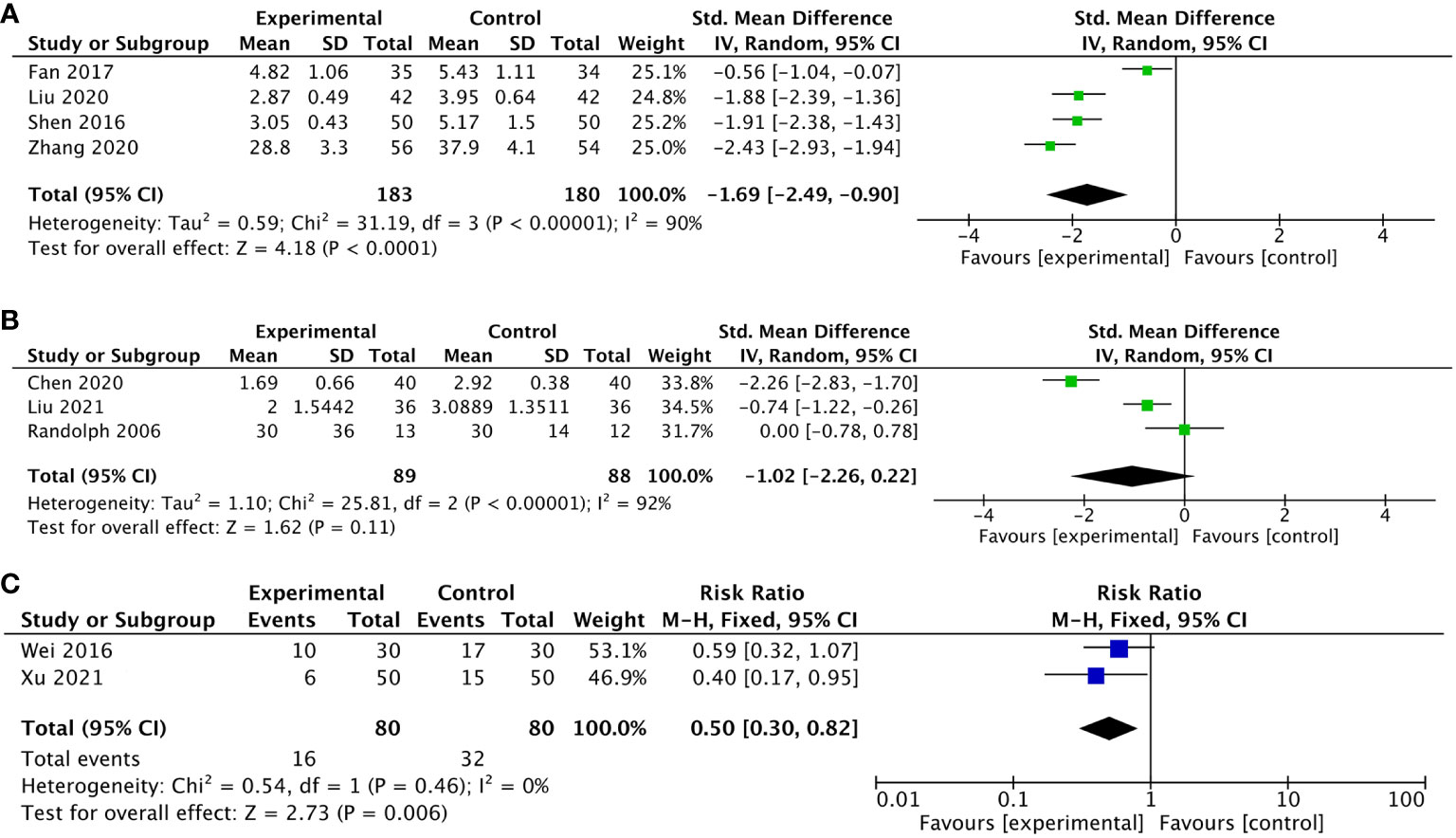
Figure 3 Forest plot of the pain in lung cancer patients treated with acupuncture and control. (A) The changes measured by the combination of the Numerical Rating Scale (NRS) score and Visual Analog Scale (VAS) pain scales in lung cancer patients with cancer pain treated with acupuncture-related intervention versus control from the baseline to the end of treatment; (B) the changes measured by the combination of NRS and VAS scores in lung cancer patients undergoing surgery treated with acupuncture-related intervention versus control from the baseline to the end of treatment; (C) the changes measured by the combination of the NRS score in lung cancer patients with cancer pain treated with acupuncture-related intervention versus control from the baseline to the end of treatment using dichotomous variables. IV, inverse variance; CI, confidence interval.
For pain measured by the PA score in EORTC QLQ-C30, Wang X et al. (41) and Wang LQ et al. (57) compared the PA scores of patients in the observation group after treatment with those in the control group, but the differences were not statistically significant in both two trials (P>0.05) (MD -3.90, 95%CI, -9.33 to 1.54, P=0.16, I2 = 58%). One RCT (41) using BPI-R showed that there was significant difference in the pain intensity between the observation group and the control group after treatment and between the observation group after treatment and before treatment (Table 5).
Subgroup analysis showed that studies with all types of the methods above had significant effect on alleviating cancer pain. In the analysis of acupuncture technique treatment, auricular acupoint treatment showed lower heterogeneity and increased effect size on reducing cancer pain (SMD -2.16, 95%CI, -2.70 to -1.62, P<0.00001, I2 = 57%). In the analysis of the TNM stage, treatments in the studies of late stage showed significant improvement in patients with lung cancer–related pain and lower heterogeneity (SMD -2.07, 95%CI, -2.43 to -1.72, P<0.00001, I2 = 34%). In the analysis of acupoint combination, studies showed a significant effect on cancer pain reduction but could not explain the heterogeneity (SMD -1.62, 95%CI, -2.37 to -0.51, P<0.00001, I2 = 93%). In the analysis of the frequency of treatment session, studies showed no statistical difference at reducing cancer pain (SMD -1.37, 95%CI, -2.38 to 0.11, P = 0.07, I2 = 95%). In the analysis of duration time, because of the different duration time of all four studies, heterogeneity could not be explained.
After further subgroup analysis, we found that Fan LY et al. (56) was the main source of heterogeneity. This trial was focused on the effect of manual acupuncture in improving patients with lung cancer–related pain at middle and late stage; therefore, the most difference between it and other trials lied in the different TNM stage. Additionally, we performed another subgroup analyses of all the outcomes based on the different control strategies used, and the results are shown in Tables 4 and 5.
In order to explore the stability of the results and the sources of heterogeneity in our meta-analysis, we pooled all studies for sensitivity analysis by excluding each study individually.
In terms of the cancer pain measured by the combination of VAS and NRS, there were significant changes in the outputs after excluding each study. After removing the study conducted by Fan LY et al. (56), the heterogeneity was significantly reduced and the result did not alter (SMD -2.07, 95%CI, -2.43 to -1.72, P<0.00001, I2 = 34%). In terms of the postoperative pain measured by the combination of VAS and NRS, the heterogeneity did not alter but the result changed to statistically significant after removing the study of Randolph et al. (60) (SMD -1.49, 95%CI, -2.98 to -0.01, P<0.05, I2 = 94%). After removing the study of Chen et al. (62), the heterogeneity decreased from 92% to 60% but with no statistical significance.
In terms of the sleep disturbances measured by PSQI, the heterogeneity decreased from 97% to 74% after removing the study of Yang H et al. (71).
In terms of the fatigue measured by PFS, after removing the study of Yang H et al. (71), the heterogeneity was significantly reduced to 0% and the result did not alter (MD -0.91, 95%CI, -1.10 to -0.73, P = 0.70, I2 = 0%).
We used meta regression analysis to clarify the sources and value of heterogeneity, and to further explain the influence of variables on the combined effect. We explored heterogeneity by taking acupuncture technique, course of treatment, frequency of treatment, year of publication, country of publication, duration time, TNM stage as variables. The results showed that the duration time in the sleep disturbances measured by PSQI was the main source of heterogeneity (p=0.017) and the other results showed that the variables were insignificant under meta regression (p>0.05). Supplementary Tables 5–8 in the Supplementary Material.
The funnel plot of 11 trials measured by KPS of the primary outcome QOL showed approximate symmetry (Figure 7). Because of the limited number of trials included for the remaining comparison measured by other PROs in the meta-analysis, funnel plots were not feasible. Therefore, we could not fully evaluate publication bias.
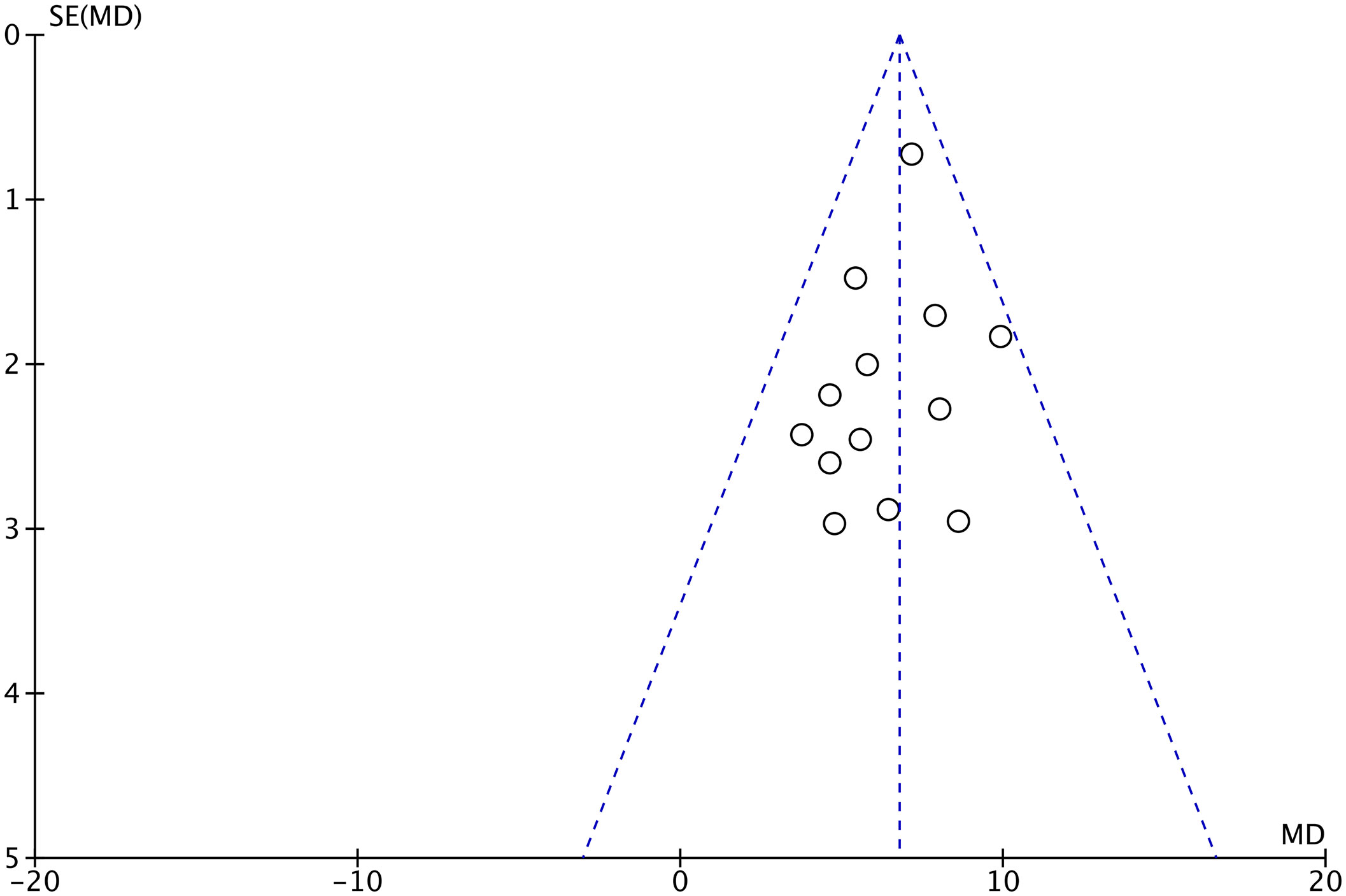
Figure 7 The funnel plot of quality of life measured by the Karnofsky Performance Status in lung cancer patients treated with acupuncture and control.
This study, including 33 RCTs, showed that acupuncture had a marked beneficial effect on improving PROs in different dimensions and different cancer stages or conditions. Compared with control groups such as usual care and pharmacotherapy, using acupuncture alone or in combination with other treatments can effectively relieve PROs, including postoperative chronic pain, and reduce anxiety and depression, so as to improve their QOL, which has a certain clinical application value.
Among 33 trials, 15 trials used ST36, and 7 trials used BL13, LI4, and PC6. One trial used only one acupoint (ST36) and five trials used two acupoints, showing significant efficacy in patients with lung cancer. It followed that ST36 can tonify qi and/or blood deficiency, increases stamina and energy, and it is the most important point to promote general wellness. Auricular acupoints were used in 7 of the 33 trials, among which TF4 was used in 6 trials, AT4 was used in 5 trials, and AH6a was used in 4 trials. It suggested that AT4 was a reference point for the diagnosis of nervous system diseases, tumors, insomnia, lethargy, and other diseases, which was of great importance for the diagnosis of malignant tumors (75). We also divided 33 trials into 4 different types to observe the commonness of acupoint selection. Of all five surgery-related trials, three used LI4 and two used ST36, SP6, and SP10. Of all 12 chemotherapy-related trials, 8 used ST36 and 4 used RN12 and PC6. One radiotherapy-related trial used auricular acupoints. The remaining trials were about lung cancer itself, and six of them used BL13 and five used LI4 and ST36. Thus, ST36 was useful in all types of trials except for the radiotherapy trials because of the selection of auricular acupoints. This study also provides a reference for the selection of effective acupoints for remedying various disorders in the PRO outcome of lung cancer patients, including the QOL, pain, nausea and vomiting, sleep disturbances, fatigue, anxiety and depression, constipation, and side effect. For example, sleep disturbance is a prominent concern in lung cancer patients, which is linked to worse prognosis and a poorer QOL (76, 77). In our study, the following acupoints were selected for sleep disorders in these trails: TF4, AT4, ST36, AH6a, LI4, BL13. However, one study found that the top 10 most frequently selected acupoints for sleep disorders were HT7, SP6, PC6, KI1, GV20, EM5, EX-HN3, EX-HN16, KI3, and MA-TF1 and also suggested that the acupoints of EX-HN3, EX-HN16, GV20 integrated with HT7, KI1, PC6 are the kernel acupoint combination in the field of acupuncture therapies for sleep disorders based on an association rule analysis (78). These acupoints are completely inconsistent with our findings. The selection of acupoints during treatment is one of the main factors affecting the efficacy of acupuncture treatment. Thus, according to the different dimensions of the QOL of lung cancer patients, optimizing and screening acupoints should be the focus of future studies.
Among 33 trials, only five trials involved follow-up, and the longest one lasted only a month. The sustained and long-term effect of acupuncture on the RPOs of patients with lung cancer is unknown since most included trials ranged in duration from 4 to 8 weeks.
Eight trials reported side effects but did not state in detail whether they were caused by acupuncture or chemotherapy. However, all the trials reported that the side effects of involved acupuncture groups were lower than those of the control group. This indicated that conventional Western medicine combined with acupuncture had the advantage of reducing toxicity and increasing effects in the treatment of lung cancer, reflecting the advantages of acupuncture in lung cancer such as safety, effectiveness, urgency, acceptability, and applicability.
Eighteen trials were about the treatment of chemotherapy-induced lung cancer-related symptoms by acupuncture, and five were about postoperative. It shows that acupuncture has more opportunities to be used in the above two situations, reflecting the advantages of acupuncture. The results showed that the scores with PROs of acupuncture on patients were also higher than that of the control group, indicating that acupuncture had a significant effect on both the QOL and other patients’ self-conscious symptoms. Acupuncture could improve the PRO of lung cancer patients at different TNM stages and under different treatments of disease.
Among the 33 included RCTs, the heterogeneity obtained by approximately half of the trials was low, which meant maybe unimportant (less than 40% according to the Cochrane Handbook for Systematic Reviews of Interventions), while obvious heterogeneity was shown in several results of meta. Among them, heterogeneity 58% and 81% was derived from two secondary outcomes in pain and insomnia. The reason for the high heterogeneity of these two groups of data after the combination was that we highly suspected the existence of problems in the original data from the same trial (57). Wang LQ et al. (57) stated in the study that two secondary outcomes QLQ-C30 NV and FA in the observation group were significantly decreased compared with the control group (P<0.05), but the data showed totally opposite results that the scores of the observation group were dramatically higher than the control group (higher scores were considered worse in these two PROs). Judging from the data, the quality of this study is debatable and should be removed. However, the primary outcome in this study was the QOL of patients with the QLQ-C30, so we chose to retain the data in this study.
Heterogeneity 90% and 92% came from the cancer pain and postoperative pain measured by the combination of VAS and NRS. After subgroup and sensitivity analysis, we found the heterogeneity based on Fan LY et al. (56) in the patients of cancer pain. This may be due to the different TNM stage of patients in this trial compared with others. However, among patients of postoperative pain, Randolph et al. (60) stated that there was a trend for lower average VAS pain scores from postoperative day 2 to day 6 in the EA group, but this did not reach statistical significance. This is most likely secondary to the error from the small sample size. When we removed the study of Chen et al., the heterogeneity decreased to 60%. The major difference between this group was that patients in this trial received TEAS for 30 min before anesthetic induction and continuous stimulation throughout the whole surgical procedure.
Heterogeneity 97% from PSQI was based on Yang H et al. (71) and Kou XW et al. (52). Heterogeneity 94% from PFS was based on the same trial, Yang H et al. (71). After meta regression, we found that the duration time in the sleep disturbances measured by PSQI was the main source of heterogeneity (p=0.017), and the heterogeneity decreased from 97% to 30% after removing these two studies. The remaining two trials (59, 73) had the same duration time of treatment due to their similar interventions, which was treated by warm acupuncture and EA. Therefore, the heterogeneity was lower compared with the other two trials using thunder-fire moxibustion and acupoint application, respectively. The male patients included in Yang H et al. (71) accounted for 81.3%, which was the four times the number of women. Moreover, the majority of patients are in the stage of I and II, which may lead to the better effect of treatment. The most significant difference was evidenced by the type of the intervention, which was the only one among the 33 included trials that used thunder-fire moxibustion as the observation group for treatment in lung cancer chemotherapy patients. A study showed that thunder-fire moxibustion has anti-inflammatory effects (79). Currently, the mechanism of cancer-related fatigue is the inflammatory hypothesis that has attracted the most attention of scholars (80). The authors suggested that thunder-fire moxibustion could relieve the fatigue symptom and improve the QOL of lung cancer patients.
We combined the trials of QOL in the different TNM stages or different stages of disease and in different comparators including WM/TCM, usual care, and placebo. The results showed that the heterogeneity was low and even no heterogeneity. After subgroup and sensitivity analysis, we found that heterogeneity varied within a small range, which did not influence the stability of results. We analyzed the possible reasons as follows: first, we strictly formulated the inclusion and exclusion criteria, so the included articles were of high homogeneity; second, this represented no statistical heterogeneity, which may exist in clinical and methodological heterogeneity; third, there were still individual differences in patients’ stages of disease.
First, for selection bias. 29 of the 33 RCTS included in this study did not mention allocation concealment. During the treatment, due to the particularity of acupuncture, it is obviously impractical and difficult to blind the experimenter as well as the patients. However, for efficacy assessors and statistical analysts, blinding can be performed to minimize possible detection bias, and no one except four studies took this factor into account. Furthermore, some PROs such as the QOL instruments are often used as non-primary outcomes in studies; authors often do not present detailed numerical or exact results (as mentioned above) or even only provide bar chart results without extracting specific numbers for statistics, which may lead to publication bias.
In this study, different acupuncture interventions were used as study objects for evaluation, and it was found that manual acupuncture, acupoint application, and auricular point were most frequently used in clinical practice. Acupoint application and the auricular point had good curative effects and, meanwhile, could be treated anytime and anywhere, which was worthy of clinical application and promotion.
The advantage of our study is that we only focused on PROs with lung cancer patients, while other studies used scales that were not PROs or not just PROs to assess the treating effects of lung cancer such as the index of immunomodulation. Compared with other studies of the same type, we not only paid attention to the change of QOL with lung cancer patients by acupuncture but also to the change of lung cancer–related symptoms, which made the results more comprehensive and effective.
In addition, some trials were of poor quality and were not reported according to the reporting specifications of CONSORT (81). For instance, the lack of follow-up of PROs and side effect reports of patients were not conducive to the judgment of the QOL of lung cancer patients. We believed that the long-term follow-up of patients to assess their subsequent PRO is clinically significant. We suggested that we should pay more attention to PROs clinically in order to judge the most real situation of the patient fully and comprehensively. Moreover, the lack of research reports on the qualifications of acupuncturists indicates a lack of attention to them. Randomized controlled trials have proven that acupuncturists with different qualifications have different therapeutic effects on acupuncture (82), so we suggest that studies at home and abroad should focus on relevant information reports.
Research on acupuncture for cancer pain has been proven. Acupuncture and/or acupressure were significantly associated with reduced pain in cancer patients compared with sham surgery controls, according to a study published in JAMA Oncology (83). In other words, acupuncture is effective in reducing cancer pain and the use of opioid painkillers. With the improvement of early screening technology and treatment of lung cancer, the survival rate of lung cancer patients will be improved, and the advantages of acupuncture in early lung cancer as well as in surgery, radiotherapy and chemotherapy, immunotherapy, and other situations will be increasingly obvious. Additionally, the synergistic optimization effect of acupuncture and targeted therapy needs further research in the future.
On this basis, the pursuit of the treatment concept of prolonging the life of lung cancer patients and constantly improving the QOL of patients with lung cancer has become the research direction of more and more researchers. In this study, we evaluated the evidence from published RCTs and found that acupuncture for lung cancer and its treatment-related symptoms has the advantages of high acceptability and safety, as well as good effects on PROs with lung cancer patients. Among the main outcome measures included in this study, the most frequently used scales were KPS, QLQ-C30, and FACT-L. We hope to popularize the PRO-scale clinical trials of acupuncture for LC in the future in order to focus on the effect of acupuncture in patients with lung cancer on their PROs, mainly in the aspect of QOL.
Considering that various designs and techniques of acupuncture were included in this study, there is a potential risk of heterogeneity in the results. A total of 15 different interventions were included in this study, including a combination of two or three acupuncture-related interventions or just one intervention. Different experimental interventions are different in the frequency and cycle of treatment. For the same interventions, there are slight differences in therapeutic efficacy due to different acupuncturists. Second, since a rigorous search and screening strategy was used to obtain available studies, the sample size of the included studies was not particularly large. Controversial academic dissertations that have not been peer-reviewed, as well as trials that have been found to reuse data during data extraction, were excluded, resulting in only 27 trials in Chinese and 6 trials in English. Due to the inclusion of trials, which were mostly published in Asia, there are bias and limited generalizability of the conclusions to some extent. Additionally, due to the limited sample size included and the low quality of the original study, Grading of Recommendations, Assessment, Development and Evaluations (GRADE) was not used to construct the system of evidence. Furthermore, considering that acupuncture may be applied to the various stages of lung cancer and situations, we did not restrict the inclusion of specific population conditions. The age of the population we included was concentrated around 50 years old and was not representative of all adults, especially the elderly, which was mainly limited by the age of the population in the original studies and the epidemiological characteristics of lung cancer.
Our study indicates that acupuncture therapies is a promising intervention in promoting PROs in lung cancer patients with all stages and regardless of postsurgery or postchemotherapy. Acupuncture should be recommended as a beneficial alternative strategy for lung cancer patients on clinic. High-quality, large-sample, multicenter original RCTs of acupuncture that focus on PROs are needed in the future.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
KW and JZ conceived and designed the study. KW, XW, and ZX searched the databases and screened the articles. ZX, XW, and ZY were involved in data extraction and the assessment of methodological quality. ZX and XW analyzed the data. All the authors contributed to the composition of the manuscript. All the authors have checked manuscripts and approved the publication of the study.
This study was supported by grants from the Project BEBPC-TCM (2019XZZX-ZJ0011); Shanghai Clinical Research Center for Acupuncture and Moxibustion Accelerating (20MC1920500); Clinical Key Specialty Construction Foundation of Shanghai (shslczdzk04701).
We thank all authors and participants in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.921151/full#supplementary-material
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2018) 68(6):394–424. doi: 10.3322/caac.21492
2. Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet (2018) 391(10125):1023–75. doi: 10.1016/s0140-6736(17)33326-3
3. World Health Organization. Lung cancer . Available at: https://gco.iarc.fr/today/data/factsheets/cancers/15-Lung-fact-sheet.pdf (Accessed January 6, 2022).
4. Thai AA, Solomon BJ, Sequist LV, Gainor JF, Heist RS. Lung Cancer. Lancet (2021) 398(10299):535–54. doi: 10.1016/s0140-6736(21)00312-3
5. Li WW, Lee TW, Lam SS, Ng CS, Sihoe AD, Wan IY, et al. Quality of life following lung cancer resection: Video-assisted thoracic surgery vs thoracotomy. Chest (2002) 122(2):584–9. doi: 10.1378/chest.122.2.584
6. Kenny PM, King MT, Viney RC, Boyer MJ, Pollicino CA, McLean JM, et al. Quality of life and survival in the 2 years after surgery for non small-cell lung cancer. J Clin Oncol (2008) 26(2):233–41. doi: 10.1200/jco.2006.07.7230
7. U.S. Department of Health and Human Services FDA Center for Drug Evaluation and Research, U.S. Department of Health and Human Services FDA Center for Biologics Evaluation and Research, U.S. Department of Health and Human Services FDA Center for Devices and Radiological Health. Guidance for industry: patient-reported outcome measures: Use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes (2006) 4:79. doi: 10.1186/1477-7525-4-79
8. Chen H, Louie AV, Boldt RG, Rodrigues GB, Palma DA, Senan S. Quality of life after stereotactic ablative radiotherapy for early-stage lung cancer: A systematic review. Clin Lung Cancer (2016) 17(5):e141–9. doi: 10.1016/j.cllc.2015.12.009
9. Khullar OV, Wei JW, Wagh K, Binongo JN, Pickens A, Sancheti MS, et al. Preoperative lung function is associated with patient-reported outcomes after lung cancer surgery. Ann Thorac Surg (2021) 112(2):415–22. doi: 10.1016/j.athoracsur.2020.09.016
10. Fernando HC, Landreneau RJ, Mandrekar SJ, Nichols FC, DiPetrillo TA, Meyers BF, et al. Analysis of longitudinal quality-of-life data in high-risk operable patients with lung cancer: Results from the ACOSOG Z4032 (Alliance) multicenter randomized trial. J Thorac Cardiovasc Surg (2015) 149(3):718–725; discussion 725-726. doi: 10.1016/j.jtcvs.2014.11.003
11. Nipp RD, El-Jawahri A, Ruddy M, Fuh C, Temel B, D'Arpino SM, et al. Pilot randomized trial of an electronic symptom monitoring intervention for hospitalized patients with cancer. Ann Oncol (2019) 30(2):274–80. doi: 10.1093/annonc/mdy488
12. Basch E, Deal AM, Kris MG, Scher HI, Hudis CA, Sabbatini P, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. J Clin Oncol (2016) 34(6):557–65. doi: 10.1200/jco.2015.63.0830
13. O'Regan D, Filshie J. Acupuncture and cancer. Auton Neurosci (2010) 157(1–2)::96–100. doi: 10.1016/j.autneu.2010.05.001
14. Fan AY, Miller DW, Bolash B, Bauer M, McDonald J, Faggert S, et al. Acupuncture's role in solving the opioid epidemic: Evidence, cost-effectiveness, and care availability for acupuncture as a primary, non-pharmacologic method for pain relief and management-white paper 2017. J Integr Med (2017) 15(6):411–25. doi: 10.1016/s2095-4964(17)60378-9
15. Shen J, Wenger N, Glaspy J, Hays RD, Albert PS, Choi C, et al. Electroacupuncture for control of myeloablative chemotherapy-induced emesis: A randomized controlled trial. Jama (2000) 284(21):2755–61. doi: 10.1001/jama.284.21.2755
16. Chiu HY, Hsieh YJ, Tsai PS. Systematic review and meta-analysis of acupuncture to reduce cancer-related pain. Eur J Cancer Care (Engl) (2017) 26(2). doi: 10.1111/ecc.12457
17. Zhang Y, Lin L, Li H, Hu Y, Tian L. Effects of acupuncture on cancer-related fatigue: A meta-analysis. Support Care Cancer (2018) 26(2):415–25. doi: 10.1007/s00520-017-3955-6
18. Ma Y, Hall DL, Ngo LH, Liu Q, Bain PA, Yeh GY. Efficacy of cognitive behavioral therapy for insomnia in breast cancer: A meta-analysis. Sleep Med Rev (2021) 55:101376. doi: 10.1016/j.smrv.2020.101376
19. Chien TJ, Liu CY, Hsu CH. Integrating acupuncture into cancer care. J Tradit Complement Med (2013) 3(4):234–9. doi: 10.4103/2225-4110.119733
20. Lu W, Dean-Clower E, Doherty-Gilman A, Rosenthal DS. The value of acupuncture in cancer care. Hematol Oncol Clin North Am (2008) 22(4):631–48. doi: 10.1016/j.hoc.2008.04.005
21. Liu XH, Chen RL, Liu JP. Assessment about domestic trials of acupuncture for cancer patients’ quality of life in the past five years. Beijing J Tradit Chin Med (2018) 37(10):954–8. doi: 10.16025/j.1674-1307.2018.10.012
22. Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. Bmj (2021) 372:n160. doi: 10.1136/bmj.n160
23. Schag CC, Heinrich RL, Ganz PA. Karnofsky performance status revisited: Reliability, validity, and guidelines. J Clin Oncol (1984) 2(2):187–93. doi: 10.1200/jco.1984.2.3.187
24. Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European organization for research and treatment of cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst (1993) 85(5):365–76. doi: 10.1093/jnci/85.5.365
25. Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The functional assessment of cancer therapy scale: Development and validation of the general measure. J Clin Oncol (1993) 11(3):570–9. doi: 10.1200/jco.1993.11.3.570
26. Ward N. The Leicester cough questionnaire. J Physiother (2016) 62(1):53. doi: 10.1016/j.jphys.2015.05.011
27. Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). i. conceptual framework and item selection. Med Care (1992) 30(6):473–83. doi: 10.1097/00005650-199206000-00002
28. Jones PW, Quirk FH, Baveystock CM. The St george's respiratory questionnaire. Respir Med (1991) 85 Suppl B:25–31; discussion 33-37. doi: 10.1016/s0954-6111(06)80166-6
29. Hjermstad MJ, Gibbins J, Haugen DF, Caraceni A, Loge JH, Kaasa S. Pain assessment tools in palliative care: an urgent need for consensus. Palliat Med (2008) 22(8):895–903. doi: 10.1177/0269216308095701
30. Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg (2009) 18(6):927–32. doi: 10.1016/j.jse.2009.03.021
31. Poquet N, Lin C. The brief pain inventory (BPI). J Physiother (2016) 62(1):52. doi: 10.1016/j.jphys.2015.07.001
32. Tan JY, Suen LK, Molassiotis A. Psychometric assessment of the Chinese version of the MASCC antiemesis tool (MAT) for measuring chemotherapy-induced nausea and vomiting. Support Care Cancer (2016) 24(9):3729–37. doi: 10.1007/s00520-016-3181-7
33. Moradian S, Shahidsales S, Ghavam Nasiri MR, Pilling M, Molassiotis A, Walshe C. Translation and psychometric assessment of the Persian version of the rhodes index of nausea, vomiting and retching (INVR) scale for the assessment of chemotherapy-induced nausea and vomiting. Eur J Cancer Care (Engl) (2014) 23(6):811–8. doi: 10.1111/ecc.12147
34. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res (1989) 28(2):193–213. doi: 10.1016/0165-1781(89)90047-4
35. Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia scale: Validation of an instrument based on ICD-10 criteria. J Psychosom Res (2000) 48(6):555–60. doi: 10.1016/s0022-3999(00)00095-7
36. Piper BF, Dibble SL, Dodd MJ, Weiss MC, Slaughter RE, Paul SM. The revised piper fatigue scale: Psychometric evaluation in women with breast cancer. Oncol Nurs Forum (1998) 25(4):677–84. Avaliable at: https://www.researchgate.net/publication/13685535
37. Mendoza TR, Wang XS, Cleeland CS, Morrissey M, Johnson BA, Wendt JK, et al. The rapid assessment of fatigue severity in cancer patients: Use of the brief fatigue inventory. Cancer (1999) 85(5):1186–96. doi: 10.1002/(sici)1097-0142(19990301)85:5<1186::aid-cncr24>3.0.co;2-n
38. Yue T, Li Q, Wang R, Liu Z, Guo M, Bai F, et al. Comparison of hospital anxiety and depression scale (HADS) and zung self-rating Anxiety/Depression scale (SAS/SDS) in evaluating anxiety and depression in patients with psoriatic arthritis. Dermatology (2020) 236(2):170–8. doi: 10.1159/000498848
39. Zung WW. A SELF-RATING DEPRESSION SCALE. Arch Gen Psychiatry (1965) 12:63–70. doi: 10.1001/archpsyc.1965.01720310065008
40. Higgins JPT T. J., Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition. Chichester (UK): John Wiley & Sons (2019).
41. Wang X. Effects of acupuncture combined with ear pressure on pain duration and quality of life of lung cancer patients. J Sichuan Tradit Chin Med (2020) 38(01):191–4.
42. Liu FY, Guan CH. Controlling effect of ear-buried seeds on cancer-related pain and fatigue in patients with advanced lung cancer. China Modern Doctor (2020) 58(34):129–32.
43. Guo X, Zhang XX, Zhang Y, Yue ZS. Effects of auricular acupoint massage combined with moxibustion on sleep disorders in patients with lung cancer after chemotherapy. Tianjin J Nurs (2019) 27(03):352–4. doi: 10.3969/j.issn.1006-9143.2019.03.035
44. Lu Y, Hou LL, Cao YH, Zhang Y. Application of ear buries bean in lung cancer patients with radiotherapy insomnia. Shanghai Nurs (2017) 17(01):41–4. doi: 10.3969/j.issn.1009-8399.2017.01.017
45. Zhang YL, Lu YX, Chen QQ. Effect of auricular acupoint pressing with beans combined with point application on quality of life in patients with advanced lung cancer. J N Chin Med (2020) 52(05):153–6. doi: 10.13457/j.cnki.jncm.2020.05.046
46. Ou W, Li YJ, Chen JL, Gao JD, Xiao HY. Survival analysis of TCM acupuncture in the treatment of advanced non-small cell lung cancer. J Clin Acupuncture Moxibustion (2016) 32(12):23–7. doi: 10.3969/j.issn.1005-0779.2016.12.008
47. Luo J, Pan JJ. Efficacy evaluation of auricular points plaster therapy combined with nutritional support for patients with anorexia associated with advanced lung cancer. China Modern Doctor (2022) 60(02):127–30.
48. Yu LT. Curative effect of Chinese herbal application combined with moxibustion for advanced lung cancer and pleural effusion and its nursing strategy. J N Chin Med (2020) 52(12):187–9. doi: 10.13457/j.cnki.jncm.2020.12.056
49. Yin YF. Clinical observation on treatment of vomiting caused by chemotherapy in patients with lung cancer treated by acupoint application and acupoint injection combined with low frequency pulse. Med Inf (2019) 32(23):82–85+92. doi: 10.3969/j.issn.1006-1959.2019.23.022
50. Ma HX, Tong LH. Therapeutic effect on cough and asthma in lung cancer at the middle and late stage lung qi deficiency treated with bufei decoction and acupoint application and the impacts on serum inflammatory factor. World J Integrated Tradit Western Med (2019) 14(07):978–82. doi: 10.13935/j.cnki.sjzx.190723
51. Zhou XQ, Jiang N, Guan QY. Therapeutic effect of acupoint application combined with electroacupuncture on nausea and vomiting in patients with lung cancer treated with cisplatin chemotherapy. Modern Nurse (2019) 26(07):93–5.
52. Kou XW, Song HT, Xue GW. Observation on the clinical effect of acupoint application on non-small cell lung cancer related insomnia. Reflexology Rehabil Med (2021) 2(13):43–5.
53. Wang YL, Li JX, Guo XQ, Fu RY, Guan XJ. Effect of acupuncture in different time on nausea and vomiting induced by chemotherapy of lung cancer. Chin Acupuncture Moxibustion (2019) 39(12):1269–73. doi: 10.13703/j.0255-2930.2019.12.004
54. Cheng CS, Chen LY, Ning ZY, Zhang CY, Chen H, Chen Z, et al. Acupuncture for cancer-related fatigue in lung cancer patients: A randomized, double blind, placebo-controlled pilot trial. Supportive Care Cancer (2017) 25(12):3807–14. doi: 10.1007/s00520-017-3812-7
55. Cheng P, Wang X. The effects of acupuncture at different intervention time points on nausea and vomiting caused by cisplatin chemotherapy in patients with lung cancer. Int J Clin Exp Med (2020) 13(10):7965–71. Avaliable at: https://e-century.us/files/ijcem/13/10/ijcem0112962.pdf.
56. Fan LY, Gao SL, Wang YQ, Qi ZP. Clinical observation of acupuncture combined with western medicine in treatment of advanced lung cancer pain. Med J Chin People’s Health (2017) 29(11):36–8. doi: 10.3969/j.issn.1672-0369.2017.11.017
57. Wang LQ, Zhang J. Influence of nutritional management combined with moxibustion on quality of life in patients with lung cancer after radical operation. China Modern Med (2017) 24(29):62–64+74. doi: 10.3969/j.issn.1674-4721.2017.29.021
58. Xu YL, Huang YS, Xu SH. Effect of moxibustion on bone metastasis pain of advanced lung cancer and correlation analysis of traditional Chinese medicine syndrome elements. J Sichuan Tradit Chin Med (2021) 39(02):176–9.
59. Shen LF, Chen WY, Lv XD, Liu JL, Yang XM, Yao M, et al. Study on the effect of electro acupuncture in improving sleep quality of patients with lung cancer -related pain. J Med Res (2016) 45(06):87–90. doi: 10.11969/j.issn.1673-548X.2016.06.022
60. Wong RHL, Lee TW, Sihoe ADL, Wan IYP, Ng CSH, Chan SKC, et al. Analgesic effect of electroacupuncture in postthoracotomy pain: A prospective randomized trial. Ann Thorac Surg (2006) 81(6):2031–6. doi: 10.1016/j.athoracsur.2005.12.064
61. Sun Y, Pang YH, Mao NQ, Luo JN, Cai DL, Chen FF. Effect of transcutaneous electrical acupoint stimulation on venous thrombosis after lung cancer surgery: A randomized controlled trial. Chin Acupuncture Moxibustion (2020) 40(12):1304–8. doi: 10.13703/j.0255-2930.20191204-k0007
62. Chen J, Zhang Y, Li X, Wan Y, Ji X, Wang W, et al. Efficacy of transcutaneous electrical acupoint stimulation combined with general anesthesia for sedation and postoperative analgesia in minimally invasive lung cancer surgery: A randomized, double-blind, placebo-controlled trial. Thorac Cancer (2020) 11(4):928–34. doi: 10.1111/1759-7714.13343
63. Hou L, Zhou C, Wu Y, Yu Y, Hu Y. Transcutaneous electrical acupoint stimulation (TEAS) relieved cancer-related fatigue in non-small cell lung cancer (NSCLC) patients after chemotherapy. J Thorac Dis (2017) 9(7):1959–66. doi: 10.21037/jtd.2017.06.05
64. Deng W, Yang LL, Zhang W. Clinical observation on acupoint injection of placenta polypeptide on chemotherapy in patients with advanced non-small cell lung cancer. Chin Medcine Modern Distance Educ China (2019) 17(04):69–72. doi: 10.3969/j.issn.1672-2779.2019.04.029
65. Pei WY, Lin SY, Zeng JC, Qian GF, Lin LZ, Lin GH. Effects of fire needle on quality of life in patients with chemotherapy of non-small cell lung cancer. Chin Acupuncture Moxibustion (2017) 37(11):1191–5. doi: 10.13703/j.0255-2930.2017.11.014
66. Li SC, Zhang Y, Lin LZ, Lin GH, Wang YH. Effect of fire needle Si-hua point on IL-6 and TNF-α in patients with advanced non-small cell lung cancer treated with chemotherapy. J N Chin Medcine (2014) 46(05):170–3. doi: 10.13457/j.cnki.jncm.2014.05.066
67. Liu XP. Effect of autonomous acupoint massage on cancer-induced fatigue in patients with lung cancer undergoing chemotherapy. World Chin Med (2016) 11:1244.
68. Dogan N, Tasci S. The effects of acupressure on quality of life and dyspnea in lung cancer: A randomized, controlled trial. Altern Therapies Health Med (2020) 26(1):49–56. >Available at: pubmed.ncbi.nlm.nih.gov/31221935
69. Liu CY, Zhao SL, Yang J, Wei Y, Sun T. Clinical observation on plum-blossom needle combined with oxycodone and acetaminophen in the treatment of chronic pain after lung cancer operation. Oncol Prog (2021) 19(06):570–4.
70. Wei YG, Zhou CP. Observation on the curative effect of acupoint embedding in the treatment of cancer pain of lung cancer. J Prev Med Chin People's Liberation Army (2016) 34(S1):297–8. doi: 10.13704/j.cnki.jyyx
71. Yang H, Lu HZ, Zhang MN, Li L, Ding LP, Yu JX. Effect of thunder⁃fire moxibustion on fatigue and sleep quality in lung cancer patients with qi⁃deficiency syndrome undergoing chemotherapy. Chin Nurs Res (2021) 35(05):892–6.
72. Wu HY, Guo HF, Xu T, Chen ML. Effect of heat sensitive moxibustion intervention on cancer-induced fatigue in patients with advanced lung cancer. J Clin Acupuncture Moxibustion (2016) 32(07):52–4.
73. Bai Y, Guo H, Wang XY, Wang B, Li YT. Clinical observation of Mongolian medicine sugemule-3 decoction combined with Mongolian medicine warm acupuncture in the treatment of sleep disturbance after chemotherapy for lung cancer. China's Naturopathy (2021) 29(24):32–4. doi: 10.19621/j.cnki.11-3555/r.2021.2412
74. Mackworth N, Fobair P, Prados MD. Quality of life self-reports from 200 brain tumor patients: Comparisons with karnofsky performance scores. J Neurooncol (1992) 14(3):243–53. doi: 10.1007/bf00172600
75. Huang LC. Auricular therapy. Beijing (China): Scientific and Technical Documentation Press (2006).
76. Chen D, Yin Z, Fang B. Measurements and status of sleep quality in patients with cancers. Support Care Cancer (2018) 26(2):405–14. doi: 10.1007/s00520-017-3927-x
77. Dean GE, Abu Sabbah E, Yingrengreung S, Ziegler P, Chen H, Steinbrenner LM, et al. Sleeping with the enemy: Sleep and quality of life in patients with lung cancer. Cancer Nurs (2015) 38(1):60–70. doi: 10.1097/NCC.0000000000000128
78. Lin CH, Lin YH, Tzeng IS, Kuo CY. An association rule analysis of the acupressure effect on sleep quality. Evid Based Complement Alternat Med (2021) 29. doi: 10.1155/2021/1399258
79. Feng QX, Miao CY, Chen P. Research progress of clinical application mechanism of thunder fire moxibustion. Zhejiang J Tradit Chin Med (2017) 52(7):544–5. doi: 10.13633/j.cnki.zjtcm.2017.07.053
80. Wang XS, Woodruff JF. Cancer-related and treatment-related fatigue. Gynecol Oncol (2015) 136(3):446–52. doi: 10.1016/j.ygyno.2014.10.013
81. CONSORT 2010 checklist of information to include when reporting a randomised trial . Available at: http://www.consort-statement.org.
82. Chai Q, Fei Y, Guo Z, Wang C, Liu Z, Liu J. Impact of acupuncturist expertise on clinical effectiveness for chemotherapy induced nausea and vomiting: A randomized controlled trial. Integr Med Res (2015) 4(1):19. doi: 10.1016/j.imr.2015.04.333
Keywords: acupuncture, lung cancer, PROs = patient-reported outcomes, systematic review, meta-analysis
Citation: Xi Z, Wei X, Ye Z, Wang K and Zhou J (2022) Acupuncture for adult lung cancer of patient-reported outcomes: A systematic review and meta-analysis. Front. Oncol. 12:921151. doi: 10.3389/fonc.2022.921151
Received: 15 April 2022; Accepted: 05 August 2022;
Published: 02 September 2022.
Edited by:
Shin Takayama, Tohoku University Hospital, JapanReviewed by:
Ling Zhao, Chengdu University of Traditional Chinese Medicine, ChinaCopyright © 2022 Xi, Wei, Ye, Wang and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ke Wang, d2FuZ2tlODQzMEAxNjMuY29t; Jia Zhou, cGR6aG91amlhQDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.