- 1Laboratory of Cancer Precision Medicine, The First Hospital of Jilin University, Changchun, China
- 2Department of Gynecology and Obstetrics, The Second Hospital of Jilin University, Changchun, China
- 3Department of Critical Care Medicine, The First Hospital of Jilin University, Changchun, China
- 4Department of Obstetrics and Gynecology, The First Hospital of Jilin University, Changchun, China
Cervical cancer is the most prevalent gynecologic malignancy, especially in women of low- and middle-income countries (LMICs). With a better understanding of the etiology and pathogenesis of cervical cancer, it has been well accepted that this type of cancer can be prevented and treated via early screening. Due to its higher sensitivity than cytology to identify precursor lesions of cervical cancer, detection of high-risk human papillomavirus (HR-HPV) DNA has been implemented as the primary screening approach. However, a high referral rate for colposcopy after HR-HPV DNA detection due to its low specificity in HR-HPV screening often leads to overtreatment and thus increases the healthcare burden. Emerging evidence has demonstrated that detection of host cell gene and/or HPV DNA methylation represents a promising approach for the early triage of cervical cancer in HR-HPV-positive women owing to its convenience and comparable performance to cytology, particularly in LMICs with limited healthcare resources. While numerous potential markers involving DNA methylation of host cell genes and the HPV genome have been identified thus far, it is crucial to define which genes or panels involving host and/or HPV are feasible and appropriate for large-scale screening and triage. An ideal approach for screening and triage of CIN/ICC requires high sensitivity and adequate specificity and is suitable for self-sampling and inexpensive to allow population-based screening, particularly in LMICs. In this review, we summarize the markers of host cell gene/HR-HPV DNA methylation and discuss their triage performance and feasibility for high-grade precancerous cervical intraepithelial neoplasia or worse (CIN2+ and CIN3+) in HR-HPV-positive women.
Introduction
Invasive cervical cancer (ICC) represents the fourth most prevalent gynecologic cancer with an estimated 604,000 new cases, which causes approximately 342,000 deaths worldwide in 2020, especially in low- and middle-income countries (LMICs) (1). To achieve the ultimate goal of eliminating ICC globally (2), the WHO has called for innovative technologies to detect cervical precancerous lesions, namely, grade 2–3 cervical intraepithelial neoplasia (CIN2-3), as well as appropriate strategies to improve the coverage and acceptance rate of ICC screening (3). To this end, a high-quality screening approach is urgently needed to identify CIN lesions, most of which are curable before progression to ICC, and ICC occurrence as early as possible.
Many studies have revealed that DNA screening of high-risk human papillomavirus (HR-HPV) is superior to cervical cytology in the detection of CIN2 or worse (CIN2+) lesions (4–11), which has been used in many countries worldwide. However, the HR-HPV DNA test can also detect transient infections that are not clinically meaningful, leading to poor specificity for detecting CIN lesions and thus unnecessary colposcopy referrals, overtreatment, and adverse events, especially in young women. This is particularly important in LMICs where the healthcare resource is limited, in association with low accessibility and acceptance for cervical cancer screening. Thus, an effective triage approach with adequate cost-effectiveness is required to screen HR-HPV DNA-positive women (11). However, multiple triage assays, such as HPV E6/E7 mRNA test, cytology, and p16-INK4a/Ki-67 dual immunostaining (12–15), are not suitable for large-scale population-based screening due to their complicated procedures that require well-trained/experienced technicians as well as because they are better applied in physician-collected samples, rather than self-collected ones. Therefore, simple and inexpensive approaches with sufficient sensitivity and specificity are urgently needed for more precisely detecting cervical precancerous lesions and excluding transient HPV infections.
During persistent HR-HPV infection and cervical oncogenesis, aberrant DNA methylation of human host cell genes or HPV genomic DNA is tightly associated with dysregulated functions of various tumor-suppressor genes (16–18). Moreover, DNA hypermethylation correlates with prolonged HR-HPV infection and is thus considered as a marker for severity of CIN lesions and risk of ICC (19). Emerging evidence supports a notion that detecting abnormal DNA methylation can distinguish the precancerous lesions from HPV infections that most likely do not develop to ICC, indicating its potential significance in the triage of patients who have CIN lesions (20) (Figures 1A, B), as shown in the flowchart for screening and triage of CINs (Figure 1C). In this review, we summarize the current status of detecting DNA methylation of host cell genes and HR-HPV for the triage of ICC precursor lesions in HR-HPV-positive women and discuss the advantages and limitations of diverse methylation markers identified thus far as well as their potential role in resolving controversial diagnosis of CIN2. To this end, a Medline search was performed for articles in English, using the MeSH terms “cervical” (Abstract) AND “cancer” OR “tumor” OR “neoplasia” OR “carcinoma” (Abstract) AND “methylation” (Abstract) AND “triage” (Text word) OR “screening” (Text word), which yielded a total of 286 papers. Among them, 180 articles were selected due to their close relationship with the content of this review article (e.g., HR-HPV-positive women as study subjects, self-sampling, population-based study, differentiation between CIN2+ and CIN3+, CIN2 diagnosis, etc.) while some additional original studies were also included due to their significant impacts on this field.
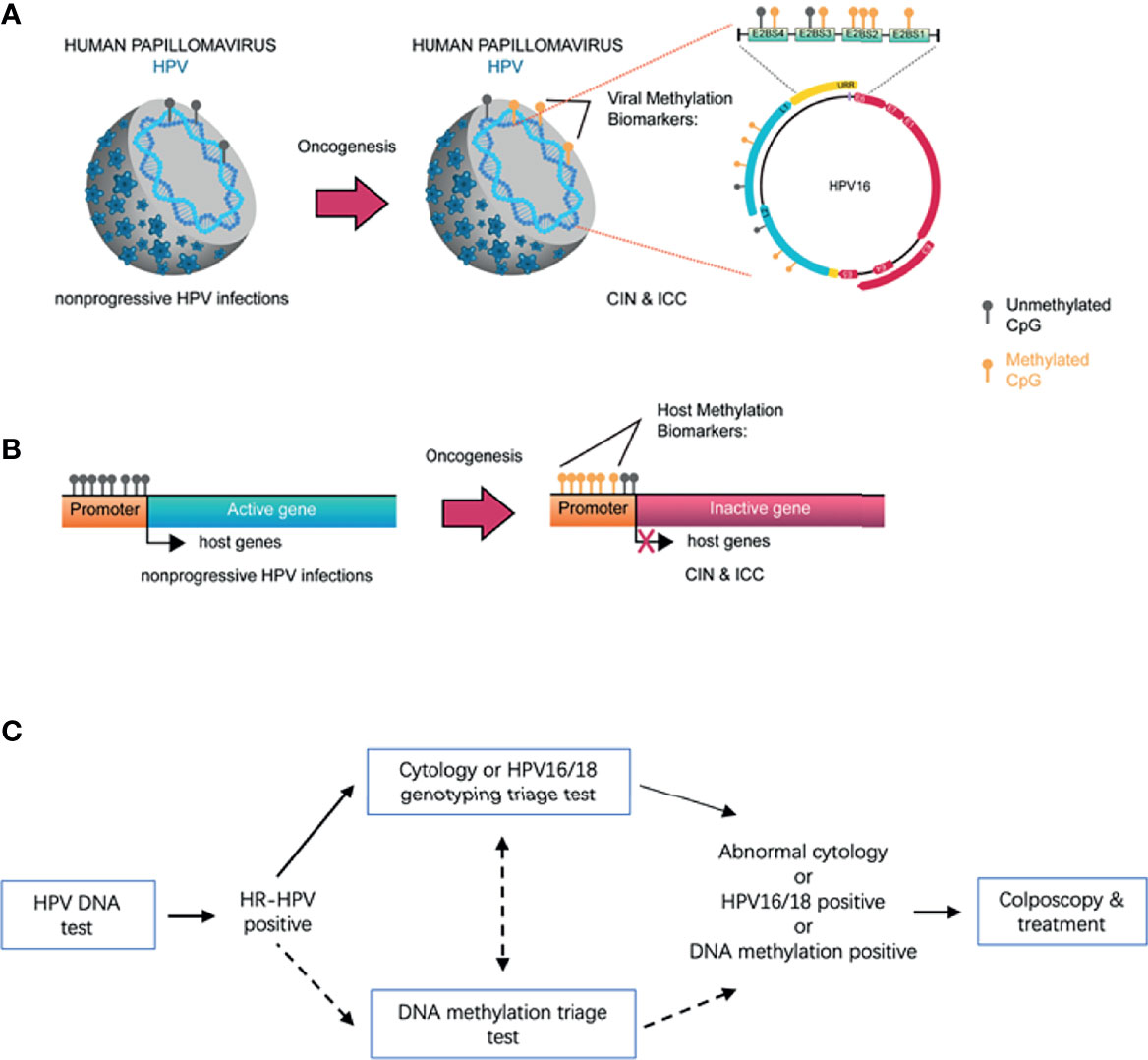
Figure 1 The mechanistic basis for detection of host gene and HPV DNA methylation for early screening of CIN/ICC. During persistent HR-HPV infection and cervical oncogenesis, hypermethylation of the host gene and viral genomic DNA is closely associated with the severity of CIN lesions and the risk of progression to ICC. With understanding the molecular mechanisms for HPV-mediated carcinogenesis, the positive correlation has been well established between CIN/ICC and hypermethylation of the CpG sites of HPV genomes (e.g., L1, L2, and E2BS) (A), or between CIN/ICC and hypermethylation of the CpG sites of host cell gene promoters (B). A number of studies have demonstrated that abnormal DNA methylations of host genes and/or HPVs, particularly in combination of multiple genes (i.e., gene panels), are capable of distinguishing non-progressive HPV infections from those associated with the potential to develop into ICC, therefore representing promising biomarkers for the triage of CIN lesions in HR-HPV infected women. Accordingly, a flowchart illustrates the potential process for the screening and triage of cervical cancer by integrating host cell gene/HPV DNA methylation detection in the future (C).
Methylation-Mediated Cervical Carcinogenesis Driven by HPV Infection
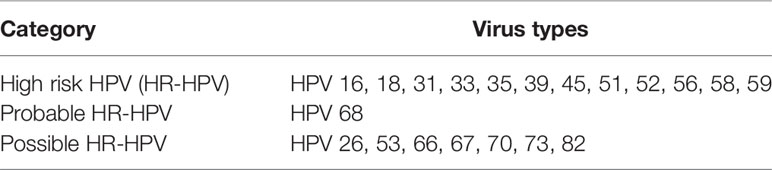
According to their epidemiological relationship with the incidence of ICC, the HR-HPV family members are divided into HR-HPV, probable HR-HPV, and possible HR-HPV (Table 1) (21), while the latter two are identified only in about 3% cervical cancer and not sufficient to be included in population-based prevention programs due to lack of biological data (22). HPV16 and HPV18 are the most prevalent HR-HPVs (23). HR-HPVs contain six early genes (E1, E2, and E4–7), which facilitate the expression and replication of the viral genome, and two late genes (L1 and L2) for capsid formation (24).
Infection with HR-HPV does not always result in ICC, while persistent HR-HPV infection that mediates cervical epithelial cell transformation is required for the development of precancerous lesions (CIN1–3) before progression to ICC. Therefore, the consequences of HR-HPV infection vary upon how cervical epithelial cells are exposed to HR-HPV, including transient, productive, and transforming infections (25). Transient infection is often not pathological due to spontaneous removal of HPV via local immunity. Productive infection is associated with productive CIN lesions (histologically corresponding to CIN1 or CIN2) that could spontaneously regress in 1–2 years, likely due to viral clearance. In contrast, transforming infections are associated with some CIN2 and most CIN3 lesions that are highly heterogeneous in regard of lesion regression versus oncogenesis, with a varied expression of E6 and E7 as well as patient survival (21). During carcinogenesis, the integration of HPV DNA to the host genome is accompanied by the downregulation of E2 but upregulation of oncogenic E6 and E7 (25–27). Moreover, the modified E2-binding sites (E2BS) in the upstream regulatory region (URR) or altered E2 expression may also be involved (28–30). For example, methylation of E2BS in the HPV16 enhancer region promotes disease progression (16, 17). However, the methylation status of a specific locus in the E6 promoter and enhancer is irrelevant to the role of HPV16 in the development of cervical precancerous lesions (31). E6 and E7 can regulate both cellular and viral gene expressions by modifying DNA methylation. E6 upregulates the expression of the DNA methyltransferase DNMT1 by suppressing TP53 (32), while E7 directly binds to and activates DNMT1 (33). Overexpression of E6/E7 oncoproteins drives uncontrolled cell proliferation, impaired apoptosis, and enhanced DNA damage repair by regulating related proteins, such as p53 and pRb (34). It also leads to chromosomal instability, accumulation of oncogenic alterations involving host cell genes, hypermethylation of tumor-suppressor gene promoters that silences target genes, and therefore malignant transformation of HR-HPV-infected cells (18, 34–36). DNA methylation refers to covalent transfer of a methyl group to the C-5 position to form 5-methylcytosine (5mC). DNA modification by methyl groups leads to translocation of transcription factors and thus alterations of gene expression by changing chromatin structure and DNA topology (37, 38). In general, hypermethylation of the CpG-rich region in gene promoters (CpG islands) suppresses transcription of target genes (21). Mechanistically, DNA methylation (e.g., 5mC) is reciprocally regulated by DNA methyltransferases (e.g., DNMT1, DNMT3A, and DNMT3B) as epigenetic writer and ten-eleven translocation (TET) methylcytosine dioxygenases (e.g., TET1-3) as eraser. To understand the potential role of DNA methylation dysregulation in ICC, we performed genome-wide analyses on the alterations of DNA methylation-regulatory genes (i.e., DNMTs and TETs) using the publicly available genomic, transcriptomic, and protein databases, including the Cervical Squamous Cell Carcinoma dataset (TGCA, PanCancer Atlas) on the cBioPortal for Cancer Genomics platform (www.cbioportal.org), the Tumor Cervical Squamous Cell Carcinoma - TCGA dataset (TCGA ID: CESC) on the R2: Genomics Analysis and Visualization Platform (http://r2.amc.nl), and the Cervical Cancer dataset on the Human Protein Atlas platform (www.proteinatlas.org), respectively. Of note, mutations of these DNA methylation-modifying genes are relatively rare (Figure 2A), including DNMT1 (5%), DNMT3A (2.7%), DNMT3B (4%), TET1 (4%), TET2 (2%), and TET3 (2.4%); however, DNMT3A and TET2 are relatively high at the protein level but vary with different ages, while the levels of DNMT1, DNMT3B, and TET3 are moderate or relatively low (Figure 2B); and the expression of these genes correlates, either positively (for DNMT3A, DNMT3B, and TET3) or negatively (for DNMT1, TET1, and TET2), with the overall survival of ICC patients (Figure 2C). These observations suggest that the abnormalities of host cell DNA methylation may be associated with dysregulation of its regulatory machinery involving DNMTs and TETs, which in turn contribute to disease progression and outcome of ICC patients.
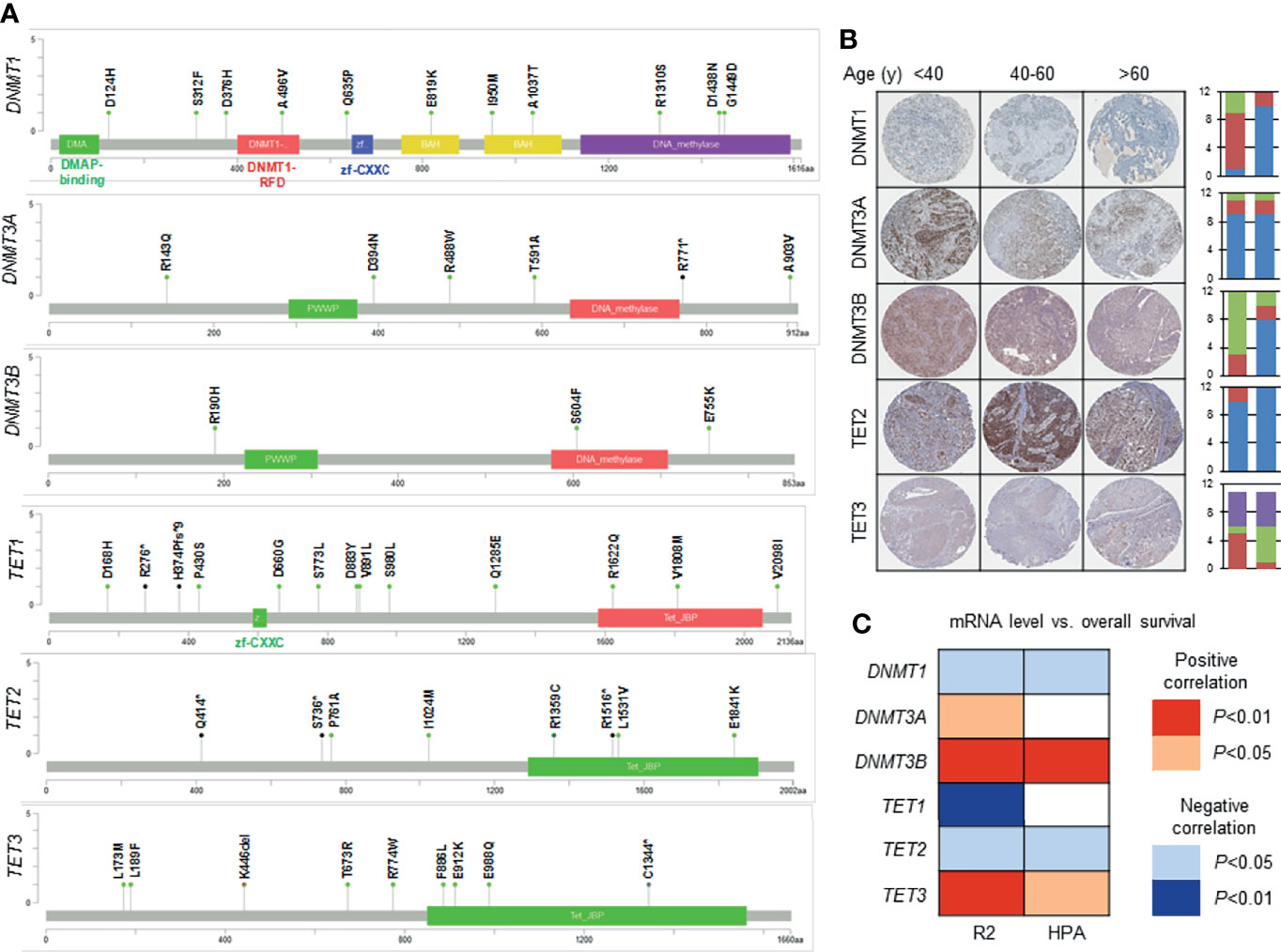
Figure 2 The alterations of DNA methylation-regulatory genes and their relationship with patient survival in ICC. The molecular alterations of DNA methylation modifiers at the genetic, transcriptomic, and protein levels, as well as their effects on the outcome of patients with ICC, are analyzed using various public available databases. (A) Genetic mutations (black—nonsense, green—missense, brown—in-frame deletion) of DNMTs and TETs in ICC, using the Cervical Squamous Cell Carcinoma dataset (TGCA, PanCancer Atlas; n = 294) on the cBioPortal for Cancer Genomics platform (www.cbioportal.org). (B) Immunohistochemical (IHC) staining of DNMTs and TETs in ICC, using the Cervical Cancer dataset on the Human Protein Atlas platform (www.proteinatlas.org). Representative images are shown. For each bar graph, the y-axis indicates the number of cases; the left bar indicates staining intensity (blue—strong, red—moderate, green—weak, purple—negative); the right bar indicates quantity (blue—>75%, red—25%~75%. green—<25%, purple—none). Note: the IHC data for TET1 are not available. (C) Relationship between mRNA levels of DNMTs or TETs and overall survival of ICC patients, using the Tumor Cervical Squamous Cell Carcinoma - TCGA dataset (TCGA ID: CESC; n = 303; DNMT1: high = 155, low = 148; DNMT3A: high = 270, low = 33; DNMT3B: high = 231, low = 72; TET1: high = 290, low = 13; TET2: high = 290, low = 13; TET3: high = 246, low = 57) on the R2: Genomics Analysis and Visualization Platform (http://r2.amc.nl) and the Cervical Cancer dataset (n = 291; DNMT1: high = 101, low = 190; DNMT3A: high = 204, low = 87; DNMT3B: high = 228, low = 63; TET1: high = 198, low = 93; TET2: high = 106, low = 185; TET3: high = 229, low = 62) on the Human Protein Atlas (HPA) platform (www.proteinatlas.org). Positive correlation = high mRNA levels correlate with poor outcome; Negative correlation = low mRNA levels correlate with poor outcome.
In addition to host cell DNA methylation, HPV DNA can also be methylated during malignant transformation. Viral genome methylation has either negative or positive effects on viral gene transcription. The HPV genome has highly condensed and conserved CpG sites (39). Altering CpG site methylation switches HPV infection from productive to transforming type (29). During carcinogenesis, HR-HPV-mediated hypermethylation is associated with the severity of cervical lesions, especially ICC (21, 40). Consistently, CIN2-3 lesions in patients with long-term (≥5 years), rather than short-term, HR-HPV infection exhibit cancer-like hypermethylation and abnormal chromatin features (40). Due to its specificity for CIN lesions and ICC pathogenesis, HPV DNA hypermethylation has attracted considerable attention in CIN/ICC screening and has been widely investigated in cervical histological and cytological specimens.
Markers of Host Cell Gene Methylation
An ideal biomarker involving DNA methylation is able to distinguish the majority (>90%) of cancer cases from non-malignant ones (41). A great number of studies have attempted to identify such markers for CIN/ICC screening. A meta-analysis on the methylation of 68 different genes from 51 studies has revealed high heterogeneity of the published data, which makes it difficult to identify appropriate methylation markers for screening cervical cancer (20, 36). Nonetheless, a number of studies have demonstrated the panels of methylated genes and non-coding RNAs for the screening and triage of CIN/ICC, of which the studies with a relatively large sample size of HR-HPV-positive women are summarized in Table 2. Among many genes investigated in these studies, some representative examples that have been relatively well studied are discussed as follows.
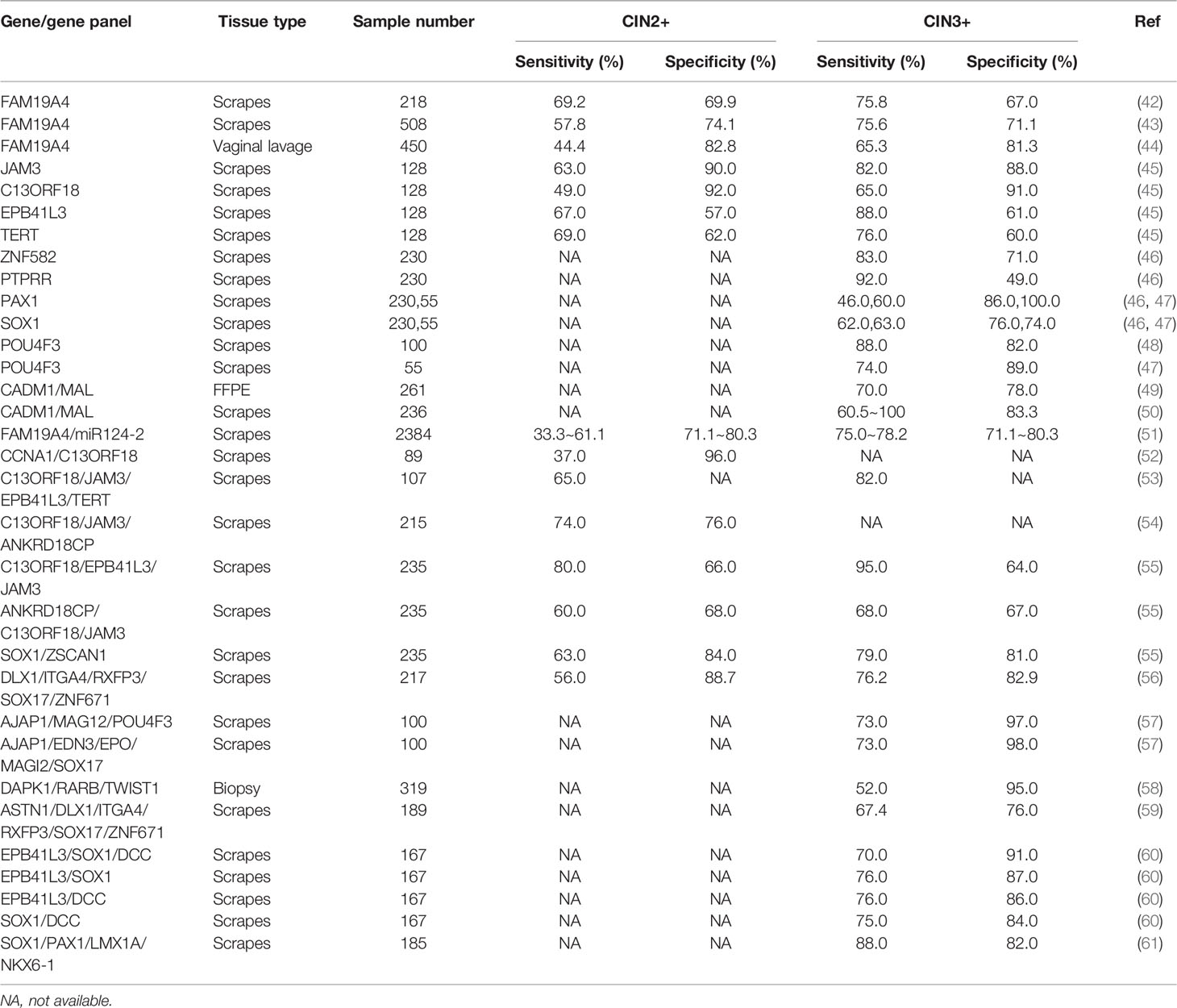
Table 2 Comparison of host gene methylation markers alone or in combination for detecting CIN2+/CIN3+ in HR-HPV-positive women.
CADM1 and MAL
CADM1 (also known as TSLC1) is a tumor-suppressor gene that encodes an intracellular adhesion protein of the immunoglobulin superfamily (62). Silencing of CADM1, due to its promoter hypermethylation, is common and associated with the severity of ICC (63). Functionally, CADM1 is involved in anchorage-independent growth of ICC cells (64). The frequency and density of methylation at the CADM1 promoter positively correlate with the grade of CIN lesions. Of note, abnormal methylation of the CADM1 promoter in cervical cytological biopsies could be detected 7 years before the diagnosis of ICC (63).
In chromosomal and transcriptional profiles of ICC, the MAL gene is downregulated in ICC samples compared to normal ones (65). MAL encodes T lymphocyte maturation-associated protein involving apical membrane transport and secretion (66, 67). Silencing of MAL via its promoter methylation contributes to the transformation and oncogenesis of HPV-infected cervical cells, suggesting MAL methylation as a diagnostic biomarker for squamous cell carcinoma (SCC) and adenocarcinoma (AdCA), as well as their precancerous lesions (68). However, another study has shown that MAL methylation fails to discriminate different grades of cervical lesions, possibly due to different methods and samples used to detect this methylation (69).
A panel combining CADM1 and MAL methylation can improve the specificity of screening cervical scraping samples and identify 90% of HR-HPV-positive women with CIN3 (49). Moreover, a prospective cohort study has investigated the triage value of a CADM1/MAL-specific methylation panel, demonstrating its performance comparable to cytology alone or in combination with HPV16/18 genotyping in distinguishing CIN3+, without missing any SCC/AdCA cases (50). However, a potential bias in favor of cytology cannot be ruled out because the women enrolled in this study are primarily referred to abnormal cytology. Notably, CADM1/MAL methylation is higher in CIN2/3 (5.3- to 6.2-fold) and carcinomas (143.5- to 454.9-fold) than those in CIN1 or normal cervical tissues; their methylation levels further increase (11.5- and 13.6-fold) in CIN2/3 with long-term HR-HPV infection (>5 years) (40). On the other hand, CADM1/MAL methylation is lesion-specific and associated with CIN severity, likely to indicate the worst lesions in women with multiple cervical lesions, particularly CIN3+ (70). Therefore, the panel combining CADM1 and MAL methylations may represent a promising triage approach for HR-HPV-positive women.
FAM19A4 and Hsa-miR-124
Hypermethylation of Hsa-miR-124, a well-recognized epigenetic silencer, has been observed in many types of cancer, including lung, breast, hepatocellular, gastric, and colon cancer, as well as leukemia (71–74). Hsa-miR-124 methylation increases in cervical scrapes and tissue specimens of women with ICC and its precancerous lesions, thus representing a common event functionally involved in oncogenesis of ICC (75).
FAM19A4 methylation has been identified as a promising biomarker for cervical oncogenesis via genome-wide DNA screening (76). In a large cohort of HR-HPV-positive women with high quality of cytology reading in Netherlands, FAM19A4 methylation assay could detect advanced CIN lesions and cervical cancer, with sensitivity and specificity of 75.8% and 67.0% for CIN3+, 69.2% and 69.9% for CIN2+, respectively (42). Moreover, the FAM19A4 methylation test displayed better clinical performance than cytology for most advanced lesions. Although its triage performance varies with age, FAM19A4 methylation is sensitive for detecting long-term CIN3 lesions and ICC (43). In HR-HPV-positive women with age >30 years, FAM19A4 methylation for detecting CIN3 exhibits similar sensitivity (88.3% versus 85.0%) and higher specificity (62.1% versus 47.6%) when compared with cytology. However, in women with age <30 years, its sensitivity is lower (50% versus 86.7%) than cytology, while the specificity is significantly higher (81.7% versus 52.4%). One explanation for such inconsistency between women with different ages is that younger women are more likely to have early CIN lesions and relatively short-term HR-HPV infection (77, 78). These findings indicate FAM19A4 methylation as an objective molecular triage marker for HR-HPV-positive women. This triage marker may be particularly useful in LMICs with poor cytology infrastructure, because it is not crucial to detect all precancerous lesions in the first screen as most of these lesions progress considerably slowly or even regress (79). While the age for ending the cervical cancer screening remains controversial, DNA methylation may offer more accurate screening-exit strategies as its alterations vary with age (80). The triage capacity of FAM19A4/miR-124-2 methylation in HPV-positive women with age >30 years, using the samples from the POBASCAM trial, has revealed 1.7% and 2.4% of 14-year cumulative ICC incidence in baseline methylation-negative and cytology-negative women, respectively (81). Compared to a negative cytology result, a negative result of the FAM19A4/miR-124-2 methylation test has similar capability to exclude the long-term risk of CIN3+ in HPV-positive women with age >30 years (82). In a multicenter prospective study, the triage capacity of combining FAM19A4/miR-124-2 methylation with HPV16/18 genotyping displayed high sensitivity (93.1% and 98.2%) and moderate specificity (49.4% and 46.3%) in women with either CIN3+ colposcopy results or age >30 years, better than either methylation test or HPV genotyping alone (83).
High sensitivity and specificity of the FAM19A4/miR-124-2 methylation test have been further validated for screening CIN/ICC in gynecologic outpatients in several other studies. In a large cohort of patients from 25 countries worldwide, the assessment of FAM19A4/miR-124-2 methylation is able to exclude the possibility of ICC by negative results, and its performance is not affected by sample types and geographical regions (84). The QIAsure methylation test used in this study to measure FAM19A4/miR124‐2 methylation has been further demonstrated to have high intra- and inter-laboratory agreement in another international study, confirming its accuracy and reproducibility, which warrant the robustness of this assay (85). Notably, the level of FAM19A4/miR-124-2 methylation in ICC is independent of histology type, geographical area, sample type, and HPV genotype (84). This finding has further been verified in a multicenter retrospective study (named VALID-SCREEN) (51). Moreover, this study has also revealed that the FAM19A4/miR-124-2 methylation test has an overall sensitivity of 77.2% and specificity of 78.3% for CIN3. Such high sensitivity and NPV for CIN3+ could be helpful to reduce the colposcopy referral rate and prolong the time to reexamination in clinical practice. Therefore, the FAM19A4/miR124-2 methylation test may represent a milestone for practical implementation of DNA methylation in cervical cancer screening.
Other Genes
In addition to the promising methylation markers described above, many other potential genes and panels have also been investigated in screening cervical tissue specimens or exfoliated cells.
The tumor-suppressor gene C13ORF18 encodes a phosphatase inhibitor, the reactivation of which inhibits tumor cell growth and induces apoptosis (86). C13ORF18 has been investigated virtually all in combination with other genes thus far. For example, methylation at the promoters of CCNA1 and C13ORF18 is associated with the severity of cervical lesions (52). Methylation of both genes displays high specificity for CIN2 or higher (97% and 100%, respectively), while the sensitivity for these lesions is low (37%) (52). A combination of primary HR-HPV testing with an assay using a methylation panel of JAM3, EPB41L3, TERT, and C13ORF18 can improve the capacity to detect CIN3+, when compared to the triage test combining HR-HPV with cytology, though in a hypothetical scenario analysis (53). A genomic methylation test of nine genes (ZSCAN1, ST6GALNAC5, ANKRD18CP, PAX2, CDH6, GFRA1, GATA4, KCNIP4, and LHX8) displays significantly different methylation patterns between CIN2/3 lesions and normal cervical samples. The combination panels of C13ORF18/JAM3/ANKRD18CP exhibited comparable sensitivity and specificity to cytology for CIN2+ in HR-HPV-positive scrapings (54). Unlike most of single-gene methylation markers that require a cutoff value to reach high specificity, no cutoff value is required for these methylation panels involving multiple genes. In a cohort of HR-HPV-positive patients, the values of three combinations involving six genes (JAM3, EPB41L3, C13ORF18, ANKRD18CP, ZSCAN1, and SOX1) for diagnosing CIN3+ have been evaluated in women who underwent colposcopy. While all three methylation panels (EPB41L3/JAM3, ANKRD18CP/C13ORF18/JAM3, and SOX1/ZSCAN1) exhibited high NPVs with sensitivities in a range of 68% to 95%, the SOX1/ZSCAN1 panel has higher specificity (84%) than the other two (55). Therefore, the methylation panels of multiple genes, rather than a single-gene methylation test, may provide a promising triage approach for cervical cancer screening.
EPB41L3 was initially identified as a tumor suppressor that is downregulated in lung carcinoma (87). Loss of its tumor suppressor activity has also been observed in breast cancer (88), prostate cancer (89), and meningiomas (90). EPB41L3 downregulation is most likely due to its promoter hypermethylation (91). An EPB41L3 methylation assay has been used to detect ICC and its precancerous lesions with promising performance, either alone or in combination with other human or viral genes, to triage HR-HPV-positive women and identify those with a risk of cervical oncogenesis (69). EPB41L3/ANKRD18CP methylation has lower sensitivity to detect CIN2+ in younger women than those with age >30 years (55). The lower methylation rate for younger women (<30 years) may be due to their relatively shorter period of HPV infection. Similar phenomena have been observed when another methylation signature involving five genes (DLX1, ITGA4, RXFP3, SOX17, and ZNF671) specific for CIN3+ was used (56).
ZNF582 is involved in DNA damage response, cell proliferation, cell-cycle regulation, and neoplastic transformation (92). Several robust studies have demonstrated that ZNF582 combined with other genes (ZNF582/PTPRR/PAX1/SOX1, ADCY8/CDH8/ZNF582) have excellent triage performance for women with cervical abnormal cytology (46, 93), while PAX1 methylation (PAX1m) alone has also shown a triage performance comparable to cytology and better accuracy, with higher specificity than HPV16/18 as the triage tool for CIN3+ in HR-HPV-positive women (94). In addition, a commercialized diagnostic test of ZNF582 methylation is undergoing development (95).
POU4F3 has diverse biological functions, including transcriptional regulation, cellular differentiation, and metabolic processes (57). Hypermethylation of POU4F3 suggests its potential role as a tumor suppressor in ICC (48). A retrospective case–control study has revealed that POU4F3 methylation exhibits good triage efficacy for CIN3+ in HR-HPV-positive women, with sensitivity of 74% and specificity of 89%, respectively (47).
Hypermethylation of DAPK1, RARB, or TWIST1 is able to identify histologically confirmed CIN3+, with specificity of 95% and relatively low sensitivity (60%) in a community-based study involving 2,609 women, which has thus been considered to have the screening performance superior to HR-HPV detection or abnormal cytology. The triage capacity of gene methylation (e.g., DAPK1 and RARB) for CIN3+ is comparable between African and non-African populations, suggesting potential use of these gene methylations in different populations (58).
Several methylation panels involving multiple genes have also been widely investigated. The triage efficacy of GynTect® (Oncgnostics GmbH, Jena, Germany), a methylation-specific real-time PCR assay targeting ASTN1, DLX1, ITGA4, RXFP3, SOX17, and ZNF671, could identify all cancer cases with an overall sensitivity of 67.7% for detecting CIN3+, particularly in women with age ≥30 years probably due to their long-term HR-HPV infection (59). In a comparison between two commercial DNA methylation-based diagnostic assays, GynTect® seems preferable due to its higher specificity for CIN2+ or CIN3+ than the QIAsure assay (96).
In an early study, methylation abnormalities of six genes (RRAD, SFRP1, MT1G, NMES1, SPARC, and TFPI2) have been observed in a subset of ICC samples but not in control samples (97). Methylation of twelve candidate genes (ADCYAP1, ASCL1, ATP10, CADM1, DCC, DBC1, HS3ST2, MOS, MYOD1, SOX1, SOX17, and TMEFF2) is significantly increased in CIN3+ but not lesions with grade <CIN2. Among them, methylation of seven genes (ADCYAP1, DCC, EPB41L3, HS3ST2, miR-124, MOS, and SOX1) has high accuracy for detecting CIN3+, despite the differences in methodology (60). A meta-analysis has validated that increased methylation at the promoters of several genes (CADM1, MAL, miR-124-2, FAM19A4, POU4F3, EPB41L3, PAX1, and SOX1) and HPV16 L1/L2 correlates to CIN lesion, with good performance in the triage of advanced CIN (20). While PEG3 methylation is associated with advanced CIN lesions (98), its efficacy for screening CIN/ICC needs to be further investigated. Because 3q gain is common in ICC, methylation of three genes (GHSR, SST, and ZIC1) is associated with 3q gain as well as the severity of CIN (99).
Among various histological types of ICC, SCC accounts for 80% of cases and thus represents the most common type, followed by AdCA (10%–20%), while other types include adenosquamous carcinoma and several rare ones (21). In this context, several methylation markers have been investigated in a histotype-dependent manner (100–106). For example, CADM1 is prevalently associated with cervical lesions in SCC than AdCA (64), while methylation of APC, TIMP3, and RASSF1A may distinguish AdCA from SCC (100). Methylation of MAL and FAM19A4 promoters is significantly increased in both SCC and AdCA compared to precancerous lesions (68, 76). Other genes (e.g., CDH1, DAPK1, EPB41L3, PAX1, PRDM14, and TERT) could also be methylated in SCC and adenocarcinoma (21). However, methylation of FAM19A4/miR-124-2 is common in ICC, including its rare histotypes (84).
Together, methylation of numerous host cell genes, either alone or in combination, have been considered powerful biomarkers to predict the progression of cervical cancer via the triage of HR-HPV positive women.
HR-HPV DNA Methylation Markers
Plenty of studies have focused on methylation changes in the HPV genome to identify specific markers for distinguishing CIN from ICC (Table 3). By understanding the molecular mechanism for HPV-mediated carcinogenesis, a link between CIN/ICC and methylation of the CpG sites of HPV L1, L2, E2-E4, E5, and URR has been well established. Particularly, a positive correlation between the level of L1 methylation and CIN2+ lesions appears to be consistent among multiple studies (107, 108, 116–120). However, the relationship between URR methylation and the severity of precancerous lesions remains controversial (17), likely due to the nature of the samples, differences in the CpG sites analyzed, and the diverse methods used.
Hypermethylation at L1, L2, and E2–4 CpG sites increases the risk of CIN3 (50-fold) compared to hypomethylation. Moreover, an increase in their methylation levels is associated with high-grade squamous intraepithelial lesion (HSIL) and the risk of advancing to CIN2+ in HPV16-positive women (116). The diagnostic value of HPV genome methylation has also been demonstrated in women with age >28 years, of which CpG methylation of L1 and L2 is particularly higher in pre-diagnostic CIN2+ samples (median time to diagnosis = 3 years) than control samples (108). The performance of HPV16 L1 CpG 6457 methylation to detect CIN2+ (sensitivity of 91.1% and specificity of 60.2%) (108) is comparable to that for p16-INK4a immunostaining (sensitivity of 92.6% and specificity of 63.2%) (121). However, it remains to be determined whether these viral methylation changes could predict CIN2+. The performance of HPV16 L1, L2 DNA methylation is consistent in different populations, suggesting a potential for expanding its application (116, 122). The average methylation level of twelve HPV16 L1 CpG loci is significantly higher in CIN3+ than in CIN1 or CIN2. However, the methylation of its loci 5,611 and 7,145 is more accurate to predict disease status than the average methylation level of 12 CpG sites, suggesting that the methylation test of a small number of CpG sites may represent a cost-effective option (109). Combining the HPV16 methylation test of six CpG sites (5,602, 6,650, 7,034, 7,461, 31, and 37) with E6 oncoprotein detection improves long-term risk stratification via triaging HPV16-positive women (110). Moreover, when combining with the E6 oncoprotein detection, the methylation test of either a single site or a panel covering multiple sites displays better predictive values than cytology.
Most studies on HR-HPV methylation and its relationship with premalignant cervical lesions have been focused on CpG sites of the HPV 16 genome (16). Approximately 40% of women with HPV16-positive cervical exfoliated cells have CIN2+ lesions (123). In the HPV16-negative women, the majority of CIN3+ cases are positive for other HR-HPV genotypes at baseline. Thus, the integration of the HPV methylation assay into the CIN/ICC screening may reduce the possibility of missing CIN3+, at least to a certain extent (110). In this context, multiple HPV DNA methylation assays can be used to improve HPV screening and genotyping for ICC (124). The whole-genome methylation analysis of HPV18/31/35 has indicated that methylation of these HR-HPV forms is common in CIN3 patients and may help determine which one is the causal infection (107). Moreover, this analysis has also revealed a high discrepancy in methylation of L1, L2, and E2 genes between CIN and ICC or CIN3 and SCC, while the methylation levels of URR, E1, E6, and E7 are considerably low. Methylation of HPV16/18/51 CpG sites is significantly higher in L1 than in URR for all three HPV forms, while the degree of methylation positively correlates with the severity of cervical neoplasia (125).
A population-based screening by co-testing cytology and HPV has indicated a clear link between increased methylation and CIN3/AIS cross all twelve HR-HPV forms, suggesting that HPV DNA methylation is a common phenomenon in transforming HPV infection. DNA methylation involving HR-HPV forms 5, 10, or 12, either alone or in combination with HPV16/18 genotyping, has a higher capability for risk assessment than cytology (111). Patients with negative results of the combination tests involving HR-HPV forms 10 and 12 also display a lower risk than cytology. However, they are currently used only in the high resource countries due to their cost.
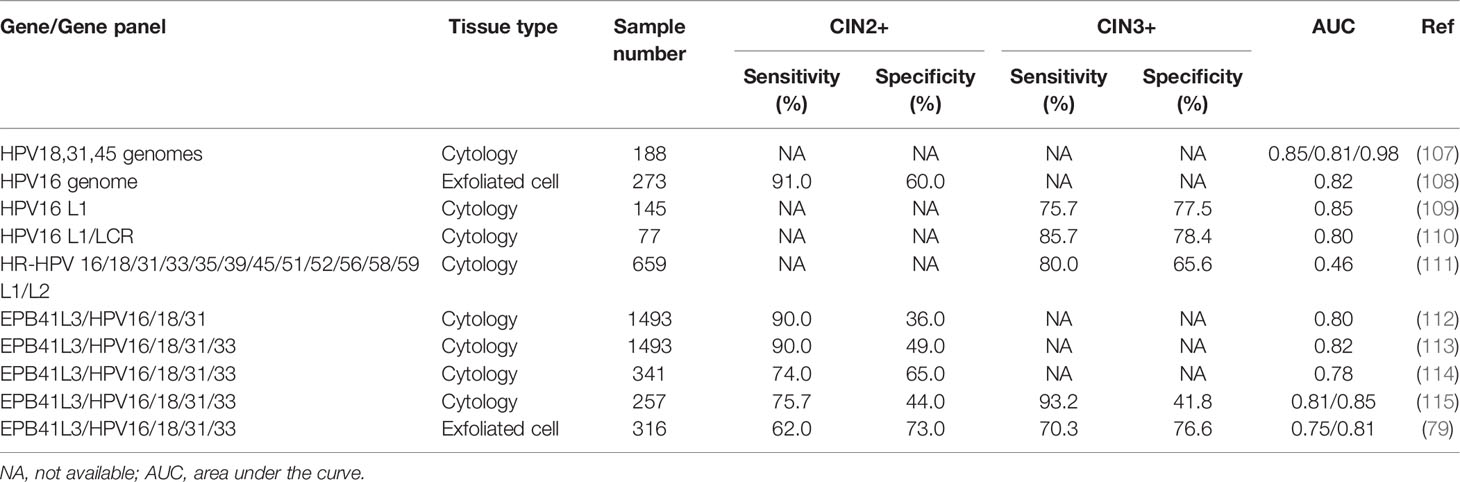
The Combination of the Host Cell Gene and HPV DNA Methylation
A test (named S4 classifier) combining the host gene EPB41L3 with HPV16-L1/L2, HPV18-L2, and HPV31-L1 to predict CIN2/3 increases the PPV with minimal loss of sensitivity in HR-HPV-positive women with abnormal cytology (112). Then, the S5 classifier upgraded from S4 by adding HPV33 significantly improves the ability to estimate early risk, with sensitivity of 90% and specificity of 49% (cut point = 0.8) for CIN2/3 in a colposcopy-referred population in Western Europe (113). Due to the limited number of the cases that could be selected from the colposcopy-referred population, the performance of S5 has been further assessed in exfoliated cervical samples from a population-based routine screening. The results have shown better sensitivity of S4 (cut point = 0.5; 69% and 74% for CIN2+ and CIN3+) or S5 (cut point = 0.8; 74% and 84% for CIN2+ and CIN3+) than HPV16/18 genotyping (54% and 58% for CIN2+ and CIN3+), with similar specificity between S5 and HPV16/18 genotyping in HPV-positive women (114). Furthermore, the performance of S5 has been evaluated in a population-based randomized controlled trial named HPV for Cervical Cancer Screening (HPV FOCAL) in North America, indicating that S5 detects a greater percentage of advanced CIN lesions (cutoff = 0.91; sensitivity = 75.7% and 93.2%, specificity = 44% and 41.8% for CIN2/3 or CIN, respectively) than other approaches (e.g., abnormal cytology and HPV16/18 genotyping) (115). These observations suggest that the S5 classifier could help identify women with a high short-term risk of progression to ICC who need immediate treatment. Another study for evaluating the performance of the S5 classifier to predict CIN2+ in HR-HPV-infected women referred for colposcopy has demonstrated that this classifier has high AUC (area under the curve) values in distinguishing women with CIN2+ from those with lesion grade < CIN2 (AUC = 0.75, 95% CI: 0.69–0.82) and for CIN3+ (AUC = 0.81, 95% CI: 0.74–0.89). As consequence, the S5 classifier could reduce colposcopy referrals by 30%–50% without affecting sensitivity for CIN2+ and CIN3+, therefore significantly improving cost-effectiveness to allow identification of women with a true risk of ICC (79).
Together, the assays for host cell gene and HR-HPV DNA methylation alone and particularly in combination represent a promising triage approach with high sensitivity, specificity, and PPV for screening premalignant cervical diseases in HR-HPV-positive women. Although most evidence has been obtained from cross-sectional or retrospective studies with a limited sample size thus far, such an approach warrants further investigation in prospective screening and intervention studies, especially to optimize host cell gene and HR-HPV DNA methylation markers.
The Potential Role of DNA Methylation Markers in Resolving Equivocal Diagnosis of CIN2
CIN2 is an equivocal diagnosis and thus considered as the least reproducible histopathologic type (126, 127), whereas approximately 40% of CIN2 lesions are manageable and only 5% would progress to ICC, compared to 33% and 12% for CIN3, respectively (128). Moreover, <1.5% of untreated patients with HSIL would progress to ICC within 24 months (129). A population-based study has shown that no less than 40% of young women (age ≤21 years) with histologically confirmed CIN2 experience spontaneous lesion regression during conservative follow-up with a median period longer than a year (130). Similarly, several studies have also revealed a high regression rate of histologically confirmed CIN2 lesions in young women (131, 132). Considering such a high regression rate, together with the risk of treatment-related adverse pregnancy outcomes (e.g., premature rupture of membranes or preterm labor) (133, 134), immediate treatment for biopsy-confirmed CIN2 lesions needs to be cautious, especially in young women who have fertility considerations (130, 135).
CIN2 represents a group of mixed lesions, including those from HPV infections (productive infections) to cancer precursors (transforming infections) as well as some early-transforming infections with insignificant risk of short-term progression to ICC (135, 136). Whereas the treatment options for CIN2 lesions vary, caution needs to be taken due to the fact that CIN2 lesions with productive infection and transforming infection cannot be distinguished morphologically (21). However, early-transforming infections could be distinguished from advanced transforming lesions based on their different degrees of genetic and epigenetic alterations. The HR-HPV-positive scrapings from women with CIN2/3 display heterogeneous DNA methylation patterns (involving ANKRD18CP, C13ORF18, EPB41L3, JAM3, SOX1, ZSCAN1, GHSR, SST, ZIC1, FAM19A4, PHACTR3, and PRDM14 genes). A study has revealed that three-quarters of CIN3 samples and half of CIN2 samples display a cancer-like hypermethylation pattern, suggesting a high risk of progression to ICC (137). Another study using methylation tests of three genes (SOX1, PAX1, and LMX1A) has shown that the percentage of methylation reference is significantly higher in CIN3+ than those for the normal cervix and CIN1 or CIN2 (61). Notably, comparable results between physician- and self-collected samples have been obtained when similar genes (PAX1, SOX1, and ZNF582) were used to detect CIN3+ (138). These observations raise a possibility to distinguish productive infections from transforming ones via examining the molecular alterations associated with transformation from viral infection to ICC. In this context, patients with high methylation levels, associated with advanced CIN lesions, should receive immediate treatment, while those with low methylation levels, reflecting low short-term progression risk of ICC, only need close follow-up.
Women with CIN2+ lesions and positive CADM1/MAL methylation are often older than those with methylation-negative CIN2+, in association with the fact that CIN2+ lesions in young women could spontaneously regress and thus belong to early CIN lesion (70). A methylation panel of ANKRD18CP and EPB41L3 genes has relatively low sensitivity to detect CIN2+ in women with age <30 years (55), consistent with other methylation tests involving DLX1, ITGA4, RXFP3, SOX17, and ZNF671 genes (56), or FAM19A4 (43), while low methylation rates have been observed in young women with CIN. In this context, young women are considered to have a shorter period of HPV infection and thus a lower methylation rate of target genes. In contrast, older women (age >30 years) with CIN2+ lesions more often have persistent HPV infection, in association with higher methylation rates and more advanced lesions (55). However, large longitudinal and multi-population studies are required to define the nature of CIN2 lesions with or without DNA methylation and to validate whether CIN2 lesions with a negative or low methylation level are less aggressive than those with a positive or high methylation level.
Incorporation of Self-Sampling Into DNA Methylation-Based Screening and Triage
Even in Western countries (e.g., Netherlands, UK, and US), there are approximately 30% of women who have not participated in annual cervical screening programs, while these women may however face a high risk of development to CIN and ICC (139–142). Moreover, more than 50% of ICC patients are diagnosed via various procedures other than population-based screening programs. Older non-attendees have a relatively higher risk of CIN lesions than younger ones, likely due to their poor screening history (143). This problem is even more severe in LMICs. Therefore, the development of a simple, inexpensive, and acceptable screening approach is crucial to increasing the participation rate of screening and thus reducing the incidence of ICC. In this case, the introduction of self-sampling HR-HPV tests could reduce the percentage of non-attendees (144–147). A systematic review and meta-analysis has demonstrated that self-sampling HR-HPV tests have comparable accuracy to those using physician-collected cervical scrapings (144, 148).
The DNA methylation analysis of C13ORF18, JAM3, EPB41L3, and TERT using a self-sampling lavage device has the diagnostic performance non-inferior to cytomorphology and the HR-HPV tests (149). The triage performance of the DNA methylation test using these four genes is also comparable between self- and physician-collected samples (45). Consistently, another methylation analysis of similar genes has also shown similar triage capacity when the samples were collected, transported, and stored under dry conditions, an approach more convenient than cervicovaginal lavage (150). A self-sampling MAL/miR-124-2 assay for CIN3+ and CIN2+ exhibits higher sensitivity than HPV16/18 genotyping (151). A randomized controlled trial of routine screening in HR-HPV-positive women has shown that the triage performance of self-sampling MAL/miR-124-2 methylation for CIN2+ is non-inferior to cytology using physician-collected smears, with a shorter diagnosis time but higher referral rate (152). A methylation assay of PAX1, SOX1, and ZNF582 has achieved moderate to high agreement between self-collected samples and physician-collected cervical scrapes (138). In a large prospective multicenter cohort study of matched self-collected cervicovaginal lavage samples and physician-taken cervical smears, a FAM19A4 methylation assay has slightly lower sensitivity but higher specificity to detect CIN3+ in self-collected samples than physician-taken ones in the HR-HPV-positive gynecologic outpatient population. Moreover, addition of HPV16/18 genotyping to this methylation assay could achieve an almost identical sensitivity between these two types of samples. Therefore, the combination of FAM19A4 methylation and HPV16/18 genotyping may represent a robust test with similar triage capacity in both sample types (44).
Unlike cytology that requires high sample quality, complicated screening procedures, well-trained/experienced cytologists, and resulting high rate of loss to follow-up (44, 153), a self-sampling approach is able to achieve one-sample one-visit screening, The latter remarkably simplifies the screening procedure and thus reduces the rate of loss to follow-up, especially in LMICs with high HR-HPV incidence but limited opportunity for screening (20, 154). However, several studies have shown that the self-sampling approach has a relatively high rate of colposcopy referral and thus an increase in medical expenses (152). Therefore, further investigations are required to address this issue to verify the value of the self-sampling DNA methylation assays in large prospective population-based screening trials.
Conclusions and Perspectives
With a marked reduction in the incidence of CIN/ICC due to effective screening and treatment in developed countries, more than 80% of cervical cancer cases currently occur in LMICs (155), primarily because of lacking various resources necessary for screening (156, 157). In this case, a simple, quick, affordable test using an objective biomarker that can be performed in the same sample used for the primary screen via a single “screen and treat” visit may help overcome this challenge in LMIC (158).
The standard of care for the triage of HR-HPV-positive women mainly includes cytology, p16-INK4A/Ki-67 immunostaining, and HPV16/18 genotyping (159). Cytology is widely used as a triage approach in developed countries (11), while the results may vary due to the influence of sampling, storage, and result interpretation (127, 160). Thus, the cytological test requires well-preserved cell morphology, complicated procedures, and skilled pathologists, which is thus not suitable for self-sampling high-throughput screening (161). Notably, an approach of cervical cytology, named ThinPrep Cytologic Test (TCT), has been developed to detect cervical cells using a liquid-based thin-layer cell detection system. TCT may improve cytological screening of CINs, particularly increasing the positive diagnosis rate of the small number and small size of high-grade squamous epithelial lesions. Nevertheless, some HPV-positive women with negative cytology may have dormant CIN lesions, even cervical cancer (162). Cross-sectional and longitudinal studies have revealed that p16-INK4A or dual-p16-INK4A and Ki-67 immunostaining is an alternative triage approach for women with HR-HPV infection (15, 163). Similar to cytology, this approach is also not suitable for application in LMICs due to lack of medical resources. HPV16/18 genotyping is recommended in the referral guidelines of the United States (164). It has a specificity of approximately 80% but a low sensitivity (~60%) for detecting CIN2+, therefore increasing colposcopy referral (161, 165, 166). The high rate of colposcopy referral increases financial burden and thus prevents HPV16/18 genotyping in LMICs (167, 168). Although several studies suggest the use of E6/E7 mRNA detection as a triage approach for HR-HPV-positive women (169, 170), its ability as an independent triage test has been considered insufficient (12, 171). In addition, HPV16/18 genotyping would miss other types of HPV infections.
Emerging evidence supports that DNA methylation changes in promoter regions of host genes and the HPV DNA genome often occur prior to carcinogenesis in ICC, which can be detected using the same sample of the HR-HPV test by relatively inexpensive assays (58, 116, 172–174). Thus, this kind of epigenetic abnormalities can be utilized either alone or in combination with cytology or HPV16/18 genotyping, for the triage of HR-HPV-positive women. These approaches are able to identify HR-HPV-infected patients that have a low short-term risk of development to ICC, especially young women with fertility requirements, who need only follow-up or treatment after childbirth. Compared to other triage approaches, the DNA methylation detection is mechanism-based and thus more precise, as well as more convenient with potential to be automated. Moreover, the methylation test can be performed on the same samples used for the HR-HPV test, thereby particularly suitable for self-collected samples, which simplifies the screening procedure and improves acceptability and coverage (11, 36, 175). This would particularly benefit LIMCs where the participation rate of screening is quite low (176). Moreover, the development of a high-throughput approach to improve the efficiency of DNA methylation detection could make it as a point-of-care test (same-day screening and treatment), which may significantly reduce the rate of loss to follow-up. Unlike cytology, the results of DNA methylation analysis are more homogeneous in multicenter studies (51, 152). Unlike HPV16/18 genotyping, DNA methylation detection is not restricted to the detection of CIN2+ involving HPV16/18 infection but also has higher sensitivity and comparable specificity for CIN2+ (20). More importantly, this type of triage approaches is anticipated to be advanced quickly due to the discovery of more sensitive and specific methylated genes and the development of new methodologies for genome-wide analysis, such as methylated DNA immunoprecipitation (MeDIP), methylated CpG island recovery assay combined with microarray analysis, and next-generation sequencing. They would allow the evaluation of novel CIN-specific methylation markers in population-based screening trials (53).
However, a number of issues remain to be addressed before applying DNA methylation detection for screening CIN/ICC. In most published studies, clinical samples for the methylation test were mainly obtained from patients screened by cytology or colposcopy referrals, which may not represent the women who anticipate population-based screening programs primarily using the HR-HPV test (51, 55). Moreover, as the indication for biopsy largely relies on the results of colposcopy, not all women enrolled into the published studies had histological endpoints, which could result in misclassification of some lesions due to the considerable variation in the sensitivity of cytology and colposcopy (177). Also considering the lower percentage of HPV-positive women with CIN lesions in the screening population than the gynecologic referral population, caution needs to be taken in translation of the findings from those studies into population-based screening (44). Cervical scraping is definitely more suitable for population-based screening and thus expected to be used widely in the near future. The value for identifying CIN3+ by a combination of multiple methylation markers in cervical tissue samples is different from that for cervical scrapes, probably due to the variation of background methylation levels caused by diverse cell types in tissue samples, but not scrapings. Therefore, the findings from the studies using tissue samples may not be applicable in cervical scrapes (68). For example, the gentle procedure, to avoid bleeding that causes poor visualization of colposcopy, for cervical scrape sampling may affect the quality of scrape samples (e.g., low concentrations of DNA that could lead to invalid results) (49). For example, a study has shown that the majority of DNA methylation results (~90%) obtained from cervical scrapes taken immediately before colposcopy could be invalid (44). Differences in the cutoff values used in the published studies may attribute to different screening population, sample size, specimen storage, etc. Thus, those cutoffs for DNA methylation tests need to be further validated in comparable populations, together with standardized procedures for sample collection and storage (122). A large proportion of the prospective studies have been conducted in the European populations (e.g., Netherlands and UK), of which most findings thus need to be further verified in other ethnic populations to avoid potential bias (20). Lastly, simple and inexpensive techniques for DNA methylation detection should be developed to make it more suitable for low-resource settings in LMICs. In this context, a consensus primer for amplifying 12 oncogenic HPV types has been developed to minimize the number of PCR reactions, representing a promising tool to detect viral methylation in women with HR-HPV infections (178).
Together, numerous studies have demonstrated that the DNA methylation detection of host cell genes or the HPV genome, or both, can serve as a primary approach for the triage of CIN/ICC. There are many advantages for using DNA methylation tests as a triage approach, including higher objectivity, more convenience, and comparable performance to cytology (158). This kind of triage approach could also help improve the allocation of healthcare resources to focus more on the treatment of high-risk women while sparing low-risk ones who only need conservative follow-up, especially in LMICs where the resources are quite limited. An ideal screening method requires both high sensitivity for detecting HR-HPV infections and strong capability for defining different infection statuses, together with adequate specificity and robust PPV for distinguishing CIN lesions (124). To this end, an increasing number of methylation markers have been shown to have higher sensitivity and non-inferior specificity compared to cytology. However, the majority of them have been investigated at the early stages in different populations thus far, while only a few have advanced to the late stage of clinical trials, and none has been approved for clinical use in daily practice. Thus, the DNA methylation markers and particularly their combination panels identified so far remain to be optimized (particularly by increasing triage specificity without impairing their high sensitivity), which may also require the identification of more novel methylation markers and panels. Nonetheless, with those advantages (e.g., relatively high sensitivity and non-inferior specificity compared to cytology, suitability for self-collected samples, and inexpensiveness), the host cell gene/HPV DNA methylation test represents a promising approach for the triage at the population level, allowing the early detection and accurate risk stratification of CINs to prevent their progression toward fatal ICC. Although there are several remaining concerns that need to be addressed, the introduction of host cell gene and HPV DNA methylation detection as a triage approach may lead to the era of molecular risk stratification for CIN lesions in HR-HPV-positive women, in order to precisely predict early and therefore prevent their progression to ICC in the near future.
Author Contributions
LZ, SZ, and YD conceptualized, designed, and wrote the review. WT and HY contributed to the literature collection and data interpretation. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (grant numbers 81471165, 81670190, 81671108, 81670189, and 81870160), Natural Science Foundation of the Jilin Province (grant numbers 20190201042JC and 20190201163JC), Science and Technology Development Program of the Jilin Province (No. 20210509010RQ), and Interdisciplinary Integration and Innovation Project of JLU.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The R2: Genomics Analysis and Visualization Platform (http://r2.amc.nl), the cBioPortal for Cancer Genomics platform (www.cbioportal.org), and Human Protein Atlas (HPA) platform (www.proteinatlas.org) were utilized for analyzing the expression of DNA methylation-regulatory genes or proteins and their relationship with overall survival in cervical cancer, respectively.
Abbreviations
HPV, human papillomavirus; HR-HPV, high-risk human papillomavirus, LMICs, low- and middle-income countries; CIN, cervical intraepithelial neoplasia; CIN1, grade 1 cervical intraepithelial neoplasia; CIN2, grade 2 cervical intraepithelial neoplasia; CIN3, grade 3 cervical intraepithelial neoplasia; CIN2+, CIN2 or worse; CIN3+, CIN3 or worse; ICC, invasive cervical cancer; SCC, squamous cell carcinoma; AdCA, adenocarcinoma; AIS, adenocarcinoma in situ; PPV, poor positive predictive value; NPV, negative predictive values; E2BS, E2-binding sites; URR, upstream regulatory region; DNMT, DNA methyltransferase; TP53, tumor protein p53; pRb, retinoblastoma protein; 5mC, 5-methylcytosine; CADM1, cell adhesion molecule 1; TSLC1, tumor suppressor in lung cancer 1; MAL, myelin and lymphocyte protein; CCNA1, cyclin A1; JAM3, junctional adhesion molecule 3; TERT, telomerase reverse transcriptase; ZSCAN1, zinc finger and SCAN domain containing 1; ST6GALNAC5, ST6 N-acetylgalactosaminide alpha-2,6-sialyltransferase 5; ANKRD18CP, ankyrin repeat domain 18C; PAX1, paired box gene 1; PAX2, paired box gene 2; CDH1, cadherin 1; CDH6, cadherin 6; GFRA1, GDNF family receptor alpha 1; GATA4, GATA-binding protein 4; KCNIP4, potassium voltage-gated channel interacting protein 4; LHX8, LIM homeobox 8; SOX1, SRY-box transcription factor 1; SOX17, SRY-box transcription factor 17; ZNF582, zinc finger protein 582; ZNF671, zinc finger protein 671; PTPRR, protein tyrosine phosphatase receptor type R; POU4F3, POU class 4 homeobox 3; DAPK1, death-associated protein kinase 1; RARB, retinoic acid receptor beta; ASTN1, astrotactin 1; DLX1, distal-less homeobox 1; ITGA4, integrin subunit alpha 4; RXFP3, relaxin family peptide receptor 3; CALCA, calcitonin-related polypeptide alpha; ESR1, estrogen receptor 1; APC, adenomatous polyposis coli; RRAD, Ras-related glycolysis inhibitor and calcium channel regulator; SFRP1, secreted frizzled related protein 1; MT1G, metallothionein 1G; NMES1, normal mucosa of esophagus-specific gene 1; SPARC, secreted protein acidic and cysteine rich; TFPI2, tissue factor pathway inhibitor 2; ADCYAP1, adenylate cyclase activating polypeptide 1; ASCL1, achaete-scute family BHLH transcription factor 1; DCC, deleted in colorectal carcinoma; DBC1, deleted in bladder cancer protein 1; HS3ST2, heparan sulfate-glucosamine 3-sulfotransferase 2; MYOD1, myogenic differentiation 1; TMEFF2, transmembrane protein with EGF like and two follistatin-like domains 2; TIMP3, tissue inhibitor of metalloproteinases 3; RASSF1, Ras association domain family member 1; PRDM14, PR/SET domain 14; qMSP, quantitative methylation-specific PCR; MeDIP, methylated DNA immunoprecipitation; AUC, area under the curve
Glossary
HPV: human papillomavirus
HR-HPV: high-risk human papillomavirus
LMICs: low- and middle-income countries
CIN: cervical intraepithelial neoplasia
CIN1: grade 1 cervical intraepithelial neoplasia
CIN2: grade 2 cervical intraepithelial neoplasia
CIN3: grade 3 cervical intraepithelial neoplasia
CIN2+: CIN2 or worse
CIN3+: CIN3 or worse
ICC: invasive cervical cancer
SCC: squamous cell carcinoma
AdCA: adenocarcinoma
AIS: adenocarcinoma in situ
PPV: poor positive predictive value
NPV: negative predictive values
E2BS: E2-binding sites
URR: upstream regulatory region
DNMT: DNA methyltransferase
TP53: tumor protein p53
pRb: retinoblastoma protein
5mC: 5-methylcytosine
CADM1: cell adhesion molecule 1
TSLC1: tumor suppressor in lung cancer 1
MAL: myelin and lymphocyte protein
CCNA1: cyclin A1
JAM3: junctional adhesion molecule 3
TERT: telomerase reverse transcriptase
ZSCAN1: zinc finger and SCAN domain containing 1
ST6GALNAC5: ST6 N-acetylgalactosaminide alpha-2,6-sialyltransferase 5
ANKRD18CP: ankyrin repeat domain 18C
PAX1: paired box gene 1
PAX2: paired box gene 2
CDH1: cadherin 1
CDH6: cadherin 6
GFRA1: GDNF family receptor alpha 1
GATA4: GATA-binding protein 4
KCNIP4: potassium voltage-gated channel interacting protein 4
LHX8: LIM homeobox 8
SOX1: SRY-box transcription factor 1
SOX17: SRY-box transcription factor 17
ZNF582: zinc finger protein 582
ZNF671: zinc finger protein 671
PTPRR: protein tyrosine phosphatase receptor type R
POU4F3: POU class 4 homeobox 3
DAPK1: death-associated protein kinase 1
RARB: retinoic acid receptor beta
ASTN1: astrotactin 1
DLX1: distal-less homeobox 1
ITGA4: integrin subunit alpha 4
RXFP3: relaxin family peptide receptor 3
CALCA: calcitonin-related polypeptide alpha
ESR1: estrogen receptor 1
APC: adenomatous polyposis coli
RRAD: Ras-related glycolysis inhibitor and calcium channel regulator
SFRP1: secreted frizzled related protein 1
MT1G: metallothionein 1G
NMES1: normal mucosa of esophagus-specific gene 1
SPARC: secreted protein acidic and cysteine rich
TFPI2: tissue factor pathway inhibitor 2
ADCYAP1: adenylate cyclase activating polypeptide 1
ASCL1: achaete-scute family BHLH transcription factor 1
DCC: deleted in colorectal carcinoma
DBC1: deleted in bladder cancer protein 1
HS3ST2: heparan sulfate-glucosamine 3-sulfotransferase 2
MYOD1: myogenic differentiation 1
TMEFF2: transmembrane protein with EGF like and two follistatin-like domains 2
TIMP3: tissue inhibitor of metalloproteinases 3
RASSF1: Ras association domain family member 1
PRDM14: PR/SET domain 14
qMSP: quantitative methylation-specific PCR
MeDIP: methylated DNA immunoprecipitation
AUC: area under the curve
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin (2021) 71:209–49. doi: 10.3322/caac.21660
2. Brisson M, Kim JJ, Canfell K, Drolet M, Gingras G, Burger EA, et al. Impact of HPV Vaccination and Cervical Screening on Cervical Cancer Elimination: A Comparative Modelling Analysis in 78 Low-Income and Lower-Middle-Income Countries. Lancet (2020) 395:575–90. doi: 10.1016/S0140-6736(20)30068-4
3. World Health Organization. WHO Director-General Calls for All Countries to Take Action to Help End the Suffering Caused by Cervical Cancer (2018). Available at: https://www.who.int/reproductivehealth/call-to-action-elimination-cervical-cancer/en/.
4. Belinson JL, Du H, Yang B, Wu R, Belinson SE, Qu X, et al. Improved Sensitivity of Vaginal Self-Collection and High-Risk Human Papillomavirus Testing. Int J Cancer (2012) 130:1855–60. doi: 10.1002/ijc.26202
5. Qiao YL, Sellors JW, Eder PS, Bao YP, Lim JM, Zhao FH, et al. A New HPV-DNA Test for Cervical-Cancer Screening in Developing Regions: A Cross-Sectional Study of Clinical Accuracy in Rural China. Lancet Oncol (2008) 9:929–36. doi: 10.1016/S1470-2045(08)70210-9
6. Leinonen M, Nieminen P, Kotaniemi-Talonen L, Malila N, Tarkkanen J, Laurila P, et al. Age-Specific Evaluation of Primary Human Papillomavirus Screening vs Conventional Cytology in a Randomized Setting. J Natl Cancer Inst (2009) 101:1612–23. doi: 10.1093/jnci/djp367
7. Balasubramanian A, Kulasingam SL, Baer A, Hughes JP, Myers ER, Mao C, et al. Accuracy and Cost-Effectiveness of Cervical Cancer Screening by High-Risk Human Papillomavirus DNA Testing of Self-Collected Vaginal Samples. J Low Genit Tract Dis (2010) 14:185–95. doi: 10.1097/LGT.0b013e3181cd6d36
8. Sowjanya AP, Paul P, Vedantham H, Ramakrishna G, Vidyadhari D, Vijayaraghavan K, et al. Suitability of Self-Collected Vaginal Samples for Cervical Cancer Screening in Periurban Villages in Andhra Pradesh, India. Cancer Epidemiol Biomarkers Prev (2009) 18:1373–8. doi: 10.1158/1055-9965.EPI-08-1171
9. Schiffman M, Wentzensen N, Wacholder S, Kinney W, Gage JC, Castle PE. Human Papillomavirus Testing in the Prevention of Cervical Cancer. J Natl Cancer Inst (2011) 103:368–83. doi: 10.1093/jnci/djq562
10. Cuzick J, Arbyn M, Sankaranarayanan R, Tsu V, Ronco G, Mayrand MH, et al. Overview of Human Papillomavirus-Based and Other Novel Options for Cervical Cancer Screening in Developed and Developing Countries. Vaccine (2008) 26:K29–41. doi: 10.1016/j.vaccine.2008.06.019
11. Lazcano-Ponce E, Lorincz AT, Cruz-Valdez A, Salmerón J, Uribe P, Velasco-Mondragón E, et al. Self-Collection of Vaginal Specimens for Human Papillomavirus Testing in Cervical Cancer Prevention (MARCH): A Community-Based Randomised Controlled Trial. Lancet (2011) 378:1868–73. doi: 10.1016/S0140-6736(11)61522-5
12. Luttmer R, Berkhof J, Dijkstra MG, van Kemenade FJ, Snijders PJ, Heideman DA, et al. Comparing Triage Algorithms Using HPV DNA Genotyping, HPV E7 mRNA Detection and Cytology in High-Risk HPV DNA-Positive Women. J Clin Virol (2015) 67:59–66. doi: 10.1016/j.jcv.2015.04.004
13. Rijkaart DC, Berkhof J, van Kemenade FJ, Coupe VM, Hesselink AT, Rozendaal L, et al. Evaluation of 14 Triage Strategies for HPV DNA-Positive Women in Population-Based Cervical Screening. Int J Cancer (2012) 130:602–10. doi: 10.1002/ijc.26056
14. Dijkstra MG, van Niekerk D, Rijkaart DC, van Kemenade FJ, Heideman DA, Snijders PJ, et al. Primary hrHPV DNA Testing in Cervical Cancer Screening: How to Manage Screen-Positive Women? A POBASCAM Trial Substudy. Cancer Epidemiol Biomarkers Prev (2014) 23:55–63. doi: 10.1158/1055-9965.EPI-13-0173
15. Carozzi F, Gillio-Tos A, Confortini M, Del Mistro A, Sani C, De Marco L, et al. Risk of High-Grade Cervical Intraepithelial Neoplasia During Follow-Up in HPV-Positive Women According to Baseline P16-INK4A Results: A Prospective Analysis of a Nested Substudy of the NTCC Randomised Controlled Trial. Lancet Oncol (2013) 14:168–76. doi: 10.1016/S1470-2045(12)70529-6
16. Clarke MA, Wentzensen N, Mirabello L, Ghosh A, Wacholder S, Harari A, et al. Human Papillomavirus DNA Methylation as a Potential Biomarker for Cervical Cancer. Cancer Epidemiol Biomarkers Prev (2012) 21:2125–37. doi: 10.1158/1055-9965.EPI-12-0905
17. Johannsen E, Lambert PF. Epigenetics of Human Papillomaviruses. Virology (2013) 445:205–12. doi: 10.1016/j.virol.2013.07.016
18. Szalmas A, Konya J. Epigenetic Alterations in Cervical Carcinogenesis. Semin Cancer Biol (2009) 19:144–52. doi: 10.1016/j.semcancer.2009.02.011
19. Lendvai A, Johannes F, Grimm C, Eijsink JJ, Wardenaar R, Volders HH, et al. Genome-Wide Methylation Profiling Identifies Hypermethylated Biomarkers in High-Grade Cervical Intraepithelial Neoplasia. Epigenetics (2012) 7:1268–78. doi: 10.4161/epi.22301
20. Kelly H, Benavente Y, Pavon MA, De Sanjose S, Mayaud P, Lorincz AT. Performance of DNA Methylation Assays for Detection of High-Grade Cervical Intraepithelial Neoplasia (CIN2+): A Systematic Review and Meta-Analysis. Br J Cancer (2019) 121:954–65. doi: 10.1038/s41416-019-0593-4
21. Steenbergen RD, Snijders PJ, Heideman DA, Meijer CJ. Clinical Implications of (Epi)Genetic Changes in HPV-Induced Cervical Precancerous Lesions. Nat Rev Cancer (2014) 14:395–405. doi: 10.1038/nrc3728
22. Halec G, Alemany L, Lloveras B, Schmitt M, Alejo, Bosch FX, et al. Pathogenic Role of the Eight Probably/Possibly Carcinogenic HPV Types 26, 53, 66, 67, 68, 70, 73 and 82 in Cervical Cancer. J Pathol (2014) 234:441–51. doi: 10.1002/path.4405
23. Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsague X, Shah KV, et al. Epidemiologic Classification of Human Papillomavirus Types Associated With Cervical Cancer. N Engl J Med (2003) 348:518–27. doi: 10.1056/NEJMoa021641
24. Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human Papillomavirus and Cervical Cancer. Lancet (2007) 370:890–907. doi: 10.1016/S0140-6736(07)61416-0
25. Doorbar J. Molecular Biology of Human Papillomavirus Infection and Cervical Cancer. Clin Sci (Lond) (2006) 110:525–41. doi: 10.1042/CS20050369
26. El Awady MK, Kaplan JB, O’Brien SJ, Burk RD. Molecular Analysis of Integrated Human Papillomavirus 16 Sequences in the Cervical Cancer Cell Line SiHa. Virology (1987) 159:389–98. doi: 10.1016/0042-6822(87)90478-8
27. Wentzensen N, Vinokurova S, von Knebel Doeberitz M. Systematic Review of Genomic Integration Sites of Human Papillomavirus Genomes in Epithelial Dysplasia and Invasive Cancer of the Female Lower Genital Tract. Cancer Res (2004) 64:3878–84. doi: 10.1158/0008-5472.CAN-04-0009
28. Snellenberg S, Schutze DM, Claassen-Kramer D, Meijer CJ, Snijders PJ, Steenbergen RD. Methylation Status of the E2 Binding Sites of HPV16 in Cervical Lesions Determined With the Luminex(R) xMAP System. Virology (2012) 422:357–65. doi: 10.1016/j.virol.2011.11.006
29. Vinokurova S, von Knebel Doeberitz M. Differential Methylation of the HPV 16 Upstream Regulatory Region During Epithelial Differentiation and Neoplastic Transformation. PloS One (2011) 6:e24451. doi: 10.1371/journal.pone.0024451
30. Bhattacharjee B, Sengupta S. CpG Methylation of HPV 16 LCR at E2 Binding Site Proximal to P97 is Associated With Cervical Cancer in Presence of Intact E2. Virology (2006) 354:280–5. doi: 10.1016/j.virol.2006.06.018
31. Piyathilake CJ, Macaluso M, Alvarez RD, Chen M, Badiga S, Edberg JC, et al. A Higher Degree of Methylation of the HPV 16 E6 Gene is Associated With a Lower Likelihood of Being Diagnosed With Cervical Intraepithelial Neoplasia. Cancer (2011) 117:957–63. doi: 10.1002/cncr.25511
32. Au Yeung CL, Tsang WP, Tsang TY, Co NN, Yau PL, Kwok TT. HPV-16 E6 Upregulation of DNMT1 Through Repression of Tumor Suppressor P53. Oncol Rep (2010) 24:1599–604. doi: 10.3892/or_00001023
33. Burgers WA, Blanchon L, Pradhan S, de Launoit Y, Kouzarides T, Fuks F. Viral Oncoproteins Target the DNA Methyltransferases. Oncogene (2007) 26:1650–5. doi: 10.1038/sj.onc.1209950
34. Moody CA, Laimins LA. Human Papillomavirus Oncoproteins: Pathways to Transformation. Nat Rev Cancer (2010) 10:550–60. doi: 10.1038/nrc2886
35. Korzeniewski N, Spardy N, Duensing A, Duensing S. Genomic Instability and Cancer: Lessons Learned From Human Papillomaviruses. Cancer Lett (2011) 305:113–22. doi: 10.1016/j.canlet.2010.10.013
36. Kremer WW, Steenbergen R, Heideman D, Kenter GG, Meijer C. The Use of Host Cell DNA Methylation Analysis in the Detection and Management of Women With Advanced Cervical Intraepithelial Neoplasia: A Review. BJOG (2021) 128:504–14. doi: 10.1111/1471-0528.16395
37. Stein RA. DNA Methylation Profiling: A Promising Tool and a Long Road Ahead for Clinical Applications. Int J Clin Pract (2011) 65:1212–3. doi: 10.1111/j.1742-1241.2011.02804.x
38. Deaton AM, Bird A. CpG Islands and the Regulation of Transcription. Genes Dev (2011) 25:1010–22. doi: 10.1101/gad.2037511
39. Galvan SC, Martinez-Salazar M, Galvan VM, Mendez R, Diaz-Contreras GT, Alvarado-Hermida M, et al. Analysis of CpG Methylation Sites and CGI Among Human Papillomavirus DNA Genomes. BMC Genomics (2011) 12:580. doi: 10.1186/1471-2164-12-580
40. Bierkens M, Hesselink AT, Meijer CJ, Heideman DA, Wisman GB, van der Zee AG, et al. CADM1 and MAL Promoter Methylation Levels in hrHPV-Positive Cervical Scrapes Increase Proportional to Degree and Duration of Underlying Cervical Disease. Int J Cancer (2013) 133:1293–9. doi: 10.1002/ijc.28138
41. Jeronimo C, Usadel H, Henrique R, Oliveira J, Lopes C, Nelson WG, et al. Quantitation of GSTP1 Methylation in Non-Neoplastic Prostatic Tissue and Organ-Confined Prostate Adenocarcinoma. J Natl Cancer Inst (2001) 93:1747–52. doi: 10.1093/jnci/93.22.1747
42. De Strooper LM, Meijer CJ, Berkhof J, Hesselink AT, Snijders PJ, Steenbergen RD, et al. Methylation Analysis of the FAM19A4 Gene in Cervical Scrapes is Highly Efficient in Detecting Cervical Carcinomas and Advanced CIN2/3 Lesions. Cancer Prev Res (Phila) (2014) 7:1251–7. doi: 10.1158/1940-6207.CAPR-14-0237
43. Luttmer R, De Strooper LM, Berkhof J, Snijders PJ, Dijkstra MG, Uijterwaal MH, et al. Comparing the Performance of FAM19A4 Methylation Analysis, Cytology and HPV16/18 Genotyping for the Detection of Cervical (Pre)Cancer in High-Risk HPV-Positive Women of a Gynecologic Outpatient Population (COMETH Study). Int J Cancer (2016) 138:992–1002. doi: 10.1002/ijc.29824
44. Luttmer R, De Strooper LM, Dijkstra MG, Berkhof J, Snijders PJ, Steenbergen RD, et al. FAM19A4 Methylation Analysis in Self-Samples Compared With Cervical Scrapes for Detecting Cervical (Pre)Cancer in HPV-Positive Women. Br J Cancer (2016) 115:579–87. doi: 10.1038/bjc.2016.200
45. Boers A, Bosgraaf RP, van Leeuwen RW, Schuuring E, Heideman DA, Massuger LF, et al. DNA Methylation Analysis in Self-Sampled Brush Material as a Triage Test in hrHPV-Positive Women. Br J Cancer (2014) 111:1095–101. doi: 10.1038/bjc.2014.392
46. Lin H, Chen TC, Chang TC, Cheng YM, Chen CH, Chu TY, et al. Methylated ZNF582 Gene as a Marker for Triage of Women With Pap Smear Reporting Low-Grade Squamous Intraepithelial Lesions - a Taiwanese Gynecologic Oncology Group (TGOG) Study. Gynecol Oncol (2014) 135:64–8. doi: 10.1016/j.ygyno.2014.08.012
47. Pun PB, Liao YP, Su PH, Wang HC, Chen YC, Hsu YW, et al. Triage of High-Risk Human Papillomavirus-Positive Women by Methylated POU4F3. Clin Epigenetics (2015) 7:85. doi: 10.1186/s13148-015-0122-0
48. Chen YC, Huang RL, Huang YK, Liao YP, Su PH, Wang HC, et al. Methylomics Analysis Identifies Epigenetically Silenced Genes and Implies an Activation of Beta-Catenin Signaling in Cervical Cancer. Int J Cancer (2014) 135:117–27. doi: 10.1002/ijc.28658
49. Overmeer RM, Louwers JA, Meijer CJ, van Kemenade FJ, Hesselink AT, Daalmeijer NF, et al. Combined CADM1 and MAL Promoter Methylation Analysis to Detect (Pre-)Malignant Cervical Lesions in High-Risk HPV-Positive Women. Int J Cancer (2011) 129:2218–25. doi: 10.1002/ijc.25890
50. Hesselink AT, Heideman DA, Steenbergen RD, Coupe VM, Overmeer RM, Rijkaart D, et al. Combined Promoter Methylation Analysis of CADM1 and MAL: An Objective Triage Tool for High-Risk Human Papillomavirus DNA-Positive Women. Clin Cancer Res (2011) 17:2459–65. doi: 10.1158/1078-0432.CCR-10-2548
51. Bonde J, Floore A, Ejegod D, Vink FJ, Hesselink A, van de Ven PM, et al. Methylation Markers FAM19A4 and Mir124-2 as Triage Strategy for Primary Human Papillomavirus Screen Positive Women: A Large European Multicenter Study. Int J Cancer (2021) 148:396–405. doi: 10.1002/ijc.33320
52. Yang N, Eijsink JJ, Lendvai A, Volders HH, Klip H, Buikema HJ, et al. Methylation Markers for CCNA1 and C13ORF18 are Strongly Associated With High-Grade Cervical Intraepithelial Neoplasia and Cervical Cancer in Cervical Scrapings. Cancer Epidemiol Biomarkers Prev (2009) 18:3000–7. doi: 10.1158/1055-9965.EPI-09-0405
53. Eijsink JJ, Lendvai A, Deregowski V, Klip HG, Verpooten G, Dehaspe L, et al. A Four-Gene Methylation Marker Panel as Triage Test in High-Risk Human Papillomavirus Positive Patients. Int J Cancer (2012) 130:1861–9. doi: 10.1002/ijc.26326
54. Boers A, Wang R, van Leeuwen RW, Klip HG, de Bock GH, Hollema H, et al. Discovery of New Methylation Markers to Improve Screening for Cervical Intraepithelial Neoplasia Grade 2/3. Clin Epigenetics (2016) 8:29. doi: 10.1186/s13148-016-0196-3
55. van Leeuwen RW, Ostrbenk A, Poljak M, van der Zee AGJ, Schuuring E, Wisman GBA. DNA Methylation Markers as a Triage Test for Identification of Cervical Lesions in a High Risk Human Papillomavirus Positive Screening Cohort. Int J Cancer (2019) 144:746–54. doi: 10.1002/ijc.31897
56. Hansel A, Steinbach D, Greinke C, Schmitz M, Eiselt J, Scheungraber C, et al. A Promising DNA Methylation Signature for the Triage of High-Risk Human Papillomavirus DNA-Positive Women. PloS One (2014) 9:e91905. doi: 10.1371/journal.pone.0091905
57. Wu X, Rauch TA, Zhong X, Bennett WP, Latif F, Krex D, et al. CpG Island Hypermethylation in Human Astrocytomas. Cancer Res (2010) 70:2718–27. doi: 10.1158/0008-5472.CAN-09-3631
58. Feng Q, Balasubramanian A, Hawes SE, Toure P, Sow PS, Dem A, et al. Detection of Hypermethylated Genes in Women With and Without Cervical Neoplasia. J Natl Cancer Inst (2005) 97:273–82. doi: 10.1093/jnci/dji041
59. Schmitz M, Wunsch K, Hoyer H, Scheungraber C, Runnebaum IB, Hansel A, et al. Performance of a Methylation Specific Real-Time PCR Assay as a Triage Test for HPV-Positive Women. Clin Epigenetics (2017) 9:118. doi: 10.1186/s13148-017-0419-2
60. Clarke MA, Luhn P, Gage JC, Bodelon C, Dunn ST, Walker J, et al. Discovery and Validation of Candidate Host DNA Methylation Markers for Detection of Cervical Precancer and Cancer. Int J Cancer (2017) 141:701–10. doi: 10.1002/ijc.30781
61. Lai HC, Lin YW, Huang RL, Chung MT, Wang HC, Liao YP, et al. Quantitative DNA Methylation Analysis Detects Cervical Intraepithelial Neoplasms Type 3 and Worse. Cancer (2010) 116:4266–74. doi: 10.1002/cncr.25252
62. Masuda M, Yageta M, Fukuhara H, Kuramochi M, Maruyama T, Nomoto A, et al. The Tumor Suppressor Protein TSLC1 is Involved in Cell-Cell Adhesion. J Biol Chem (2002) 277:31014–9. doi: 10.1074/jbc.M203620200
63. Steenbergen RD, Kramer D, Braakhuis BJ, Stern PL, Verheijen RH, Meijer CJ, et al. TSLC1 Gene Silencing in Cervical Cancer Cell Lines and Cervical Neoplasia. J Natl Cancer Inst (2004) 96:294–305. doi: 10.1093/jnci/djh031
64. Overmeer RM, Henken FE, Snijders PJ, Claassen-Kramer D, Berkhof J, Helmerhorst TJ, et al. Association Between Dense CADM1 Promoter Methylation and Reduced Protein Expression in High-Grade CIN and Cervical SCC. J Pathol (2008) 215:388–97. doi: 10.1002/path.2367
65. Wilting SM, de Wilde J, Meijer CJ, Berkhof J, Yi Y, van Wieringen WN, et al. Integrated Genomic and Transcriptional Profiling Identifies Chromosomal Loci With Altered Gene Expression in Cervical Cancer. Genes Chromosomes Cancer (2008) 47:890–905. doi: 10.1002/gcc.20590
66. Martin-Belmonte F, Puertollano R, Millan J, Alonso MA. The MAL Proteolipid is Necessary for the Overall Apical Delivery of Membrane Proteins in the Polarized Epithelial Madin-Darby Canine Kidney and Fischer Rat Thyroid Cell Lines. Mol Biol Cell (2000) 11:2033–45. doi: 10.1091/mbc.11.6.2033
67. Martin-Belmonte F, Arvan P, Alonso MA. MAL Mediates Apical Transport of Secretory Proteins in Polarized Epithelial Madin-Darby Canine Kidney Cells. J Biol Chem (2001) 276:49337–42. doi: 10.1074/jbc.M106882200
68. Overmeer RM, Henken FE, Bierkens M, Wilting SM, Timmerman I, Meijer CJ, et al. Repression of MAL Tumour Suppressor Activity by Promoter Methylation During Cervical Carcinogenesis. J Pathol (2009) 219:327–36. doi: 10.1002/path.2598
69. Vasiljevic N, Scibior-Bentkowska D, Brentnall AR, Cuzick J, Lorincz AT. Credentialing of DNA Methylation Assays for Human Genes as Diagnostic Biomarkers of Cervical Intraepithelial Neoplasia in High-Risk HPV Positive Women. Gynecol Oncol (2014) 132:709–14. doi: 10.1016/j.ygyno.2014.02.001
70. van Baars R, van der Marel J, Snijders PJ, Rodriquez-Manfredi A, ter Harmsel B, van den Munckhof HA, et al. CADM1 and MAL Methylation Status in Cervical Scrapes is Representative of the Most Severe Underlying Lesion in Women With Multiple Cervical Biopsies. Int J Cancer (2016) 138:463–71. doi: 10.1002/ijc.29706
71. Ando T, Yoshida T, Enomoto S, Asada K, Tatematsu M, Ichinose M, et al. DNA Methylation of microRNA Genes in Gastric Mucosae of Gastric Cancer Patients: Its Possible Involvement in the Formation of Epigenetic Field Defect. Int J Cancer (2009) 124:2367–74. doi: 10.1002/ijc.24219
72. Furuta M, Kozaki KI, Tanaka S, Arii S, Imoto I, Inazawa J. miR-124 and miR-203 are Epigenetically Silenced Tumor-Suppressive microRNAs in Hepatocellular Carcinoma. Carcinogenesis (2010) 31:766–76. doi: 10.1093/carcin/bgp250
73. Lujambio A, Ropero S, Ballestar E, Fraga MF, Cerrato C, Setien F, et al. Genetic Unmasking of an Epigenetically Silenced microRNA in Human Cancer Cells. Cancer Res (2007) 67:1424–9. doi: 10.1158/0008-5472.CAN-06-4218
74. Roman-Gomez J, Agirre X, Jimenez-Velasco A, Arqueros V, Vilas-Zornoza A, Rodriguez-Otero P, et al. Epigenetic Regulation of microRNAs in Acute Lymphoblastic Leukemia. J Clin Oncol (2009) 27:1316–22. doi: 10.1200/JCO.2008.19.3441
75. Wilting SM, van Boerdonk RA, Henken FE, Meijer CJ, Diosdado B, Meijer GA, et al. Methylation-Mediated Silencing and Tumour Suppressive Function of hsa-miR-124 in Cervical Cancer. Mol Cancer (2010) 9:167. doi: 10.1186/1476-4598-9-167
76. Steenbergen RD, Ongenaert M, Snellenberg S, Trooskens G, van der Meide WF, Pandey D, et al. Methylation-Specific Digital Karyotyping of HPV16E6E7-Expressing Human Keratinocytes Identifies Novel Methylation Events in Cervical Carcinogenesis. J Pathol (2013) 231:53–62. doi: 10.1002/path.4210
77. Ho GY, Bierman R, Beardsley L, Chang CJ, Burk RD. Natural History of Cervicovaginal Papillomavirus Infection in Young Women. N Engl J Med (1998) 338:423–8. doi: 10.1056/NEJM199802123380703
78. Insinga RP, Perez G, Wheeler CM, Koutsky LA, Garland SM, Leodolter S, et al. Incidence, Duration, and Reappearance of Type-Specific Cervical Human Papillomavirus Infections in Young Women. Cancer Epidemiol Biomarkers Prev (2010) 19:1585–94. doi: 10.1158/1055-9965.EPI-09-1235
79. Hernandez-Lopez R, Lorincz AT, Torres-Ibarra L, Reuter C, Scibior-Bentkowska D, Warman R, et al. Methylation Estimates the Risk of Precancer in HPV-Infected Women With Discrepant Results Between Cytology and HPV16/18 Genotyping. Clin Epigenetics (2019) 11:140. doi: 10.1186/s13148-019-0743-9
80. Bowden SJ, Lathouras K, Kyrgiou M. Can DNA Methylation Tests Improve the Accuracy of Cervical Screening? BJOG (2021) 128:515. doi: 10.1111/1471-0528.16448
81. De Strooper LMA, Berkhof J, Steenbergen RDM, Lissenberg-Witte BI, Snijders PJF, Meijer C, et al. Cervical Cancer Risk in HPV-Positive Women After a Negative FAM19A4/mir124-2 Methylation Test: A Post Hoc Analysis in the POBASCAM Trial With 14 Year Follow-Up. Int J Cancer (2018) 143:1541–8. doi: 10.1002/ijc.31539
82. Dick S, Kremer WW, De Strooper LMA, Lissenberg-Witte BI, Steenbergen RDM, Meijer C, et al. Long-Term CIN3+ Risk of HPV Positive Women After Triage With FAM19A4/miR124-2 Methylation Analysis. Gynecol Oncol (2019) 154:368–73. doi: 10.1016/j.ygyno.2019.06.002
83. Leeman A, Del Pino M, Marimon L, Torne A, Ordi J, Ter Harmsel B, et al. Reliable Identification of Women With CIN3+ Using hrHPV Genotyping and Methylation Markers in a Cytology-Screened Referral Population. Int J Cancer (2019) 144:160–8. doi: 10.1002/ijc.31787
84. Vink FJ, Meijer C, Clifford GM, Poljak M, Ostrbenk A, Petry KU, et al. FAM19A4/miR124-2 Methylation in Invasive Cervical Cancer: A Retrospective Cross-Sectional Worldwide Study. Int J Cancer (2020) 147:1215–21. doi: 10.1002/ijc.32614
85. Floore A, Hesselink A, Ostrbenk A, Alcaniz E, Rothe B, Pedersen H, et al. Intra- and Inter-Laboratory Agreement of the FAM19A4/mir124-2 Methylation Test: Results From an International Study. J Clin Lab Anal (2019) 33:e22854. doi: 10.1002/jcla.22854
86. Huisman C, Wisman GB, Kazemier HG, van Vugt MA, van der Zee AG, Schuuring E, et al. Functional Validation of Putative Tumor Suppressor Gene C13ORF18 in Cervical Cancer by Artificial Transcription Factors. Mol Oncol (2013) 7:669–79. doi: 10.1016/j.molonc.2013.02.017
87. Tran YK, Bogler O, Gorse KM, Wieland I, Green MR, Newsham IF. A Novel Member of the NF2/ERM/4.1 Superfamily With Growth Suppressing Properties in Lung Cancer. Cancer Res (1999) 59:35–43.
88. Takahashi Y, Iwai M, Kawai T, Arakawa A, Ito T, Sakurai-Yageta M, et al. Aberrant Expression of Tumor Suppressors CADM1 and 4.1B in Invasive Lesions of Primary Breast Cancer. Breast Cancer (2012) 19:242–52. doi: 10.1007/s12282-011-0272-7
89. Bernkopf DB, Williams ED. Potential Role of EPB41L3 (Protein 4.1B/Dal-1) as a Target for Treatment of Advanced Prostate Cancer. Expert Opin Ther Targets (2008) 12:845–53. doi: 10.1517/14728222.12.7.845
90. Gutmann DH, Donahoe J, Perry A, Lemke N, Gorse K, Kittiniyom K, et al. Loss of DAL-1, a Protein 4.1-Related Tumor Suppressor, is an Important Early Event in the Pathogenesis of Meningiomas. Hum Mol Genet (2000) 9:1495–500. doi: 10.1093/hmg/9.10.1495
91. Kikuchi S, Yamada D, Fukami T, Masuda M, Sakurai-Yageta M, Williams YN, et al. Promoter Methylation of DAL-1/4.1B Predicts Poor Prognosis in Non-Small Cell Lung Cancer. Clin Cancer Res (2005) 11:2954–61. doi: 10.1158/1078-0432.CCR-04-2206
92. Urrutia R. KRAB-Containing Zinc-Finger Repressor Proteins. Genome Biol (2003) 4:231. doi: 10.1186/gb-2003-4-10-231
93. Shen-Gunther J, Xia Q, Stacey W, Asusta HB. Molecular Pap Smear: Validation of HPV Genotype and Host Methylation Profiles of ADCY8, CDH8, and ZNF582 as a Predictor of Cervical Cytopathology. Front Microbiol (2020) 11:595902. doi: 10.3389/fmicb.2020.595902
94. Chang CL, Ho SC, Su YF, Juan YC, Huang CY, Chao AS, et al. DNA Methylation Marker for the Triage of hrHPV Positive Women in Cervical Cancer Screening: Real-World Evidence in Taiwan. Gynecol Oncol (2021) 161:429–35. doi: 10.1016/j.ygyno.2021.02.011
95. Beltran-Garcia J, Osca-Verdegal R, Mena-Molla S, Garcia-Gimenez JL. Epigenetic IVD Tests for Personalized Precision Medicine in Cancer. Front Genet (2019) 10:621. doi: 10.3389/fgene.2019.00621
96. Dippmann C, Schmitz M, Wunsch K, Schutze S, Beer K, Greinke C, et al. Triage of hrHPV-Positive Women: Comparison of Two Commercial Methylation-Specific PCR Assays. Clin Epigenetics (2020) 12:171. doi: 10.1186/s13148-020-00963-w
97. Sova P, Feng Q, Geiss G, Wood T, Strauss R, Rudolf V, et al. Discovery of Novel Methylation Biomarkers in Cervical Carcinoma by Global Demethylation and Microarray Analysis. Cancer Epidemiol Biomarkers Prev (2006) 15:114–23. doi: 10.1158/1055-9965.EPI-05-0323
98. Bosire C, Vidal AC, Smith JS, Jima D, Huang Z, Skaar D, et al. Association Between PEG3 DNA Methylation and High-Grade Cervical Intraepithelial Neoplasia. Infect Agent Cancer (2021) 16:42. doi: 10.1186/s13027-021-00382-3
99. Verlaat W, Snijders PJF, Novianti PW, Wilting SM, De Strooper LMA, Trooskens G, et al. Genome-Wide DNA Methylation Profiling Reveals Methylation Markers Associated With 3q Gain for Detection of Cervical Precancer and Cancer. Clin Cancer Res (2017) 23:3813–22. doi: 10.1158/1078-0432.CCR-16-2641
100. Wisman GB, Nijhuis ER, Hoque MO, Reesink-Peters N, Koning AJ, Volders HH, et al. Assessment of Gene Promoter Hypermethylation for Detection of Cervical Neoplasia. Int J Cancer (2006) 119(8):1908–14. doi: 10.1002/ijc.22060
101. Wilting SM, Snijders PJ, Meijer GA, Ylstra B, van den Ijssel PR, Snijders AM, et al. Increased Gene Copy Numbers at Chromosome 20q are Frequent in Both Squamous Cell Carcinomas and Adenocarcinomas of the Cervix. J Pathol (2006) 209:220–30. doi: 10.1002/path.1966
102. Dong SM, Kim HS, Rha SH, Sidransky D. Promoter Hypermethylation of Multiple Genes in Carcinoma of the Uterine Cervix. Clin Cancer Res (2001) 7:1982–6.
103. Jeong DH, Youm MY, Kim YN, Lee KB, Sung MS, Yoon HK, et al. Promoter Methylation of P16, DAPK, CDH1, and TIMP-3 Genes in Cervical Cancer: Correlation With Clinicopathologic Characteristics. Int J Gynecol Cancer (2006) 16:1234–40. doi: 10.1111/j.1525-1438.2006.00522.x
104. Kang S, Kim JW, Kang GH, Lee S, Park NH, Song YS, et al. Comparison of DNA Hypermethylation Patterns in Different Types of Uterine Cancer: Cervical Squamous Cell Carcinoma, Cervical Adenocarcinoma and Endometrial Adenocarcinoma. Int J Cancer (2006) 118:2168–71. doi: 10.1002/ijc.21609
105. Kang S, Kim HS, Seo SS, Park SY, Sidransky D, Dong SM. Inverse Correlation Between RASSF1A Hypermethylation, KRAS and BRAF Mutations in Cervical Adenocarcinoma. Gynecol Oncol (2007) 105:662–6. doi: 10.1016/j.ygyno.2007.01.045
106. Narayan G, Arias-Pulido H, Koul S, Vargas H, Zhang FF, Villella J, et al. Frequent promoter methylation of CDH1, DAPK, RARB, And HIC1 Genes in Carcinoma of Cervix Uteri: Its Relationship to Clinical Outcome. Mol Cancer (2003) 2:24. doi: 10.1186/1476-4598-2-24
107. Wentzensen N, Sun C, Ghosh A, Kinney W, Mirabello L, Wacholder S, et al. Methylation of HPV18, HPV31, and HPV45 Genomes and Cervical Intraepithelial Neoplasia Grade 3. J Natl Cancer Inst (2012) 104:1738–49. doi: 10.1093/jnci/djs425
108. Mirabello L, Schiffman M, Ghosh A, Rodriguez AC, Vasiljevic N, Wentzensen N, et al. Elevated Methylation of HPV16 DNA is Associated With the Development of High Grade Cervical Intraepithelial Neoplasia. Int J Cancer (2013) 132:1412–22. doi: 10.1002/ijc.27750
109. Kottaridi C, Kyrgiou M, Pouliakis A, Magkana M, Aga E, Spathis A, et al. Quantitative Measurement of L1 Human Papillomavirus Type 16 Methylation for the Prediction of Preinvasive and Invasive Cervical Disease. J Infect Dis (2017) 215:764–71. doi: 10.1093/infdis/jiw645
110. Dong L, Zhang L, Hu SY, Feng RM, Zhao XL, Zhang Q, et al. Risk Stratification of HPV 16 DNA Methylation Combined With E6 Oncoprotein in Cervical Cancer Screening: A 10-Year Prospective Cohort Study. Clin Epigenetics (2020) 12:62. doi: 10.1186/s13148-020-00853-1
111. Clarke MA, Gradissimo A, Schiffman M, Lam J, Sollecito CC, Fetterman B, et al. Human Papillomavirus DNA Methylation as a Biomarker for Cervical Precancer: Consistency Across 12 Genotypes and Potential Impact on Management of HPV-Positive Women. Clin Cancer Res (2018) 24:2194–202. doi: 10.1158/1078-0432.CCR-17-3251
112. Brentnall AR, Vasiljevic N, Scibior-Bentkowska D, Cadman L, Austin J, Szarewski A, et al. A DNA Methylation Classifier of Cervical Precancer Based on Human Papillomavirus and Human Genes. Int J Cancer (2014) 135:1425–32. doi: 10.1002/ijc.28790
113. Brentnall AR, Vasiljevic N, Scibior-Bentkowska D, Cadman L, Austin J, Cuzick J, et al. HPV33 DNA Methylation Measurement Improves Cervical Pre-Cancer Risk Estimation of an HPV16, HPV18, HPV31 and \Textit{EPB41L3} Methylation Classifier. Cancer biomark (2015) 15:669–75. doi: 10.3233/CBM-150507
114. Lorincz AT, Brentnall AR, Scibior-Bentkowska D, Reuter C, Banwait R, Cadman L, et al. Validation of a DNA Methylation HPV Triage Classifier in a Screening Sample. Int J Cancer (2016) 138:2745–51. doi: 10.1002/ijc.30008
115. Cook DA, Krajden M, Brentnall AR, Gondara L, Chan T, Law JH, et al. Evaluation of a Validated Methylation Triage Signature for Human Papillomavirus Positive Women in the HPV FOCAL Cervical Cancer Screening Trial. Int J Cancer (2019) 144:2587–95. doi: 10.1002/ijc.31976
116. Mirabello L, Sun C, Ghosh A, Rodriguez AC, Schiffman M, Wentzensen N, et al. Methylation of Human Papillomavirus Type 16 Genome and Risk of Cervical Precancer in a Costa Rican Population. J Natl Cancer Inst (2012) 104:556–65. doi: 10.1093/jnci/djs135
117. Kalantari M, Garcia-Carranca A, Morales-Vazquez CD, Zuna R, Montiel DP, Calleja-Macias IE, et al. Laser Capture Microdissection of Cervical Human Papillomavirus Infections: Copy Number of the Virus in Cancerous and Normal Tissue and Heterogeneous DNA Methylation. Virology (2009) 390:261–7. doi: 10.1016/j.virol.2009.05.006
118. Badal V, Chuang LS, Tan EH, Badal S, Villa LL, Wheeler CM, et al. CpG Methylation of Human Papillomavirus Type 16 DNA in Cervical Cancer Cell Lines and in Clinical Specimens: Genomic Hypomethylation Correlates With Carcinogenic Progression. J Virol (2003) 77:6227–34. doi: 10.1128/JVI.77.11.6227-6234.2003
119. Kalantari M, Calleja-Macias IE, Tewari D, Hagmar B, Lie K, Barrera-Saldana HA, et al. Conserved Methylation Patterns of Human Papillomavirus Type 16 DNA in Asymptomatic Infection and Cervical Neoplasia. J Virol (2004) 78:12762–72. doi: 10.1128/JVI.78.23.12762-12772.2004
120. Turan T, Kalantari M, Calleja-Macias IE, Cubie HA, Cuschieri K, Villa LL, et al. Methylation of the Human Papillomavirus-18 L1 Gene: A Biomarker of Neoplastic Progression? Virology (2006) 349:175–83. doi: 10.1016/j.virol.2005.12.033
121. Denton KJ, Bergeron C, Klement P, Trunk MJ, Keller T, Ridder R, et al. The Sensitivity and Specificity of P16(INK4a) Cytology vs HPV Testing for Detecting High-Grade Cervical Disease in the Triage of ASC-US and LSIL Pap Cytology Results. Am J Clin Pathol (2010) 134:12–21. doi: 10.1309/AJCP3CD9YKYFJDQL
122. Lorincz AT, Brentnall AR, Vasiljevic N, Scibior-Bentkowska D, Castanon A, Fiander A, et al. HPV16 L1 and L2 DNA Methylation Predicts High-Grade Cervical Intraepithelial Neoplasia in Women With Mildly Abnormal Cervical Cytology. Int J Cancer (2013) 133:637–44. doi: 10.1002/ijc.28050
123. Piyathilake CJ, Macaluso M, Brill I, Heimburger DC, Partridge EE. Lower Red Blood Cell Folate Enhances the HPV-16-Associated Risk of Cervical Intraepithelial Neoplasia. Nutrition (2007) 23:203–10. doi: 10.1016/j.nut.2006.12.002
124. Gradissimo A, Burk RD. Molecular Tests Potentially Improving HPV Screening and Genotyping for Cervical Cancer Prevention. Expert Rev Mol Diagn (2017) 17:379–91. doi: 10.1080/14737159.2017.1293525
125. Simanaviciene V, Popendikyte V, Gudleviciene Z, Zvirbliene A. Different DNA Methylation Pattern of HPV16, HPV18 and HPV51 Genomes in Asymptomatic HPV Infection as Compared to Cervical Neoplasia. Virology (2015) 484:227–33. doi: 10.1016/j.virol.2015.06.008
126. Holowaty P, Miller AB, Rohan T, To T. Natural History of Dysplasia of the Uterine Cervix. J Natl Cancer Inst (1999) 91:252–8. doi: 10.1093/jnci/91.3.252
127. Stoler MH, Schiffman M. Atypical Squamous Cells of Undetermined Significance-Low-Grade Squamous Intraepithelial Lesion Triage Study (ALTS) Group. Interobserver Reproducibility of Cervical Cytologic and Histologic Interpretations: Realistic Estimates From the ASCUS-LSIL Triage Study. JAMA (2001) 285:1500–5. doi: 10.1001/jama.285.11.1500
128. Ostor AG. Natural History of Cervical Intraepithelial Neoplasia: A Critical Review. Int J Gynecol Pathol (1993) 12:186–92. doi: 10.1097/00004347-199304000-00018
129. Melnikow J, Nuovo J, Willan AR, Chan BK, Howell LP. Natural History of Cervical Squamous Intraepithelial Lesions: A Meta-Analysis. Obstet Gyneco (1998) 92:727–35. doi: 10.1097/00006250-199810001-00046
130. Fuchs K, Weitzen S, Wu L, Phipps MG, Boardman LA. Management of Cervical Intraepithelial Neoplasia 2 in Adolescent and Young Women. J Pediatr Adolesc Gyneco (2007) 20:269–74. doi: 10.1016/j.jpag.2007.04.012
131. Moscicki AB, Ma Y, Wibbelsman C, Darragh TM, Powers A, Farhat S, et al. Rate of and Risks for Regression of Cervical Intraepithelial Neoplasia 2 in Adolescents and Young Women. Obstet Gyneco (2010) 116:1373–80. doi: 10.1097/AOG.0b013e3181fe777f
132. Tainio K, Athanasiou A, Tikkinen KAO, Aaltonen R, Cardenas J, Hernandes, et al. Clinical Course of Untreated Cervical Intraepithelial Neoplasia Grade 2 Under Active Surveillance: Systematic Review and Meta-Analysis. BMJ (2018) 360:k499. doi: 10.1136/bmj.k499
133. Wright TC Jr, Massad LS, Dunton CJ, Spitzer M, Wilkinson EJ, Solomon D, et al. 2006 Consensus Guidelines for the Management of Women With Cervical Intraepithelial Neoplasia or Adenocarcinoma in Situ. Am J Obstet Gyneco (2007) 197:340–5. doi: 10.1016/j.ajog.2007.07.050
134. Kyrgiou M, Athanasiou A, Paraskevaidi M, Mitra A, Kalliala I, Martin-Hirsch P, et al. Adverse Obstetric Outcomes After Local Treatment for Cervical Preinvasive and Early Invasive Disease According to Cone Depth: Systematic Review and Meta-Analysis. BMJ (2016) 354:i3633. doi: 10.1136/bmj.i3633
135. Castle PE, Stoler MH, Solomon D, Schiffman M. The Relationship of Community Biopsy-Diagnosed Cervical Intraepithelial Neoplasia Grade 2 to the Quality Control Pathology-Reviewed Diagnoses: An ALTS Report. Am J Clin Pathol (2007) 127:805–15. doi: 10.1309/PT3PNC1QL2F4D2VL
136. Carreon JD, Sherman ME, Guillen D, Solomon D, Herrero R, Jeronimo J, et al. CIN2 is a Much Less Reproducible and Less Valid Diagnosis Than CIN3: Results From a Histological Review of Population-Based Cervical Samples. Int J Gynecol Pathol (2007) 26:441–6. doi: 10.1097/pgp.0b013e31805152ab
137. Verlaat W, Van Leeuwen RW, Novianti PW, Schuuring E, Meijer C, van der Zee AGJ, et al. Host-Cell DNA Methylation Patterns During High-Risk HPV-Induced Carcinogenesis Reveal a Heterogeneous Nature of Cervical Pre-Cancer. Epigenetics (2018) 13:769–78. doi: 10.1080/15592294.2018.1507197
138. Chang CC, Huang RL, Liao YP, Su PH, Hsu YW, Wang HC, et al. Concordance Analysis of Methylation Biomarkers Detection in Self-Collected and Physician-Collected Samples in Cervical Neoplasm. BMC Cancer (2015) 15:418. doi: 10.1186/s12885-015-1411-x
139. Peto J, Gilham C, Fletcher O, Matthews FE. The Cervical Cancer Epidemic That Screening has Prevented in the UK. Lancet (2004) 364:249–56. doi: 10.1016/S0140-6736(04)16674-9
140. Sasieni PD, Cuzick J, Lynch-Farmery E, the National Co-ordinating Network for Cervical Screening Working Group. Estimating the Efficacy of Screening by Auditing Smear Histories of Women With and Without Cervical Cancer. Br J Cancer (1996) 73:1001–5. doi: 10.1038/bjc.1996.196
141. Sawaya GF, Grimes DA. New Technologies in Cervical Cytology Screening: A Word of Caution. Obstet Gyneco (1999) 94:307–10. doi: 10.1097/00006250-199908000-00029
142. Bos AB, Rebolj M, Habbema JD, van Ballegooijen M. Nonattendance Is Still the Main Limitation for the Effectiveness of Screening for Cervical Cancer in the Netherlands. Int J Cancer (2006) 119:2372–5. doi: 10.1002/ijc.22114
143. Gok M, Heideman DA, van Kemenade FJ, de Vries AL, Berkhof J, Rozendaal L, et al. Offering Self-Sampling for Human Papillomavirus Testing to Non-Attendees of the Cervical Screening Programme: Characteristics of the Responders. Eur J Cancer (2012) 48:1799–808. doi: 10.1016/j.ejca.2011.11.022
144. Snijders PJ, Verhoef VM, Arbyn M, Ogilvie G, Minozzi S, Banzi R, et al. High-Risk HPV Testing on Self-Sampled Versus Clinician-Collected Specimens: A Review on the Clinical Accuracy and Impact on Population Attendance in Cervical Cancer Screening. Int J Cancer (2013) 132:2223–36. doi: 10.1002/ijc.27790
145. Bais AG, van Kemenade FJ, Berkhof J, Verheijen RH, Snijders PJ, Voorhorst F, et al. Human Papillomavirus Testing on Self-Sampled Cervicovaginal Brushes: An Effective Alternative to Protect Nonresponders in Cervical Screening Programs. Int J Cancer (2007) 120:1505–10. doi: 10.1002/ijc.22484
146. Gok M, van Kemenade FJ, Heideman DA, Berkhof J, Rozendaal L, Spruyt JW, et al. Experience With High-Risk Human Papillomavirus Testing on Vaginal Brush-Based Self-Samples of Non-Attendees of the Cervical Screening Program. Int J Cancer (2012) 130:1128–35. doi: 10.1002/ijc.26128
147. Racey CS, Withrow DR, Gesink D. Self-Collected HPV Testing Improves Participation in Cervical Cancer Screening: A Systematic Review and Meta-Analysis. Can J Public Health (2013) 104:e159–66. doi: 10.1007/BF03405681
148. Arbyn M, Verdoodt F, Snijders PJ, Verhoef VM, Suonio E, Dillner L, et al. Accuracy of Human Papillomavirus Testing on Self-Collected Versus Clinician-Collected Samples: A Meta-Analysis. Lancet Oncol (2014) 15:172–83. doi: 10.1016/S1470-2045(13)70570-9
149. Eijsink JJ, Yang N, Lendvai A, Klip HG, Volders HH, Buikema HJ, et al. Detection of Cervical Neoplasia by DNA Methylation Analysis in Cervico-Vaginal Lavages, a Feasibility Study. Gynecol Oncol (2011) 120:280–3. doi: 10.1016/j.ygyno.2010.10.029
150. van Baars R, Bosgraaf RP, ter Harmsel BW, Melchers WJ, Quint WG, Bekkers RL. Dry Storage and Transport of a Cervicovaginal Self-Sample by Use of the Evalyn Brush, Providing Reliable Human Papillomavirus Detection Combined With Comfort for Women. J Clin Microbiol (2012) 50:3937–43. doi: 10.1128/JCM.01506-12
151. Hesselink AT, Heideman DA, Steenbergen RD, Gok M, van Kemenade FJ, Wilting SM, et al. Methylation Marker Analysis of Self-Sampled Cervico-Vaginal Lavage Specimens to Triage High-Risk HPV-Positive Women for Colposcopy. Int J Cancer (2014) 135:880–6. doi: 10.1002/ijc.28723
152. Verhoef VM, Bosgraaf RP, van Kemenade FJ, Rozendaal L, Heideman DA, Hesselink AT, et al. Triage by Methylation-Marker Testing Versus Cytology in Women Who Test HPV-Positive on Self-Collected Cervicovaginal Specimens (PROHTECT-3): A Randomised Controlled Non-Inferiority Trial. Lancet Oncol (2014) 15:315–22. doi: 10.1016/S1470-2045(14)70019-1
153. Brink AA, Meijer CJ, Wiegerinck MA, Nieboer TE, Kruitwagen RF, van Kemenade F, et al. High Concordance of Results of Testing for Human Papillomavirus in Cervicovaginal Samples Collected by Two Methods, With Comparison of a Novel Self-Sampling Device to a Conventional Endocervical Brush. J Clin Microbiol (2006) 44:2518–23. doi: 10.1128/JCM.02440-05
154. Gok M, Heideman DA, van Kemenade FJ, Berkhof J, Rozendaal L, Spruyt JW, et al. HPV Testing on Self Collected Cervicovaginal Lavage Specimens as Screening Method for Women Who do Not Attend Cervical Screening: Cohort Study. BMJ (2010) 340:c1040. doi: 10.1136/bmj.c1040
155. Simms KT, Steinberg J, Caruana M, Smith MA, Lew JB, Soerjomataram I, et al. Impact of Scaled Up Human Papillomavirus Vaccination and Cervical Screening and the Potential for Global Elimination of Cervical Cancer in 181 Countries, 2020-99: A Modelling Study. Lancet Oncol (2019) 20:394–407. doi: 10.1016/S1470-2045(18)30836-2
156. Vaccarella S, Laversanne M, Ferlay J, Bray F. Cervical Cancer in Africa, Latin America and the Caribbean and Asia: Regional Inequalities and Changing Trends. Int J Cancer (2017) 141:1997–2001. doi: 10.1002/ijc.30901
157. Basu P, Mittal S, Bhadra Vale D, Chami Kharaji Y. Secondary Prevention of Cervical Cancer. Best Pract Res Clin Obstet Gynaecol (2018) 47:73–85. doi: 10.1016/j.bpobgyn.2017.08.012
158. Cuschieri K, Ronco G, Lorincz A, Smith L, Ogilvie G, Mirabello L, et al. Eurogin Roadmap 2017: Triage Strategies for the Management of HPV-Positive Women in Cervical Screening Programs. Int J Cancer (2018) 143:735–45. doi: 10.1002/ijc.31261
159. Cuzick J, Bergeron C, von Knebel Doeberitz M, Gravitt P, Jeronimo J, Lorincz AT, et al. New Technologies and Procedures for Cervical Cancer Screening. Vaccine (2012) 30 Suppl 5:F107–16. doi: 10.1016/j.vaccine.2012.05.088
160. Cuzick J, Clavel C, Petry KU, Meijer CJ, Hoyer H, Ratnam S, et al. Overview of the European and North American Studies on HPV Testing in Primary Cervical Cancer Screening. Int J Cancer (2006) 119:1095–101. doi: 10.1002/ijc.21955
161. Ebisch RM, Siebers AG, Bosgraaf RP, Massuger LF, Bekkers RL, Melchers WJ. Triage of High-Risk HPV Positive Women in Cervical Cancer Screening. Expert Rev Anticancer Ther (2016) 16:1073–85. doi: 10.1080/14737140.2016.1232166
162. Kinney W, Fetterman B, Cox JT, Lorey T, Flanagan T, Castle PE. Characteristics of 44 Cervical Cancers Diagnosed Following Pap-Negative, High Risk HPV-Positive Screening in Routine Clinical Practice. Gynecol Oncol (2011) 121:309–13. doi: 10.1016/j.ygyno.2010.12.361
163. Ikenberg H, Bergeron C, Schmidt D, Griesser H, Alameda F, Angeloni C, et al. Screening for Cervical Cancer Precursors With P16/Ki-67 Dual-Stained Cytology: Results of the PALMS Study. J Natl Cancer Inst (2013) 105:1550–7. doi: 10.1093/jnci/djt235
164. Twiggs LB, Hopkins M. High-Risk HPV DNA Testing and HPV-16/18 Genotyping: What is the Clinical Application? J Low Genit Tract Dis (2011) 15:224–30. doi: 10.1097/LGT.0b013e3181fb46d8
165. Luttmer R, De Strooper LM, Steenbergen RD, Berkhof J, Snijders PJ, Heideman DA, et al. Management of High-Risk HPV-Positive Women for Detection of Cervical (Pre)Cancer. Expert Rev Mol Diagn (2016) 16:961–74. doi: 10.1080/14737159.2016.1217157
166. Castle PE, Stoler MH, Wright TC Jr, Sharma A, Wright TL, Behrens CM. Performance of Carcinogenic Human Papillomavirus (HPV) Testing and HPV16 or HPV18 Genotyping for Cervical Cancer Screening of Women Aged 25 Years and Older: A Subanalysis of the ATHENA Study. Lancet Oncol (2011) 12:880–90. doi: 10.1016/S1470-2045(11)70188-7
167. Lazcano-Ponce E, Lorincz AT, Torres L, Salmeron J, Cruz A, Rojas R, et al. Specimen Self-Collection and HPV DNA Screening in a Pilot Study of 100,242 Women. Int J Cancer (2014) 135:109–16. doi: 10.1002/ijc.28639
168. Beal CM, Salmeron J, Flores YN, Torres L, Granados-Garcia V, Dugan E, et al. Cost Analysis of Different Cervical Cancer Screening Strategies in Mexico. Salud Publica Mex (2014) 56:429–501. doi: 10.21149/spm.v56i5.7374
169. Yang YM, Wang SJ, Wang FY, Chen R, Xiao Q, Kang N, et al. Preliminary Study of the Use of E6/E7mRNA Detection in Screening and Triage Management of HR-HPV Infection During Pregnancy. Ann Transl Med (2021) 9:1428. doi: 10.21037/atm-21-4026
170. Yao YL, Tian QF, Cheng B, Cheng YF, Ye J, Lu WG. Human Papillomavirus (HPV) E6/E7 mRNA Detection in Cervical Exfoliated Cells: A Potential Triage for HPV-Positive Women. J Zhejiang Univ Sci B (2017) 18:256–62. doi: 10.1631/jzus.B1600288
171. Rossi PG, Carozzi F, Ronco G, Allia E, Bisanzi S, Gillio-Tos A, et al. P16/Ki67 and E6/E7 mRNA Accuracy and Prognostic Value in Triaging HPV DNA-Positive Women. J Natl Cancer Inst (2021) 113:292–300. doi: 10.1093/jnci/djaa105
172. Turan T, Kalantari M, Cuschieri K, Cubie HA, Skomedal H, Bernard HU. High-Throughput Detection of Human Papillomavirus-18 L1 Gene Methylation, a Candidate Biomarker for the Progression of Cervical Neoplasia. Virology (2007) 361:185–93. doi: 10.1016/j.virol.2006.11.010
173. Brandsma JL, Sun Y, Lizardi PM, Tuck DP, Zelterman D, Haines GK 3rd, et al. Distinct Human Papillomavirus Type 16 Methylomes in Cervical Cells at Different Stages of Premalignancy. Virology (2009) 389:100–7. doi: 10.1016/j.virol.2009.03.029
174. Badal S, Badal V, Calleja-Macias IE, Kalantari M, Chuang LS, Li BF, et al. The Human Papillomavirus-18 Genome is Efficiently Targeted by Cellular DNA Methylation. Virology (2004) 324:483–92. doi: 10.1016/j.virol.2004.04.002
175. De Strooper LMA, Verhoef VMJ, Berkhof J, Hesselink AT, de Bruin HME, van Kemenade FJ, et al. Validation of the FAM19A4/mir124-2 DNA Methylation Test for Both Lavage- and Brush-Based Self-Samples to Detect Cervical (Pre)Cancer in HPV-Positive Women. Gynecol Oncol (2016) 141:341–7. doi: 10.1016/j.ygyno.2016.02.012
176. Almonte M, Murillo R, Sanchez GI, Jeronimo J, Salmeron J, Ferreccio C, et al. [New Paradigms and Challenges in Cervical Cancer Prevention and Control in Latin America]. Salud Publica Mex (2010) 52:544–59. doi: 10.1590/s0036-36342010000600010
177. Louwers J, Zaal A, Kocken M, Ter Harmsel W, Graziosi G, Spruijt J, et al. Dynamic Spectral Imaging Colposcopy: Higher Sensitivity for Detection of Premalignant Cervical Lesions. BJOG (2011) 118:309–18. doi: 10.1111/j.1471-0528.2010.02806.x
Keywords: DNA methylation, host cell gene, high-risk human papillomavirus, cervical intraepithelial neoplasia, cervical cancer, triage
Citation: Zhang L, Tan W, Yang H, Zhang S and Dai Y (2022) Detection of Host Cell Gene/HPV DNA Methylation Markers: A Promising Triage Approach for Cervical Cancer. Front. Oncol. 12:831949. doi: 10.3389/fonc.2022.831949
Received: 09 December 2021; Accepted: 28 February 2022;
Published: 25 March 2022.
Edited by:
Mariela Vasileva-Slaveva, Shterev Hospital, BulgariaReviewed by:
Pengming Sun, Fujian Women and Children Hospital, ChinaYu Ligh Liou, The First Affiliated Hospital of Guangdong Pharmaceutical University, China
Bea Wisman, University Medical Center Groningen, Netherlands
Copyright © 2022 Zhang, Tan, Yang, Zhang and Dai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Songling Zhang, c2x6aGFuZ0BqbHUuZWR1LmNu; Yun Dai, ZGFpeXVuQGpsdS5lZHUuY24=; ZGFpeXVuNjJAaG90bWFpbC5jb20=
†ORCID: Yun Dai, orcid.org/0000-0003-2285-0818
 Lingyi Zhang
Lingyi Zhang Wenxi Tan
Wenxi Tan Hongmei Yang
Hongmei Yang Songling Zhang
Songling Zhang Yun Dai
Yun Dai