- 1Department of Anesthesiology, Shanghai Chest Hospital, Shanghai Jiaotong University, Shanghai, China
- 2Department of Thoracic Surgery, Shanghai Chest Hospital, Shanghai Jiaotong University, Shanghai, China
Background: There are few studies on the impact of body position on variations in circulation and breathing, and it has not been confirmed whether body position changes can reduce the pulmonary complications of thoracoscopic-assisted oesophagectomy.
Methods: A single-center retrospective study included patients undergoing thoracoscopic-assisted oesophagectomy in the prone position or semiprone position between 1 July 2020, and 30 June 2021, at the Shanghai Chest Hospital. There were 103 patients with thoracoscopic-assisted oesophagectomy in the final analysis, including 43 patients undergoing thoracoscopic-assisted oesophagectomy in the prone position. Postoperative pulmonary complication (PPC) incidence was the primary endpoint. The incidence of cardiovascular and other complications was the secondary endpoint. Chest tube duration, patient-controlled anaesthesia (PCA) pressing frequency within 24 h, ICU stay, and the postoperative hospital length of stay (LOS) were also collected.
Results: Compared with the semiprone position, the prone position decreased the incidence of atelectasis (12% vs. 30%, P = 0.032). Nevertheless, there were no considerable differences in the rates of cardiovascular and other complications, ICU stay, or LOS (P >0.05). Multivariable logistic regression analysis showed that the prone position (OR = 0.196, P = 0.011), no smoking (OR = 0.103, P <0.001), preoperative DLCO% ≥90% (OR = 0.230, P = 0.003), and an operative time <180 min (OR = 0.268, P = 0.006) were associated with less atelectasis.
Conclusions: Our study shows that artificial pneumothorax under right bronchial occlusion one-lung ventilation for patients with thoracoscopic-assisted oesophagectomy in the prone position can decrease postoperative atelectasis compared with the semiprone position.
1 Introduction
Oesophagectomy with thoracoscopic assistance is a lengthy and traumatising procedure. Postoperative pulmonary complications (PPCs) are the most common serious complications after this type of surgery. PPCs are major causes of morbidity or mortality, prolonged hospital stays and added resource use (1–3). An extensive patient, anaesthetic, and surgical elements are related to PPCs (4).
Some studies have indicated that the prone position decreases postoperative respiratory complications (5, 6) with technical merit. This approach has many advantages, including good oxygen saturation (7).The prone position for patients having oesophageal cancer was found to be secure and effective. Additionally, the prone position might be a less invasive manoeuvre than the semiprone position (8–12).
It is suggested that artificial pneumothorax under two-lung ventilation is beneficial for maintaining steady haemodynamics and oxygenation in thoracoscopic-assisted oesophagectomy in the prone position (13). Despite common anaesthetic administration with one-lung ventilation, prone position-based thoracoscopic-assisted oesophagectomy has been popular as it can guarantee the operative field and manoeuvrability. The demands for mastery extend beyond surgical steps to anaesthetic administration and surgical nursing during the introduction of prone position surgery.
At our hospital, under right bronchial occlusion, one-lung ventilation-based prone position oesophagectomy was adopted to create artificial pneumothorax in 43 cases from July 2020 to June 2021. Since 2020, surgery has been performed with artificial pneumothorax pressure and gravity-based exclusion of the lungs from the operative field under a single lumen tube-based anaesthetic administration, applying bronchial blocking devices. The current research investigated the advantages of thoracoscopic-assisted oesophagectomy for oesophageal cancer, which was conducted under right bronchial occlusion with one-lung ventilation in the prone position.
2 Methods
2.1 Patients and data collection
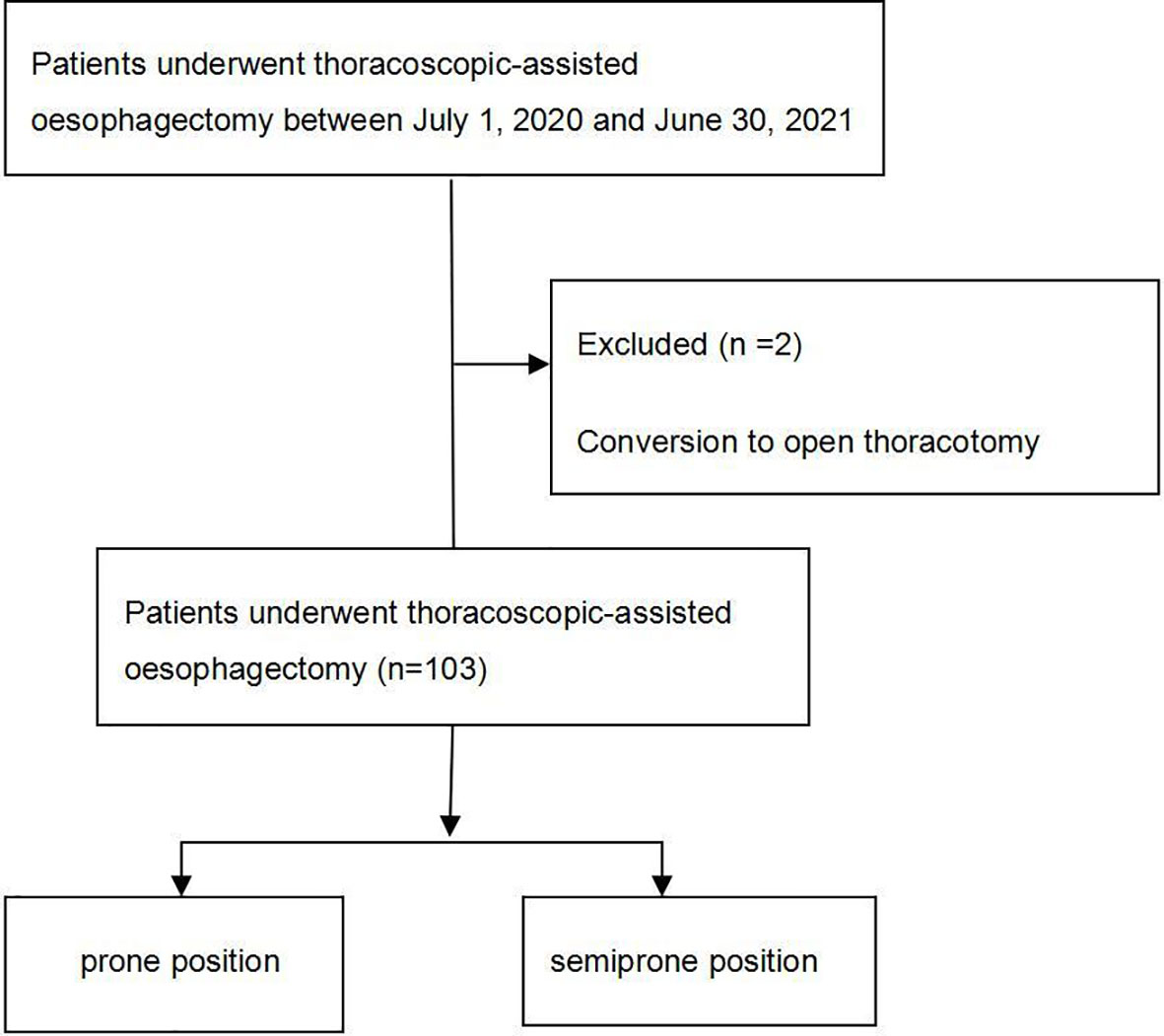
This study gathered 105 thoracoscopic-assisted oesophagectomy anaesthesia records from the same surgeon via the Anaesthesia Information Management System (AIMS) from July 2020 to June 2021. The patients underwent oesophageal surgery in the prone position (n = 43) or the semiprone position (n = 62).
2.1.1 Inclusion and exclusion criteria
Inclusion criteria were ASA II–III grade scheduling for artificial pneumothorax under right bronchial occlusion, one-lung ventilation, thoracoscopic-assisted oesophagectomy in the prone position or the semiprone position. The choice of the prone position or the semiprone position depends on the preference of the surgeon. Conversion to open thoracotomy or laparotomy, total laryngectomy, lung resection, and reoperation were excluded.
Ultimately, 103 patients with thoracoscopic-assisted oesophagectomy were included in the final analysis, including 43 patients in the prone position.
2.2 Preoperative preparations and anaesthesia protocol
No premedication was administered to the patients. In the operating room, the patients were monitored with noninvasive blood pressure (NIBP), bispectral index (BIS), pulse oximetry, electrocardiography (ECG), and right internal jugular central venous catheterization (CVC). The patients were injected with crystalloid (6 ml/kg) via a catheter inserted into a peripheral vein. Invasive blood pressure was monitored through cannulation of the radial artery after local administration of lidocaine anaesthesia. A target-controlled infusion (TCI) of 2% propofol was adopted to induce anaesthesia at an effect-site concentration (Ce) of 4 μg/ml, sufentanil at 0.6 μg/kg, cisatracurium at 0.2 mg/kg, and dexmedetomidine (DEX) at 1 μg/kg for 10 min; patients were intubated with a single-lumen endotracheal tube applying bronchial blockers by senior thoracic anaesthesiologists taking part in the research, and a fibreoptic bronchoscope (FOB) to confirm the correct location. During the periods of two-lung ventilation (TLV) and one-lung ventilation (OLV), a tidal volume of 7 ml/kg, a respiratory rate of 12 bpm, and an I/E proportion of 1:2 were realized. Cisatracurium at 0.12 mg/kg/h and 2% propofol Ce at 2–3 μg/ml titrated were used to maintain anaesthesia to keep BIS between 40 and 50; the average arterial blood pressure (MAP) and heart rate (HR) were 20% lower than the baseline values. The placement of the patient in a lateral semiprone position or prone position done after right internal jugular central venous catheterization. A FOB was adopted to confirm the correct bronchial blocker location. Then, 100% oxygen was used to initiate and maintain anaesthesia induction and one-lung ventilation (OLV). The pressure of the artificial pneumothorax was 8 mmHg, and the flow of the artificial pneumothorax was 8 L/min. At the end of the procedure, the chest was closed, the bronchial blocker was removed, the lung was restored with a manoeuvre, and the inspiratory pressure was increased to 40 cmH2O. Fifty percent oxygen and 5 cm H2O of positive end expiratory pressure (PEEP) were adopted to maintain two-lung ventilation. While completing the operation, an electronic infusion pump (FSQ-11 PCA; Inc., JiangSu AIPENG, ED, China) for patient-controlled anaesthesia (PCA) was set up for each patient. After surgery, patients are transported to the post-anaesthetic care unit (PACU).
2.3 Measurements
Baseline demographic and clinical data were collected, including age, sex, BMI, ASA grade, hypertension, diabetes, coronary heart disease, stroke, radiotherapy/chemotherapy, FEV1/FVC, DLCO, and respiratory comorbidity. The intraoperative and post-operative variables, such as total operative time, chest tube duration, total fluid volume, total blood loss, intraoperative blood transfusion, urine volume, intraoperative hypoxemia (SpO2 <90%), conversion to open thoracotomy, length of stay in the PACU, and PCA pressing frequency in 24 h, were collected too.
2.3.1 Primary outcome
The primary endpoint measures were PPCs (atelectasis, bronchospasm, aspiration pneumonitis, pulmonary infection, and respiratory failure). Radiologists measured atelectasis by chest X-ray (CXR) within 3 days after the operation. Respiratory failure and pulmonary infection were assessed with reference to the European Perioperative Clinical Outcome (EPCO) (14). All PPCs were evaluated within 7 days of the operation.
2.3.2 Secondary outcomes
The secondary endpoint measures were reintubation, anastomotic leakage, chylothorax, surgical site infection, atrial arrhythmia, acute cerebral infarction, myocardial infarction, reoperation, recurrent laryngeal nerve palsy, chest tube duration, postoperative length of stay, and ICU stay.
2.4 Statistical analysis
Quantitative variables are shown as the mean ± standard deviation. Categorical variables are presented as frequencies and fractions. SPSS version 25.0 (SPSS, Chicago, IL) was used to perform the statistical research. The comparison of all categorical variables was made with the χ2 test or Fisher’s exact test. The nonparametric Mann–Whitney U test or t-test was adopted to test continuous variables with a nonnormal distribution. Atelectasis was significantly associated with all risk factors by univariate analysis and was entered into a multivariable logistic regression model using a forward (LR) selection strategy. ROC analysis was used to determine the thresholds for DLCO% and surgery time. Two-sided p values <0.05 were considered indicative of statistical significance.
3 Results
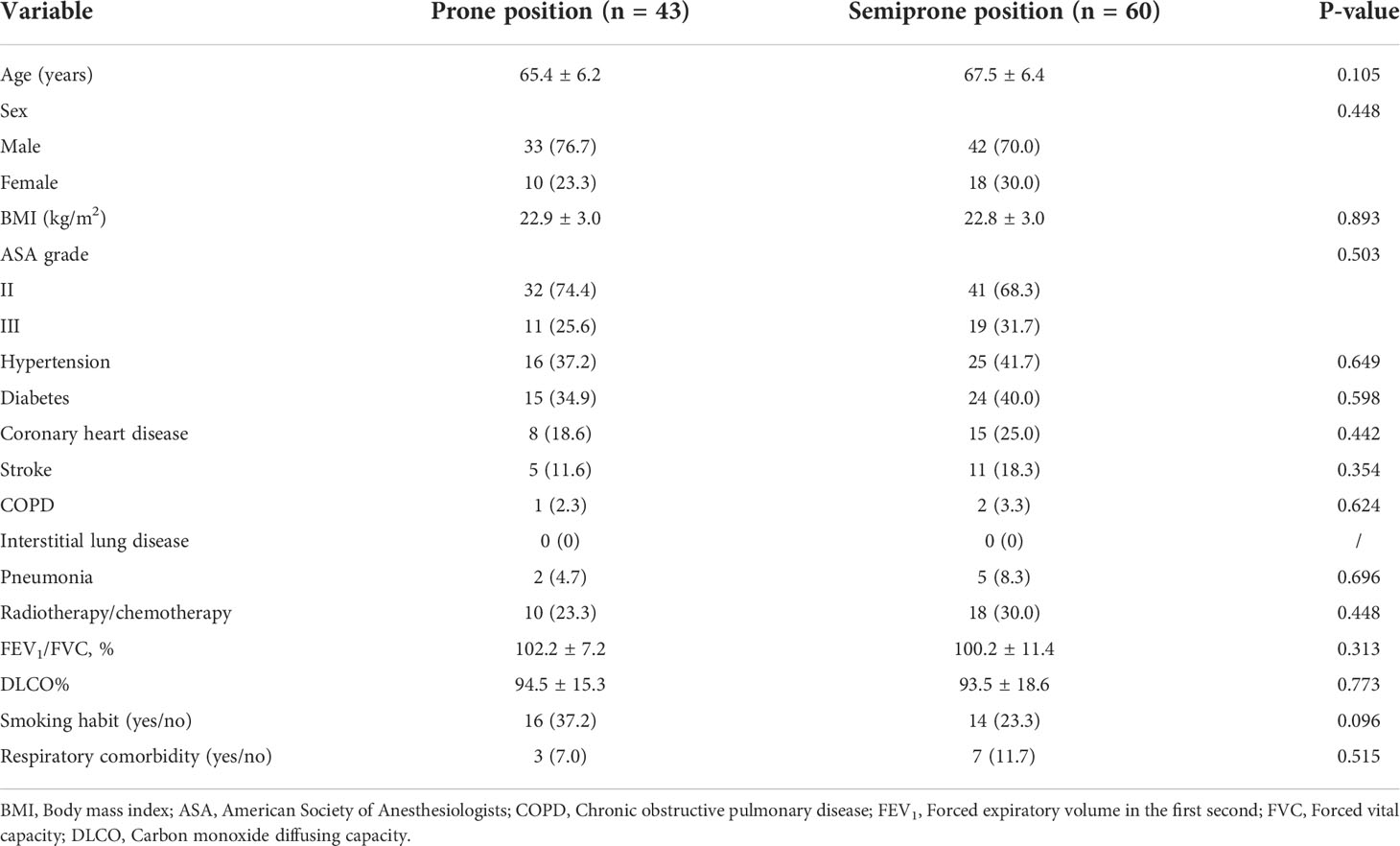
There were 105 patients in this research, but two were excluded. The final analysis (Figure 1) used information about 103 patients. No significant differences were found between the demographic data of the groups (Table 1), namely age, sex, BMI, ASA grade, hypertension, diabetes, coronary heart disease, stroke, radiotherapy/chemotherapy, FEV1/FVC, DLCO, and respiratory comorbidity (P >0.05, Table 1).
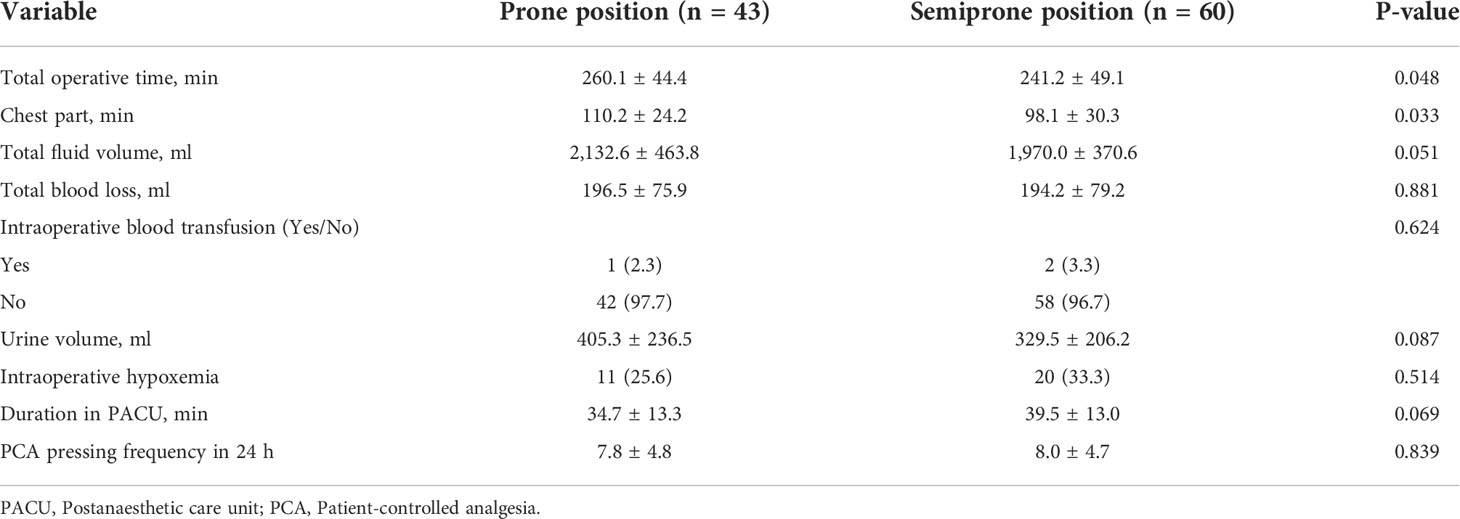
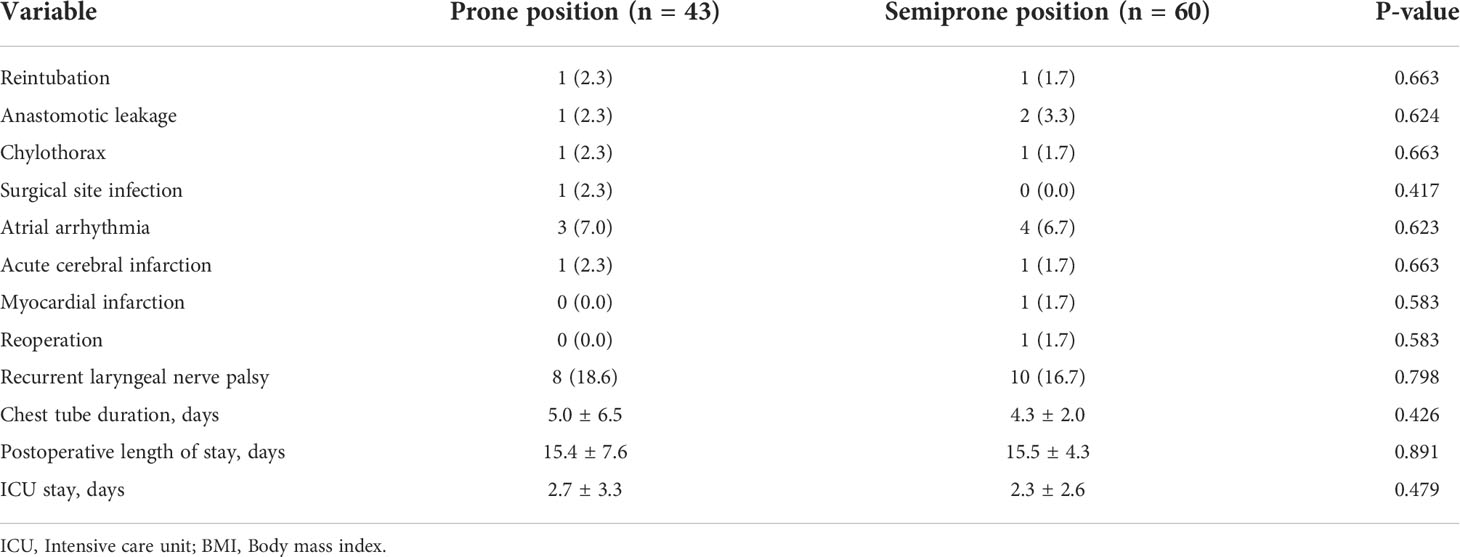
As shown in Table 2, patients in the prone position had a longer total operative time (260.1 ± 44.4 min vs 241.2 ± 49.1 min, P = 0.048). The other intraoperative surgical outcomes did not differ significantly. The patients in the prone position had a decreased incidence of atelectasis (12% vs. 30%, P = 0.032) (p <0.05, Table 3). No significant differences in the rates of cardiovascular and other complications, length of ICU stay, or LOS were found between the two groups (P >0.05) (Table 4).
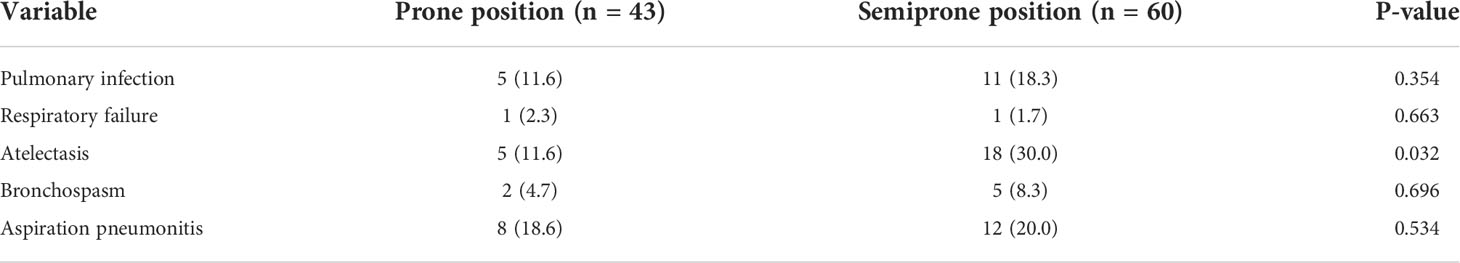
Table 3 Postoperative pulmonary complications between the prone position and semiprone position group.
Multivariable logistic regression analysis showed that the prone position (OR = 0.196, P = 0.011), smoking (OR = 0.103, P <0.001), preoperative DLCO% ≥90% (OR = 0.230, P = 0.003), and an operative time <180 min (OR = 0.268, P = 0.006) were associated with less atelectasis (Table 5).
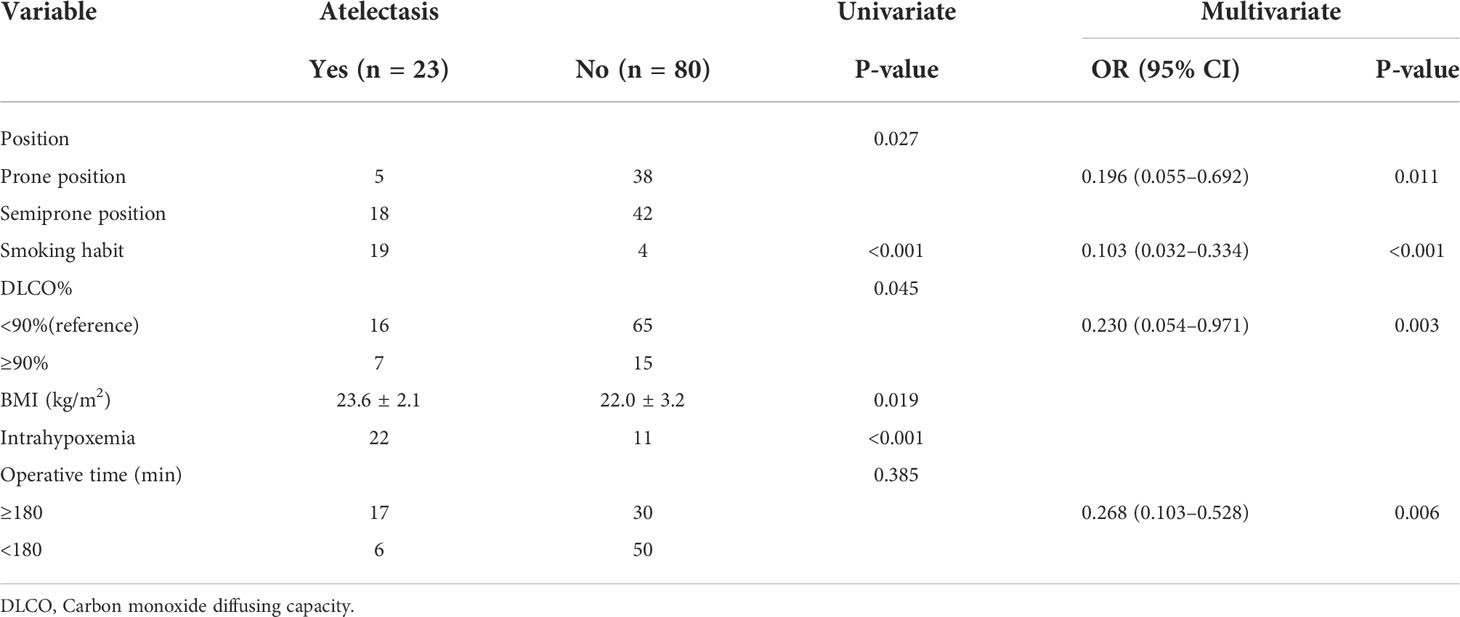
Table 5 The results of the bivariate and multivariate analyses of the factors associated with atelectasis.
4 Discussion
Our study showed that artificial pneumothorax under one-lung ventilation for patients with thoracoscopic-assisted oesophagectomy in the prone position was related to fewer PPCs than that in the semiprone position. The prone position could reduce the rate of atelectasis. Nevertheless, according to the results, in thoracoscopic-assisted oesophagectomy, the prone position has no effect on cardiovascular and other complications, ICU stay length and LOS. Therefore, in terms of PPCs, thoracoscopic-assisted oesophagectomy in the prone position may help to provide patients with more benefits.
It is not surprising that approximately 22.3% (23/103) of patients scheduled for thoracoscopic-assisted oesophagectomy have possible PPCs given the same prevalence of PPCs in other clinical studies (7). For example, recent studies have reported postoperative pulmonary complication rates of 19%–32% and in-hospital mortality rates ranging from 2 to 6% (7). The definition of PPCs in this research is based on the European Perioperative Clinical Outcome definition (14). From a surgical perspective, the operative field perspective in the prone position without compression of the right lung is improved by artificial pneumothorax and gravity, leading to no mechanical damage to the lungs. This technique has considerable merits, including enhanced surgeon ergonomics, increased operative field exposure, and excellent respiratory outcomes (15). Thoracoscopic-assisted oesophagectomy in the prone position is related to better surgical ergonomics compared with that in the semiprone position because of gravity pooling blood outside the operative field and the decreased demand for lung retraction (16).
A higher risk of airway secretions flowing into the left lung will be observed if the patient is placed in the semiprone position compared with the prone position. The enhancement in oxygenation may be one of the causes of reduced atelectasis in the prone position. The prone position could stop recurrent nerve palsy due to the wider view (17).
Thoracoscopic-assisted oesophagectomy in the prone position was related to fewer PPCs and decreased mortality in patients compared with that in the semiprone position (7). Therefore, this study confirms that PPCs could be reduced by thoracoscopic-assisted oesophagectomy in the prone position as opposed to the semiprone position. On the basis of this research, no great differences were shown in the rates of other postoperative complications, ICU stay length, or LOS.
It was shown that the prone position improves oxygenation in different diseases, including acute respiratory distress syndrome, pneumonia, and atelectasis (18–21). Physiologically, patients lying in the prone position have a satisfactory functional residual capacity (FRC) and ventilation/perfusion proportion. The prone position did not greatly influence the respiratory system or lung and chest wall compliance but improved lung volumes and oxygenation during general anaesthesia (22). FRC is reduced in the semiprone position because of increased intra-abdominal pressure and exclusion from the mediastinum compared with the supine position. In contrast, the FRC is increased in the prone position because of reduced cephalad pressure on the diaphragm (3). In the current research, there was mild variation in the ventilation/perfusion proportion in the prone position; alternatively, the decline in the ventilation/perfusion proportion in the semiprone position may be caused by increased blood flow to the left lung because of gravity. Moreover, while increasing the constriction of lung blood vessels, a higher carbon dioxide partial pressure (pCO2) caused by artificial CO2 pneumothorax enhances the ventilation/perfusion proportion in the prone position (23, 24).
There are several limitations to this research. First, the analyses on the basis of administrative coding data may be susceptible to reporting bias or coding mistakes. Second, the patients were not randomized into receiving artificial pneumothorax under right bronchial occlusion one-lung ventilation with thoracoscopic-assisted oesophagectomy in the prone position or the semiprone position. Future studies, such as randomized trials, may be indispensable for a more precise discussion to compensate for selection bias.
In conclusion, our study shows that artificial pneumothorax under right bronchial occlusion one-lung ventilation for patients with thoracoscopic-assisted oesophagectomy in the prone position may decrease PPCs by decreasing atelectasis in patients undergoing thoracic surgery compared with those in the semiprone position.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
QL: This author helped design and writing original draft preparation. MZ: This author helped data analysis and collection and manuscript writing. DW: This author conceptualization, methodology, and manuscript writing. XG: This author helped data collection, analysis and manuscript critical revision. JW: This author helped conceptualization, methodology, administrative support, manuscript writing, reviewing and editing. All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This work was supported by the Shanghai Shen Kang Hospital Development Center Project (SHDC2020CR4063) and the Nurturing Projects for Basic Research of Shanghai Chest Hospital (2021YNJCQ10) & 2019YNJCM08.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kitagawa H, Namikawa T, Munekage M, Fujisawa K, Munekgae E, Kobayashi M, et al. Outcomes of thoracoscopic esophagectomy in prone position with laparoscopic gastric mobilization for esophageal cancer. Langenbecks Arch Surg (2016) 401(5):699–705. doi: 10.1007/s00423-016-1446-8
2. Canet J, Gallart L, Gomar C, Paluzie G, Vallès J, Castillo J, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology (2010) 113(6):1338–50. doi: 10.1097/ALN.0b013e3181fc6e0a
3. Warner DO. Preventing postoperative pulmonary complications: the role of the anesthesiologist. Anesthesiology (2000) 92(5):1467–72. doi: 10.1097/00000542-200005000-00037
4. Mazo V, Sabaté S, Canet J, Gallart L, Abreu MG, Belda , et al. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology (2014) 121(2):219–31. doi: 10.1097/ALN.0000000000000334
5. Palanivelu C, Prakash A, Senthilkumar R, Senthilnathan P, Parthasarathi R, Rajan PS, et al. Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position–experience of 130 patients. J Am Coll Surg (2006) 203(1):7–16. doi: 10.1016/j.jamcollsurg.2006.03.016
6. Feng M, Shen Y, Wang H, Tan L, Zhang Y, Khan MA, et al. Thoracolaparoscopic esophagectomy: is the prone position a safe alternative to the decubitus position. J Am Coll Surg (2012) 214(5):838–44. doi: 10.1016/j.jamcollsurg.2011.12.047
7. Otsubo D, Nakamura T, Yamamoto M, Kanaji S, Kanemitsu K, Yamashita K, et al. Prone position in thoracoscopic esophagectomy improves postoperative oxygenation and reduces pulmonary complications. Surg Endosc (2017) 31(3):1136–41. doi: 10.1007/s00464-016-5081-9
8. Kubo N, Ohira M, Yamashita Y, Sakurai K, Lee T, Toyokawa T, et al. Thoracoscopic esophagectomy in the prone position versus in the lateral position for patients with esophageal cancer: a comparison of short-term surgical results. Surg Laparosc Endosc Percutan Tech (2014) 24(2):158–63. doi: 10.1097/SLE.0b013e31828fa6d7
9. Iwahashi M, Nakamori M, Nakamura M, Ojima T, Katsuda M, Lida T, et al. Clinical benefits of thoracoscopic esophagectomy in the prone position for esophageal cancer. Surg Today (2014) 44(9):1708–15. doi: 10.1007/s00595-013-0782-3
10. Koyanagi K, Ozawa S, Tachimori Y. Minimally invasive esophagectomy in the prone position improves postoperative outcomes: role of c-reactive protein as an indicator of surgical invasiveness. Esophagus (2018) 15(2):95–102. doi: 10.1007/s10388-017-0602-8
11. Teshima J, Miyata G, Kamei T, Nakano T, Abe S, Katsura K, et al. Comparison of short-term outcomes between prone and lateral decubitus positions for thoracoscopic esophagectomy. Surg Endosc (2015) 29(9):2756–62. doi: 10.1007/s00464-014-4003-y
12. Kim DJ, Hyung WJ, Lee CY, Lee JG, Haam SJ, Park IK, et al. Thoracoscopic esophagectomy for esophageal cancer: feasibility and safety of robotic assistance in the prone position. J Thorac Cardiovasc Surg (2010) 139(1):53–9. doi: 10.1016/j.jtcvs.2009.05.030
13. Saikawa D, Okushiba S, Kawata M, Okubo T, Kitashiro S, Kawarada Y, et al. Efficacy and safety of artificial pneumothorax under two-lung ventilation in thoracoscopic esophagectomy for esophageal cancer in the prone position. Gen Thorac Cardiovasc Surg (2014) 62(3):163–70. doi: 10.1007/s11748-013-0335-0
14. Jammer I, Wickboldt N, Sander M, Smith A, Schultz MJ, Pelosi P, et al. Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European perioperative clinical outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol (2015) 32(2):88–105. doi: 10.1097/EJA.0000000000000118
15. Petri R, Zuccolo M, Brizzolari M, Rossit L, Rosignoli A, Durastante V, et al. Minimally invasive esophagectomy: thoracoscopic esophageal mobilization for esophageal cancer with the patient in prone position. Surg Endosc (2012) 26(4):1102–7. doi: 10.1007/s00464-011-2006-5
16. Bonavina L, Laface L, Abate E, Punturieri M, Agosteo E, Nencioni M. Comparison of ventilation and cardiovascular parameters between prone thoracoscopic and ivor Lewis esophagectomy. Updates Surg (2012) 64(2):81–5. doi: 10.1007/s13304-012-0156-1
17. Fukuda N, Shichinohe T, Ebihara Y, Nakanishi Y, Asano T, Noji N, et al. Thoracoscopic esophagectomy in the prone position versus the lateral position (Hand-assisted thoracoscopic surgery): A retrospective cohort study of 127 consecutive esophageal cancer patients. Surg Laparosc Endosc Percutan Tech (2017) 27(3):179–82. doi: 10.1097/SLE.0000000000000395
18. Tanaka E, Okabe H, Kinjo Y, Tsunoda S, Obama K, Hisamori S, et al. Advantages of the prone position for minimally invasive esophagectomy in comparison to the left decubitus position: better oxygenation after minimally invasive esophagectomy. Surg Today (2015) 45(7):819–25. doi: 10.1007/s00595-014-1061-7
19. Hale DF, Cannon JW, Batchinsky AI, Cancio LC, Aden JK, White CE, et al. Prone positioning improves oxygenation in adult burn patients with severe acute respiratory distress syndrome. J Trauma Acute Care Surg (2012) 72(6):1634–9. doi: 10.1097/TA.0b013e318247cd4f
20. Gattinoni L, Tognoni G, Pesenti A, Taccone P, Mascheroni D, Malacrida R, et al. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med (2001) 345(8):568–73. doi: 10.1056/NEJMoa010043
21. Yatabe T, Kitagawa H, Yamashita K, Hanazaki K, Yokoyama M. Comparison of the perioperative outcome of esophagectomy by thoracoscopy in the prone position with that of thoracotomy in the lateral decubitus position. Surg Today (2013) 43(4):386–91. doi: 10.1007/s00595-012-0375-6
22. Pelosi P, Croci M, Calappi E, Cerisara M, Mulazzi D, Vicardi P, et al. The prone positioning during general anesthesia minimally affects respiratory mechanics while improving functional residual capacity and increasing oxygen tension. Anesth Analg (1995) 80(5):955–60. doi: 10.1097/00000539-199505000-00017
23. Barer GR, Howard P, Shaw JW. Stimulus-response curves for the pulmonary vascular bed to hypoxia and hypercapnia. J Physiol (1970) 211(1):139–55. doi: 10.1113/jphysiol.1970.sp009271
Keywords: oesophagectomy, thoracoscopy, artificial pneumothorax, one-lung ventilation (OLV), prone position, semiprone position
Citation: Li Q, Zhao M, Wu D, Guo X and Wu J (2022) Adverse outcomes of artificial pneumothorax under right bronchial occlusion for patients with thoracoscopic-assisted oesophagectomy in the prone position versus the semiprone position. Front. Oncol. 12:919910. doi: 10.3389/fonc.2022.919910
Received: 14 April 2022; Accepted: 12 July 2022;
Published: 09 August 2022.
Edited by:
Luigi Bonavina, University of Milan, ItalyReviewed by:
Carlo Alberto Manzo, University of Milan, ItalyIsabella Pezzoli, University of Milan, Italy
Copyright © 2022 Li, Zhao, Wu, Guo and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jingxiang Wu, d2p4MTEzMkAxNjMuY29t; Xufeng Guo, c2hhbmRhZ3hmQDEyNi5jb20=; Dongjin Wu, d3VkajAwMDFAcXEuY29t
†These authors contributed equally to this work and share first authorship
‡These authors contributed equally to this work and share last authorship
 Qiongzhen Li
Qiongzhen Li Mingye Zhao
Mingye Zhao Dongjin Wu
Dongjin Wu Xufeng Guo
Xufeng Guo Jingxiang Wu
Jingxiang Wu