- 1Department of Breast Surgery, Second Hospital of Dalian Medical University, Dalian, China
- 2Department of Obstetrics and Gynecology, Second Hospital of Dalian Medical University, Dalian, China
- 3Department of Breast Surgery, Cancer Hospital of China Medical University, Liaoning Cancer Hospital and Institute, Shenyang, China
- 4Department of Operation Room, Second Hospital of Dalian Medical University, Dalian, China
- 5Department of Neurology, Boao Yiling Life Care Center, Boao, China
- 6Department of Breast Surgery, Affiliated Zhongshan Hospital of Dalian University, Dalian, China
D-dimer level is often used to assess the severity of trauma as well as the risk of thrombosis. This study investigated the risk factors for high postoperative D-dimer level. This study included a total of 2706 patients undergoing breast cancer surgery to examine the associations between various clinicopathological factors and variation in D-dimer levels. After adjusting for other factors, T stage, neoadjuvant chemotherapy, blood loss, surgery type, diabetes, and elevated leukocyte and neutrophil counts were found to be significant risk factors for D-dimer variation. This study identified several factors associated with elevated D-dimer levels and consequent thrombosis after breast cancer surgery, which may aid in the development of more precise preventive measures and interventions as well as serve as a reference for future research.
Introduction
Breast cancer has recently become the most common malignancy worldwide and is also the leading type of cancer in China. With advances in treatment techniques, relatively good therapeutic effects are generally achieved in the treatment of breast cancer (1, 2). Therefore, good survival rates and quality of life are expected in early-stage patients (3, 4). There are relatively few severe complications in the perioperative period of breast cancer surgery, with the most severe being venous thrombosis of the lower extremities and the consequent pulmonary embolism, which often lead to serious damage to health or death of patients and a heavy financial burden (5). In general, a smaller scope of surgery can effectively reduce the occurrence of complications and is indicative of better postoperative breast appearance (6–8). Therefore, breast-conserving surgery has become an increasingly popular approach among patients who meet the relevant indications. The reduced degree of injury provides several benefits, including fewer surgical complications, faster recovery, and increased long-term survival (9–11). However, these methods pose new challenges for the postoperative care of patients with breast cancer. Thus, a comprehensive analysis of the clinicopathological features and surgical approach of patients is required to assess the degree of trauma and risk of thrombosis.
To maintain normal physiological status, the coagulation system is activated to prevent blood loss in the event of vascular injury. Despite its lack of specificity, an elevated D-dimer level serves as a relatively sensitive biomarker for thrombosis in the circulatory system. Therefore, D-dimer level is often utilized in clinical practice to aid in the diagnosis of venous thromboembolism, deep vein thrombosis, and pulmonary embolism. D-dimer level has also been shown to correlate directly with the degree of trauma, making it an appropriate indicator for assessing injury severity (12, 13). Therefore, when we use D-dimer level as an index to measure the risk of thrombosis, we should realize the limitations of D-dimer as a negative predictive factor for adverse events and pay attention to excluding other influencing factors, such as trauma scope, age, preoperative treatment, disease stage, etc., and analyze the independent risk of different factors under the coexistence of multiple factors. At the same time, in the era of epidemic, the treatment of tumor also has some new challenges. Have patients with COVID-19 affected the coagulation of blood because of pathological changes in the lungs? (14) Whether or not you have ever suffered from COVID-19, will the vaccination affect the hemagglutination state? (15) For tumor patients, their own diseases may bring blood hypercoagulability. At the same time, tumor patients also have the characteristics of relatively old age. In these patients, how to measure the relationship between coagulation indexes and thrombosis risk is also a subject that needs special analysis (16, 17). In order to more accurately understand the potential risk of thrombosis in patients, we should also continuously refine the monitoring process of D-dimer, find the most accurate time point for blood sampling and testing, and develop more biomarkers for modeling and prediction, so as to avoid the influence of multiple confounding factors caused by simple D-dimer (18–21). In a word, under the situation of epidemic situation, aging population and increasing tumor incidence rate, how to give consideration to the treatment effect of tumor and the quality of life of patients, and maximize the net benefit of patients is a subject that needs to be continuously studied. In this context, the present study investigated the role of D-dimer level in thrombosis and injury before and after surgery for the treatment of breast cancer. We aimed to explore independent risk factors for elevated postoperative D-dimer level and the influencing factors of the degree of trauma and risk of thrombosis to provide a basis for the identification of patients who require close monitoring.
Methods
Patients
This study enrolled 2706 patients who underwent breast cancer surgery from 2013-2020, including total mastectomy (glandectomy), and breast-conserving surgery, at the Second Hospital of Dalian Medical University, and the Affiliated Zhongshan Hospital of Dalian University. The inclusion criteria were: 1. The patient was diagnosed with breast cancer and underwent breast cancer surgery, and the time from the last general anesthesia operation was more than one year; 2. Received or not neoadjuvant therapy before operation; 3. 18-75 years old; 4. No distant metastasis; 5. Complete clinicopathological information, especially the test results of D-dimer before and after operation. The exclusion criteria were: 1. Received general anesthesia within one year; 2. The patient was younger than 18 years old or older than 75 years old; 3. There were distant metastatic lesions before operation; 4. The clinicopathological information is incomplete. The clinical, surgical, and pathological findings and all medical data, including age, tumor stage, nodal stage, neoadjuvant chemotherapy, operative time, blood loss, surgery, preoperative and postoperative complications were collected prospectively and recorded in a database.
This study was approved by the Ethics Committee of Second Hospital of Dalian Medical University. All methods were performed in accordance with the relevant guidelines and regulations. Informed consent was obtained from all participants.
Blood Sampling
Blood samples for the determination of pre- and postoperative D-dimer levels were acquired together with the samples used for other hematological tests. Preoperative sampling was usually performed on the second day after admission, approximately 3 days before surgery. Before surgery, in addition to D-dimer, we will detect the patient’s blood routine, liver function, renal function, coagulation, blood glucose, blood lipid, blood ions, etc. Postoperative sampling was usually performed 1 day after surgery. After the operation, we will detect the blood routine, blood ions, four items of coagulation, D-dimer, etc.
Statistical Analyses
Chi-square tests were used to analyze the differences between groups of various D-dimer levels. Correlation analyses were used to identify the influencing factors of D-dimer levels. Multivariate analyses using the ENTER method were conducted to assess the risk factors for increased D-dimer levels. All analyses were performed using IBM SPSS Statistics for Windows, version 23.0. Two-sided P-values <0.05 were considered statistically significant.
Results
Patient Characteristics
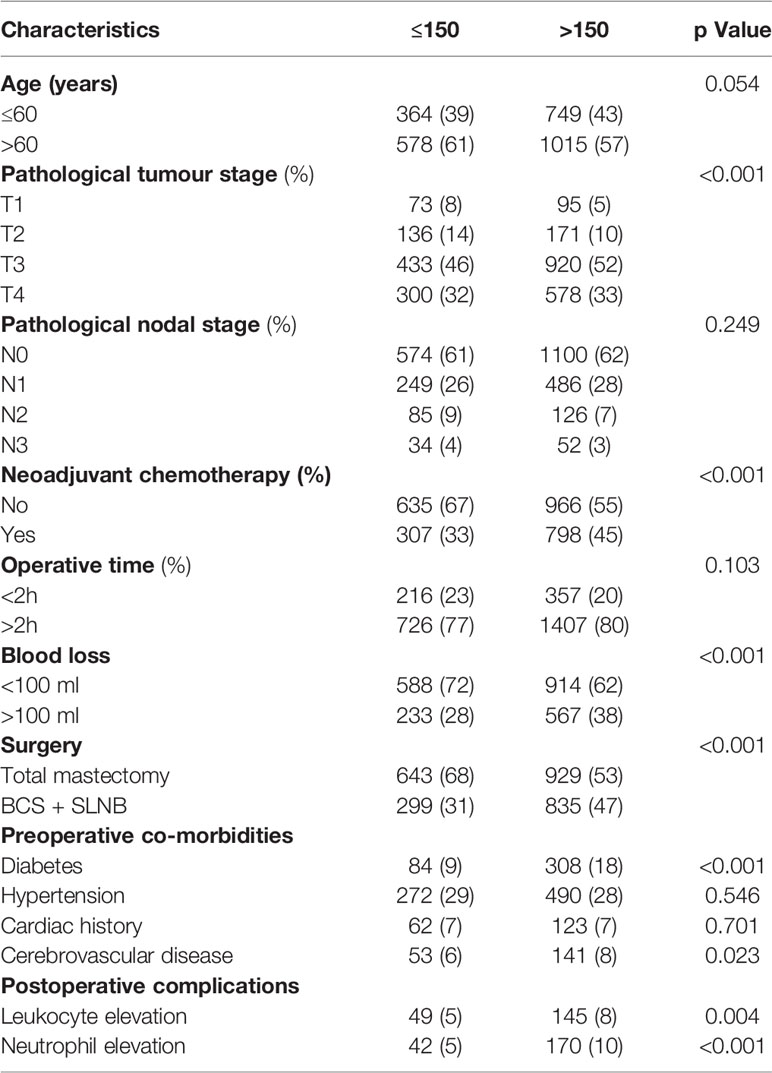
A total of 13 clinicopathological factors were identified and included in the analysis. The distribution of various clinicopathological factors was subsequently compared between the two groups (pre- and postoperative D-dimer levels). Of these, T stage, neoadjuvant chemotherapy, blood loss, surgery, diabetes, and leukocyte and neutrophil elevation differed significantly between the two D-dimer groups (Table 1). The factors with significantly different distributions between the two groups were identified as possible risk factors for D-dimer variation.
Correlation Analysis
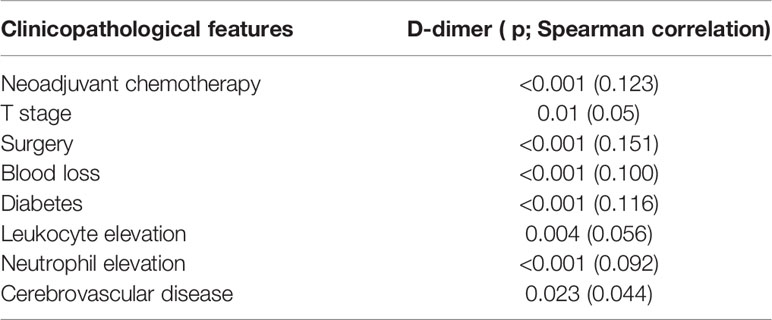
Spearman correlation analysis showed linear correlations between D-dimer difference and neoadjuvant chemotherapy, T stage, surgery, blood loss, diabetes, leukocyte and neutrophil elevation, and cerebrovascular disease (Table 2).
Risk Factor Analysis
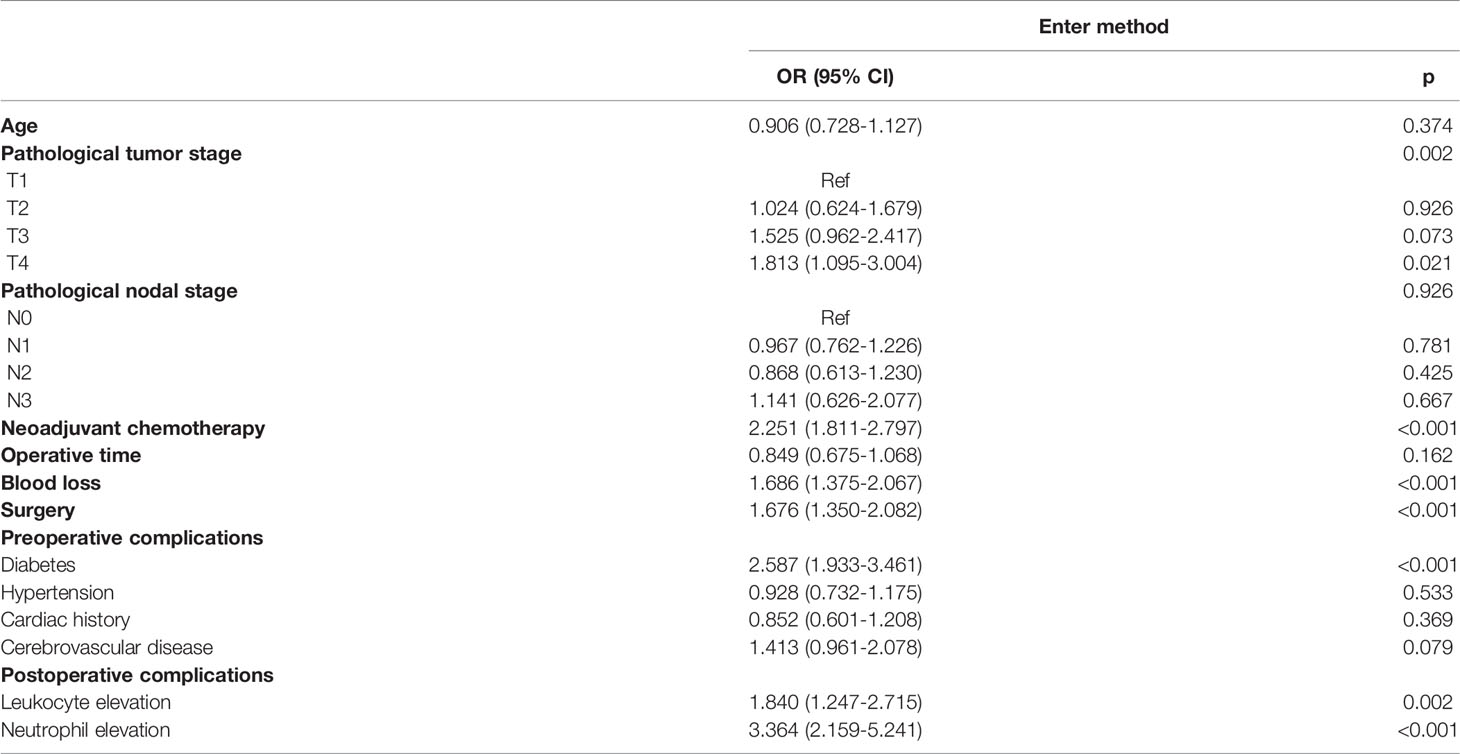
The associations between the possible risk factors and elevated D-dimer level is shown in Table 3. After adjusting for the 13 variables, T stage, neoadjuvant chemotherapy, blood loss, surgery type, diabetes, and leukocyte and neutrophil elevation were identified as significant risk factors.
Discussion
In recent years, increasing attention has been paid to the concept of fast-track surgery, which aims to provide postoperative patients with a variety of integrated treatment approaches to achieve rapid recovery. This leads to the reduction of psychological and organic traumatic stress reactions, which ultimately reduces postoperative complications, shortens the average length of hospital stay, decreases the risk of death, and reduces health care costs (22). However, fast-track surgery is not yet optimized and remains under development. Modifications are also required for specific treatment measures to enhance their suitability for the Chinese population. Therefore, clinicopathological data, surgical information, postoperative complication data, and the prognostic and follow-up information of patients requiring surgery must be collected continuously to perform statistical analysis to aid the development of more reliable and effective diagnostic and treatment modalities for the Chinese population (23, 24).
The present study identified T stage, neoadjuvant chemotherapy, blood loss, surgery type, diabetes, and leukocyte and neutrophil elevation as risk factors for significantly increased D-dimer level.
Our results differ from those of previous studies in that age was not an independent risk factor. Although this is contradictory to the conventional belief that older age is associated with a higher risk of concomitant thrombosis, it suggests that younger patients should also be monitored closely for the occurrence of postoperative venous thrombosis (25–29).
With the increase in the proportion of patients undergoing neoadjuvant chemotherapy, there is a greater need to closely monitor D-dimer level and the possible risk of venous thrombosis (20). During surgery, efforts should also be made to minimize operative time and reduce intraoperative bleeding. For patients in whom the breast and axilla can be preserved, the scope of surgery should also be minimized. To a certain extent, D-dimer level can reflect the degree of damage to the body. Previous studies did not report surgical approach as having a significant effect on D-dimer level; however, its effects have gradually become pronounced with the increasing number of cases (30–32). This may be attributed to the presence of confounding bias among surgical approaches in previous studies, such as the prolonged operative time and intraoperative pathological waiting time for breast-conserving surgery and sentinel lymph node biopsy. Operative time was also not an independent factor due to various confounding factors.
Diabetes mellitus is a known risk factor for thrombosis (33, 34). In particular, the physiological changes following general anesthesia often result in high blood glucose levels, which increase the risk of thrombosis when combined with prolonged bed rest. Thus, careful patient monitoring is required.
Postoperative infection, especially cellular infection that results in elevated neutrophil count, is a risk factor for thrombosis (35–37). It may also exacerbate injury and lead to elevated D-dimer levels. Although the degree of D-dimer elevation does not necessarily correlate with the risk of thrombosis and degree of physical injury, measures should still be adopted to prevent postoperative infections such as drain-related, wound, and urinary tract infections.
A high postoperative D-dimer level may correspond to more severe physical injury and a higher risk of postoperative thrombosis. Our findings indicated that, despite advances in diagnosis and treatment, it is still critical for researchers to collect data on basic patient information, records of previous treatment, and the prevention and treatment of perioperative complications.
Conclusions
The results of the present study revealed multiple risk factors that may cause a significant increase in D-dimer level in the postoperative period. These findings suggest the need to pay particular attention to these patients during the perioperative period, adopt adequate preventive measures, and conduct relevant research.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
This study was reviewed and approved by Second Hospital of Dalian Medical University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
LQ, YQW, YYW and XL participated in the study design and manuscript drafting. SW, HZ, and YJ participated in the study design and manuscript drafting. DC, HZ, and YJ participated in the statistical analysis and manuscript drafting. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by Dalian Medical Science Research Project (1612023).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ginsburg O, Badwe R, Boyle P, Derricks G, Dare A, Evans T, et al. Changing Global Policy to Deliver Safe, Equitable, and Affordable Care for Women's Cancers. Lancet (2017) 389(10071):871–80. doi: 10.1016/S0140-6736(16)31393-9
2. Li T, Mello-Thoms C, Brennan PC. Descriptive Epidemiology of Breast Cancer in China: Incidence, Mortality, Survival and Prevalence. Breast Cancer Res Treat (2016) 159(3):395–406. doi: 10.1007/s10549-016-3947-0
3. Nardin S, Mora E, Varughese FM, D'Avanzo F, Vachanaram AR, Rossi V, et al. Breast Cancer Survivorship, Quality of Life, and Late Toxicities. Front Oncol (2020) 10:864. doi: 10.3389/fonc.2020.00864
4. Invernizzi M, de Sire A, Lippi L, Venetis K, Sajjadi E, Gimigliano F, et al. Impact of Rehabilitation on Breast Cancer Related Fatigue: A Pilot Study. Front Oncol (2020) 10:556718. doi: 10.3389/fonc.2020.556718
5. Runowicz CD, Leach CR, Henry NL, Henry KS, Mackey HT, Cowens-Alvarado RL, et al. American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. CA Cancer J Clin (2016) 66(1):43–73. doi: 10.3322/caac.21319
6. Yan Z, Wang Q, Sun X, Ban B, Lu Z, Dang Y, et al. OSbrca: A Web Server for Breast Cancer Prognostic Biomarker Investigation With Massive Data From Tens of Cohorts. Front Oncol (2019) 9:1349. doi: 10.3389/fonc.2019.01349
7. Invernizzi M, Corti C, Lopez G, Michelotti A, Despini L, Gambini D, et al. Lymphovascular Invasion and Extranodal Tumour Extension are Risk Indicators of Breast Cancer Related Lymphoedema: An Observational Retrospective Study With Long-Term Follow-Up. BMC Cancer (2018) 18(1):935. doi: 10.1186/s12885-018-4851-2
8. Rockson SG. Lymphedema After Breast Cancer Treatment. N Engl J Med (2018) 379(20):1937–44. doi: 10.1056/NEJMcp1803290
9. Lee GK, Sheckter CC. Breast Reconstruction Following Breast Cancer Treatment-2018. JAMA (2018) 320(12):1277–8. doi: 10.1001/jama.2018.12190
10. Cutress RI, McIntosh SA, Potter S, Goyal A, Kirwan CC, Harvey J, et al. Opportunities and Priorities for Breast Surgical Research. Lancet Oncol (2018) 19(10):e521–33. doi: 10.1016/S1470-2045(18)30511-4
11. Mamtani A, Morrow M. Why Are There So Many Mastectomies in the United States? Annu Rev Med (2017) 68:229–41. doi: 10.1146/annurev-med-043015-075227
12. Dong Y, Duan G, Wang H, Ru J, Cui Y. A Cohort Study of Rivaroxaban Combined With D-Dimer Dynamic Monitoring in the Prevention of Deep Venous Thrombosis After Knee Arthroplasty. Comput Math Methods Med (2022) 2022:3965039. doi: 10.1155/2022/3965039
13. Alharbi OA, Alahmadi KO. The Diagnostic Utility of Unenhanced Computed Tomography of the Brain and D-Dimer Levels in Acute Cerebral Venous Sinus Thrombosis: A Quantitative Study. J Clin Imaging Sci (2022) 12:15. doi: 10.25259/JCIS_76_2021
14. Kazantsev AN, Karkayeva MR, Tritenko AP, Korotkikh AV, Zharova AS, Chernykh KP, et al. Carotid Enadrterectomy For Internal Carotid Thrombosis In Patients With Covid-19. Curr Probl Cardiol (2022) 13:101252. doi: 10.1016/j.cpcardiol.2022.101252
15. Brito-Dellan N, Tsoukalas N, Font C. Thrombosis, Cancer, and COVID-19. Support Care Cancer (2022) 14:1–10. doi: 10.1007/s00520-022-07098-z
16. Hayashida K, Kawabata Y, Saito K, Fujita S, Choe H, Kato I, et al. Prevalence and Risk Factors of Preoperative Venous Thromboembolism in Patients With Malignant Musculoskeletal Tumors: An Analysis Based on D-Dimer Screening and Imaging. Thromb J (2022) 20(1):22. doi: 10.1186/s12959-022-00382-2
17. Invernizzi M, Michelotti A, Noale M, Lopez G, Runza L, Giroda M, et al. Breast Cancer Systemic Treatments and Upper Limb Lymphedema: A Risk-Assessment Platform Encompassing Tumor-Specific Pathological Features Reveals the Potential Role of Trastuzumab. J Clin Med (2019) 8(2):138. doi: 10.3390/jcm8020138
18. Xu L, Ji C, Miao X, Ge J, Li F, Xu C, et al. Combination of Circulating miR-125a-5p, miR-223-3p and D-Dimer as a Novel Biomarker for Deep Vein Thrombosis. Am J Med Sci (2022) S0002-9629(22):00226-9. doi: 10.1016/j.amjms.2022.04.033
19. Zhang L, He M, Jia W, Xie W, Song Y, Wang H, et al. Analysis of High-Risk Factors for Preoperative DVT in Elderly Patients With Simple Hip Fractures and Construction of a Nomogram Prediction Model. BMC Musculoskelet Disord (2022) 23(1):441. doi: 10.1186/s12891-022-05377-8
20. Akagawa M, Kijima H, Kimura Y, Saito H, Saito K, Wakabayashi I, et al. Fibrin Monomer Complex on Postoperative Day 1 is Correlated With the Volume of Deep Vein Thrombosis After Knee Surgery. J Exp Orthop (2022) 9(1):47. doi: 10.1186/s40634-022-00482-y
21. Wang X, Jiang Z, Li Y, Gao K, Gao Y, He X, et al. Prevalence of Preoperative Deep Venous Thrombosis (DVT) Following Elderly Intertrochanteric Fractures and Development of a Risk Prediction Model. BMC Musculoskelet Disord (2022) 23(1):417. doi: 10.1186/s12891-022-05381-y
22. Ljungqvist O, Scott M, Fearon KC. Enhanced Recovery After Surgery: A Review. JAMA Surg (2017) 152(3):292–8. doi: 10.1001/jamasurg.2016.4952
23. Kim L, McGee L, Tomczyk S, Beall B. Biological and Epidemiological Features of Antibiotic-Resistant Streptococcus Pneumoniae in Pre- and Post-Conjugate Vaccine Eras: A United States Perspective. Clin Microbiol Rev (2016) 29(3):525–52. doi: 10.1128/CMR.00058-15
24. Wainwright TW, Immins T, Middleton RG. Enhanced Recovery After Surgery (ERAS) and its Applicability for Major Spine Surgery. Best Pract Res Clin Anaesthesiol (2016) 30(1):91–102. doi: 10.1016/j.bpa.2015.11.001
25. Johnson ED, Schell JC, Rodgers GM. The D-Dimer Assay. Am J Hematol (2019) 94(7):833–9. doi: 10.1002/ajh.25482
26. Linkins LA, Takach Lapner S. Review of D-Dimer Testing: Good, Bad, and Ugly. Int J Lab Hematol (2017) 39 Suppl 1:98–103. doi: 10.1111/ijlh.12665
27. Olaf M, Cooney R. Deep Venous Thrombosis. Emerg Med Clin North Am (2017) 35(4):743–70. doi: 10.1016/j.emc.2017.06.003
28. Hayakawa M, Maekawa K, Kushimoto S, Kato H, Sasaki J, Ogura H, et al. High D-Dimer Levels Predict a Poor Outcome in Patients With Severe Trauma, Even With High Fibrinogen Levels on Arrival: A Multicenter Retrospective Study. Shock (2016) 45(3):308–14. doi: 10.1097/SHK.0000000000000542
29. Yumoto T, Naito H, Yamakawa Y, Iida A, Tsukahara K, Nakao A. Venous Thromboembolism in Major Trauma Patients: A Single-Center Retrospective Cohort Study of the Epidemiology and Utility of D-Dimer for Screening. Acute Med Surg (2017) 4:394–400. doi: 10.1002/ams2.290
30. Lin Y, Liu Z, Qiu Y, Zhang J, Wu H, Liang R, et al. Clinical Significance of Plasma D-Dimer and Fibrinogen in Digestive Cancer: A Systematic Review and Meta-Analysis. Eur J Surg Oncol (2018) 44(10):1494–503. doi: 10.1016/j.ejso.2018.07.052
31. Greenberg CS. The Role of D-Dimer Testing in Clinical Hematology and Oncology. Clin Adv Hematol Oncol (2017) 15(8):580–3.
32. Favresse J, Lippi G, Roy PM, Chatelain B, Jacqmin H, Ten Cate H, et al. D-Dimer: Preanalytical, Analytical, Postanalytical Variables, and Clinical Applications. Crit Rev Clin Lab Sci (2018) 55(8):548–77. doi: 10.1080/10408363.2018.1529734
33. Westein E, Hoefer T, Calkin AC. Thrombosis in Diabetes: A Shear Flow Effect? Clin Sci (Lond) (2017) 131(12):1245–60. doi: 10.1042/CS20160391
34. Pechlivani N, Ajjan RA. Thrombosis and Vascular Inflammation in Diabetes: Mechanisms and Potential Therapeutic Targets. Front Cardiovasc Med (2018) 5:1. doi: 10.3389/fcvm.2018.00001
35. Kapoor S, Opneja A, Nayak L. The Role of Neutrophils in Thrombosis. Thromb Res (2018) 170:87–96. doi: 10.1016/j.thromres.2018.08.005
36. Hisada Y, Mackman N. Cancer-Associated Pathways and Biomarkers of Venous Thrombosis. Blood (2017) 130(13):1499–506. doi: 10.1182/blood-2017-03-743211
Keywords: D-dimer, breast cancer, surgery, nursing, thrombosis
Citation: Wang Y, Liang X, Wang S, Wang Y, Qin L, Chen D, Jiang Y and Zhang H (2022) Analysis of the Risk Factors for Elevated D-Dimer Level After Breast Cancer Surgery: A Multicenter Study Based on Nursing Follow-Up Data. Front. Oncol. 12:772726. doi: 10.3389/fonc.2022.772726
Received: 08 September 2021; Accepted: 21 June 2022;
Published: 19 July 2022.
Edited by:
Julio de la Torre, Comillas Pontifical University, SpainReviewed by:
Marcus Vetter, University Hospital of Basel, SwitzerlandHon-Yi Shi, Kaohsiung Medical University, Taiwan
Copyright © 2022 Wang, Liang, Wang, Wang, Qin, Chen, Jiang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xi Liang, a28wMzEzQDE2My5jb20=; Shujun Wang, ODA1MTAxNjRAcXEuY29t; Yuying Wang, d2FuZ3l1eWluZzhAb3V0bG9vay5jb20=; Ling Qin, NzY1MjIzMTQxQHFxLmNvbQ==; Hao Zhang, aGFvemhhbmc4NDA1MTRAMTYzLmNvbQ==
 Yanqiu Wang
Yanqiu Wang Xi Liang1*
Xi Liang1*