- 1General Surgery, Dangdong First Hospital, Dandong, China
- 2Key Laboratory of Hepatosplenic Surgery, Department of Hepatic Surgery, The First Affiliated Hospital of Harbin Medical University, Harbin, China
- 3The Medical Department, Jiangsu Simcere Diagnostics Co., Ltd, Nanjing, China
- 4Nanjing Simcere Medical Laboratory Science Co., Ltd, Nanjing, China
- 5The State Key Lab of Translational Medicine and Innovative Drug Development, Jiangsu Simcere Diagnostics Co., Ltd, Nanjing, China
- 6Department of Gastrointestinal/Hernia and Abdominal Wall Surgery, The First Hospital of China Medical University, Shenyang, China
- 7Department of Hepatopancreatobiliary Surgery, Liaoning Cancer Hospital and Institute, Cancer Hospital of China Medical University, Shenyang, China
More than half of new cases of hepatocellular carcinoma (HCC) and associated deaths occurring annually worldwide are recorded in China. Chinese patients with HCC exhibit special characteristics in terms of etiology, leading to differences in prognosis versus Western patients. In recent years, several angiogenesis inhibitors were approved, and immune checkpoint blockers (ICBs) were recommended as second-line therapy for advanced HCC. In addition, the recent success of a combination of atezolizumab with bevacizumab signals resulted in an essential change in the first-line treatment of HCC. We investigated the characteristics of patients with HCC in China and summarized the rapidly emerging relevant clinical data, which relate to the prospects and challenges associated with the use of ICBs in this setting. We further evaluated the efficacy of ICBs in Chinese patients with HCC based on data obtained from global trials, and discussed possible factors influencing the effectiveness of ICBs in patients with HCC in China. Immunotherapy offers new options for the treatment of advanced HCC, though responses varied between patients. Currently, there is a need to discover specific biomarkers for the accurate identification of patients who would more likely benefit from immunotherapy. Furthermore, investigation of patient characteristics in different countries is necessary to provide a clinical practice basis and reference value for the diagnosis and treatment of HCC.
Introduction
According to 2018 Global Cancer Statistics, liver cancer is the sixth most common and fourth most deadly type of cancer worldwide, and hepatocellular carcinoma (HCC) accounts for 75%–85% of cases (1). HCC is very common in China, accounting for 55.41% and 53.96% of the total number of new liver cancer cases and related deaths, respectively, reported worldwide in 2018 (2). Despite advances in medicine, the 5-year survival rate of patients with HCC in China remains very low (i.e., < 13%) (3). The reasons for this poor survival rate are as follows. Firstly, most patients have both HCC and fundamental liver disease, such as viral hepatitis and cirrhosis, which complicates disease management. Secondly, HCC is usually diagnosed at advanced stages, limiting therapeutic options. Finally, there are few drugs available for the treatment of patients with advanced HCC, namely sorafenib (4, 5), lenvatinib (6), and systemic chemotherapy containing oxaliplatin (7). However, differences in background characteristics and etiology between Chinese and Western patients (8) result in a low objective response rate to treatment and limited survival benefits (9, 10). Following the failure of first-line treatment, the efficacy of second-line treatment is insufficient, and the drug accessibility is poor; hence, there is an urgent clinical need for the development of new drugs.
Immunotherapy is effective and safe for the treatment of solid tumors, such as lung cancer and melanoma. Based on the marked improvement in progression-free survival and overall survival (OS) observed in the IMbrave 150 trial (11), atezolizumab + bevacizumab (T + A) was approved by the US Food and Drug Administration as first-line treatment for advanced HCC, initiating a new era of HCC immunotherapy. Currently, clinical studies on immunotherapy for patients with HCC in China are ongoing, showing significant benefits.
In this review, we summarized recent clinical data of studies on immune checkpoint blockers (ICBs) in Chinese patients with HCC. Moreover, we analyzed differences in the efficacy of immunotherapy between Chinese and Western patients according to global results. We also discussed possible factors influencing the efficacy of immunotherapy uniquely in Chinese patients with HCC. More clinical trials tailored to national and ethnic characteristics are warranted to investigate differences in clinical results due to particular patient characteristics in different geographical regions.
ICBs in Chinese Patients With Advanced HCC
The liver is considered an immune-tolerant organ, and HCC is a typical inflammatory-associated malignancy with a complex immune microenvironment. ICBs can stimulate immune cells to recognize and kill tumor cells by enhancing the immune response, inducing tumor-specific immunity, overcoming immune tolerance, and reactivating immune cells (12–14). These effects propose a new treatment strategy for patients with HCC, involving the use of ICBs alone or in combination with targeted therapies, or other therapies.
ICB Monotherapy
A phase I clinical trial (NCT02742935) was initiated to evaluate the safety, pharmacokinetics, pharmacodynamics, and preliminary antitumor activity of the ICB camrelizumab (15). A total of 36 patients with advanced solid tumors were enrolled, including two patients with HCC. The data showed that 25% of the patients treated with all doses of camrelizumab had a sustained objective response. Two patients with HCC received camrelizumab (400 mg) intravenously, with an overall response rate (ORR) of 50% (1/2). Although the sample size was limited, the results of this clinical trial demonstrated the favorable antitumor efficacy of camrelizumab.
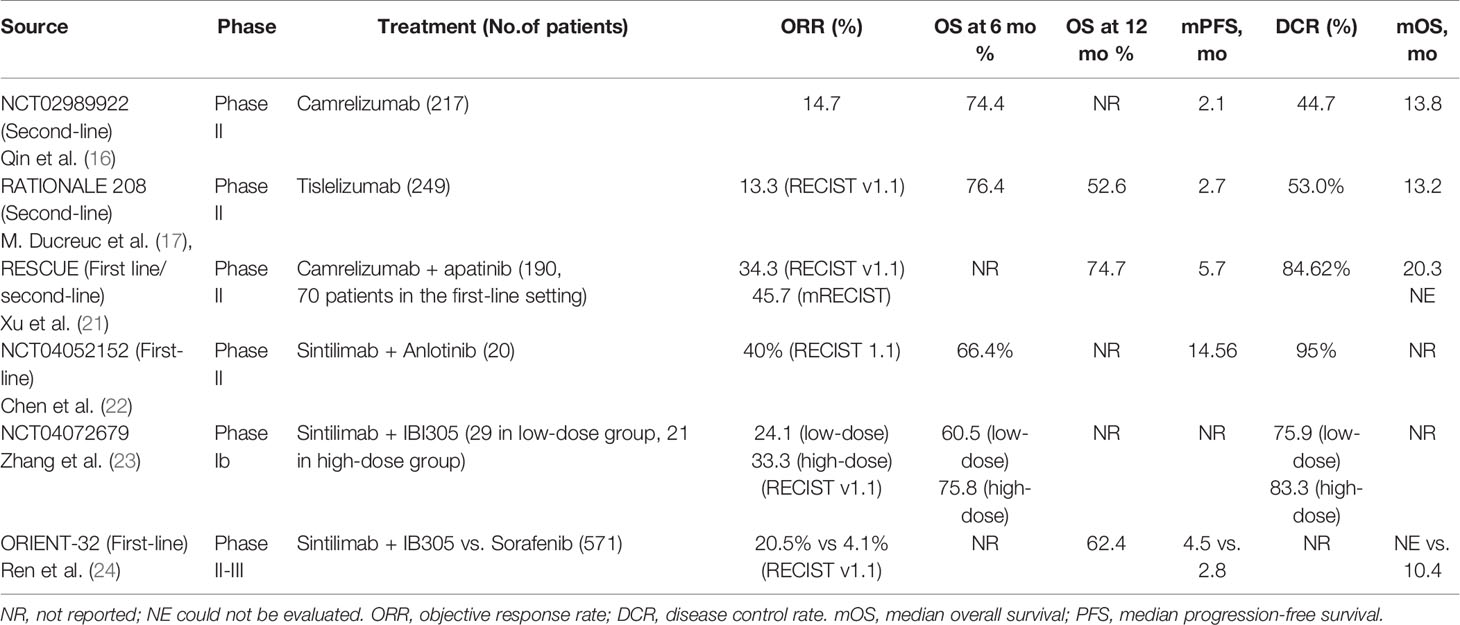
Subsequently, a multicenter, open-label, parallel-grouped, randomized phase II trial (NCT02989922) was promptly initiated to evaluate the efficacy and safety of camrelizumab in the second-line treatment of advanced HCC (16). A total of 220 eligible patients were enrolled; 217 patients were treated and included in the analysis. The patients were randomly assigned (1:1) to receive monotherapy with camrelizumab at a dose of 3 mg/kg every 2 or 3 weeks. The primary endpoints were ORR (per blinded independent central review) and 6-month OS. The results showed that, in patients pretreated with at least one line of systemic therapy, camrelizumab achieved an ORR of 14.7% (95% confidence interval [CI]: 10.3–20.2) and a 6-month OS probability of 74.4% (95% CI: 68.0–79.7). Based on this finding, camrelizumab was approved as a second-line treatment for patients with advanced HCC by the National Medical Products Administration (NMPA).
Thus far, this is the largest clinical study of immunotherapy in Chinese patients with intermediate- to advanced-stage HCC. In addition, it is the largest global clinical study of a programmed cell death 1 (PD-1) inhibitor for the treatment of advanced HCC with hepatitis B virus (HBV) infection. This investigation offers more hope for the patients with advanced HCC in the condition of few treatment options.
RATIONALE 208 (17) is a global, multicenter, phase II clinical study evaluating the efficacy and safety of tislelizumab monotherapy in patients with HCC who have previously received at least one line of systemic therapy. Patients with Barcelona Clinic Liver Cancer stage B/C, Child–Pugh grade A HCC were enrolled and treated with tislelizumab (200 mg) intravenously once every 3 weeks until they developed intolerable toxicity, expressed their desire to withdraw from the study, or did not benefit from the treatment as determined by the investigator.
The primary endpoint of the study was ORR assessed by the Independent Evaluation Committee in accordance with the Response Evaluation Criteria in Solid Tumors, version 1.1 (RECIST v1.1). This study recruited 249 patients (122 in China), including >100 who had received at least two lines of treatment prior to enrolment. The efficacy data were impressive. The ORR for the total population and second-line population was 13.3% and 13.8%, respectively. The median OS was 13.2 and 13.8 months, respectively. The disease control rate (DCR) for the general population was 53.0%, and the 12-month event-free rate was 79.2%. These data showed the advantages offered by tislelizumab in the treatment of HCC. Tislelizumab is a promising option for the second-line treatment of HCC in the future, and will also benefit numerous patients with HCC. At present, the results disclosed in this study do not compare the efficacy of tislelizumab between Chinese and Western populations; hence, we look forward to more detailed results from the follow-up of this clinical study. In addition, there is an ongoing phase III clinical trial (RATIONALE 301 study) involving a head-to-head comparison of tislelizumab with sorafenib for the first-line treatment of advanced HCC; results, from the follow-up of this study are currently awaited.
CheckMate 459 is a randomized, multicenter, phase III study of nivolumab versus sorafenib as first-line treatment in patients with advanced HCC. A total of 743 patients with advanced HCC were enrolled, and the primary endpoint was OS. Although the results did not reach the predefined threshold for statistical significance, this trial yielded some interesting and important findings. Clinical benefit was observed across predefined subgroups, including hepatitis infection status and region (Asia vs. non-Asia) (18). A similar observation was recorded in KEYNOTE-240, which involved 408 patients with advanced HCC; the coprimary endpoints in this study were OS and progression-free survival (PFS). It has been reported that benefits in OS and PFS were associated with viral status and geographical region. Particularly, OS was positively correlated with HBV infection (hazard ratio [HR] = 0.57; 95% CI: 0.35–0.94) and Asia, except for Japan (HR = 0.59; 95% CI: 0.37–0.95) (19). Notably, pembrolizumab reduced the risk of death by 45% in the Asian subgroup compared with 22% in the overall cohort. In the Asian subpopulation, the median PFS was 2.8 months versus 1.4 months in the pembrolizumab group versus the control group, respectively (HR = 0.48; 95% CI: 0.32–0.70; P < 0.0001). The median OS was 13.8 months versus 8.3 months, respectively (HR = 0.55; 95% CI: 0.37–0.80; P = 0.0009). The ORR was 20.6% versus 2.0%, respectively (treatment difference: 18.5%; 95% CI: 8.3–27.6; P = 0.0014). The median DCR was 8.6 months versus 2.8 months, respectively, while the DCR was 59.8% versus 40.0%, respectively (treatment difference: 20.1%; 95% CI: 3.1–35.7; P = 0.0101). The rate of treatment-related adverse events was 58.9% versus 48.0%, respectively. The rate of grades 3–5 treatment-related adverse events was 13.1% versus 4.0%, respectively. Notably, there was no occurrence of treatment-related deaths. These results suggested that pembrolizumab is effective and well tolerated in the second-line treatment of advanced HCC in Asian patients (20) (Table 1).
ICBs + Antiangiogenic Agents
Previous studies have indicated that antiangiogenic agents can enhance the efficacy of immunotherapy against cancer (25, 26). Thus, the combination of antiangiogenic therapy with immunotherapy can synergistically benefit patients with HCC.
A phase I trial of camrelizumab in combination with apatinib (vascular endothelial growth factor receptor 2 [VEGFR2] inhibitor) in the treatment of HCC, gastric cancer, and gastroesophageal junction cancer (NCT02942329) (27) was performed. The study included 43 patients (15 and 28 patients in phases Ia and Ib, respectively). The primary endpoints were safety and tolerability and RP2D (phase II dose) determination of apatinib in combination with camrelizumab. The efficacy endpoints included investigator-assessed ORR, DCR, PFS, and OS. Of the 16 patients with HCC, eight achieved a partial response: the ORR and DCR were 50% and 93.8%, respectively; the median OS was not reached. These results were impressive since the patients with HCC enrolled in this study were refractory patients who had previously received first-line treatment with sorafenib, reflecting the effectiveness of the combination of camrelizumab and apatinib.
Based on the results of this phase I trial, a non-randomized, open, multicenter, phase II clinical study was conducted in 25 centers in China (RESCUE) (21), involving patients with HCC who were refractory to initial treatment or first-line targeted therapy. The study included 190 Chinese patients, who received camrelizumab intravenously (200 mg [for bodyweight ≥ 50 kg] or 3 mg/kg [for bodyweight < 50 kg] every 2 weeks) + apatinib (250 mg/day, 4-week cycles). The primary endpoint was ORR assessed by the Independent Review Board according to the RECIST v1.1. At the data cutoff in June 2021 (28), in the first- and second-line treatment cohorts, the median follow-up time was 19.8 and 21.7 months; the median OS was 20.1 and 21.8 months; and the 24-month OS was 43.3% and 44.6%, respectively.
According to the baseline characteristics of the enrolled patients, >80% had a history of HBV infection, and most had advanced HCC with portal vein tumor thrombus. These findings are in line with the current situation in China, providing strong evidence for the treatment of HCC. In terms of therapeutic effect, the ORR and OS observed in the first- and second-line treatment groups undoubtedly reflect the good application prospects of the combination of camrelizumab with apatinib in the first- and second-line treatment of liver cancer. It is preferable to become a new first-line therapeutic option for HCC. The safety profile of the combination therapy was similar to that noted with camrelizumab monotherapy, and the overall toxicity was controllable and tolerated. In addition, the combination regimen can significantly reduce the incidence of reactive skin capillary hyperplasia.
Based on the above data, the combination of camrelizumab and apatinib may change the paradigm for the treatment of HCC in the future. Of note, a phase III clinical trial (NCT03764293) of camrelizumab combined with apatinib versus sorafenib in the first-line treatment of advanced HCC is currently underway.
Furthermore, another phase Ib trial of Chinese PD-1 inhibitor, sintilimab, in combination with a bevacizumab biosimilar (IBI305) for the treatment of advanced HCC was launched (NCT04072679) (23). A total of 50 patients were enrolled, and the ORR reached 33.3%. The results confirmed both the safety and efficacy of this combination regimen, paving the way for subsequent phase II/III trials.
Sintilimab + IBI305 versus sorafenib for the first-line treatment of advanced HCC (ORIENT-32 trial) was a phase III, randomized, open-label, international multicenter study (24). A total of 571 patients with unresectable or metastatic HCC who had not received systematic treatment were enrolled. The coprimary endpoints were OS and PFS, determined by the Independent Radiologic Review Committee according to the RECIST v1.1. The majority of patients (94.2%) had HBV, and 4.2% had Child–Pugh-B status chronic liver disease. The median PFS (4.5 vs. 2.8 months) and OS (not evaluable vs.10.4 months; HR = 0.57) were significantly prolonged in the sintilimab + IBI305 group versus the sorafenib group; the 1-year OS rate was 62.4% versus 48.5%, respectively. In all relevant subgroups, the OS and PFS of sintilimab + IBI305 were superior to sorafenib. The ORR, assessed by the Independent Radiologic Review Committee according to the RECIST v1.1, was 20.5% in the sintilimab + IBI305 group and 4.1% in the sorafenib group; the ORR evaluated by the RECIST v1.1 was 19.6% versus 2.9%, respectively. Among patients receiving at least one dose of the drug, the incidence of treatment-related adverse events was 88.7% (n = 380) in the sintilimab + IBI305 group and 93.5% (n = 185) in the sorafenib group. The incidence of grades 3–4 treatment-related adverse events was 33.7% and 35.7%, respectively. The combination of sintilimab with IBI305 in the first-line treatment of advanced HCC demonstrated significantly greater clinical efficacy compared with sorafenib monotherapy. Moreover, the combination immunotherapy did not increase the risk of adverse effects. Based on these impressive clinical data, on June 25, 2021, the NMPA approved the combination of sintilimab with IBI305 for the first-line systemic treatment of HCC (Table 1).
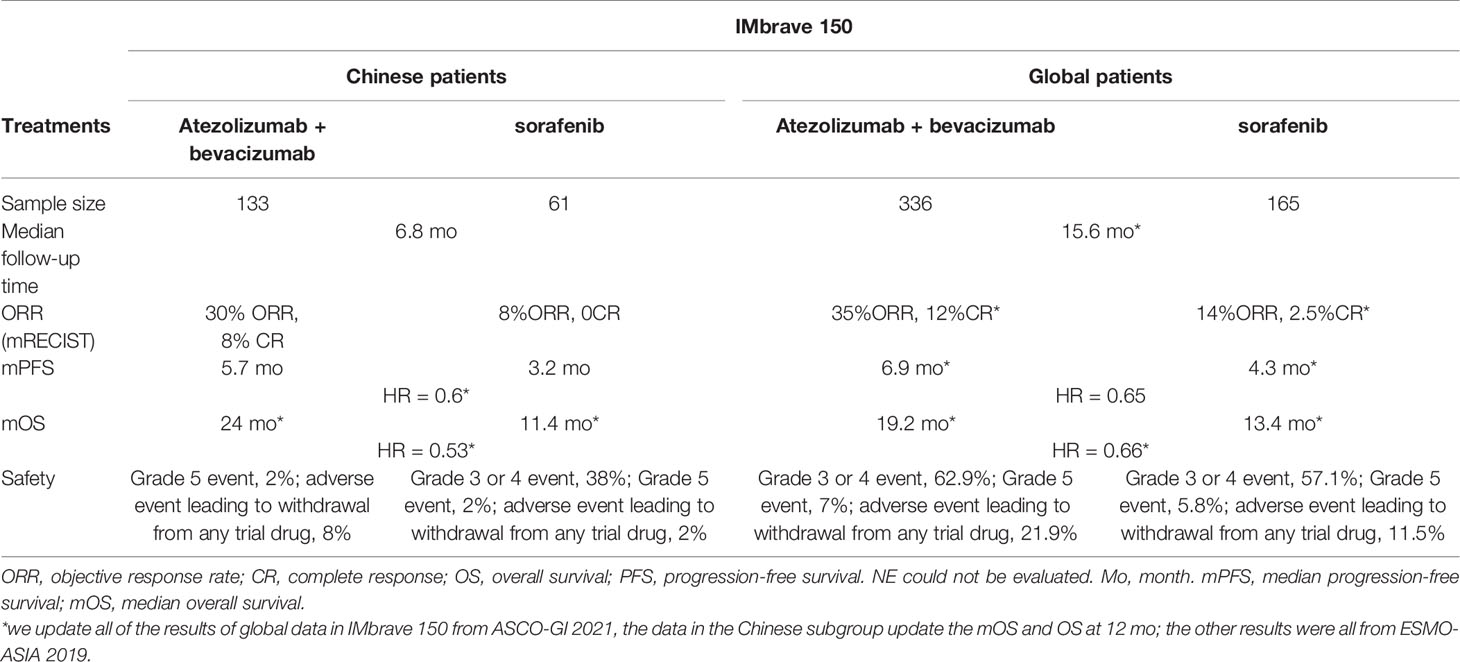
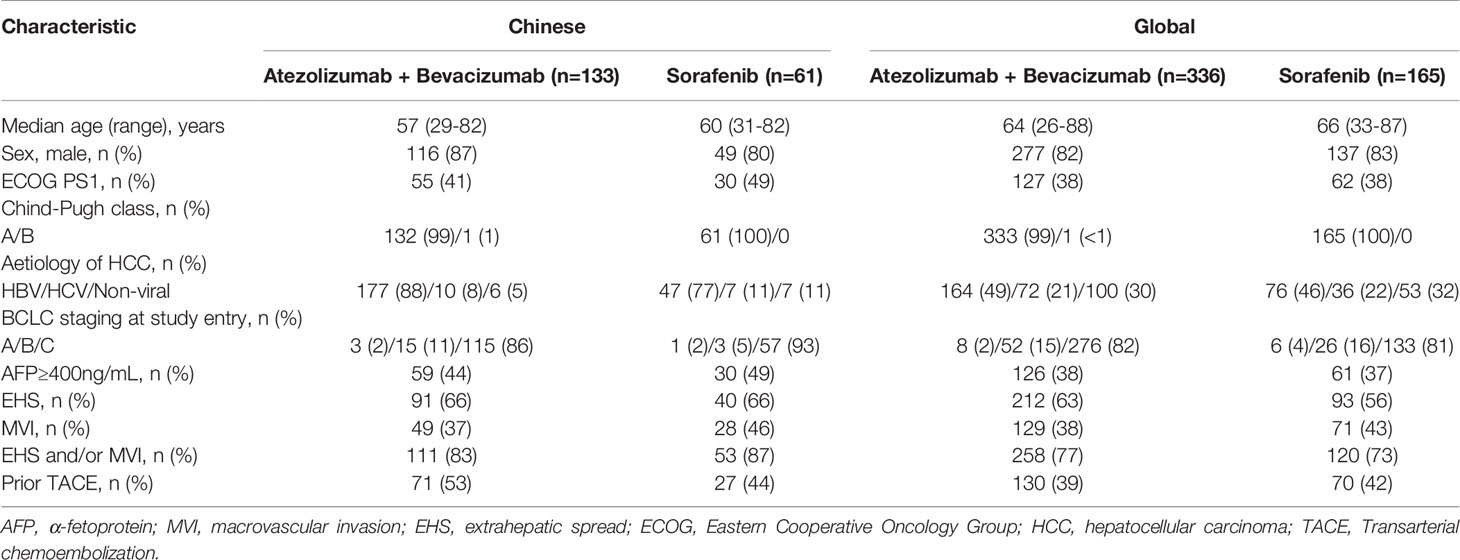
IMbrave 150 was an international, multicenter, clinical trial involving 501 patients with unresectable HCC who had not previously received systemic treatment; the study population included 194 patients from China (137 from the IMbrave150 Global Study and 57 from the China extension enrolment phase). Patients were randomly assigned to the T + A (Atezolizumab plus Bevacizumab) or sorafenib group in a 2:1 ratio, and the coprimary endpoints were OS and PFS assessed at an independent review facility according to the RECIST v1.1. In terms of effectiveness, the latest data showed that the global median OS in the T + A group was 19.2 months, reducing the risk of death by 34% (HR: 0.66, 95% CI: 0.52–0.85). Interestingly, the patients with HBV had longer PFS (HR = 0.47; 95% CI: 0.33–0.67) and OS (HR = 0.51; 95% CI: 0.32–0.81) (29). In the subgroup of 133 Chinese patients treated with T + A, the median OS reached up to 24 months, reducing the risk of death by 47% (HR: 0.53, 95% CI: 0.35–0.80) (30). Data from the Chinese subgroup, presented at the Liver Cancer Summit of the European Association for the Study of the Liver earlier this year, also suggested that T + A may be a more suitable option for Chinese patients (31). Specifically, the data showed that the HR value of OS in the Chinese subgroup was 0.53, and the 6-month survival rate of patients was 86.6%. These findings indicated that the efficacy was better in Chinese patients than other patients (Table 2), though these patients had a higher overall rate of HBV infection, extensive vessel invasion/extrahepatic metastasis, alpha-fetoprotein levels ≥ 400 ng/ml, and other adverse prognostic factors (Table 3). Additionally, the safety data showed that the toxicity of this regimen in the Chinese population was similar to the global population, and could be managed (Table 2).
Both ORIENT32 and IMbrave150 were approved in China, so which one is the better choice for the Chinese HCC patients? In ORIENT-32, sintilimab was PD-1 antibody, while atezolizumab was PD-L1 in IMbrave150. Moreover, the characteristics of patients included in these two studies differed. Patients who enrolled in ORIENT-32 had poor performance status scores; a high proportion of these patients also had adverse prognostic factors, such as HBV infection, extrahepatic metastasis, and alpha-fetoprotein levels ≥ 400 ng/ml (24). Therefore, the results of ORIENT-32 are more meaningful for the treatment of HCC in China, as it reflected the characteristics of Chinese patients with HBV-related HCC. Particularly, the impaired liver function due to cirrhosis impairs the efficacy of sorafenib-targeted therapy in Asian patients with HCC, and at present there is an unmet need for the treatment of such patients. In addition, the two treatment regimens led to similar benefits in OS and PFS; however, the ORR of sintilimab + IBI305 was slightly lower than T + A combination, which may be caused by the coronavirus disease in 2019. Besides, the T + A combination is more expensive, whereas sintilimab + IBI305 is cost effective, highly accessible, and covered by domestic medical insurance schemes in China. In summary, sintilimab + IBI305 may be a more suitable option for first-line treatment in Chinese and other Asian patients.
In addition, the use of sintilimab + anlotinib as first-line therapy in patients with advanced HCC was investigated in a single-arm phase II study(NCT04052152). Until January 15, 2021, 20 patients (all with HBV infection, 18 men and two women) had enrolled in the clinical trial. The primary endpoints (i.e., safety and ORR) were evaluated after first-line treatment with sintilimab (200 mg, intravenously, D1) + anlotinib (12 mg, orally, once daily, D1–14) every 3 weeks. The phase results of this clinical trial were reported at the 2021 American Society of Clinical Oncology Annual Meeting (22): the ORR was 40.0% (8/20); one, seven, and 11 patients had complete response, partial response, and stable disease, respectively. The most common treatment-related adverse events were grades 1–2. According to these preliminary results, the combination of sintilimab and anlotinib showed promising clinical efficacy with manageable toxicity for the first-line treatment of advanced HCC. This treatment regimen further enriches the available options for the first-line treatment of patients with advanced HCC. We look forward to the complete results of this study.
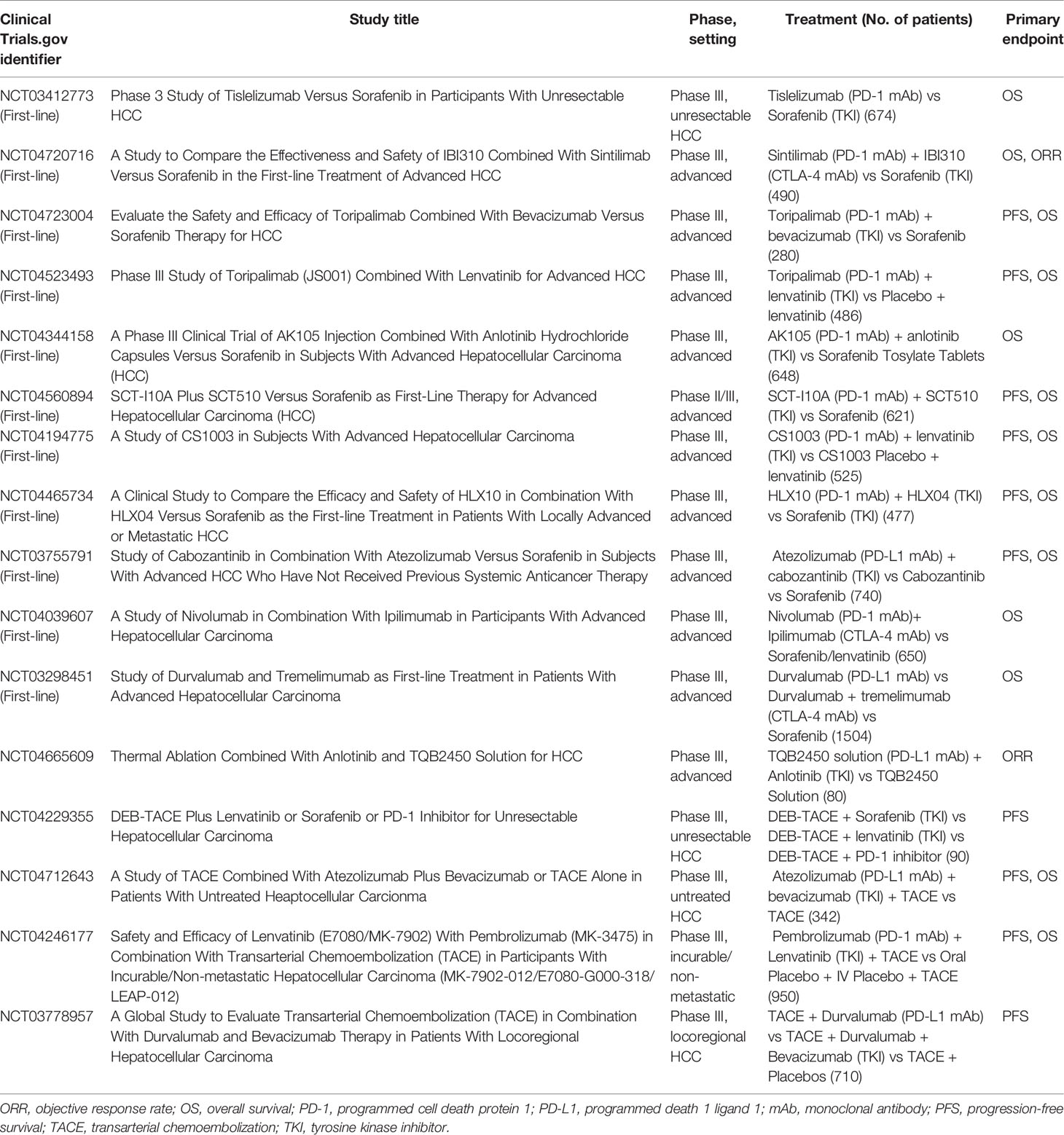
Numerous multicenter, phase III, clinical trials are currently ongoing (Table 4); we hope that these investigations will provide more clinical data to support the application of ICBs.
ICBs Combined With Interventional Therapy
Apart from the aforementioned immunotherapy methods, the combination of ICBs with interventional therapy is another treatment strategy. The most commonly used local treatments or interventional therapies include transcatheter arterial chemoembolization (TACE), transhepatic artery radioembolization (TARE), and hepatic artery infusion chemotherapy (HAIC).TACE can cause tumor necrosis, which promotes the release of tumor-associated antigens and neoantigens. Thus, theoretically, the combination of TACE with ICBs may exhibit synergy, thereby enhancing the antitumor immune effect (32–35). Preliminary study results of nivolumab combined with drug-eluting bead-TACE, reported in the 2020 Gastrointestinal Cancers Symposium of the American Society of Clinical Oncology (36), have confirmed the safety and efficacy of this regimen. A preliminary retrospective case series demonstrated that TARE combined with immunotherapy was safe and effective, and the combination therapy may improve PFS and OS in patients with liver metastases from uveal melanoma (37). A case report showed a significant response following consecutive treatment with TARE, sorafenib, and nivolumab in a patient with metastatic HCC (38). This finding suggested that TARE, sorafenib, and nivolumab may exert a synergistic effect on the immune response to HCC. However, large-scale, prospective clinical trials are warranted to validate these results. A retrospective study evaluated the efficacy of HAIC or HAIC combined with anti-PD-1 immunotherapy (HAICAP) in patients with advanced HCC. The investigators found that patients treated with HAICAP had significantly better treatment response and survival benefits than those treated with HAIC (39).
Another retrospective study (40) compared the efficacy of lenvatinib + toripalimab (PD-1 monoclonal antibody) + HAIC (LeToHAIC, n = 71) with that of lenvatinib (n = 86) in patients with advanced HCC. The results revealed that LeTOHAIC was associated with longer PFS (11.1 vs. 5.1 months, respectively; HR = 0.48, 95% CI: 0.33–0.7, P < 0.001) and OS (< 11 months; HR = 0.4, 95% CI: 0.24–0.66, P < 0.001). The DCR (90.1% vs. 72.1%, respectively, P = 0.005) and ORR (RECIST: 59.2% vs. 9.3%, respectively, P < 0.001; modified RECIST: 67.6% vs. 16.3%, respectively, P < 0.001) in the LeTOHAIC group were superior to those recorded in the lenvatinib monotherapy group. Immuno-targeted therapy could eradicate residual tumor lesions after HAIC, and patients achieved longer survival. A real-world study of HAIC combined with anti-PD-1 immunotherapy and tyrosine kinase inhibitors (TKIs) for advanced HCC showed that HAIC + anti-PD-1 antibody + oral TKIs were effective and safe. In this study, ORR (63% vs. 36.7%–46%, respectively) and median PFS (10.6 vs. 5.5–9.3 months, respectively) were higher than those reported in a previous study of anti-PD-1 antibody combined with TKI for unresectable HCC (41).
Although combined immunotherapy has entered an era of blooming flowers, and the efficacy of advanced HCC patients has been greatly improved, there are still many issues worth considering and exploring. Firstly, targeted therapy combined immunotherapy has brought gratifying results, suggesting that we have various systemic therapies deserve further investigation, including but not limited to immune checkpoint inhibitors + antiangiogenic agents or tyrosinase inhibitors (TKIs). New targets, new drugs with different mechanisms, and new combination regimens are all worth trying, for example, a stronger combination: PD-1 inhibitor + targeted therapy + TACE, etc. Secondly, we have revealed good efficacy of combined immunotherapy in advanced patients, and the application of immunotherapy combination models in early and mid-stage HCC needs to be further explored, such as immunotherapy combined targeted therapy for the perioperative treatment of HCC. Finally, we need to explore the dominant populations that benefit from immunotherapy and look for biomarkers that can effectively predict the efficacy. Numerous larger prospective studies are currently underway in China, investigating the optimal combination therapy; the results of these studies are anticipated (Table 4).
Chinese Patients With HCC: Characteristics and Their Correlation With Immunotherapy
HCC in China is characterized by distinct etiology, biological events at the molecular level, and prognosis, thus requiring a specific treatment strategy. Firstly, >70% of patients with HCC in China have HBV infection (8); it is thought that these patients who are more prone to develop progressive disease and have poorer prognoses than those with hepatitis B virus (HCV) infection (9, 10). Secondly, there are significant differences in the mutation landscape between Chinese and Western patients. Jia Fan et al. reported that the mutation frequencies in axin 1 (AXIN1), tuberous sclerosis complex subunit 2 (TSC2), SWI/SNF related, matrix associated, actin dependent regulator of chromatin, subfamily a, member 2 (SMARCA2), ATRX chromatin remodeler (ATRX), and lysine methyltransferase 2C (KMT2C) were relatively higher, whereas that of catenin beta 1 (CTNNB1) was significantly lower in the Chinese HBV-positive HCC cohort versus the HBV-positive HCC subgroup from The Cancer Genome Atlas (42). Thirdly, approximately 60%–70% of patients with HCC were diagnosed at intermediate-to-advanced stages of the disease, and most had undergone TACE as first-line palliative treatment instead of surgical excision (43). Finally, traditional Chinese medicine (TCM) is widely used in China, and is effective in improving the quality of life, modulating immune functions, preventing recurrence and metastasis, delaying tumor progression, and prolonging survival in patients with cancer (44–49). Almost 80% of patients with HBV in China are treated with TCM (50). Moreover, aristolochic acid (AA), a compound used in TCM, can cause genomic damage and particular gene mutations in liver cells (51–54). These effects occurred in 78% and 47% of Taiwanese and Chinese patients, respectively; these proportions are markedly higher than those reported in Western countries (55).
HBV Infection
HBV infection could lead to changes in the liver immune microenvironment. It causes immunosuppression, and leads to peripheral immune tolerance with the development of chronic infection. Finally, it mediates tumorigenesis due to impaired immune surveillance (56). In chronic viral hepatitis, immunosuppressive checkpoints, including PD-1/PD-L1, cytotoxic T-lymphocyte associated protein 4 (CTLA4), and T cell immunoglobulin and mucin domain 3 (TIM3), play an important role in immunosuppression by downregulating the T cell response (57).
Lim et al. (58) reported that regulatory T cells and CD8+ resident memory T cells were enriched in HBV-related HCC. Regulatory T cells and memory T cells obtained from patients with HBV-related HCC expressed more PD-1 and were functionally more immunosuppressive and exhausted than those of nonvirus-related HCC. This immunosuppression by PD-1 + regulatory T cells could be reversed by anti-PD-1 blockade. The microenvironment of HBV-related HCC is more immunosuppressive and exhausted than that of nonviral-related HCC. Despite the lack of comparison with HCV-HCC, these results had important implications in the management of HBV-HCC.
The results of two studies with small sample sizes, namely CheckMate 040 (59) and KEYNOTE-224 (60), showed that the efficacy of ICBs was not affected by HBV or HCV infection. Nevertheless, further data from the CheckMate 459 and KEYNOTE-240 studies revealed that clinical benefit was associated with the infection status. In KEYNOTE-240, the ORR associated with pembrolizumab or placebo at the time of the final analysis was 18% and 4%, respectively (one-sided P < 0.001). In the Asian subgroup, the ORR was 21% and 2%, respectively (P < 0.001). Notably, the proportion of patients with HBV infection status was markedly higher in the Asian subgroup versus the overall group (51% vs. 25%, respectively). In the corresponding subgroup analysis of data from the IMbrave 150 study, patients with HBV-HCC may benefit more than those with nonviral HCC. Notably, T + A significantly extended the median PFS of patients with HBV-positive HCC compared with sorafenib; however, this effect was not observed in patients with nonviral HCC (median PFS, HBV-positive HCC: 6.7 vs. 2.8 months, respectively; nonviral HCC: 7.1 vs. 5.6 months, respectively) (61). Additional prospective clinical trials are warranted in the future to confirm the relationship between the infection status and efficacy of ICBs.
Gene Mutation Landscapes
Fan et al. (42) reported that the mutation frequencies in genes AXIN1, TSC2, SMARCA2, ATRX, and KMT2C were relatively higher, whereas that of CTNNB1 was significantly lower, in Chinese HCC patients with HBV infection cohort than in the HBV-positive HCC subgroup from The Cancer Genome Atlas. AXIN1, TSC2, ATRX, and KMT2C genes were positively correlated with immunotherapy. TSC2 and mechanistic target of rapamycin complex 1 (mTORC1) played specific roles in the induction of antitumor immunity. TSC2-deficient tumors behaviors T cell exhaustion and response to anti-PD-1/anti-CTLA4 immunotherapy (62). ATRX mutation may be a predictive biomarker for the efficacy of ICBs in female patients with gastric cancer (63). Members of the KMT2 family (e.g., KMT2A, KMT2C, and KMT2D) exhibit a high mutation rate in nonsmall cell lung cancer tumors (64, 65), and these mutations were associated with higher tumor mutational burden (TMB) and PD-L1 expression, as well as higher PD-L1+/TMB-high proportions. Importantly, nonsmall cell lung cancer patients with tumor protein p53 (TP53)/KMT2C comutations who underwent treatment with ICBs had significantly longer PFS and greater durable clinical benefit (66). CTNNB1 is one of the most common mutant genes in HCC, which encodes a β-catenin protein and is involved in the regulation of the Wnt signaling pathway. Recent studies have shown that the activation of Wnt/CTNNB1 signaling can promote the immune escape of liver tumors, leading to the development of resistance to PD-1 immunotherapy (67).
TACE
TACE is closely related to immunotherapy; for example, TACE can rapidly “starve” the tumor by blocking the blood supply, while the necrotic tumor tissue will further stimulate the body’s high T cell response, revealing a synergistic mechanism (35, 68, 69). In other words, TACE kills HCC cells and induces the release of tumor-associated antigens, thereby enhancing the tumor-specific CD8+ T cell response. TACE can significantly increase the CD4/CD8 ratio (70) and number of T helper 17 cells (71), as well as improve the immune microenvironment of the liver to a certain extent (72) which subsequently transforms cold tumors into hot tumors. Nevertheless, TACE increased the expression of PD-1 and PD-L1 in HCC (73, 74), potentially inhibiting antitumor immunity. Therefore, the combination of TACE and ICBs may be a promising therapeutic option for optimizing tumor response and downtime therapy. However, in all clinical trials of immune monotherapy conducted thus far (i.e., KEYNOTE-224, KEYNOTE-240, CheckMate 040, CheckMate 459), TACE was not included in the subgroup analysis. Therefore, there is no evidence regarding the effect of TACE on the efficacy of immune monotherapy. In the phase 2–3 ORIENT-32 study (24), the researchers found that patients could benefit from treatment regardless of the use of TACE: TACE (OS, HR = 0.59, 95% CI: 0.46–0.76; PFS, HR = 0.59, 95% CI: 0.41–0.84); no TACE (OS, HR = 0.48, 95% CI: 0.33–0.70; PFS, HR = 0.59, 95% CI: 0.38–0.91). Therefore, the potential contribution of TACE to immunotherapy remains to be further investigated.
TCM and AA
Long-term clinical practice has proven that treatment of HCC with TCM is effective in improving symptoms, delaying disease recurrence, reducing toxicity, increasing efficacy, and prolonging survival. At present, there is rich practical experience accumulated with regard to many Chinese patent medicines used in the treatment of primary liver cancer. For example, Huaier granules (47), Jinlong capsules (48), Chinese herbal injections (45), and elemene (44) have been included in the 2020 Chinese Society of Clinical Oncology guidelines for the diagnosis and treatment of primary liver cancer. In addition, the “Guidelines for the Diagnosis and Treatment of Chinese Medicine Tumors,” that are in line with international standards, are consistent with modern clinical practice (75). Owing to its advantages (i.e., strengthening the body, enhancing the immune system, and inducing few toxic reactions), TCM plays a complementary role in improving the symptoms, immune function, and the quality of life of patients with liver cancer. For example, Huaier granules can regulate the body’s immunity by stimulating the release of cytokines, and can also result in antitumor responses by inducing cell cycle arrest and inhibiting tumor angiogenesis. Elemene can induce apoptosis in liver cancer cells, block the cycle of liver cancer cells, and inhibit the proliferation, invasion, and metastasis of liver cancer cells. It can also inhibit angiogenesis by liver cancer cells, and regulate immune function. Jinlong capsules can reduce tumor angiogenesis, prevent recurrence and metastasis, improve immunity, and relieve pain, fatigue, and symptoms of the digestive tract. In conclusion, the regulatory effect of TCM on the human immune system cannot be ignored.
AA and its derivatives are components of numerous traditional medicines that have been used for thousands of years, particularly in Asian countries (76). Since the recognition of the nephrotoxicity and carcinogenicity of AA, the US Food and Drug Administration and the regulatory agencies of some other countries have issued warnings to prohibit the use and import of products containing Aristolochia (77). Nonetheless, in China and some Asian countries, herbal preparations and products containing Aristolochia and Asarum continue to be widely used. The role of AA in liver cancer remains controversial. Although many studies have shown that AA can cause liver damage and is a risk factor for HCC, there are also research results indicating that the role of AA needs to be reexamined (78). It is established that higher TMB levels and neoantigen load indicate a potential benefit from immunotherapy, such as ICBs (79). Fan et al. (42) found that the levels of TMB in AA-signature-containing HCC tumors were two-fold higher than those detected in non-AA HCC tumors. Moreover, the predicted neoantigen counts were more than two-fold higher in HCC tumors with an AA signature. They harbored significantly denser infiltrating CD8+ T cells (42) and exhibited higher expression of PD-L1, which were particularly related to tumor microenvironmental immune tolerance (80). It is suggested that HCC patients with the AA signature may benefit from immunotherapy.
Regrettably, Chinese and international clinical trials have not included the use of TCM in the subgroup analysis. Even in the ORIENT-32 clinical trial, patients with HCC who had received TCM within 2 weeks were excluded from the trial. Based on the existing research results, we cannot analyze the impact of TCM on ICBs in the real-world setting.
In addition to the factors mentioned above related to immunotherapy alone, the combination of treatments can affect immunotherapy, which also warrants further study. For example, the HBV virus can induce genetic mutations and regulate the expression of genes (81), such as telomerase reverse transcriptase (TERT) (82) and TP53 (83, 84), which may be indirectly related to immunotherapy. Some investigators found that TCM may improve immune response in patients with HCC undergoing TACE (85). It is suggested that the combination of interventional therapy and TCM may promote the immune response of patients with unresectable HCC. Moreover, studies have shown that the hepatic viral infection status, principally HBV infection, is a beneficial factor in the treatment of HCC patients with Chinese medicine combined with TACE (HR = 0.67; 95% CI: 0.53–0.84) (47). However, there is a lack of relevant evidence, and additional randomized controlled clinical trials are warranted.
Conclusion
Currently, there are several options for the first-line treatment of HCC, including targeted drugs, immunotherapy + antivascular agents. According to two phase III studies, the combination of ICBs + antivascular agents is the preferred choice. Among them, sintilimab + IBI305 may be more suitable for Chinese patients with HCC. However, Challenges of immunotherapy include the selection of suitable patients and subsequent treatment after disease progression. Therefore, further investigation is needed.
PD-1 monotherapy is also an option for patients with TKI intolerance or contraindications to bevacizumab. In addition, the combination of tislelizumab, camrelizumab, and other ICBs with targeted therapy, chemotherapy, local therapy, and other immunotherapies is also being explored. Future research results are expected to provide diversified options for the treatment of HCC. Concerning second-line treatment of HCC, the current results are based on phase II clinical studies of immunomonotherapy, and the results of phase III studies are expected in the future.
Chinese HCC patients exhibit different characteristics compared with Western patients, such as HBV infection, exposure to aflatoxin B1 (86). Additionally, a considerable number of patients received TCM. Furthermore, the genetic mutations differ between these populations. These characteristics influence the immune microenvironment of patients, thereby affecting the efficacy of immunotherapy. Therefore, it is necessary to design clinical study specific to the Chinese HCC patients. Besides, in the large, global, clinical trials, further detailed subgroup analyses should be conducted to obtain more accurate results. Such data would provide more scientific and specific reference value for clinical guidance.
Author Contributions
YW and HL, investigation and original draft preparation. XY, TG and TS, writing–original draft, review, and editing. HX and XF, conceptualization, investigation, supervision, writing–original draft, review, and editing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
Author XY, TG and TS were employed by Jiangsu Simcere Diagnostics Co., Ltd and Nanjing Simcere Medical Laboratory Science Co., Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Dr. Chuang Qi from Simceredx for his kind assistance. The authors thank all current and former researchers and investigators as well as patients and their families who participated in clinical trials establishing ICBs as a key agent in cancer therapy.
Abbreviations
AA, Aristolochic acid; DCR, Disease control rate; HAIC, Hepatic artery infusion chemotherapy; HBV, Hepatitis B virus; HCC, Hepatocellular carcinoma; HR, Hazard ratio; ICB, Immune checkpoint blockers; NMPA, National Medical Products Administration; ORR, Overall response rate; OS, Overall survival; PFS, Progression-free survival; TCM, Traditional Chinese medicine; TKI, Tyrosine kinase inhibitors; TMB, Tumor mutational burden; VEGF, Vascular endothelial growth factor.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin (2018) 68:394–424. doi: 10.3322/caac.21492
2. Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer Statistics in China, 2015. CA Cancer J Clin (2016) 66:115–32. doi: 10.3322/caac.21338
3. Zeng H, Chen W, Zheng R, Zhang S, Ji JS, Zou X, et al. Changing Cancer Survival in China During 2003-15: A Pooled Analysis of 17 Population-Based Cancer Registries. Lancet Glob Health (2018) 6:e555–67. doi: 10.1016/S2214-109X(18)30127-X
4. Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al. Sorafenib in Advanced Hepatocellular Carcinoma. N Engl J Med (2008) 359:378–90. doi: 10.1056/NEJMoa0708857
5. Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, et al. Efficacy and Safety of Sorafenib in Patients in the Asia-Pacific Region With Advanced Hepatocellular Carcinoma: A Phase III Randomised, Double-Blind, Placebo-Controlled Trial. Lancet Oncol (2009) 10:25–34. doi: 10.1016/S1470-2045(08)70285-7
6. Kudo M, Finn RS, Qin S, Han KH, Ikeda K, Piscaglia F, et al. Lenvatinib Versus Sorafenib in First-Line Treatment of Patients With Unresectable Hepatocellular Carcinoma: A Randomised Phase 3 Non-Inferiority Trial. Lancet (2018) 391:1163–73. doi: 10.1016/S0140-6736(18)30207-1
7. Qin S, Bai Y, Lim HY, Thongprasert S, Chao Y, Fan J, et al. Randomized, Multicenter, Open-Label Study of Oxaliplatin Plus Fluorouracil/Leucovorin Versus Doxorubicin as Palliative Chemotherapy in Patients With Advanced Hepatocellular Carcinoma From Asia. J Clin Oncol (2013) 31:3501–8. doi: 10.1200/JCO.2012.44.5643
8. de Martel C, Maucort-Boulch D, Plummer M, Franceschi S. World-Wide Relative Contribution of Hepatitis B and C Viruses in Hepatocellular Carcinoma. Hepatology (2015) 62:1190–200. doi: 10.1002/hep.27969
9. Sinn DH, Gwak GY, Cho J, Paik SW, Yoo BC. Comparison of Clinical Manifestations and Outcomes Between Hepatitis B Virus- and Hepatitis C Virus-Related Hepatocellular Carcinoma: Analysis of a Nationwide Cohort. PloS One (2014) 9:e112184. doi: 10.1371/journal.pone.0112184
10. Cantarini MC, Trevisani F, Morselli-Labate AM, Rapaccini G, Farinati F, Del Poggio P, et al. Effect of the Etiology of Viral Cirrhosis on the Survival of Patients With Hepatocellular Carcinoma. Am J Gastroenterol (2006) 101:91–8. doi: 10.1111/j.1572-0241.2006.00364.x
11. Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, et al. Atezolizumab Plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N Engl J Med (2020) 382:1894–905. doi: 10.1056/NEJMoa1915745
12. Hato T, Goyal L, Greten TF, Duda DG, Zhu AX. Immune Checkpoint Blockade in Hepatocellular Carcinoma: Current Progress and Future Directions. Hepatology (2014) 60:1776–82. doi: 10.1002/hep.27246
13. Pinter M, Jain RK, Duda DG. The Current Landscape of Immune Checkpoint Blockade in Hepatocellular Carcinoma: A Review. JAMA Oncol (2021) 7:113–23. doi: 10.1001/jamaoncol.2020.3381
14. Giraud J, Chalopin D, Blanc JF, Saleh M. Hepatocellular Carcinoma Immune Landscape and the Potential of Immunotherapies. Front Immunol (2021) 12:655697. doi: 10.3389/fimmu.2021.655697
15. Mo H, Huang J, Xu J, Chen X, Wu D, Qu D, et al. Safety, Anti-Tumour Activity, and Pharmacokinetics of Fixed-Dose SHR-1210, an Anti-PD-1 Antibody in Advanced Solid Tumours: A Dose-Escalation, Phase 1 Study. Br J Cancer (2018) 119:538–45. doi: 10.1038/s41416-018-0100-3
16. Qin S, Ren Z, Meng Z, Chen Z, Chai X, Xiong J, et al. Camrelizumab in Patients With Previously Treated Advanced Hepatocellular Carcinoma: A Multicentre, Open-Label, Parallel-Group, Randomised, Phase 2 Trial. Lancet Oncol (2020) 21:571–80. doi: 10.1016/S1470-2045(20)30011-5
17. Ducreux M, Abou-Alfa GK, Ren Z, Edeline J, Li Z, Assenat E, et al. Results From a Global Phase 2 Study of Tislelizumab, an Investigational PD-1 Antibody. In: Patients With Previously Treated Advanced Hepatocellular Carcinoma. ESMO World Congress on Gastrointestinal Cancer (2021). p. Abstract O–1.
18. Yau T, Park JW, Finn RS, Cheng AL, Mathurin P, Edeline J, et al. Nivolumab Versus Sorafenib in Advanced Hepatocellular Carcinoma (CheckMate 459): A Randomised, Multicentre, Open-Label, Phase 3 Trial. Lancet Oncol (2022) 23:77–90. doi: 10.1016/S1470-2045(21)00604-5
19. Finn RS, Ryoo BY, Merle P, Kudo M, Bouattour M, Lim HY, et al. Pembrolizumab As Second-Line Therapy in Patients With Advanced Hepatocellular Carcinoma in KEYNOTE-240: A Randomized, Double-Blind, Phase III Trial. J Clin Oncol (2020) 38:193–202. doi: 10.1200/JCO.19.01307
20. Kudo M, Lim HY, Cheng AL, Chao Y, Yau T, Ogasawara S, et al. Pembrolizumab as Second-Line Therapy for Advanced Hepatocellular Carcinoma: A Subgroup Analysis of Asian Patients in the Phase 3 KEYNOTE-240 Trial. Liver Cancer (2021) 10:275–84. doi: 10.1159/000515553
21. Xu J, Shen J, Gu S, Zhang Y, Wu L, Wu J, et al. Camrelizumab in Combination With Apatinib in Patients With Advanced Hepatocellular Carcinoma (RESCUE): A Nonrandomized, Open-Label, Phase II Trial. Clin Cancer Res (2021) 27:1003–11. doi: 10.1158/1078-0432.CCR-20-2571
22. Chen X, Li W, Wu X, Zhao F, Wang D, Wu H, et al. Sintilimab Plus Anlotinib as First-Line Therapy in Patients (Pts) With Advanced Hepatocellular Carcinoma (aHCC). J Clin Oncol (2021) 39(15_suppl):e16146–6. doi: 10.1200/JCO.2021.39.15_suppl.e16146
23. Zhang W, Bi X, Sun Y, Yu Y, Zhou J-g, Zeng H, et al. Preliminary Results of Sintilimab Plus Different Dose of IBI305 (Anti-VEGF Monoclonal Antibody) in Patients With Advanced Hepatocellular Carcinoma: A Phase Ib Study. J Clin Oncol (2020) 3(15_suppl):3079–9. doi: 10.1200/jco.2020.38.15_suppl.3079
24. Ren Z, Xu J, Bai Y, Xu A, Cang S, Du C, et al. Sintilimab Plus a Bevacizumab Biosimilar (IBI305) Versus Sorafenib in Unresectable Hepatocellular Carcinoma (ORIENT-32): A Randomised, Open-Label, Phase 2-3 Study. Lancet Oncol (2021) 22:977–90. doi: 10.1016/S1470-2045(21)00252-7
25. Atkins MB, Plimack ER, Puzanov I, Fishman MN, McDermott DF, Cho DC, et al. Axitinib in Combination With Pembrolizumab in Patients With Advanced Renal Cell Cancer: A Non-Randomised, Open-Label, Dose-Finding, and Dose-Expansion Phase 1b Trial. Lancet Oncol (2018) 19:405–15. doi: 10.1016/S1470-2045(18)30081-0
26. Stein S, Pishvaian MJ, Lee MS, Lee K-H, Hernandez S, Kwan A, et al. Safety and Clinical Activity of 1L Atezolizumab + Bevacizumab in a Phase Ib Study in Hepatocellular Carcinoma (HCC). J Clin Oncol (2018) 36(15_suppl):4074–4. doi: 10.1200/JCO.2018.36.15_suppl.4074
27. Xu J, Zhang Y, Jia R, Yue C, Chang L, Liu R, et al. Anti-PD-1 Antibody SHR-1210 Combined With Apatinib for Advanced Hepatocellular Carcinoma, Gastric, or Esophagogastric Junction Cancer: An Open-Label, Dose Escalation and Expansion Study. Clin Cancer Res (2019) 25:515–23. doi: 10.1158/1078-0432.CCR-18-2484
28. Zhang Y, Xu J, Shen J, Gu S, Wu L, Wu J, et al. Update on Overall Survival (OS) of RESCUE: An Open-Label, Phase 2 Trial of Camrelizumab (C) in Combination With Apatinib (A) in Patients With Advanced Hepatocellular Carcinoma (HCC). J Clin Oncol (2021) 39(15_suppl):4076–6. doi: 10.1200/JCO.2021.39.15_suppl.4076
29. Kudo M. A New Era in Systemic Therapy for Hepatocellular Carcinoma: Atezolizumab Plus Bevacizumab Combination Therapy. Liver Cancer (2020) 9:119–37. doi: 10.1159/000505189
30. Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim T-Y, et al. IMbrave150: Updated Overall Survival (OS) Data From a Global, Randomized, Open-Label Phase III Study of Atezolizumab (Atezo) + Bevacizumab (Bev) Versus Sorafenib (Sor) in Patients (Pts) With Unresectable Hepatocellular Carcinoma (HCC). J Clin Oncol (2021) 39(3_suppl):267–7. doi: 10.1200/JCO.2021.39.3_suppl.267
31. Qin S, Ren Z, Feng YH, Yau T, Wang B, Zhao H, et al. Atezolizumab Plus Bevacizumab Versus Sorafenib in the Chinese Subpopulation With Unresectable Hepatocellular Carcinoma: Phase 3 Randomized, Open-Label IMbrave150 Study. Liver Cancer (2021) 10:296–308. doi: 10.1159/000513486
32. Kohles N, Nagel D, Jüngst D, Stieber P, Holdenrieder S. Predictive Value of Immunogenic Cell Death Biomarkers HMGB1, sRAGE, and DNase in Liver Cancer Patients Receiving Transarterial Chemoembolization Therapy. Tumour Biol (2012) 33:2401–9. doi: 10.1007/s13277-012-0504-2
33. Galluzzi L, Buqué A, Kepp O, Zitvogel L, Kroemer G. Immunological Effects of Conventional Chemotherapy and Targeted Anticancer Agents. Cancer Cell (2015) 28:690–714. doi: 10.1016/j.ccell.2015.10.012
34. Kroemer G, Galluzzi L, Kepp O, Zitvogel L. Immunogenic Cell Death in Cancer Therapy. Annu Rev Immunol (2013) 31:51–72. doi: 10.1146/annurev-immunol-032712-100008
35. Singh P, Toom S, Avula A, Kumar V, Rahma OE. The Immune Modulation Effect of Locoregional Therapies and Its Potential Synergy With Immunotherapy in Hepatocellular Carcinoma. J Hepatocell Carcinoma (2020) 7:11–7. doi: 10.2147/JHC.S187121
36. Harding JJ, Yarmohammadi H, Reiss KA, Chou JF, Capanu M, Do RKG, et al. Nivolumab (NIVO) and Drug Eluting Bead Transarterial Chemoembolization (Deb-TACE): Preliminary Results From a Phase I Study of Patients (Pts) With Liver Limited Hepatocellular Carcinoma (HCC). J Clin Oncol (2020) 38(4_suppl):525–5. doi: 10.1200/JCO.2020.38.4_suppl.525
37. Zheng J, Irani Z, Lawrence D, Flaherty K, Arellano RS. Combined Effects of Yttrium-90 Transarterial Radioembolization Around Immunotherapy for Hepatic Metastases From Uveal Melanoma: A Preliminary Retrospective Case Series. J Vasc Interv Radiol (2018) 29:1369–75. doi: 10.1016/j.jvir.2018.04.030
38. Adcock CS, Puneky LV, Campbell GS. Favorable Response of Metastatic Hepatocellular Carcinoma to Treatment With Trans-Arterial Radioembolization Followed by Sorafenib and Nivolumab. Cureus (2019) 11:e4083. doi: 10.7759/cureus.4083
39. Mei J, Li SH, Li QJ, Sun XQ, Lu LH, Lin WP, et al. Anti-PD-1 Immunotherapy Improves the Efficacy of Hepatic Artery Infusion Chemotherapy in Advanced Hepatocellular Carcinoma. J Hepatocell Carcinoma (2021) 8:167–76. doi: 10.2147/JHC.S298538
40. He MK, Liang RB, Zhao Y, Xu YJ, Chen HW, Zhou YM, et al. Lenvatinib, Toripalimab, Plus Hepatic Arterial Infusion Chemotherapy Versus Lenvatinib Alone for Advanced Hepatocellular Carcinoma. Ther Adv Med Oncol (2021) 13:17588359211002720. doi: 10.1177/17588359211002720
41. Liu BJ, Gao S, Zhu X, Guo JH, Kou FX, Liu SX, et al. Real-World Study of Hepatic Artery Infusion Chemotherapy Combined With Anti-PD-1 Immunotherapy and Tyrosine Kinase Inhibitors for Advanced Hepatocellular Carcinoma. Immunotherapy (2021) 13:1395–405. doi: 10.2217/imt-2021-0192
42. Gao Q, Zhu H, Dong L, Shi W, Chen R, Song Z, et al. Integrated Proteogenomic Characterization of HBV-Related Hepatocellular Carcinoma. Cell (2019) 179:561–77.e22. doi: 10.1016/j.cell.2019.08.052
43. Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, Burroughs AK, et al. Clinical Management of Hepatocellular Carcinoma. Conclusions of the Barcelona-2000 EASL Conference. European Association for the Study of the Liver. J Hepatol (2001) 35:421–30. doi: 10.1016/s0168-8278(01)00130-1
44. Yao Y, Chen J, Jiao D, Li Y, Zhou X, Han X. Elemene Injection Combined With Transcatheter Arterial Chemoembolization for Unresectable Hepatocellular Carcinoma: A Meta-Analysis. Med (Baltimore) (2019) 98:e17813. doi: 10.1097/MD.0000000000017813
45. Zhang D, Wang K, Zheng J, Wu J, Duan X, Ni M, et al. Comparative Efficacy and Safety of Chinese Herbal Injections Combined With Transcatheter Hepatic Arterial Chemoembolization in Treatment of Liver Cancer: A Bayesian Network Meta-Analysis. J Tradit Chin Med (2020) 40:167–87.
46. Kuo YT, Chang TT, Muo CH, Wu MY, Sun MF, Yeh CC, et al. Use of Complementary Traditional Chinese Medicines by Adult Cancer Patients in Taiwan: A Nationwide Population-Based Study. Integr Cancer Ther (2018) 17:531–41. doi: 10.1177/1534735417716302
47. Chen Q, Shu C, Laurence AD, Chen Y, Peng BG, Zhen ZJ, et al. Effect of Huaier Granule on Recurrence After Curative Resection of HCC: A Multicentre, Randomised Clinical Trial. Gut (2018) 67:2006–16. doi: 10.1136/gutjnl-2018-315983
48. Wu GL, Zhang L, Li TY, Chen J, Yu GY, Li JP. Short-Term Effect of Combined Therapy With Jinlong Capsule and Transcatheter Arterial Chemoembolization on Patients With Primary Hepatic Carcinoma and Its Influence on Serum Osteopontin Expression. Chin J Integr Med (2010) 16:109–13. doi: 10.1007/s11655-010-0109-9
49. Fan Y, Ma Z, Zhao L, Wang W, Gao M, Jia X, et al. Anti-Tumor Activities and Mechanisms of Traditional Chinese Medicines Formulas: A Review. BioMed Pharmacother (2020) 132:110820. doi: 10.1016/j.biopha.2020.110820
50. Zhang L, Wang G, Hou W, Li P, Dulin A, Bonkovsky HL. Contemporary Clinical Research of Traditional Chinese Medicines for Chronic Hepatitis B in China: An Analytical Review. Hepatology (2010) 51:690–8. doi: 10.1002/hep.23384
51. Debelle FD, Vanherweghem JL, Nortier JL. Aristolochic Acid Nephropathy: A Worldwide Problem. Kidney Int (2008) 74:158–69. doi: 10.1038/ki.2008.129
52. Grollman AP, Shibutani S, Moriya M, Miller F, Wu L, Moll U, et al. Aristolochic Acid and the Etiology of Endemic (Balkan) Nephropathy. Proc Natl Acad Sci USA (2007) 104:12129–34. doi: 10.1073/pnas.0701248104
53. Stiborová M, Arlt VM, Schmeiser HH. Balkan Endemic Nephropathy: An Update on Its Aetiology. Arch Toxicol (2016) 90:2595–615. doi: 10.1007/s00204-016-1819-3
54. Lu ZN, Luo Q, Zhao LN, Shi Y, Wang N, Wang L, et al. The Mutational Features of Aristolochic Acid-Induced Mouse and Human Liver Cancers. Hepatology (2020) 71:929–42. doi: 10.1002/hep.30863
55. Ng AWT, Poon SL, Huang MN, Lim JQ, Boot A, Yu W, et al. Aristolochic Acids and Their Derivatives Are Widely Implicated in Liver Cancers in Taiwan and Throughout Asia. Sci Transl Med (2017) 9:eaan6446. doi: 10.1126/scitranslmed.aan6446
56. Vandeven N, Nghiem P. Pathogen-Driven Cancers and Emerging Immune Therapeutic Strategies. Cancer Immunol Res (2014) 2:9–14. doi: 10.1158/2326-6066.CIR-13-0179
57. Makarova-Rusher OV, Medina-Echeverz J, Duffy AG, Greten TF. The Yin and Yang of Evasion and Immune Activation in HCC. J Hepatol (2015) 62:1420–9. doi: 10.1016/j.jhep.2015.02.038
58. Lim CJ, Lee YH, Pan L, Lai L, Chua C, Wasser M, et al. Multidimensional Analyses Reveal Distinct Immune Microenvironment in Hepatitis B Virus-Related Hepatocellular Carcinoma. Gut (2019) 68:916–27. doi: 10.1136/gutjnl-2018-316510
59. Yau T, Hsu C, Kim TY, Choo SP, Kang YK, Hou MM, et al. Nivolumab in Advanced Hepatocellular Carcinoma: Sorafenib-Experienced Asian Cohort Analysis. J Hepatol (2019) 71:543–52. doi: 10.1016/j.jhep.2019.05.014
60. Zhu AX, Finn RS, Edeline J, Cattan S, Ogasawara S, Palmer D, et al. Pembrolizumab in Patients With Advanced Hepatocellular Carcinoma Previously Treated With Sorafenib (KEYNOTE-224): A Non-Randomised, Open-Label Phase 2 Trial. Lancet Oncol (2018) 19:940–52. doi: 10.1016/S1470-2045(18)30351-6
61. Li B, Yan C, Zhu J, Chen X, Fu Q, Zhang H, et al. Anti-PD-1/PD-L1 Blockade Immunotherapy Employed in Treating Hepatitis B Virus Infection-Related Advanced Hepatocellular Carcinoma: A Literature Review. Front Immunol (2020) 11:1037. doi: 10.3389/fimmu.2020.01037
62. Liu HJ, Lizotte PH, Du H, Speranza MC, Lam HC, Vaughan S, et al. TSC2-Deficient Tumors Have Evidence of T Cell Exhaustion and Respond to Anti-PD-1/Anti-CTLA-4 Immunotherapy. JCI Insight (2018) 3:e98674. doi: 10.1172/jci.insight.98674
63. Ge Y, Wei F, Du G, Fei G, Li W, Li X, et al. The Association of Sex-Biased ATRX Mutation in Female Gastric Cancer Patients With Enhanced Immunotherapy-Related Anticancer Immunity. BMC Cancer (2021) 21:240. doi: 10.1186/s12885-021-07978-3
64. Rampias T, Karagiannis D, Avgeris M, Polyzos A, Kokkalis A, Kanaki Z, et al. The Lysine-Specific Methyltransferase KMT2C/MLL3 Regulates DNA Repair Components in Cancer. EMBO Rep (2019) 20:e46821. doi: 10.15252/embr.201846821
65. Yang B, Li J, Li F, Zhou H, Shi W, Shi H, et al. Comprehensive Analysis of Age-Related Somatic Mutation Profiles in Chinese Young Lung Adenocarcinoma Patients. Cancer Med (2019) 8:1350–8. doi: 10.1002/cam4.1839
66. Shi Y, Lei Y, Liu L, Zhang S, Wang W, Zhao J, et al. Integration of Comprehensive Genomic Profiling, Tumor Mutational Burden, and PD-L1 Expression to Identify Novel Biomarkers of Immunotherapy in Non-Small Cell Lung Cancer. Cancer Med (2021) 10:2216–31. doi: 10.1002/cam4.3649
67. Pinyol R, Sia D, Llovet JM. Immune Exclusion-Wnt/CTNNB1 Class Predicts Resistance to Immunotherapies in HCC. Clin Cancer Res (2019) 25:2021–3. doi: 10.1158/1078-0432.CCR-18-3778
68. Sangro B, Salem R. Transarterial Chemoembolization and Radioembolization. Semin Liver Dis (2014) 34:435–43. doi: 10.1055/s-0034-1394142
69. Wáng YX, De Baere T, Idée JM, Ballet S. Transcatheter Embolization Therapy in Liver Cancer: An Update of Clinical Evidences. Chin J Cancer Res (2015) 27:96–121. doi: 10.3978/j.issn.1000-9604.2015.03.03
70. Liao J, Xiao J, Zhou Y, Liu Z, Wang C. Effect of Transcatheter Arterial Chemoembolization on Cellular Immune Function and Regulatory T Cells in Patients With Hepatocellular Carcinoma. Mol Med Rep (2015) 12:6065–71. doi: 10.3892/mmr.2015.4171
71. Liao Y, Wang B, Huang ZL, Shi M, Yu XJ, Zheng L, et al. Increased Circulating Th17 Cells After Transarterial Chemoembolization Correlate With Improved Survival in Stage III Hepatocellular Carcinoma: A Prospective Study. PloS One (2013) 8:e60444. doi: 10.1371/journal.pone.0060444
72. Quan Y, Liu JG, Cai YC, Zhang JR. Changes of Immune Function in Liver Cancer Patients After Transcatheter Arterial Chemoembolizaton Combined With Interstitial Therapy. Nan Fang Yi Ke Da Xue Xue Bao (2009) 29:2288–90.
73. Montasser A, Beaufrère A, Cauchy F, Bouattour M, Soubrane O, Albuquerque M, et al. Transarterial Chemoembolisation Enhances Programmed Death-1 and Programmed Death-Ligand 1 Expression in Hepatocellular Carcinoma. Histopathology (2021) 79:36–46. doi: 10.1111/his.14317
74. Ma XL, Qu XD, Yang WJ, Wang BL, Shen MN, Zhou Y, et al. Elevated Soluble Programmed Death-Ligand 1 Levels Indicate Immunosuppression and Poor Prognosis in Hepatocellular Carcinoma Patients Undergoing Transcatheter Arterial Chemoembolization. Clin Chim Acta (2020) 511:67–74. doi: 10.1016/j.cca.2020.09.026
75. Liu J, Wang S, Zhang Y, Fan HT, Lin HS. Traditional Chinese Medicine and Cancer: History, Present Situation, and Development. Thorac Cancer (2015) 6:561–9. doi: 10.1111/1759-7714.12270
76. Han J, Xian Z, Zhang Y, Liu J, Liang A. Systematic Overview of Aristolochic Acids: Nephrotoxicity, Carcinogenicity, and Underlying Mechanisms. Front Pharmacol (2019) 10:648. doi: 10.3389/fphar.2019.00648
77. Zhou Q, Pei J, Poon J, Lau AY, Zhang L, Wang Y, et al. Worldwide Research Trends on Aristolochic Acids (1957-2017): Suggestions for Researchers. PloS One (2019) 14(5):e0216135. doi: 10.1371/journal.pone.0216135
78. Zhang HM, Zhao XH, Sun ZH, Li GC, Liu GC, Sun LR, et al. Recognition of the Toxicity of Aristolochic Acid. J Clin Pharm Ther (2019) 44:157–62. doi: 10.1111/jcpt.12789
79. Samstein RM, Lee CH, Shoushtari AN, Hellmann MD, Shen R, Janjigian YY, et al. Tumor Mutational Load Predicts Survival After Immunotherapy Across Multiple Cancer Types. Nat Genet (2019) 51:202–6. doi: 10.1038/s41588-018-0312-8
80. Hu ZQ, Xin HY, Luo CB, Li J, Zhou ZJ, Zou JX, et al. Associations Among the Mutational Landscape, Immune Microenvironment, and Prognosis in Chinese Patients With Hepatocellular Carcinoma. Cancer Immunol Immunother (2021) 70:377–89. doi: 10.1007/s00262-020-02685-7
81. Dhanasekaran R, Nault JC, Roberts LR, Zucman-Rossi J. Genomic Medicine and Implications for Hepatocellular Carcinoma Prevention and Therapy. Gastroenterology (2019) 156:492–509. doi: 10.1053/j.gastro.2018.11.001
82. Zhao LH, Liu X, Yan HX, Li WY, Zeng X, Yang Y, et al. Genomic and Oncogenic Preference of HBV Integration in Hepatocellular Carcinoma. Nat Commun (2016) 7:12992. doi: 10.1038/ncomms12992
83. Lee SG, Rho HM. Transcriptional Repression of the Human P53 Gene by Hepatitis B Viral X Protein. Oncogene (2000) 19:468–71. doi: 10.1038/sj.onc.1203312
84. Kwon JA, Rho HM. Transcriptional Repression of the Human P53 Gene by Hepatitis B Viral Core Protein (HBc) in Human Liver Cells. Biol Chem (2003) 384:203–12. doi: 10.1515/BC.2003.022
85. Meng MB, Wen QL, Cui YL, She B, Zhang RM. Meta-Analysis: Traditional Chinese Medicine for Improving Immune Response in Patients With Unresectable Hepatocellular Carcinoma After Transcatheter Arterial Chemoembolization. Explore (NY) (2011) 7:37–43. doi: 10.1016/j.explore.2010.10.002
Keywords: hepatocellular carcinoma (HCC), immune checkpoint blockers (ICBs), combination immunotherapy, transcatheter arterial chemoembolization (TACE), traditional Chinese medicines (TCM)
Citation: Wu Y, Lin H, You X, Guo T, Sun T, Xu H and Fu X (2022) Immune Checkpoint Blockade in Chinese Patients With Hepatocellular Carcinoma: Characteristics and Particularity. Front. Oncol. 12:764923. doi: 10.3389/fonc.2022.764923
Received: 08 September 2021; Accepted: 14 February 2022;
Published: 10 March 2022.
Edited by:
Jiang Chen, Zhejiang University, ChinaCopyright © 2022 Wu, Lin, You, Guo, Sun, Xu and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hao Xu, aHh1QGNtdS5lZHUuY24=; Xibo Fu, ZnV4aWJvQHNpbmEuY29t
†These authors have contributed equally to this work and share first authorship
 Yaoqiang Wu1†
Yaoqiang Wu1† Taiyan Guo
Taiyan Guo Xibo Fu
Xibo Fu