- 1Division of Gynecologic Oncology, Department of Gynecology and Obstetrics, Loma Linda University School of Medicine, Loma Linda, CA, United States
- 2Division of Gynecologic Oncology, Department of Oncology, Karmanos Cancer Institute, Wayne State University, Detroit, MI, United States
- 3Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Kaiser Permanente Washington, Seattle, WA, United States
- 4Division of Gynecologic Oncology, Department of Obstetrics, Gynecology and Women’s Health, University of Minnesota, Minneapolis, MN, United States
- 5Department of Oncology, Sutter Medical Group, Sacramento, CA, United States
- 6Division of Gynecologic Oncology and Gynecology, Department of Surgery, Virginia Mason Medical Center, Seattle, WA, United States
- 7Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Prevea Health, Green Bay, WI, United States
- 8Independent Researcher, Washington, DC, United States
Objective: Women make up a majority of the gynecologic oncology workforce. Increasing the numbers of women in leadership has been proposed as a path towards professional gender equity. This study examined whether leadership gender and departmental infrastructure impact the work environment for women gynecologic oncologists.
Methods: Members of a 472-member private Facebook group “Women of Gynecologic Oncology” (WGO) who self-identified as women gynecologic oncologists provided demographics, practice infrastructure, personal experience with workplace bullying, gender discrimination, microaggressions using a REDcap survey platform.
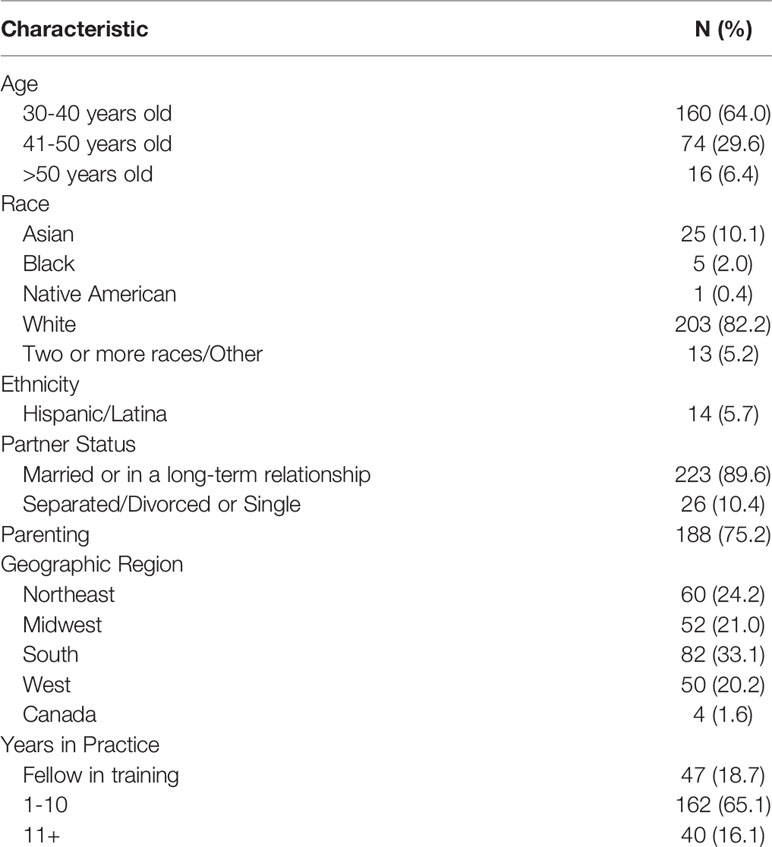
Results: Of 250 (53%) respondents to this survey, most were younger than age 50 years (93.6%); White (82.2%) and non-Hispanic (94.3%); married (84.7%); and parenting (75.2%). Practice environments included academic (n=152, 61.0%), hospital employed (n=57, 22.9%), and private practice (n=31, 12.4%), and 89.9% supervised trainees. A significant percent of respondents had experienced bullying (52.8%), gender discrimination (57%) and microaggressions (83%). Age, race, ethnicity, practice setting, or mentorship were not statistically significantly associated with these experiences. Reported perpetrators were varied and included colleagues (84%), patients (44%), staff (41%), administrators (18%), and trainees (16%). Prevalence of bullying (55.0 vs 47.7%, p=0.33), gender discrimination (59.1 vs 52.3%, p=0.33) and microaggressions (83.3 vs 83.0%, p=1.00) were similar irrespective of departmental leadership gender.
Conclusions: Women gynecologic oncologists report a high prevalence of workplace bullying, gender discrimination and microaggressions regardless of the gender of their immediate leadership. Proactive and deliberate structural interventions to improve the work environment for surgeons who are women are urgently needed.
Introduction
Gender equity remains a critical issue for physicians who are surgeons (1). Although women have comprised more than half of medical students since 2003, women have remained less likely to enter and remain within surgical specialties (1, 2). Gynecology is a notable exception. By the 1990’s half of trainees in obstetrics and gynecology were women. More than half of physicians practicing obstetrics and gynecology have been women since 2012; currently 59% of practicing gynecologists are women and 83% of trainees are women (3–5). Gynecologic oncology is a unique gynecologic subspecialty that requires competency in radical pelvic surgery including upper abdominal, bowel and bladder procedures. Similar to obstetrics and gynecology as a whole, increasing numbers of women have entered this field. In 2020, more than half of gynecologic oncologists and 70% of trainees self-identified as female (6).
Despite the majority of gynecologic oncologists identifying as women, recent literature supports the persistence of significant gender disparities in attaining leadership (7), a gender wage gap that is unexplained by experience or skill (6, 8), and high rates of perceived discrimination (9, 10). In a recent survey of gynecologic oncologists, 64% of female respondents endorsed gender discrimination in training or practice (10). Women remain under-represented in leadership relevant to gynecologic oncology including division director and department chair, but the presence of women in leadership roles has been previously associated with positive work environments within the subspecialty (7).
The objective of this study was to assess whether leadership gender and practice infrastructure are associated with the prevalence of bullying, gender discrimination, and microaggressions among surgeons who are women.
Methods
A sample of women gynecologic oncologists was recruited from the Facebook group, the “Women of Gynecologic Oncology” (WGO), an online Facebook community established August 18, 2017. At the time of the study, there were 472 members of this group of an estimated 1126 gynecologic oncologists in the United States (77.6% of the women workforce in gynecologic oncology) (6). The group is active with 453 members who signed on the month of the survey with 98 new posts, 972 comments, and 1,956 reactions from members during this time period. A link to an anonymous, secure survey administered via Research Electronic Data Capture (REDCap) (11) was posted on the WGO Facebook page and remained active between 7/20/2020 and 8/19/2020. The survey was optimized for use on computers as well as mobile devices. Written informed consent was included in the survey. The study was granted exemption status by the Institutional Review Boards at Loma Linda University Health.
The survey included 69 multiple choice items with branching logic. Demographic data collected included age, race/ethnicity, marital status, parenting status, geographic location, and years in practice. Practice setting was categorized as academic, hospital employed, private practice, HMO, military or other. Respondents were asked whether they oversee trainees, the department to which they report, their leadership gender and sub-specialty and whether they have a formal assigned mentor. Satisfaction with parental leave and whether breast-feeding goals had been met were queried to assess work-life balance.
Bullying was defined within the survey for respondents as “the use of negative and aggressive interpersonal behaviors to intimidate and dominate others. Bullying behaviors often are persistent and repeated. Examples include humiliation, insults, threats, coercion, isolation, and overwork—sometimes involving repetitive or meaningless tasks. Discrimination was defined as “negatively charged, differential treatment based on one’s personal characteristics or attributes, including, but not limited to, gender, race, religion, sexual orientation, culture, ethnicity, disability, or age.” Microaggressions were evaluated using questions felt to be most relevant to a surgical practice from the validated survey the “sexist mess” (12, 13) and defined as “everyday verbal, nonverbal, and environmental slights, snubs, or insults, whether intentional or unintentional, which communicate hostile, derogatory, or negative messages to target persons”.
Data regarding bullying, harassment, and microaggression including perpetrators and effects on the respondent’s career were captured. Missing values were excluded by line. Descriptive statistics were compiled. Univariate analysis was performed using χ2 tests. A multivariate logistic regression model was created to study the association of partner occupation with the respondents’ desire to switch to a less demanding career or specialty while controlling for potential confounders. Variables were chosen based on contextual plausibility and statistical significance on initial univariate analysis. All p values were from 2-sided tests, and results were deemed statistically significant at p ≤ .05. All analyses were performed using JMP®, Version 15. SAS Institute Inc., Cary, NC, 1989-2019.
Results
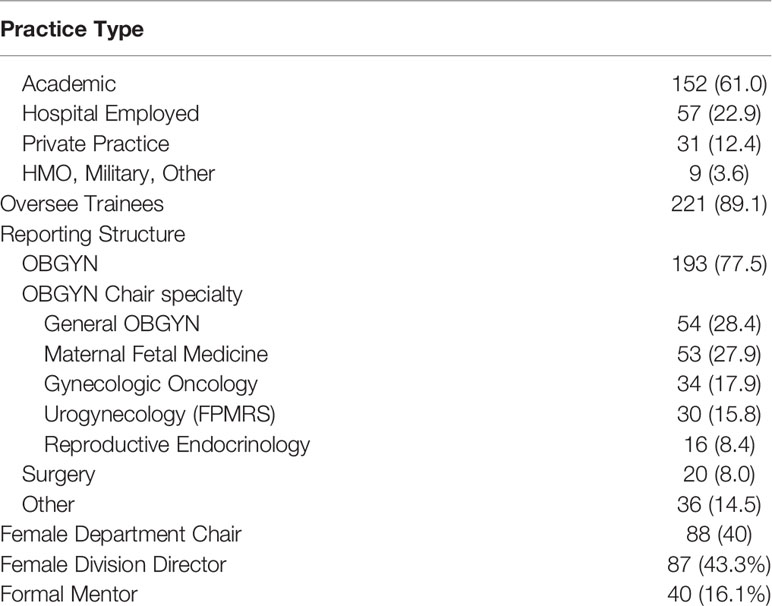
Four hundred and fifty three of 472 WGO members logged onto the Facebook group while the survey was active. Of these members 250 (55%) submitted survey responses. Demographics of those respondents are detailed in Table 1. Most respondents were younger than age 50 years (93.6%), white (82.2%) and non-Hispanic (94.3%). A majority were married (84.7%) and had children (75.2%). Practice environments are described in Table 2 and included academic (n=152, 61.0%), private practice (n=31, 12.4%), and hospital employed (n=57, 22.9%), and 89.9% supervised trainees. Most respondents reported within a department of obstetrics and gynecology (77.5%) to male division directors (56.7%) and male department chairs (60%). Only 16.1% of respondents had a formal, assigned mentor.
The experience of bullying was endorsed by 131 of 248 (52.8%) of respondents, 100 (76.3%) in training and 81 (61.8%) in practice. Gender discrimination was endorsed by 142 of 249 respondents, 112 (78.9%) in training and 92 (64%) in practice. Two hundred and eight (83.5%) respondents endorsed being the target of any microaggression. Experiences included the following: (1) hiding personal life or changed personality to adapt to a work environment (56.6%); (2) pretending to be interested in an activity to feel included in a conversation (41.9%); (3) being told to smile more (30.9%); (4) being told at work to dress a certain way (19.7%); and being told to act more female, nurturing and/or motherly (16.1%). No demographic or practice characteristics, including having an assigned mentor were statistically associated with experiences of bullying, discrimination, and microaggressions.
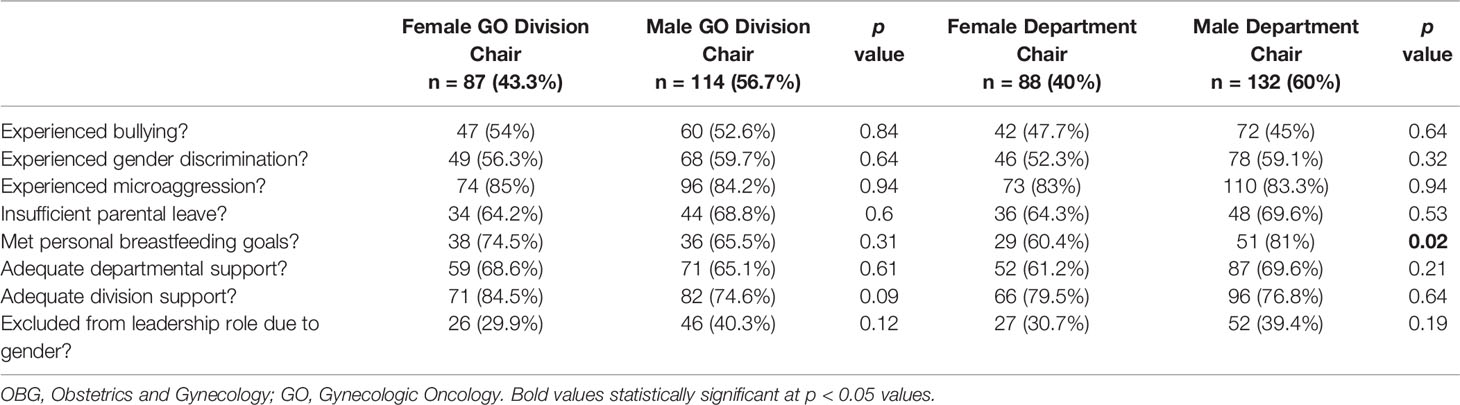
Division director gender, specialty or department reporting structure were not statistically significantly associated with the experience of bullying, gender discrimination or microaggressions (Table 3). Compared to respondents with a male chair, those with a female chair experienced similar rates of bullying (55.0 vs 47.7%, p=0.33); gender discrimination (59.1 vs 52.3%, p=0.33); and microaggressions (83.3 vs 83.0%, p=1.00). Women with male department chairs were more likely to meet breast-feeding goals (81 vs 60.4%, p-0.02). No other significant associations were identified between chair gender and perceived work environment for respondents.
Formal institutional reporting of bullying and discrimination was uncommon (24.4 and 19% respectively). When reported, bullying and discrimination was most commonly reported to a chief or chair (78.1 and 77.8%, respectively) and human resources (18.8% and 29.6%, respectively). The frequency of reporting was not associated with practice environment. Respondents who worked for a woman department chair were more likely to report experiences of bullying (33.3% vs 16.7%, p= 0.04) but not discrimination.
Multiple and varied perpetrators of bullying, gender discrimination and microaggression were reported (Figure 1). Individuals instigating these behaviors were identified as colleagues with authority (84%), patients (44%), staff (41%), administrators (18%), and trainees (16%). Perpetrators of bullying and discrimination were more commonly male, but significant numbers of respondents reported female instigators and/or an equal amount of bullying and discrimination from men and women.
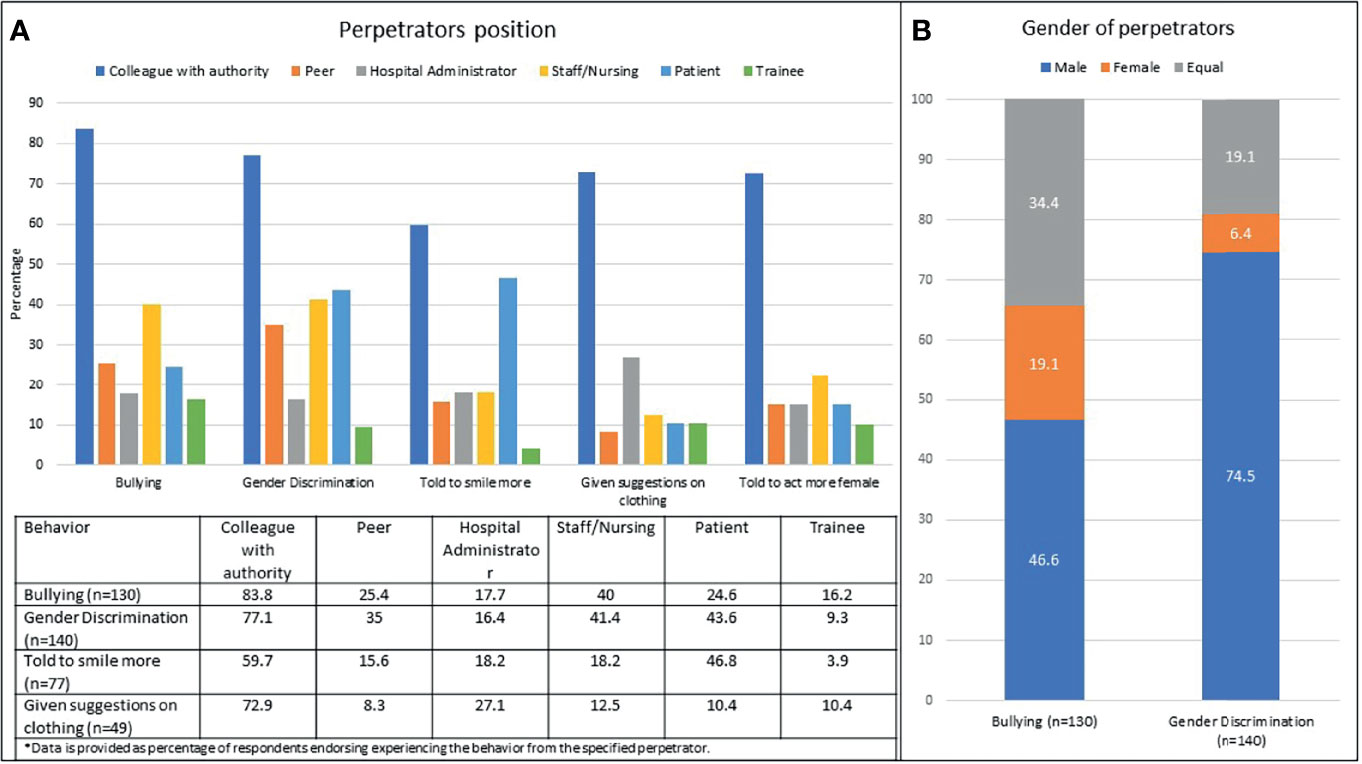
Figure 1 Perpetrators of bullying and discrimination were multiple and varied. (A) Positions of the perpetrators; (B) Gender of the perpetrators.
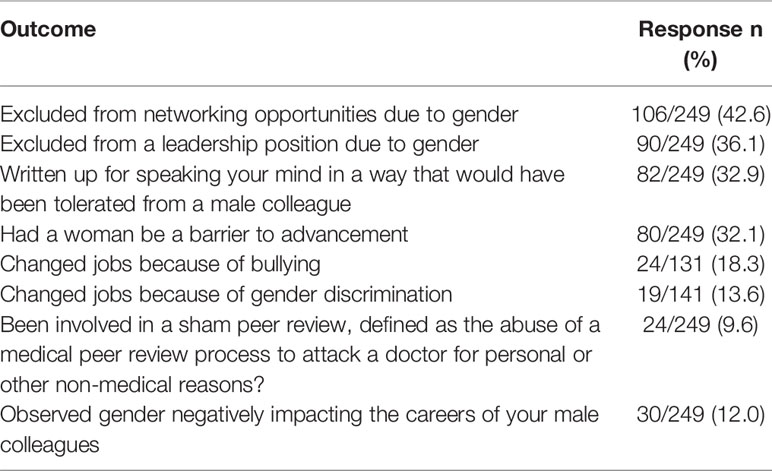
Survey respondents endorsed that gender had impacted their careers and advancement (Table 4). Bullying and gender discrimination led to job changes for 18.3 and 13.6%, respectively, of participants. Nearly half of respondents endorsed exclusion from networking opportunities and over a third reported exclusion from leadership that was perceived to be related to gender. A woman in a leadership role was perceived as having been a barrier to advancement for 32.1% of respondents. Being written up for speaking one’s mind that was perceived to have been tolerated from male colleagues was common. Ten percent of respondents had been the subject of a sham peer review (defined as the abuse of a medical peer review process to attack a doctor for personal or other non-medical reasons). Few respondents (12%) felt that gender negatively impacts their male colleagues.
Discussion
The findings of the current study confirm that gender-based discrimination remains a common experience for gynecologic oncologists who are women; that reporting of these experiences is uncommon; and provides evidence that this environment negatively impacts the career trajectories of women, leading to lost opportunities and job changes. By capturing perceived bullying and microaggressions, this study demonstrates the pervasiveness of hostility related to gender for women, despite the large numbers of women practicing within this surgical specialty. A previous, recent survey of gynecologic oncologists demonstrated that 71% of women and 51% of men reported experiencing sexual harassment in training or in practice. Few targets (14.5%) reported their experience. Female respondents were more likely to have had the experience impact their career advancement or compensation (10). Prior reports have linked experiences of gender discrimination and sexual harassment to increased reports of burnout, job changes and career dissatisfaction (9, 10, 14–17).
“Critical mass” theory of the 1970’s proposed that once women represented a third of a professional group, the culture of the group would shift such that they would no longer be perceived as a minority or subordinate (18). However, increasing proportions of women in a surgical work environment does not necessarily correlate to decreased prevalence of gender discrimination or sexual harassment. In a survey of general surgery training programs, increasing proportions of female residents was correlated with program-level rates of gender discrimination (r=0.64; 95% CI, 0.56-0,70) and sexual harassment (r=0.17; 95% CI, 0.06-0.28) (19). In gynecologic oncology experiences of bullying and discrimination persists despite large numbers of women – most recently in the “2020 Society of Gynecologic Oncology State of the Specialty” report, 54% of gynecologic oncologists self-identified as female (6), at rates remarkably similar to those reported in surgical specialties that remain predominated by men. A survey of the members of the American College of Surgeons and Association of Women Surgeons, found that 58% of women and 25% of men experienced sexual harassment in the preceding 12 months (20). In a survey of 927 practicing orthopedic surgeons 81% of women reported having experienced harassment, discrimination or bullying (21).
The professional roles and genders of the perpetrators of bullying and harassment reported in this study were multiple and varied. Significant numbers of respondents identified peers, staff/nursing, administrators, patients and trainees as the source of unprofessional behaviors. Nurses were the most commonly identified perpetrators of harassment in a recent survey of 270 general surgery trainees in which 48% percent of female and 22% of male respondents reported being harassed by nursing staff (22). Another recent survey of trainees identified the most common sources of discrimination as patients and nurses and that events occurred more often in the emergency and operating rooms (23). A qualitative study of 30 women surgeons described frequent workplace conflict with a non-physician and those interactions frequently resulting in formal reporting of the surgeon. Common impact themes, including personal (emotional and physical), professional, and patient safety were identified (24).
Promoting more women into leadership has often been proposed as a means with to reduce gender inequities in medicine and surgery (7, 25, 26). Yet despite large numbers of women in divisions and departments led by women, our study did not find an association between leadership gender and the experiences of bullying, gender discrimination or microaggressions. The only significant associations with women whose department chairs were men were more likely to reach breast feeding goals, while women were more likely to report bullying when working for a female department chair. These findings support the concept that organizational and institutional acknowledgement, accountability and education for leaders is necessary in order for culture change to be successful in traditionally hierarchical academic medical centers (27).
Our study confirmed that reporting of bullying and discrimination is uncommon among targets of sexual harassment (1, 10, 15, 22). Organizational prioritization of reporting and investigating harassment is necessary to create the transparency required to address the culture that allows bullying, harassment and microaggressions. In 2017 an anonymous reporting system was developed and implemented at the Mayo Clinic demonstrating the feasibility of institutional accountability. All allegations of sexual harassment are duly investigated by an HR representative in conjunction with the legal department. Over the first 2 years, 153 allegations were made and 88 (57.5%) substantiated. Of these, 71 (80.7%) included inappropriate comments and/or unwelcome sexual advances, 22 (25%) unwanted touch or physical contact, and 16 (18.2%) virtual or electronic harassment (e.g., email, messenger, text). Investigations resulted in 31 employees receiving formal coaching, 22 receiving written warnings, and 35 terminations or resignations (28). An improved culture has not yet been documented; however, the perception of fairness and justice are important foundations for eliminating cultures that allow harassment (1, 29, 30).
The negative effects of bullying and harassment in the workplace extend to surgeons of any gender. Observing discriminatory behavior is detrimental to the well-being of those exposed (15, 17, 31). Engaging bystanders may also be a key component to changing the culture of surgery as bystanders interventions are an effective evidence-based tool that can be used to combat discrimination (32, 33).
This study was designed to provide information about the effect of gender on work environment among women who are surgeons in a specialty with a majority women workforce. As such the prevalence and impact of bullying, discrimination and microaggressions among men were not captured. The results presented in this manuscript are limited by the biases inherent in a survey design and the convenience sample used to obtain responses. Gender bias in medicine is often insidious (34, 35) and our results may reflect recall bias. Gynecologic oncologists who experience a negative work environment may be more likely to actively participate in a social media support group. Our results may have undercounted the experiences of bullying and harassment across a woman’s career as our survey respondents were primarily young, therefor may not yet have experienced the accumulation of events reported by midcareer and senior surgeons who are women (36). Similarly, most participants were White, and may not have experienced the amplified experiences bullying and harassment reported by physicians from historically underrepresented in medicine communities who are also women (21, 37, 38). In addition, we were unable to assess the leadership gender within the broader context of the organization which may have contributed to our findings. The strengths of this study, however, include the large proportion of gynecologic oncologists who are women who participate actively in this social media group, the WGO and the high response rate (over half of active participants).
An urgent need to correct gender-based hostility within the surgical work environments exists. Inclusion of women into a specialty and into leadership positions is insufficient to create belong within surgical workplaces. Department and institutional leaders and mentors need to actively help women navigate unprofessional behavior, gender bias, and exclusion at work. Although gynecology was the first surgical specialty to attract a majority women workforce, increasing numbers of women are entering all surgical specialties (1, 39). With an increasing number of women in the surgical workforce, attention to creating spaces where all surgeons can thrive should be prioritized by all healthcare systems. Further studies are needed to address how the systemic change can occur and be standardized in institutions.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Loma Linda University Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
LH, ST, MB, and LR contributed to conception and design of the study. LH, DT, MB, and ST designed the survey. LR organized the database. LR performed the statistical analysis. ST wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
William P. McGuire, MD is acknowledged for support and proof reading.
References
1. Stephens EH, Heisler CA, Temkin SM, Miller P. The Current Status of Women in Surgery: How to Affect the Future. JAMA Surg (2020) 155:876–85. doi: 10.1001/jamasurg.2020.0312
2. Peel JK, Schlachta CM, Alkhamesi NA. A Systematic Review of the Factors Affecting Choice of Surgery as a Career. Can J Surg (2018) 61:58–67. doi: 10.1503/cjs.008217
3. Rayburn WF. The Obstetrician-Gynecologist Workforce in the United States. Washington DC: American Congress of Obstetricians and Gynecologists (2017).
4. Heisler CA, Mark K, Ton J, Miller P, Temkin SM. Has a Critical Mass of Women Resulted in Gender Equity in Gynecologic Surgery? Am J Obstet Gynecol (2020) 223(5):665–73. doi: 10.1016/j.ajog.2020.06.038
7. Temkin SM, Rubinsak L, Benoit MF, Hong L, Chandavarkar U, Heisler CA, et al. Take Me to Your Leader: Reporting Structures and Equity in Academic Gynecologic Oncology. Gynecol Oncol (2020) 157(3):759–64. doi: 10.1016/j.ygyno.2020.03.031
8. Jena AB, Olenski AR, Blumenthal DM. Sex Differences in Physician Salary in US Public Medical Schools. JAMA Intern Med (2016) 176:1294–304. doi: 10.1001/jamainternmed.2016.3284
9. Brown J, Drury L, Raub K, Levy B, Brantner P, Krivak TC, et al. Workplace Harassment and Discrimination in Gynecology: Results of the AAGL Member Survey. J Minimally Invasive Gynecol (2019) 26(5):838–46. doi: 10.1016/j.ygyno.2019.04.031
10. Stasenko M, Tarney CM, Veith M, Seier K, Casablanca Y, Brown CL. Survey of Sexual Harassment and Gender Disparities Among Gynecologic Oncologists. Am Soc Clin Oncol (2019) 159(2):317–21. doi: 10.1200/JCO.2019.37.18_suppl.LBA10502
11. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap)–a Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J Biomed Inf (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
12. Barnes KL, Dunivan G, Sussman AL, McGuire L, McKee R. Behind the Mask: An Exploratory Assessment of Female Surgeons’ Experiences of Gender Bias. Acad Med (2020) 95:1529–38. doi: 10.1097/ACM.0000000000003569
13. Derthick AO. The Sexist Mess: Development and Initial Validation of the Sexist Microaggressions Experiences and Stress Scale and the Relationship of Sexist Microaggressions to Women’s Mental Health. Ann Arbor, MI: University of Alaska Anchorage (2015).
14. Nunez-Smith M, Pilgrim N, Wynia M, Desai MM, Bright C, Krumholz HM, et al. Health Care Workplace Discrimination and Physician Turnover. J Natl Med Assoc (2009) 101:1274–82. doi: 10.1016/S0027-9684(15)31139-1
15. National Academies of Sciences E, Medicine. Sexual Harassment of Women: Climate, Culture, and Consequences in Academic Sciences, Engineering, and Medicine. Washington: National Academies Press (2018).
16. Mathews E, Hammarlund R, Kullar R, Mulligan L, Le T, Lauve S, et al. Sexual Harassment in the House of Medicine and Correlations to Burnout: A Cross-Sectional Survey. Ochsner J (2019) 19:329–39. doi: 10.31486/toj.19.0019
17. Vargas EA, Brassel ST, Cortina LM, Settles IH, Johnson TR, Jagsi R. # MedToo: A Large-Scale Examination of the Incidence and Impact of Sexual Harassment of Physicians and Other Faculty at an Academic Medical Center. J Women’s Health (2019) 29(1):13–20. doi: 10.1089/jwh.2019.7766
18. Derthick AO. The Sexist Mess: Development and Initial Validation of the Sexist Microaggressions Experiences and Stress Scale and the Relationship of Sexist Microaggressions to Women’s Mental Health. [PhD diss.]. University of Alaska Anchorage (2015).
19. Schlick CJR, Ellis RJ, Etkin CD, Greenberg CC, Greenberg JA, Turner PL, et al. Experiences of Gender Discrimination and Sexual Harassment Among Residents in General Surgery Programs Across the US. JAMA Surg (2021) 156(10):942–52. doi: 10.1001/jamasurg.2021.3195
20. Nayyar A, Scarlet S, Strassle P, Ollila D, Erdahl L, McGuire K, et al. A National Survey of Sexual Harassment Among Surgeons. In: 14th Annual Academic Surgical Congress. Houston, Texas (2019).
21. Samora JB, Van Heest A, Weber K, Ross W, Huff T, Carter C. Harassment, Discrimination, and Bullying in Orthopaedics: A Work Environment and Culture Survey. JAAOS-J Am Acad Orthopaedic Surgeons (2020) 28:e1097–104. doi: 10.5435/JAAOS-D-19-00822
22. Freedman-Weiss MR, Chiu AS, Heller DR, Cutler AS, Longo WE, Ahuja N, et al. Understanding the Barriers to Reporting Sexual Harassment in Surgical Training. Ann Surg (2020) 271:608–13. doi: 10.1097/SLA.0000000000003295
23. Brown A, Bonneville G, Glaze S. Nevertheless, They Persisted: How Women Experience Gender-Based Discrimination During Postgraduate Surgical Training. J Surg Educ (2020) 78(1):17–34. doi: 10.1016/j.jsurg.2020.06.027
24. Dossett LA, Vitous CA, Lindquist K, Jagsi R, Telem DA. Women Surgeons’ Experiences of Interprofessional Workplace Conflict. JAMA Netw Open (2020) 3:e2019843–e. doi: 10.1001/jamanetworkopen.2020.19843
25. Pories SE, Turner PL, Greenberg CC, Babu MA, Parangi S. Leadership in American Surgery: Women Are Rising to the Top. Ann Surg (2019) 269(2):199–205. doi: 10.1097/SLA.0000000000002978
26. Carnes M, Morrissey C, Geller SE. Women’s Health and Women’s Leadership in Academic Medicine: Hitting the Same Glass Ceiling? J Women’s Health (2008) 17:1453–62. doi: 10.1089/jwh.2007.0688
27. Helitzer DL, Newbill SL, Cardinali G, Morahan PS, Chang S, Magrane D. Changing the Culture of Academic Medicine: Critical Mass or Critical Actors? J Women’s Health (2017) 26:540–8. doi: 10.1089/jwh.2016.6019
28. Rihal CS, Baker NA, Bunkers BE, Buskirk SJ, Caviness JN, Collins EA, et al. Addressing Sexual Harassment in the #MeToo Era: An Institutional Approach. In: Mayo Clinic Proceedings. Elsevier (2020). p. 749–57. doi: 10.1016/j.mayocp.2019.12.021
29. ACS. 2018 ACS Governors Survey: Gender Inequality and Harassment Remain a Challenge in Surgery. Bulletin of the American College of Surgeons (2019).
30. Fairchild AL, Holyfield LJ, Byington CL. National Academies of Sciences, Engineering, and Medicine Report on Sexual Harassment: Making the Case for Fundamental Institutional Change. Jama (2018) 320:873–4. doi: 10.1001/jama.2018.10840
31. Miner-Rubino K, Cortina LM. Beyond Targets: Consequences of Vicarious Exposure to Misogyny at Work. J Appl Psychol (2007) 92:1254. doi: 10.1037/0021-9010.92.5.1254
32. Aggarwal R, Brenner AM. #MeToo: The Role and Power of Bystanders (Aka Us) Vol. 44. Academic Psychiatry (2020) p. 5–10. doi: 10.1007/s40596-019-01173-0
33. Mello MM, Jagsi R. Standing Up Against Gender Bias and Harassment-A Matter of Professional Ethics. New Engl J Med (2020) 382:1385. doi: 10.1056/NEJMp1915351
34. Torres MB, Salles A, Cochran A. Recognizing and Reacting to Microaggressions in Medicine and Surgery. JAMA Surg (2019) 154(9):868–72. doi: 10.1001/jamasurg.2019.1648
35. Files JA, Mayer AP, Ko MG, Friedrich P, Jenkins M, Bryan MJ, et al. Speaker Introductions at Internal Medicine Grand Rounds: Forms of Address Reveal Gender Bias. J Women’s Health (2017) 26:413–9. doi: 10.1089/jwh.2016.6044
36. Lewiss RE, Silver JK, Bernstein CA, Mills AM, Overholser B, Spector ND. Is Academic Medicine Making Mid-Career Women Physicians Invisible? J Women’s Health (2019) 29(2):187–92. doi: 10.1089/jwh.2019.7732
37. Cropsey KL, Masho SW, Shiang R, Sikka V, Kornstein SG, Hampton CL. Why Do Faculty Leave? Reasons for Attrition of Women and Minority Faculty From a Medical School: Four-Year Results. J Women’s Health (2008) 17:1111–8. doi: 10.1089/jwh.2007.0582
38. Westring AF, Sammel MD, Speck RM, Tuton LW, Grisso JA, Abbuhl SB. Career Trajectories of Women From Underrepresented Minority Groups at an Academic Medical Center. JAMA Netw Open (2021) 4:e212723. doi: 10.1001/jamanetworkopen.2021.2723
Keywords: gender discrimination, women in medicine (WIM), women in surgery, gynecologic oncologists, inclusion, microaggressions, bullying
Citation: Hong LJ, Rubinsak L, Benoit MF, Teoh D, Chandavarkar U, Brockmeyer A, Stevens E, Ioffe Y and Temkin SM (2022) Gynecologic Oncology and Inclusion of Women Into the Surgical Workforce: The Canary in This Coal Mine. Front. Oncol. 12:789910. doi: 10.3389/fonc.2022.789910
Received: 06 October 2021; Accepted: 07 March 2022;
Published: 06 April 2022.
Edited by:
Maria Irene Bellini, Sapienza University of Rome, ItalyReviewed by:
Marilyn Huang, University of Miami Health System, United StatesDeborah Verran, Consultant, Sydney, NSW, Australia
Copyright © 2022 Hong, Rubinsak, Benoit, Teoh, Chandavarkar, Brockmeyer, Stevens, Ioffe and Temkin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Linda J. Hong, bGluZGFoaG9uZ0BnbWFpbC5jb20=
 Linda J. Hong
Linda J. Hong Lisa Rubinsak
Lisa Rubinsak Michelle F. Benoit3
Michelle F. Benoit3 Deanna Teoh
Deanna Teoh Uma Chandavarkar
Uma Chandavarkar Erin Stevens
Erin Stevens Yevgeniya Ioffe
Yevgeniya Ioffe Sarah M. Temkin
Sarah M. Temkin