- 1Department of Ultrasound, The Cancer Hospital of the University of Chinese Academy of Sciences (Zhejiang Cancer Hospital), Institute of Basic Medicine and Cancer (IBMC), Chinese Academy of Sciences, Hangzhou, China
- 2Key Laboratory of Head & Neck Cancer Translational Research of Zhejiang Province, Hangzhou, China
- 3Graduate School, Wannan Medical College, Wuhu, China
- 4The Postgraduate Training Base, Wen Zhou Medical University, Hangzhou, China
Background: Minimally invasive treatment of thyroid tumors has become increasingly common, but has mainly focused on benign thyroid tumors, whereas thermal ablation of thyroid cancer remains controversial. Clinical studies analyzing the efficacy of thermal ablation of papillary thyroid carcinoma (PTC) have been conducted in several countries to verify its safety. Here, we screened and reviewed recent studies on the efficacy and safety of thermal ablation of PTC as well as psychological assessment, patient prognosis, recurrence, and factors affecting ablation.
Summary: The most significant controversy surrounding ablative treatment of PTC centers on its effectiveness and safety, and >40 studies have been conducted to address this issue. The studies include papillary thyroid microcarcinoma (PTMC) and non-PTMC, single PTC and multiple PTC, and controlled studies of ablative therapy and surgical treatment. In general, ablation techniques can be carefully performed and promoted under certain conditions and with active follow-up of postoperative patients. Ablation is a promising alternative treatment especially in patients who are inoperable.
Conclusions: Clinical studies on PTC ablation have provided new perspectives on local treatment. However, because PTC grows very slowly, it is an indolent tumor; therefore, studies with larger sample sizes and extended post-procedure follow-ups are necessary to confirm the investigators’ hypotheses.
Introduction
Thyroid cancer is the most common malignant tumor of the head and neck; papillary thyroid carcinoma (PTC) is the most common type, and its incidence is increasing worldwide (1). There are many reasons for the increasing incidence of PTC, among which improved quality of life (QoL), increased health awareness, and the widespread popularity of medical checkups are the main reasons (2–4). A national screening program in South Korea resulted in a 15-fold increase in the incidence of thyroid cancer over a period of 18 years (5). However, the mortality rate of thyroid cancer has decreased because of the slow progression and low risk of most thyroid cancers. These cancers are referred to as low-risk PTCs, and they are characterized by the absence of significant capsule invasion, extra-thyroidal expansion, lymph node metastasis, and distant metastasis (6). Low-risk PTCs are often detected at autopsy or during physical examination. In recent years, local ablation treatment has been applied to low risk PTCs. The ablation methods include radiofrequency ablation (RFA) microwave ablation (MWA), laser ablation (LA), and ethanol injection, and the first three methods are collectively known as thermal ablation. Thermal ablation only damages the tumor while sparing most of the thyroid glands and periglandular tissues, which opens up a new way of thinking about the treatment of thyroid cancer.
Review
Thermal Ablation Study of Papillary Thyroid Microcarcinoma
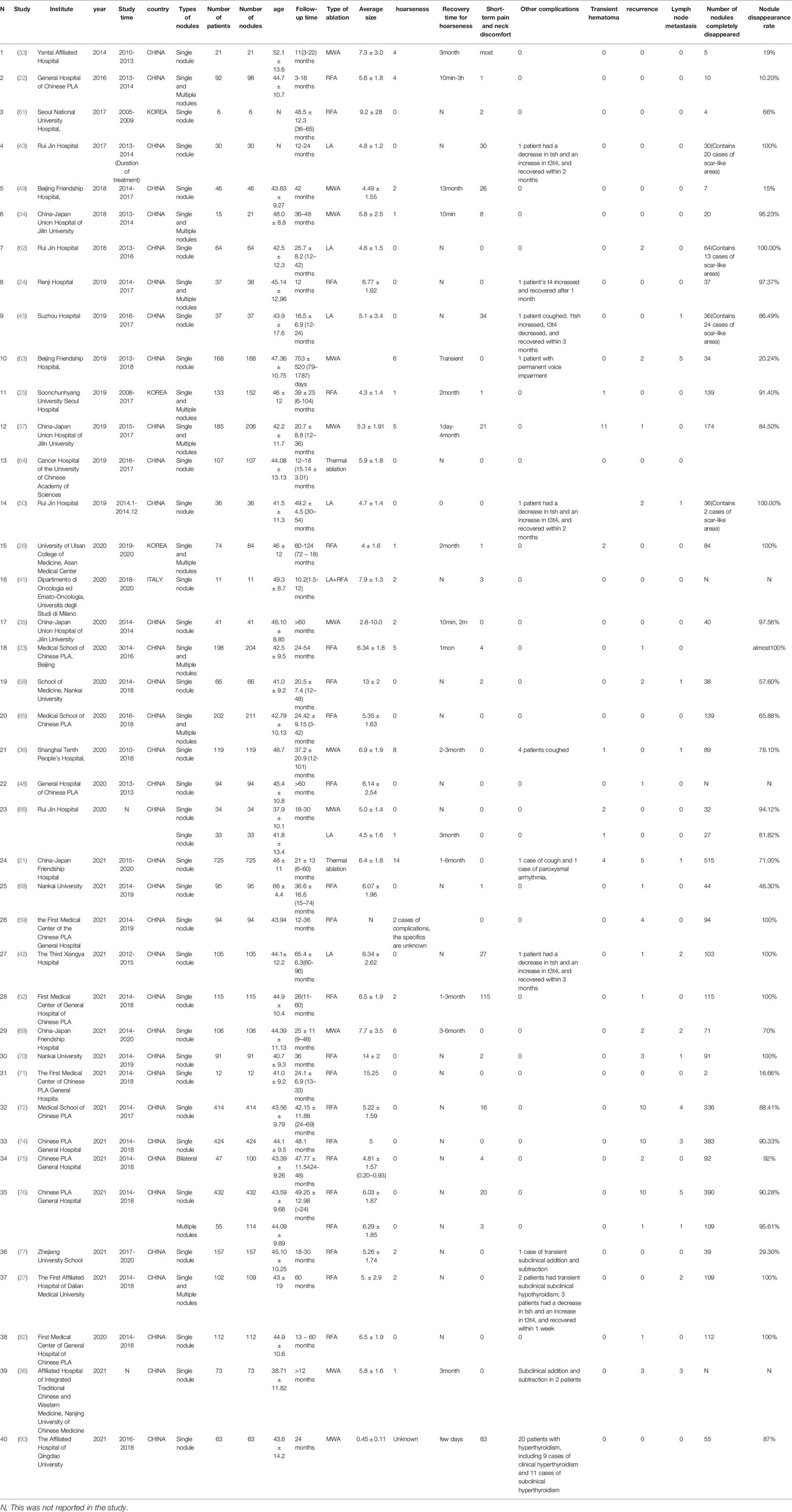
Papillary thyroid microcarcinoma (PTMC) is a thyroid cancer of ≤10 mm in diameter and is usually considered to be a very low risk thyroid cancer (7). PTMC is often considered an inert tumor with a favorable prognosis, and several clinical studies have confirmed the stability of PTMC (8). The American Thyroid Association (ATA), the British Thyroid Association, and the European Society for Medical Oncology recommend regular follow-up for low-risk PTMC, which does not require immediate surgery because of its good prognosis (9–11). One study reported a 20-year survival rate of 99% for PTMC (8). Sugitani et al. (12) analyzed 415 asymptomatic patients with PTMC for up to 22 years of follow-up and showed that only 6% of the nodules increased in size, 91% did not change, and 3% showed shrinkage. Similarly, Professor Ito in Japan reported (13) that 1,235 patients with low risk PTMC treated with observational therapy did not develop distant metastases from thyroid cancer and none of the patients died from PTMC over a period of 1.5–19 years. Although the prevailing treatment remains surgery (14–16), some patients are not eligible for surgery because of systemic disease. Furthermore, surgery may lead to recurrent laryngeal nerve paralysis, hypothyroidism, neck scarring, and lifelong medication dependency (17–20). In addition, surgical treatment has the potential to lead to overtreatment of PTMCs. The 2015 ATA guidelines suggest that patients with low risk PTMCs can also be actively monitored (15); however, some patients are unable to undergo long-term follow-up because of anxiety about the disease, and in these cases, ablation of PTMC is a compromise between surgery and observation. A multicenter PTMC ablation study conducted in China that included 11 centers and 725 patients (21) showed a significant reduction in tumor size at 6 months after ablation compared with that before ablation. On ultrasound, 515 (71.0%) PTMCs disappeared completely. Six (0.8%) patients showed disease progression after ablation, including five (0.7%) patients with new PTMCs and one (0.1%) patient with metastasis in the cervical lymph nodes. Increasing evidence supports that RFA, LA, and MWA can effectively treat PTMC with satisfactory clinical results (Table 1).
RFA
RFA is a treatment method that introduces electrodes into the lesion area to generate thermal effects by releasing radiofrequency currents, thereby achieving a high local temperature and inducing solidified necrosis and tissue degeneration. RFA is widely used in the treatment of solid tumors, and it has been applied in PTMC since 2016, when RFA was used to ablate 98 PTMCs in 92 patients in China (22). The results of the study showed a 100% volume reduction rate (VRR) at a follow-up of 18 months, with no tumor recurrence or metastasis during the follow-up period. Ultrasound-guided core needle biopsy (CNB) histopathology confirmed the lack of residual tumor or recurrence. The same group then conducted a clinical study with a larger sample size (23) in which RFA was performed on 204 cases of PTMC. The nodules disappeared completely after 24 months of follow-up, the VRR was 100%, and there were only nine cases of mild complications. In 2019 (24), a retrospective analysis of the safety, effectiveness, and long-term efficacy of RFA treatment was performed including 38 PTMC nodules in 37 patients, and similar results were obtained. In addition to studies in China, Korean scholars (25) followed 133 PTMC patients who refused surgery and had a high-risk for surgery for 12 months after RFA; the results showed that 91.4% (139/152) of the tumors disappeared and all patients were free of recurrence and metastasis. The overall complication rate was 3%. PTMC is considered to be an inert cancer, and although some studies have shown complete ablation of RFA with no recurrence, this does not prove the importance of this intervention in the short term. Studies have thus increased the follow-up period and included a larger sample size. Cho et al. (26) reported complete disappearance rates of 98.8% and 100% at 24 and 60 months after RFA for PTMC, respectively, with no local tumor progression, lymph node metastasis, distant metastasis, delayed complications, surgery-related death, or delayed surgery. A 5-year retrospective study of RFA for PTMC was also conducted in China (27), and all nodes were completely absorbed at the end of follow-up, with only 2 patients developing ipsilateral lateral cervical lymph node metastasis. These studies confirm the effectiveness and safety of RFA for the treatment of PTMC.
MWA
Compared with RFA, MWA is a relatively new technique that has been widely used for ablation of various benign and malignant tumors, including benign thyroid tumors (28–30). MWA provides a larger ablation area than RFA, which decreases the time necessary to complete treatment and improves tumor inactivation. MWA is thus less susceptible to heat sink effects. The heat sink effect is an important factor leading to local tumor recurrence after RFA (31, 32), which has increased interest in the MWA technique. The first study of 21 patients with PTMC treated with MWA was conducted and reported in China in 2014 (33). The patients were followed-up for 11 months, and no recurrence or metastasis was detected. Eight of the patients underwent ultrasound-guided biopsy, and the pathology results showed no signs of recurrence; four patients recovered in a short period of time after suffering from hoarseness. Teng et al. used low power MWA (34) to treat 15 patients with a total of 21 nodules. After a follow-up period of 3 years, 20 nodules completely resolved without recurrence. However, studies to date have included a small number of cases and a short follow-up time. The long-term effectiveness and safety of MWA were examined in a study that analyzed 41 cases of PTMC (35); after 60 months of follow-up, the nodule reduction rate was 99.37% ± 4.02%, and no tumor progression was detected during the follow-up period. Yue et al. (36) and Teng DK et al. (37) followed 119 and 185 patients for 2 years after MWA and showed complete absorption rates of 93.9% and 84.5%, respectively; in the former study, one patient developed cervical lymph node metastasis at 26 months of follow-up and underwent successful MWA treatment; in the latter study, only minor complications were observed.
Lu et al. (38) evaluated patients using ultrasonography for up to 24 months after treatment and showed a nodule disappearance rate of 100%. This study performed fine needle aspiration biopsy (FNAB) or CNB of the ablated areas at 3 or 6 months after treatment, and the results showed no atypical or malignant follicular cells by pathological histology. The most common pathological features were fibroblast proliferation (87.18%) and chronic inflammation (82.05%), followed by infarction (53.85%).
LA
Although most of the ablations for low risk PTMC are currently performed by WMA and RFA, another type of thermal ablation, LA, has achieved some efficacy in the treatment of certain systemic tumors. Apini et al. reported (39) a case of a patient with a PTMC of approximately 8 mm in diameter in the thyroid gland that was found on examination due to cirrhotic decompensation combined with renal failure. The patient was treated with LA. FNAB and CNB were performed at 1 and 12 months after PLA, which detected necrotic material and inflammatory cells but no living tumor cells. The nodule was recurrence-free and continued to shrink at 24 months after treatment. Since then, LA has been used for thyroid cancer ablation. Another scholar reported three cases of PTMC treated with LA in 2014 (40). In 2020, an Italian study (41) reported the results of RFA and LA in 11 patients; all patients were free of recurrence and metastasis after surgery; three patients experienced minor postoperative discomfort, which resolved with medication; there were no complications, and patients had a satisfaction score of 10.
A special study on LA was conducted in China (42) including 105 cases of pathologically confirmed solitary PTMC treated with ultrasound-guided LA at Xiangya III Hospital of Central South University. The mean follow-up was >5 years, and the results showed a 100% nodal disappearance rate at 24 months after ablation with no serious complications such as tracheal, esophageal, vascular, or laryngeal nerve injury. Cervical lymph node metastasis occurred in two patients. In 2017, Ruijin Hospital of Shanghai Jiaotong University reported 30 patients treated with LA; at the final follow-up, 10 ablation areas (33.3%) disappeared and 20 ablation areas (66.67%) remained as scar-like lesions, with no post-treatment tumor regrowth detected (43). Institutional studies of cases treated with LA for longer periods were also reported. Kim et al. (44) followed 90 patients for up to 10 years after PTMC ablation and showed a 100% disappearance rate of nodules by 12 months of follow-up. However, after 17–56 months of treatment, five patients (5.5%) developed a new cancerous lesion and one case of lymph node metastasis was found at 2 months after treatment, which was eventually determined to be an undetected cancer site rather than a recurrence. All recurrent patients were treated surgically and remained recurrence-free for 5 years. Ji et al. investigated the effectiveness of ultrasound-guided percutaneous LA for PTMC (45) and achieved similar results. Regarding the pathological features after LA treatment, three cases of thyroid cancer with total thyroidectomy immediately after LA treatment were reported (40), and the pathology showed tissue destruction and charring, complete loss of the entire ablated area and margins of normal tissue surrounding the tumor, and expression of TTF1 and anti-mitochondrial antibodies indicating lack of viability. However, lymph node micrometastases were found in one of the cases. Therefore, the investigators concluded that LA for PTMC should only be used in a subset of designated patients at this stage. In addition, they indicated LA technology may become the first choice for PTMC in the future when precise identification of microlesions in the thyroid and lymph nodes is achieved.
A systematic review of the three methods (RFA/WMA/LA) (46) was performed including 1,187 patients and 1,284 PTMCs, and the results showed that the volume of PTMC was significantly reduced after ablation with all three techniques. MWA was more effective than the other two techniques, but the difference was not statistically significant. There was no difference between the three techniques in terms of complications and recurrence. A meta-analysis also found that LA treatment was less effective for PTMC reduction (47), but the authors concluded that all three techniques are effective and safe for PTMC ablation and can be used as an alternative to surgery in some cases.
A Comparative Study of Thermal Ablation Versus Surgical Procedures
The main treatment for PTMC remains surgical resection; however, thermal ablation has been shown to benefit patients with PTMC as an alternative to surgery. Several studies have been conducted to compare the two treatment modalities (48–53), thermal ablation and surgery, and the results show that thermal ablation has comparable efficacy to surgery in the treatment of PTMC. A meta-analysis including 339 thermal ablation and 314 surgical patients (54) showed no statistically significant differences in the rates of local tumor recurrence, lymph node metastasis, distant metastasis, and salvage surgery between surgery and ablation. In a long-term follow-up study (27), two patients treated with thermal ablation developed ipsilateral cervical lymph node metastases; however, a study by Myung et al. (55) showed a recurrence rate of 1.4% in patients followed for 5–6 years after surgery. By contrast, ablation does not affect the prognosis of patients treated with or without surgery, and it preserves at least one side of the thyroid gland in most patients. In a related meta-analysis (56), the incidence of temporary laryngeal recurrent nerve injury after thyroidectomy and total thyroidectomy was 10.1 and 8.1%, respectively, and permanent hypocalcemia occurred in 2.8% and 3.3% of patients. In addition, these patients had permanent surgical scarring in the neck, as well as a decrease in QoL because of the need for lifelong medication. RFA treatment can prevent these complications. Another meta-analysis of seven studies including 867 patients (57) showed that thermal ablation is effective for reducing patient complications and decreasing the length of hospital stay, and it is a relatively safe and cost-effective option for the treatment of PTMC.
Ablation of PTC (Nodule Diameter >1 cm)
Although the use of thermal ablation in the treatment of PTMC is currently in the clinical research stage, advances in technology and the effectiveness and safety of this technique have led scholars to conduct studies on thyroid tumors >1 cm in diameter. In 2020, the Chinese People’s Liberation Army General Hospital (58) performed RFA in 66 patients with T1bN0M0 PTC (all refused or were unsuitable for surgery), and the results of the study showed a technical success rate of 100% with no major complications. There was a significant reduction in tumor volume. At the final follow-up, the tumor VRR was 99.11 ± 2.44% (range 92.62%–100%), and 38 cases (57.6%) showed disappearance of tumors. Puncture results at 3 or 6 months after ablation showed malignant cells in two lesions (3.0%) and cervical lymph node metastasis in one case (1.5%). Cao et al. (53) performed RFA and MWA in patients with T1N0M0 PTC who volunteered for ablation or were not suitable for surgical treatment. During a mean follow-up of 22 months, the nodule disappearance rate, the disease progression, and the complication rates were higher in the T1b group than in the T1a group; however, thermal ablation showed effectiveness and safety for T1N0M0 PTC. Studies comparing the efficacy and safety of RFA treatment and surgical resection in patients with T1bN0M0 PTC belonging to different age groups (59) showed that RFA was more cost effective and associated with a shorter operative time than the surgical group, but there was no significant difference in tumor progression and complication rates. In addition, subgroup analyses of patients older than forty-five years and patients younger than forty-five years showed no significant differences in the incidence of tumor progression and complications. Hospitalization costs were higher in older patients than in younger patients in the surgical group, whereas no difference was observed in the RFA group. Ablation of stage T1b thyroid cancer has not been assessed clinically on a large scale, therefore, it cannot be used as an alternative to surgery; however, it has been a local clinical treatment preference for patients who lack indications for surgery.
Complications
The main complications of thermal ablation of thyroid cancer are pain, voice changes, bleeding, and changes in thyroid function. Patients have widespread pain after ablation, with a 100% incidence of postoperative pain demonstrated by Zhou (43), Song (52), and Wang (60). Although criteria for assessing postoperative pain are difficult to establish, the duration of pain was short in all studies, and pain relief occurred within 1 week postoperatively. Hoarseness is one of the most common complications of thermal ablation. The heat generated by RFA or MWA during ablation causes transient damage to the recurrent laryngeal nerve, and some patients experience voice changes, with an incidence of hoarseness of 0%–3.57% and a recovery time of approximately 10 min–6 months (21–27, 33–37, 41–45, 48–54, 58, 59, 61–77). One patient with permanent voice change as a complication was reported. In addition, the rich blood supply to the thyroid gland can lead to transient bleeding at the end of the ablation, although this can be relieved with compression. Finally, a small number of patients experience complications such as altered thyroid function (24, 27, 49, 50, 60, 77) and cough (21, 36, 45) after thermal ablation, which normally resolve during the postoperative period.
Recurrence
Recurrence and metastasis after ablative treatment of PTC are major concerns for researchers and clinicians as well as patients. Thermal ablation is a new medical technology and there are many uncertainties. Studies including small sample sizes have shown that a fraction of patients have no recurrence and metastasis (22, 33, 34, 43, 49, 60–62), whereas another fraction of patients experience lymph node metastasis and tumor recurrence (24–27, 42, 52, 58, 69, 76). However, the small sample size of these studies makes it difficult to draw consistent conclusions. A study of unifocal low-risk PTMC that included a large sample showed an overall incidence of local tumor progression of 3.62% at a follow-up time of 42.15 ± 11.88 months (range, 24–69 months) (72). One patient (0.24%) was diagnosed with residual cancer, 4 (0.97%) had lymph node metastasis, and 10 (2.42%) had recurrent PTMC. Of the 10 patients who recurred, one opted for active surveillance and showed stable volume at the 1-year follow-up. Nine patients received additional RFA treatment. All lesions were successfully treated and disappeared at follow-up in seven cases, and no distant metastases were detected. In addition, 70% of recurrent PTMC in this study occurred in the contralateral glandular lobe, which could suggest that thyroid lobectomy does not prevent recurrence of low-risk PTMC. A controlled study of 884 patients comparing surgery versus ablation (74) showed no significant differences between the surgical and RFA groups in terms of local tumor progression (9/460 [2.0%] vs. 15/424 [3.5%], P = 0.148), LNM (3/460 [0.7%] vs. 4/424 [0.9%], P = 0.914), recurrent PTMC (6/460 [1.3%] vs. 10/424 [2.4%], P = 0.240) and persistent lesions (0/460 [0%] vs. 1/424 [0.2%], P = 0.298). Recurrence was assessed based on relevant imaging examinations at the time of patient follow-up; however, some patients underwent CNB of the ablated central zone, peripheral zone, and surrounding thyroid parenchyma at 3 or 6 months after ablation to assess tumor recurrence (65). The results showed that in 202 patients with low risk PTMC who underwent CNB assessment after ablation, three ablation areas in the peripheral region showed positive biopsy results for CNB. However, early judgment of recurrence could be made when ultrasound images failed to identify CNB but biopsy could. Another study (73) investigated unifocal PTMC and found residual peripheral tumor tissue after CNB puncture, in two patients who subsequently underwent re-RFA.
Factors Influencing the Effectiveness and Safety of PTC ablation Therapy
PTC Near the Capsule of the Thyroid Gland
Whether ablation of PTCs located near the thyroid capsule is feasible remains to be determined. The expert consensus on thyroid ablation of the 2019 edition of the Chinese Medical Doctor Association (69) states that the nodule diameter needs to be <5 mm when performing ablation, but the diameter can be 10 mm if the PTC is located near the thyroid capsule. The association of nodules close to the capsule with the risk of metastasis and recurrence remains controversial. A study that included 174 patients (78) showed that the location of nodules within 1.9 mm of the thyroid capsule is associated with increased risk of lymph node metastasis. Another study (79) showed that a shorter distance between the nodule and the thyroid capsule was associated with a higher likelihood of metastasis. In contrast, a study that included 1,922 patients (80) showed that the distance of the tumor from the thyroid capsule was not associated with lymph node metastasis. Therefore, whether the distance between thyroid tumors and the thyroid capsule is related to lymph node metastasis has not been conclusively established, and whether nodes closer to the thyroid capsule should be ablated needs to be further investigated. A clinical study was conducted to answer this question (69). The study included 71 patients with PTC 0–2 mm from the thyroid capsule. The investigators performed PTC ablation and thyroid capsule ablation with a 25 ± 11 month follow-up, and the results showed that all nodules disappeared during the follow-up period, and the incidence of lymph node metastasis and new tumors was 1.9% (2/106). Although the study showed that thermal ablation is safe and feasible for nodes close to the capsule, the safety and efficacy of thermal ablation of nodes close to the capsule needs to be investigated in additional large-sample multicenter studies.
PTC Located in the Isthmus of the Thyroid Gland
Approximately 39.2% of PTCs are located in the isthmus of the thyroid gland, and there are no definitive guidelines regarding the treatment of PTCs in the isthmus (81). Similarly, the expert consensus on thyroid cancer ablation developed by the Chinese Medical Doctor Association clearly states that cancer located in the thyroid isthmus is a contraindication to ablation (69). The isthmus is a flattened gland that is close to the anterior cervical musculature and the trachea, therefore thermal ablation is not indicated because ablation could damage the surrounding tissues if not performed properly. However, whether PTC in the thyroid isthmus is an absolute contraindication to thermal ablation remains unclear. A clinical study enrolled 112 patients with PTC in the isthmus of the thyroid gland to analyze the effect of ablation treatment (82). The results showed that at 18 months after the procedure, the nodules disappeared at a rate of 100% and were even completely absorbed at 1 month after the procedure, although one patient had a recurrence at 7 months after the procedure. The study demonstrated the effectiveness of the thermal ablation technique in the treatment of isthmic nodules. Next, the same group compared thermal ablation with surgery in the treatment of thyroid isthmus nodules (52). There was no metastasis or recurrence except for one patient in the RFA group who recurred. However, the operative time, bleeding, hospital stay, and treatment cost were higher in the surgical group than in the RFA group, and the THYCA-QOL score was significantly higher in the RFA group than in the surgical group. Although ablative treatment for thyroid isthmus nodules has not been reported extensively, the current study shows that thermal ablation can lead to a significant improvement in the postoperative QoL of patients and is an alternative to surgery for PTC in the isthmus.
Age
Although there are indicators or models that can definitively predict issues such as the progression of PTC, age is the only independent prognostic factor affecting thyroid cancer-related mortality (83). Many studies have used 45 years as the cut-off point for staging (84–86). The 5-year survival rate of 65-year-old patients with PTMC who were not treated with surgery is 23% (87).. A clinical study analyzed the outcome and safety of PTMC thermal ablation in patients >55 years of age (68). The results showed that all nodules were completely ablated and the VPR at the last follow-up was 99.78 ± 1.54%; there were no serious complications. One patient developed lymph node metastasis and one had a recurrence, and all were treated with a second RFA with satisfactory results. From the perspective of treatment modality, older patients have more systemic underlying diseases and are at a greater risk of complications from general anesthesia during surgical procedures. In contrast, ablation techniques commonly use local infiltration anesthesia, which is associated with fewer complications and is safer. A comparison of the efficacy and safety of RFA and surgical resection in patients with T1bN0M0 PTC >45 years of age (59) showed that the prognosis was similar in both groups; however, the overall cost and complications were lower in the ablation group, indicating that RFA may be an effective and safe alternative to surgery for the treatment of patients with T1bN0M0 PTC. The effect of age on the results of thermal ablation needs to be validated over a longer period of time and in larger studies.
Chronic Lymphocytic Thyroiditis (CLT)
CLT is an autoimmune disease characterized by extensive infiltration, fibrosis, and atrophy of the thyroid parenchyma. Approximately 33.3% of PTC cases are associated with CLT (88), and that the coexistence of PTC and CLT is strongly associated with prognosis, lymph node metastasis, and distant metastasis and recurrence rates (89). A study assessing the effect of CLT on the efficacy and safety of thermal ablation in PTMC patients (90) showed that the safety and therapeutic outcomes were not different from those of patients undergoing PTMC alone after ablative treatment for more than 20–48 months. The authors concluded that this study provided a basis for studying the mechanisms of immunomodulation induced by necrosis in thyroid cancer.
Number of PTCs
The current indications for thyroid cancer ablation studies are limited to solitary PTMC. Multiple PTMCs are divided into unilateral glandular lobe with multiple PTMCs and bilateral glandular lobe with at least one nodule, and the incidence of bilateral PTMC is 10%–30% (91). The main treatment for bilateral PTMC is surgery because bilateral PTMC is considered a high risk factor for tumor recurrence (92, 93). However, studies indicate that bilateral lesions are not associated with an increased risk of recurrence (91). Therefore, this issue remains controversial. According to the 8th AJCC/TNM Mortality Risk System and ATA Risk Stratification (14, 94), bilateral PTMC is classified as stage I with a low risk of recurrence. The safety and efficacy of RFA for bilateral PTMC was analyzed in 47 cases (75). The results showed a complete disappearance rate of 92%, but recurrence was observed in two patients. This study demonstrated the safety and efficacy of RFA for the treatment of bilateral PTMC, and the authors concluded that RFA holds promise as an alternative treatment in patients with bilateral PTMC who are not eligible for surgery. In a study by Teng et al. (37), ablation was performed in 18 patients with two or more tumors, but was not reported separately. A recent study included 55 patients with multifocal PTMC and 432 patients with PTMC alone, and a comparative study was performed (76). After 49.25 ± 12.98 months of follow-up, there were no significant differences in VRR, local tumor progression, and recurrence and metastasis rates. The authors concluded that RFA is a promising treatment method after adequate preoperative evaluation.
Quality of Life After Ablation in Patients With PTC
Due to the specificity of thyroid cancer treatment, the QoL of patients after treatment has become an essential and important part of the treatment process. The SF-36 scale and thyroid cancer-specific health-related QoL (HRQoL) questionnaire were administered to 100 PTMC patients after treatment (95). The results showed that the main risk factors affecting QoL in patients with PTMC after ultrasound-guided RFA were female gender, psychological burden, inattention, and neuromuscular system and pharyngeal/oral symptoms. Therefore, preoperative examinations are necessary to assess related symptoms, and psychological intervention should be provided after RFA to improve the QoL of PTMC patients after treatment. A study comparing QoL after surgery and PTMC (96) included 54 patients in the PTMC group and 34 patients in the surgical group. The patients were scored on HRQoL using the 36-item Health Short Form Questionnaire (SF-36), Thyroid Cancer Specific Quality of Life, and Fear of Progression Short Form Questionnaire, and the results showed that ultrasound-guided PTMC ablation treatment was superior to surgery in terms of HRQoL, indirectly suggesting that the ablation patients had a higher postoperative QoL than the surgical group.
Conclusions
The treatment options for thermal ablation of PTC are still controversial. A growing number of researchers have demonstrated the safety and efficacy of thermal ablation with longer follow-up periods and larger sample sizes. Finally, it is hoped that thermal ablation technology will truly benefit patients with PTC.
After reviewing so many studies, it seems to me that for T1aN0M0 PTC ablation techniques are well established and can achieve essentially the same efficacy and fewer number of complications as surgery during clinical treatment. Several academics are already focusing their research on PTC of T1bN0M0, and I think this will be a focus of future research.
Author Contributions
The three authors collected the information together, CC and DO organized and wrote the article, and DX guide the content and writing of the article. DO and CC contributed equally to this work. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the National Natural Science Foundation of China (NO.82071946), National Natural Science Foundation of China (NO.81871370), Zhejiang Province Science and Technology Plan of Traditional Chinese Medicine (NO.2020ZB033).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hershman JM. Trends in Thyroid Cancer Incidence and Mortality in the United States. Clin Thyroidol (2017) 29:221–3. doi: 10.1089/ct.2017;29.221-223
2. Wiltshire JJ, Drake TM, Uttley L, Balasubramanian SP. Systematic Review of Trends in the Incidence Rates of Thyroid Cancer. Thyroid (2016) 26(11):1541–52. doi: 10.1089/thy.2016.0100
3. La Vecchia C, Malvezzi M, Bosetti C, Garavello W, Bertuccio P, Levi F, et al. Thyroid Cancer Mortality and Incidence: A Global Overview. Int J Cancer (2015) 136(9):2187–95. doi: 10.1002/ijc.29251
4. Schneider DF, Chen H. New Developments in the Diagnosis and Treatment of Thyroid Cancer. CA A Cancer J Clin (2013) 63(6):373–94. doi: 10.3322/caac.21195
5. Ahn HS, Kim HJ, Welch HG. Korea's Thyroid-Cancer “Epidemic”–Screening and Overdiagnosis. N Engl J Med (2014) 371(19):1765–7. doi: 10.1056/NEJMp1409841
6. Lohia S, Hanson M, Tuttle RM, Morris LGT. Active Surveillance for Patients With Very Low-Risk Thyroid Cancer. Laryngoscope Invest Otolaryngol (2020) 5:175–82. doi: 10.1002/lio2.356
7. Zafon C, Baena JA, Castellví J, Obiols G, Monroy G, Mesa J. Differences in the Form of Presentation Between Papillary Microcarcinomas and Papillary Carcinomas of Larger Size. J Thyroid Res (2010) 2011:639156. doi: 10.4061/2011/639156
8. Brito JP, Hay ID, Morris JC. Low Risk Papillary Thyroid Carcinoma. BMJ (2014) 348(jun16 9):g3045–5. doi: 10.1136/bmj.g3045
9. Haugen BR. 2015 American Thyroid Association Management Guidelines for Adult Patients With Thyroid Nodules and Differentiated Thyroid Cancer: What is New and What has Changed? Cancer (2017) 123(3):372–81. doi: 10.1002/cncr.30360
10. Filetti S, Durante C, Hartl D, Leboulleux S, Locati LD, Newbold K, et al. Thyroid Cancer: ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up†. Ann Oncol (2019) 30(12):1856–83. doi: 10.1093/annonc/mdz400
11. Perros P, Boelaert K, Colley S, Evans C, Evans RM, Gerrard G, et al. Guidelines for the Management of Thyroid Cancer. Clin Endocrinol, 2nd (2014) 81:1–122.
12. Sugitani I, Fujimoto Y, Yamada K. Association Between Serum Thyrotropin Concentration and Growth of Asymptomatic Papillary Thyroid Microcarcinoma. World J Surg (2014) 38(3):673–8. doi: 10.1007/s00268-013-2335-8
13. Ito Y, Miyauchi A, Kihara M, Higashiyama T, Kobayashi K, Miya A. Patient Age is Significantly Related to the Progression of Papillary Microcarcinoma of the Thyroid Under Observation. Thyroid Off J Am Thyroid Assoc (2014) 24(1):27. doi: 10.1089/thy.2013.0367
14. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. : 2015 American Thyroid Association Management Guidelines for Adult Patients With Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid (2016) 26(1):1–133. doi: 10.1089/thy.2015.0020
15. Gharib H, Papini E, Paschke R, Duick DS, Vitti P. American Association of Clinical Endocrinologists, American College of Endocrinology, and Assosiazione Medici Endocrinologi Medical Guidelines for Clinical Practice for the Diagnosis and Managment of Thyroid Nodules–2016 Update. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol (2016) 22(5):622–39. doi: 10.4158/EP161208.GL
16. Pacini F. European Consensus for the Management of Patients With Differentiated Thyroid Carcinoma of the Follicular Epithelium. Eur J Endocrinol (2006) 154(6):787. doi: 10.1530/eje.1.02158
17. Gharib H. Changing Trends in Thyroid Practice: Understanding Nodular Thyroid Disease. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol (2004) 10(1):31. doi: 10.4158/EP.10.1.31
18. Rafferty MA, Goldstein DP, Rotstein L, Asa SL, Panzarella T, Gullane P, et al. Completion Thyroidectomy Versus Total Thyroidectomy: Is There a Difference in Complication Rates? An Analysis of 350 Patients. J Am Coll Surg (2007) 205(4):602–7. doi: 10.1016/j.jamcollsurg.2007.05.030
19. Linos D, Economopoulos KP, Kiriakopoulos A, Linos E, Petralias A. Scar Perceptions After Thyroid and Parathyroid Surgery: Comparison of Minimal and Conventional Approaches. Surgery (2013) 153(3):400–7. doi: 10.1016/j.surg.2012.08.008
20. Lang HH, Lo CY. Total Thyroidectomy for Multinodular Goiter in the Elderly. Am J Surg (2005) 190(3):418–23. doi: 10.1016/j.amjsurg.2005.03.029
21. Cao XJ, Yu MA, Zhu YL, Qi L, Cong ZB, Yan GZ, et al. Ultrasound-Guided Thermal Ablation for Papillary Thyroid Microcarcinoma: A Multicenter Retrospective Study. Int J Hyperthermia (2021) 38(1):916–22. doi: 10.1080/02656736.2021.1936218
22. Zhang M, Luo Y, Zhang Y, Tang J. Efficacy and Safety of Ultrasound-Guided Radiofrequency Ablation for Treating Low-Risk Papillary Thyroid Microcarcinoma: A Prospective Study. Thyroid (2016) 26(11):1581–7. doi: 10.1089/thy.2015.0471
23. Wu R, Luo Y, Tang J, Yang M, Li J, Zhang Y, et al. Ultrasound-Guided Radiofrequency Ablation for Papillary Thyroid Microcarcinoma: A Retrospective Analysis of 198 Patients. Int J Hyperthermia (2020) 37(1):168–74. doi: 10.1080/02656736.2019.1708480
24. Ding M, Tang X, Cui D, Chi J, Shi Y, Wang T, et al. Clinical Outcomes of Ultrasound-Guided Radiofrequency Ablation for the Treatment of Primary Papillary Thyroid Microcarcinoma. Clin Radiol (2019) 74(9):712–7. doi: 10.1016/j.crad.2019.05.012
25. Lim HK, Cho SJ, Baek JH, Lee KD, Son CW, Son JM, et al. US-Guided Radiofrequency Ablation for Low-Risk Papillary Thyroid Microcarcinoma: Efficacy and Safety in a Large Population. Korean J Radiol (2019) 20(12):1653–61. doi: 10.3348/kjr.2019.0192
26. Cho SJ, Baek SM, Lim HK, Lee KD, Son JM, Baek JH. Long-Term Follow-Up Results of Ultrasound-Guided Radiofrequency Ablation for Low-Risk Papillary Thyroid Microcarcinoma: More Than 5-Year Follow-Up for 84 Tumors. Thyroid (2020) 30(12):1745–51. doi: 10.1089/thy.2020.0106
27. Zhu Y, Che Y, Gao S, Ren S, Tong M, Wang L, et al. Long-Term Follow-Up Results of PTMC Treated by Ultrasound-Guided Radiofrequency Ablation: A Retrospective Study. Int J Hyperthermia (2021) 38(1):1225–32. doi: 10.1080/02656736.2021.1963850
28. Li X, Fan WJ, Zhang L, Zhang XP, Jiang H, Zhang JL, et al. CT-Guided Percutaneous Microwave Ablation of Liver Metastases From Nasopharyngeal Carcinoma. J Vasc Interv Radiol (2013) 24(5):680–4. doi: 10.1016/j.jvir.2013.02.005
29. Liang P, Wang Y, Zhang D, Yu X, Gao Y, Ni X. Ultrasound Guided Percutaneous Microwave Ablation for Small Renal Cancer: Initial Experience. J Urol (2008) 180(3):844–8. doi: 10.1016/j.juro.2008.05.012
30. Wang Y, Liang P, Yu X, Cheng Z, Yu J, Dong J. Ultrasound-Guided Percutaneous Microwave Ablation of Adrenal Metastasis: Preliminary Results. Int J Hyperthermia (2009) 25(6):455–61. doi: 10.1080/02656730903066608
31. Qian GJ, Wang N, Shen Q, Sheng YH, Zhao JQ, Kuang M, et al. Efficacy of Microwave Versus Radiofrequency Ablation for Treatment of Small Hepatocellular Carcinoma: Experimental and Clinical Studies. Eur Radiol (2012) 22(9):1983–90. doi: 10.1007/s00330-012-2442-1
32. Dodd GD 3rd, Dodd NA, Lanctot AC, Glueck DA. : Effect of Variation of Portal Venous Blood Flow on Radiofrequency and Microwave Ablations in a Blood-Perfused Bovine Liver Model. Radiology (2013) 267(1):129–36. doi: 10.1148/radiol.12120486
33. Yue W, Wang S, Yu S, Wang B. Ultrasound-Guided Percutaneous Microwave Ablation of Solitary T1N0M0 Papillary Thyroid Microcarcinoma: Initial Experience. Int J Hyperthermia (2014) 30(2):150–7. doi: 10.3109/02656736.2014.885590
34. Teng D, Sui G, Liu C, Wang Y, Xia Y, Wang H. Long-Term Efficacy of Ultrasound-Guided Low Power Microwave Ablation for the Treatment of Primary Papillary Thyroid Microcarcinoma: A 3-Year Follow-Up Study. J Cancer Res Clin Oncol (2018) 144(4):771–9. doi: 10.1007/s00432-018-2607-7
35. Teng DK, Li WH, Du JR, Wang H, Yang DY, Wu XL. Effects of Microwave Ablation on Papillary Thyroid Microcarcinoma: A Five-Year Follow-Up Report. Thyroid (2020) 30(12):1752–8. doi: 10.1089/thy.2020.0049
36. Yue WW, Qi L, Wang DD, Yu SJ, Wang XJ, Xu HX, et al. US-Guided Microwave Ablation of Low-Risk Papillary Thyroid Microcarcinoma: Longer-Term Results of a Prospective Study. J Clin Endocrinol Metab (2020) 105(6):dgaa128. doi: 10.1210/clinem/dgaa128
37. Teng DK, Li HQ, Sui GQ, Lin YQ, Luo Q, Fu P, et al. Preliminary Report of Microwave Ablation for the Primary Papillary Thyroid Microcarcinoma: A Large-Cohort of 185 Patients Feasibility Study. Endocrine (2019) 64(1):109–17. doi: 10.1007/s12020-019-01868-2
38. Lu C, Li X, Chu X, Li R, Li J, Wang J, et al. Clinical Effects of Microwave Ablation in the Treatment of Low-Risk Papillary Thyroid Microcarcinomas and Related Histopathological Changes. Front Endocrinol (Lausanne) (2021) 12:751213. doi: 10.3389/fendo.2021.751213
39. Papini E, Guglielmi R, Gharib H, Misischi I, Graziano F, Chianelli M, et al. Ultrasound-Guided Laser Ablation of Incidental Papillary Thyroid Microcarcinoma: A Potential Therapeutic Approach in Patients at Surgical Risk. Thyroid (2011) 21(8):917–20. doi: 10.1089/thy.2010.0447
40. Valcavi R, Piana S, Bortolan GS, Lai R, Barbieri V, Negro R. Ultrasound-Guided Percutaneous Laser Ablation of Papillary Thyroid Microcarcinoma: A Feasibility Study on Three Cases With Pathological and Immunohistochemical Evaluation. Thyroid (2013) 23(12):1578–82. doi: 10.1089/thy.2013.0279
41. Mauri G, Orsi F, Carriero S, Della Vigna P, De Fiori E, Monzani D, et al. Image-Guided Thermal Ablation as an Alternative to Surgery for Papillary Thyroid Microcarcinoma: Preliminary Results of an Italian Experience. Front Endocrinol (Lausanne) (2020) 11:575152. doi: 10.3389/fendo.2020.575152
42. Peng K, Zhou P, Liu W. Long-Term Efficacy of Ultrasound-Guided Percutaneous Laser Ablation for Low-Risk Papillary Thyroid Microcarcinoma: A 5-Year Follow-Up Study. BioMed Res Int (2021) 2021:6616826. doi: 10.1155/2021/6616826
43. Zhou W, Jiang S, Zhan W, Zhou J, Xu S, Zhang L. Ultrasound-Guided Percutaneous Laser Ablation of Unifocal T1N0M0 Papillary Thyroid Microcarcinoma: Preliminary Results. Eur Radiol (2017) 27(7):2934–40. doi: 10.1007/s00330-016-4610-1
44. Kim HJ, Chung SM, Kim H, Jang JY, Yang JH, Moon JS, et al. Long-Term Efficacy of Ultrasound-Guided Laser Ablation for Papillary Thyroid Microcarcinoma: Results of a 10-Year Retrospective Study. Thyroid (2021) 31(11):1723–9. doi: 10.1089/thy.2021.0151
45. Ji L, Wu Q, Gu J, Deng X, Zhou W, Fan X, et al. Ultrasound-Guided Percutaneous Laser Ablation for Papillary Thyroid Microcarcinoma: A Retrospective Analysis of 37 Patients. Cancer Imaging (2019) 19(1):16. doi: 10.1186/s40644-019-0204-x
46. Tong M, Li S, Li Y, Li Y, Feng Y, Che Y. Efficacy and Safety of Radiofrequency, Microwave and Laser Ablation for Treating Papillary Thyroid Microcarcinoma: A Systematic Review and Meta-Analysis. Int J Hyperthermia (2019) 36(1):1278–86. doi: 10.1080/02656736.2019.1700559
47. Choi Y, Jung SL. Efficacy and Safety of Thermal Ablation Techniques for the Treatment of Primary Papillary Thyroid Microcarcinoma: A Systematic Review and Meta-Analysis. Thyroid (2020) 30(5):720–31. doi: 10.1089/thy.2019.0707
48. Zhang M, Tufano RP, Russell JO, Zhang Y, Zhang Y, Qiao Z, et al. Ultrasound-Guided Radiofrequency Ablation Versus Surgery for Low-Risk Papillary Thyroid Microcarcinoma: Results of Over 5 Years' Follow-Up. Thyroid (2020) 30(3):408–17. doi: 10.1089/thy.2019.0147
49. Li J, Liu Y, Liu J, Qian L. Ultrasound-Guided Percutaneous Microwave Ablation Versus Surgery for Papillary Thyroid Microcarcinoma. Int J Hyperthermia (2018) 34(5):653–9. doi: 10.1080/02656736.2018.1453092
50. Zhou W, Ni X, Xu S, Zhang L, Chen Y, Zhan W. Ultrasound-Guided Laser Ablation Versus Surgery for Solitary Papillary Thyroid Microcarcinoma: A Retrospective Study. Int J Hyperthermia (2019) 36(1):897–904. doi: 10.1080/02656736.2019.1649475
51. Xu B, Zhou NM, Cao WT, Gu SY. Comparative Study on Operative Trauma Between Microwave Ablation and Surgical Treatment for Papillary Thyroid Microcarcinoma. World J Clin cases (2018) 6(15):936–43. doi: 10.12998/wjcc.v6.i15.936
52. Song Q, Gao H, Ren L, Tian X, Lan Y, Yan L, et al. Radiofrequency Ablation Versus Total Thyroidectomy in Patients With Papillary Thyroid Microcarcinoma Located in the Isthmus: A Retrospective Cohort Study. Int J Hyperthermia (2021) 38(1):708–14. doi: 10.1080/02656736.2021.1916625
53. Cao XJ, Wang SR, Che Y, Liu J, Cong ZB, He JF, et al. Efficacy and Safety of Thermal Ablation for Treatment of Solitary T1N0M0 Papillary Thyroid Carcinoma: A Multicenter Retrospective Study. Radiology (2021) 300(1):209–16. doi: 10.1148/radiol.2021202735
54. Kim HJ, Cho SJ, Baek JH. Comparison of Thermal Ablation and Surgery for Low-Risk Papillary Thyroid Microcarcinoma: A Systematic Review and Meta-Analysis. Korean J Radiol (2021) 22(10):1730–41. doi: 10.3348/kjr.2020.1308
55. Lee MC, Kim MJ, Choi HS, Cho SW, Park DJ. Postoperative Thyroid-Stimulating Hormone Levels did Not Affect Recurrence After Thyroid Lobectomy in Patients With Papillary Thyroid Carcinoma. 2019 Endocrinol Metab (Seoul) (2019) 34:150–7. doi: 10.3803/EnM.2019.34.2.150
56. Li YJ, Wang YZ, Yi ZB, Chen LL, Zhou XD. Comparison of Completion Thyroidectomy and Primary Total Surgery for Differentiated Thyroid Cancer: A Meta-Analysis. Oncol Res Treat (2015) 38:528–31. doi: 10.1159/000440690
57. Shen K, Xue S, Xie Y, Wang H, Li J, Sun Y, et al. Et Al: Comparison of Thermal Ablation and Routine Surgery for the Treatment of Papillary Thyroid Microcarcinoma: A Systematic Review and Meta-Analysis. Int J Hyperthermia (2020) 37(1):913–24. doi: 10.1080/02656736.2020.1777331
58. Xiao J, Zhang M, Zhang Y, Yan L, Lan Y, Zhu Y, et al. Efficacy and Safety of Ultrasonography-Guided Radiofrequency Ablation for the Treatment of T1bN0M0 Papillary Thyroid Carcinoma: A Retrospective Study. Int J Hyperthermia (2020) 37(1):392–8. doi: 10.1080/02656736.2020.1752945
59. He H, Wu R, Zhao J, Song Q, Zhang Y, Luo Y. Ultrasound-Guided Radiofrequency Ablation Versus Surgical Resection for the Treatment of T1bN0M0 Papillary Thyroid Carcinoma in Different Age Groups. Front Endocrinol (Lausanne) (2021) 12:734432. doi: 10.3389/fendo.2021.734432
60. Wang X, Niu X, Mu S, Zhang M, Jiang W, Zhai L, et al. Analysis and Evaluation of the Efficacy of Ultrasound-Guided Microwave Ablation for Papillary Thyroid Microcarcinoma. Int J Hyperthermia (2021) 38:1476–85. doi: 10.1080/02656736.2021.1988152
61. Kim JH, Baek JH, Sung JY, Min HS, Kim KW, Hah JH, et al. Radiofrequency Ablation of Low-Risk Small Papillary Thyroidcarcinoma: Preliminary Results for Patients Ineligible for Surgery. Int J Hyperthermia (2017) 33(2):212–9. doi: 10.1080/02656736.2016.1230893
62. Zhang L, Zhou W, Zhan W, Peng Y, Jiang S, Xu S. Percutaneous Laser Ablation of Unifocal Papillary Thyroid Microcarcinoma: Utility of Conventional Ultrasound and Contrast-Enhanced Ultrasound in Assessing Local Therapeutic Response. World J Surg (2018) 42(8):2476–84. doi: 10.1007/s00268-018-4500-6
63. Li J, Liu Y, Liu J, Yang P, Hu X, Qian L. A Comparative Study of Short-Term Efficacy and Safety for Thyroid Micropapillary Carcinoma Patients After Microwave Ablation or Surgery. Int J Hyperthermia (2019) 36(1):640–6. doi: 10.1080/02656736.2019.1626492
64. Wang L, Xu D, Yang Y, Li M, Zheng C, Qiu X, et al. Safety and Efficacy of Ultrasound-Guided Percutaneous Thermal Ablation in Treating Low-Risk Papillary Thyroid Microcarcinoma: A Pilot and Feasibility Study. J Cancer Res Ther (2019) 15(7):1522–9. doi: 10.4103/jcrt.JCRT_214_19
65. Yan L, Luo Y, Zhang Y, Zhu Y, Xiao J, Lan Y, et al. The Clinical Application of Core-Needle Biopsy After Radiofrequency Ablation for Low-Risk Papillary Thyroid Microcarcinoma: A Large Cohort of 202 Patients Study. J Cancer (2020) 11(18):5257–63. doi: 10.7150/jca.42673
66. Zhou W, Ni X, Xu S, Zhang L, Chen Y, Zhan W. Ultrasound-Guided Laser Ablation Versus Microwave Ablation for Patients With Unifocal Papillary Thyroid Microcarcinoma: A Retrospective Study. Lasers Surg Med (2020) 52(9):855–62. doi: 10.1002/lsm.23238
67. Cao XJ, Liu J, Zhu YL, Qi L, Liu G, Wang HL, et al. Efficacy and Safety of Thermal Ablation for Solitary T1bN0M0 Papillary Thyroid Carcinoma: A Multicenter Study. J Clin Endocrinol Metab (2021) 106(2):e573–81. doi: 10.1210/clinem/dgaa776
68. He H, Song Q, Lan Y, Yan L, Xiao J, Zhang Y, et al. Efficacy and Safety of Ultrasound-Guided Radiofrequency Ablation for Low-Risk Papillary Thyroid Microcarcinoma in Patients Aged 55 Years or Older: A Retrospective Study. Int J Hyperthermia (2021) 38(1):604–10. doi: 10.1080/02656736.2021.1912416
69. Wu J, Zhao ZL, Cao XJ, Wei Y, Peng LL, Li Y, et al. A Feasibility Study of Microwave Ablation for Papillary Thyroid Carcinoma Close to the Thyroid Capsule. Int J Hyperthermia (2021) 38(1):1217–24. doi: 10.1080/02656736.2021.1962549
70. Xiao J, Zhang Y, Zhang M, Lan Y, Yan L, Luo Y, et al. Ultrasonography-Guided Radiofrequency Ablation vs. Surgery for the Treatment of Solitary T1bN0M0 Papillary Thyroid Carcinoma: A Comparative Study. Clin Endocrinol (Oxf) (2021) 94(4):684–91. doi: 10.1111/cen.14361
71. Xiao J, Zhang Y, Zhang M, Xie F, Yan L, Luo Y, et al. Ultrasonography-Guided Radiofrequency Ablation for the Treatment of T2N0M0 Papillary Thyroid Carcinoma: A Preliminary Study. Int J Hyperthermia (2021) 38(1):402–8. doi: 10.1080/02656736.2021.1895332
72. Yan L, Lan Y, Xiao J, Lin L, Jiang B, Luo Y. Long-Term Outcomes of Radiofrequency Ablation for Unifocal Low-Risk Papillary Thyroid Microcarcinoma: A Large Cohort Study of 414 Patients. Eur Radiol (2021) 31(2):685–94. doi: 10.1007/s00330-020-07128-6
73. Yan L, Song Q, Xiao J, Zhang Y, Luo YK. [Value of Ultrasound-Guided Core-Needle Biopsy for Evaluating the Performance of Radiofrequency Ablation for Low-Risk Papillary Thyroid Microcarcinoma]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao (2021) 43(4):584–9. doi: 10.3881/j.issn.1000-503X.13277
74. Yan L, Zhang M, Song Q, Luo Y. Ultrasound-Guided Radiofrequency Ablation Versus Thyroid Lobectomy for Low-Risk Papillary Thyroid Microcarcinoma: A Propensity-Matched Cohort Study of 884 Patients. Thyroid 31:2021.01001. doi: 10.1089/thy.2021.0100
75. Yan L, Zhang M, Song Q, Xiao J, Zhang Y, Luo Y. The Efficacy and Safety of Radiofrequency Ablation for Bilateral Papillary Thyroid Microcarcinoma. Front Endocrinol (Lausanne) (2021) 12:663636. doi: 10.3389/fendo.2021.663636
76. Yan L, Zhang M, Song Q, Xie F, Luo Y. Clinical Outcomes of Radiofrequency Ablation for Multifocal Papillary Thyroid Microcarcinoma Versus Unifocal Papillary Thyroid Microcarcinoma: A Propensity-Matched Cohort Study. Eur Radiol (2021) 32(2):1–11. doi: 10.1007/s00330-021-08133-z
77. Zhang C, Yin J, Hu C, Ye Q, Wang P, Huang P. Comparison of Ultrasound Guided Percutaneous Radiofrequency Ablation and Open Thyroidectomy in the Treatment of Low-Risk Papillary Thyroid Microcarcinoma: A Propensity Score Matching Study. Clin Hemorheol Microcirc (2021) 80:1–9. doi: 10.3233/CH-201087
78. Seong CY, Chai YJ, Lee SM, Kim SJ, Choi JY, Lee KE, et al. Significance of Distance Between Tumor and Thyroid Capsule as an Indicator for Central Lymph Node Metastasis in Clinically Node Negative Papillary Thyroid Carcinoma Patients. PLoS One (2018) 13(7):e0200166. doi: 10.1371/journal.pone.0200166
79. Wang QC, Cheng W, Wen X, Li JB, Jing H, Nie CL. Shorter Distance Between the Nodule and Capsule has Greater Risk of Cervical Lymph Node Metastasis in Papillary Thyroid Carcinoma. Asian Pac J Cancer Prev (2014) 15(2):855–60. doi: 10.7314/APJCP.2014.15.2.855
80. Zhu M, Zheng W, Xiang Y, Gu J, Wang K, Shang J. The Relationship Between Central Lymph Node Metastasis and the Distance From Tumor to Thyroid Capsule in Papillary Thyroid Microcarcinoma Without Capsule Invasion. Gland Surg (2020) 9(3):727–36. doi: 10.21037/gs-20-478
81. Xu R, Yin X, Xu W, Jin L, Lu M, Wang Y. Assessment of Carotid Plaque Neovascularization by Contrast-Enhanced Ultrasound and High Sensitivity C-Reactive Protein Test in Patients With Acute Cerebral Infarction: A Comparative Study. Neurol Sci (2016) 37(7):1107–12. doi: 10.1007/s10072-016-2557-2
82. Song Q, Gao H, Tian X, Ren L, Lan Y, Yan L, et al. Evaluation of Ultrasound-Guided Radiofrequency Ablation as a Treatment Option for Papillary Thyroid Microcarcinoma in the Isthmus: A Retrospective Study. Front Endocrinol (Lausanne) (2020) 11:599471. doi: 10.3389/fendo.2020.599471
83. Nilubol N, Kebebew E. Should Small Papillary Thyroid Carcinoma be Observed? A Population-Based Study. Cancer (2015) 121(7):1017–24. doi: 10.1002/cncr.29123
84. Miyauchi A, Kudo T, Ito Y, Oda H, Sasai H, Higashiyama T, et al. Estimation of the Lifetime Probability of Disease Progression of Papillary Microcarcinoma of the Thyroid During Active Surveillance. Surgery (2018) 163(1):48–52. doi: 10.1016/j.surg.2017.03.028
85. Adam MA, Reed SD, Roman SA, Sosa JA. Does Current Thyroid Cancer Staging Accurately Reflect the Impact of Lymph Node Metastases on Survival in Younger Patients? Int J Endocr Oncol (2016) 3(1):1–3. doi: 10.2217/ije.15.25
86. Adam MA, Thomas S, Hyslop T, Scheri RP, Roman SA, Sosa JA. Exploring the Relationship Between Patient Age and Cancer-Specific Survival in Papillary Thyroid Carcinoma: Rethinking Current Staging Systems. J Clin Oncol (2016) 34(36):4415–20. doi: 10.1200/JCO.2016.68.9372
87. Megwalu UC. Observation Versus Thyroidectomy for Papillary Thyroid Microcarcinoma in the Elderly. J Laryngol Otol (2017) 131(2):173–6. doi: 10.1017/S0022215116009762
88. Resende de Paiva C, Grønhøj C, Feldt-Rasmussen U, von Buchwald C. Association Between Hashimoto's Thyroiditis and Thyroid Cancer in 64,628 Patients. Front Oncol (2017) 7:53. doi: 10.3389/fonc.2017.00053
89. Ieni A, Vita R, Magliolo E, Santarpia M, Di Bari F, Benvenga S, et al. One-Third of an Archivial Series of Papillary Thyroid Carcinoma (Years 2007-2015) has Coexistent Chronic Lymphocytic Thyroiditis, Which is Associated With a More Favorable Tumor-Node-Metastasis Staging. Front Endocrinol (Lausanne) (2017) 8:337. doi: 10.3389/fendo.2017.00337
90. Zhang Y, Zhang MB, Luo YK, Li J, Zhang Y, Tang J. Effect of Chronic Lymphocytic Thyroiditis on the Efficacy and Safety of Ultrasound-Guided Radiofrequency Ablation for Papillary Thyroid Microcarcinoma. Cancer Med (2019) 8(12):5450–8. doi: 10.1002/cam4.2406
91. Zhou YL, Gao EL, Zhang W, Yang H, Guo GL, Zhang XH, et al. Factors Predictive of Papillary Thyroid Micro-Carcinoma With Bilateral Involvement and Central Lymph Node Metastasis: A Retrospective Study. World J Surg Oncol (2012) 10:67. doi: 10.1186/1477-7819-10-67
92. Cheng F, Chen Y, Zhu L, Zhou B, Xu Y, Chen Y, et al. Risk Factors for Cervical Lymph Node Metastasis of Papillary Thyroid Microcarcinoma: A Single-Center Retrospective Study. Int J Endocrinol (2019) 2019:8579828. doi: 10.1155/2019/8579828
93. Karatzas T, Vasileiadis I, Charitoudis G, Karakostas E, Tseleni-Balafouta S, Kouraklis G. Bilateral Versus Unilateral Papillary Thyroid Microcarcinoma: Predictive Factors and Associated Histopathological Findings Following Total Thyroidectomy. Horm (Athens) (2013) 12(4):529–36. doi: 10.14310/horm.2002.1441
94. Tuttle RM, Haugen B, Perrier ND. Updated American Joint Committee on Cancer/Tumor-Node-Metastasis Staging System for Differentiated and Anaplastic Thyroid Cancer (Eighth Edition): What Changed and Why? Thyroid (2017) 27(6):751–6. doi: 10.1089/thy.2017.0102
95. Lan Y, Jin Z, Zhang M, Song Q, Xiao J, Yan L, et al. Factors Affecting Quality of Life of Patients Undergoing Radiofrequency Ablation for Papillary Thyroid Microcarcinoma]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao (2020) 42(5):632–9. doi: 10.3881j.issn.1000-503X.12993
Keywords: thyroid cancer, ablation, papillary thyroid carcinoma, thermal ablation, recurrence
Citation: Ou D, Chen C, Jiang T and Xu D (2022) Research Review of Thermal Ablation in the Treatment of Papillary Thyroid Carcinoma. Front. Oncol. 12:859396. doi: 10.3389/fonc.2022.859396
Received: 21 January 2022; Accepted: 24 May 2022;
Published: 01 July 2022.
Edited by:
Gianlorenzo Dionigi, University of Milan, ItalyReviewed by:
Yin Detao, First Affiliated Hospital of Zhengzhou University, ChinaMingbo Zhang, PLA General Hospital, China
Copyright © 2022 Ou, Chen, Jiang and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dong Xu, eHVkb25nQHpqY2Mub3JnLmNu
†These authors have contributed equally to this work
 Di Ou
Di Ou Chen Chen3†
Chen Chen3† Tian Jiang
Tian Jiang Dong Xu
Dong Xu