- 1Department of Biomedicine and Health Sciences, The Catholic University Liver Research Center, College of Medicine, POSTECH-Catholic Biomedical Engineering Institute, The Catholic University of Korea, Seoul, South Korea
- 2Division of Gastroenterology and Hepatology, Department of Internal Medicine, College of Medicine, Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, South Korea
- 3Department of Computer Science and Engineering, Incheon National University, Incheon, South Korea
The introduction of immune checkpoint inhibitors (ICIs) represents a key shift in the management strategy for patients with hepatocellular carcinoma (HCC). However, there is a paucity of predictive biomarkers that facilitate the identification of patients that would respond to ICI therapy. Although several researchers have attempted to resolve the issue, the data is insufficient to alter daily clinical practice. The use of minimally invasive procedures to obtain patient-derived specimen, such as using blood-based samples, is increasingly preferred. Circulating tumor DNA (ctDNA) can be isolated from the blood of cancer patients, and liquid biopsies can provide sufficient material to enable ongoing monitoring of HCC. This is particularly significant for patients for whom surgery is not indicated, including those with advanced HCC. In this review, we summarize the current state of understanding of blood-based biomarkers for ICI-based therapy in advanced HCC, which is promising despite there is still a long way to go.
Introduction
Hepatocellular carcinoma (HCC) is the most common primary liver cancer and is the sixth most common cancer and the third leading cause of malignancy-associated deaths worldwide (1, 2). HCC primarily occurs after liver cirrhosis, and the most common associated risk factor is chronic hepatitis B virus (HBV) infection; other causes include chronic hepatitis C virus (HCV) infection, alcoholic liver disease, and non-alcoholic fatty liver disease (NAFLD) (3). Liver cancer staging is usually determined by using the 20-year-old Barcelona Clinic Liver Cancer (BCLC) method or its updated versions, and the analysis outcome is used to stratify and allocate HCC patients into appropriate treatment streams (4). According to the BCLC staging system, a considerable number of HCC patients have BCLC stage C HCC, indicating an advanced stage cancer for which curative or locoregional therapies are unsuitable (5, 6). As more than 50% of patients with HCC have a tumor that is too-advanced for curative therapy, HCC represents the second leading cause of death from cancer; with a 3% survival rate at 5 years globally (7). Sorafenib has been used for over ten years as the primary treatment and was the first tyrosine kinase inhibitor (TKI) for patients with advanced HCC. Recently, treatment options for patients with advanced HCC have increased as several novel therapies have gained approval. These include the use of TKIs such as lenvatinib, regorafenib, and cabozantinib and immune-based therapies such as the immune checkpoint inhibitors (ICIs) atezolizumab, nivolumab, and pembrolizumab (8, 9). According to the recent European Association for the Study of the Liver (EASL) guideline, atezolizumab plus bevacizumab or durvalumab plus tremelimumab administration are the preferred first-line treatment in patients with advanced HCC (4, 10, 11).
The liver is characterized by immune tolerance controlled by antigen-presenting cells, which are responsible for the active control of immunogenicity (8). Moreover, during hepatocarcinogenesis, the gradual dysfunction of innate and adaptive immune cells and an increase in the number of immune-regulatory cells contribute to the generation of immunosuppressive tumor microenvironment (TME) (8, 12). M2-polarized tumor-associated macrophages (TAMs), which act as immune suppressors, critically contribute to the immunosuppressive character of the HCC TME (13, 14). Exhausted T cells show upregulated expression of several inhibitory receptors, including programmed cell death protein-1 (PD-1), T cell immunoreceptor with Ig and ITIM domains (TIGIT), T cell immunoglobulin, mucin-domain containing-3 (TIM-3), and lymphocyte activation gene 3 (LAG3), and the effector function of the cells is impaired by transcriptional changes mediated by thymocyte selection-associated HMG BOX (TOX) (15). Blocking such inhibitory receptors with ICIs reinvigorates exhausted T cells and enhances effector function. Over the past ten years, several clinical trials have demonstrated the contribution of ICIs to the improvement of overall survival (OS) of patients with various tumors. Notably, immunotherapies are generally safe and well-tolerated by patients (16); however, under some circumstances, ICI therapy can cause serious adverse events (AEs), resulting in discontinuation and disease hyper-progression in some cases (17). It is critical to identify reliable biomarkers that would facilitate the selection of patients who will be responsive to ICI treatment as well as those likely to suffer serious AEs.
Molecular biomarkers are prevalent in the blood or tissues (18). Several putative biomarkers are being evaluated in clinical trials for ICI therapy against HCC, including programmed death ligand-1 (PD-L1) expression, microsatellite instability (MSI), tumor mutational burden (TMB), DNA damage repair gene alterations, gut microbiome, and various blood biomarkers (16, 19). Among these, markers in blood samples are easily measured and can serve as tools for clinical management, diagnosis, staging, and evaluation of therapeutic response (18). Here, we comprehensively review blood-based biomarkers for the prediction of ICI responses in patients with HCC.
Currently used immune-based treatments for HCC
ICI treatment (nivolumab, pembrolizumab, ipilimumab, tremelimumab, and durvalumab)
Nivolumab, the initial humanized IgG4 monoclonal antibody directed against PD-1, reinvigorates the immune response of the host towards cancer cells through the competitive inhibition of PD-1-dependent signaling (20). In patients with advanced HCC recruited to the phase I/II CheckMate-040 study, nivolumab showed an objective response rate (ORR) and disease control rate (DCR) of 15%–20% and 58%–64%, respectively, with an acceptable safety profile (20). Subsequently, the international phase III randomized controlled trial, CheckMate 495, was conducted to determine the efficacy of nivolumab versus sorafenib as first-line monotherapy in patients with advanced HCC (21). The mean OS for patients treated with nivolumab was similar to that for a cohort administered with sorafenib, i.e., 16.4 vs. 14.7 months (HR, 0.85; p = 0.0752), although the predetermined criterion for significance was not met (HR, 0.84; p = 0.0419). When compared with the sorafenib group, the cohort that received nivolumab had a superior ORR, i.e., 7% vs. 15%. A more favorable toxicity profile was obtained using nivolumab, and grade 3–4 AEs associated with therapy were also fewer, i.e., 22% vs. 49% (21).
After the successful demonstration of the safety and anti-tumor activity of pembrolizumab in patients with advanced HCC in the KEYNOTE-224 study (22), a randomized placebo-controlled phase III trial (KEYNOTE-240) assessed the efficacy and safety of pembrolizumab versus best supportive care compared to the placebo in patients with advanced HCC. However, the enhanced OS and progression-free survival (PFS) did not reach the required significance, i.e., 13.9 vs. 10.6 months (p = 0.0238) and 3.0 vs. 2.0 months (p = 0.0022), respectively, when compared with patients administered placebo in sorafenib progressors (23). Another anti-PD-1 antibody, camrelizumab, was also shown to be effective in patients with unresectable HCC. In a phase 2 study with advanced HCC with prior treatment, camrelizumab administration resulted in a 6-month survival rate and response rate of 74.4% and 14.7%, respectively (24).
The checkpoint molecule CTLA-4 also constrains the immune response by restricting the excessive stimulation of effector T cells (25). The human IgG2 monoclonal antibody tremelimumab binds to CTLA-4, which overrides the B7-CTLA-4-mediated downregulation of the T-cell response in the tumor microenvironment. A phase III trial for tremelimumab in patients with advanced HCC reported an ORR of 17.6%, time to progression (TTP) of 6.48 months, and acceptable AEs (26). Ipilimumab is another anti-CTLA-4 antibody that shows superior anti-cancer activity in combination with other drugs (27). In March 2020, a combination of nivolumab and ipilimumab was approved by the FDA for the treatment of patients with advanced HCC who had earlier received sorafenib, which was based on the results of phase I/II CheckMate-040 cohort 4 data (27).
A phase I/II open-label randomized trial investigating combinatorial treatment using durvalumab (anti-PD-L1 monoclonal antibody) plus single-dose tremelimumab in patients with advanced HCC reported positive results (28). In the study, combined therapy with tremelimumab (high priming, 300 mg) plus durvalumab had the longest median OS of 18.7 months, tremlimumab administration alone had a median OS of 15.1 months, durvalumab alone had a median OS of 13.57 months, and the combination of tremelimumab (75 mg) plus durvalumab had the lowest median OS of 11.30 months (28). In a recent open-label phase 3 trial of tremelimumab plus durvalumab, a regimen termed STRIDE (Single 300mg Tremelimumab Regular Interval Durvalumab) was compared with durvalumab alone or sorafenib, for first-line treatment for unresectable HCC patients, STRIDE resulted in the significant improvement of OS when compared with sorafenib (11). Moreover, in the study, durvalumab monotherapy was not inferior to sorafenib as a first-line treatment for unresectable HCC (11). Overall, a very recently published BCLC treatment guideline for unresectable HCC recommends STRIDE regimen as a first line treatment option (4).
ICI + targeted therapy
Atezolizumab is a humanized IgG1 mAb targeting PD-L1. Bevacizumab, commercially known as Avastin, was one of the first approved angiogenesis inhibitors that were effective in treating breast cancer, non-small-cell lung cancer, cervical cancer, and glioblastoma (29). The pivotal open-label phase III IMbrave150 trial assessed the efficacy of the combined treatment with atezolizumab plus bevacizumab compared to sorafenib therapy as the first-line of treatment in unresectable HCC patients (10). The combination therapy resulted in a significant improvement in the twelve-month OS compared to sorafenib monotherapy (67.2% vs. 54.6%, respectively). Additionally, the median PFS was greater (6.8 months) for the combination therapy relative to sorafenib (4.3 months). The hazard ratio (HR) for disease progression or death was 0.59 (95% CI 0.47–0.76; p < 0.001) (10).
Lenvatinib, a multikinase inhibitor used in the first-line treatment for advanced HCC, depletes immunosuppressive TAMs and reverses T cell exhaustion within the tumor microenvironment (30, 31). These actions may maximize the clinical efficacy of PD-1 antibodies in reinstating antitumor responses. Based on this hypothesis, a multicenter, open-label study including 104 patients with advanced HCC treated with a combination of lenvatinib and pembrolizumab was conducted. The study reported a median OS and PFS of 22 and 9.3 months, respectively, and grade 3 or higher AEs were reported in 67% of study participants (32). However, phase 3 LEAP-002 trial investigating pembrolizumab plus lenvatinib versus lenvatinib monotherapy did not meet its dual primary endpoints of OS and PFS as a first-line treatment for patients with unresectable HCC (33).
The phase III COSMIC-312 study reached the primary endpoint, demonstrating a significant improvement in PFS with cabozantinib plus atezolizumab compared to sorafenib in unresectable treatment-naive HCC patients, although a statistically significant benefit was not proved for OS (34). Median PFS was 6·8 months (99% CI 5.6–8.3) in the combination treatment group versus 4·2 months (2.8–7.0) in the sorafenib group (99% CI 0.44–0.91, p = 0.0012) (34). The improvement in PFS with cabozantinib plus atezolizumab in this study demonstrates that the combination may benefit patients with unresectable HCC (34). Recently, a trial was designed to assess the efficacy of nivolumab in combination with cabozantinib (group A), or nivolumab plus cabozantinib plus ipilimumab (group B), in 71 patients with advanced HCC randomized into two groups for patients that were treated or untreated with sorafenib (35). The disease control rate for groups A and B were 81% and 83%, respectively, and the median PFS was 5.5 and 6.8 months, respectively. Neither arm achieved the median OS. Grade 3/4 AEs were 42% and 71% in groups A and B, respectively (35).
Blood-based biomarkers for immune-based treatment in advanced HCC
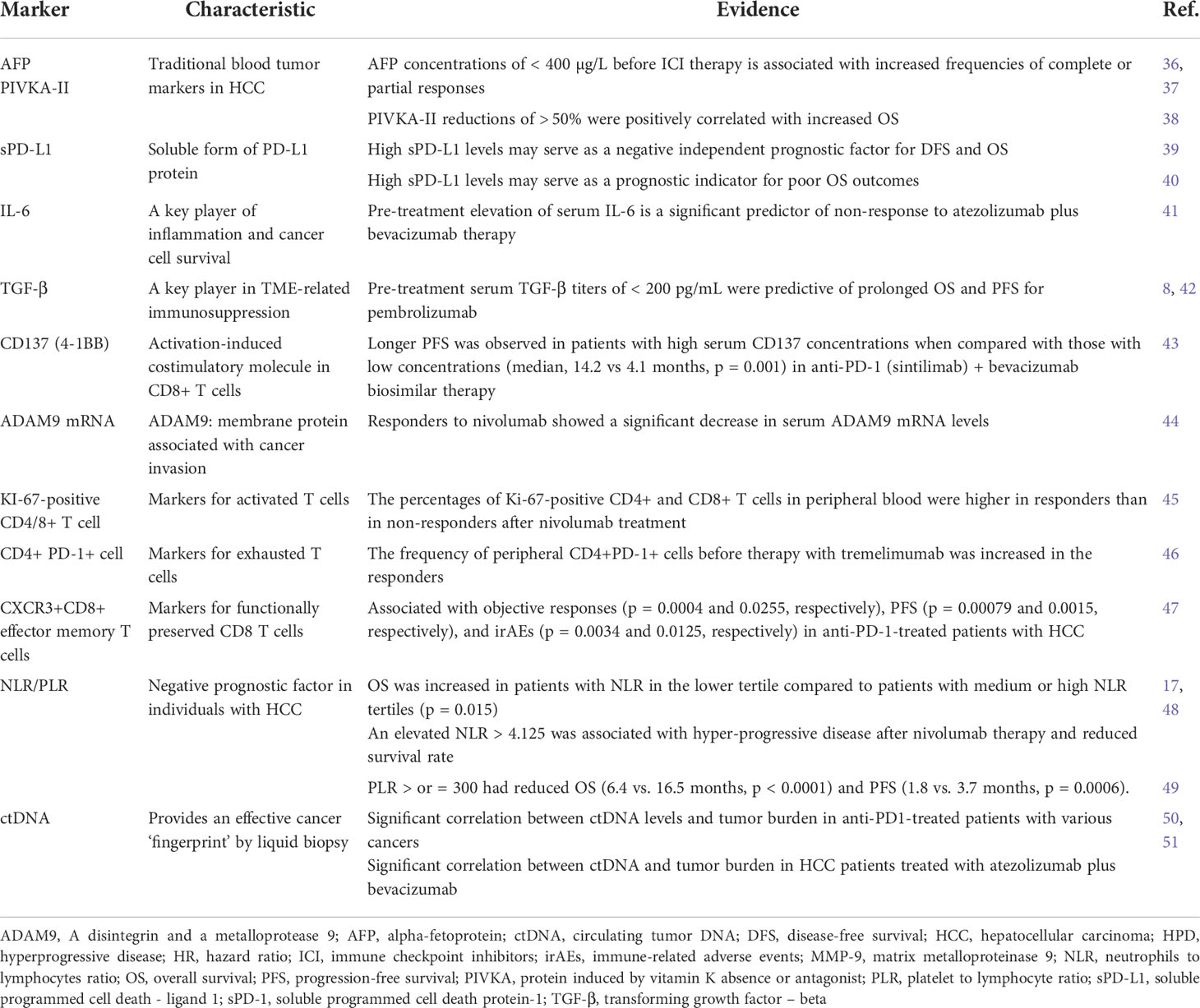
In individuals with HCC, no biomarker has shown reliable accuracy in the prediction of response to ICIs. The extensive variability of HCC lesions in terms of genomic profile and TME raises concerns over the utility of analyses performed on lone tissue specimens. A key merit of circulating biomarkers is that they can be collected easily and measured following immune-based treatment. Recently, the improved survival and response to therapy with nivolumab has been attributed to a small number of biomarkers due to the facilitation of the evaluation of the expression of PD-L1, favorable alpha-fetoprotein (AFP) responses, inflammatory cytokines, and phenotypes of the peripheral serum mononuclear cells. For ICI + targeted therapy, a recent study also showed that pre-existing immunity (high expression of CD274, T-effector signature, and intratumoral CD8+ T cell density) was associated with better clinical outcomes with atezolizumab + bevacizumab therapy (36). In contrast, reduced responses to the therapy were associated with high regulatory T cell to effector T cell ratio and high GPC3 and AFP expression (36). Currently, efforts to identify blood-based biomarkers are on-going for immune-based combination therapies against advanced HCC. Table 1 shows the currently available blood-based biomarkers in immune-based therapies in HCC.
AFP and PIVKA-II
In general, elevated AFP and protein induced by vitamin K absence or antagonist II (PIVKA-II) titers are negative prognostic factors in individuals with HCC (37). AFP concentrations of <400 µg/L before ICI therapy have been associated with increased frequencies of complete or partial responses as the optimal outcomes (52). Early decreases in serum AFP concentrations have been associated with superior responses to ICI therapy in patients with advanced HCC (38). Another report demonstrated a positive correlation between an AFP reduction > 50% or a PIVKA-II reduction > 50%, and ORR of ICI (anti-PD-1), in HCC (48). In addition, AFP and PIVKA-II reductions of > 50% were positively correlated with increased OS (p = 0.003 and 0.006) (48). Nevertheless, data from the CheckMate040 study indicated that even though baseline AFP titers of <400 µg/L reflect prolonged OS compared when compared patients with AFP levels ≥ 400 µg/L, the ORR and DCR for nivolumab therapy remained comparable, irrespective of the APF results (53).
A recent study demonstrated that AFP response at 6 weeks after start of atezolizumab + bevacizumab treatment for advanced HCC is a potential blood biomarker for responses to the therapy (45). The authors derived AFP cutoffs of 75% decrease from baseline at 6 weeks to identify responders (45).
Soluble PD-L1/PD-1
In the CheckMate 040 trial, investigators assessed multiple biomarkers present in the TME to identify putative associations with the higher response rate for nivolumab in patients with advanced HCC (53). Multiple gene expression signatures for inflammation were assessed in fresh and stored tumor samples from both the dose-escalation and -expansion arms of the trial. The results showed that patients who expressed PD-L1 in their tumor samples had survival benefits, and the median OS for patients with detectable (> 1%) expression of PD-L1 was 28.1 months (95% CI 18.2–N/A), whereas that for patients who did not express PD-L1 (< 1% expression) was 16.6 months (95% CI 14.2–20.2, p = 0.032) (53). Notably, although PD-L1 appears to be a reliable indicator of tumor response, the study was limited by several factors. Specifically, the use of an unstandardized cut-off of 1% for PD-L1 expression as a marker of positivity, the temporal and spatial heterogeneity of PD-L1 expression, and the highly complex analytic methods required for analysis may prevent the wide application of the results (14, 39). Therefore, as a single biomarker in HCC, the use of PD-L1 expression as a prognostic marker for response to ICI therapy appears restricted and remains unvalidated. Given the absence of a notable heterogeneity of HCC between tumor samples and between individuals, the appraisal of immunogenicity within a tumor may require a range of biomarkers instead of using PD-L1 expression as a single marker.
Recently, Chinese researchers have evaluated the prognostic impact of sPD-L1, which was a negative independent prognostic factor (disease-free survival (DFS), HR = 2.58, 95% CI 1.14–5.84, p = 0.023; OS, HR 1.77, 95% CI 1.01–3.12, p = 0.048), whereas sPD-1 was a favorable independent prognostic factor (DFS, HR 0.32, 95% CI 0.14–0.74, p = 0.007; OS, HR 0.54, 95% CI 0.30–0.98, p = 0.044) in patients with HCC (40). Another report showed that high sPD-L1 levels may serve as a potential prognostic indicator for poor OS outcomes in patients with HCC (54). In a recent Korean study with an analysis of 72 patient samples, the median sPD-L1 and sPD-1 levels were 25.72 and 341.44 pg/mL, respectively. Further, the sPD-1 levels in patients treated with nivolumab as a second-line therapy changed serially, and a reduction of >50% in sPD-1 levels was observed immediately after nivolumab administration. However, in that study, sPD-1 levels were not associated directly with prognosis in patients with advanced HCC (55).
Cytokines and other serum markers
Interleukin (IL)-6 is produced by various cell types such as tumor cells, stromal cells, and various immune cells in TME. It usually contributes to tumor progression by causing intra- and peritumoral inflammation and promoting angiogenesis (41). A recent study measured 34 plasma proteins in sera from HCC patients treated with atezolizumab plus bevacizumab and identified that elevated plasma IL-6 was a significant predictor of non-response to atezolizumab plus bevacizumab therapy (42). IL8 is a proinflammatory CXC chemokine for neutrophil chemotaxis (41). IL-8 is elevated in various types of malignancies and contributes to tumor angiogenesis and metastasis. A recent study demonstrated that HBV-induced IL-8 promotes HCC metastasis and intrahepatic regulatory T cell accumulation, suggesting the potential negative role of IL-8 in immune-based therapy in HCC (56).
Transforming growth factor-β (TGF-β) is a key player in TME-related immunosuppression and cancer cell circumvention of immune responses (8). The combined delivery of antibodies inhibiting TGF-β and PD-L1 enabled the permeation of T cells into the tumor center and induced potent anti-cancer immune activity (43). In advanced HCC, a robust link exists between TGF-β and exhausted immune signatures (57). Several pertinent serum indicators were assessed in a phase II study which included 29 individuals with unresectable HCC who had undergone treatment with pembrolizumab. Among the serum biomarkers, pre-treatment serum TGF-β titers of <200 pg/mL were predictive of greater OS and PFS (58). Galunisertib, a TGF-β receptor 1 inhibitor, has been evaluated in clinical studies and the results showed an OS of 16.8 months in individuals with advanced HCC in whom pre-therapy AFP titers were < 1.5 × upper normal limit (44).
A recent study further identified soluble levels of CD137 (4-1BB) as one of the blood-based biomarkers for anti-PD-1 (sintilimab) + bevacizumab biosimilar (46). CD137 is an activation-induced costimulatory molecule and its expression on CD8+ tumor-infiltrating lymphocytes reportedly represented a distinct activation state among highly exhausted CD8+ T cells in HCC (59). In addition, a markedly longer PFS was observed in patients with high CD137 concentrations when compared with those with low concentrations (median, 14.2 vs 4.1 months, P = 0.001) (46).
Matrix metalloproteinase 9 (MMP-9) secreted by TAMs has been recently reported to be a potential predictor of immune characteristics and immunotherapeutic responses in HCC (60). ADAMs (a disintegrin and metalloprotease) are membrane proteins containing both protease and adhesion domains and thus may be potentially important in cancer invasion and metastasis (61). The ADAM9 mRNA levels in blood samples derived from patients with advanced HCC revealed that among four patients treated with nivolumab therapy, two exhibited a clinical response and showed a significant decrease in serum ADAM9 mRNA levels, whereas the other two patients showed no response to nivolumab and no change in ADAM9 mRNA levels. Although the sample size was small, the results of the present study suggested that ADAM9 mRNA might serve as a predictive biomarker for clinical responses to immunotherapy (61).
Circulating immune cells
Recently, our group reported that the percentages of Ki-67-positive CD4+ and CD8+ T cells in peripheral blood were higher in responders than in non-responders after nivolumab treatment (39). The frequency of CD4+PD-1+ cells within serum mononuclear cells before therapy with tremelimumab was increased in the responders (62). Decreased serum B cell PD-1 expression at baseline and PD-L1 expression in monocytes following therapy was linked with the disease control in 16 individuals with HCC, who received nivolumab (63).
A recently identified single-cell peripheral immune signature provides promising non-invasive biomarkers for the early detection of HCC and early assessment of anti-PD-1 immunotherapy efficacy in patients with advanced HCC (64). Single-cell analyses using cytometry by time of flight (CyTOF) identified CXCR3+CD8+ effector memory T cells and CD11c+ antigen-presenting cells as being associated with objective responses (p = 0.0004 and 0.0255, respectively), PFS (p = 0.00079 and 0.0015, respectively), and immune-related adverse events (irAEs) (p = 0.0034 and 0.0125, respectively) in anti-PD-1-treated patients with HCC. Type-1 conventional dendritic cells were also identified as the specific antigen-presenting cells associated with the immunotherapy response, whereas two immunosuppressive CD14+ myeloid clusters were linked to reduced irAEs. Another recent report analyzed CXCR3+CD8+ effector memory T cells and showed cell–cell interactions specific to the response to immunotherapy vs. irAEs (65). The anti-PD-1 and anti-TNFR2 combination led to uncouple the efficacy of ICI and irAEs of it, resulting in enhanced response without increased irAEs, in a murine HCC model (65).
NLR/PLR
Regardless of the underlying causes associated with HCC, inflammation remains a major factor, especially because the evolution of hepatic fibrosis to neoplasia may rely on several intra-hepatic proinflammatory cascades (14, 66). In general, adverse survival statistics and the cancer progression is frequently associated with systemic inflammation (67). Neutrophils may exhibit phenotypic plasticity and can exist both under tumor-promoting and tumor-suppressing states. Tumor-associated neutrophils (TANs) contributes to tumor progression by mitigating antitumor immunity (49). The proinflammatory cytokine IL-17 recruits TANs to the TME of HCC (49). TANs also have additional immunosuppressive functions by the recruitment of regulatory T cells and TAMs to the HCC TME (68). TANs and peripheral blood neutrophils produce CCL2 and CCL17 chemokines, and these recruit macrophages into the TME of HCC (68). A recent report suggested that neutrophils hamper the efficacy of ICIs, especially in non-alcoholic steatohepatitis (NASH)-induced HCC (69). The neutrophils to lymphocytes ratio (NLR) may serve as indicators of systemic inflammation, and the ratio is increased in individuals with HCC, owing to relative increases and decreases in neutrophils and lymphocytes, respectively (70). The association between an elevated NLR and adverse clinical outcomes in individuals with HCC has been demonstrated consistently for several treatment options for HCC, e.g. resection, transplantation, radiotherapy, and TACE (47, 71–73).
NLR has shown promise as a prognostic factor in individuals with advanced HCC treated with nivolumab. In contrast to patients with an NLR ≥ 5, an NLR < 5 before and after therapy was associated with enhanced OS of 23 vs. 10 months; (p = 0.004), and 35 vs. 9 months (p < 0.0001), respectively (74). Another study using patient data from the Checkmate 040 trial demonstrated that OS was increased in patients with NLR in the lower tertile compared to patients with medium or high NLR tertiles (p = 0.015) (53). Furthermore, a multi-center study conducted in Korea demonstrated that an elevated NLR > 4.125 was associated with HPD after nivolumab therapy and reduced survival rate (17). Additionally, the baseline and treatment kinetics for the NLR are effective prognostic indicators in nivolumab-treated patients with HCC (75). During treatment, the NLR increased rapidly in patients with hyperprogressive disease (HPD) (75). In addition, a recent study showed that patients treated with various ICIs and ICI-based combination therapies with an NLR ≥ 5 had reduced OS (7.7 vs. 17.6 months, p < 0.0001), reduced PFS (2.1 vs. 3.8 months, p = 0.025), and decreased ORR (12% vs. 22%, p = 0.034), suggesting that systemic inflammation indicated by NLR is an independent negative prognostic factor in patients with HCC undergoing ICI therapy (76).
The platelet to lymphocyte ratio (PLR) is an additional potential prognostic ranking method, with an increased value indicating a relative rise in the platelet count and a fall in lymphocyte numbers. The former occurs frequently in individuals with HCC and is indicative of portal hypertension, as observed in a study of individuals with late-stage HCC receiving ICI therapy (74). Another study showed that patients with PLR > or = 300 had reduced OS (6.4 vs. 16.5 months, p < 0.0001) and PFS (1.8 vs. 3.7 months, p = 0.0006). In that study, NLR emerged as an independent prognostic factor for OS in univariate and multivariate analysis (HR 1.95, p < 0.001; HR 1.73, p = 0.002, respectively) and the PLR remained an independent prognostic factor for both OS and PFS in multivariate analysis (HR 1.60, p = 0.020; HR 1.99, p = 0.021) (76).
The prognostic nutritional index (PNI) is an immune-nutritional indicator and is calculated from the serum albumin (ALB) level and the peripheral blood and lymphocyte (LYM) count (77). A recent study defined the inflammation‐immunity‐nutrition score (IINS), which was simply based on highly sensitive C-reactive protein (hsCRP), LYM, and ALB (50). HCC Patients with low IINS had longer OS and PFS in response to anti-PD-1, suggesting that IINS may serve as an independent prognostic factor for HCC patients treated with anti‐PD‐1 therapy (51).
Although these preliminary observations hold promise, the inflammatory condition inexorably oscillates during pathological evolution and advance, and therefore the NLR and PLR will change based on the timing of specimen acquisition (67). Generally, these relationships require verification before their implementation in clinical practice through additional analysis in individuals with HCC.
Circulating tumor DNAs
Recently, liquid biopsy potentially offers a non-invasive tool for monitoring and diagnosis for cancer patients. The application of the method has been encouraging for early diagnosis, determination of residual disease, and decision-making to facilitate systemic treatment for HCC (78). Regarding the choice of liquid biopsy analytes that may be used in HCC, circulating tumor DNA (ctDNA) has made an invaluable contribution to the prognosis and monitoring of disease (79). Cell-free DNA (cfDNA) contains only a small proportion of ctDNA, which demands the application of highly sensitive and reliable methods of detection. Point mutations are determined by either droplet digital PCR (ddPCR) or by NGS-based sequencing (79). Subsequent to tumor cell apoptosis and necrosis, ctDNA can be found in the blood stream of cancer patients (80) and provides an effective cancer ‘fingerprint’ as it has the tumor’s molecular characteristics. ctDNA can be differentiated from normal circulating DNA using various markers, including mutation signatures (80, 81) and epigenetic alterations (82). The variation in the concentration of ctDNA in the blood provides a quantitative measure, whereas assessment of gene mutations, changes in DNA copy number, and methylation profiles provide a qualitative assessment of the disease condition. In some situations, ctDNA analysis may help identify mutations that were not obtained from a single tumor biopsy (83). Both genomic and epigenetic biomarker modifications in HCC are important factors to consider in recurrence monitoring and precision oncology (84). The results highlight the value of incorporating ctDNA analysis for the diagnosis and prognosis of patients with HCC. Our recent study using targeted NGS technique identified at least one pathogenic variant of two major HCC driver genes (TP53 and CTNNB1), including 16 variants of TP53 and nine variants of CTNNB1 in 65% HCC patients (13/20) (81).
To relate ctDNA to immunotherapy for cancers, a recent study demonstrated that significant correlation between ctDNA levels and tumor burden in anti-PD1-treated patients with various cancers (85). From the patients enrolled in the phase 1b clinical trial of atezolizumab plus bevacizumab, researchers were able to identify a statistically significant correlation between ctDNA and tumor burden (p < 0.03). Of this sub-cohort, patients who achieved a complete response, partial response, stable disease state, and disease progression, ctDNA was undetectable in 70%, 27%, 9% and 0% of these groups, respectively. Furthermore, in cases where ctDNA was not detectable during their treatment period, the patients thereafter experienced a longer PFS (86). Another very recent study using patient cohort treated with camrelizumab plus apatinib demonstrated that patients who were ctDNA positive after adjuvant therapy presented a trend of shorter RFS than those who were ctDNA negative (87). The role of methylated ctDNA in predicting immunotherapy responses is studied in other cancer types such as colorectal cancer (CRC). For example, in four case studies of methylated SEPTIN9 gene (mSEPT9) as a marker of response to immunotherapy in metastatic CRC on four patients, the marker shows that a decrease in ctDNA levels is indicative of a tumor response to immunotherapy while an increase in ctDNA levels corresponds to tumor progression in response to immunotherapy (88, 89). A similar study that focuses on HCC, however, has yet to be found. Another study that looked at predicting immunotherapy responses in HCC but with a methylated RNA molecule (SNRPC) instead, showed a similar pattern in that high-SNRPC groups showed no response to anti-PD1 therapy while low-SNRPC groups showed more patients responding to immune checkpoint inhibitor therapy (90).
TMB, an emergent determinant of immunotherapy responses, is a measure of the total number of somatic non-synonymous mutations per mega-base in the tumor, and its levels between ctDNA and tumor tissues were found to be consistent. Consequently, analysis of blood samples for TMB prior to immunotherapy in advanced primary liver cancer can be beneficial in predicting the responses (91). However, a recent study using 121 HCC blood samples found that mutational analysis ctDNA was associated with a response to systemic TKI treatment, not with ICI treatment (80).
Limitations and future perspectives
Currently, blood-based biomarkers are newly identified and validated in immune-based treatments for the various cancer types, although the researches have been mostly focusing on immunogenic tumors such as malignant melanoma or lung cancer for which ICIs are being most actively used. Hopefully, soon, blood-based biomarkers including ctDNA may be approved for predicting of responses to ICIs in these types of immunogenic cancers. However, because each type of cancer has its own immune TME and cytokine milieu, a more complex blood-based biomarker discovery may be needed for other types of heterogeneous tumors. Although several studies have been conducted to identify predictive biomarkers to enable the stratification of patients who could benefit from ICI treatment in HCC, few have been prospectively validated and none have resulted in the rewriting of current clinical guidelines or entered clinical practice. Here, we have summarized the progress of immunotherapies for HCC in recent years, with a particular emphasis on predictive biomarkers. However, as immunotherapy development for HCC is still in its infancy, basic research and clinical trials exploring the predictive efficacy of immunotherapeutic biomarkers are still limited, and it is not yet possible to determine which biomarker(s) can effectively predict the efficacy of immunotherapy. Although evaluation of human tissues using various technologies is now routine for the derivation of biomarkers, the utility of straightforward instruments to obtain prognostic data, and which are easily accessible from general blood samples should not be discounted, as they may represent a simpler and more widely available option in daily clinical settings. To address the issue of low concentrations of biomarkers in blood, platforms such as the SomaScan, are able to measure ~7000 proteins in a drop of serum simultaneously, leading the way for novel protein biomarker discoveries (92). One more thing to consider is irAEs. A recent report demonstrated that development of low-grade irAEs was associated with favorable responses for HCC patients treated with ICIs (93). Because there are no reliable biomarkers for irAEs in HCC either, clinicians should be vigilant for detection of irAEs when treating HCC patients with ICIs or combination therapy.
Regardless of the potential value of using ctDNA as a biomarker for diagnosis and treatment responses, there are several limitations associated with its current use. Specifically, in the early stages of tumorigenesis, the levels of ctDNA in the blood are extremely low, which can hinder the early diagnosis of HCC. Further, there is currently no standardized methodology associated with sample collection, preparation, and data analysis. The current method cannot adequately capture spatial tumor heterogeneity, which is indicative of clonal differences within or across tumor metastases (94–96). To resolve these issues, a combinatorial and/or multiparametric process is required to enhance the sensitivity and specificity of using ctDNA as a putative HCC biomarker. The use of blood-based biomarkers including ctDNA to determine the efficacy of immunotherapy against HCC necessitates additional, well-controlled clinical trials, so that the value and clinical relevance of such research endeavors can be realized.
Conclusion
Recent advances in research techniques, such as NGS, scRNA sequencing, and artificial intelligence, should facilitate a more comprehensive understanding of the various com-ponents of the TME and their interactions in HCC. Moreover, recent unsatisfactory out-comes in immune-based treatment in advanced HCC urges clinicians to identify blood-based biomarkers for favorable responses to such treatments. Future research should focus on the identification of blood-based protein and cell-free nucleic acid biomarkers for immune-based therapy in HCC.
Author contributions
Conceptualization, PS and JA; methodology, PS; data curation, PS; writing—original draft preparation, IL, PR, and MK; writing—review and editing, PS and JA; supervision, JA and SY; project administration, PS, JA and SY; funding acquisition, PS and JA; All authors have read and agreed to the published version of the manuscript.
Funding
The Basic Science Research Program is supported by the Basic Science Research Program through an NRF grant funded by the Ministry of Science and ICT (NRF-2019R1A2C3005212 to JA). Research Fund of Seoul St. Mary’s Hospital of The Catholic University of Korea (to PS).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sangro B, Sarobe P, Hervas-Stubbs S, Melero I. Advances in immunotherapy for hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol (2021) 18(8):525–43. doi: 10.1038/s41575-021-00438-0
2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2021) 71(3):209–49. doi: 10.3322/caac.21660
3. Chon YE, Jeong SW, Jun DW. Hepatocellular carcinoma statistics in South Korea. Clin Mol Hepatol (2021) 27(3):512–4. doi: 10.3350/cmh.2021.0171
4. Reig M, Forner A, Rimola J, Ferrer-Fabrega J, Burrel M, Garcia-Criado A, et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J Hepatol (2022) 76(3):681–93. doi: 10.1016/j.jhep.2021.11.018
5. Ogasawara S, Ooka Y, Koroki K, Maruta S, Kanzaki H, Kanayama K, et al. Switching to systemic therapy after locoregional treatment failure: Definition and best timing. Clin Mol Hepatol (2020) 26(2):155–62. doi: 10.3350/cmh.2019.0021n
6. Chon YE, Park SY, Hong HP, Son D, Lee J, Yoon E, et al. Hepatocellular carcinoma incidence is decreasing in Korea but increasing in the very elderly. Clin Mol Hepatol (2022). doi: 10.3350/cmh.2021.0395
7. McGlynn KA, Petrick JL, El-Serag HB. Epidemiology of hepatocellular carcinoma. Hepatology (2021) 73 Suppl 1:4–13. doi: 10.1002/hep.31288
8. Sung PS. Crosstalk between tumor-associated macrophages and neighboring cells in hepatocellular carcinoma. Clin Mol Hepatol (2021) 28(3):333–50. doi: 10.3350/cmh.2021.0308
9. Lee CH, Lee YB, Kim MA, Jang H, Oh H, Kim SW, et al. Effectiveness of nivolumab versus regorafenib in hepatocellular carcinoma patients who failed sorafenib treatment. Clin Mol Hepatol (2020) 26(3):328–39. doi: 10.3350/cmh.2019.0049n
10. Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med (2020) 382(20):1894–905. doi: 10.1056/NEJMoa1915745
11. Abou-Alfa GK, Lau G, Kudo M, Chan SL, Kelley RK, Furuse J, et al. Tremelimumab plus durvalumab in unresectable hepatocellular carcinoma. NEJM Evidence (2022) 1(8). doi: 10.1056/EVIDoa2100070
12. Cancer Genome Atlas Research Network. Electronic address wbe, cancer genome atlas research n. comprehensive and integrative genomic characterization of hepatocellular carcinoma. Cell (2017) 169(7):1327–41.e23. doi: 10.1016/j.cell.2017.05.046
13. Ma R-Y, Black A, Qian B-Z. Macrophage diversity in cancer revisited in the era of single-cell omics. Trends Immunol (2022) 43(7):546–63. doi: 10.1016/j.it.2022.04.008
14. Sung PS, Park DJ, Roh PR, Mun KD, Cho SW, Lee GW, et al. Intrahepatic inflammatory IgA(+)PD-L1(high) monocytes in hepatocellular carcinoma development and immunotherapy. J Immunother Cancer (2022) 10(5):e003618. doi: 10.1136/jitc-2021-003618
15. Wang X, He Q, Shen H, Xia A, Tian W, Yu W, et al. TOX promotes the exhaustion of antitumor CD8(+) T cells by preventing PD1 degradation in hepatocellular carcinoma. J Hepatol (2019) 71(4):731–41. doi: 10.1016/j.jhep.2019.05.015
16. Machairas N, Tsilimigras DI, Pawlik TM. Current landscape of immune checkpoint inhibitor therapy for hepatocellular carcinoma. Cancers (Basel) (2022) 14(8):2018. doi: 10.3390/cancers14082018
17. Kim CG, Kim C, Yoon SE, Kim KH, Choi SJ, Kang B, et al. Hyperprogressive disease during PD-1 blockade in patients with advanced hepatocellular carcinoma. J Hepatol (2021) 74(2):350–9. doi: 10.1016/j.jhep.2020.08.010
18. Oloomi M, Moazzezy N, Bouzari S. Comparing blood versus tissue-based biomarkers expression in breast cancer patients. Heliyon (2020) 6(4):e03728. doi: 10.1016/j.heliyon.2020.e03728
19. Llovet JM, Pinyol R, Kelley RK, El-Khoueiry A, Reeves HL, Wang XW, et al. Molecular pathogenesis and systemic therapies for hepatocellular carcinoma. Nat Cancer (2022) 3(4):386–401. doi: 10.1038/s43018-022-00357-2
20. El-Khoueiry AB, Sangro B, Yau T, Crocenzi TS, Kudo M, Hsu C, et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet (2017) 389(10088):2492–502. doi: 10.1016/S0140-6736(17)31046-2
21. Yau T, Park JW, Finn RS, Cheng AL, Mathurin P, Edeline J, et al. Nivolumab versus sorafenib in advanced hepatocellular carcinoma (CheckMate 459): A randomised, multicentre, open-label, phase 3 trial. Lancet Oncol (2022) 23(1):77–90. doi: 10.1016/S1470-2045(21)00604-5
22. Zhu AX, Finn RS, Edeline J, Cattan S, Ogasawara S, Palmer D, et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): A non-randomised, open-label phase 2 trial. Lancet Oncol (2018) 19(7):940–52. doi: 10.1016/S1470-2045(18)30351-6
23. Finn RS, Ryoo BY, Merle P, Kudo M, Bouattour M, Lim HY, et al. Pembrolizumab as second-line therapy in patients with advanced hepatocellular carcinoma in KEYNOTE-240: A randomized, double-blind, phase III trial. J Clin Oncol (2020) 38(3):193–202. doi: 10.1200/JCO.19.01307
24. Qin S, Ren Z, Meng Z, Chen Z, Chai X, Xiong J, et al. Camrelizumab in patients with previously treated advanced hepatocellular carcinoma: A multicentre, open-label, parallel-group, randomised, phase 2 trial. Lancet Oncol (2020) 21(4):571–80. doi: 10.1016/S1470-2045(20)30011-5
25. Baretti M, Kim AK, Anders RA. Expanding the immunotherapy roadmap for hepatocellular carcinoma. Cancer Cell (2022) 40(3):252–4. doi: 10.1016/j.ccell.2022.02.017
26. Sangro B, Gomez-Martin C, de la Mata M, Inarrairaegui M, Garralda E, Barrera P, et al. A clinical trial of CTLA-4 blockade with tremelimumab in patients with hepatocellular carcinoma and chronic hepatitis c. J Hepatol (2013) 59(1):81–8. doi: 10.1016/j.jhep.2013.02.022
27. Tsang J, Wong JSL, Kwok GGW, Li BCW, Leung R, Chiu J, et al. Nivolumab + ipilimumab for patients with hepatocellular carcinoma previously treated with sorafenib. Expert Rev Gastroenterol Hepatol (2021) 15(6):589–98. doi: 10.1080/17474124.2021.1899808
28. Kelley RK, Sangro B, Harris W, Ikeda M, Okusaka T, Kang YK, et al. Safety, efficacy, and pharmacodynamics of tremelimumab plus durvalumab for patients with unresectable hepatocellular carcinoma: Randomized expansion of a phase I/II study. J Clin Oncol (2021) 39(27):2991–3001. doi: 10.1200/JCO.20.03555
29. Liu JKH, Irvine AF, Jones RL, Samson A. Immunotherapies for hepatocellular carcinoma. Cancer Med (2022) 11(3):571–91. doi: 10.1002/cam4.4468
30. Sung PS, Cho SW, Lee J, Yang H, Jang JW, Bae SH, et al. Infiltration of T cells and programmed cell death ligand 1-expressing macrophages as a potential predictor of lenvatinib response in hepatocellular carcinoma. J Liver Cancer (2020) 20(2):128–34. doi: 10.17998/jlc.20.2.128
31. Lee J, Sung PS, Yang H, Lee SK, Nam HC, Yoo SH, et al. A real-world comparative analysis of lenvatinib and sorafenib as a salvage therapy for transarterial treatments in unresectable HCC. J Clin Med (2020) 9(12):4121. doi: 10.3390/jcm9124121
32. Finn RS, Ikeda M, Zhu AX, Sung MW, Baron AD, Kudo M, et al. Phase ib study of lenvatinib plus pembrolizumab in patients with unresectable hepatocellular carcinoma. J Clin Oncol (2020) 38(26):2960–70. doi: 10.1200/JCO.20.00808
33. Merck And eisai provide update on phase 3 LEAP-002 trial evaluating KEYTRUDA® (pembrolizumab) plus LENVIMA® (lenvatinib) versus LENVIMA monotherapy in patients with unresectable hepatocellular carcinoma . Available at: https://www.merck.com/news/merck-and-eisai-provide-update-on-phase-3-leap-002-trial-evaluating-keytruda-pembrolizumab-plus-lenvima-lenvatinib-versus-lenvima-monotherapy-in-patients-with-unresectable-hepatocellul/.
34. Kelley RK, Rimassa L, Cheng A-L, Kaseb A, Qin S, Zhu AX, et al. Cabozantinib plus atezolizumab versus sorafenib for advanced hepatocellular carcinoma (COSMIC-312): A multicentre, open-label, randomised, phase 3 trial. Lancet Oncol (2022) 23(8):995–1008. doi: 10.1016/S1470-2045(22)00326-6
35. Thomas Yau VZ, Santoro A, Acosta-Rivera M, Choo SuP, Matilla A, He AR, et al. Nivolumab (NIVO) + ipilimumab (IPI) + cabozantinib (CABO) combination therapy in patients (pts) with advanced hepatocellular carcinoma (aHCC): Results from CheckMate 040. J Clin Oncol (2020) 38:478. doi: 10.1200/JCO.2020.38.4_suppl.478
36. Zhu AX, Abbas AR, de Galarreta MR, Guan Y, Lu S, Koeppen H, et al. Molecular correlates of clinical response and resistance to atezolizumab in combination with bevacizumab in advanced hepatocellular carcinoma. Nat Med (2022) 28(8):1599–611. doi: 10.1038/s41591-022-01868-2
37. Sung PS, Yang K, Bae SH, Oh JS, Chun HJ, Nam HC, et al. Reduction of intrahepatic tumour by hepatic arterial infusion chemotherapy prolongs survival in hepatocellular carcinoma. Anticancer Res (2019) 39(7):3909–16. doi: 10.21873/anticanres.13542
38. Shao YY, Liu TH, Hsu C, Lu LC, Shen YC, Lin ZZ, et al. Early alpha-foetoprotein response associated with treatment efficacy of immune checkpoint inhibitors for advanced hepatocellular carcinoma. Liver Int (2019) 39(11):2184–9. doi: 10.1111/liv.14210
39. Park DJ, Sung PS, Lee GW, Cho S, Kim SM, Kang BY, et al. Preferential expression of programmed death ligand 1 protein in tumor-associated macrophages and its potential role in immunotherapy for hepatocellular carcinoma. Int J Mol Sci (2021) 22(9):4710. doi: 10.3390/ijms22094710
40. Chang B, Huang T, Wei H, Shen L, Zhu D, He W, et al. The correlation and prognostic value of serum levels of soluble programmed death protein 1 (sPD-1) and soluble programmed death-ligand 1 (sPD-L1) in patients with hepatocellular carcinoma. Cancer Immunol Immunother (2019) 68(3):353–63. doi: 10.1007/s00262-018-2271-4
41. An HJ, Chon HJ, Kim C. Peripheral blood-based biomarkers for immune checkpoint inhibitors. Int J Mol Sci (2021) 22(17):9414. doi: 10.3390/ijms22179414
42. Myojin Y, Kodama T, Sakamori R, Maesaka K, Matsumae T, Sawai Y, et al. Interleukin-6 is a circulating prognostic biomarker for hepatocellular carcinoma patients treated with combined immunotherapy. Cancers (Basel) (2022) 14(4):883. doi: 10.3390/cancers14040883
43. Mariathasan S, Turley SJ, Nickles D, Castiglioni A, Yuen K, Wang Y, et al. TGFbeta attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature (2018) 554(7693):544–8. doi: 10.1038/nature25501
44. Kelley RK, Gane E, Assenat E, Siebler J, Galle PR, Merle P, et al. A phase 2 study of galunisertib (TGF-beta1 receptor type I inhibitor) and sorafenib in patients with advanced hepatocellular carcinoma. Clin Transl Gastroenterol (2019) 10(7):e00056. doi: 10.14309/ctg.0000000000000056
45. Zhu AX, Dayyani F, Yen CJ, Ren Z, Bai Y, Meng Z, et al. Alpha-fetoprotein as a potential surrogate biomarker for atezolizumab + bevacizumab treatment of hepatocellular carcinoma. Clin Cancer Res (2022) 28(16):3537–45. doi: 10.1158/1078-0432.CCR-21-3275
46. Zhang W, Gong C, Peng X, Bi X, Sun Y, Zhou J, et al. Serum concentration of CD137 and tumor infiltration by M1 macrophages predict the response to sintilimab plus bevacizumab biosimilar in advanced hepatocellular carcinoma patients. Clin Cancer Res (2022) 28(16):3499–508. doi: 10.1158/1078-0432.CCR-21-3972
47. Chan SL, Chan AW, Chan AK, Jian P, Mo F, Chan CM, et al. Systematic evaluation of circulating inflammatory markers for hepatocellular carcinoma. Liver Int (2017) 37(2):280–9. doi: 10.1111/liv.13218
48. Sun X, Mei J, Lin W, Yang Z, Peng W, Chen J, et al. Reductions in AFP and PIVKA-II can predict the efficiency of anti-PD-1 immunotherapy in HCC patients. BMC Cancer (2021) 21(1):775. doi: 10.1186/s12885-021-08428-w
49. Arvanitakis K, Mitroulis I, Germanidis G. Tumor-associated neutrophils in hepatocellular carcinoma pathogenesis, prognosis, and therapy. Cancers (Basel) (2021) 13(12):2899. doi: 10.3390/cancers13122899
50. Li XY, Yao S, He YT, Ke SQ, Ma YF, Lu P, et al. Inflammation-Immunity-Nutrition score: A novel prognostic score for patients with resectable colorectal cancer. J Inflammation Res (2021) 14:4577–88. doi: 10.2147/JIR.S322260
51. Zhang Z, Liang Y, Zhong D, Dai Z, Shang J, Lai C, et al. Prognostic value of inflammation-immunity-nutrition score in patients with hepatocellular carcinoma treated with anti-PD-1 therapy. J Clin Lab Anal (2022) 36(5):e24336. doi: 10.1002/jcla.24336
52. Spahn S, Roessler D, Pompilia R, Gabernet G, Gladstone BP, Horger M, et al. Clinical and genetic tumor characteristics of responding and non-responding patients to PD-1 inhibition in hepatocellular carcinoma. Cancers (Basel) (2020) 12(12):3830. doi: 10.3390/cancers12123830
53. Sangro B, Melero I, Wadhawan S, Finn RS, Abou-Alfa GK, Cheng AL, et al. Association of inflammatory biomarkers with clinical outcomes in nivolumab-treated patients with advanced hepatocellular carcinoma. J Hepatol (2020) 73(6):1460–9. doi: 10.1016/j.jhep.2020.07.026
54. Finkelmeier F, Canli O, Tal A, Pleli T, Trojan J, Schmidt M, et al. High levels of the soluble programmed death-ligand (sPD-L1) identify hepatocellular carcinoma patients with a poor prognosis. Eur J Cancer (2016) 59:152–9. doi: 10.1016/j.ejca.2016.03.002
55. Lee HW, Cho KJ, Shin SY, Kim HY, Lee EJ, Kim BK, et al. Serum PD-1 levels change with immunotherapy response but do not predict prognosis in patients with hepatocellular carcinoma. J Liver Cancer (2019) 19(2):108–16. doi: 10.17998/jlc.19.2.108
56. Zhang C, Gao Y, Du C, Markowitz GJ, Fu J, Zhang Z, et al. Hepatitis b-induced IL8 promotes hepatocellular carcinoma venous metastasis and intrahepatic treg accumulation. Cancer Res (2021) 81(9):2386–98. doi: 10.1158/0008-5472.CAN-20-3453
57. Chen J, Zaidi S, Rao S, Chen JS, Phan L, Farci P, et al. Analysis of genomes and transcriptomes of hepatocellular carcinomas identifies mutations and gene expression changes in the transforming growth factor-beta pathway. Gastroenterology (2018) 154(1):195–210. doi: 10.1053/j.gastro.2017.09.007
58. Feun LG, Li YY, Wu C, Wangpaichitr M, Jones PD, Richman SP, et al. Phase 2 study of pembrolizumab and circulating biomarkers to predict anticancer response in advanced, unresectable hepatocellular carcinoma. Cancer (2019) 125(20):3603–14. doi: 10.1002/cncr.32339
59. Kim HD, Park S, Jeong S, Lee YJ, Lee H, Kim CG, et al. 4-1BB delineates distinct activation status of exhausted tumor-infiltrating CD8(+) T cells in hepatocellular carcinoma. Hepatology (2020) 71(3):955–71. doi: 10.1002/hep.30881
60. Ding H, Hu H, Tian F, Liang H. A dual immune signature of CD8+ T cells and MMP9 improves the survival of patients with hepatocellular carcinoma. Biosci Rep (2021) 41(3):BSR20204219. doi: 10.1042/BSR20204219
61. Oh S, Park Y, Lee HJ, Lee J, Lee SH, Baek YS, et al. A disintegrin and metalloproteinase 9 (ADAM9) in advanced hepatocellular carcinoma and their role as a biomarker during hepatocellular carcinoma immunotherapy. Cancers (Basel) (2020) 12(3):745. doi: 10.3390/cancers12030745
62. Agdashian D, ElGindi M, Xie C, Sandhu M, Pratt D, Kleiner DE, et al. The effect of anti-CTLA4 treatment on peripheral and intra-tumoral T cells in patients with hepatocellular carcinoma. Cancer Immunol Immunother (2019) 68(4):599–608. doi: 10.1007/s00262-019-02299-8
63. Hung YP, Shao YY, Lee JM, Hsu C, Hsu CH, Yang MH, et al. Potential of circulating immune cells as biomarkers of nivolumab treatment efficacy for advanced hepatocellular carcinoma. J Chin Med Assoc (2021) 84(2):144–50. doi: 10.1097/JCMA.0000000000000477
64. Shi J, Liu J, Tu X, Li B, Tong Z, Wang T, et al. Single-cell immune signature for detecting early-stage HCC and early assessing anti-PD-1 immunotherapy efficacy. J Immunother Cancer (2022) 10(1):e003133. doi: 10.1136/jitc-2021-003133
65. Chuah S, Lee J, Song Y, Kim HD, Wasser M, Kaya NA, et al. Uncoupling immune trajectories of response and adverse events from anti-PD-1 immunotherapy in hepatocellular carcinoma. J Hepatol (2022) 77(3):683–94. doi: 10.1016/j.jhep.2022.03.039
66. Sung PS, Kim CM, Cha JH, Park JY, Yu YS, Wang HJ, et al. A unique immune-related gene signature represents advanced liver fibrosis and reveals potential therapeutic targets. Biomedicines (2022) 10(1):180. doi: 10.3390/biomedicines10010180
67. Muhammed A, D’Alessio A, Enica A, Talbot T, Fulgenzi CAM, Nteliopoulos G, et al. Predictive biomarkers of response to immune checkpoint inhibitors in hepatocellular carcinoma. Expert Rev Mol Diagn (2022) 22(3):253–64. doi: 10.1080/14737159.2022.2049244
68. Zhou SL, Zhou ZJ, Hu ZQ, Huang XW, Wang Z, Chen EB, et al. Tumor-associated neutrophils recruit macrophages and T-regulatory cells to promote progression of hepatocellular carcinoma and resistance to sorafenib. Gastroenterology (2016) 150(7):1646–58 e17. doi: 10.1053/j.gastro.2016.02.040
69. Leslie J, Mackey JBG, Jamieson T, Ramon-Gil E, Drake TM, Fercoq F, et al. CXCR2 inhibition enables NASH-HCC immunotherapy. Gut (2022) 71(10):2093–106. doi: 10.1101/2022.02.24.481779
70. Fan Y, Xue H, Zheng H. Systemic therapy for hepatocellular carcinoma: Current updates and outlook. J Hepatocell Carcinoma (2022) 9:233–63. doi: 10.2147/JHC.S358082
71. Son SH, Park EY, Park HH, Kay CS, Jang HS. Pre-radiotherapy neutrophil-to-lymphocyte ratio as an independent prognostic factor in patients with locally advanced hepatocellular carcinoma treated with radiotherapy. Oncotarget (2017) 8(10):16964–71. doi: 10.18632/oncotarget.15209
72. Na GH, Kim DG, Han JH, Kim EY, Lee SH, Hong TH, et al. Inflammatory markers as selection criteria of hepatocellular carcinoma in living-donor liver transplantation. World J Gastroenterol (2014) 20(21):6594–601. doi: 10.3748/wjg.v20.i21.6594
73. Oh BS, Jang JW, Kwon JH, You CR, Chung KW, Kay CS, et al. Prognostic value of c-reactive protein and neutrophil-to-lymphocyte ratio in patients with hepatocellular carcinoma. BMC Cancer (2013) 13:78. doi: 10.1186/1471-2407-13-78
74. Dharmapuri S, Ozbek U, Lin JY, Sung M, Schwartz M, Branch AD, et al. Predictive value of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in advanced hepatocellular carcinoma patients treated with anti-PD-1 therapy. Cancer Med (2020) 9(14):4962–70. doi: 10.1002/cam4.3135
75. Choi WM, Kim JY, Choi J, Lee D, Shim JH, Lim YS, et al. Kinetics of the neutrophil-lymphocyte ratio during PD-1 inhibition as a prognostic factor in advanced hepatocellular carcinoma. Liver Int (2021) 41(9):2189–99. doi: 10.1111/liv.14932
76. Muhammed A, Fulgenzi CAM, Dharmapuri S, Pinter M, Balcar L, Scheiner B, et al. The systemic inflammatory response identifies patients with adverse clinical outcome from immunotherapy in hepatocellular carcinoma. Cancers (Basel) (2021) 14(1):186. doi: 10.3390/cancers14010186
77. Chen W, Zhang M, Chen C, Pang X. Prognostic nutritional index and Neutrophil/Lymphocyte ratio can serve as independent predictors of the prognosis of hepatocellular carcinoma patients receiving targeted therapy. J Oncol (2022) 2022:1389049. doi: 10.1155/2022/1389049
78. von Felden J, Garcia-Lezana T, Schulze K, Losic B, Villanueva A. Liquid biopsy in the clinical management of hepatocellular carcinoma. Gut (2020) 69(11):2025–34. doi: 10.1136/gutjnl-2019-320282
79. Maravelia P, Silva DN, Rovesti G, Chrobok M, Stal P, Lu YC, et al. Liquid biopsy in hepatocellular carcinoma: Opportunities and challenges for immunotherapy. Cancers (Basel) (2021) 13(17):4434. doi: 10.3390/cancers13174334
80. von Felden J, Craig AJ, Garcia-Lezana T, Labgaa I, Haber PK, D’Avola D, et al. Mutations in circulating tumor DNA predict primary resistance to systemic therapies in advanced hepatocellular carcinoma. Oncogene (2021) 40(1):140–51. doi: 10.1038/s41388-020-01519-1
81. Chae H, Sung PS, Choi H, Kwon A, Kang D, Kim Y, et al. Targeted next-generation sequencing of plasma cell-free DNA in Korean patients with hepatocellular carcinoma. Ann Lab Med (2021) 41(2):198–206. doi: 10.3343/alm.2021.41.2.198
82. Xu RH, Wei W, Krawczyk M, Wang W, Luo H, Flagg K, et al. Circulating tumour DNA methylation markers for diagnosis and prognosis of hepatocellular carcinoma. Nat Mater (2017) 16(11):1155–61. doi: 10.1038/nmat4997
83. Pelizzaro F, Cardin R, Penzo B, Pinto E, Vitale A, Cillo U, et al. Liquid biopsy in hepatocellular carcinoma: Where are we now? Cancers (Basel) (2021) 13(9):2274. doi: 10.3390/cancers13092274
84. Cai Z, Chen G, Zeng Y, Dong X, Li Z, Huang Y, et al. Comprehensive liquid profiling of circulating tumor DNA and protein biomarkers in long-term follow-up patients with hepatocellular CarcinomaComprehensive ctDNA profile integration to monitor HCC. Clin Cancer Res (2019) 25(17):5284–94. doi: 10.1158/1078-0432.CCR-18-3477
85. Cabel L, Riva F, Servois V, Livartowski A, Daniel C, Rampanou A, et al. Circulating tumor DNA changes for early monitoring of anti-PD1 immunotherapy: A proof-of-concept study. Ann Oncol (2017) 28(8):1996–2001. doi: 10.1093/annonc/mdx212
86. Hsu C-H, Lu S, Abbas A, Guan Y, Zhu AX, Aleshin A, et al. Longitudinal and personalized detection of circulating tumor DNA (ctDNA) for monitoring efficacy of atezolizumab plus bevacizumab in patients with unresectable hepatocellular carcinoma (HCC). Am Soc Clin Oncol (2020) 38(15):3531. doi: 10.1200/JCO.2020.38.15_suppl.3531
87. Xia Y, Tang W, Qian X, Li X, Cheng F, Wang K, et al. Efficacy and safety of camrelizumab plus apatinib during the perioperative period in resectable hepatocellular carcinoma: A single-arm, open label, phase II clinical trial. J Immunother Cancer (2022) 10(4):e004656. doi: 10.1136/jitc-2022-004656
88. Gong J, Aguirre F, Hazelett D, Alvarez R, Zhou L, Hendifar A, et al. Circulating tumor DNA dynamics and response to immunotherapy in colorectal cancer. Mol Clin Oncol (2022) 16(5):1–6. doi: 10.3892/mco.2022.2533
89. Nassar FJ, Msheik ZS, Nasr RR, Temraz SN. Methylated circulating tumor DNA as a biomarker for colorectal cancer diagnosis, prognosis, and prediction. Clin Epigenetics (2021) 13(1):1–25. doi: 10.1186/s13148-021-01095-5
90. Cai J, Zhou M, Xu J. N6-methyladenosine (m6A) RNA methylation regulator SNRPC is a prognostic biomarker and is correlated with immunotherapy in hepatocellular carcinoma. World J Surg Oncol (2021) 19(1):1–12. doi: 10.1186/s12957-021-02354-8
91. Zhao W, Qiu L, Liu H, Xu Y, Zhan M, Zhang W, et al. Circulating tumor DNA as a potential prognostic and predictive biomarker during interventional therapy of unresectable primary liver cancer. J Gastrointest Oncol (2020) 11(5):1065–77. doi: 10.21037/jgo-20-409
92. Qiao Z, Pan X, Parlayan C, Ojima H, Kondo T. Proteomic study of hepatocellular carcinoma using a novel modified aptamer-based array (SOMAscan™) platform. Biochim Biophys Acta (BBA)-Proteins Proteomics (2017) 1865(4):434–43. doi: 10.1016/j.bbapap.2016.09.011
93. Xu S, Lai R, Zhao Q, Zhao P, Zhao R, Guo Z. Correlation between immune-related adverse events and prognosis in hepatocellular carcinoma patients treated with immune checkpoint inhibitors. Front Immunol (2021) 12:794099. doi: 10.3389/fimmu.2021.794099
94. Zhang Q, Lou Y, Yang J, Wang J, Feng J, Zhao Y, et al. Integrated multiomic analysis reveals comprehensive tumour heterogeneity and novel immunophenotypic classification in hepatocellular carcinomas. Gut (2019) 68(11):2019–31. doi: 10.1136/gutjnl-2019-318912
95. Yang H, Sung PS, Lee J, Yoon SK, Jung ES, Park CS, et al. Heterogenous responses to nivolumab in a single metastatic nodule in hepatocellular carcinoma: role of salvage surgery. Hepatobiliary Surg Nutr (2019) 8(5):569–71. doi: 10.21037/hbsn.2019.08.10
Keywords: hepatocellular carcinoma, immune checkpoint inhibitors, biomarker, circulating tumor DNA, patient outcomes
Citation: Sung PS, Lee IK, Roh PR, Kang MW, Ahn J and Yoon SK (2022) Blood-based biomarkers for immune-based therapy in advanced HCC: Promising but a long way to go. Front. Oncol. 12:1028728. doi: 10.3389/fonc.2022.1028728
Received: 26 August 2022; Accepted: 17 October 2022;
Published: 31 October 2022.
Edited by:
Emilio Francesco Giunta, Università degli Studi della Campania Luigi Vanvitelli, ItalyReviewed by:
Changqing Xie, Clinical Center (NIH), United StatesSu Jong Yu, Seoul National University College of Medicine, South Korea
Copyright © 2022 Sung, Lee, Roh, Kang, Ahn and Yoon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Seung Kew Yoon, yoonsk@catholic.ac.kr; Jaegyoon Ahn, jgahn@inu.ac.kr
†These authors have contributed equally to this work
 Pil Soo Sung
Pil Soo Sung