
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol. , 22 April 2022
Sec. Surgical Oncology
Volume 12 - 2022 | https://doi.org/10.3389/fonc.2022.853662
This article is part of the Research Topic Laparoscopic Surgery in Colorectal Cancer View all 10 articles
 Kai Li1
Kai Li1 Junjie Zeng1
Junjie Zeng1 Pengcheng Pang1
Pengcheng Pang1 Hua Cheng1
Hua Cheng1 Xiaobo He1
Xiaobo He1 Fengyu Cao1
Fengyu Cao1 Qiang Luo2
Qiang Luo2 Shilun Tong1
Shilun Tong1 Yongbin Zheng1*
Yongbin Zheng1*Background: Station 253 node dissection with high ligation of the inferior mesenteric artery (IMA) is difficult to perform without damage to the surrounding autonomic nerve plexuses. This study aimed to investigate the significance of the nerve plane for inferior mesenteric plexus (IMP) preservation in laparoscopic rectal cancer surgery.
Methods: A total of 56 consecutive rectal patients underwent laparoscopic en bloc station 253 node dissection with high ligation of the IMA. Station 253 nodes were divided into the extra- and intra-nerve plane station 253 nodes for further H&E staining and immunohistochemical analysis. Based on IMP nerve plane-based evidence and histopathological results, a novel nerve-sparing technique, IMP nerve plane orientation, was proposed and performed on 68 rectal cancer patients. Urinary and sexual functions in all patients were evaluated at 6 months postoperatively.
Results: Lymph node metastasis was not found, but abundant nerve bundles containing gangliocytes were observed in extra-nerve plane station 253 nodes. The nerve plane was identified intraoperatively and then confirmed by both postoperative gross specimen evaluation and histopathological analysis. The novel nerve-sparing technique (IMP nerve plane orientation) was successfully performed with no postoperative complications, and the operated patients had improved postoperative urinary and sexual functions.
Conclusion: The nerve plane is helpful for IMP preservation and station 253 node dissection. This novel nerve-sparing technique of nerve plane orientation is technically feasible and safe, which could result in faster recovery of urinary and sexual functions.
The Japanese criteria practically define station 253 nodes as nodes that lie along the inferior mesenteric artery (IMA) from the origin of the left colic artery (LCA) to the origin of the IMA (1). The incidence of station 253 node metastasis is relatively low, i.e., approximately 0.3% to 8.6%, in different tumor stages (2). Station 253 node metastasis is more likely to occur in locally advanced rectal cancer above the peritoneal reflection (3); besides, en bloc station 253 node dissection is technically demanding and carries a risk of damage to the surrounding inferior mesenteric plexus (IMP), which may be associated with postoperative organ dysfunction, including urinary and sexual dysfunctions (4, 5). However, station 253 node metastasis is an important prognostic factor of rectal cancer. Therefore, whether en bloc station 253 node dissection is suitable for all rectal cancer patients remains controversial. Moreover, the current definition of station 253 nodes is limited to around the IMA, which is vague, and there is no consistent evidence about the clear border of the area of station 253 nodes.
The nerve plane was defined as the overlying tiny membranous tissue including the nerve, the adipose tissue, and extremely tiny capillaries around the nerve, as described in our previous studies (6–8). Similarly, there is still the IMP nerve plane around the IMA, which divides routine station 253 nodes into extra- and intra-nerve plane station 253 nodes. In the present study, we hypothesized that the nerve plane is the dorsal boundary of station 253 nodes, which should be preserved during station 253 node dissection; intra-nerve plane station 253 nodes are regional lymph nodes, which should be cleaned; and extra-nerve plane station 253 nodes are extra-mesenteric lymph nodes, which are unnecessarily cleaned. We believe that intraoperative IMP nerve plane preservation not only ensures that intra-mesenteric regional lymph nodes are cleaned totally but also better prevents damage to pelvic autonomic nerves. Therefore, the IMP nerve plane is clinically important in IMP preservation and station 253 node dissection in laparoscopic surgery for rectal cancer.
Therefore, the present study aimed to investigate the significance of the nerve plane for IMP preservation in laparoscopic rectal cancer surgery and to propose a novel nerve-sparing technique of nerve plane orientation for station 253 node dissection.
A total of 124 rectal cancer patients were enrolled in this study; patients were divided into a nerve plane-oriented group and a no nerve plane-oriented group. From October 2019 to June 2020, a total of 56 rectal cancer patients in the no nerve plane-oriented group undergoing laparoscopic radical resection with en bloc station 253 node dissection in the Department of Gastrointestinal Surgery, Renmin Hospital of Wuhan University, were prospectively enrolled. Pelvic autonomic nerves including the IMP were preserved as much as possible, although en bloc station 253 nodes were cleaned. The IMP nerve plane was intraoperatively identified, and the routine station 253 nodes were divided into extra- and intra-nerve plane nodes (Figure 1). These lymph node tissues were dehydrated, paraffin embedded, cut into 5-µm sections, and processed for H&E staining. In addition, immunohistochemistry was performed to identify autonomic nerve fibers. Neuronal immunolabeling was performed with anti-rabbit Protein S100 antibodies (S100, 1:400; Abcam, Cambridge, MA, USA). S100 is a general immunolabeling marker of all nerves, which can specifically identify the nucleus and cytoplasm of Schwann cells in formalin-fixed paraffin-embedded nerve tissue specimens.
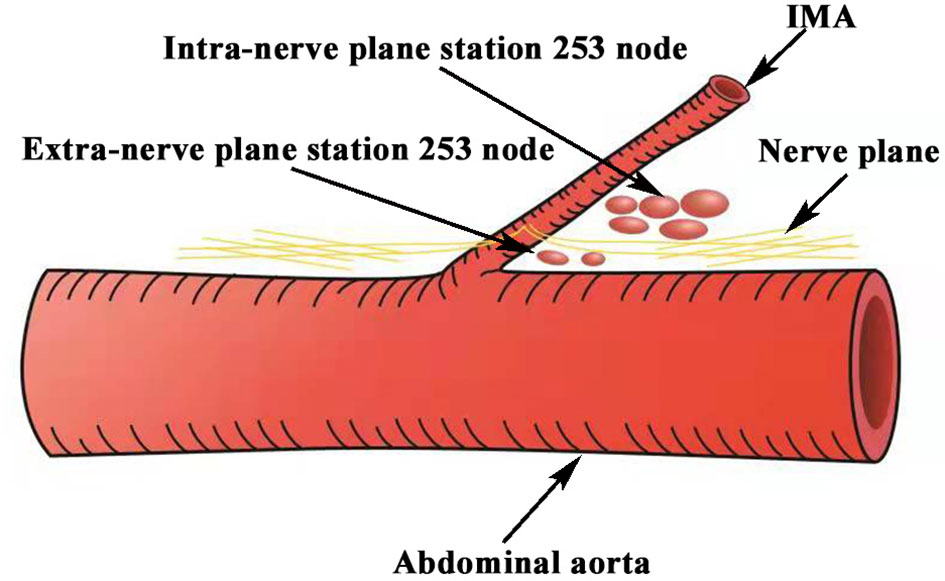
Figure 1 Schematic representation of the extra- and intra-nerve plane station 253 nodes. Station 253 nodes were divided into the extra- and intra-nerve plane station 253 nodes by the IMP nerve plane. IMA, inferior mesenteric artery; IMP, inferior mesenteric plexus.
Based on IMP nerve plane-based evidence and histopathological examination, a novel nerve-sparing technique of nerve plane orientation for IMP preservation was performed on 68 rectal cancer patients in the nerve plane-oriented group between July 2020 and February 2021. Extra-nerve plane station 253 nodes were preserved, and intra-nerve plane station 253 nodes were cleaned and examined by H&E and immunohistochemical (S100) staining. All operations were performed by Prof. Yongbin Zheng, a chief physician of the Department of Gastrointestinal Surgery, Renmin Hospital of Wuhan University, with a 20-year post-certification experience performing approximately 350 cases of laparoscopic rectal cancer radical resection annually. Patient baseline data, tumor characteristics, and surgical outcomes were recorded, and all operative procedures were videotaped. Informed consent was obtained from all participating patients. This study was approved by the Institutional Review Board of Renmin Hospital, Wuhan University (no. WDRY2021-K126).
The urinary function was evaluated by the International Prostate Symptom Score (IPSS) questionnaire (9). IPSS total score ranged from 0 to 35: the higher the score, the severer the urinary dysfunction. Moderate-to-severe urinary dysfunction was defined as an IPSS score >8 points (10). Male sexual function was evaluated by the 5-item version of the International Index of Erectile Function (IIEF-5) (11) questionnaire and ejaculation function grading. IIEF-5’s total score ranged from 1 to 25: the lower the score, the severer the erectile dysfunction. Male erectile dysfunction was defined as an IIEF-5 score ≤11 points. Ejaculation was functionally classified as follows: grade I, normal ejaculation; grade II, retrograde ejaculation; and grade III, anejaculation. Ejaculation dysfunction was identified as grade II or III ejaculation in this study (12). Female sexual function was evaluated by the Female Sexual Function Index (FSFI) system, which is a validated questionnaire comprised of 19 items. FSFI’s total score ranged from 2 to 36; the higher the score, the severer the sexual dysfunction (13). Female sexual dysfunction was defined as an FSFI score <26.55 points in this study (14). Urinary and sexual functions were evaluated before surgery and at 6 postoperative months.
Data were presented as mean ( ± SD) and number (frequency, %) for continuous and categorical variables, respectively. Dichotomous clinical variables were assessed by a chi-square test. Two-sided p < 0.05 was considered statistically significant. All statistical analyses were performed with SPSS version 20.0 (IBM, Armonk, New York, NY, USA).
A total of 124 rectal cancer patients were evaluated in this study. All participating patients received laparoscopic radical resection without conversion. Patient clinical characteristics are shown in Table 1. Variables, including age, sex, body mass index (BMI), prostatic hyperplasia or not, tumor location, tumor differentiation, pathological TNM stage, intra-nerve plane station 253 nodes retrieved, and total lymph nodes retrieved, had no significant differences between the two groups. Patients in the nerve plane-oriented group had reduced operative blood loss (49.6 ± 13.6 vs. 22.6 ± 13.7, p < 0.001) but longer operative time (165.2 ± 20.6 vs. 175 ± 25.7, p = 0.016) compared with patients in the no nerve plane-oriented group.
In all patients, the typical structural features of the nerve plane were observed, as shown in Supplementary Video 1. The “Holy plane” was revealed more clearly in the anterior of the abdominal aorta by enforcing traction and anti-traction, and the IMP was lifted by the IMA as a “tent” when the extension was closed to the root of the IMA; the IMP was surrounded by the adipose tissue and extremely tiny capillaries and covered by a tiny membranous tissue, i.e., the IMP nerve plane (Figure 2A). Similarly, the abdominal aortic plexus and superior hypogastric plexus nerve planes were also observed. These nerve planes are continuous and form a novel landmark for pelvic autonomic nerve protection in laparoscopic rectal cancer surgery. Station 253 nodes within the nerve plane are called intra-nerve plane station 253 nodes, which should be cleaned in rectal cancer surgery; conversely, station 253 nodes beyond the nerve plane are called extra-nerve plane lymph nodes, which are rarely involved in tumor metastasis due to the protective effect of the nerve plane (Figure 2B). Subsequently, en bloc station 253 nodes were marked and divided into extra- and intra-nerve plane nodes after the specimen was removed (Figure 2C), which were sent to a pathological lab for further examination. Eventually, the mean number of intra-nerve plane station 253 nodes retrieved was 3.0 (range, 0–7), and 5 cases (5/56 = 8.9%) with intra-nerve plane station 253 node metastasis were confirmed by H&E staining. The mean number of extra-nerve plane station 253 nodes retrieved was 1.5 (range, 0–4), and no metastatic extra-nerve plane station 253 nodes were found. In the nerve plane-oriented group, the mean number of intra-nerve plane station 253 nodes retrieved was 3.1 (range, 1–6), and 6 cases (6/68 = 8.8%) showed intra-nerve plane station 253 node metastasis, as shown in Table 1.
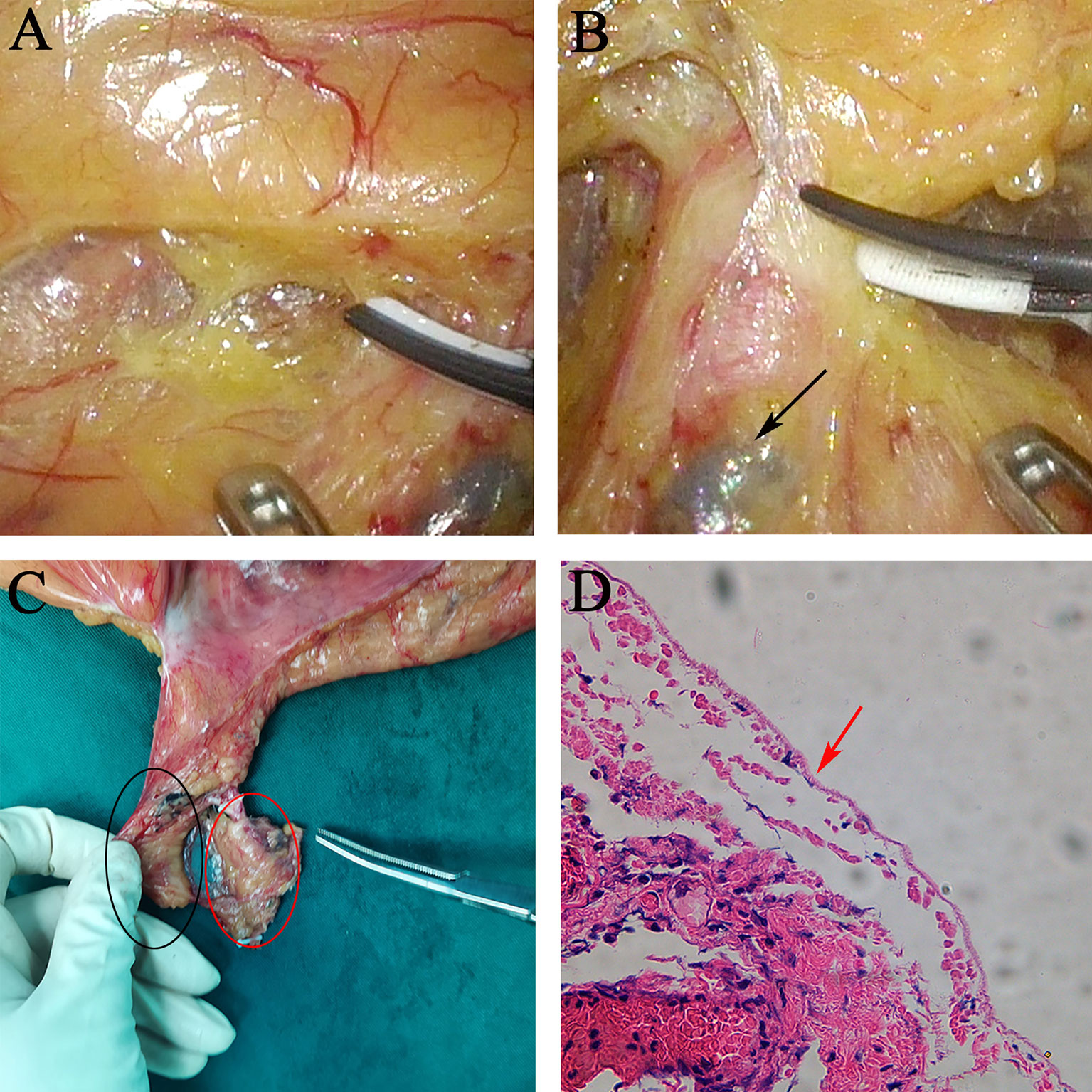
Figure 2 Relationship between extra- and intra-nerve plane station 253 nodes. (A) Inferior mesenteric plexus nerve plane. The IMP was surrounded by the adipose tissue and extremely tiny capillaries and covered by a tiny membranous tissue. (B) Extra-nerve plane station 253 nodes were black-dyed by carbon nanoparticles. (C) Postoperative gross specimen of en bloc station 253 nodes. Black and red ovals show intra- and extra-nerve plane station 253 nodes, respectively. (D) H&E staining showing completely excised mesorectum of intra-nerve plane station 253 nodes; no nerve bundles were found in intra-nerve plane station 253 nodes. IMA, inferior mesenteric artery; IMP, inferior mesenteric plexus.
Nerve fibers positively stained for S100 were deep brown, and nerve bundles containing gangliocytes were observed in extra-nerve plane station 253 nodes (Figure 3). No nerve bundles were found in intra-nerve plane station 253 nodes, and the mesorectum in postoperative specimens was intact as shown by H&E staining (Figure 2D).
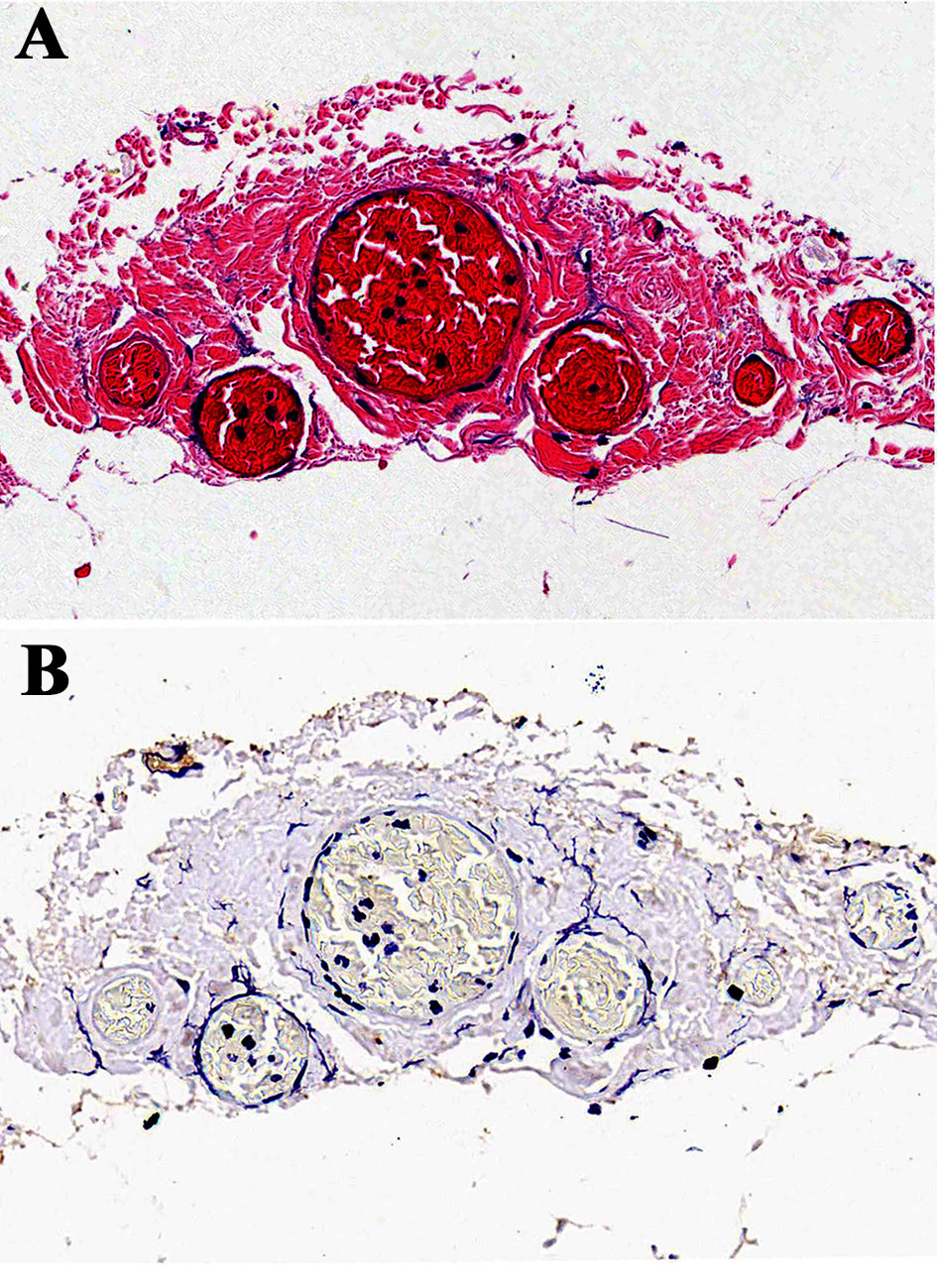
Figure 3 H&E and immunohistochemical staining (S100) of extra-nerve plane station 253 nodes. (A) H&E staining of extra-nerve plane station 253 nodes. (B) Immunohistochemical staining of extra-nerve plane station 253 nodes with anti-S100 antibodies. Abundant nerve fibers positively stained for S100 were deep brown and observed in extra-nerve plane station 253 nodes.
Based on the above nerve plane-based evidence and histopathological results, a novel nerve-sparing technique of nerve plane orientation was proposed. The details of the surgical procedure are shown in Supplementary Video 2. Briefly, dissection above the abdominal aortic plexus nerve plane was performed and extended up to the lower edge of the duodenum and down to the entrance of the IMP nerve plane (Figure 4A). After extension from the superior hypogastric plexus nerve plane to the IMP nerve plane posterior to the IMA (Figure 4B), dissection was continued over the IMP nerve plane from caudal to cephalic by the “slope climbing” approach. After crossing the IMA, dissection was continued from cephalic to caudal by the “slope downhill” approach, and the abdominal aortic plexus nerve plane was gradually entered (Figure 4C). Finally, the IMA was ligated and cut above the IMP nerve plane (Figure 4D). After a specimen was collected, the nerve plane around the IMA showed preserved integrity.
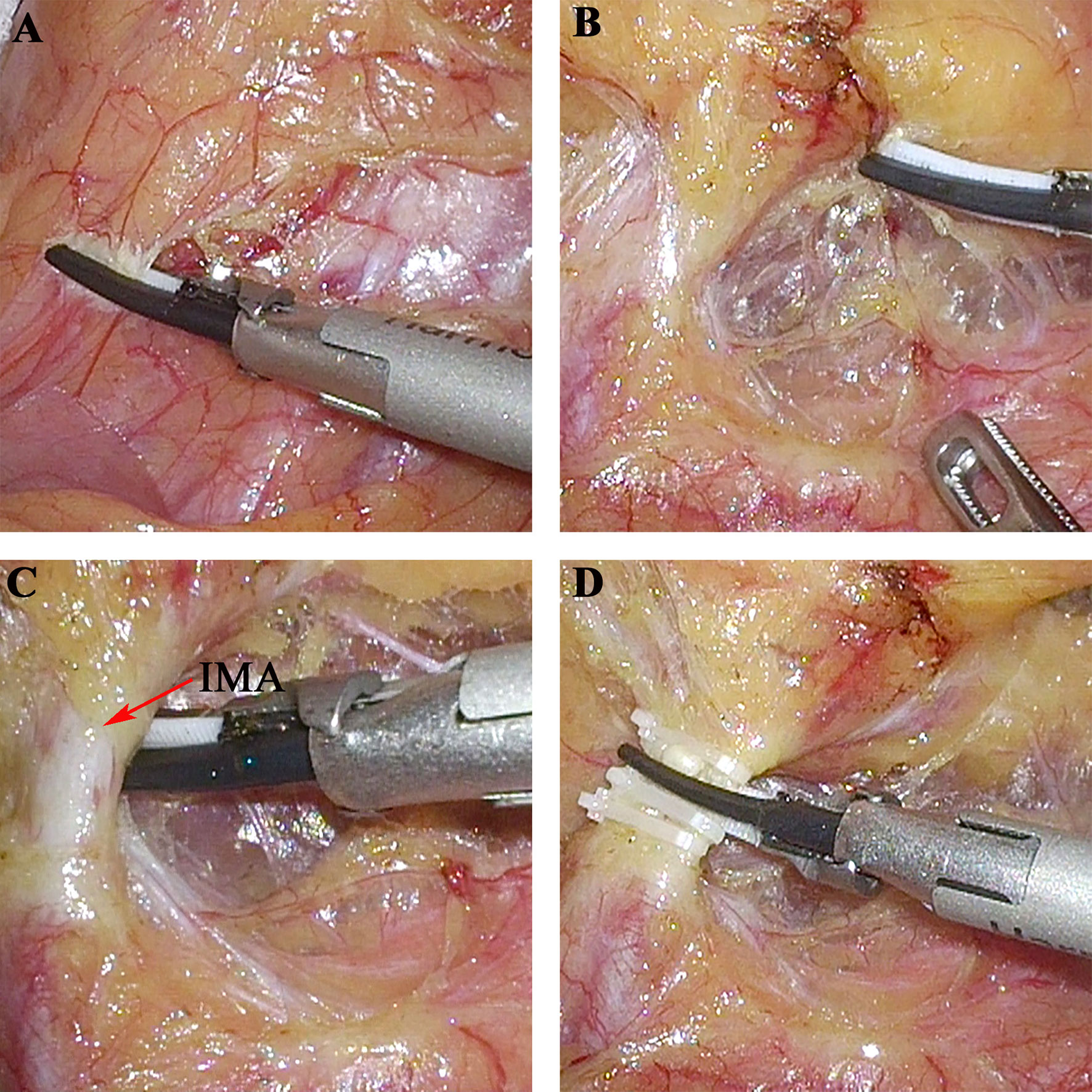
Figure 4 The nerve-sparing technique of nerve plane-oriented. (A) The dissection extended up to the lower edge of the duodenum. (B) Extension from the superior hypogastric plexus nerve plane to the IMP nerve plane posterior to the IMA. (C) Abdominal aortic plexus nerve plane was gradually entered from cephalic to caudal by the “slope downhill” approach. (D) The IMA was ligated and cut above the IMP nerve plane. IMA, inferior mesenteric artery; IMP, inferior mesenteric plexus.
As shown in Table 2, there were no significant differences in IPSS (4.3 ± 2.9 vs. 5.2 ± 2.5, p = 0.062), IIEF-5 (16.5 ± 3.4 vs. 17.7 ± 3.7, p = 0.132), and FSFI (29.2 ± 3.8 vs. 29.5 ± 3.7, p = 0.638) scores before surgery between the two groups. Patients in the nerve plane-oriented group showed higher IIEF-5 (13.9 ± 3.1 vs. 15.8 ± 3.7, p = 0.015) and FSFI (24.6 ± 4.6 vs. 27.7 ± 3.1, p = 0.006) scores than those in the no nerve plane-oriented group, although IPSS scores (6.4 ± 4.7 vs. 6.0 ± 3.4, p = 0.635) showed no significant difference between the two groups at 6 postoperative months.
There were no significant differences in urinary (8.9% vs. 7.3%, p = 0.748) and sexual (12.5% vs. 13.2%, p = 0.903) dysfunction rates before surgery between the two groups. However, patients in the nerve plane-oriented group had lower urinary (26.8% vs. 11.7%, p = 0.032) and sexual (35.7% vs. 19.1%, p = 0.037) dysfunction rates than those in the no nerve plane-oriented group at 6 postoperative months. Therefore, the patients who underwent the nerve-sparing technique of nerve plane orientation had better postoperative urinary and sexual functions.
With the introduction of total mesorectal excision (TME) surgery, rectal cancer prognosis has been greatly improved; however, the quality of life of patients after surgery has not been paid enough attention to by surgeons, which includes urinary, sexual, and bowel dysfunctions related to intraoperative pelvic autonomic nerve injury. Therefore, preserving the pelvic autonomic nerve, including IMP preservation, in rectal cancer surgery has become increasingly important. Many studies have found that station 253 node metastasis is an important prognostic factor in patients with colorectal cancer (15–17). Many consensus opinions, including the Japanese Society for Cancer of the Colon and Rectum (JSCCR) and The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines, recommended station 253 node dissection and high ligation of the IMA in rectal cancer patients with preoperative clinical T2–4N+ stage (18, 19). However, high ligation of the IMA and station 253 node dissection in laparoscopic anterior resection for rectal cancer increase the risk of IMP damage and result in postoperative urinary and sexual dysfunctions. Therefore, how to improve surgical techniques for IMP preservation is essential and represents a technical challenge for most surgeons; surgical techniques for IMP preservation are still lacking.
In the present study, the nerve plane was used as an optimal surgical landmark for laparoscopic rectal surgery, for several potential reasons. First, pelvic autonomic nerves, including the IMP, are located outside the mesorectal plane (20, 21); therefore, this technique should theoretically have consistent oncologic outcomes with routine nerve-sparing surgery. Second, not only the nerves but also the continuous nerve plane covered with the membranous tissue are preserved; thus, it could reduce intraoperative damage to pelvic autonomic nerves due to heat conduction and physicochemical factors such as wound exudate and inflammatory mediators. Finally, the nerves were not intentionally exposed during the operation, which differs from other nerve-sparing techniques such as nerve-guided technique (22, 23), active exposure of the nerve could increase nerve stretching and the risk of nerve damage. The nerve-sparing technique of nerve plane orientation for IMP preservation has been a standardized laparoscopic procedure in our institution since 2013, with satisfactory postoperative urinary and sexual functions despite the lack of follow-up for survival prognosis.
Currently, numerous studies have proposed various nerve-sparing techniques for IMP preservation. Liang et al. (24) recommended that the IMP should be preserved by sparing the pre-aortic connective tissue and leaving a 1- to 2-cm-long stump of the IMA in situ, consistent with most nerve-sparing techniques (25, 26). Huscher et al. (27) reported a clear identification of the branches climbing around the IMA with the Cavitron ultrasonic surgical aspirator for IMP preservation; while performing a high ligation, this nerve-sparing technique relies more on advanced medical devices than surgical technology. Sun et al. (28) also reported three anatomical levels, including the parietal fascia, the neurofascial layer, and the mesosigmoid, for IMP preservation in laparoscopic rectal cancer surgery and proposed an effective procedure for high ligation of the IMA. The latter technique was somewhat similar to ours; however, the neurofascial layer could not form a continuous plane in their surgical procedure, as shown in the current technique. Recently, Zheng et al. (29) reported that the left trunk of the IMP is a part of the IMA vascular sheath and proposed intrasheath separation of the IMA and left trunk for IMP preservation. In the present study, we believed that the IMP nerve plane could be separated from the IMA by enforcing traction and anti-traction. To maintain a balance between oncology and function, the nerve-sparing technique of nerve plane orientation was successfully performed in 68 patients without postoperative complications or urinary/sexual dysfunction. Therefore, this surgical technique is technically safe and feasible.
Moreover, the clear border of station 253 nodes remains vague and not standardized, and the area of station 253 nodes is regarded as an area containing the fat tissue around the IMA. Studies recommended that the left side is the inferior mesenteric vein (IMV), with the side dissection being the abdominal aorta, the cephalic side being the duodenum, and the caudal side being the IMA, which are the borders of station 253 nodes (30). In addition, most Chinese experts believe that the borders of station 253 nodes include the medial border as the area of the trunk between the point of origin of the IMA and the LCA, the lateral border as the medial margin of the IMV, the caudal border as the point of origin of the LCA to its intersection with the IMV, and the cephalic border as the level of the root of the IMA (31). However, most studies have no clear definition of the dorsal border of station 253 nodes. In the present work, we believed that the IMP nerve plane is the dorsal border of station 253 nodes and should be preserved, which not only avoids damaging the IMP but also ensures station 253 node dissection in laparoscopic rectal cancer surgery.
Regarding urinary and sexual functions, in the present study, at 6 months after laparoscopic rectal cancer surgery, with the routine nerve-sparing technique, the rate of urinary dysfunction was increased by 17.9% (from 8.9% to 26.8%), while the sexual dysfunction rate was increased by 23.2% (from 12.5% to 35.7%). However, in the nerve-sparing technique of nerve plane orientation, the rate of urinary dysfunction was increased by 4.4% (from 7.3% to 11.7%), and the sexual dysfunction rate was increased by 5.9% (from 13.2% to 19.1%). Therefore, the nerve-sparing technique of nerve plane orientation confers faster recovery of urinary and urogenital functions.
In the present study, we regarded extra-nerve plane station 253 nodes as extra-mesenteric lymph nodes, which are unnecessarily cleaned, especially for patients with early rectal cancer. Extended station 253 node dissection not only provides no additional survival benefit but also increases the risk of nerve damage. However, some limitations should be acknowledged in this study, including the relatively small sample size and the lack of long-term follow-up for oncological outcomes. Therefore, further studies with large samples and long-term follow-up with oncological outcomes are required.
The presence of the nerve plane is helpful for IMP preservation. This nerve-sparing technique of nerve plane orientation is technically feasible and safe, which confers faster recovery of urinary and sexual functions.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by The Institutional Review Board of the Renmin Hospital of Wuhan University. The patients/participants provided their written informed consent to participate in this study.
KL designed the study and prepared the manuscript draft. PP, HC, and JZ performed the data collection and analysis. QL and ST performed the H&E staining and immunohistochemical analysis. XH, FC, and YZ critically revised the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
This work was supported by grants from the Chenxiao-ping Foundation for the Development of Science and Technology of Hubei Province (CXPJJH121003-2103).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.853662/full#supplementary-material
1. Japanese Society for Cancer of the Colon and Rectum. General Rules for Clinical and Pathological Studies on Cancer of the Colon, Rectum, and Anus. 6th ed. Tokyo: Kanahara Shuppan (1998).
2. Lange MM, Buunen M, van de Velde CJ, Lange JF. Level of Arterial Ligation in Rectal Cancer Surgery: Low Tie Preferred Over High Tie. A Review. Dis Colon Rectum (2008) 51:1139–45. doi: 10.1007/s10350-008-9328-y
3. Sun Y, Chi P, Lin H, Lu X, Huang Y, Xu Z, et al. Inferior Mesenteric Artery Lymph Node Metastasis in Rectal Cancer Treated With Neoadjuvant Chemoradiotherapy: Incidence, Prediction and Prognostic Impact. Eur J Surg Oncol (EJSO) (2017) 43:85–91. doi: 10.1016/j.ejso.2016.09.005
4. Liang JT, Lai HS, Lee PH, Chang KJ. Laparoscopic Pelvic Autonomic Nerve-Preserving Surgery for Sigmoid Colon Cancer. Ann Surg Oncol (2008) 15:1609–16. doi: 10.1245/s10434-008-9861-x
5. Nano M, Dal Corso H, Ferronato M, Solej M, Hornung JP, Dei PM. Ligation of the Inferior Mesenteric Artery in the Surgery of Rectal Cancer: Anatomical Considerations. Dig Surg (2004) 21:123–6. doi: 10.1159/000077347
6. Li K, He X, Zheng Y. An Optimal Surgical Plane for Laparoscopic Functional Total Mesorectal Excision in Rectal Cancer. J Gastrointest Surg (2021) 25:2726–7. doi: 10.1007/s11605-021-05035-9
7. Li K, He X, Tong S, Zheng Y. Nerve Plane: An Optimal Surgical Plane for Laparoscopic Rectal Cancer Surgery? Med Hypotheses (2021) 154:110657. doi: 10.1016/j.mehy.2021.110657
8. Deng WH, Zheng YB, Tong SL, Cao FY, He XB, Xiao K, et al. Efficiency Analysis on Functional Protection of Nerve Plane-Oriented Laparoscopic Total Mesorectal Excision. Zhonghua Wei Chang Wai Ke Za Zhi (2019) 22:1144–51. doi: 10.3760/cma.j.issn.1671-0274.2019.12.009
9. Barry MJ, Fowler FJ, O'Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American Urological Association Symptom Index for Benign Prostatic Hyperplasia. The Measurement Committee of the American Urological Association. J Urol (1992) 148:1549–57. doi: 10.1016/s0022-5347(17)36966-5
10. Kim HS, Kang JH, Yang SY, Kim NK. Long-Term Voiding and Sexual Function in Male Patients After Robotic Total Mesorectal Excision With Autonomic Nerve Preservation for Rectal Cancer: A Cross-Sectional Study. Surg Laparosc Endosc Percutan Tech (2020) 30:137–43. doi: 10.1097/SLE.0000000000000779
11. Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Pena BM. Development and Evaluation of an Abridged, 5-Item Version of the International Index of Erectile Function (Iief-5) as a Diagnostic Tool for Erectile Dysfunction. Int J Impot Res (1999) 11:319–26. doi: 10.1038/sj.ijir.3900472
12. Wei B, Zheng Z, Fang J, Xiao J, Han F, Huang M, et al. Effect of Denonvilliers' Fascia Preservation Versus Resection During Laparoscopic Total Mesorectal Excision on Postoperative Urogenital Function of Male Rectal Cancer Patients: Initial Results of Chinese Puf-01 Randomized Clinical Trial. Ann Surg (2020) 274:e473–80. doi: 10.1097/SLA.0000000000004591
13. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (Fsfi): A Multidimensional Self-Report Instrument for the Assessment of Female Sexual Function. J Sex Marital Ther (2000) 26:191–208. doi: 10.1080/009262300278597
14. Wiegel M, Meston C, Rosen R. The Female Sexual Function Index (Fsfi): Cross-Validation and Development of Clinical Cutoff Scores. J Sex Marital Ther (2005) 31:1–20. doi: 10.1080/00926230590475206
15. Huh JW, Kim YJ, Kim HR. Distribution of Lymph Node Metastases Is an Independent Predictor of Survival for Sigmoid Colon and Rectal Cancer. Ann Surg (2012) 255:70–8. doi: 10.1097/SLA.0b013e31823785f6
16. Kang J, Hur H, Min BS, Kim NK, Lee KY. Prognostic Impact of Inferior Mesenteric Artery Lymph Node Metastasis in Colorectal Cancer. Ann Surg Oncol (2011) 18:704–10. doi: 10.1245/s10434-010-1291-x
17. Ubukata M, Itabashi M, Kameoka S. Japanese D3 Lymph Node Dissection in Low Rectal Cancer With Inferior Mesenteric Lymph Node Metastases. World J Surg (2014) 38:2724–9. doi: 10.1007/s00268-014-2617-9
18. Watanabe T, Muro K, Ajioka Y, Hashiguchi Y, Ito Y, Saito Y, et al. Japanese Society for Cancer of the Colon and Rectum (Jsccr) Guidelines 2016 for the Treatment of Colorectal Cancer. Int J Clin Oncol (2018) 23:1–34. doi: 10.1007/s10147-017-1101-6
19. Vogel JD, Eskicioglu C, Weiser MR, Feingold DL, Steele SR. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Treatment of Colon Cancer. Dis Colon Rectum (2017) 60:999–1017. doi: 10.1097/DCR.0000000000000926
20. Kinugasa Y, Murakami G, Suzuki D, Sugihara K. Histological Identification of Fascial Structures Posterolateral to the Rectum. Br J Surg (2007) 94:620–6. doi: 10.1002/bjs.5540
21. Mike M, Kano N. Laparoscopic-Assisted Low Anterior Resection of the Rectum–A Review of the Fascial Composition in the Pelvic Space. Int J Colorectal Dis (2011) 26:405–14. doi: 10.1007/s00384-010-1107-2
22. Runkel N, Reiser H. Nerve-Oriented Mesorectal Excision (Nome): Autonomic Nerves as Landmarks for Laparoscopic Rectal Resection. Int J Colorectal Dis (2013) 28:1367–75. doi: 10.1007/s00384-013-1705-x
23. Zhou H, Ruan C, Sun Y, Zhang J, Wang Z, Hu Z. Nerve-Guided Laparoscopic Total Mesorectal Excision for Distal Rectal Cancer. Ann Surg Oncol (2015) 22:550–1. doi: 10.1245/s10434-014-4161-0
24. Liang JT, Lai HS, Lee PH. Laparoscopic Pelvic Autonomic Nerve-Preserving Surgery for Patients With Lower Rectal Cancer After Chemoradiation Therapy. Ann Surg Oncol (2007) 14:1285–7. doi: 10.1245/s10434-006-9052-6
25. Tejedor P, Sagias F, Celentano V, Khan JS. Nerve-Sparing Total Mesorectal Excision and Pelvic Neuroanatomy for Colorectal Surgeons. Dis Colon Rectum (2019) 62:1548–9. doi: 10.1097/DCR.0000000000001502
26. Li K, Chen D, Chen W, Liu Z, Jiang W, Liu X, et al. A Case-Control Study of Using Carbon Nanoparticles to Trace Decision-Making Lymph Nodes Around Inferior Mesenteric Artery in Rectal Cancer. Surg Endosc (2019) 33:904–10. doi: 10.1007/s00464-018-6384-9
27. Huscher CG, Rossetti A. Nerve-Sparing High Ligation of the Inferior Mesenteric Artery With Cavitron Ultrasonic Surgical Aspirator (Cusa). Tech Coloproctol (2017) 21:163. doi: 10.1007/s10151-016-1574-8
28. Sun Y, Zhang ZC, Zhou YD, Li P, Zeng QS, Zhang XP. High Ligation of the Inferior Mesenteric Artery With Nerve-Sparing in Laparoscopic Surgery for Advanced Colorectal Cancer. Tech Coloproctol (2021) 25:343–4. doi: 10.1007/s10151-020-02355-x
29. Zheng Z, Wang X, Huang Y, Lu X, Zhao X, Chi P. An Intrasheath Separation Technique for Nerve-Sparing High Ligation of the Inferior Mesenteric Artery in Colorectal Cancer Surgery. Front Oncol (2021) 11:694059. doi: 10.3389/fonc.2021.694059
30. Li K, Li Z, Yan B, Tan J, Chen D, Chen W, et al. Preoperative Carbon Nanoparticle Injection Improves Inferior Mesenteric Artery Lymph Node Retrieval in Patients With Rectal Cancer. Surgery (2021) 13:S0039–6060(21)00793-5. doi: 10.1016/j.surg.2021.08.023
31. Editorial Committee of Chinese Expert Consensus on Radical Resection of Rectal Cancer with Preservation of Left Colorectal Artery (2021 edition), Comprehensive Treatment Group of Colorectal Cancer, Anorectal Doctor Branch, Chinese Medical Doctor Association, Expert Committee on Prevention and Treatment of Rectal Cancer, Special Committee for General Surgery, Society of Integrated Traditional Chinese and Western Medicine. Chinese Expert Consensus on Radical Resection of Rectal Cancer With Preservation of Left Colonic Artery (2021 Edition). Zhonghua Wei Chang Wai Ke Za Zhi (2021) 24:950–5. doi: 10.3760/cma.j.cn441530-20210927-00389
Keywords: nerve plane, inferior mesenteric plexus, laparoscopic surgery, rectal cancer, station 253 node
Citation: Li K, Zeng J, Pang P, Cheng H, He X, Cao F, Luo Q, Tong S and Zheng Y (2022) Significance of Nerve Plane for Inferior Mesenteric Plexus Preservation in Laparoscopic Rectal Cancer Surgery. Front. Oncol. 12:853662. doi: 10.3389/fonc.2022.853662
Received: 12 January 2022; Accepted: 18 March 2022;
Published: 22 April 2022.
Edited by:
Ren Zhao, Shanghai Jiao Tong University, ChinaReviewed by:
Francesco Bianco, Ospedale San Leonardo ASLNA3, ItalyCopyright © 2022 Li, Zeng, Pang, Cheng, He, Cao, Luo, Tong and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yongbin Zheng, eW9uZ2JpbnpoZW5nQHdodS5lZHUuY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.