- 1Midwifery Department, Ministry of Health and Medical Education, Tehran, Iran
- 2Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran
- 3Department of Midwifery and Reproductive Health, Faculty of Nursing and Midwifery, Qom University of Medical Sciences, Qom, Iran
- 4Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran
- 5School of Nursing and Midwifery, Tabriz University of Medical Sciences, Tabriz, Iran
- 6Department of Midwifery and Reproductive Health, Mother and Child Care Research Center, School of Nursing and Midwifery, Hamadan University of Medical Sciences, Hamadan, Iran
- 7Nursing Care Research Center, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran
- 8Social Determinants of Health Research Center, Birjand University of Medical Sciences, Birjand, Iran
- 9Head of Midwifery Department at Ministry of Health and Medical Education, Tehran, Iran
- 10University Hospitals Schleswig-Holstein, Kiel School of Gynaecological Endoscopy, Kiel, Germany
Background: Female breast cancer (FBC) is the most common type of cancer and is associated with a considerable disease burden as well as significant mortality rates. The present study aimed to provide an update on the incidence, mortality, and burden of FBC in 2019, based on the Global Burden of Disease (GBD) Study.
Materials: The incidence, death rate, disability-adjusted life years (DALYs), years of life lost (YLLs), years lived with disability (YLDs), the age-standardized rates (ASR) of FBC in 204 countries, and a variety of classifications, were retrieved from the Global Burden of Disease Study. Data on tobacco use, alcohol consumption, and drug use were collected. The incidence, mortality, and burden of FBC were registered and compared between regions. Associations between age-standardized incidence rates and age-standardized mortality rates of FBC with smoking, drinking, and drug use were determined.
Results: The highest incidence of FBC was observed in countries with a high socioeconomic status such as those of the European continent. Despite the lower incidence of FBC in countries with a low socio-demographic index (SDI), mortality rates secondary to FBC are higher in these countries than in high-income countries. The highest age-standardized mortality rate has been reported in the Eastern Mediterranean Region (EMRO), followed by the African Region (AFRO). The highest age-standardized rates of DALY and YLL per 100,000 population in 2019 were observed in lower-income countries, while the highest ASR of YLD per 100,000 population was reported in high-income countries.
Conclusion: The present GBD-based study provides a comprehensive review of the incidence, mortality, and burden of FBC in 2019. The incidence of FBC is higher in regions with a higher socioeconomic status, whereas mortality rates and DALYs are higher in poorly developed regions. We suggest better screening measures and early detection programs for the latter regions.
Introduction
Female breast cancer (FBC) is one of the most commonly diagnosed cancer types, with an estimated 2.3 million new cases (11.7%), and 685,000 deaths in 2020 (1). The figures are expected to reach 4.4 million in 2070 (2).
Incidence and mortality rates for FBC vary between countries. The age-standardized incidence ranges from 112.3 per 100,000 population in Belgium to 35.8 per 100,000 population in Iran. The highest age-standardized mortality rate was registered in Fiji (41.0 per 100,000 population), and the lowest in South Korea (6.4 per 100,000 population) (3).
Population structure, lifestyle, genetic factors, the environment (4), smoking, and alcohol consumption have been implicated as risk factors or protective factors for cancer (5–7). However, some studies reported the absence of a significant association between smoking and breast cancer or revealed that moderate or high consumption of alcohol did not increase the risk of breast cancer (8).
Currently, the burden of non-communicable diseases is growing due to prolonged life expectancy and lifestyle changes (9). At the end of 2020, one study reported 7.8 million living women diagnosed with breast cancer in the past 5 years (10).
Awareness of the incidence of disease and its geographic distribution is essential for effective health planning (11). In fact, the successful prevention and control of cancer depend on evidence-based policies that take epidemiological settings and the distribution of associated risk factors into account. The purpose of the present study was to provide an update on the incidence, mortality, and burden of FBC throughout the world. This is the first study to present breast cancer data based on different classifications for better understanding and interpretation. The incorporation of a variety of classifications (socio-demographic index SDI, World Health Organization WHO regions, continents, World Bank regions, and Global Burden of Disease GBD regions) permitted a comprehensive interpretation of data. These epidemiological data could also be used to devise measures of cancer prevention and screening strategies in the future.
Materials and Methods
The aims of the present study were the following:
a. To determine the incidence, mortality, and burden of FBC;
b. To compare the incidence, mortality, and burden of FBC based on different classifications;
c. To determine associations between age-standardized incidence rates and age-standardized mortality rates of FBC with smoking, drinking, and drug use.
FBC was defined according to the International Classification of Diseases (ICD)-10 code as C50-C50.9, D05-D05.9, D24-D24.9, D48.6, and D49.3, as well as according to the ICD-9 code as 174–175.9, 217–217.8, 233.0, 238.3, 239.3, and 610–610.9 (12).
Data Sources
The incidence, mortality, and burden of FBC in 2019 were derived from the Global Health Data Exchange (GHDx) database for all countries in 2019, as this is the calendar year for which the most recent incidence and mortality figures are available. These data can be viewed at http://ghdx.healthdata.org. The incidence, deaths, disability-adjusted life years (DALYs), years of life lost (YLLs), years lived with disability (YLDs), and age-standardized rates of FBC were extracted from the online global burden of disease (GBD) data. The GBD has estimated epidemiological indicators of 369 diseases and injuries for both sexes in 204 countries and territories based on various divisions of countries. For an accurate interpretation, we extracted FBC data for 204 countries and for a variety of classifications based on the socio-demographic index (SDI), World Health Organization (WHO) regions, continents, World Bank regions, and GBD regions (13). The SDI is a summary measure that identifies the position of countries or geographic areas on a scale of development from 0 (lowest) to 100 (highest). The SDI is based on three factors: i) per capita income; ii) average years of schooling; and iii) total fertility rate (TFR) (14). The World Bank classifies economies for analytical purposes into four income groups: low, lower-middle, upper-middle, and high income. For this purpose, it employs gross national income (GNI) per capita in U.S. dollars, converted from the local currency based on the World Bank Atlas method. The latter is commonly used for smoothing exchange rate fluctuations (15).
The study was approved by the ethics committee of the Birjand University of Medical Sciences (ethics committee approval code IR.BUMS.REC.1400.316). As we used routinely collected anonymized electronic data, patient consent was not required. All procedures were performed in accordance with the relevant guidelines and regulations, and no personal information was disclosed or published.
Statistical Analysis
Data were expressed as values with a 95% confidence interval (CI). Incidence, deaths, DALYs, YLLs, YLDs, and age-standardized rates were expressed as numbers per 100,000 population. Selected indicators were described separately for the individual classifications. Using the SPSS software (version 16) and Pearson’s correlation coefficient, we determined correlations between smoking, alcohol, drug use, secondhand smoke, and age-standardized incidence rates. Furthermore, we determined correlations between smoking, alcohol, drug use, secondhand smoke, and age-standardized mortality rates. To eliminate the influence of different ages in the patient population and ensure the comparability of statistical indicators, we used age-standardized rates of breast cancer incidence, death, and DALY (per 100,000 population). Definitions of the terms used are available at https://www.healthdata.org/terms-defined and https://www.healthdata.org/gbd/. A P-value less than 0.05 was considered statistically significant.
Results
Global Incidence of FBC
A total of 1,977,212 (95% CI; 1807615-2145215) new cases of FBC were reported worldwide in 2019, with an age-standardized incidence rate (ASR) of 45.86 per 100,000 population. The highest ASR of FBC has been reported in countries with a high SDI, such as the European region (EURO) and the American region (AMRO) (78.70-79.22 per 100,000). The lowest ASR of FBC has been reported in less developed countries such as those of the African region (AFRO) (30.99 per 100,000) (Table 1).
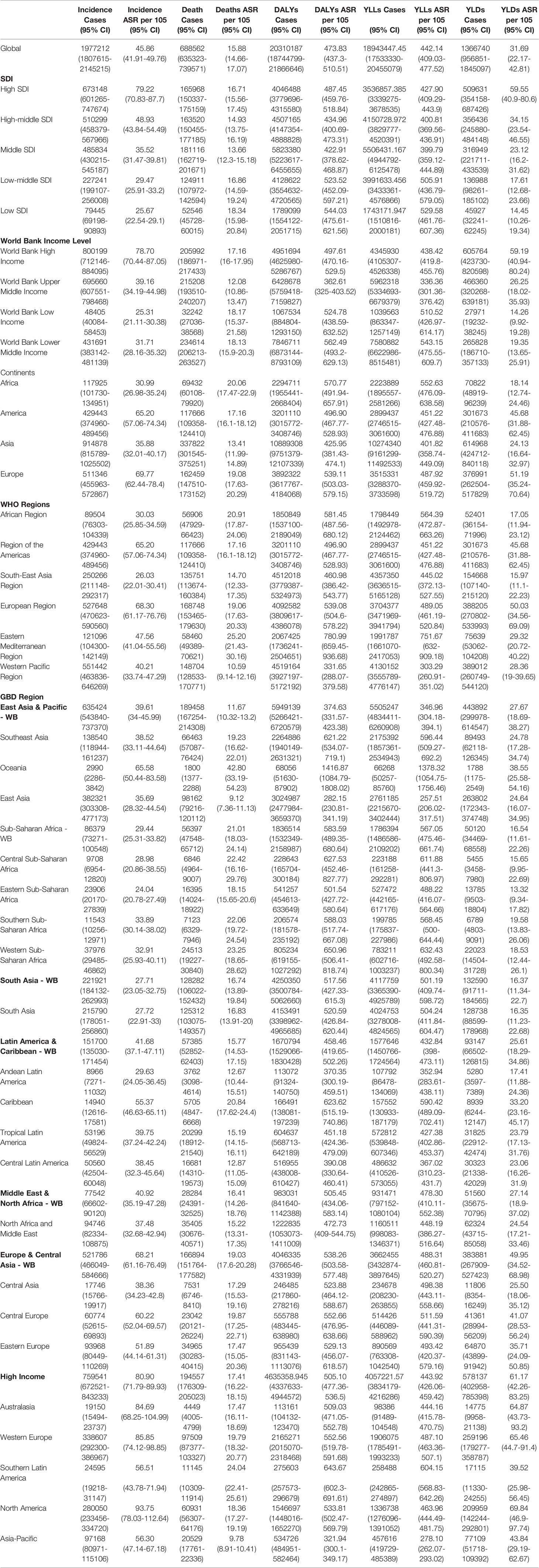
Table 1 Breast cancer incidence cases, age-standardized incidence rate, deaths, age-standardized mortality rates, DALYs, age-standardized DALY rates, YLLs, age-standardized YLLs rates, YLDs, and age-standardized YLDs rates in 2019.
Global FBC Mortality
In 2019, the number of deaths due to FBC worldwide were 688,562 (95% CI; 635,323-739,571), and the age-standardized mortality rate was 15.88 (95% CI; 14.66-17.07). Countries with a low SDI had the highest age-standardized mortality rate of 18.34, whereas countries with a high and middle SDI had age-standardized mortality rates of 16.71 and 13.66, respectively. Among the continents, the highest age-standardized mortality rate was reported in Africa and the lowest in Asia (Table 1).
Global Disability-Adjusted Life Years for FBC
In 2019, the number of DALYs due to FBC worldwide were 20,310,187 (95% CI 18,744,799-21,866,646), of which 18,943,447 were related to YLLs and 1,366,740 to YLDs.
The global ASR-DALY, ASR-YLLs, and ASR-YLDs due to FBC were 473.83, 442.14, and 31.69, respectively. The highest ASR of DALYs per 100,000 population in 2019 was noted in lower middle-income countries [562.49; 95% CI (493.2-629.13)], followed by low-income [524.78; 95% CI (438.59-632.52)] countries. The lowest ASR-DALYs were registered in countries with a middle SDI. The ASR of YLLs per 100,000 population was highest in Africa [552.63; 95% CI (476.09-638.58)] and lowest in Asia [425.95; 95% CI (381.43-474.1)]. However, with regard to the ASR of YLDs per 100,000 population, the highest rate was noted in high-income countries [59.19; 95% CI (40.94-80.24)], and the lowest in low-income countries [14.26; 95% CI (9.92-19.28)] (Table 1).
Correlation Between Global FBC Incidence, Mortality, and Smoking, Drinking, and Drug Use
The age-standardized incidence rates of FBC increased with the use of tobacco (r = 0.43, p < 0.001), smoking (r = 0.64, p < 0.001), alcohol (r = 0.48, p < 0.001), and drugs (r = 0.4, p < 0.001) (Figures 1A–D). No statistically significant correlation was registered between age-standardized incidence rates of FBC and secondhand smoke.
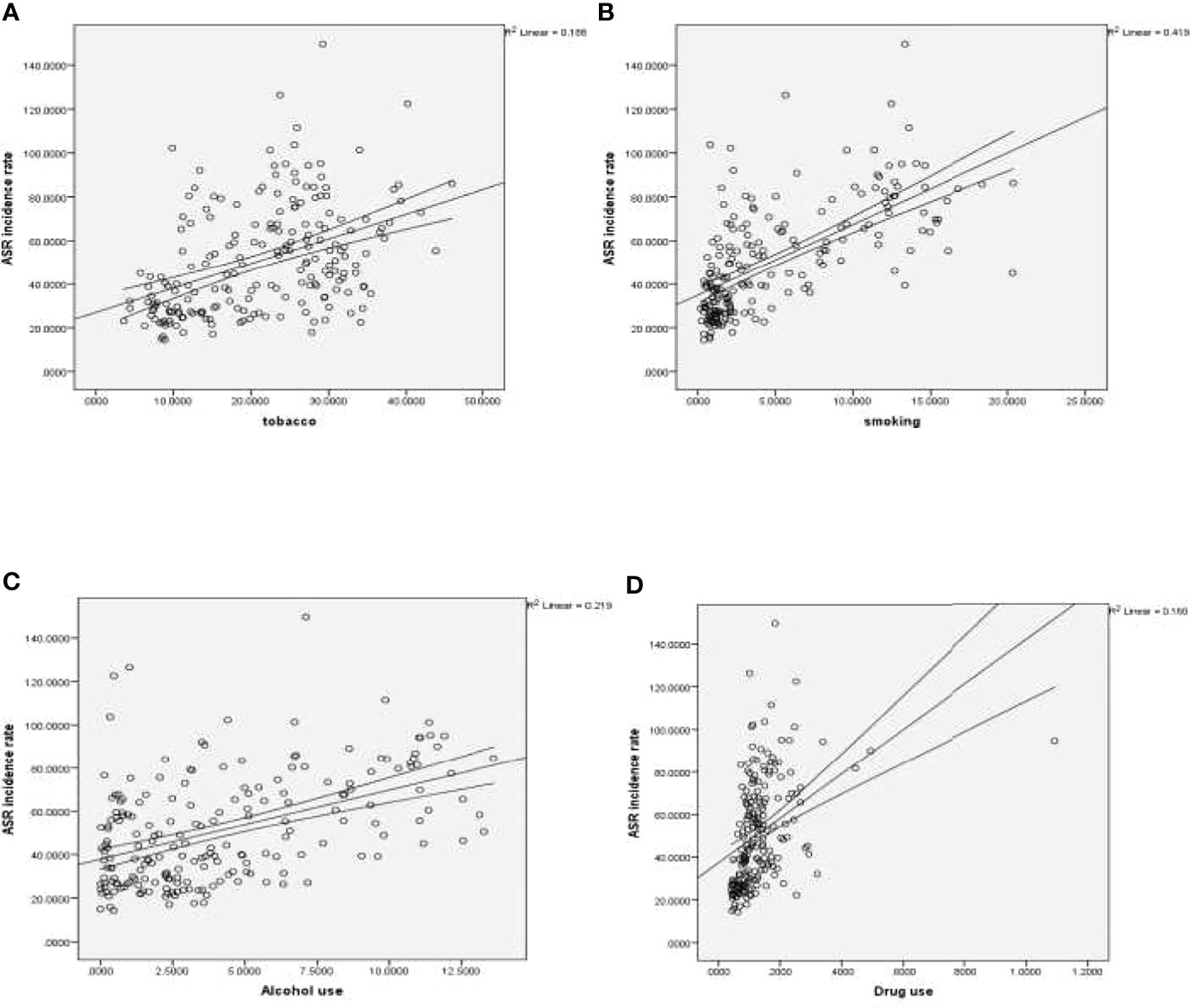
Figure 1 (A) Correlation between age-standardized incidence rate of FBC and tobacco. (B) Correlation between age-standardized incidence rate of FBC and smoking. (C) Correlation between age-standardized incidence rate of FBC and alcohol. (D) Correlation between age-standardized incidence rate of FBC and drug use.
The age-standardized mortality rate for FBC was significantly correlated with secondhand smoke (r = 0.156, p = 0.25).
Discussion
The significance of FBC is evidenced by its high incidence and mortality rates. In most countries, FBC is among the leading causes of death (16). We addressed the incidence, mortality rates, and disease burden of FBC based on a variety of classifications, as well as the association between the disease and smoking, drinking, and drug use in 2019. The present study revealed the highest incidence of FBC in countries with a high socioeconomic status such as the EURO. The higher incidence of FBC in regions with a higher socioeconomic status may be at least partly attributed to drastic changes in lifestyle and the built environment, which have influenced risk factors for breast cancer such as obesity, alcohol consumption (17), urbanization, sedentary behavior (18, 19), postponement of childbearing, lower overall fertility rates, lower breastfeeding rates (1, 20–22), and the use of hormone replacement therapy (23). Another important risk factor that might explain the difference is early detection rates and screening measures in countries with a higher socioeconomic status (20, 24). Screening investigations disclose cancer in earlier asymptomatic stages and identify cases that would not have been diagnosed otherwise. Another reason for the high incidence of breast cancer in countries with a higher socioeconomic status may be the availability of, and actual access to, treatment (21). Furthermore, the burden of cancer in countries with a lower socioeconomic status may be underestimated because these countries frequently lack reliable cancer registries and reporting systems (25). The systems of reporting epidemiological data in regions with a higher socioeconomic status are generally more robust (24, 26, 27). In view of these reporting biases (28), data concerning the incidence of cancer across regions should be interpreted with caution.
The present investigation revealed lower incidence rates of FBC in the EMRO and AFRO regions, yet higher mortality rates secondary to FBC in these regions than in countries with a higher incidence of the disease. The higher mortality rates secondary to FBC in regions with a lower socioeconomic status may be largely attributed to limited resources and the absence of well-organized health policies, leading to inadequate diagnosis, late-stage presentation, and untimely and inappropriate treatment (29–32). These reasons were confirmed in a study which reported that more than half of women with breast cancer in the Middle East are diagnosed in the third and fourth stages of the disease with lymph node involvement (33). In countries with a high socioeconomic status, on the other hand, very few women are diagnosed in the third and fourth stages of the disease (34). The fact that 69% of patients diagnosed with advanced stages die within five years after treatment (32) might explain the high mortality rates in the EMRO and AFRO regions. One of the important factors contributing to poor health in the EMRO is war, which causes large numbers of displaced persons, disruption of care structures and supplies, lack of qualified healthcare personnel, and financial restraints on patients and healthcare systems in countries with a large influx of refugees (35, 36).
While the traditional cancer metrics of incidence and mortality are crucial, DALY estimates provide a view of the healthy years of life lost due to cancer morbidity and mortality on a global basis (37). In the present study, the highest ASR of DALYs per 100,000 population was observed in the EMRO and AFRO regions, but the highest ASR of YLDs per 100,000 population was registered in Europe followed by the United States, while the lowest rate was noted in Africa. The high rates of YLDs in higher SDI settings is consistent with improved survival (38), as well as wider access to cancer screening (39, 40), diagnosis (41, 42), and treatment (43, 44) with increasing SDI. The highest ASR of YLLs were noted in low SDI regions.
The incidence and mortality rates of cancer are growing rapidly worldwide, reflecting aging, population growth, and changes in the prevalence and distribution of the principal risk factors for cancer. Many of these risk factors are associated with socioeconomic development (45). Taken together, these data emphasize the need for intensified efforts to prevent and control cancer (46), as well as the need to accelerate progress in lower SDI areas and thus reduce the impact of the growing burden (47, 48). One important step in this regard is educating women in all countries about early detection and treatment. Tailored integration of cancer into health planning may serve to reduce the global burden of the disease and eliminate the current inequities between transitioning and transitioned countries.
Strengths and Limitations
This GBD-based study is an update of the incidence patterns, mortality, DALYs associated with FBC worldwide, and the most relevant risk factors. The limitations of the present analysis are worthy of mention. First, it is based on GBD 2019 and thus shares the overall limitations described in previous publications (49, 50), including the challenges of quantifying all sources of uncertainty, lags in data availability, variations in coding practices, and other biases. Second, the paucity of reliable cancer registries and reporting systems in countries with a low SDI may have influenced the interpretation of data. Third, the investigation did not encompass a comparative assessment of other risk factors. Data concerning other risk factors were not available in the online dataset. For the above-mentioned reasons, the current data should be interpreted with caution.
Conclusion
This GBD-based 2019 study provides a comprehensive summary of the incidence, mortality, and burden of breast cancer, which is one of the most common types of cancer in the world. Despite the higher incidence of the disease in regions with a higher socioeconomic status, mortality rates and DALYs secondary to breast cancer are higher in poorly developed regions. The reasons for this phenomenon are poor accessibility to novel drugs and the limited application of clinical guidelines in the latter regions. Steps should be taken to reduce the burden of breast cancer, especially in lower SDI countries, and halt the acceleration of disparities. Patients in underdeveloped countries are affected to a greater extent by the burden of the disease. The information reported in this study illustrates the global disease burden of breast cancer and may be used to guide the allocation of healthcare resources for the prevention, screening, and treatment of the disease.
Data Availability Statement
The data presented in this study are available on request from corresponding author.
Author Contributions
LA, HS, and IA designed and conceived the study. AM and HS collected the data. LA, AM, HS, and IA analyzed and interpreted the data. LA, AM, ZM, AR, SH, MGH, and FB, drafted manuscript. HS and IA provided administrative, technical, or material support. LA and IA provided oversight. All authors contributed to the article and approved the submitted version.
Acknowledgments
We acknowledge financial support by DFG within the funding program Open Access Publikationskosten.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: Cancer J Clin (2021) 71(3):209–49. doi: 10.3322/caac.21660
2. Soerjomataram I, Bray F. Planning for Tomorrow: Global Cancer Incidence and the Role of Prevention 2020-2070. Nat Rev Clin Oncol (2021) 18(10):663–72. doi: 10.1038/s41571-021-00514-z
3. Lei S, Zheng R, Zhang S, Wang S, Chen R, Sun K, et al. Global Patterns of Breast Cancer Incidence and Mortality: A Population-Based Cancer Registry Data Analysis From 2000 to 2020. Cancer Commun (London England) (2021) 41(11):1183–94. doi: 10.1002/cac2.12207
4. Momenimovahed Z, Salehiniya H. Epidemiological Characteristics of and Risk Factors for Breast Cancer in the World. Breast Cancer (Dove Med Press) (2019) 11:151–64. doi: 10.2147/BCTT.S176070
5. Luo J, Margolis KL, Wactawski-Wende J, Horn K, Messina C, Stefanick ML, et al. Association of Active and Passive Smoking With Risk of Breast Cancer Among Postmenopausal Women: A Prospective Cohort Study. BMJ (2011) 342:d1016. doi: 10.1136/bmj.d1016
6. Viswanath K, Herbst RS, Land SR, Leischow SJ, Shields PG. Tobacco and Cancer: An American Association for Cancer Research Policy Statement. Cancer Res (2010) 70(9):3419–30. doi: 10.1158/0008-5472.CAN-10-1087
7. Land SR, Liu Q, Wickerham DL, Costantino JP, Ganz PA. Cigarette Smoking, Physical Activity, and Alcohol Consumption as Predictors of Cancer Incidence Among Women at High Risk of Breast Cancer in the NSABP P-1 Trial. Cancer Epidemiol Biomarkers Prev (2014) 23(5):823–32. doi: 10.1158/1055-9965.EPI-13-1105-T
8. Roddam AW, Pirie K, Pike MC, Chilvers C, Crossley B, Hermon C, et al. Active and Passive Smoking and the Risk of Breast Cancer in Women Aged 36–45 Years: A Population Based Case–Control Study in the UK. Br J Cancer (2007) 97(3):434–9. doi: 10.1038/sj.bjc.6603859
9. Kassa M, Grace J. The Global Burden and Perspectives on non-Communicable Diseases (NCDs) and the Prevention, Data Availability and Systems Approach of NCDs in Low-Resource Countries. In: Anugwom EE, Awofeso N. Public Health in Developing Countries-Challenges and Opportunities - Challenges and Opportunities. (London:IntechOpen) (2019). doi: 10.5772/intechopen.89516
10. WHO. Breast Cancer (2021). Available at: https://www.who.int/news-room/fact-sheets/detail/breast-cancer#:~:text=In%202020%2C%20there%20were%202.3,the%20world’s%20most%20prevalent%20cancer.
11. Almasi Z, Rafiemanesh H, Salehiniya H. Epidemiology Characteristics and Trends of Incidence and Morphology of Stomach Cancer in Iran. Asian Pacific J Cancer Prev (2015) 16(7):2757–61. doi: 10.7314/APJCP.2015.16.7.2757
12. Yin X, Zhang T, Zhang Y, Man J, Yang X, Lu M. The Global, Regional, and National Disease Burden of Breast Cancer Attributable to Low Physical Activity From 1990 to 2019: An Analysis of the Global Burden of Disease Study 2019. Int J Behav Nutr Phys Activity (2022) 19(1):42. doi: 10.1186/s12966-022-01283-3
13. Collaborators GA. Global, Regional, and National Burden of Diseases and Injuries for Adults 70 Years and Older: Systematic Analysis for the Global Burden of Disease 2019 Study. BMJ (2022) 376:e068208. doi: 10.1136/bmj-2021-068208
14. Go DS, Kim YE, Yoon SJ. Subnational Burden of Disease According to the Sociodemographic Index in South Korea. Int J Environ Res Public Health (2020) 17(16):5788. doi: 10.3390/ijerph17165788
15. Bank TW. The World by Income and Region (2021). Available at: https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html.
16. Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, MacIntyre MF, et al. The Global Burden of Cancer 2013. JAMA Oncol (2015) 1(4):505–27. doi: 10.1001/jamaoncol.2015.0735
17. Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early Breast Cancer: ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up†. Ann Oncol (2019) 30(8):1194–220. doi: 10.1093/annonc/mdz173
18. Kumar S, Preetha G. Health Promotion: An Effective Tool for Global Health. Indian J Community Med (2012) 37(1):5–12. doi: 10.4103/0970-0218.94009
19. Mahdavifar N, Pakzad R, Ghoncheh M, Pakzad I, Moudi A, Salehiniya H. Spatial Analysis of Breast Cancer Incidence in Iran. Asian Pacific J Cancer Prevention: APJCP (2016) 17(S3):59–64. doi: 10.7314/APJCP.2016.17.S3.59
20. Ghoncheh M, Pournamdar Z, Salehiniya H. Incidence and Mortality and Epidemiology of Breast Cancer in the World. Asian Pacific J Cancer Prevention: APJCP (2016) 17(S3):43–6. doi: 10.7314/APJCP.2016.17.S3.43
21. Dafni U, Tsourti Z, Alatsathianos I. Breast Cancer Statistics in the European Union: Incidence and Survival Across European Countries. Breast Care (2019) 14(6):344–53. doi: 10.1159/000503219
22. McCormack VA, Boffetta P. Today’s Lifestyles, Tomorrow’s Cancers: Trends in Lifestyle Risk Factors for Cancer in Low- and Middle-Income Countries. Ann Oncol (2011) 22(11):2349–57. doi: 10.1093/annonc/mdq763
23. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global Cancer Statistics, 2012. CA: Cancer J Clin (2015) 65(2):87–108. doi: 10.3322/caac.21262
24. Ghoncheh M, Mohammadian M, Mohammadian-Hafshejani A, Salehiniya H. The Incidence and Mortality of Colorectal Cancer and Its Relationship With the Human Development Index in Asia. Ann Global Health (2016) 82(5):726–37. doi: 10.1016/j.aogh.2016.10.004
25. Siddiqui AH, Zafar SN. Global Availability of Cancer Registry Data. J Global Oncol (2018) 4:1–3. doi: 10.1200/JGO.18.00116
26. Razi S, Enayatrad M, Mohammadian-Hafshejani A, Salehiniya H, Fathali-Loy-Dizaji M, Soltani S. The Epidemiology of Skin Cancer and its Trend in Iran. Int J Prev Med (2015) 6. doi: 10.4103/2008-7802.161074
27. Arabsalmani M, Mohammadian-Hafshejani A, Ghoncheh M, Hadadian F, Towhidi F, Vafaee K, et al. Incidence and Mortality of Kidney Cancers, and Human Development Index in Asia; a Matter of Concern. J Nephropathol (2017) 6(1):30–42. doi: 10.15171/jnp.2017.06
28. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer Incidence and Mortality Worldwide: Sources, Methods and Major Patterns in GLOBOCAN 2012. Int J Cancer (2015) 136(5):E359–86. doi: 10.1002/ijc.29210
29. Farmer P, Frenk J, Knaul FM, Shulman LN, Alleyne G, Armstrong L, et al. Expansion of Cancer Care and Control in Countries of Low and Middle Income: A Call to Action. Lancet (London England) (2010) 376(9747):1186–93. doi: 10.1016/S0140-6736(10)61152-X
30. GBD 2015 Eastern Mediterranean Region Cancer Collaborators. Burden of Cancer in the Eastern Mediterranean Region, 2005-2015: Findings From the Global Burden of Disease 2015 Study. Int J Public Health (2018) 63(Suppl 1):151–64. doi: 10.1007/s00038-017-0999-9
31. Figueiredo F, Almeida T, Cardial DT, Maciel É DS, Fonseca FLA, Adami F. The Role of Health Policy in the Burden of Breast Cancer in Brazil. BMC Women’s Health (2017) 17(1):121. doi: 10.1186/s12905-017-0477-9
32. Downing A, Prakash K, Gilthorpe M, Mikeljevic J, Forman D. Socioeconomic Background in Relation to Stage at Diagnosis, Treatment and Survival in Women With Breast Cancer. Br J Cancer (2007) 96(5):836–40. doi: 10.1038/sj.bjc.6603622
33. Bhikoo R, Srinivasa S, Yu T-C, Moss D, Hill AG. Systematic Review of Breast Cancer Biology in Developing Countries (Part 1): Africa, the Middle East, Eastern Europe, Mexico, the Caribbean and South America. Cancers (2011) 3(2):2358–81. doi: 10.3390/cancers3022358
34. Munzone E. Highlights From the Ninth European Breast Cancer Conference, Glasgow, 19–21 March 2014. Ecancermedicalscience (2014) 8:426. doi: 10.3332/ecancer.2014.426"10.3332/ecancer.2014.426
35. Spiegel P, Khalifa A, Mateen FJ. Cancer in Refugees in Jordan and Syria Between 2009 and 2012: Challenges and the Way Forward in Humanitarian Emergencies. Lancet Oncol (2014) 15(7):e290–7. doi: 10.1016/S1470-2045(14)70067-1
36. Sahloul E, Salem R, Alrez W, Alkarim T, Sukari A, Maziak W, et al. Cancer Care at Times of Crisis and War: The Syrian Example. J Global Oncol (2017) 3(4):338–45. doi: 10.1200/JGO.2016.006189
37. Collaboration GBoDC. Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA Oncol (2022) 8(3):420–44. doi: 10.1001/jamaoncol.2021.6987
38. Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, et al. Global Surveillance of Trends in Cancer Survival 2000-14 (CONCORD-3): Analysis of Individual Records for 37 513 025 Patients Diagnosed With One of 18 Cancers From 322 Population-Based Registries in 71 Countries. Lancet (2018) 391(10125):1023–75. doi: 10.1016/S0140-6736(17)33326-3
39. Sankaranarayanan R. Screening for Cancer in Low- and Middle-Income Countries. Ann Global Health (2014) 80(5):412–7. doi: 10.1016/j.aogh.2014.09.014
40. Shah SC, Kayamba V, Peek RM Jr., Heimburger D. Cancer Control in Low- and Middle-Income Countries: Is It Time to Consider Screening? J Global Oncol (2019) 5:1–8. doi: 10.1200/JGO.18.00200
41. Brand NR, Qu LG, Chao A, Ilbawi AM. Delays and Barriers to Cancer Care in Low- and Middle-Income Countries: A Systematic Review. Oncol (2019) 24(12):e1371–e80. doi: 10.1634/theoncologist.2019-0057
42. Hricak H, Abdel-Wahab M, Atun R, Lette MM, Paez D, Brink JA, et al. Medical Imaging and Nuclear Medicine: A Lancet Oncology Commission. Lancet Oncol (2021) 22(4):e136–e72. doi: 10.1016/S1470-2045(20)30751-8
43. Cortes J, Perez-García JM, Llombart-Cussac A, Curigliano G, El Saghir NS, Cardoso F, et al. Enhancing Global Access to Cancer Medicines. CA Cancer J Clin (2020) 70(2):105–24. doi: 10.3322/caac.21597
44. Martei YM, Iwamoto K, Barr RD, Wiernkowski JT, Robertson J. Shortages and Price Variability of Essential Cytotoxic Medicines for Treating Children With Cancers. BMJ Global Health (2020) 5(11):e003282. doi: 10.1136/bmjgh-2020-003282
45. Lin L, Yan L, Liu Y, Yuan F, Li H, Ni J. Incidence and Death in 29 Cancer Groups in 2017 and Trend Analysis From 1990 to 2017 From the Global Burden of Disease Study. J Hematol Oncol (2019) 12(1):96. doi: 10.1186/s13045-019-0783-9
46. Franceschi S, Wild CP. Meeting the Global Demands of Epidemiologic Transition - the Indispensable Role of Cancer Prevention. Mol Oncol (2013) 7(1):1–13. doi: 10.1016/j.molonc.2012.10.010
47. Foreman KJ, Marquez N, Dolgert A, Fukutaki K, Fullman N, McGaughey M, et al. Forecasting Life Expectancy, Years of Life Lost, and All-Cause and Cause-Specific Mortality for 250 Causes of Death: Reference and Alternative Scenarios for 2016-40 for 195 Countries and Territories. Lancet (2018) 392(10159):2052–90. doi: 10.1016/S0140-6736(18)31694-5
48. Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global Cancer Transitions According to the Human Development Index (2008-2030): A Population-Based Study. Lancet Oncol (2012) 13(8):790–801. doi: 10.1016/S1470-2045(12)70211-5
49. Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. The Lancet (2020) 396(10258):1204–22. doi: 10.1016/S0140-6736(20)30925-9
50. Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, et al.Global Burden of 87 Risk Factors in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. The Lancet (2020) 396(10258):1223–49. doi: 10.1016/S0140-6736(20)30752-2
Keywords: global, incidence, mortality, burden, breast cancer, smoking, drinking, drug use
Citation: Allahqoli L, Mazidimoradi A, Momenimovahed Z, Rahmani A, Hakimi S, Tiznobaik A, Gharacheh M, Salehiniya H, Babaey F and Alkatout I (2022) The Global Incidence, Mortality, and Burden of Breast Cancer in 2019: Correlation With Smoking, Drinking, and Drug Use. Front. Oncol. 12:921015. doi: 10.3389/fonc.2022.921015
Received: 15 April 2022; Accepted: 07 June 2022;
Published: 27 July 2022.
Edited by:
Hussain Gadelkarim Ahmed, University of Khartoum, SudanReviewed by:
Abdelbaset Mohamed Elasbali, Jouf University College of Applied Medical Science Qurayyat, Saudi ArabiaAhmed Abdalla Agab Eldour, Kordofan University, South Sudan
Copyright © 2022 Allahqoli, Mazidimoradi, Momenimovahed, Rahmani, Hakimi, Tiznobaik, Gharacheh, Salehiniya, Babaey and Alkatout. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ibrahim Alkatout, SWJyYWhpbS5BbGthdG91dEB1a3NoLmRl
 Leila Allahqoli
Leila Allahqoli Afrooz Mazidimoradi
Afrooz Mazidimoradi Zohre Momenimovahed
Zohre Momenimovahed Azam Rahmani4
Azam Rahmani4 Hamid Salehiniya
Hamid Salehiniya