- 1School of Public Health, Saint Peter Specialized Hospital, Addis Ababa, Ethiopia
- 2School of Medical Laboratory Sciences, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 3Department of Public Health and Health Policy, School of Public Health, Haramaya University, Harar, Ethiopia
- 4School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Background: Cervical cancer is the fourth most frequent cancer in women representing 6.6% of all female cancers occurring in low and middle-income countries, where resources for cancer prevention programs are often scarce. So this study aimed to assess the prevalence of precancerous cervical lesion and associated factors among adult women with human immune deficiency virus (HIV) on Anti Retroviral Therapy (ART) at Saint Peter Specialized Hospital, Addis Ababa, Ethiopia.
Methods: An institution-based cross-sectional study was conducted from November 06 to July 20, 2020 among 267 adult women with HIV on Anti Retroviral Therapy At Saint Peter Specialized Hospital, Ethiopia. Data were collected using face-to-face interview, patient chart review, and the examination of the squamo-columnar junction by the visual inspection with the acetic acid method. The collected data were entered into Epi-data version 3.1 and exported to Statistical Package for the Social Sciences (SPSS) version 24.0 for analysis. Bivariate and multivariable binary logistic regression analysis were used to identify factors associated with the precancerous cervical lesion. Statistical significance was considered at a P-valve less than 0.05.
Result: A total of 267 women who were on ART were included in the study and the prevalence of precancerous cervical lesion was 7.5% with 95% CI =4.10%-10.50%. Modern family planning (AOR = 4.14, 95% CI = 1.23-13.87), history of sexual transmission infection (STI) (AOR=5.39, 95% CI= 1.56-18.70) and viral load (AOR=20.85, 95% CI = 6.19-70.25) had significant association with precancerous cervical lesion
Conclusion: In this study, the prevalence of precancerous cervical lesion is relatively low compared to studies in low and middle-income countries. Modern family planning, history of sexual transmitted infection, and viral load had a significant association with a precancerous cervical lesion. Hence, encouraging modern family planning, and routine screening of women for pre-cancerous cervical lesions for those with high viral load have enormous contributions to decreasing cervical cancer disease among Women with Human Immune Deficiency Virus through Anti Retroviral Therapy.
Introduction
Despite the fact that cervical cancer is preventable through vaccination, screening, and treatment, approximately 570 000 cases of the disease and 311 000 deaths occurred worldwide in 2018. However, cervical cancer is the fourth leading cause of cancer deaths in women globally, and nearly 90% of cervical cancer deaths occurred in the developing world. Sub-Saharan Africa contains about 22% of global cervical cancer cases (1–3). The number of deaths is expected to rise by 67% by 2030, reaching 443,000 (4) In Ethiopia, an estimated 7000 new cases and 5000 deaths from cervical cancer occur each year (5).
The disproportionately high prevalence of cervical cancer in Sub-Saharan Africa, parts of Latin America and the Caribbean, and other medically underserved populations are primarily due to a lack of screening (3). Human papillomavirus (HPV), a sexually transmitted infection, is associated with a higher prevalence of HIV infection, especially in Sub-Saharan Africa (6–9); and in Ethiopia such to human papillomavirus (HPV), cultural factors, poverty, co-infection, and lack of awareness are common risk factors of cervical cancer (10). Furthermore, there is no standard policy or protocol for cervical cancer screening in Ethiopia; rather, it is patchy or inconsistent, and Ethiopian women typically present for cancer care at a late stage in the disease, when treatment is likely ineffective (5).
Screening high-risk and vulnerable populations for asymptomatic precancerous cervical lesions reduce the burden of cervical cancer-related morbidities and mortalities significantly (11) Ethiopia is currently implementing a Precancerous cervical lesion (PCCL) screening program in order to meet the 2020 target of screening at least 80% of 30-49-year-old women (12) and takes the cervical cancer crisis seriously, particularly because 99% of HIV+ women received a VIA test (13). Despite various prevention and control strategies, cervical cancer is still on the rise in Ethiopia. According to the 2016 Ethiopian demographic health survey (EDHS), the prevalence of HIV/AIDS among women aged 15 to 49 years was 1.2% (14). In Ethiopia, 534,000 women aged 15 and above are infected with HIV. These women are among the most vulnerable to cervical cancer because their risk of pre-cancerous lesions is ten times higher and they are more likely to develop invasive cervical cancer than uninfected women (9, 15).
According to WHO guidelines, every sexually active woman aged 30–49 years should have cervical cancer screening at least every 5 years. However, sexually active and HIV-positive women of any age should be screened every three years (1) Ethiopia adopted the WHO recommendation in 2015, recommending that HIV-positive women begin screening at HIV diagnosis, regardless of age, and re-screen every 5 years (15). Ethiopia’s government has placed a greater emphasis on programs aimed at detecting cervical cancer at an early stage. To combat cervical cancer, various stakeholders such as academia, professionals, the media, and development partners have made several advocacy efforts (15).
Despite the government’s commitment and the interventions of various stakeholders, the magnitude and major risk factors of Precancerous Cervical Lesions remain unabated. Moreover, to the knowledge of the investigator concerned, there is a paucity of research regarding predictors of Precancerous Cervical Lesions among adult women with HIV on Anti Retroviral Therapy at the study area level to help those working on the problem take evidence-based coordinated measures. As the result, the purpose of this study is to determine the magnitude and factors associated with precancerous cervical lesions among HIV-positive women who are on ART in St. Peter Specialized Hospital.
Methods and Materials
Study Design, Setting, and Period
An institutional-based cross-sectional study was conducted in St. Peter Specialized Hospital, Addis Ababa, the Capital City of Ethiopia from November 06 to July 20, 2020. St. Peter Specialized Hospital is one of the largest public hospital found in Addis Ababa city. The hospital was built in the early 1948G.C and currently, it has around 280 inpatient beds. The hospital is currently providing ART services for about 2300 HIV-positive clients by two medical doctors and 6 nurses. The hospital has started cervical cancer screening services since 2015 for all reproductive age women and has recently offered VIA cervical cancer screening and cryotherapy services.
Population and Eligibility Criteria
All HIV Positive women at age of 18 up to 65 years, who were on ART follow-up and didn’t get cervical cancer screening services in the last five years were the study population. Those who were diagnosed with cervical cancer before the study period were excluded from the study.
Sample Size and Sampling Procedures
The sample size was calculated using single population proportion formula with the assumptions of: Zα/2 = 1.96, 95% confidence level, 5% margin of error, and 20.2% proportion of precancerous cervical lesion among HIV positive women (taken from a study conducted in the Tigray Region, Northern Ethiopia (16). Since our study population was less than 10,000 (1540), finite population correction formula was used and the adjusted sample size was 242. By considering a 10% non-response rate, the final sample size was 267.
A systematic random sampling technique was used to select the study participants. Both primary and secondary data were collected through face-to-face interview, patient chart review, and visual inspection method.
Data Collection Tools, Procedures, and Quality Control
A structured questionnaire developed by reviewing other similar studies conducted before (8, 16, 17) was used to data related to socio-demographic and behavioral related factors. Wealth index tools were used in Ethiopia’s demographic health survey (14). A clinically related variable was collected from a patient chart review. Following the face-to-face interview study participants were tested for cervical cancer using visual inspection with acetic acid (VIA).
Trained nurses working in the precancerous cervical lesion screening and treatment centers of the Saint Peters hospitals were undertake the screening procedure and interviewed those patients after screening patients then review the patient chart.
Visual Inspection Methods
An un-lubricated bivalve speculum was inserted into the vagina and the cervix was visualized using a halogen focus lamp to identify the Squamo-Columnar Junction (SCJ). After cleaning away any excess mucus using a cotton swab, a five percent acetic acid solution was applied to the cervix for visual inspection with acetic acid. A finding was visible one minute after application. Precancerous lesions were defined as being dense aceto-white lesions with well-defined margins observed within the vicinity of the transformation zone originating from the SCJ, or if the whole cervix or cervical growth turned white (18). A suspicion of invasive cervical cancer was defined as any cervical ulcer or growth being observed. Results of VIA were classified as negative, positive, or suspicious for Invasive Cervical Cancer (ICC) according to the International Agency for Research on Cancer (IARC) training manual. Whenever there was uncertainty about the screening result, the nurses consulted a trained gynecologist, and he/she would confirm the diagnosis (19).
The questionnaire was initially prepared in English and then translated into the local language (Amharic language) by language experts then translated it back into English to ensure consistency. The data collectors and field supervisors received training on the data collection tool and procedures. Before the actual study, the pretest was conducted among 10% of study participants in similar settings. The investigators and experienced field research supervisors provided regular supervision.
Operational Definition and Measurement
Precancerous Cervical Lesions
Defined as being dense aceto-white lesions with well-defined margins observed within the vicinity of the transformation zone originating from the SCJ, or if the whole cervix or cervical growth turned white during VIA. It was classified as negative, positive, or suspicious for Invasive Cervical Cancer (ICC) according to the International Agency for Research on Cancer (IARC) training manual (18).
Suspicious of Cervical Cancer
Any abnormal mass around the cervical and ulcer mass with an unusual sign and symptom, or in the 12 months prior (20).
Extensive/Large Lesion
If the lesion extends beyond the cryoprobe being used, or extends more than 2 mm into the cervical canal or the vaginal wall (21).
Alcohol Use
A study participant who drinks or has a history of drinking at least two bottles of beer per day or at least ten bottles of beer per week was considered an alcohol user (6).
Cigarette Smoking
Current Smoker
A study participant who has smoked at least 100 cigarettes in her lifetime and who currently smokes cigarettes (22).
Former Smoker
A study participant who has smoked at least 100 cigarettes in her life but who had quit smoking at the time of interview (22).
Non-smoker: A study participant who has never smoked cigarettes, or who has smoked less than 100 cigarettes in her lifetime (22).
Data Processing and Analysis
The collected data were checked for completeness, cleaned, coded, and entered into EpiData version 3.1. Then, the data were exported to SPSS version 24 for analysis. Descriptive and summary statistics were done and the information was presented using tables.
A binary logistic regression model was fitted to check for the association between independent variables and the outcome variable. The assumptions of binary logistic regression were checked. The goodness of fit was checked by Hosmer-Lemeshow statistic and omnibus tests. The assumptions were fulfilled and the model was fitted for the data. All variables with p < 0.25 in the bivariate analysis were included in the final multivariable analysis to identify the true predictors of precancerous cervical lesions among adult women with HIV on Anti Retroviral Therapy. Multi-collinearity test was carried out to check the presence of correlation between independent variables by using the standard error and co-linearity statistics but there was no multi-collinearity found among the variables. The direction and strength of statistical association were measured by odds ratio (OR) along with the 95% confidence interval (CI). P-value < 0.05 was considered to declare statistical significance.
Results
Socio-Demographic Characteristics
A total of 267 women who were on ART were included with a response rate of 100%. The mean age of study participants was 39.7 (SD ±8.08) years old, and 125 (46.8%) were in the age category of 31-40 years. Two hundred fifty-seven (96.3%) and 226 (84.6%) of study participants were urban residents and Orthodox followers, respectively. Eighty (30.0%) were unable to read and write and 13 (4.9%) had college or above education status. Housewife 106 (39.7%) and daily laborer 74 (27.7%) were more frequently mentioned occupations of study participants. The study participants’ mean ages at menarche, first sexual intercourse, and first marriage were 14.4 (1.08%) years, 19.4 (1.82%) years, and 22.5 (3.23%) years, respectively. There were 237 people who had two or more sexual partners at some point in their lives (88.9%). In terms of pregnancy history, the average age at first pregnancy was 23.7 (3.22%) (Table 1).
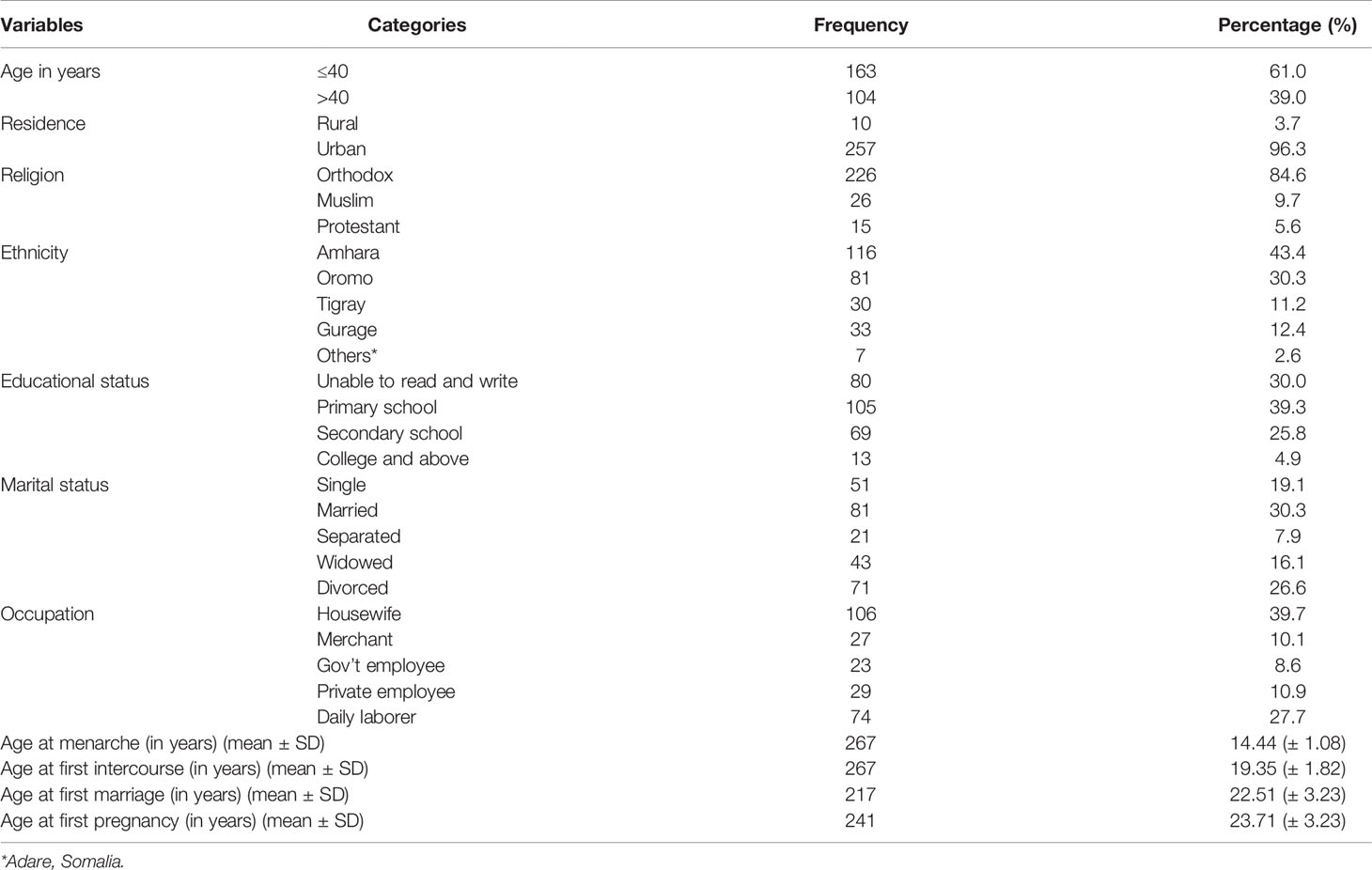
Table 1 Sociodemographic characteristics of study participants in Saint Peter Specialized Hospital, ART clinic, Ethiopia, 2020 (n=267).
Lifestyle and Behavioral Characteristics
Seven (2.6%) of the women in the study had a history of cigarette smoking, and only one woman reported being a current smoker. Fifty-two (19.5%) of study participants had a history of drinking alcohol, and 33 (12.4%) were current drinkers. One hundred seventy-four (65.1%) and 165 (75.7%) were multi-gravid and multi-para, respectively. Among the 232(86.9%) study participants who had a pregnancy history for more than 28 weeks, 57(24.6%) had one child, 107(46.1%) had two children, and 68(29.3%) had three or more children. Of 23 (9.5%) with a history of abortion, 14 (60.9%) participants were who had a history of abortion two or more times. Of the 214 (80.1%) modern family planning users, 125 (58.4%) used condoms and 56 (26.2%) used injectable family planning methods, respectively (Table 2).
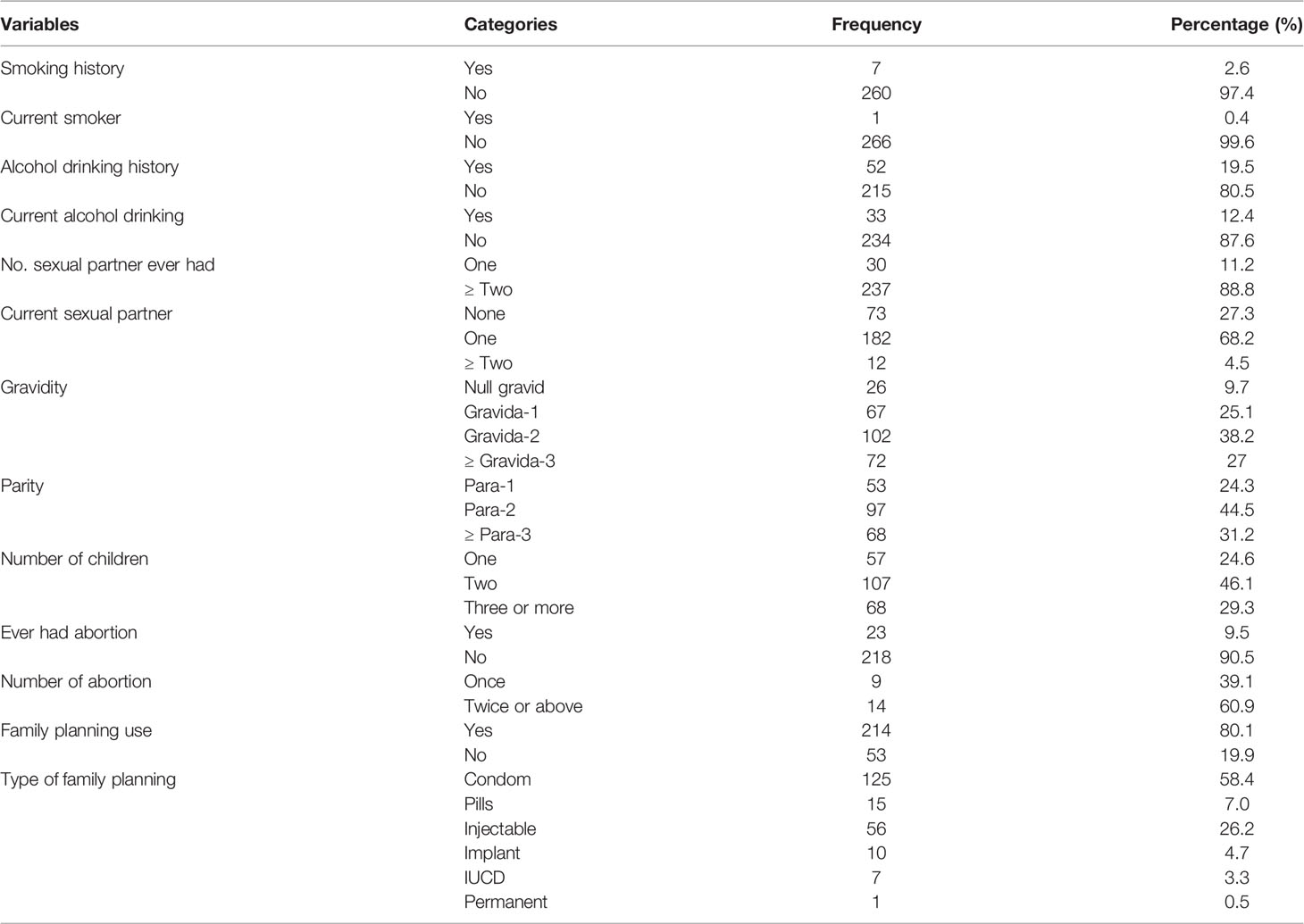
Table 2 Lifestyle and behavioural characteristics of study participants in Saint Peter Specialized Hospital, ART clinic, Ethiopia, 2020 (n=267).
Reproductive and Other Clinical Health
Forty-seven (17.6%) of the participants had a history of STIs, and 18 (6.7%) had a family history of cervical cancer. One hundred thirteen (42.3%) of study participants had HIV for more than ten years, followed by 84 (31.5%) for six to ten years and 70 (26.2%) for one to five years. Participants in the study who had been on ART for 1-5, 6-10, and >10 years were 80 (30.0%), 94 (35.2%), and 93 (34.8%), respectively. Currently, 239 (89.5%) had good ART drug adherence, and 26 (9.7%) were placed on second-line ART drug regimens. At the outset, 104 (39.0%) and 22 (8.2%) of study participants were in WHO clinical stages III and IV, respectively. A baseline CD4 count of 200 cells/ml was found in 111 (41.6%) of the participants. The most recent viral load count of 230 (86.1%) study participants was undetectable. Vaginal good abnormality was found in 16 (6.0%) of the participants (Table 3).
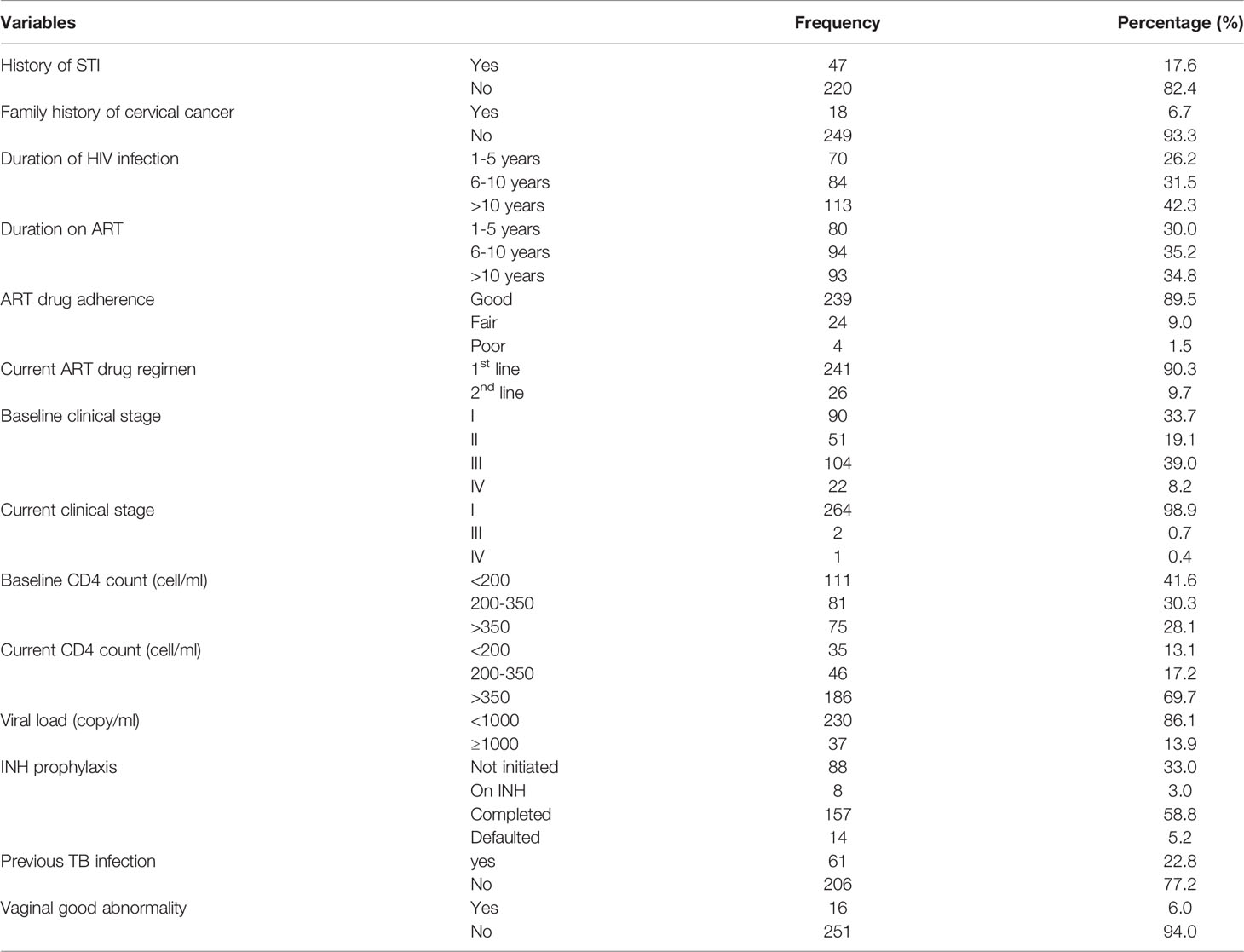
Table 3 Reproductive health and clinical characteristics of participants in Saint Peter Specialized Hospital, ART clinic, Ethiopia, 2020 (n=267).
Prevalence of Precancerous Cervical Lesion
The prevalence of precancerous cervical lesions among ART clients in St. Peter Specialized Hospital was 20(7.5%) with 95%CI of (4.1%-10.5%).
Factors Associated With Precancerous Cervical Lesion
In bivariate binary logistic regression analysis, age, age at first sexual intercourse, age at first pregnancy, modern family planning use, previous STI, duration on ART, current ART drug regimen, drug adherence, and viral load of mothers were significantly associated with the precancerous cervical lesion. But, in the multivariable binary logistic regression analysis, modern family planning use, previous STI, and viral load were factors significantly associated with a precancerous cervical lesion (Table 4).
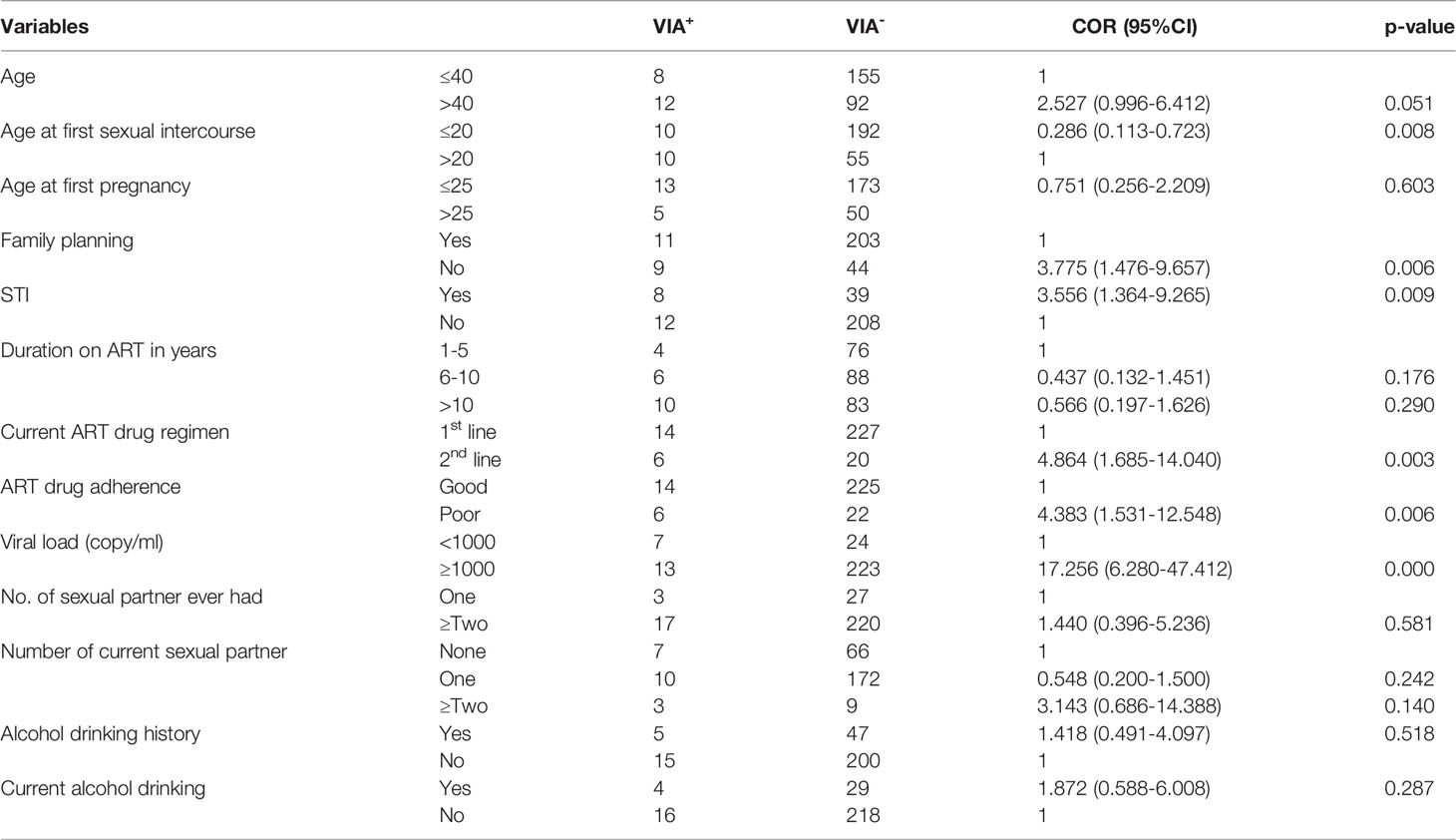
Table 4 Bivariate analysis of sociodemographic, reproductive and clinical health with precancerous cervical lesion in SPSH ART clinic, 2020.
The odds of developing precancerous cervical lesion among women who did not use modern family planning was 4.14 times the odds of those women who used modern family planning (AOR = 4.14; 95% CI = 1.23-13.87). The odds of developing precancerous cervical lesion among women who had a history of STI was 5.39 times the odds of those women who had no history of STI (AOR=5.39, 95% CI =1.56-18.70). The odds of developing precancerous cervical lesion among women who had a high viral load (≥1000 copy/ml) was 20.85 times the odds of those women who had suppressed viral load (<1000copy/ml) (AOR=20.85, 95% CI= 6.19-70.25) (Table 5).
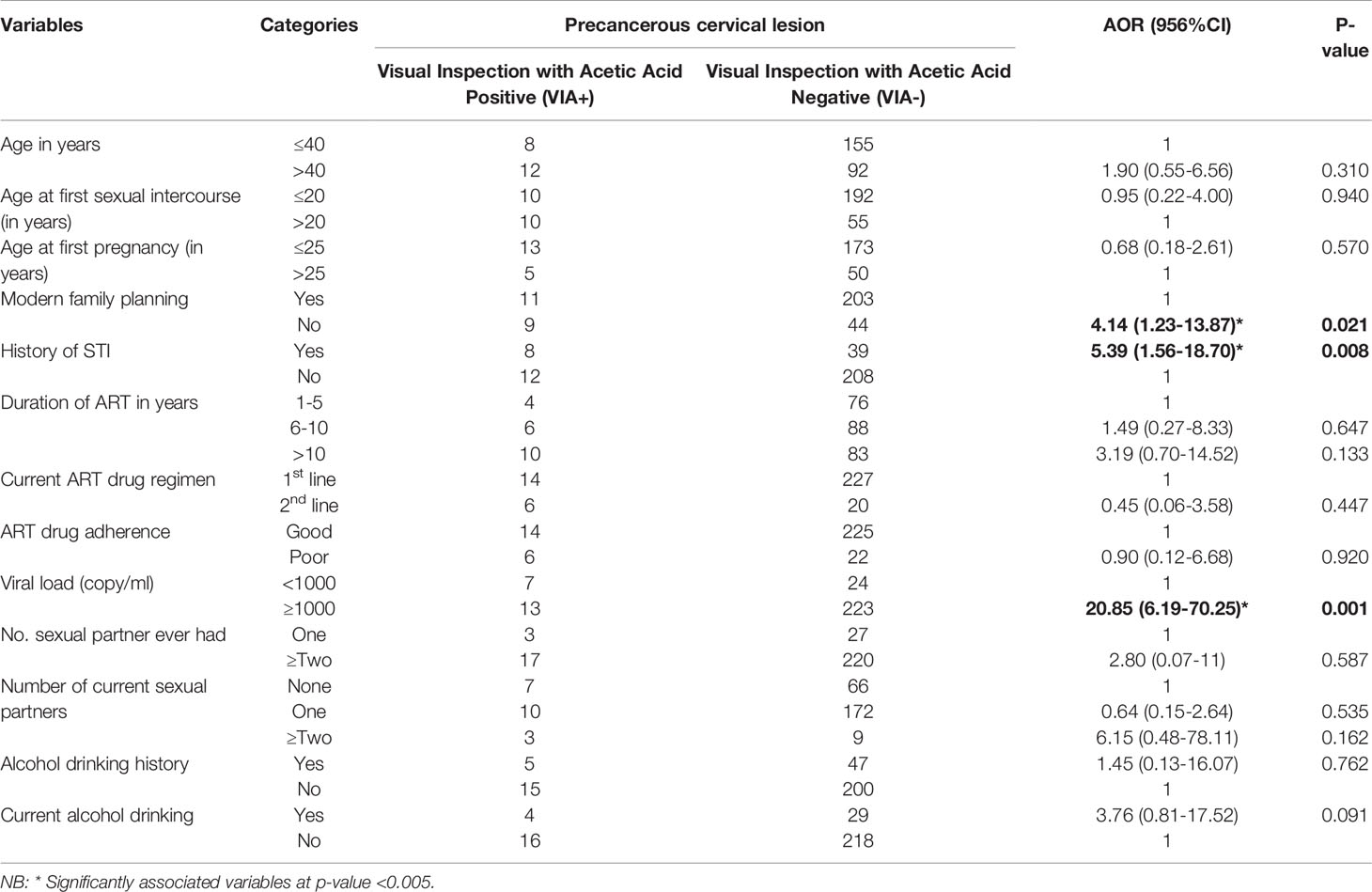
Table 5 Multivariable analysis of sociodemographic, reproductive, and clinical health with the precancerous cervical lesion in Saint Peter Specialized Hospital, ART clinic, Ethiopia, 2020.
Discussion
This study assessed the magnitude of the precancerous cervical lesion and its associated factors among adult women with HIV on Anti Retroviral Therapy at Saint Peter Specialized Hospital, Ethiopia. It revealed that the magnitude of the precancerous cervical lesion among adult women with HIV on Anti Retroviral Therapy was 7.5% (95%CI: 4.1%-10.5%). HIV-positive women who did not utilize modern family planning, who had a history of STI and poor viral suppression were significantly associated with precancerous cervical lesions.
According to a finding of this study the prevalence of precancerous cervical lesions among HIV-positive women attending ART clinics in St. Peter Specialized Hospital was 7.5%. A similar finding was reported in a study conducted in Nigeria (6%) (23) and Uganda (6.3%) (24). This could be due to the fact that they use a similar strategy and methods for screening and have a similar social structure. In contrast to this, the finding of this study is lower than the studies done in Zambia (52%) (25), Kenya (26.7%), (26), and Brazil (23.4%) (27). The observed inconsistency in the prevalence of precancerous cervical lesions could be attributed to differences in sociodemographic or clinical characteristics of study participants, such as age composition, ART initiation, and adherence to ART drugs. Differences in precancerous cervical lesion screening methods could also explain the observed discrepancy in precancerous cervical lesion prevalence.
In this study, the odds of developing precancerous cervical lesion among women who did not use modern family planning was 4.14 times the odds of those women who used modern family planning methods. This could be related to the fact that the majority of modern family planning methods thicken the cervical mucus, which helps to prevent the entry of infections such as HPV, which is a widely accepted cause of cervical cancer. In contrast to this, a finding from a few studies suggests that oral contraceptive use increased the occurrence of precancerous cervical lesions as prolonged use of oral contraceptives may increase the eversion of the columnar epithelium to the ectocervix, which enhances the exposure of the columnar epithelium to HPV infection (7, 28, 29). Our study pointed out that nearly 60% of the 80.1% of family planning users were condom users, which have a dual purpose of family planning and STI prevention, including human papillomavirus (HPV) infection. This could explain why, in our study, modern family planning had a protective effect on the precancerous cervical lesion. Condom use was consistently advised to HIV patients; this could be the most effective method of protecting against STIs, which were the most risk factor for Cervical Cancer.
This study pointed out that the odds of developing precancerous cervical lesion among women who had a history of STI was 5.39 times the odds of those women who had no history of STI. One possible explanation could be the co-infection of HPV with other STIs, which severely affects immunocompromised women and makes them vulnerable to other opportunistic infections. This is in harmony with studies done in Addis Ababa (30) and Adama (7) of Ethiopia which revealed that women with a history of STIs were significantly associated with the cervical precancerous lesion. Another study in Uganda found that women who did not have STI at the time of their visit had a 76% lower risk of developing precancerous cervical lesions (24). The majority of evidence suggested that cervical cancer is caused by a viral infection and that the virus spreads through sexual contact. Chlamydia trachomatis infection, for instant, has been linked to the severity of abnormal cervical cytology and HPV infection.
According to the findings of the current study, the odds of developing precancerous cervical lesion among women who had a high viral load (≥1000 copy/ml) was 20.85 times the odds of those women who had suppressed viral load <1000 copy/ml). Clients’ immune status is directly related to their CD4 count and HIV-viral load. A high viral load indicates immune suppression and a poor response to ART medications. Similarly, a follow-up study at the Chittaranjan National Cancer Institute found that women with high viral loads had a fourfold higher risk of cervical intraepithelial neoplasia than those with low viral loads (20). This could be because HPV DNA integration into host cells is required for malignant transformation by the E6 and E7 proteins. HPV DNA load has been proposed as a risk factor for dysplasia and cervical cancer.
Limitation of the Study
Visual inspection with an acetic acid test result of postmenopausal women may not be reliable, because the transformation zone of these women is often inside the cervical canal which may have an impact on the magnitude.
Conclusions
In this study, the prevalence of precancerous cervical lesions was relatively lower than what had been reported in low and middle-income countries. Modern family planning, history of sexual transmitted infection, and viral load had a significant association with a precancerous cervical lesion. Hence, encouraging modern family planning, and routine screening of women for pre-cancerous cervical lesions for those with high viral load have enormous contributions to decreasing cervical cancer disease among Women with Human Immune Deficiency Virus through Anti Retroviral Therapy.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Haramaya University College of Health and Medical Sciences Institutional Health Research Ethics Review Committee (IHRERC). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the manuscript; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Haramaya University provided financial support for this study. But the funding agency had no role in the collection, analysis, and interpretation of the data as well as the writing-up of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors are very thankful to Haramaya University, heads and staff of Saint Peter Specialized Hospital, the study participants, data collectors, and field supervisors.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.910915/full#supplementary-material
Abbreviations
CC, Cervical Cancer; CI, Continuous Integration; CIN, Cervical Intraepithelial Neoplasia; HSV, Herpes Simplex Virus; ICC, Invasive Cervical Cancer; PCL, Precancerous Cervical Lesions; PLHIV, People Living With Human Immunodeficiency Virus; OC, Oral Contraceptive; SPSH, Saint Peter Specialized Hospital.
References
1. WHO. Guidelines for Screening and Treatment of Precancerous Lesions for Cervical Cancer Prevention. Geneva: World Health Organization (2013). p. 58.
2. Begoihn M, Mathewos A, Aynalem A. Cervical Cancer in Ethiopia Predictors of Advanced Stage and Prolonged Time to Diagnosis. BMC:Infectious Agent Cancer (2019) 14:1–7. doi: 10.1186/s13027-019-0255-4
3. Cecilia NC, A.M R, I S. Global Burden of Cervical Cancer. Int J Public Health Clin Sci (2017) 4:664–70.
4. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin (2018) 68:394–424. doi: 10.3322/caac.21492
5. Asseffa NA. Cervical Cancer: Ethiopia’s Outlook. J Gynecol Women’s Health (2017) 5:555660. doi: 10.19080/jgwh.2017.05.555660
7. Roza T. Risk Factors Associated With Precancerous Cervical Lesion Among Women Screened at Marie Stops Ethiopia, Adama Town, Ethiopia. BMC Res (2018) 11(1):2–5. doi: 10.1186/s13104-018-3244-6
8. Tadesse B, Habtamu M, Fitsum W. Precancerous Cervical Lesion and Associated Factors Among HIV-Infected Women on ART in Amhara Regional State,Ethiopia: A Hospital-Based Cross-Sectional Study. Int J Collab Res Internal Med Public Health (2019) 13:4–9.
9. Hailemariam T, Yohannes B, Mamaye E. Prevalence of Cervical Cancer and Associated Risk Factors Among Women Attending Cervical Cancer Screening and Diagnosis Center at Yirgalem General Hospital, Southern Ethiopia. J Cancer Sci Ther (2017) 9(11):1–6. doi: 10.4172/1948-5956.1000500
10. Arbyn M, Weiderpass E, Bruni L, De Sanjosé S, Saraiya M, Ferlay J, et al. Estimates of Incidence and Mortality of Cervical Cancer in 2018: A Worldwide Analysis. Lancet Global Health (2020) 8:e191–203. doi: 10.1016/S2214-109X(19)30482-6
11. WHO. Strategic Planning for Cervical Cancer Prevention and Control in Africa. Training Manual. Geneva: World Health Organization (2020). CC BY-NC-SA 3.0 IGO.
12. FMOH, F. D. R. O. E. M. O. H. Guideline for Cervical Cancer Prevention and Control in Ethiopia, Vol. 8. Addis Ababa, Ethiopia: Federal Ministry of Health New York, NY: World Health Organization (2015).
13. FMOH. Guideline for Cervical Cancer Prevention Andcontrol in Ethiopia. Addis Ababa, Ethiopia: Federal Ministry of Health (2015).
14. Ethiopia Demographic and Health Survey. Key Indicators Report. New York, NY: CSA and ICF (2016). p. 59.
15. FMOH. Guideline for Cervical Cancer Prevention and Control in Ethiopia. Addis Ababa, Ethiopia: Federal Ministry of Health (2015).
16. Gebrehiwot H, Kumari S, Berhane Y. Pre-Cancerous Cervical Lesion Using Visual Inspection With Acetic Acid Among Women Attending Anti-Retroviral Therapy. Eur J Pharm Med Res 4 (2017) 4(2):41–6.
17. Zekariase G, Zemen T, Mussie A, Hiruye A, Yeneneh G, Miliard D. Determinant Factors of Visual Inspection With Acetic Apcid (via) Positive Lesions Among Hiv Positive Women in Mekelle Hospital, Northern Ethiopia. Ethiop Med (2015) 2:17–22.
19. Odendal L. Cervical Cancer in Women With HIVHIV and AIDS Treatment in Practice Health. (2011)12911:314–20.
20. Mittal S, Basu P, Muwonge R. Risk of High Grade Precancerous Lesions and Invasive Cancers in High Risk HPV Positive Women With Normal Cervix. Int J Cancer (2017) 140:1850–9. doi: 10.1002/ijc.30609
21. Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R. Cancer of the Cervix Uteri: 2021 Update. Int J Gynaecol Obstet (2021) 155 Suppl 1:28–44. doi: 10.1002/ijgo.13865
23. Ononogbu U, Almujtaba M, Modibbo F, Lawal I, Offiong R, Olaniyan O, et al. Cervical Cancer Risk Factors Among HIV-Infected Nigerian Women (2013). Available at: http://nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-ofuse#LAA.
24. Izudi J, Adrawa N, Amongin D. Precancerous Cervix in Human Immunodeficiency Virus Infected Women Thirty Years Old and Above in Northern Uganda. J Oncol (2016) 2016:54736817. doi: 10.1155/2016/5473681
25. Bateman AC, Katundu K, Mwanahamuntu MH, Kapambwe S, Sahasrabuddhe VV, Hicks ML, et al. The Burden of Cervical Pre-Cancer and Cancer in HIV Positive Women in Zambia: A Modeling Study. BMC Cancer (2015) 15:541. doi: 10.1186/s12885-015-1558-5
26. Memiah P, Mbuthia W, Kiiru G, Agbor S, Odhiambo F, Ojoo S, et al. Prevalence and Risk Factors Associated With Precancerous Cervical Cancer Lesions Among HIV-Infected Women in Resource-Limited Settings. AIDS Res Treat (2012) 2012:7. doi: 10.1155/2012/953743
27. Teixeira NCP, Araujo ACL, Correa CM. Prevalence and Risk Factors for Cerviintraepithelial Neoplasia Among HIV-Infected Women, Brazil Salvador. Infect Dis (2012) 16:1413–8670. doi: 10.1590/s1516-31802010000400004
28. Melkamu G, Baye G, Abinet S. Prevalence and Predictors of Pap Smear Cervical Epithelial Cell Abnormality Among HIV-Positive and Negative Women Attending Gynecological Examination in Cervical Cancer Screening. BMC Clin Pathol (2015) 15:1–10. doi: 10.1186/s12907-015-0016-2
29. Wabo B, Nsagha DS, Nana TN, Assob CJN. Prevalence and Risk Factors Associated With Precancerous Cervical Lesions Among Women in Two Cities in Cameroon. Pan Afr Med J (2022) 41:1–15. doi: 10.11604/pamj.2022.41.276.21972
Keywords: precancerous cervical lesion, HIV, ART, prevalence, Ethiopia
Citation: Zelalem W, Weldegebreal F, Ayele BH, Deressa A, Debella A, Eyeberu A, Hassen FA and Dessie Y (2022) Precancerous Cervical Lesion Among Adult Women With Human Immune Deficiency Virus on Anti Retroviral Therapy At Saint Peter Specialized Hospital, Ethiopia: A Hospital-Based Cross-Sectional Study. Front. Oncol. 12:910915. doi: 10.3389/fonc.2022.910915
Received: 01 April 2022; Accepted: 31 May 2022;
Published: 22 July 2022.
Edited by:
Nadia Judith Jacobo-Herrera, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (INCMNSZ), MexicoReviewed by:
Mesafint Abeje Tiruneh, Ministry of Health, EthiopiaCarla M. A. Pinto, Instituto Superior de Engenharia do Porto (ISEP), Portugal
Copyright © 2022 Zelalem, Weldegebreal, Ayele, Deressa, Debella, Eyeberu, Hassen and Dessie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fitsum Weldegebreal, ZndtbGFiMjAwMEBnbWFpbC5jb20=; orcid.org/0000-0002-78671483-a
 Wondimu Zelalem
Wondimu Zelalem Fitsum Weldegebreal
Fitsum Weldegebreal Behailu Hawulte Ayele
Behailu Hawulte Ayele Alemayehu Deressa
Alemayehu Deressa Adera Debella
Adera Debella Addis Eyeberu
Addis Eyeberu Fila Ahmed Hassen
Fila Ahmed Hassen Yadeta Dessie
Yadeta Dessie