
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
METHODS article
Front. Oncol. , 08 June 2022
Sec. Cancer Epidemiology and Prevention
Volume 12 - 2022 | https://doi.org/10.3389/fonc.2022.841951
This article is part of the Research Topic Cancer Prevention, Treatment and Survivorship in the LGBTQIA Community View all 15 articles
 Katie J. Myers1
Katie J. Myers1 Talya Jaffe1
Talya Jaffe1 Deborah A. Kanda1
Deborah A. Kanda1 V. Shane Pankratz1,2
V. Shane Pankratz1,2 Bernard Tawfik1,2
Bernard Tawfik1,2 Emily Wu1,3
Emily Wu1,3 Molly E. McClain4
Molly E. McClain4 Shiraz I. Mishra1,5
Shiraz I. Mishra1,5 Miria Kano1,2
Miria Kano1,2 Purnima Madhivanan6,7,8
Purnima Madhivanan6,7,8 Prajakta Adsul1,2*
Prajakta Adsul1,2*Purpose: Around 5% of United States (U.S.) population identifies as Sexual and Gender Diverse (SGD), yet there is limited research around cancer prevention among these populations. We present multi-pronged, low-cost, and systematic recruitment strategies used to reach SGD communities in New Mexico (NM), a state that is both largely rural and racially/ethnically classified as a “majority-minority” state.
Methods: Our recruitment focused on using: (1) Every Door Direct Mail (EDDM) program, by the United States Postal Services (USPS); (2) Google and Facebook advertisements; (3) Organizational outreach via emails to publicly available SGD-friendly business contacts; (4) Personal outreach via flyers at clinical and community settings across NM. Guided by previous research, we provide detailed descriptions on using strategies to check for fraudulent and suspicious online responses, that ensure data integrity.
Results: A total of 27,369 flyers were distributed through the EDDM program and 436,177 impressions were made through the Google and Facebook ads. We received a total of 6,920 responses on the eligibility survey. For the 5,037 eligible respondents, we received 3,120 (61.9%) complete responses. Of these, 13% (406/3120) were fraudulent/suspicious based on research-informed criteria and were removed. Final analysis included 2,534 respondents, of which the majority (59.9%) reported hearing about the study from social media. Of the respondents, 49.5% were between 31-40 years, 39.5% were Black, Hispanic, or American Indian/Alaskan Native, and 45.9% had an annual household income below $50,000. Over half (55.3%) were assigned male, 40.4% were assigned female, and 4.3% were assigned intersex at birth. Transgender respondents made up 10.6% (n=267) of the respondents. In terms of sexual orientation, 54.1% (n=1371) reported being gay or lesbian, 30% (n=749) bisexual, and 15.8% (n=401) queer. A total of 756 (29.8%) respondents reported receiving a cancer diagnosis and among screen-eligible respondents, 66.2% reported ever having a Pap, 78.6% reported ever having a mammogram, and 84.1% reported ever having a colonoscopy. Over half of eligible respondents (58.7%) reported receiving Human Papillomavirus vaccinations.
Conclusion: Study findings showcase effective strategies to reach communities, maximize data quality, and prevent the misrepresentation of data critical to improve health in SGD communities.
In the United States (U.S.), about 5% of the population identifies as Sexual and Gender Diverse (SGD) (1). SGD is an umbrella term used to describe individuals who are part of the LGBTQIA+ (lesbian, gay, bisexual, transgender, queer, intersex, asexual, and many other sexual orientations and gender identities) community. Despite SGD individuals representing a significant proportion of the population, there is limited research to identify and understand cancer prevention practices among SGD populations, both nationally and in NM.
NM is a minority-majority state, with 49.3% of the population being Hispanic or Latino, 11% being American Indian/Alaska Native, and 36.8% being non-Hispanic White (2). Additionally, about one third of New Mexicans report speaking a language other than English at home, with Spanish being the top language (3). NM is the third poorest state in the union with an average poverty rate of 16.2% compared to the U.S. average of 11.2% (4). Additionally, the Congressional Research Office considers 14 out of 33 NM counties to be Persistent Poverty Counties (poverty rates of 19.5% or greater), based on 1990 Census, Census 2000, and 2019 Small Area Income and Poverty Estimates (5). NM is also a very rural state, which can further contribute to disparities (6). Applying the most recent 2010 Rural-Urban Commuting Area (RUCA) codes, approximately 36% of New Mexicans live in rural areas, as defined by the Health Resources and Services Administration (HRSA) (7).
Recent data from the Williams Institute that reports results from the Gallup Survey (1) suggests that 4.5% of the New Mexico (NM) population identify themselves as Lesbian, Gay, Bisexual, or Transgender (LGBT) (8). Among NM SGD populations, 45% report male gender and 55% report female gender. The average age is 37.7 years and they are primarily Latino/a (49%) with 43% being white. Thirty nine percent report a high school education as their highest educational attainment and 14% report being uninsured. Finally, 26% of LGBTQ individuals in New Mexico report having an income less than $24,000 (8). Overall, the SGD communities in NM are relatively younger and primarily belong to groups that experience racial and socioeconomic inequities.
Collectively, the social determinants of health highlighted above can contribute to significant health disparities experienced by people living in NM, further highlighting the need to better understand population perspectives for designing and developing equity-oriented health interventions. For SGD populations, these determinants of health can intersect with their sexual and gender identities, and further exacerbate disparities (9, 10). For example, a transgender man who belongs to a group experiencing racial inequities and has a lower socioeconomic status would face greater barriers to access care as each one of these aspects of his identity is associated with lower access to care (11–13). The most recent (2014) epidemiological data from the NM Department of Health show differences in cervical and breast cancer screening uptake based on sexual orientation, but these data do not document disparities based on gender identity and for other types of cancer (2).
There is a dearth of data around NM SGD populations, especially for rural SGD populations. These populations can face different challenges than SGD populations in urban areas due to the complexity associated with socially conservative locals where they may not feel safe being “out” (14, 15). Juxtaposed with this notion, much of the extant SGD studies have been conducted in large urban cities, with these populations considered as “hard-to-reach” (16, 17). To address this gap, we sought to understand the determinants to cancer prevention practices (e.g. smoking, vaccination, cancer screening, among others) in order to develop future interventions. We proposed conducting a state-wide survey to better understand cancer prevention and control related practices among NM’s SGD populations. This paper presents the systematic and innovative strategies that were employed for reaching the NM SGD populations, with the goal of recruiting them to participate in a cross-sectional, purposive sampled, web-based survey.
The purpose of this paper is to present empirical data supporting the multi-pronged, low-cost, and systematic recruitment strategies to engage SGD communities in NM, a state that is largely rural, poor, and racially/ethnically classified as a “majority-minority” state. Additionally, we describe the characteristics of the study sample that was recruited using the aforementioned strategies. Data from the SGD communities were collected using online questionnaires which presented unique threats to sample and data validity. We also provide a detailed description on using research-informed strategies to detect fraudulent or suspicious responses and ensure data quality, and these methods can inform similar future efforts.
Recruitment for the survey took place from January to March 2021. To ensure state-wide reach, we focused on four methods (1): Every Door Direct Mail (EDDM) program, by the United States Postal Services (USPS) (2); advertisements on Google and Facebook (3); organizational outreach via emails to SGD-friendly businesses; and (4) personal outreach via flyers at clinical and community settings across NM. All flyers, ads, and emails contained QR codes (optical labels that contain links that can be accessed using a cellphone camera) and/or links to a survey in both English and Spanish.
The EDDM program by the USPS was the team’s primary method employed to reach SGD populations across the state. This program was originally designed to help businesses promote their products by mailing promotional materials to certain audiences in neighboring mailing routes (18). We worked with Taradel® which is an affiliate of the USPS, that provides access and services in addition to EDDM (i.e. digital ads on Google, email outreach, and Facebook ads) (19). Taradel® provides an online mapping tool (See Figure 1), which allowed the team to select mailing routes based on attributes such as residential or business addresses, household income, age, home ownership, gender, and presence of children, collated using data from the US Census Bureau (20). To inform the selection of the mailing routes, three criteria could be chosen from a drop-down menu, which then generated a heatmap overlay of mailing routes, indicating how each mailing route matched up with the specified criteria (Figure 1). We selected three criteria for this study: residential addresses, household income below 50,000, and age of residents 25 and older. These criteria allowed us to recruit individuals below the median income of NM of $50,000 per year (21) and around the age range at which cervical, breast, colorectal, and lung cancer screening tests are recommended (22–25). Based on the heatmaps generated with these criteria, we selected mailing routes across NM with at least a 50% match probability, oversampling where we had local knowledge of SGD friendly neighborhoods. This resulted in the selection of 61 mailing routes, with a total of 27,369 individual addresses. Flyers for the study were then sent to these addresses (See Figure 2 for flyers).
The second method of using Google and Facebook ads was an added service provided by Taradel®, that overlapped with the 61 selected mailing routes for the flyers. With the help of their digital services department, we created digital ads that could be displayed through Google and Facebook Ads (See Figure 3 for Google and Facebook Ads). To create these ads, we used publicly-available stock photos provided in The Gender Spectrum Collection (26) that represent transgender and nonbinary individuals. The Facebook Ads were created in collaboration with the UNM Comprehensive Cancer Center (UNMCCC), that allowed for the Ads to be hosted on UNMCCC’s Facebook page, lending credibility to the study recruitment. Both Google and Facebook Ads were disseminated using targeted e-mail and Facebook services provided by Taradel®.
The two other methods for reaching and recruiting individuals into the study relied on building organizational and interpersonal relationships with the NM community to help distribute the flyers and ads created in the previous strategies via email outreach. The NM OUT Business Alliance is an advocacy organization that seeks to “advance the common business interests, economic growth, and equality in the workplace and society for its LGBTQ members, businesses, and allies by providing educational, networking, and community building opportunities” (27). Toward their goal of cultivating certified suppliers, they offer a free certification for businesses and approximately 100 business in NM were advertised on their webpage in early 2021. We identified the publicly available email addresses for contacts listed on their online directory and sent them flyers.
We also partnered with the UNMCCC’s Office of Community Outreach and Engagement to promote the study outreach activities (e.g., regular newsletters sent out to members) and listservs. Similar efforts were undertaken through connections made with the NM Cancer Council (28), New Mexico State University’s Community Health Education Core, the University of New Mexico Health Sciences Center (UNM HSC) LGBTQ Collaborative (29), the UNM LGBTQ Resource Center (30), and Transgender Resource Center of New Mexico (31). Finally, laminated flyers (a requirement imposed due to the ongoing COVID-19 pandemic in order to make them easy to disinfect and clean) were placed in clinical and community settings (including the Southeast Heights Family Health Clinic (32) and the UNM Truman Clinic (33), (both providing care for the SGD populations in Albuquerque, NM) across the state, through study team relationships. Additionally, study team members searched for LGBTQIA+ Facebook groups throughout the state and sent them a message containing the flyer and Facebook ad, asking them to post to their pages.
All study procedures received approval from University of New Mexico’s Human Research Protection Office (Study number 20-393). All surveys were managed using Research Electronic Data Capture (REDCap) tools hosted by the University of New Mexico (34, 35), that provides a secure, web-based application designed to support data collections for research studies. The surveys were designed in English and translated into Spanish by a certified translation specialist, and both English and Spanish versions were used for data collection. All surveys were pilot tested by the research team and a small group of volunteers prior to data collection. The surveys were designed with two specific objectives (1): to screen individuals that could participate in the survey, and (2) to elicit individual’s self-report of cancer screening and prevention practices.
The eligibility survey (Supplementary Appendix 1A, 1B) queried about their age range, NM resident status, whether they were a member of SGD community, and how they heard about the study. If respondents answered that they were between 21-80 years old, were a resident of NM, and were members of the SGD community, they were considered eligible These criteria were used to specifically recruit individuals in the age range where cervical (21 – 65 years), breast (50 – 75 years), colorectal (45 – 36), and lung cancer (50 – 80 years) screenings are recommended (18, 19, 34, 35) and those who were members of the NM SGD community. All flyers, ads, and emails contained QR codes and/or links to a survey in both English and Spanish. All responses to the eligibility screener were reviewed by the study team weekly and duplicate emails, incomplete, and ineligible responses were removed.
All eligible respondents received the cancer prevention practices survey (Supplementary Appendix 2A, 2B) which was adapted from the annual and lifetime surveys developed by the PRIDE study (37). We asked questions about demographics, body organs, physical health, Human Papillomavirus (HPV) vaccination, health care access, cancer screening practices (for cervical, breast, colorectal, and lung cancer) as well as what influenced these practices, and whether they would like to hear from us regarding study findings. Branching logic was applied depending on the age of the participant, their current body organs, whether they had been diagnosed with the type of cancer that was being asked about, and certain behaviors (i.e., if they had smoked at least 100 cigarettes in their lifetime for lung cancer screening). Two open-ended questions asked about anything else they would like to share about their health and if they had any additional comments about the survey. A total of 45-73 close-ended questions and two open-ended questions were included in the final survey. The survey was pre-tested and estimated to take 10-20 minutes, depending on branching logic.
To determine how many respondents were residents of rural counties, we asked the survey respondents to provide zip codes. We matched these with State-County-Tract FIPS codes, which were then matched with 2010 RUCA codes (7). The HRSA definition defines rural as all non-metro counties, tracts with RUCA codes between 4-10, and large metro tracts of at least 400 square miles in an area with a population density of 35 or less per square mile with RUCA codes 2-3. HRSA uses this definition to decide which areas are eligible for rural health funding (38). This definition of rural was then used to determine the percentage of respondents that provided a zip code in a rural area in NM.
The cancer prevention practices survey was sent to the eligible respondents either by email with a unique link to the survey or a paper copy of the survey mailed to their addresses, either in English or Spanish depending on their indicated preference in the eligibility survey. Emails that failed to deliver or bounced back were removed by default. We sent three reminders to those who requested the online version of the survey. The first 200 eligible participants who completed the survey received $20 provided in acknowledgement of the respondent’s time and expertise via Amazon gift card codes.
Having respondents complete the eligibility survey before the cancer prevention practices survey allowed researchers to exclude social bots [software that is programmed to enter many responses in order to receive incentives (39)], duplicates, and ineligible respondents. Despite these phased approaches, there were instances of duplicate qualitative responses in the survey data, which triggered an additional search for strategies to ensuring data quality. We followed the detailed and systematic guidance provided by Pozzar and colleagues (40), in ensuring quality of data collected through social media research. Based on guidance from this research, we defined and operationalized four fraudulent and 17 suspicious criteria (details on the list of fraudulent and suspicious criteria are provided in Table 1). We removed responses with one fraudulent criterion or three or more suspicious criteria.
For fraudulent criteria, we considered responses that had (1) mismatched email addresses noted in answers from the same respondent (2); exact matches in qualitative responses greater than three words (3); reported non-US zip codes; and (4) reported to be heterosexual and cisgender. The 17 suspicious criteria broadly fell under four categories of responses with (1): non-NM zip codes (2); Height greater than or equal to 7feet or less than 4 feet and weight less than 90 pounds (3); nonsensical qualitative responses; and (4) incongruence between SAAB (sex assigned at birth), gender identity, sexual orientation, and current body organs. This last category considered suspicious were based on definitions of terms (i.e., “transgender”, “cisgender”, “straight” and “lesbian”) (42, 47) as well as current practices in genital gender affirmation surgeries (43–46).
The strategies of recruitment and data quality assurance detailed above collectively contributed to the recruitment of the overall sample of 2,534 respondents included in the analysis for this study. The overall study flow is shown in Figure 4. With the EDDM program, we selected over 61 mailing routes across the state where 27,369 flyers (highlighted as Direct Mail in Figure 5; this figure was altered in the form of color change to increase visibility and accessibility) were distributed to the residential addresses. The EDDM vendor provided detailed data (see Figure 5) on the overlapping strategy for the targeted Google Ads and Facebook Ads to residents on these mailing routes that collectively led to 393,523 impressions [i.e. how many times an ad was displayed on a person’s screen for Facebook (48) or on a search result page for Google (49)], resulting in 686 clicks (i.e. how many times a person clicked on the ad). The same vendor also sent 15,284 emails, of which 7,595 were delivered, 52 were opened, and 15 people clicked on the content inside the email. Based on these numbers, we believed we reached a total of 436,177 individuals, with the total cost of 3¢ per person reached (i.e. 436,177 impressions) or approximately $6 per complete response (i.e. 2,534 responses included in the final analyses) including incentives for the first 200 respondents (50).
Although it was difficult to estimate the reach of the other strategies that utilized the team members and organizational connections in the community, we asked survey respondents how they heard about the study in both the eligibility survey and the cancer screening practices survey. Tables 2.1, 2.2 presents detailed data on these responses; overall, however, respondents noted social media as the most common way they heard about the study. In seven weeks of data collection, we received a total of 6,920 responses on the eligibility survey (English:6,139; Spanish:781). Of these, 27% (n=1,888) were duplicate, incomplete, or ineligible responses with the majority (98%) being duplicate responses that were likely sent from bots. We sent 5,032 unique survey links and mailed five paper surveys. No paper surveys were returned, and we received 3,120 complete online responses (English:2,811; Spanish:309), indicating a response rate of 62%. Survey responses were received from 163 unique NM zip codes and 18% reported living in rural areas in NM as defined by the HRSA (38).
As shown in Table 1, of the 3,120 responses, 16% (n=489) were fraudulent and were removed. Of the remaining 2,631 respondents, 4% (n=97) met three or more criteria for being deemed suspicious and were excluded from analysis, leaving a total of 2,534 responses included in analysis. Thirteen percent (n=330) met two or more of the suspicious criteria and 30% (n=788) met at least one suspicious criterion, neither of which were grounds for removal from analysis.
Table 3 provides detailed data about the characteristics of the survey respondents included in the final analysis (n=2534). Over half of the respondents (55.3%) were assigned male at birth, 40.4% were assigned female at birth, and 4.3% were assigned intersex at birth. Transgender respondents made up 10.6% (n=267) of the study sample, while 46.1% of respondents reported being cisgender men and 33.8% reported being cisgender women. In terms of sexual orientation, 54.1% (n=1371) reported being gay or lesbian, 30% (n=749) bisexual, and 15.8% (n=401) queer. Around 85% of the respondents were between the age of 21-40 years. Black, Hispanic, and American Indian/Alaska Native respondents comprised 39.6% of the respondents. Regarding education, income, and employment, 43.7% reported high school or some vocational training as their highest level of education, 45.9% had an annual household income below $50,000, and 19% reported being unemployed.
In relation to their access to health care (shown in Table 4), 22.3% (n=564) reported being uninsured, 27.3% (n=691) reported not having a place to go to for routine check-ups, and 42.2% (n=1069) reported unnecessary delays in getting medical care in their lifetime. Overall, 66.3% reported having a primary care provider, however, in the past 12 months, 30% had not seen their provider. In the past 12 months, 47% reported having no insurance, 34% had trouble finding a provider, and 55.5% reported being unable to obtain care. Overall, 31.1% reported being denied or given lower quality medical care in the past 12 months. Among the 797 respondents that were asked about cervical cancer screening, 66.2% (n=528) of pap smear-eligible respondents reported ever being screened with Pap smears. Similarly, 78.6% (n=55) of the 70 mammogram-eligible respondents reported ever receiving a mammogram, 84.1% (n=53) of the 63 colorectal cancer screening-eligible respondents had ever been screened for colorectal cancer, and 33.3% (n=5) of the 15 lung cancer screening-eligible respondents reported ever being screened for lung cancer. A total of 756 (29.8%) people reported receiving a cancer diagnosis. Of respondents who were eligible (i.e. below 46 years old) for the HPV vaccine (n=2379), 58.7% reported receiving a vaccine for HPV.
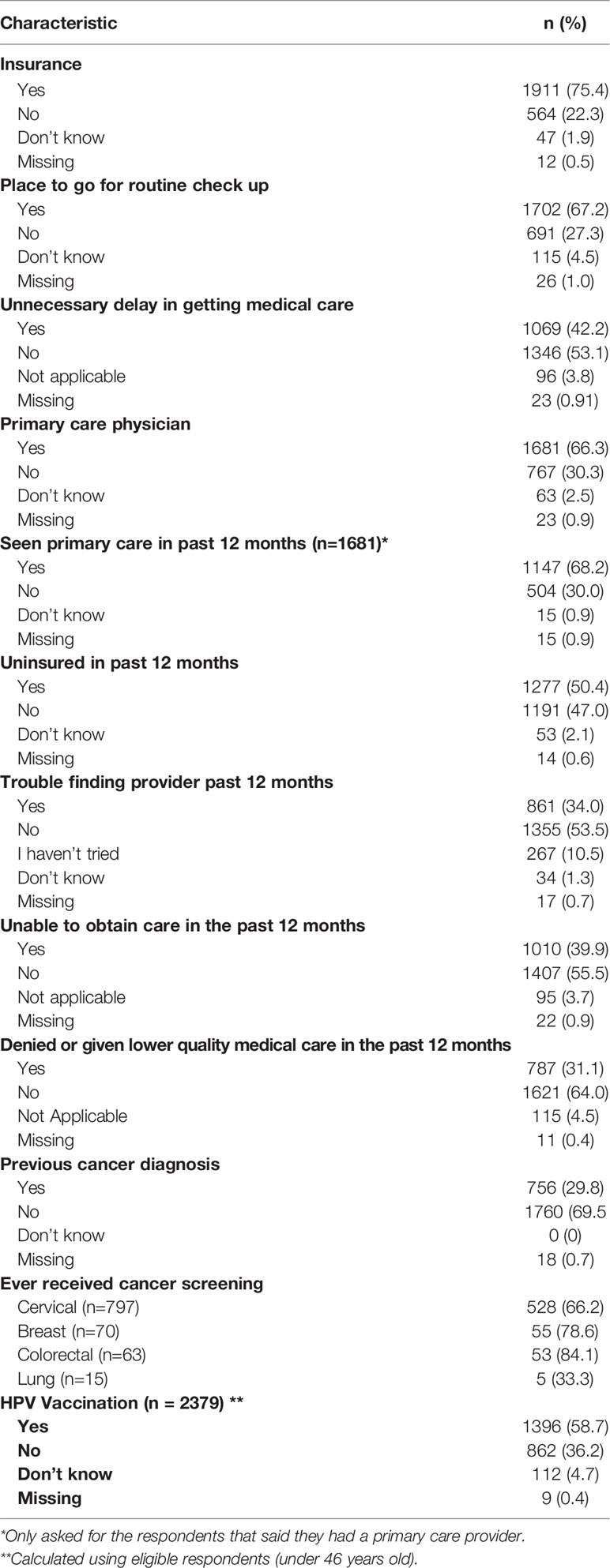
Table 4 Characteristics of the population in terms of access to care and cancer prevention practices.
A total of 1752 (69%) respondents confirmed that they would like to hear from us regarding study findings and 371 (47%) respondents with a cervix answered that they would be interested in participating in a focus group about cervical cancer screening. On the open-ended questions, many respondents expressed their appreciation of the inclusive nature of the survey in queries around sexual orientation and gender identity (SOGI) status. For example, a respondent stated,
“Appreciated the survey trying really hard to be gender and orientation inclusive! I think fat shaming comes up for a lot of queer and trans folks as well so I appreciated that note…”
Other participants noted the importance of such a study and the resources for their community, stating:
“Thank you for doing this study! It’s very important and I appreciate that you are doing this work … Thank you for conducting a survey on such an important topic and for providing excellent resources at the end. I didn’t know about some of these resources and hope to reach out for myself and share them with others”.
Reaching SGD populations has been a challenge for the field of health research and it is crucial to find ways to mitigate this issue, especially in regards to research on healthcare and health behaviors (51, 52). This paper highlights the variety of methods (i.e. flyers, social media, organizational, and personal outreach) available to the cancer research community to reach diverse populations. We also present additional considerations to ensure that survey questions are asked in a respectful, culturally appropriate manner, which is especially important when surveying populations that have been marginalized. Finally, as opposed to conceptual guidance, we present detailed guidance on how we applied strategies, informed by prior social media research (40, 51, 53), to ensure data quality for SGD research.
To our knowledge, this is one of the few studies to employ EDDM to distribute flyers for an online, population-based health survey (54, 55). This survey’s ability to reach individuals from rural areas of the state indicates that utilizing social media and USPS is likely to be an effective method for states with significant rural populations when seeking diverse engagement. Among younger SGD populations, social media has been used successfully to engage and recruit participants (56). However, its use remains limited in engaging rural and adult populations (15), both of whom remain significantly underrepresented in population-based SGD research. Innovative and systematic efforts are needed in order to develop meaningful interventions that address the healthcare needs of marginalized rural SGD individuals (57). In this study, more than 85% of respondents were between 21-40 years old, so additional methods may be needed to support recruitment for the over-40 SGD community. Some studies have had success with crowdsourcing platforms (58) and other methods, such as referrals from current participants and review of electronic medical records to identify eligible participants (59). However, social media provides an important opportunity to engage the SGD community with the potential for future public health interventions and behavioral research. In previous public health studies, impressions have been considered to be equivalent to reaching populations, while clicks indicated the actual behavior of the person (53, 60).
Advocates for promoting SGD research express that these populations are eager to participate in research, especially if their participation can benefit their community (57). This might partly explain the overwhelming response to our recruitment strategies (i.e. 62% response rate). The survey took anywhere from 10-20 minutes to complete and had a monetary incentive, which may have further influenced the response rate. We surmise that another reason for the high number of responses was because people spent most of their time at home during a major wave of the COVID-19 pandemic that occurred in early 2021, which was when we started recruiting participants. However, other research done during the COVID-19 pandemic provides contrasting data. While survey-based research increased significantly during the pandemic, people’s responses to surveys tended to decline. The Census found that responses to surveys initially increased at the start of the pandemic, but declined and remained lower than non-pandemic years around the summer of 2020 (61). It has been suggested that the three-fold increase in social media-based recruitment and online survey administration during the pandemic likely led to “survey fatigue.” (62)
Another potential justification for the large number of respondents may be that we ensured an appropriate inquiry into SOGI status for the respondents. As mentioned above, the comments left at the end of the survey indicated appreciation for the respectful ways in which the questions were asked, and gratitude that the research was being conducted in the first place. These responses underscore the importance of gender expansive, non-heteronormative language in both research and healthcare. Using gendered and heteronormative language can alienate SGD populations and lead to reduced care-seeking practices (63). This highlights the need for using gender expansive language in educational materials as well as in intake forms and when speaking to patients and other healthcare providers.
Social media and other internet-based methods are considered to be cost-effective and often provide greater reach to the populations of interest (64, 65). However, they do present issues with people enrolling more than once, social bots, and respondents who do not fit the eligibility criteria (40, 65). Additional strategies to manage this type of data collection and prevent/detect fraudulent responses are necessary (40). We created consistent criteria with which to evaluate responses in order to determine authenticity and mitigate fraud. We also filtered out-of-country zip codes, along with removing any users with identical answers to open-ended questions. These methods proved to be efficient for removing many of the most obviously fraudulent responses. Less apparent instances of fraud were difficult to detect, but employing parameters such as height and weight, as well as incongruent answers to SAAB and gender, to deem a response fraudulent or suspicious worked well in this study’s data cleaning process. These criteria, however, were challenging to apply for the intersex population in this study and may partially explain their higher proportion (4.3%) in the study sample compared to rest of the population (1.7%) (66).
Compared to the Williams Institute, there were slightly more respondents in our study who reported male gender, with 51% of study respondents reporting male gender versus 45% from the Williams Institute. There were also more white respondents in our study (52.2% vs 43%). Respondents in our study had higher educational attainment with 55.7% of them reporting post-graduate schooling versus 16% reported from the Williams Institute (2). Access to care for this study population reflects previous studies (67), in that it shows lower insurance rates among SGD populations as well as a lower number of SGD individuals reporting having a primary care provider. The uninsured rate in this study population (22.0%) higher than the state average for adults 19 – 64 years old (18.8%) (68, 69), and the percentage of individuals with a primary care provider (66.3%) is also lower than the state average of 71.5% (70). These data represent a troubling trend around access to care for SGD populations which can lead to decreased rates of cancer screening services as well as treatment for other serious conditions (71). This disparity in access to care is likely multifactorial with stigmatization and discrimination in healthcare (72, 73) as well as in the workplace being a large contributor (74). Stigmatization and discrimination in healthcare can lead to SGD individuals’ decreased interaction with the healthcare system (71, 72), while discrimination in the workplace can lead to lower insurance rates among this population (74). Additionally, results gathered by this study illustrate the impact that COVID-19 has had on the healthcare field and the accessibility of services for all populations (75)., showing decreased access to care over the previous 12 months. This impact was more pronounced among populations that experience inequities due to their rural residence, since a common solution for access to care during the pandemic was telehealth, which, further exacerbated the digital divide in these communities and a considerable drop in cancer screening (36, 76).
About 69% of the survey respondents expressed interest in staying engaged and finding out more about the study. Respectful of this enthusiasm and in line with the guidance from the cancer research community working with SGD populations, we are committed to centering the study findings and future research within community perspectives (40, 63, 64). We utilized the Community Engagement Studio (CES) as a strategy to build relationships within the community. The CES is a consultative model that allows for research specific consultations from community members, often led by the Clinical Translational Center (60, 61). We conducted a Community Engagement Studio (CES) with 11 members from the NM SGD community. Conversations with the community members helped gather insights on communication strategies, future research endeavors, and opportunities to collaborate with the SGD community in NM. When asked about engagement, studio participants described their preferences in not using the term “sexual gender diverse communities” because they did not identify with the term, and instead preferred being referred to as the “LGBTQ+” community. Several mentioned the need for quick, relevant communication materials to engage the community (e.g., a 60-90 second video via Tik-Tok, YouTube, or Instagram/Facebook stories, or an Instagram/Twitter infographic with a “link in bio” or QR code). The group mentioned engaging young adults early in prevention, educating clinicians on the importance of inclusive language, collaborating with clinics that have direct trans and queer healthcare provision experience, and addressing the bias against the community from the medical providers. The majority of the community experts expressed interest in continued future discussions and we hope to engage them as a study-specific advisory council for gathering guidance on future research endeavors.
As with most research, this study is subject to certain limitations. These limitations primarily result from the use of a purposive sampling technique, volunteer bias, and the use of the internet to both recruit participants and to administer the survey. Purposive sampling, a process in which researchers pick particular segments of the population to recruit for a study, is prone to researcher bias and can result in a lack of generalizability (77). Such a strategy was suitable, because this was a pilot study aimed at gaining a preliminary understanding of the cancer screening practices of the SGD community in NM. Using purposive sampling to determine whether or not a perceived issue needs more research and resources devoted to it is widely regarded as a reasonable and effective use of this sampling method despite its inherent limitations (77). Even though two of our four methods relied on personal and organizational outreach, these relationships (i.e., community outreach and engagement offices in cancer centers, and LGBTQ-friendly businesses, among others) exist in several academic-community environments and could be leveraged for similar research studies. We also did not send survey links to people who requested paper surveys because they only provided a postal mailing address in the eligibility. Similarly, we did not attempt to send a paper survey to respondents who did not complete the online survey because they did not provide a postal mailing address. Older people are less likely to respond to web-based surveys (78) and it is likely that we could have had a higher proportion of older LGBTQIA+ adults with the paper survey.
Volunteer bias may have also played a role in our research, as it does in most survey-based studies. The pool of respondents was undoubtedly limited by the fact that participants were asked to answer questions regarding their sexual orientation and gender identity. Many people are not willing or not able to be open with such intimate information. This also applies to other portions of the survey, such as questions that asked about anatomy, cervical cancer screening, or colorectal cancer screening. Many people are not comfortable discussing such topics, and thus those who chose to participate in this survey were likely only a subset of the SGD population in NM. Furthermore, the recruitment flyers advertised a monetary incentive, which may have biased participation towards those experiencing financial need.
Finally, using the internet for reaching these populations can be limiting, as internet access in NM is poor, ranking 45th in the country (18). Internet-based research also typically reaches individuals of higher socioeconomic status and a younger population sample, which may not be representative of the target population (79). Younger people tend to use technology more than older people, which aligns with our findings that over 80% of survey respondents were under 40 years old (80). We believe that some of these barriers were overcome by mailing out flyers. Flyers however, were only delivered to individuals with residential addresses. This is especially pertinent information to take into account when doing research with the SGD community whose members, on average, experience homelessness more than twice as much as their cisgender, heterosexual counterparts (81).
To reach state-wide SGD communities and engage them in population-based research, innovative and systematic efforts are needed. Social media and postal flyers may provide successful recruitment opportunities with potential to use these methods for future public health interventions in these populations. When using the online surveys to maximize reach, additional strategies to manage these data and prevent/detect fraudulent responses are needed. While time-intensive, the methods in this study were an effective way to ensure accurate data and to narrow down the responses to include only genuine answers that each represented one individual. Findings from this paper have the potential to maximize data integrity and prevent misrepresentation of health data for these communities.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by University of New Mexico’s Human Research Protection Office (Study number 20-393). The participants provided their written informed consent to participate in this study.
PA, conceptualized the article and PA, KM, and TJ drafted the manuscript. DK, VP, BT, EW, MM, SM, MK, and PM participated in the workgroup discussions that informed the manuscript making substantial contributions to the design and analysis presented in the paper and revised it critically for important intellectual content. All authors contributed to the article and approved the submitted version.
The research reported in this paper was funded by an Internal Research Grant (PI: PA) from the American Cancer Society 131567-IRG-17-178-22-IRG (PI: Ozbun, M.) and was partially supported by UNM Comprehensive Cancer Center Support Grant NCI P30CA118100 and the Behavioral Measurement and Population Sciences shared resource. The Community Engagement Studio received support from the University of New Mexico’s Clinical Translational Science Center.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors wish to thank all participants in the research study for their time and insights, as well as the contributions of Karen Quezada and David Rogers. The authors would also like to acknowledge support from the University of New Mexico Health Sciences Center Biostatistical Shared Resource, the New Mexico Out Business Alliance, the Transgender Resource Center of New Mexico, the University of New Mexico Comprehensive Cancer Center’s Office of Community Outreach and Engagement, the Comprehensive Cancer Coalition in New Mexico, the New Mexico Cancer Council, the University of New Mexico Health Sciences Center LGBTQ Collaborative, the University of New Mexico LGBTQ Resource Center, the New Mexico State University’s Community Health Education Core, PFLAG Silver City, and the New Mexico Department of Health. The authors also wish to thank the participants of the Community Engagement Studio and the University of New Mexico’s Clinical Translational Science Center Community Engagement Research Core (UNM CTSC CERC) team for leading the studio.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2022.841951/full#supplementary-material
Supplementary Appendix 1A | Eligibility survey in English.
Supplementary Appendix 1B | Eligibility survey in Spanish.
Supplementary Appendix 2A | Cancer prevention practices survey in English.
Supplementary Appendix 2B | Cancer prevention practices survey in Spanish.
EDDM, Every Door Direct Mail; HPV, Human Papillomavirus; HRSA, Health Resources and Services Administration; LGBTQIA, Lesbian, Gay, Bisexual, Transgender, Queer, Intersex, Asexual + many other sexual orientations and genders; REDCap, Research Electronic Data Capture; RUCA, Rural-Urban Commuting Area; SAAB, Sex Assigned at Birth; SGD, Sexual and Gender Diverse; SOGI, Sexual Orientation and Gender Identity; UNMCCC, University of New Mexico Comprehensive Cancer Center; USPS, United States Postal Service.
1. Jones JM. Lgbt Identification Rises to 5.6% in Latest U.S. Estimate (2021). Available at: https://news.gallup.com/poll/329708/lgbt-identification-rises-latest-estimate.aspx.
2. Quickfacts New Mexico (2019). Available at: https://www.census.gov/quickfacts/NM.
3. Complete Health Indicator Report of New Mexico Population - Language Other Than English Spoken at Home. New Mexico Department of Health, Indicator-Based Information System for Public Health (2019). Available at: https://ibis.health.state.nm.us/indicator/complete_profile/NMPopDemoNoEnglish.html.
4. Shrider EA, Kollar M, Chen F, Semega J. U.S. Census Bureau, Current Population Reports, P60-273, Income and Poverty in the United States: 2020, Washington, DC: U.S. Government Publishing Office (2021).
5. Dalaker J. The 10-20-30 Provision: Defining Persistent Poverty Counties. Congressional Research Service (2021).
6. Zahnd WE, Murphy C, Knoll M, Benavidez GA, Day KR, Ranganathan R, et al. The Intersection of Rural Residence and Minority Race/Ethnicity in Cancer Disparities in the United States. Int J Environ Res Public Health (2021) 18(4):1384. doi: 10.3390/ijerph18041384
7. Rural-Urban Commuting Area Codes. U.S. Department of Agriculture (2020). Available at: https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/.
8. Lgbt Demographic Data Interactive. UCLA School of Law (2019). Available at: https://williamsinstitute.law.ucla.edu/visualization/lgbt-stats/?topic=LGBT#about-the-data.
9. Hulko W, Hovanes J. Intersectionality in the Lives of LGBTQ Youth: Identifying as LGBTQ and Finding Community in Small Cities and Rural Towns. J Homosexual (2018) 65(4):427–55. doi: 10.1080/00918369.2017.1320169
10. McGarrity LA, Huebner DM. Is Being Out About Sexual Orientation Uniformly Healthy? The Moderating Role of Socioeconomic Status in a Prospective Study of Gay and Bisexual Men. Ann Behav Med (2013) 47(1):28–38. doi: 10.1007/s12160-013-9575-6
11. Manuel JI. Racial/Ethnic and Gender Disparities in Health Care Use and Access. Health Serv Res (2018) 53(3):1407–29. doi: 10.1111/1475-6773.12705
12. Gonzales G, Henning-Smith C. Barriers to Care Among Transgender and Gender Nonconforming Adults. Milbank Q (2017) 95(4):726–48. doi: 10.1111/1468-0009.12297
13. Fiscella K, Williams DR. Health Disparities Based on Socioeconomic Inequities: Implications for Urban Health Care. Acad Med (2004) 79(12):1139–47. doi: 10.1097/00001888-200412000-00004
14. Willging C. "I'm Not That Innocent": Recruiting Sexual and Gender Minorities for Rural Mental Health Research. Practicing Anthropol (2007) 29(2):10–4. doi: 10.17730/praa.29.2.3t6r78t4366563q1
15. Henriquez NR, Ahmad N. “The Message Is You Don't Exist”: Exploring Lived Experiences of Rural Lesbian, Gay, Bisexual, Transgender, Queer/Questioning (Lgbtq) People Utilizing Health Care Services. SAGE Open Nur (2021) 7:23779608211051174. doi: 10.1177/23779608211051174
16. Russomanno J, Patterson JG, Jabson Tree JM. Social Media Recruitment of Marginalized, Hard-to-Reach Populations: Development of Recruitment and Monitoring Guidelines. JMIR Public Health Surveill (2019) 5(4):e14886. doi: 10.2196/14886
17. Forstie C. Theory Making From the Middle: Researching LGBTQ Communities in Small Cities. City Community (2020) 19:153–168. doi: 10.1111/cico.12446
18. Service USP. Using Every Door Direct Mail . Available at: https://www.usps.com/business/every-door-direct-mail.htm.
19. Taradel. Taradel: Target Smart (2019). Available at: https://www.taradel.com/.
20. Service USP. Every Door Direct Mail - User Guide. (2017). Available at: https://www.usps.com/business/pdf/every-door-direct-mail-user-guide.pdf.
21. Median Household Income . Available at: https://ibis.health.state.nm.us/.
22. Force USPST, Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, et al. Screening for Lung Cancer: US Preventive Services Task Force Recommendation Statement. JAMA (2021) 325(10):962–70. doi: 10.1001/jama.2021.1117
23. Force USPST, Davidson KW, Barry MJ, Mangione CM, Cabana M, Caughey AB, et al. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA (2021) 325(19):1965–77. doi: 10.1001/jama.2021.6238
24. Force USPST, Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, et al. Screening for Cervical Cancer: US Preventive Services Task Force Recommendation Statement. JAMA (2018) 320(7):674–86.
25. Siu AL, Force USPST. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med (2016) 164(4):279–96. doi: 10.7326/M15-2886
26. Media V. About This Project (2020). Available at: https://genderphotos.vice.com/guidelines.
27. Alliance NMOB. Welcome to NMOBA (2021). Available at: https://www.nmoba.org/.
28. Council NMC. Nm Cancer Council (2021). Available at: https://www.nmcancercouncil.org/.
30. Mexico TUON. Lgbtq Resource Center . Available at: http://lgbtqrc.unm.edu/.
31. TGRCNM. Transgender Resource Center of New Mexico (2021). Available at: https://tgrcnm.org/.
32. Mexico TUON. Primary Care Locations (2021). Available at: https://unmhealth.org/services/primary-care/locations.html.
33. Mexico TUON. Helping You Live a Healthy Life: Respectful, Private HIV & AIDS Care (2021). Available at: https://unmhealth.org/services/hiv-aids/.
34. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, et al. The REDCap Consortium: Building an International Community of Software Platform Partners. J BioMed Inform (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208
35. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (Redcap)–A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J BioMed Inform (2009) 42(2):377–81. doi: 10.1016/j.jbi.2008.08.010
36. Jaffe DH, Lee L, Huynh S, Haskell TP. Health Inequalities in the Use of Telehealth in the United States in the Lens of COVID-19. Popul Health Manag (2020) 23(5):368–77. doi: 10.1089/pop.2020.0186
37. Lunn MR, Lubensky M, Hunt C, Flentje A, Capriotti MR, Sooksaman C, et al. A Digital Health Research Platform for Community Engagement, Recruitment, and Retention of Sexual and Gender Minority Adults in a National Longitudinal Cohort Study—The PRIDE Study. J Am Med Inf Assoc (2019) 26(8-9):737–48. doi: 10.1093/jamia/ocz082
38. Policy FOORH. Defining Rural Population. Health Resources & Services Administration (2021). Available at: https://www.hrsa.gov/rural-health/about-us/definition/index.html.
39. Allem J-P, Ferrara E. Could Social Bots Pose a Threat to Public Health? Am J Public Health (2018) 108(8):1005–6. doi: 10.2105/AJPH.2018.304512
40. Pozzar R, Hammer MJ, Underhill-Blazey M, Wright AA, Tulsky JA, Hong F, et al. Threats of Bots and Other Bad Actors to Data Quality Following Research Participant Recruitment Through Social Media: Cross-Sectional Questionnaire. J Med Internet Res (2020) 22(10):e23021. doi: 10.2196/23021
41. NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, Treatment of Obesity in Adults (US) Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda (MD): National Heart, Lung, and Blood Institute. (1998). Available at: https://www.ncbi.nlm.nih.gov/books/NBK2003/
42. Silva TJ. Straight Identity and Same-Sex Desire: Conservatism, Homophobia, and Straight Culture. Soc Forces (2018) 97(3):1067–94. doi: 10.1093/sf/soy064
43. Safa B, Lin WC, Salim AM, Deschamps-Braly JC, Poh MM. Current Concepts in Feminizing Gender Surgery. Plast Reconstr Surg (2019) 143(5):1081e–91e. doi: 10.1097/PRS.0000000000005595
44. Danker S, Esmonde N, Berli JU. "Staging" in Phalloplasty. Urol Clin North Am (2019) 46(4):581–90. doi: 10.1016/j.ucl.2019.07.011
45. Jones BP, Williams NJ, Saso S, Thum MY, Quiroga I, Yazbek J, et al. Uterine Transplantation in Transgender Women. BJOG (2019) 126(2):152–6. doi: 10.1111/1471-0528.15438
46. Safa B, Lin WC, Salim AM, Deschamps-Braly JC, Poh MM. Current Concepts in Masculinizing Gender Surgery. Plast Reconstr Surg (2019) 143(4):857e–71e. doi: 10.1097/PRS.0000000000005453
47. Campaign THR. Glossary of Terms . Available at: https://www.hrc.org/resources/glossary-of-terms.
48. Facebook. What's the Difference Between Page Views, Reach and Impressions on Facebook? : Meta (2021). Available at: www.facebook.com/help/274400362581037/?helpref=uf_share.
49. Google. Impressions: Definition (2021). Available at: https://support.google.com/google-ads/answer/6320.
50. Ramo DE, Rodriguez TM, Chavez K, Sommer MJ, Prochaska JJ. Facebook Recruitment of Young Adult Smokers for a Cessation Trial: Methods, Metrics, and Lessons Learned. Internet Interv (2014) 1(2):58–64. doi: 10.1016/j.invent.2014.05.001
51. Guillory J, Wiant KF, Farrelly M, Fiacco L, Alam I, Hoffman L, et al. Recruiting Hard-to-Reach Populations for Survey Research: Using Facebook and Instagram Advertisements and In-Person Intercept in LGBT Bars and Nightclubs to Recruit Lgbt Young Adults. J Med Internet Res (2018) 20(6):e197. doi: 10.2196/jmir.9461
52. Salk RH, Thoma BC, Choukas-Bradley S. The Gender Minority Youth Study: Overview of Methods and Social Media Recruitment of a Nationwide Sample of U.S. Cisgender and Transgender Adolescents. Arch Sex Behav (2020) 49(7):2601–10. doi: 10.1007/s10508-020-01695-x
53. McInroy LB. Pitfalls, Potentials, and Ethics of Online Survey Research: LGBTQ and Other Marginalized and Hard-to-Access Youths. Soc Work Res (2016) 40(2):83–94. doi: 10.1093/swr/svw005
54. Al-Muhanna K, Plakias Z, Hanks A, Garner J, Glenn J. O32 Leveraging Every Door Direct Mail for Remote Recruitment of a Rural Study Sample: Response Rate and Representativeness. J Nutr Educ Behavior (2021) 53(7, Supplement):S15. doi: 10.1016/j.jneb.2021.04.041
55. Grubert E. Every Door Direct Mail in US Survey Research: An Anonymous Census Approach to Mail Survey Sampling. Methodol Innovations (2019) 12(2):2059799119862104. doi: 10.1177/2059799119862104
56. Escobar-Viera CG, Melcher EM, Miller RS, Whitfield DL, Jacobson-López D, Gordon JD, et al. A Systematic Review of the Engagement With Social Media–Delivered Interventions for Improving Health Outcomes Among Sexual and Gender Minorities. Internet Interv (2021) 25:100428. doi: 10.1016/j.invent.2021.100428
57. Waters AR, Tennant K, Cloyes KG. Cultivating LGBTQ+ Competent Cancer Research: Recommendations From LGBTQ+ Cancer Survivors, Care Partners, and Community Advocates. Semin Oncol Nur (2021) 37(6):151227. doi: 10.1016/j.soncn.2021.151227
58. Turner AM, Engelsma T, Taylor JO, Sharma RK, Demiris G. Recruiting Older Adult Participants Through Crowdsourcing Platforms: Mechanical Turk Versus Prolific Academic. AMIA Annu Symp Proc (2020) 2020:1230–8.
59. Wood SF, Brooks J, Eliason MJ, Garbers S, McElroy JA, Ingraham N, et al. Recruitment and Participation of Older Lesbian and Bisexual Women in Intervention Research. Womens Health Issues (2016) 26 Suppl 1:S43–52. doi: 10.1016/j.whi.2016.04.003
60. Huesch MD, Galstyan A, Ong MK, Doctor JN. Using Social Media, Online Social Networks, and Internet Search as Platforms for Public Health Interventions: A Pilot Study. Health Serv Res (2016) 51 Suppl 2(Suppl 2):1273–90. doi: 10.1111/1475-6773.12496
61. Statistics USBOL. Effects of COVID-19 Pandemic and Response on the Consumer Expenditure Surveys. United States Department of Labor (2021). Available at: https://www.bls.gov/covid19/effects-of-covid-19-pandemic-and-response-on-the-consumer-expenditure-surveys.htm.
62. de Koning R, Egiz A, Kotecha J, Ciuculete AC, Ooi SZY, Bankole NDA, et al. Survey Fatigue During the COVID-19 Pandemic: An Analysis of Neurosurgery Survey Response Rates. Front Surg (2021) 8:690680. doi: 10.3389/fsurg.2021.690680
63. Stroumsa D, Wu JP. Welcoming Transgender and Nonbinary Patients: Expanding the Language of "Women's Health". Am J Obstet Gynecol (2018) 219(6):585.e1–.e5. doi: 10.1016/j.ajog.2018.09.018
64. Griffin M, Martino RJ, LoSchiavo C, Comer-Carruthers C, Krause KD, Stults CB, et al. Ensuring Survey Research Data Integrity in the Era of Internet Bots. Qual Quant (2021), 1–12. doi: 10.1007/s11135-021-01252-1
65. Campbell RM, Venn TJ, Anderson NM. Cost and Performance TraOdeoffs Between Mail and Internet Survey Modes in a Nonmarket Valuation Study. J Environ Manag (2018) 210:316–27. doi: 10.1016/j.jenvman.2018.01.034
66. Sax L. How Common is Intersex? A Response to Anne Fausto-Sterling. J Sex Res (2002) 39(3):174–8. doi: 10.1080/00224490209552139
67. Macapagal K, Bhatia R, Greene GJ. Differences in Healthcare Access, Use, and Experiences Within a Community Sample of Racially Diverse Lesbian, Gay, Bisexual, Transgender, and Questioning Emerging Adults. LGBT Health (2016) 3(6):434–42. doi: 10.1089/lgbt.2015.0124
69. KFF. State Health Facts - Distribution of the Nonelderly Uninsured by Age (2020). Available at: https://www.kff.org/other/state-indicator/distribution-of-the-nonelderly-uninsured-by-age-cps/?currentTimeframe=0&selectedDistributions=adults-19-64&selectedRows=%7B%22states%22:%7B%22new-mexico%22:%7B%7D%7D%7D&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
70. Primary Care Provider. New Mexico Department of Health (2018). Available at: https://ibis.health.state.nm.us/.
71. Romanelli M, Hudson KD. Individual and Systemic Barriers to Health Care: Perspectives of Lesbian, Gay, Bisexual, and Transgender Adults. Am J orthopsychiatry (2017) 87(6):714–28. doi: 10.1037/ort0000306
72. Willging C, Kano M, Green AE, Sturm R, Sklar M, Davies S, et al. Enhancing Primary Care Services for Diverse Sexual and Gender Minority Populations: A Developmental Study Protocol. BMJ Open (2020) 10(2):e032787. doi: 10.1136/bmjopen-2019-032787
73. Taskiran Eskici G, Alan H, Eskin Bacaksiz F, Gumus E, Cakir H, Harmanci Seren AK. Under the Same Rainbow: A Study on Homophobia and Discrimination Among Private Sector Health care Professionals. J Nurs Manage (2021) 29: 3–15. doi: 10.1111/jonm.13167
74. Cech E, Rothwell W. Lgbt Workplace Inequality in the Federal Workforce: Intersectional Processes, Organizational Contexts, and Turnover Considerations. ILR Review (2019) 73:001979391984350. doi: 10.1177/0019793919843508
75. Núñez A, Sreeganga SD, Ramaprasad A. Access to Healthcare During COVID-19. Int J Environ Res Public Health (2021) 18(6):2980. doi: 10.3390/ijerph18062980
76. Shah SK, McElfish PA. Cancer Screening Recommendations During the COVID-19 Pandemic: Scoping Review. JMIR Cancer (2022) 8(1):e34392. doi: 10.2196/34392
77. Sharma G. Pros and Cons of Different Sampling Techniques. Int J Appl Res (2017) 3(7):749–52. doi: 10.22271/allresearch
78. Yetter G, Capaccioli K. Differences in Responses to Web and Paper Surveys Among School Professionals. Behav Res Methods (2010) 42(1):266–72. doi: 10.3758/BRM.42.1.266
79. Jaap JA, Denissen LN, van Zalk M. How the Internet Is Changing the Implementation of Traditional Research Methods, Peopel’s Daily Lives, and the Way in Which Developmental Scientists Conduct Research. Int J Behav Dev (2010) 34(6):564–75. doi: 10.1177/0165025410383746
80. Czaja SJ, Charness N, Fisk AD, Hertzog C, Nair SN, Rogers WA, et al. Factors Predicting the Use of Technology: Findings From the Center for Research and Education on Aging and Technology Enhancement (Create). Psychol Aging (2006) 21(2):333–52. doi: 10.1037/0882-7974.21.2.333
81. Wilson BDM, Choi SK, Harper GW, Lightfoot M, Russell ST, Meyer IH, et al. Homelessness Among LGBT Adults in the US. Los Angeles, CA: The Williams Institute, UCLA School of Law (2020). Available at: http://bibpurl.oclc.org/web/94835.
Keywords: cancer screening (MeSH), sexual orientation, gender identity (MeSH), recruitment, cancer, cancer prevention
Citation: Myers KJ, Jaffe T, Kanda DA, Pankratz VS, Tawfik B, Wu E, McClain ME, Mishra SI, Kano M, Madhivanan P and Adsul P (2022) Reaching the “Hard-to-Reach” Sexual and Gender Diverse Communities for Population-Based Research in Cancer Prevention and Control: Methods for Online Survey Data Collection and Management. Front. Oncol. 12:841951. doi: 10.3389/fonc.2022.841951
Received: 23 December 2021; Accepted: 26 April 2022;
Published: 08 June 2022.
Edited by:
Hajo Zeeb, Leibniz Institute for Prevention Research and Epidemiology (LG), GermanyReviewed by:
Scherezade K. Mama, University of Texas MD Anderson Cancer Center, United StatesCopyright © 2022 Myers, Jaffe, Kanda, Pankratz, Tawfik, Wu, McClain, Mishra, Kano, Madhivanan and Adsul. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Prajakta Adsul, cGFkc3VsQHNhbHVkLnVubS5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.