- 1Department of General Surgery, Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2Department of Gastroenterology, Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
With the development of materials science and biomedicine, the application of nanomaterials in the medical field is further promoted. In the process of the diagnosis and treatment of diseases, a variety of drugs need to be used. It is an ideal state to make these drugs arrive at a specific location at a specific time and release at a specific speed, which can improve the bioavailability of drugs and reduce the adverse effects of drugs on normal tissues. Traditional drug delivery methods such as tablets, capsules, syrups, and ointments have certain limitations. The emergence of a new nano-drug delivery system further improves the accuracy of drug delivery and the efficacy of drugs. It is well known that the development of the cancer of the stomach is the most serious consequence for the infection of Helicobacter pylori. For the patients who are suffering from gastric cancer, the treatments are mainly surgery, chemotherapy, targeted and immune therapy, and other comprehensive treatments. Although great progress has been made, the diagnosis and prognosis of gastric cancer are still poor with patients usually diagnosed with cancer at an advanced stage. Current treatments are of limited benefits for patients, resulting in a poor 5-year survival rate. Nanomaterials may play a critical role in early diagnosis. A nano-drug delivery system can significantly improve the chemotherapy, targeted therapy, and immunotherapy of advanced gastric cancer, reduce the side effects of the original treatment plan and provide patients with better benefits. It is a promising treatment for gastric cancer. This article introduces the application of nanomaterials in the diagnosis and treatment of H. pylori and gastric cancer.
Introduction
Gastric cancer is the fifth most common cancer and fourth most deadly cancer in the world, causing more than 1 million new cases and about 769,000 deaths worldwide in 2020 (1). At present, the etiology of gastric cancer is not very clear, but it is related to regional, dietary, and genetic factors, Helicobacter pylori infection, and chronic diseases (2).
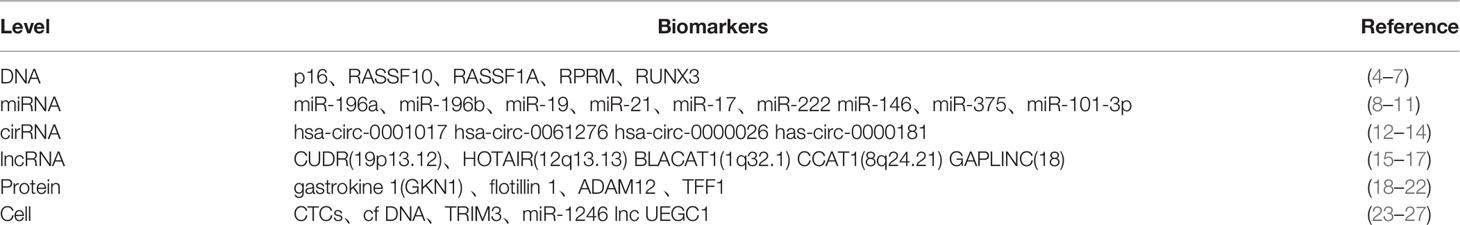
Gastric cancer can be divided into two types according to the site of carcinoma occurrence, cardia cancer, and non-cardia cancer. They differ in risk factors, carcinogenesis, and epidemiology. Patients with chronic H. pylori infection will develop non-cardiac cancer with serious consequences (1). H. pylori can cause gastric mucosa inflammation and injury through many ways and has a carcinogenic effect. Around half of the world’s population is infected with H. pylori, a high rate of infection (3). At present, great attention has been paid to the early control of H. pylori infection in order to achieve the prevention and treatment of gastric cancer. In addition, finding molecular markers that can predict early gastric cancer can achieve early detection, diagnosis, and treatment of gastric cancer patients. Because of the low sensitivity and specificity of current gastric cancer serum tumor markers, molecular markers such as protein, cell, DNA, and RNA have good clinical application prospects according to current research findings (Table 1) .
The treatment strategy of gastric cancer is comprehensive treatment with surgery as the main way. At present, chemotherapy, immunotherapy, and targeted therapy have become the focus of comprehensive treatment of gastric cancer. Traditional chemotherapeutic drugs are highly toxic and cause serious damage to normal cells due to their poor ability to recognize tumor cells. Drug resistance can also develop after several doses of the drug (28, 29). Immunotherapy has attracted worldwide attention due to its anticancer effect but has not been shown to have the same effect on all cancer patients (30).Although it has developed rapidly in recent years, great challenges have also been encountered in some specific situations, such as the drug resistance of immune checkpoint inhibitors and weak immunogenicity of therapeutic vaccines (31, 32).
The development of nanomaterial technology and biotechnology has promoted the innovation of nanomedicine. The nano-delivery system could avoid the poor selectivity of cancer therapies currently in use, which can damage healthy cells, so that drugs can reliably reach tumor tissues and reduce side effects caused by off-target in clinical application. This is due to the advantages of nanomaterials such as small volume and large surface area (33), higher permeability and retention; they can show greater specificity and can be combined with a variety of biological materials to reduce their toxicity and improve their biocompatibility. It could be used in nano- delivery systems, cancer detection, imaging, and drug-controlled release to targeted drugs (34, 35). It can effectively retain and control drug release and improve the efficiency of cancer treatment (36). The electrical, mechanical, optical, magnetic, and biological properties of nanomaterials are being used in the diagnosis and treatment of cancer (37). A variety of nanomaterials with good anticancer potential and improved diagnostic levels have been developed.
The application of nanomaterials in the medical field is in line with the promotion of personalized precision therapy. A nano-drug delivery system’s advantages will also get more application in clinics. Therefore, this paper briefly summarizes the progress of the application of the nanomaterials and deliver the medication system in H. pylori and gastric cancer, providing a reference for individual therapy to patients.
H. pylori and Nanomaterials
H. pylori is a spiral, Gram-negative microaerobe. The infection rate of H. pylori is more than 50% worldwide. Its means of transmission is not very clear; the most likely way between people is the mouth–mouth and dung–mouth travels (38, 39). The cause of the disease is caused by many factors, such as bacterial flagella, adhesion, urease, protease, vacuolar toxin, endotoxin, and other synergistic effects. H. pylori can survive in the strong acid environment in the stomach because the urease it produces breaks down urea into ammonia and carbon dioxide, and the gastric acid is neutralized by ammonia, thus enabling it to survive in the stomach with high acidity (40).
Nanomaterials could play a crucial role in the early detection and treatment of H. pylori. For example, an immune sensor for H. pylori was prepared for the early detection of cytotoxin-related gene antibodies (41). Jain U has developed super-sensitive electrochemical sensors for the early noninvasive detection of H. pylori in clinical samples (42). Nanomaterials can also be used to prepare nano-drug delivery systems and develop effective nanotherapy for H. pylori infection.
Relationship Between H. pylori Infection and Gastric Cancer
H. pylori was first discovered in patients with gastritis in 1982 by J. Robin Warren and Barry Marshall (43), in which an infection with this type of bacteria is one of the main reasons for various gastroduodenal diseases (44), including gastritis, peptic ulcer disease, and gastric cancer. This bacterium secretes versatile bacterial colonization factors and virulence factors, leading to gastric epithelial cell damage. After infection, chronic gastritis is first caused, which further results in gastric ulcer and atrophy, and gastric cancer is developed in severe cases (45). Unless receiving the specific antibacterial treatment, patients will carry these bacteria for life. The World Health Organization classified H. pylori as a class 1 carcinogen in 1994 (46). So, experts think that the early detection of H. pylori infection and timely and effective use of antibiotics to kill H. pylori have great significance to prevent stomach carcinoma. The timely diagnosis and cure of H. pylori have attracted people’s attention.
H. pylori Pathogenicity in Gastric Carcinogenesis
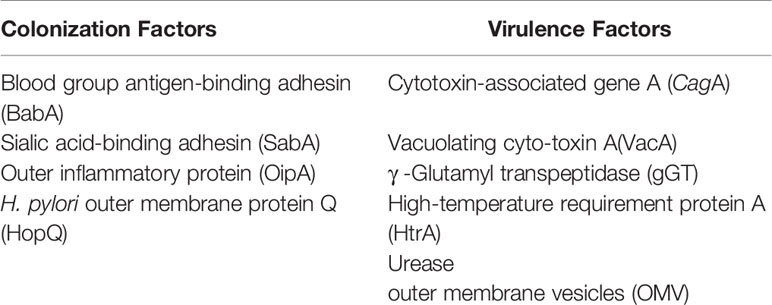
The pathogenic mechanism of H. pylori is very complicated, and the damage mechanism of H. pylori to the gastric mucosa and human body has not been completely understood. At present, the factors involved in the pathogenesis of H. pylori are classified into colonization factors and virulence factors. which damage gastric epithelial cells through outer proteins such as BabA, SabA, and many variants of outer membrane proteins (Table 2) (45, 47). When H. pylori attaches to stomach cells, it forms microcolonies on the surface of the stomach for nutrients to ensure that its initial colonization is successful (48). H. pylori expresses virulent proteins such as CagA and VacA that control the host’s immune system to escape immune detection (49). Studies reveal that in the presence of VacA, CagA accumulates in dysfunctional autophagosomes, providing a possible explanation for the synergistical work of VacA and CagA (50).
Nanomaterials and Detection of H. pylori
The CagA gene encodes immune dominant Cag protein, which causes gastric injury. Karakus et al. developed an immunochromatographic strip (ICTS) for detecting CagA antibodies in the sera of infected patients. Compared with PCR and commercial enzyme linked immunosorbent assay (ELISA), the sensitivity and specificity of ICTS were 95% and 100%, indicating that ICTS can be applied to rapidly detect patients with CagA-positive H. pylori infection. Without the need for an invasive method for testing (41), Gupta et al. promoted a novel H. pylori immunosensor to detect the CagA antibody, which is based on platinum nanoparticles (NPs). The new immune sensor has good accuracy, precision, reliability, and storage stability (51).
Jain et al. built an unlabeled electrochemical immunosensor for detecting H. pylori by a covalently immobilized antibody (CagA) on a nanomaterial-modified gold electrode. The results of H. pylori determination in human feces showed good accuracy. The support of nanometer technical for the development of electrochemical sensors with super sensitive and early detection of non-invasive clinical samples of H. pylori laid a solid foundation (42).
The BabA immunosensor was based on nanohybridization, which was synthesized by the electrodeposition of palladium NPs on a gold electrode. The stable BabA antigen–antibody complex, with its high sensitivity and non-invasive detection method, will have broad application prospects in the early detection of H. pylori (52).
Nano-Drug Delivery System and H. pylori Therapy
The pathogenic potential of H. pylori has been confirmed in many laboratories since its first discovery, and the World Health Organization classified H. pylori as a class 1 carcinogen (46).
There was a parallel relationship between H. pylori infection and gastric cancer mortality. Therefore, the timely detection and eradication of H. pylori treatment have aroused people’s attention. It also has a preventive effect on the occurrence of gastric cancer. Due to the development of H. pylori resistance, quadruple therapy was recommended as a first-line treatment, which has a really higher eradication rate (bismuth plus PPI plus two antibiotics) (53).
Nanocarriers could protect antibiotics in harsh gastric environments. Amoxicillin is an antibiotic commonly used to eradicate H. pylori. Because it is easily degraded by stomach acid, it needs to be taken in large doses and used in combination with other drugs. Treatments sometimes fail because of side effects. Yang et al. built a nano-drug carrier that is composed of chitosan/poly(acrylic acid) particles, superparamagnetic iron oxide NPs, and amoxicillin (SPIO/AMO@PAA/CHI). It avoids the failure of treatment because of the easy degradation of antibiotics and the side effects caused by high dose administration. It can improve the stranded time of drugs in the stomach (54).
Biofilm formation is thought to be one of the causes of treatment failure. Gopalakrishnan et al. clarify that N-acyl homoserine lactonase-stabilized silver NPs inhibit quorum sensing (QS) by degradation, thereby reducing biofilm formation and improving the effect treatment. (55). Niaz prepared a nanodelivery system that is composed of a protein/polysaccharide core-shell crown. This compound can improve the stability and bioaccessibility of ϵ-polylysine (ϵ-PL) in the treatment of H. pylori. Therefore, this nanosystem can raise the efficacy of antibacterial agents and develop effective nanotherapies for gastric infection (56).
The studies of Jawed et al. indicated that curcumin has many biological functions with low bio-availability, which limits their uses as therapeutic for H. pylori. When it is encapsulated into a biocompatible copolymer, the PLGA NP might be used as potential therapeutics against H. pylori (57). Nanocarriers show therapeutic potential, owing to their mucosal penetrating capacities and modifiable properties (58).
As a matter of fact, the first step in the development of H. pylori pathogenicity is the adhesion to the gastric epithelium (59). It is very critical to design NPs with adhesion ability to mucosa for the treatment of H. pylori. For this reason, Arif et al. designed cysteine-conjugated chitosan (CysCS)/PMLA-targeting NPs that encapsulate amoxicillin. It can delay antibiotics release in gastric acid and can be targeted to mucosa. These results indicate that the multifunctional amoxicillin-loaded NPs have great potential for the effective treatment of H. pylori infection (60).
Gastric Cancer and Nanomaterials
Gastric cancer is treated in different ways according to different stages of development. In the early stages of gastric cancer, the lesions are confined to the mucosa and submucosa, regardless of the size of their range and whether there is lymph node metastasis. Endoscopic submucosal dissection (ESD) and endoscopic mucosal resection (EMR) are minimally invasive treatments and can be used for the treatment of early gastric cancer (61). The main treatment methods for advanced gastric cancer, surgical treatment, radiotherapy and chemotherapy, immunotherapy, and targeted therapy, have gradually risen in status and become hot research in recent years (62). Nanomaterials, small chemicals with novel properties in at least one dimension on the scale of 1–100 nm, have also received great attention from researchers in recent years as a tool for cancer treatment. The application of nanotechnology in medicine has been greatly developed, and it also plays a unique role in the early diagnosis and comprehensive treatment of gastric cancer. There is room for improvement in diagnosis and treatment, and these advances hold great potential for the development of nanomaterials for cancer treatment. A number of nanomaterials are currently used for cancer treatment.
Early Diagnosis of Gastric Cancer and Nanomaterials
Most gastric cancer patients have no typical clinical symptoms in the early stage, and the diagnosis is already advanced, which makes it difficult to completely remove the tumor. Early diagnosis and accurate personalized intervention are important questions to improve the prognosis of gastric cancer. Therefore, it is difficult to find effective and specific markers for the early diagnosis and treatment of gastric cancer. Magnetic nanomaterials have their own advantages in this aspect.
The relationship between SNP and the DNA specificity of some genes in gastric cancer treatment pathway was analyzed by using a magnetic nanomaterial molecular carrier. The RAS-BRAF gene was introduced on the surface of magnetic NPs, which is used to isolate and detect protein and pathogens. The results show that the system has good detection sensitivity and separation selectivity. Studies suggest that the PLCE1 gene may be a susceptibility gene of tumor cells and is closely related to disease prognosis (63).
The dysregulation of microRNA concentration has been considered as a marker of disease. Decreased Mir-17 concentration has been found in gastric cancer. Therefore, rapid, specific, and simple microRNA quantification techniques are becoming key factors for early diagnosis and treatment. Miti et al. reported an immobilized gold NP for the detection of Mir-17. The process is fast, and the detection range is effective. This technique may be a promising alternative to traditional laboratory techniques for detection and quantification (64).
Zhuang et al. have developed biosensor CPs/AUNP-AUE, combined with a DNA capture probe to detect the Mir-100 content in the serum of GC patients. The biosensor detection of Mir-100 is highly specific and can be used as a reliable strategy for clinical gastric cancer detection (65).
Nanomaterials and Chemotherapy
The common chemotherapeutic drugs for gastric cancer include fluorouracil (5-FU, S-1, and capecitabine), platinum (cisplatin and oxaliplatin), taxane (paclitaxel, docetaxel), topoisomerase inhibitors (irinotecan), and anthracene (epirubicin) (61)
At present, most of the first-generation nanochemotherapy reagents on the market use non-targeted delivery systems, which lack selectivity to tumor tissues and are distributed to the whole body after administration, with low bioavailability, limited efficacy, great damage to normal cells, and obvious side effects. An intelligent responsive drug delivery system is developed by using stimulus-responsive materials, which responds to changes in the internal environment of the lesion and carries out self-feedback to realize on-demand drug release, improve efficacy, and reduce side effects. Commonly used stimulus nano-drug delivery systems include acid response, reduction response, temperature response, light response, and enzyme response. After receiving the corresponding stimulus, the conformation of the drug changes, the separation between the drug and the carrier occurs, and the drug can achieve controlled release and play a role in the body.
Chemotherapy drug resistance is a difficult clinical challenge. Miao et al. developed zinc oxide nanoparticles (ZnO-NPs), which have been proven to be a promising anticancer drug. It can inhibit the proliferation, migration, and invasion of gastric cancer cells and induce apoptosis. ZnO-NP is a kind of potential drug candidate for gastric cancer therapy by inhibiting autophagy to reduce chemotherapy resistance (29).
Signal transducers and transcriptional activator 3 (STAT3) are key transcription factors that are overactivated in gastric cancer and play a crucial role in the induction of chemotherapy resistance. Zheng et al. developed polylactic acid-hydroxy acetic acid (PLGA) NPs for simultaneous codelivery of doxorubicin (DOX) and nifuratel. DNNPs have been shown to induce mitochondria-dependent apoptosis, inhibit STAT3 phosphorylation, and enhance the anticancer effect. It can inhibit the STAT3 pathway and amplify apoptosis (66).
Azimee et al. utilized the autophagy potential of TiO (2) NPs to improve the chemotherapy effect of 5-fluorouracil (5-FU) on human AGS gastric cells. In in vitro gastric cancer models, they confirmed the beneficial effect of TiO (2) NPs combined with chemotherapy, which lay a foundation for the development of a possible solution to cancer chemotherapy resistance. It was promising to improve the efficacy of current cancer treatment strategies (67).
Paclitaxel (Ptx) is one of the main chemotherapy drugs for advanced gastric cancer. Its clinical application is limited due to poor solubility. Yu et al. designed Ptx-NPs with more effective antitumor drug and fewer side effects, which are composed of methoxy poly (ethylene glycol) and poly (epsilon-caprolactone) NPs. The cytotoxicity of the treated group by Ptx-NPs was superior to that of the same dose of free Ptx. The Ptx-NPs group had more autophagy, which enhanced the anticancer effect. (68). Deng et al. developed a novel Se@Albumin composite NP. In mouse models, it can improve cisplatin-induced intestinal mucositis and will provide new information for clinical treatment (69).
Poor hydrophobicity of docetaxel and poor solubility of the PI3K/AKT signaling pathway inhibitor LY294002 limit their clinical application. Cai et al. developed polylactic acid/glycolic acid (PLGA) NPs with TXT and LY294002. In vitro and in vivo model experiments showed that PLGA(TXT+LY294002) showed controlled release, decreased proliferation ability, and increased apoptosis rate, showing tumor-targeting properties, non-toxic to main organs, controlled release, and targeted tumor, which provide a new idea for the targeted therapy of gastric cancer (70).
Gastric cancer stem cells (CSCs) have the characteristics of chemotherapy drug resistance and uncertain proliferation. Yao et al. developed novel CSCs targeting glioma-associated oncogene homolog 1 (Gli1) small interfering RNA (siRNA) NPs, which were shown to significantly inhibit the malignant features of CSC and specifically eliminated gastric CSCs, indicating that these novel delivery systems provide a promising therapeutic approach for gastric cancer treatment (71).
Nanomaterials and Targeted Therapy
Molecular targeted therapy is an important treatment for advanced gastric cancer. Its target of the epidermal growth factor receptor (EGFR) and vascular endothelial growth factor receptor (VEGF) can prolong the overall survival of advanced gastric cancer. Although targeted therapy has made great progress in gastric cancer, only a few targeted drugs have been approved for clinical use, such as trastuzumab (anti-HER2 drugs) and apatinib (antiangiogenic pathway drugs) (72).
Abnormal overexpression of HER2 protein is associated with gastric cancer and is one of the factors contributing to poor prognosis of gastric cancer. Therefore, HER2 is a therapeutic target for gastric cancer (73).
Trastuzumab (Tmab) is a humanized monoclonal antibody that selectively targets the human epidermal growth factor receptor 2 (HER2), and while Tmab has shown improvement in patient prognosis, the acquired resistance to this drug remains an issue. Kanaya et al. developed gold NPs bound to Tmab by taking advantage of their in vivo stability and ease of surface modification and demonstrated their efficacy in treating HER2-positive, Tmab-resistant gastric cancer cell lines (74). Kubota et al. developed HER2-targeted AuNPs (Tmab-AuNPs) and showed that they have an effective antitumor effect against Tmab-resistant cell lines. In addition, when HER2 is overexpressed artificially, Tmab-AuNPs are effective against HER2-negative gastric cancer cell lines (75). Kubota et al. designed HER2-targeted AuNP (T-AUNP). Combined with Tmab, it is a promising approach to overcome Tmab resistance in gastric cancer (76). Zhang et al. developed a gold nanoshell drug carrier targeting HER-2 and immune adjuvant CPG sequence for the delivery and selective photothermal release of targeted genes in gastric cancer cells. This drug delivery system has better gene transduction ability and combination therapy effect, which is expected to become a translational therapy for gastric cancer (77).
Angiogenesis plays a critical role in tumor genesis, growth, and metastasis. The expression of vascular endothelial growth factor (VEGF) is high in most solid tumors, and many VEGF inhibitors have been used in clinics (78). The strong tyrosine kinase activity of VEGFR2 makes targeting VEGFR2 therapy an important strategy for antitumor therapy (79).
Apatinib, a small-molecule tyrosine kinase inhibitor targeting VEGFR2, is approved for the treatment of gastric cancer (80). Apatinib can selectively target VEGFR2 and bind to its intracellular binding site of ATP, blocking the corresponding signaling pathway, thereby inhibiting tumor angiogenesis. Long et al. developed nanocomplex LP-R/C@AC(LP: PH-responsive liposome R/C: mixed membrane A: apatinib C: cinobufagin), which killed tumor cells in vitro and also significantly inhibited tumor invasion and metastasis. In addition, it showed stronger antitumor activity in a mouse model of gastric cancer compared to a single agent. Emerging nanotechnology offers an alternative approach to building novel drug delivery systems with high targeting capability and solubility (81). In the Zhang et al. study, PLGA-based NPs coloaded Sal with apatinib (Apa), The surface of the NPs was modified with tumor-homing peptide (iVR1 peptides). Studies have shown that Sal can improve the chemical sensitivity of gastric cancer to Apa, and this compound can achieve efficient tumor-targeted delivery (82)
Nanomaterials and Immunotherapy
The emergence of immunotherapy has changed the mode of tumor treatment (83, 84), which activates the body’s own immune system to kill tumor cells. Immunotherapy is regarded as a treatment or cure for certain types of cancer with promising strategies. Immunotherapy has become a research focus of tumor therapy in recent years, and a series of progress has been made, but the proportion of patients who respond to immunotherapy is still deficient. The cause of this phenomenon is the production of immune tolerance. On the one hand, because of the low immunogenicity of tumor cells, less specific antigen on the surface; on the other hand, there are less immune cells within the tumor, due to the immunosuppressive microenvironment in the tumor (85), In view of the above two reasons, there are two steps to improve the tolerance of tumor immunotherapy. The first step is to enhance the immunogenicity of tumor tissue and improve the response rate. The second step is to regulate the tumor-immunosuppressive microenvironment and overcome the immune tolerance. The nano-drug delivery system plays a crucial role in improving immune tolerance. which can reverse immunosuppression and activate tumor immune response to play a role, increasing the traditional immunotherapy treatment effect, reducing the immune treatment of adverse reactions (86, 87). The role of several nanomaterials in immunotherapy is described below.
As one of the most promising immunotherapies, immune checkpoint inhibitors have attracted attention. Immune checkpoint therapy has made a remarkable clinical development in the cure of cancer (88). As the most thoroughly studied class of immunotherapies to date, immune checkpoint molecules, cytotoxic T lymphocyte antigen 4 (CTLA-4), and programmed cell death protein 1 (PD-1) have received special attention. Pd-1 and CTLA-4, which has already become the approved target of cancer therapy (89, 90).
Pd-l1 is a symbol of poor prognosis in gastric cancer (91). Luo et al. developed siRNA delivery systems for PD-L1 knockdown to achieve effective therapy and diagnosis in gastric cancer (92).
NPs play a critical role in enhancing immune regulation by integrating various molecules. NPs can manipulate immune cells by promoting targeted delivery to release drugs, antigens, and adjuvants at their intended target sites and escaping the pathological physiological disorders at the same time (84, 93, 94); therefore, drugs can be mediated by NP-potent drug therapeutic potential to expand treatment drugs.
Applications of Nanomaterials in Other Aspects of Gastric Cancer
Photodynamic therapy is a novel approach to treat tumors. After photosensitive drugs are delivered to tumor tissues, the photosensitive agents are activated and reactive oxygen species are generated to produce toxic effects on tumor cells after local irradiation with appropriate wavelength light (95, 96). This treatment has fewer side effects and can achieve precise and effective treatment. It is considered as a promising approach for the treatment of cancer (97). Yang et al. used the cell membrane (CM) from SGC7901 cells to decorate silica nanoparticles (SLNs) and load the photodynamic agent chloride ion e6 (Ce6) to construct CM/SLN/Ce6 suitable for gastric cancer tumor targeting PDT. SGC7901 cells were specifically targeted in vitro and in vivo. It has a better anticancer effect. This may be an effective tumor-targeted photodynamic therapy for gastric carcinoma platforms (97).
Ultrasound-focused chemotherapy is a non-invasive treatment with excellent penetrating performance, which is used to treat deep tumors. However, it will inevitably cause harm to normal tissues around the lesions. Low-intensity focused ultrasound (LIFU) was used to overcome this problem, achieving precisely controlled imaging and treatment. Liu et al. developed a simple, versatile nanoplatform (DPP-R) that responds to LIFU and simultaneously provides targeted drug delivery. Its targeting ability, imaging function, and antitumor effect have been approved in vitro and in vivo. DPP-R combined with LIFU is a new treatment method for gastric cancer (98).
The carbon nanolayer tracer method can improve the lymph node black staining rate and lymph node detection rate and improve the accuracy of gastric cancer staging (99). It is safe and feasible to apply neoadjuvant chemotherapy in D2 radical gastrectomy for gastric cancer. It can increase the number of lymph nodes detected, which is conducive to the evaluation of chemotherapy effects and prognosis of patients (100).
Discussion
The further application of nanomaterial synthesis technology in the biomedical field is due to advances in materials science, medicine and biomedicine. We have applied the properties of nanomaterials themselves to the biomedical field, showing unique advantages in the early diagnosis of H. pylori and gastric cancer. It can also be used to improve the deficiency of original treatment, reduce the side effects of drugs, and provide new methods for the prevention, early diagnosis, and treatment of gastric cancer. The application of these nanomaterials is in line with the requirements of individualized precision therapy advocated today. Nanodelivery systems provide new ideas and new approaches for individual therapy.
However, the transformation of nanomaterials into clinical applications comes with a number of challenges, including stability, gastrointestinal degradation, and immune response. Some nanomaterials are not biodegradable in the human body and their impact on human health is unclear. For example, metal NPs will remain in the body after using them for a long time, and they may increase the cytotoxicity. There are no uniform standards for nano-drug delivery systems. Nanomaterials must be biodegradable and biocompatible to obtain better clinical application value. A simple NP design and quality control mechanisms are essential for the clinical transformation of nanomedicine.
Although currently, there are limitations in their use, many related studies are being carried out, and nanomedicine has shown great efficacy improvement in preclinical studies. It is believed that more nanomaterials will be designed and approved in clinical trials soon. In the future, nanomaterials will be more widely used in the biomedical field and provide more therapeutic effects for patients in need by seriously addressing the issues related to nanomaterial design and clinical trial design.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This research was funded by Science and Technology Commission of shanghai municipality, (grant number 19140903602). The APC was funded by Science and Technology Commission of shanghai municipality.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin (2021) 71(3):209–49. doi: 10.3322/caac.21660
2. Alexander SM, Retnakumar RJ, Chouhan D, Devi TNB, Dharmaseelan S, Devadas K, et al. H. Pylori in Human Stomach: The Inconsistencies in Clinical Outcomes and the Probable Causes. Front Microbiol (2021) 12:713955. doi: 10.3389/fmicb.2021.713955
3. Hooi JKY, Lai WY, Ng WK, Suen MMY, Underwood FE, Tanyingoh D, et al. Global Prevalence of H. Pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology (2017) 153(2):420–9. doi: 10.1053/j.gastro.2017.04.022
4. Guo L, Huang C, Ji QJ. Aberrant Promoter Hypermethylation of P16, Survivin, and Retinoblastoma in Gastric Cancer. Bratisl Lek Listy (2017) 118(3):164–8. doi: 10.4149/bll_2017_033
5. Peng D, Zhang H, Sun G. The Relationship Between P16 Gene Promoter Methylation and Gastric Cancer: A Meta-Analysis Based on Chinese Patients. J Cancer Res Ther (2014) 10 Suppl:292–5. doi: 10.4103/0973-1482.151535
6. Saliminejad K, Soleymani Fard S, Khorram Khorshid HR, Yaghmaie M, Mahmoodzadeh H, Mousavi SA, et al. Methylation Analysis of P16, RASSF1A, RPRM, and RUNX3 in Circulating Cell-Free DNA for Detection of Gastric Cancer: A Validation Study. Avicenna J Med Biotechnol (2020) 12(2):99–106.
7. Hu Y, Ma P, Feng Y, Li P, Wang H, Guo Y, et al. Predictive Value of the Serum RASSF10 Promoter Methylation Status in Gastric Cancer. J Int Med Res (2019) 47(7):2890–900. doi: 10.1177/0300060519848924
8. Stojanovic J, Tognetto A, Tiziano DF, Leoncini E, Posteraro B, Pastorino R, et al. MicroRNAs Expression Profiles as Diagnostic Biomarkers of Gastric Cancer: A Systematic Literature Review. Biomarkers (2019) 24(2):110–9. doi: 10.1080/1354750x.2018.1539765
9. Ranjbar R, Hesari A, Ghasemi F, Sahebkar A. Expression of microRNAs and IRAK1 Pathway Genes are Altered in Gastric Cancer Patients With H. Pylori Infection. J Cell Biochem (2018) 119(9):7570–6. doi: 10.1002/jcb.27067
10. Emami SS, Nekouian R, Akbari A, Faraji A, Abbasi V, Agah S. Evaluation of Circulating miR-21 and miR-222 as Diagnostic Biomarkers for Gastric Cancer. J Cancer Res Ther (2019) 15(1):115–9. doi: 10.4103/jcrt.JCRT_592_17
11. Sawaki K, Kanda M, Kodera Y. Review of Recent Efforts to Discover Biomarkers for Early Detection, Monitoring, Prognosis, and Prediction of Treatment Responses of Patients With Gastric Cancer. Expert Rev Gastroenterol Hepatol (2018) 12(7):657–70. doi: 10.1080/17474124.2018.1489233
12. Necula L, Matei L, Dragu D, Neagu AI, Mambet C, Nedeianu S, et al. Recent Advances in Gastric Cancer Early Diagnosis. World J Gastroenterol (2019) 25(17):2029–44. doi: 10.3748/wjg.v25.i17.2029
13. Huang YS, Jie N, Zou KJ, Weng Y. Expression Profile of Circular RNAs in Human Gastric Cancer Tissues. Mol Med Rep (2017) 16(3):2469–76. doi: 10.3892/mmr.2017.6916
14. Zhao Q, Chen S, Li T, Xiao B, Zhang X. Clinical Values of Circular RNA 0000181 in the Screening of Gastric Cancer. J Clin Lab Anal (2018) 32(4):e22333. doi: 10.1002/jcla.22333
15. Dong L, Qi P, Xu MD, Ni SJ, Huang D, Xu QH, et al. Circulating CUDR, LSINCT-5 and PTENP1 Long Noncoding RNAs in Sera Distinguish Patients With Gastric Cancer From Healthy Controls. Int J Cancer (2015) 137(5):1128–35. doi: 10.1002/ijc.29484
16. Zhou X, Yin C, Dang Y, Ye F, Zhang G. Identification of the Long non-Coding RNA H19 in Plasma as a Novel Biomarker for Diagnosis of Gastric Cancer. Sci Rep (2015) 5:11516. doi: 10.1038/srep11516
17. Yörüker EE, Keskin M, Kulle CB, Holdenrieder S, Gezer U. Diagnostic and Prognostic Value of Circulating lncRNA H19 in Gastric Cancer. BioMed Rep (2018) 9(2):181–6. doi: 10.3892/br.2018.1116
18. Yoon JH, Choi WS, Kim O, Choi BJ, Nam SW, Lee JY, et al. Gastrokine 1 Inhibits Gastric Cancer Cell Migration and Invasion by Downregulating RhoA Expression. Gastric Cancer (2017) 20(2):274–85. doi: 10.1007/s10120-016-0617-1
19. Stella di Stadio C, Faraonio R, Federico A, Altieri F, Rippa E, Arcari P. GKN1 Expression in Gastric Cancer Cells Is Negatively Regulated by miR-544a. Biochimie (2019) 167:42–8. doi: 10.1016/j.biochi.2019.09.005
20. Gao W, Xu J, Wang F, Zhang L, Peng R, Shu Y, et al. Plasma Membrane Proteomic Analysis of Human Gastric Cancer Tissues: Revealing Flotillin 1 as a Marker for Gastric Cancer. BMC Cancer (2015) 15:367. doi: 10.1186/s12885-015-1343-5
21. Shimura T, Dayde D, Wang H, Okuda Y, Iwasaki H, Ebi M, et al. Novel Urinary Protein Biomarker Panel for Early Diagnosis of Gastric Cancer. Br J Cancer (2020) 123(11):1656–64. doi: 10.1038/s41416-020-01063-5
22. Pantel K, Alix-Panabières C. Liquid Biopsy in 2016: Circulating Tumour Cells and Cell-Free DNA in Gastrointestinal Cancer. Nat Rev Gastroenterol Hepatol (2017) 14(2):73–4. doi: 10.1038/nrgastro.2016.198
23. Shi Y, Wang Z, Zhu X, Chen L, Ma Y, Wang J, et al. Exosomal miR-1246 in Serum as a Potential Biomarker for Early Diagnosis of Gastric Cancer. Int J Clin Oncol (2020) 25(1):89–99. doi: 10.1007/s10147-019-01532-9
24. Kang HM, Kim GH, Jeon HK, Kim DH, Jeon TY, Park DY, et al. Circulating Tumor Cells Detected by Lab-on-a-Disc: Role in Early Diagnosis of Gastric Cancer. PloS One (2017) 12(6):e0180251. doi: 10.1371/journal.pone.0180251
25. Sumbal S, Javed A, Afroze B, Zulfiqar HF, Javed F, Noreen S, et al. Circulating Tumor DNA in Blood: Future Genomic Biomarkers for Cancer Detection. Exp Hematol (2018) 65:17–28. doi: 10.1016/j.exphem.2018.06.003
26. Fu M, Gu J, Jiang P, Qian H, Xu W, Zhang X. Exosomes in Gastric Cancer: Roles, Mechanisms, and Applications. Mol Cancer (2019) 18(1):41. doi: 10.1186/s12943-019-1001-7
27. Lin LY, Yang L, Zeng Q, Wang L, Chen ML, Zhao ZH, et al. Tumor-Originated Exosomal Lncuegc1 as a Circulating Biomarker for Early-Stage Gastric Cancer. Mol Cancer (2018) 17(1):84. doi: 10.1186/s12943-018-0834-9
28. Turner NC, Reis-Filho JS. Genetic Heterogeneity and Cancer Drug Resistance. Lancet Oncol (2012) 13(4):e178–185. doi: 10.1016/s1470-2045(11)70335-7
29. Miao YH, Mao LP, Cai XJ, Mo XY, Zhu QQ, Yang FT, et al. Zinc Oxide Nanoparticles Reduce the Chemoresistance of Gastric Cancer by Inhibiting Autophagy. World J Gastroenterol (2021) 27(25):3851–62. doi: 10.3748/wjg.v27.i25.3851
30. Song R, Li T, Ye J, Sun F, Hou B, Saeed M, et al. Acidity-Activatable Dynamic Nanoparticles Boosting Ferroptotic Cell Death for Immunotherapy of Cancer. Adv Mater (2021) 33(31):e2101155. doi: 10.1002/adma.202101155
31. Francis DM, Thomas SN. Progress and Opportunities for Enhancing the Delivery and Efficacy of Checkpoint Inhibitors for Cancer Immunotherapy. Adv Drug Deliv Rev (2017) 114:33–42. doi: 10.1016/j.addr.2017.04.011
32. Mu W, Chu Q, Liu Y, Zhang N. A Review on Nano-Based Drug Delivery System for Cancer Chemoimmunotherapy. Nanomicro Lett (2020) 12(1):142. doi: 10.1007/s40820-020-00482-6
33. Rai A, Noor S, Ahmad SI, Alajmi MF, Hussain A, Abbas H, et al. Recent Advances and Implication of Bioengineered Nanomaterials in Cancer Theranostics. Med (Kaunas) (2021) 57(2). doi: 10.3390/medicina57020091
34. Quader S, Kataoka K. Nanomaterial-Enabled Cancer Therapy. Mol Ther (2017) 25(7):1501–13. doi: 10.1016/j.ymthe.2017.04.026
35. Doughty ACV, Hoover AR, Layton E, Murray CK, Howard EW, Chen WR. Nanomaterial Applications in Photothermal Therapy for Cancer. Materials (Basel) (2019) 12(5). doi: 10.3390/ma12050779
36. Chen C, Wang S, Li L, Wang P, Chen C, Sun Z, et al. Bacterial Magnetic Nanoparticles for Photothermal Therapy of Cancer Under the Guidance of MRI. Biomaterials (2016) 104:352–60. doi: 10.1016/j.biomaterials.2016.07.030
37. Wei W, Rosenkrans ZT, Luo QY, Lan X, Cai W. Exploiting Nanomaterial-Mediated Autophagy for Cancer Therapy. Small Methods (2019) 3(2). doi: 10.1002/smtd.201800365
38. Bui D, Brown HE, Harris RB, Oren E. Serologic Evidence for Fecal-Oral Transmission of H. Pylori. Am J Trop Med Hyg (2016) 94(1):82–8. doi: 10.4269/ajtmh.15-0297
39. Mamishi S, Eshaghi H, Mahmoudi S, Bahador A, Hosseinpour Sadeghi R, Najafi M, et al. Intrafamilial Transmission of H. Pylori: Genotyping of Faecal Samples. Br J BioMed Sci (2016) 73(1):38–43. doi: 10.1080/09674845.2016.1150666
40. Weeks DL, Eskandari S, Scott DR, Sachs G. A H+-Gated Urea Channel: The Link Between H. Pylori Urease and Gastric Colonization. Science (2000) 287(5452):482–5. doi: 10.1126/science.287.5452.482
41. Karakus C, Ulupinar Z, Akbas F, Yazici D. Detection of Anti-CagA Antibodies in Sera of H. Pylori-Infected Patients Using an Immunochromatographic Test Strip. J Chromatogr Sci (2020) 58(3):217–22. doi: 10.1093/chromsci/bmz093
42. Jain U, Gupta S, Soni S, Khurana MP, Chauhan N. Triple-Nanostructuring-Based Noninvasive Electro-Immune Sensing of CagA Toxin for H. Pylori Detection. Helicobacter (2020) 25(4):e12706. doi: 10.1111/hel.12706
43. Warren JR, Marshall B. Unidentified Curved Bacilli on Gastric Epithelium in Active Chronic Gastritis. Lancet (1983) 1(8336):1273–5. Epub 1983/06/04.
44. Espinoza JL, Matsumoto A, Tanaka H, Matsumura I. Gastric Microbiota: An Emerging Player in H. Pylori-Induced Gastric Malignancies. Cancer Lett (2018) 414:147–52. doi: 10.1016/j.canlet.2017.11.009
45. Wroblewski LE, Peek RM Jr., Wilson KT. H. Pylori and Gastric Cancer: Factors That Modulate Disease Risk. Clin Microbiol Rev (2010) 23(4):713–39. doi: 10.1128/cmr.00011-10
46. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Infection With Helicobacter Pylori. IARC Monogr Eval Carcinog Risks Hum (1994) 61:177–240
47. Matsuo Y, Kido Y, Yamaoka Y. Helicobacter Pylori Outer Membrane Protein-Related Pathogenesis. Toxins (Basel) (2017) 9(3). doi: 10.3390/toxins9030101
48. Tan S, Noto JM, Romero-Gallo J, Peek RM Jr., Amieva MR. Helicobacter Pylori Perturbs Iron Trafficking in the Epithelium to Grow on the Cell Surface. PLoS Pathog (2011) 7(5). doi: 10.1371/journal.ppat.1002050
49. Link A, Langner C, Schirrmeister W, Habendorf W, Weigt J, Venerito M, et al. Helicobacter Pylori Vaca Genotype Is a Predominant Determinant of Immune Response to Helicobacter Pylori Caga. World J Gastroenterol (2017) 23(26):4712–23. doi: 10.3748/wjg.v23.i26.4712
50. Abdullah M, Greenfield LK, Bronte-Tinkew D, Capurro MI, Rizzuti D, Jones NL. Vaca Promotes Caga Accumulation in Gastric Epithelial Cells During Helicobacter Pylori Infection. Sci Rep (2019) 9(1):38. doi: 10.1038/s41598-018-37095-4
51. Gupta S, Tiwari A, Jain U, Chauhan N. Synergistic Effect of 2D Material Coated Pt Nanoparticles With PEDOT Polymer on Electrode Surface Interface for a Sensitive Label Free H. Pylori CagA((Ag-Ab)) Immunosensing. Mater Sci Eng C Mater Biol Appl (2019) 103:109733. doi: 10.1016/j.msec.2019.05.018
52. Gupta S, Jain U, Murti BT, Putri AD, Tiwari A, Chauhan N. Nanohybrid-Based Immunosensor Prepared for H. Pylori BabA Antigen Detection Through Immobilized Antibody Assembly With @ Pd(nano)/rGO/PEDOT Sensing Platform. Sci Rep (2020) 10(1):21217. doi: 10.1038/s41598-020-78068-w
53. Liou JM, Fang YJ, Chen CC, Bair MJ, Chang CY, Lee YC, et al. Concomitant, Bismuth Quadruple, and 14-Day Triple Therapy in the First-Line Treatment of H. Pylori: A Multicentre, Open-Label, Randomised Trial. Lancet (2016) 388(10058):2355–65. doi: 10.1016/s0140-6736(16)31409-x
54. Yang SJ, Huang CH, Yang JC, Wang CH, Shieh MJ. Residence Time-Extended Nanoparticles by Magnetic Field Improve the Eradication Efficiency of H. Pylori. ACS Appl Mater Interf (2020) 12(49):54316–27. doi: 10.1021/acsami.0c13101
55. Gopalakrishnan V, Masanam E, Ramkumar VS, Baskaraligam V, Selvaraj G. Influence of N-Acylhomoserine Lactonase Silver Nanoparticles on the Quorum Sensing System of H. Pylori: A Potential Strategy to Combat Biofilm Formation. J Basic Microbiol (2020) 60(3):207–15. doi: 10.1002/jobm.201900537
56. Niaz T, Ihsan A, Abbasi R, Shabbir S, Noor T, Imran M. Chitosan-Albumin Based Core Shell-Corona Nano-Antimicrobials to Eradicate Resistant Gastric Pathogen. Int J Biol Macromol (2019) 138:1006–18. doi: 10.1016/j.ijbiomac.2019.07.165
57. Alam J, Dilnawaz F, Sahoo SK, Singh DV, Mukhopadhyay AK, Hussain T, et al. Curcumin Encapsulated into Biocompatible Co-Polymer Plga Nanoparticle Enhanced Anti-Gastric Cancer and Anti-Helicobacter Pylori Effect. Asian Pac J Cancer Prev (2022) 23(1):61–70. doi: 10.31557/apjcp.2022.23.1.61.
58. Zhang Q, Wu W, Zhang J, Xia X. Eradication of Helicobacter Pylori: The Power of Nanosized Formulations. Nanomed (Lond) (2020) 15(5):527–42. doi: 10.2217/nnm-2019-0329.
59. Gottesmann M, Goycoolea FM, Steinbacher T, Menogni T, Hensel A. Smart Drug Delivery Against Helicobacter Pylori: Pectin-Coated, Mucoadhesive Liposomes with Antiadhesive Activity and Antibiotic Cargo. Appl Microbiol Biotechnol (2020) 104(13):5943–57. doi: 10.1007/s00253-020-10647-3.
60. Arif M, Dong QJ, Raja MA, Zeenat S, Chi Z, Liu CG. Development of Novel Ph-Sensitive Thiolated Chitosan/Pmla Nanoparticles for Amoxicillin Delivery to Treat Helicobacter Pylori. Mater Sci Eng C Mater Biol Appl (2018) 83:17–24. doi: 10.1016/j.msec.2017.08.038.
61. National Health Commission Of The People's Republic Of, C. Chinese Guidelines for Diagnosis and Treatment of Gastric Cancer 2018 (English Version). Chin J Cancer Res (2019) 31(5):707–37. doi: 10.21147/j.issn.1000-9604.2019.05.01
62. Ajani JA, D'Amico TA, Almhanna K, Bentrem DJ, Chao J, Das P, et al. Gastric Cancer, Version 3.2016, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw (2016) 14(10):1286–312. doi: 10.6004/jnccn.2016.0137
63. Qi M, Liu D, Wang H, Bianba C, Ji W. Correlation of Single Nucleotide Gene Polymorphisms and Gastric Cancer Based on Magnetic Nanoparticles. J Nanosci Nanotechnol (2021) 21(2):928–34. doi: 10.1166/jnn.2021.18628
64. Miti A, Thamm S, Müller P, Csáki A, Fritzsche W, Zuccheri G. A miRNA Biosensor Based on Localized Surface Plasmon Resonance Enhanced by Surface-Bound Hybridization Chain Reaction. Biosens Bioelectron (2020) 167:112465. doi: 10.1016/j.bios.2020.112465
65. Zhuang J, Wan H, Zhang X. Electrochemical Detection of miRNA-100 in the Sera of Gastric Cancer Patients Based on DSN-Assisted Amplification. Talanta (2021) 225:121981. doi: 10.1016/j.talanta.2020.121981
66. Zheng H, Chen Z, Cai A, Lin X, Jiang X, Zhou B, et al. Nanoparticle Mediated Codelivery of Nifuratel and Doxorubicin for Synergistic Anticancer Therapy Through STAT3 Inhibition. Colloids Surf B Biointerfaces (2020) 193:111109. doi: 10.1016/j.colsurfb.2020.111109
67. Azimee S, Rahmati M, Fahimi H, Moosavi MA. TiO(2) Nanoparticles Enhance the Chemotherapeutic Effects of 5-Fluorouracil in Human AGS Gastric Cancer Cells via Autophagy Blockade. Life Sci (2020) 248:117466. doi: 10.1016/j.lfs.2020.117466
68. Yu N, Li J, Singh PK, Ding D, Sun W, Tang Q, et al. The Superior Anticancer Effect of Reactive Oxygen Species-Responsive Paclitaxel Nanoparticles is Mediated Through Autophagic Cell Death. J BioMed Nanotechnol (2019) 15(11):2251–61. doi: 10.1166/jbn.2019.2847
69. Deng L, Zeng H, Hu X, Xiao M, He D, Zhang Y, et al. Se@Albumin Nanoparticles Ameliorate Intestinal Mucositis Caused by Cisplatin via Gut Microbiota-Targeted Regulation. Nanoscale (2021) 13(25):11250–61. doi: 10.1039/d0nr07981b
70. Cai J, Qian K, Zuo X, Yue W, Bian Y, Yang J, et al. PLGA Nanoparticle-Based Docetaxel/LY294002 Drug Delivery System Enhances Antitumor Activities Against Gastric Cancer. J Biomater Appl (2019) 33(10):1394–406. doi: 10.1177/0885328219837683
71. Yao H, Sun L, Li J, Zhou X, Li R, Shao R, et al. A Novel Therapeutic siRNA Nanoparticle Designed for Dual-Targeting CD44 and Gli1 of Gastric Cancer Stem Cells. Int J Nanomed (2020) 15:7013–34. doi: 10.2147/ijn.S260163
72. Wang FH, Zhang XT, Li YF, Tang L, Qu XJ, Ying JE, et al. The Chinese Society of Clinical Oncology (CSCO): Clinical Guidelines for the Diagnosis and Treatment of Gastric Cance. Cancer Commun (Lond) (2021) 41(8):747–95. doi: 10.1002/cac2.12193
73. Tai W, Mahato R, Cheng K. The Role of HER2 in Cancer Therapy and Targeted Drug Delivery. J Control Release (2010) 146(3):264–75. doi: 10.1016/j.jconrel.2010.04.009
74. Kanaya N, Kuroda S, Kubota T, Morihiro T, Kikuchi S, Nishizaki M, et al. [Novel Therapeutic Strategy for Human Epidermal Growth Factor Receptor 2-Positive Gastric Cancer]. Gan To Kagaku Ryoho (2017) 44(10):883–5.
75. Kubota T, Kuroda S, Morihiro T, Tazawa H, Kagawa S, Fujiwara T. [Novel HER2-Targeted Therapy Combined With Gold Nanoparticles]. Gan To Kagaku Ryoho (2016) 43(10):1237–9.
76. Kubota T, Kuroda S, Kanaya N, Morihiro T, Aoyama K, Kakiuchi Y, et al. HER2-Targeted Gold Nanoparticles Potentially Overcome Resistance to Trastuzumab in Gastric Cancer. Nanomedicine (2018) 14(6):1919–29. doi: 10.1016/j.nano.2018.05.019
77. Zhang W, Ding X, Cheng H, Yin C, Yan J, Mou Z, et al. Dual-Targeted Gold Nanoprism for Recognition of Early Apoptosis, Dual-Model Imaging and Precise Cancer Photothermal Therapy. Theranostics (2019) 9(19):5610–25. doi: 10.7150/thno.34755
78. Lee YJ, Karl DL, Maduekwe UN, Rothrock C, Ryeom S, D'Amore PA, et al. Differential Effects of VEGFR-1 and VEGFR-2 Inhibition on Tumor Metastases Based on Host Organ Environment. Cancer Res (2010) 70(21):8357–67. doi: 10.1158/0008-5472.Can-10-1138
79. Hicklin DJ, Ellis LM. Role of the Vascular Endothelial Growth Factor Pathway in Tumor Growth and Angiogenesis. J Clin Oncol (2005) 23(5):1011–27. doi: 10.1200/jco.2005.06.081
80. Scott LJ. Apatinib: A Review in Advanced Gastric Cancer and Other Advanced Cancers. Drugs (2018) 78(7):747–58. doi: 10.1007/s40265-018-0903-9
81. Long Y, Wang Z, Fan J, Yuan L, Tong C, Zhao Y, et al. A Hybrid Membrane Coating Nanodrug System Against Gastric Cancer via the VEGFR2/STAT3 Signaling Pathway. J Mater Chem B (2021) 9(18):3838–55. doi: 10.1039/d1tb00029b
82. Zhang Z, Yang W, Ma F, Ma Q, Zhang B, Zhang Y, et al. Enhancing the Chemotherapy Effect of Apatinib on Gastric Cancer by Co-Treating With Salidroside to Reprogram the Tumor Hypoxia Micro-Environment and Induce Cell Apoptosis. Drug Deliv (2020) 27(1):691–702. doi: 10.1080/10717544.2020.1754528
83. Gao J, Wang WQ, Pei Q, Lord MS, Yu HJ. Engineering Nanomedicines Through Boosting Immunogenic Cell Death for Improved Cancer Immunotherapy. Acta Pharmacol Sin (2020) 41(7):986–94. doi: 10.1038/s41401-020-0400-z
84. Riley RS, June CH, Langer R, Mitchell MJ. Delivery Technologies for Cancer Immunotherapy. Nat Rev Drug Discov (2019) 18(3):175–96. doi: 10.1038/s41573-018-0006-z
85. Goldberg MS. Improving Cancer Immunotherapy Through Nanotechnology. Nat Rev Cancer (2019) 19(10):587–602. doi: 10.1038/s41568-019-0186-9
86. Hou B, Zhou L, Wang H, Saeed M, Wang D, Xu Z, et al. Engineering Stimuli-Activatable Boolean Logic Prodrug Nanoparticles for Combination Cancer Immunotherapy. Adv Mater (2020) 32(12):e1907210. doi: 10.1002/adma.201907210
87. Yang B, Gao J, Pei Q, Xu H, Yu H. Engineering Prodrug Nanomedicine for Cancer Immunotherapy. Adv Sci (Weinh) (2020) 7(23):2002365. doi: 10.1002/advs.202002365
88. Sharma P, Allison JP. The Future of Immune Checkpoint Therapy. Science (2015) 348(6230):56–61. doi: 10.1126/science.aaa8172
89. Granier C, De Guillebon E, Blanc C, Roussel H, Badoual C, Colin E, et al. Mechanisms of Action and Rationale for the Use of Checkpoint Inhibitors in Cancer. ESMO Open (2017) 2(2):e000213. doi: 10.1136/esmoopen-2017-000213
90. Webb ES, Liu P, Baleeiro R, Lemoine NR, Yuan M, Wang YH. Immune Checkpoint Inhibitors in Cancer Therapy. J BioMed Res (2018) 32(5):317–26. doi: 10.7555/jbr.31.20160168
91. Thompson ED, Zahurak M, Murphy A, Cornish T, Cuka N, Abdelfatah E, et al. Patterns of PD-L1 Expression and CD8 T Cell Infiltration in Gastric Adenocarcinomas and Associated Immune Stroma. Gut (2017) 66(5):794–801. doi: 10.1136/gutjnl-2015-310839
92. Luo X, Peng X, Hou J, Wu S, Shen J, Wang L. Folic Acid-Functionalized Polyethylenimine Superparamagnetic Iron Oxide Nanoparticles as Theranostic Agents for Magnetic Resonance Imaging and PD-L1 siRNA Delivery for Gastric Cancer. Int J Nanomed (2017) 12:5331–43. doi: 10.2147/ijn.S137245
93. Wang H, Mooney DJ. Biomaterial-Assisted Targeted Modulation of Immune Cells in Cancer Treatment. Nat Mater (2018) 17(9):761–72. doi: 10.1038/s41563-018-0147-9
94. Wang W, Saeed M, Zhou Y, Yang L, Wang D, Yu H. Non-Viral Gene Delivery for Cancer Immunotherapy. J Gene Med (2019) 21(7):e3092. doi: 10.1002/jgm.3092
95. Dolmans DE, Fukumura D, Jain RK. Photodynamic Therapy for Cancer. Nat Rev Cancer (2003) 3(5):380–7. doi: 10.1038/nrc1071
96. Jeong H, Park W, Kim DH, Na K. Dynamic Nanoassemblies of Nanomaterials for Cancer Photomedicine. Adv Drug Deliv Rev (2021) 177:113954. doi: 10.1016/j.addr.2021.113954
97. Yang J, Teng Y, Fu Y, Zhang C. Chlorins E6 Loaded Silica Nanoparticles Coated With Gastric Cancer Cell Membrane for Tumor Specific Photodynamic Therapy of Gastric Cancer. Int J Nanomed (2019) 14:5061–71. doi: 10.2147/ijn.S202910
98. Liu Z, Ran H, Wang Z, Zhou S, Wang Y. Targeted and pH-Facilitated Theranostic of Orthotopic Gastric Cancer via Phase-Transformation Doxorubicin-Encapsulated Nanoparticles Enhanced by Low-Intensity Focused Ultrasound (LIFU) With Reduced Side Effect. Int J Nanomed (2019) 14:7627–42. doi: 10.2147/ijn.S212888
99. Cai YQ, Liang YX, Yu SY, Tu RS. [Clinical Value of Carbon Nanoparticles Tracer in Gastric Cancer Surgery to Increase the Number of Lymph Nodes Retrieval]. Zhonghua Wei Chang Wai Ke Za Zhi (2020) 23(10):984–9. doi: 10.3760/cma.j.cn.441530-20191031-00469
Keywords: nanoparticles, nanomaterials, nano-drug delivery systems, gastric cancer, Helicobacter pylori
Citation: Zhu X, Su T, Wang S, Zhou H and Shi W (2022) New Advances in Nano-Drug Delivery Systems: Helicobacter pylori and Gastric Cancer. Front. Oncol. 12:834934. doi: 10.3389/fonc.2022.834934
Received: 20 December 2021; Accepted: 29 March 2022;
Published: 10 May 2022.
Edited by:
Zhiqing Pang, Fudan University, ChinaReviewed by:
Ruixiang Li, Shanghai University of Traditional Chinese Medicine, ChinaBo Zhang, Huazhong University of Science and Technology, China
Copyright © 2022 Zhu, Su, Wang, Zhou and Shi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huiqing Zhou, aHEuemhvdUB5YWhvby5jb20uY24=; Weibin Shi, d2VpYmluZHJAYWxpeXVuLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Xiang Zhu1†
Xiang Zhu1† Weibin Shi
Weibin Shi