- Department of Hematology, Oncology, and Clinical Immunology, Heinrich-Heine-University Hospital Duesseldorf, Duesseldorf, Germany
The WHO-category Myelodysplastic/Myeloproliferative neoplasms (MDS/MPNs) recognizes a unique group of clonal myeloid malignancies exhibiting overlapping features of myelodysplastic as well as myeloproliferative neoplasms. The group consists of chronic myelomonocytic leukemia (CMML), atypical chronic myeloid leukemia, BCR-ABL1-negative (aCML), juvenile myelomonocytic leukemia (JMML), myelodysplastic/myeloproliferative neoplasm with ringed sideroblasts and thrombocytosis (MDS/MPN-RS-T), and myelodysplastic/myeloproliferative neoplasms, unclassifiable (MDS/MPN-U). The most frequent entity in this category is CMML, while all other diseases are extremely rare. Thus, only very limited data on the epidemiology of these subgroups exists. An appropriate diagnosis and classification can be challenging since the diagnosis is still largely based on morphologic criteria and myelodysplastic as well as myeloproliferative features can be found in various occurrences. The diseases in this category share several features that are common in this specific WHO-category, but also exhibit specific traits for each disease. This review summarizes published data on epidemiological features and offers a brief overview of the main diagnostic criteria and clinical characteristics of the five MDS/MPN subgroups.
Introduction
The World Health Organization (WHO) recognizes a group of rare clonal hematopoietic malignancies with mixed features of Myelodysplastic Syndrome (MDS) as well as Myeloproliferative Neoplasms (MPNs) (1). These malignancies are placed in a separate WHO-category named myelodysplastic/myeloproliferative neoplasms (MDS/MPN). The group consists of myeloid diseases including chronic myelomonocytic leukemia (CMML), atypical chronic myeloid leukemia, BCR-ABL1-negative (aCML), juvenile myelomonocytic leukemia (JMML), myelodysplastic/myeloproliferative neoplasm with ringed sideroblasts and thrombocytosis (MDS/MPN-RS-T), and myelodysplastic/myeloproliferative neoplasms, unclassifiable (MDS/MPN-U). Diagnosing these diseases can be challenging, as they can exhibit different features of MDS and MPNs. While the simultaneous existence of dysplasia and proliferation is mandatory, other features might be cytopenias, often in coexistence with “cytoses” and organomegaly. “MDS-like” symptoms as a result of ineffective hematopoiesis including fatigue, dyspnea, infections, and bleeding occur in parallel to the more “MPN-like” symptoms resulting from proliferative hematopoiesis, namely night sweats, weight loss, and increased risk of thromboembolic complications. Unfortunately, the morphological features of MDS/MPNs are not specific but can be found in other myeloid malignancies at presentation or as part of disease progression. Diagnostically, there is a considerable overlap between the different MDS/MPNs as well as the different myelodysplastic and myeloproliferative neoplasms. At present, no cytogenetic or molecular genetic abnormalities specific for any of the MDS/MPN subtypes exist. Nevertheless, genetic abnormalities play an important role in excluding a diagnosis of a particular MDS/MPN and some abnormalities might at least help ascertain the correct subtype (2–17).
The existence of disorders with overlapping myelodysplastic and myeloproliferative features has been described years ago. A true recognition and classification of this group of diseases, however, occurred much more recently. In 1976 the French-American-British (FAB) cooperative group introduced a classification and nomenclature of the acute myeloid and lymphoid leukemias (18). Two types of MDS, RAEB and CMML, were presented as an addendum. Then, in 1982, the FAB-group introduced a classification and nomenclature of the MDS (19). CMML was included as one of the 5 subtypes of MDS in this classification system. Only with the introduction of the WHO-classification (20) in 2001 the existence of overlap syndromes between MDS and MPN was formally recognized and CMML was moved into this new founded category of myeloid malignancies. In addition to CMML the new group included aCML, JMML, and MDS/MPN-U. Refractory anemia with ringed sideroblasts associated with marked thrombocytosis (RARS-T) was initially proposed as a provisional entity in the WHO 2001 classification of myeloid neoplasms (20) and only 2016 recognized as a formal subgroup (MDS/MPN-RS-T) of MDS/MPN by the latest version of the WHO-classification (1). Additional entities that have been discussed and might represent separate entities of MDS/MPN in future classifications are MDS with isolated del(5q) and JAK2-V617F mutation and MDS/MPN with isolated isochromosome 17q (21–30).
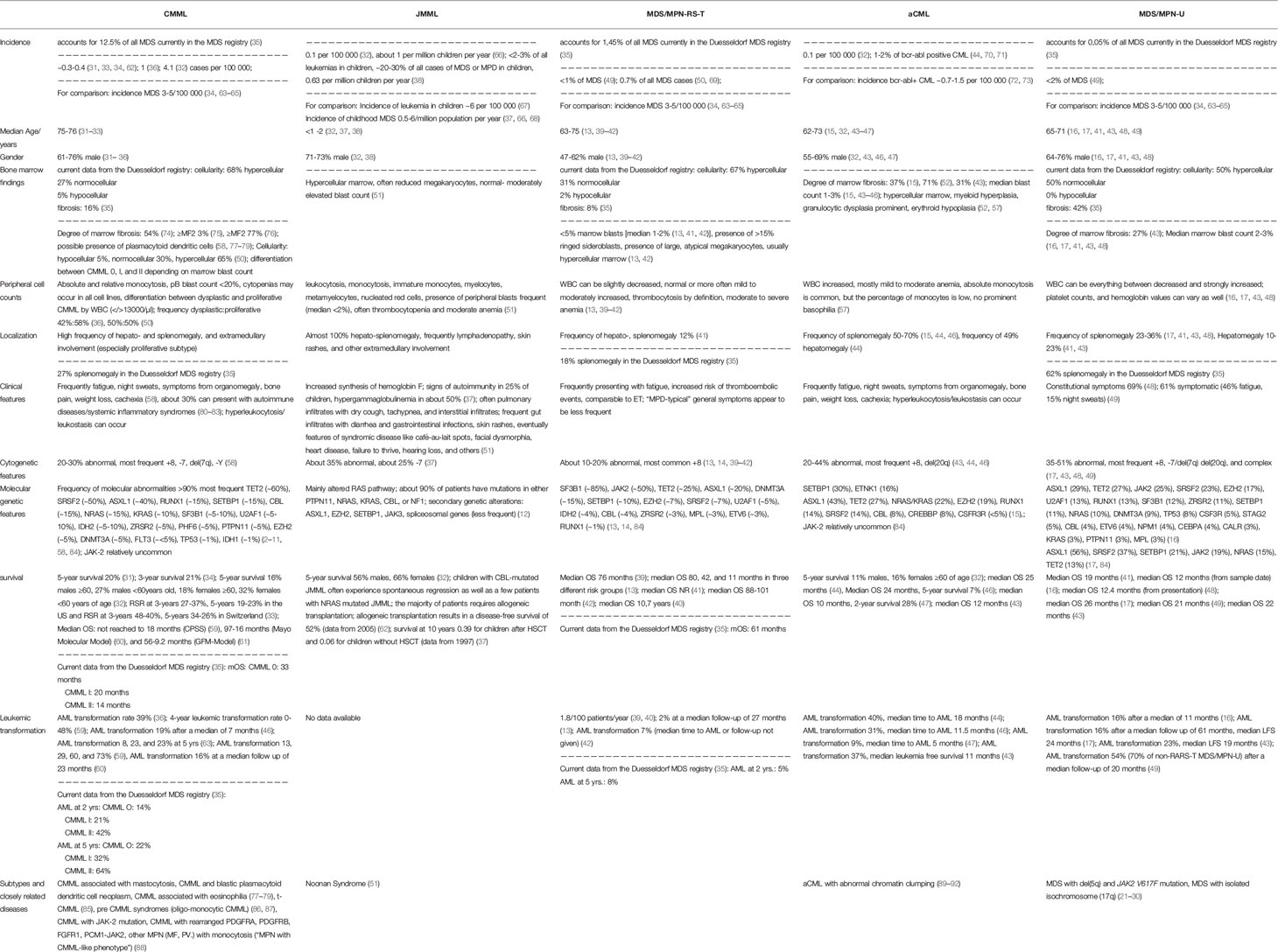
The WHO-category MDS/MPN encompasses three relatively well-defined entities, namely CMML, JMML, and MDS/MPN-RS-T, the diagnostic criteria for which are easy to follow. In contrast, aCML and MDS/MPN-U are less well-defined and their diagnosis largely remains a matter of exclusion of other myeloid neoplasms (1). Main diagnostic criteria of the MDS/MPN subgroups according to WHO 2016 are depicted in Table 1.
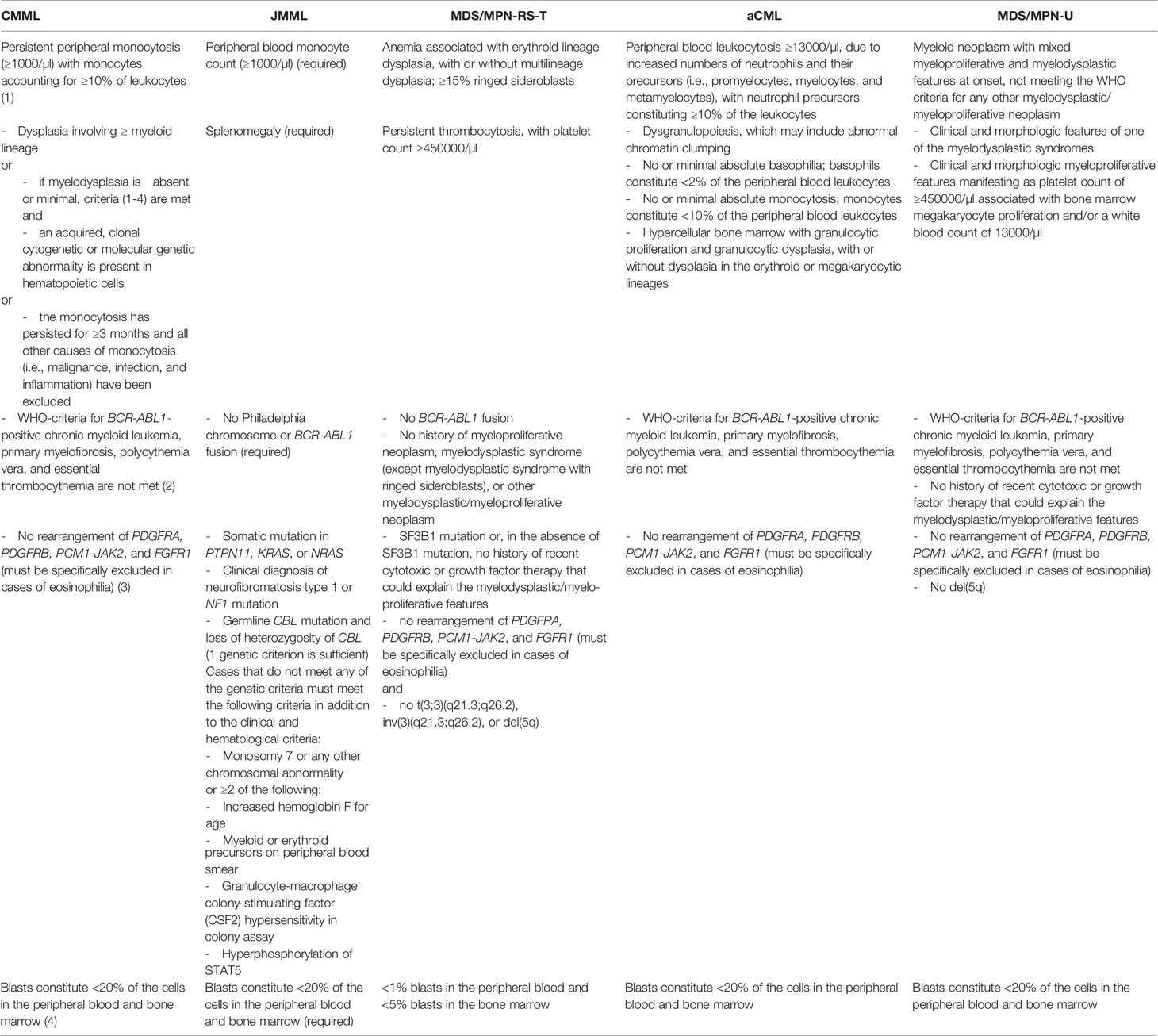
Table 1 Main diagnostic criteria of the MDS/MPN subgroups according to WHO 2016 (1).
The entities included within the WHO-category MDS/MPN share several common features, but also exhibit differences defining the individual disease (13, 15, 31–54). The hallmark of MDS/MPNs is the unique mixture of cytopenias and “cytoses”. Therefore, the bone marrow is typically hypercellular due to the combination of a very effective “myeloproliferative” hematopoiesis and an ineffective, dysplastic hematopoiesis (54–57). Dysplasia is seen in at least one hematopoietic lineage. By definition, the diseases have further characteristics in common: The percentage of blasts in PB and BM must be <20%. Certain cytogenetic abnormalities must be ruled out to exclude other genetically defined myeloid malignancies sharing features of myelodysplastic and myeloproliferative diseases. These include BCR-ABL1, PDGFRA, PDGFRB, PCM1-JAK2, and FGFR1 (1). Except JMML, MDS/MPN are diseases of the elderly and all MDS/MPN show a clear male preponderance, with the possible exception of MDS/MPN-RS-T where the gender distribution differs between publications and some even exhibit a slight predominance of the female gender (13, 15, 31–53). A high frequency of anemia is a further characteristic of most MDS/MPN, while other cytopenias are often less pronounced when compared to MDS, or “cytoses” occur. An increased WBC is frequent or mandatory in proliferative CMML, JMML, aCML, MDS/MPN-U and MDS/MPN-RS-T. Thrombocytosis is mandatory in MDS/MPN-RS-T and can occur in all other MDS/MPN subtypes as well (1, 50–54, 57).
The majority of patients show fatigue and most, maybe except MDS/MPN-RS-T, exhibit frequent general (MPN-like) symptoms like night sweats as well as symptoms of organomegaly and extramedullary disease. Spleno- and often an additional hepatomegaly are frequent clinical findings, especially in CMML and JMML. Again, an exception might be MDS/MPN-RS-T, but the data on these clinical features is unfortunately sparse regarding this rare entity (15, 17, 41, 43, 44, 46, 48–54, 58).
MDS/MPN also share a very low frequency of cytogenetic aberrations compared to MDS. In this regard the exception might be MDS/MPN-U. If cytogenetic abnormalities occur, +8 is by far the most frequent (13, 14, 17, 37, 39–44, 46, 48–54, 58). The frequency of molecular abnormalities on the other hand is very high. Such aberrations can be found in more than 90% of patients (2–17, 50–54, 58). Except in MDS/MPN-RS-T and partly in MDS/MPN-U, the frequency of JAK-2 mutations is very low when compared to classical MPNs (50–54).
Unfortunately, another feature, shared by this group of overlap diseases, is a poor response to treatment other than allogeneic stem cell transplantation. CMML, aCML, and MDS/MPN-U share a poor prognosis in general and afflicted patients are often too old for transplantation (16, 17, 31–36, 41, 43, 44, 46–54, 59–61). JMML might have a special role, as some children show spontaneous regression and otherwise most afflicted patients can be transplanted, but on the other hand the severity of the disease is obvious regarding the still unsatisfying long-term survival and the poor response to treatment other than transplantation can be observed for JMML as well (32, 37, 62). The only true exception seems to be MDS/MPN-RS-T which exhibits a low risk of progression and a long median survival time (13, 39–42). An overview of differences and similarities between the MDS/MPN subgroups is given in Table 2.
Epidemiology of MDS/MPN
Epidemiological studies on MDS/MPNs are scarce and most of the existing data is limited to CMML. For other MDS/MPN subtypes only vague estimations exist.
Regarding CMML, Dinmohamed et al. (31) find an annual standardized incidence (ASR) rate of 0.3 per 100.000 for the period of 1989 to 2012 in the Netherlands. The ASR increased from 1989 to 2007 and remained then stable at 0.38/100 000 until 2012. The ASR was higher in males (0.42) when compared to females (0.18) and increased with age from 0.02 per 100.000 under the age of 50 years to 3.62 in patients ≥80 years old. Relative survival did not improve over time with the 5-year relative survival rate (RSR) being only 16, 20, and 20% in the three time periods investigated. Interestingly, the RSR was poor in all age groups, ranging from 12% in the group above 80 years to 21% in patients younger than 50 years of age.
In a study on the epidemiology of MDS and MPDs in the United States from 2001 to 2004, data from the NAACCR as well as the SEER programs was used by Rollison et al. (34). They found an age adjusted incidence of 0.3 per 100 000, about one-tenth that of MDS. Survival of patients with CMML was worse when compared to MDS and MPD, the 3-year survival being 21%. While 3-year survival decreased with increasing age, similar to the Dutch study survival was again poor in all age groups. 3-year survival was 12% in patients over the age of 80 and, in comparison, still only 33% in patients with an age between 50 and 59 years. This was clearly inferior when compared to MDS (37% and 54%) and MPD (66 and 89%), respectively.
Another US study on Seer data reported incidence and survival of patients with MDS and MPDs between 2001 and 2012 (32). An age adjusted incidence rate of 4.3 per 100 000 was reported for all MDS/MPN taken together. The largest proportion represented by far the patients with CMML (4.1 per 100 000). Patients with aCML had an age adjusted incidence rate of 0.1 same as patients with JMML. Incidence rates for MDS/MPN-U or MDS/MPN-RS-T were not reported in this study. Incidence rates were higher in males when compared to females for all 3 overlap syndromes reported (male: female ratio 2.31 for CMML, 2.05 for aCML, and 2.30 for JMML). Incidence increased exponentially with increasing age. This was especially apparent for CMML when compared to MPNs. For aCML and JMML such data was not available. The incidence rates for CMML were significantly lower in Hispanics (3.0), Blacks (3.1), or Asian/Pacific Islanders (2.7) compared to Non-Hispanic Whites (4.4). For the other subgroups numbers were too low for such calculations. Incidence rates for CMML did not increase significantly over the time period investigated. As in the other studies survival of CMML patients was generally very poor, but slightly better in women vs men and younger vs. older patients (5-year survival 16% males ≥60, 27% males <60 years old, 18% females ≥60, 32% females <60 years of age). For aCML 5-year survival was even worse with 11% for male patients compared to 16% for female patients over the age of 60. In children with JMML the 5-year survival rate was 56% for males and 66% for females, without treatment data given.
In an investigation on the incidence of MDS in Western Greece during a 20-year period (1990-2009) Avgerinou et al. (36) found an incidence of MDS of 6 per 100.000 inhabitants. From the data given, a crude incidence of 1 per 100 000 can be calculated for CMML while the incidence is only 0.1 per 100 000 for all other MDS/MPD together. The incidence of CMML remained stable over the time period investigated. Within the period under investigation 39% of CMML patients progressed to AML.
In a comparative study between Switzerland and the US (SEER-data) Benzarti et al. described epidemiological trends regarding CMML between 1999 and 2014 (33). The age standardized incidence was similar and remained relatively stable in both countries, being 0.32 (1999-2006) and 0.38 (2007-2014) in Switzerland and 0.37 and 0.35 in the US. In both countries and time periods it was much higher in patients above the age of 75 (3.01-4.83 ≥75 vs. 0.17-0.25 <75 years of age) and higher in males when compared to females (0.51-0.57 vs. 0.17-0.25). There were an increasing proportion of older patients ≥75 years of age observed in the Swiss Cancer Registry compared to a decreasing in the US SEER database. Relative survival improved significantly in the US database (3-years 27-37%, 5-years 19-23%) and remained stable in Switzerland (3-years 48-40%, 5-years 34-26%).
In our MDS registry CMML accounts for about 12.5% of all MDS during a period from 1982 to 2020, leading to a rough incidence of 0.4 per 100.000 that remained relatively stable over the investigated time period (35).
CMML is by far the most frequent of MDS/MPNs. Published incidence rates range from 0.3-4.1 per 100 000 inhabitants with a median age above 70 years and a male predominance (31–36, 63). CMML might be described as even more heterogeneous when compared to MDS, with hematological characteristics ranging from solely dysplastic forms, presenting often cytopenic and resembling MDS with peripheral monocytosis to very proliferative forms, characterized by high white blood cell counts, but also by splenomegaly, extramedullary involvement, and strong general symptoms. Therefore, the initial distinction, as proposed by the FAB-classification (19), between dysplastic and proliferative CMML remains useful from a clinical point of view. Diagnosis is based on the presence of sustained (>3 months) peripheral blood monocytosis, along with bone marrow dysplasia. In the current WHO-classification CMML is subdivided into 3 different groups (CMML 0-II) according to blast count (1, 93). In 386 patients from our Duesseldorf registry Schuler et al. found a distribution of 26% CMML-0, 53% CMML-I, and 21% CMML-II (94).
Chromosomal abnormalities are less frequent in CMML when compared to MDS and have been described in about 10-40% of cases. On the other hand, more than 90% of CMML patients exhibit molecular mutations. These are relatively homogenous compared to other myeloid malignancies and mostly belong to a subset of 20 frequently mutated genes (58, 61, 66, 95). The clinical course of CMML patients is extremely variable, with wide differences in survival and leukemic transformation risk. Generally, survival is low around 20-35% at 5 years (35, 36, 58, 60, 93), even in lower age groups, but varies between the different prognostic risk groups. In several studies on CMML prognosis (CPSS, Mayo- Molecular Model, GFM- Model) (59–61) median survival ranged from 56 months to not reached in the best and 9-18 months in the worst prognostic group. The risk of leukemic transformation is around 15% over 3-5 years (59–61), but again varies considerably between subgroups (4-year leukemic transformation rate 0-48% [CPSS-paper) (59)].
JMML is a clonal hematopoietic stem cell disorder of childhood. It is extremely rare with an incidence rate of about 1 per 1 000 000 children under the age of 14 years (12, 37, 38, 96). Like CMML the disease is characterized by proliferation of the monocytic lineage. The age at diagnosis can vary between 1 month and early adolescence, but at least 50% of children are below 2 years old and only 5% are 5 years or older (37). Splenomegaly occurs in almost all cases, and hepatomegaly, lymphadenopathy as well as extramedullary involvement including skin, lung, and gastro-intestinal tract are common. While JMML shares a number of features with CMML, its pathobiology is unique. About a third of patients have cytogenetic abnormalities, about a quarter show monosomy 7. Molecular abnormalities occur in at least 90% of patients and usually involve the RAS pathway. About 90% of cases belong to one of 5 groups with mutations in either PTPN11, NRAS, KRAS, CBL, or NF1. The first three subtypes (PTPN11, NRAS, KRAS) are characterized by heterozygous somatic gain-of-function mutations in non-syndromic children, while JMML in neurofibromatosis type 1 and JMML in children with CBL-syndrome are characterized by germ line RAS disease and acquired biallelic inactivation of the NF1 or CBL gene in hematopoietic cells (12, 37). Clinical presentation as well as outcome differs between these 5 JMML subtypes. Secondary genetic alterations like ASXL1, EZH2, SETBP1, JAK3, and mutations in spliceosomal genes often result in disease progression. Generally, a wide variation exists regarding the clinical course of the disease. In about 15% of children, most frequently in CBL mutated disease, spontaneous regression occurs. The majority of children affected by JMML, however, require allogeneic transplantation to cure the disease. An allogeneic stem cell transplantation from a histo-compatible sibling or HLA-matched unrelated donor results in a disease-free survival of 52% in a study from 2005 by Locatelli et al. (62). In an earlier study (1997) the probability of survival at 10 years was 0.39 for children having received allogeneic stem cell transplantation and 0.06 for children that did not receive HSCT (37). Variables like age, level of HbF, platelet count, or, more recently described, genome-wide DNA methylation profiles may be helpful to predict the clinical course.
aCML is a rare, BCR-ABL1-negative, MDS/MPN overlap syndrome characterized by leukocytosis, granulocytic dysplasia, and a dismal prognosis. It was first described as a variant CML lacking the Philadelphia chromosome, but diagnostic criteria have evolved since. However, it can still be challenging to distinguish aCML from other MPNs like chronic neutrophilic leukemia or from other MDS/MPN like MDS/MPN-U, as the diagnosis largely relies on morphologic criteria. Its frequency is not well known, but it is estimated to account for 1-2% of BCR-ABL1-positive CML (~0.5-2/100000) (44, 70–73). The disorder affects elderly patients with a median age of 62-73 years and a male predominance (15, 32, 43–47, 97, 98). The clinical picture is comparable to Philadelphia positive CML including elevated WBC with co-occurrence of mature and immature cells of the granulocytic lineage, splenomegaly, and mild to moderate anemia. Typical for aCML, however, are severe dysplastic features predominantly in the granulocytic lineage. Also, in contrast to classical CML, the genetic basis of the disease is heterogeneous, with SETBP1 and ETNK1 mutations being recurrent, but several other mutations, typical for MDS and/or MPNs can be found as well (15). Cytogenetic abnormalities are less frequent and occur in 20-40% of patients only (43, 44, 46). Median survival varies between 10 and 25 months (43, 44, 46, 47). AML evolution occurs in about 31-40% of patients with a median time to AML of 11-18 months (43, 44, 46).
Of the MDS/MPN overlap syndromes, MDS/MPN-U is the least well defined. It encompasses such patients, that show features of myelodysplastic as well as myeloproliferative disease, who do not fit into one of the other 4 subgroups. The diagnosis is extremely rare, accounting for less than 2% of MDS (49). In the Duesseldorf MDS registry it currently accounts for only 0.05% of all MDS (35). Patients with MDS/MPN-U are relatively old with a median age of 70 years and show the male predominance that is seen in other MDS/MPN subgroups. Regarding cytogenetic features, the percentage of abnormal, including complex karyotypes is higher when compared to other MDS/MPN. Of the molecular abnormalities found in patients with MDS/MPN-U the JAK2-V617F mutation is relatively frequent in contrast to the other overlap syndromes except MDS-RS-T. Clinical characteristics are not well established and often seem to show similarities with one of the other MDS/MPN-subgroups. Thus, MDS/MPN-U is rather a mixture of patients not fulfilling all criteria for the diagnosis of one of the other MDS/MPN subtypes (i.e. not enough peripheral monocytes to fulfill the diagnosis CMML or slightly less than 450.000 thrombocytes not fulfilling the criteria for MDS-RS-T, WBC too low for aCML,…). This is, of course, due to the fact, that all thresholds are more or less arbitrary. This fact might be unsatisfactory, but as thresholds are necessary, a solution might be to form subgroups of “CMML-like MDS/MPN-U” and “MDS-RS-T like MDS/MPN-U” and so on or to allow the diagnosis of pre-CMML syndromes like oligo-monocytic CMML (86, 87). Patients should be checked at regular intervals whether they still fit into the MDS/MPN-U category or might be transferred into a better defined MDS/MPN subtype. With a median survival of 1-2 years, survival of patients with MDS/MPN-U is generally poor. However, some subgroups like the “MDS-RS-T like MDS/MPN-U” might do better than others.
Refractory anemia with ringed sideroblasts associated with marked thrombocytosis (MDS-RS-T) is the latest “member” in the group of MDS/MPN. It was proposed as a provisional entity in the WHO 2001 classification of myeloid neoplasms. The latest WHO-classification has now recognized MDS/MPN-RS-T as a formal subgroup of the MDS/MPN overlap syndromes. MDS/MPN-RS-T shares clinical features with MDS-RS-SLD and essential thrombocythemia. It is characterized by the co-occurrence of ringed sideroblasts in the bone marrow (≥15%), together with an increased platelet count (≥450 000/µl) and large, atypical megakaryocytes. As for most of the other MDS/MPNs epidemiological data is scarce, due to the rarity of the disease. Its frequency can be estimated to be below or about 1% of all MDS (49, 50, 69). In our current MDS registry it accounts for 1,45% of all MDS (35). The median age at presentation ranges from 71-75 years (13, 39–42). In contrast to other MDS/MPN the male predominance seems less pronounced but varies between studies (13, 39–42). Hepato-splenomegaly and extramedullary involvement appear to be less frequent compared to other MDS/MPD, same as the “MPD-typical” constitutional symptoms, although data on these clinical features is still very limited. In addition, the prognosis is generally better than that of other MDS/MPD as it resembles the two relatively “benign” diseases MDS-RS-SLD on the one hand and ET on the other hand, leading to a relatively low risk of leukemic transformation, but also to an increased risk of thromboembolic events and an often symptomatic anemia as the typical presentation of this unique MDS/MPD subgroup. Regarding cytogenetics, about 80% of patients exhibit a normal karyotype. Gene mutations, conversely, are frequent and observed in >90% of patients (13, 14). The most frequent are SF3B1 as well as JAK-2 mutations. Patients with RARS-T have a shorter overall (76 vs. 117 months) and leukemia-free survival than patients with essential thrombocythemia along with a comparable risk of thromboembolic complications (3.6 vs. 3.9/100 patient years). On the other hand, they exhibit a longer survival (76 vs. 63 months), but a higher risk of thrombosis when compared to patients with MDS-RS (3.6 vs. 0.9/100 patient years) (39).
Two groups that are not recognized as (separate) entities within the MDS/MPN but show unique features and an overlap of both MDS and MPN are patients with del(5q) and JAK2 V617F mutation and patients with isolated isochromosome (17q). These groups are small, but usually show the typical overlapping symptoms of both myelodysplastic and myeloproliferative disease. MDS with del(5q) and JAK2 are currently subsumed under MDS with isolated del(5q). This makes sense on the one hand since patients appear to have a comparable prognosis when compared to patients with isolated del(5q) without the JAK2 mutation and treatment with lenalidomide appears to be active in both subgroups. However, lenalidomide shows activity in MPNs like myelofibrosis as well. On the other hand, the most recent and most extensive publication on this small subgroup of MDS patients by Sangiorgio et al. (21) shows that median cell counts regarding platelets, but also WBC, and even red blood cell counts, are higher when compared to MDS with del(5q) and JAK2-wildtype. 3 patients did not even meet the criteria for MDS and del(5q) because they lacked sufficient cytopenias. In addition, all 3 patients with data available showed splenomegaly, 4 of 5 patients with available bone marrow histology were hypercellular and all these patients had grade 1 or 2 fibrosis. Dysplasia in the erythroid or granulocytic lineage was lacking. Still, megakaryocytes were not typical for MPN, but clearly exhibited dysplastic, del(5q) like features, with hypo- and monolobulated nuclei, while large hypernucleated forms existed as well. Thus, one could argue that such patients, according to their clinical presentation, might better be recognized as MDS/MPN overlap syndromes than MDS. In this study 12.7% of all MDS with isolated del(5q) were found to have a JAK2 V617F mutation. Others found a slightly lower frequency (22). The JAK2 V617F mutation identifies a subgroup of MDS patients with isolated deletion 5q and a proliferative bone marrow.
Isolated isochromosome (17q) can be a finding within complex karyotypes occurring in different myeloid malignancies, but also, rarely, exists as sole chromosomal abnormality. In this case, it often presents as MDS/MPN overlap syndrome. The median age is around 60 years, with the typical male predominance (23–30). Patients often present with anemia, leukocytosis, and splenomegaly. The bone marrow is hypercellular, often exhibiting some grade of fibrosis, and dysgranulopoiesis, including hypo- and non-segmented forms, ring nuclei, hypogranularity, and chromatin clumping is typically prominent. The blast count is usually low. Monocytosis occurs frequently, thus many cases are currently subsumed under CMML. A few might present like aCML, but most other cases can only be placed in MDS/MPN-U. As patients with this unique cytogenetic feature share many clinical features and seem to have a relatively uniform poor prognosis and high risk of leukemic evolution it is a matter of discussion, whether it might make sense to form a new, cytogenetically well-defined subgroup of MDS/MPN. However, in the Duesseldorf MDS registry currently only one patient with isolated isochromosome (17q) can be detected. This patient was diagnosed as CMML.
Conclusion
The WHO-category MDS/MPN encompasses a unique group of clonal myeloid neoplasms exhibiting hybrid features of myelodysplastic as well as myeloproliferative malignancies. As most entities are quite rare, epidemiological data is sparse. In adults the most frequent MDS/MPN by far is CMML, followed by MDS/MPN-RS-T. aCML and MDS/MPN-U are extremely rare diseases and not very well defined. An appropriate diagnosis and classification are difficult, but essential for further prognostication and treatment decisions. Although diagnosis of most subtypes is still largely based on morphologic criteria, diagnosing MDS/MPD properly should require a comprehensive clinical and laboratory assessment with thorough integration of morphological, immunophenotypic, genetic, as well as clinical examination. While single gene mutations might occur in different MDS/MPN or other myeloid diseases certain gene combinations may be more specific for certain subtypes and might aid in determining the correct diagnosis (69). Despite an enormous gain of knowledge regarding molecular genetics and in some subgroups pathophysiology as well we are still far from satisfactory treatment options in this rare and heterogeneous group of myeloid overlap syndromes.
Author Contributions
AKu, UG, and AKa contributed to conception and design of the paper. AKu wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 Revision to the World Health Organization Classification of Myeloid Neoplasms and Acute Leukemia. Blood (2016) 127:2391–405. doi: 10.1182/blood-2016-03-643544
2. Elena C, Gallì A, Such E, Meggendorfer M, Germing U, Rizzo E, et al. Integrating Clinical Features and Genetic Lesions in the Risk Assessment of Patients With Chronic Myelomonocytic Leukemia. Blood (2016) 128:1408–17. doi: 10.1182/blood-2016-05-714030
3. Itzykson R, Fenaux P, Bowen D, Cross NCP, Cortes J, De Witte T, et al. Diagnosis and Treatment of Chronic Myelomonocytic Leukemias in Adults: Recommendations From the European Hematology Association and the European Leukemianet. Hemasphere (2018) 2:e150. doi: 10.1097/HS9.000000000000015
4. Kohlmann A, Grossmann V, Klein HU, Schindela S, Weiss T, Kazak B, et al. Next-Generation Sequencing Technology Reveals a Characteristic Pattern of Molecular Mutations in 72.8% of Chronic Myelomonocytic Leukemia by Detecting Frequent Alterations in TET2, CBL, RAS, and RUNX1. J Clin Oncol (2010) 28:3858–65. doi: 10.1200/JCO.2009.27.1361
5. Kohlmann A, Grossmann V, Haferlach T. Integration of Next-Generation Sequencing Into Clinical Practice: Are We There Yet? Semin Oncol (2012) 39:26–36. doi: 10.1053/j.seminoncol.2011.11.008
6. Patnaik MM, Lasho TL. Genomics of Myelodysplastic Syndrome/Myeloproliferative Neoplasm Overlap Syndromes. Hematol Am Soc Hematol Educ Program (2020) 2020:450–9. doi: 10.1182/hematology.2020000130
7. Jankowska AM, Makishima H, Tiu RV, Szpurka H, Huang Y, Traina F, et al. Mutational Spectrum Analysis of Chronic Myelomonocytic Leukemia Includes Genes Associated With Epigenetic Regulation: UTX, EZH2, and DNMT3A. Blood (2011) 118:3932–41. doi: 10.1182/blood-2010-10-311019
8. Cervera N, Itzykson R, Coppin E, Prebet T, Murati A, Legall S, et al. Gene Mutations Differently Impact the Prognosis of the Myelodysplastic and Myeloproliferative Classes of Chronic Myelomonocytic Leukemia. Am J Hematol (2014) 89:604–9. doi: 10.1002/ajh.23702
9. Smith AE, Mohamedali AM, Kulasekararaj A, Lim Z, Gäken J, Lea NC, et al. Next-Generation Sequencing of the TET2 Gene in 355 MDS and CMML Patients Reveals Low-Abundance Mutant Clones With Early Origins, But Indicates No Definite Prognostic Value. Blood (2010) 116:3923–32. doi: 10.1182/blood-2010-03-274704
10. Federmann B, Abele M, Rosero Cuesta DS, Vogel W, Boiocchi L, Kanz L, et al. The Detection of SRSF2 Mutations in Routinely Processed Bone Marrow Biopsies is Useful in the Diagnosis of Chronic Myelomonocytic Leukemia. Hum Pathol (2014) 45:2471–9. doi: 10.1016/j.humpath.2014.08.014
11. Malcovati L, Papaemmanuil E, Ambaglio I, Elena C, Galli A, Della Porta MG, et al. Driver Somatic Mutations Identify Distinct Disease Entities Within Myeloid Neoplasms With Myelodysplasia. Blood (2014) 124:1513–21. doi: 10.1182/blood-2014-03-560227
12. Niemeyer CM. JMML Genomics and Decisions. Hematol Am Soc Hematol Educ Program (2018) 2018:307–12. doi: 10.1182/asheducation-2018.1.307
13. Patnaik MM, Lasho TL, Finke CM, Hanson CA, King RL, Ketterling RP, et al. Predictors of Survival in Refractory Anemia With Ring Sideroblasts and Thrombocytosis (RARS-T) and the Role of Next-Generation Sequencing. Am J Hematol (2016) 91:492–8. doi: 10.1002/ajh.24332
14. Jeromin S, Haferlach T, Weissmann S, Meggendorfer M, Eder C, Nadarajah N, et al. Refractory Anemia With Ring Sideroblasts and Marked Thrombocytosis Cases Harbor Mutations in SF3B1 or Other Spliceosome Genes Accompanied by JAK2V617F and ASXL1 Mutations. Haematologica (2015) 100:e125–7. doi: 10.3324/haematol.2014.119032
15. Fontana D, Ramazzotti D, Aroldi A, Redaelli S, Magistroni V, Pirola A, et al. Integrated Genomic, Functional, and Prognostic Characterization of Atypical Chronic Myeloid Leukemia. Hemasphere (2020) 4:e497. doi: 10.1097/HS9.0000000000000497
16. Bose P, Nazha A, Komrokji RS, Patel KP, Pierce SA, Al-Ali N, et al. Mutational Landscape of Myelodysplastic/Myeloproliferative Neoplasm-Unclassifiable. Blood (2018) 132:2100–3. doi: 10.1182/blood-2018-05-848473
17. Mangaonkar AA, Swoboda DM, Coltro G, Lasho TL, Novotny PJ, Pophali P, et al. Clinicopathologic Characteristics, Prognostication and Treatment Outcomes for Myelodysplastic/Myeloproliferative Neoplasm, Unclassifiable (MDS/MPN-U): Mayo Clinic-Moffitt Cancer Center Study of 135 Consecutive Patients. Leukemia (2020) 34:656–61. doi: 10.1038/s41375-019-0574-x
18. Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposals for the Classification of the Acute Leukaemias. French-American-British (FAB) Co-Operative Group. Br J Haematol (1976) 33:451–8. doi: 10.1111/j.1365-2141.1976.tb03563.x
19. Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposals for the Classification of the Myelodysplastic Syndromes. Br J Haematol (1982) 51:189–99. doi: 10.1111/j.1365-2141.1982.tb08475.x
20. Jaffe ES, Harris NL, Stein H, Vardiman JW eds. World Health Organization Classification of Tumours. In: Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues. Lyon, France: IARC Press.
21. Sangiorgio VFI, Geyer JT, Margolskee E, Al-Kawaaz M, Mathew S, Tam W, et al. Myeloid Neoplasms With Isolated Del(5q) and JAK2 V617F Mutation: A “Grey Zone” Combination of Myelodysplastic and Myeloproliferative Features? Haematologica (2020) 105(6):e276–9. doi: 10.3324/haematol.2019.227686
22. Ingram W, Lea NC, Cervera J, Germing U, Fenaux P, Cassinat B, et al. The JAK2 V617F Mutation Identifies a Subgroup of MDS Patients With Isolated Deletion 5q and a Proliferative Bone Marrow. Leukemia (2006) 20:1319–21. doi: 10.1038/sj.leu.2404215
23. McClure RF, Dewald GW, Hoyer JD, Hanson HD. Isolated Isochromosome 17q: A Distinct Type of Mixed Myeloproliferative Disorder/Myelodysplastic Syndrome With an Aggressive Clinical Course. Br J Haematol (1999) 106:445–54. doi: 10.1046/j.1365-2141.1999.01537.x
24. Kanagal-Shamanna R, Luthra R, Yin CC, Patel KP, Takahashi K, Lu X, et al. Myeloid Neoplasms With Isolated Isochromosome 17q Demonstrate a High Frequency of Mutations in SETBP1, SRSF2, ASXL1 and NRAS. Oncotarget (2016) 7:14251–8. doi: 10.18632/oncotarget.7350
25. Kanagal-Shamanna R, Bueso-Ramos CE, Barkoh B, Lu G, Wang S, Garcia-Manero G, et al. Myeloid Neoplasms With Isolated Isochromosome 17q Represent a Clinicopathologic Entity Associated With Myelodysplastic/Myeloproliferative Features, a High Risk of Leukemic Transformation, and Wild-Type TP53. Cancer (2012) 118(11):2879–88. doi: 10.1002/cncr.26537
26. Koczkodaj D, Muzyka-Kasietczuk J, Chocholska S, Podhorecka M. Prognostic Significance of Isochromosome 17q in Hematologic Malignancies. Oncotarget (2021) 12:708–18. doi: 10.18632/oncotarget.27914
27. Ganguly S, Uvodich M, Dias A, McGuirk JP. Clinical Characteristics and Treatment Outcome of Patients With Isochromosome 17q (I17q) Abnormality and Myeloid Neoplasms: A Single Center Experience. Leuk Res Rep (2018) 10:55–6. doi: 10.1016/j.lrr.2018.06.002
28. Fioretos T, Strömbeck B, Sandberg T, Johansson B, Billström R, Borg A, et al. Isochromosome 17q in Blast Crisis of Chronic Myeloid Leukemia and in Other Hematologic Malignancies is the Result of Clustered Breakpoints in 17p11 and is Not Associated With Coding TP53 Mutations. Blood (1999) 94:225–32. doi: 10.1182/blood.V94.1.225.413k24_225_232
29. Weh HJ, Kuse R, Hossfeld DK. Acute Nonlymphocytic Leukemia (ANLL) With Isochromosome I(17q) as the Sole Chromosomal Anomaly: A Distinct Entity? Eur J Haematol (1990) 44:312–4. doi: 10.1111/j.1600-0609.1990.tb00401.x
30. Solé F, Torrabadella M, Granada I, Florensa L, Vallespi T, Ribera JM, et al. Isochromosome 17q as a Sole Anomaly: A Distinct Myelodysplastic Syndrome Entity? Leuk Res (1993) 17:717–20. doi: 10.1016/0145-2126(93)90080-5
31. Dinmohamed AG, Brink M, Visser O, Sonneveld P, van de Loosdrecht AA, Jongen-Lavrencic M, et al. Trends in Incidence, Primary Treatment and Survival in Chronic Myelomonocytic Leukaemia: A Population-Based Study of 1359 Patients Diagnosed in the Netherlands From 1989 to 2012. Br J Haematol (2015) 171:436–9. doi: 10.1111/bjh.13414
32. Srour SA, Devesa SS, Morton LM, Check DP, Curtis RE, Linet MS, et al. Incidence and Patient Survival of Myeloproliferative Neoplasms and Myelodysplastic/Myeloproliferative Neoplasms in the United States, 2001-12. Br J Haematol (2016) 174:382–96. doi: 10.1111/bjh.14061
33. Benzarti S, Daskalakis M, Feller A, Bacher VU, Schnegg-Kaufmann A, Rüfer A, et al. Trends of Incidence and Survival of Patients With Chronic Myelomonocytic Leukemia Between 1999 and 2014: A Comparison Between Swiss and American Population-Based Cancer Registries. Cancer Epidemiol (2019) 59:51–7. doi: 10.1016/j.canep.2019.01.003
34. Rollison DE, Howlader N, Smith MT, Strom SS, Merritt WD, Ries LA, et al. Epidemiology of Myelodysplastic Syndromes and Chronic Myeloproliferative Disorders in the United States, 2001-2004, Using Data From the NAACCR and SEER Programs. Blood (2008) 112:45–52. doi: 10.1182/blood-2008-01-134858
35. Germing U. Data From the Duesseldorf MDS Registry as at 2021. Duesseldorf: Duesseldorf MDS Registry (2021).
36. Avgerinou C, Alamanos Y, Zikos P, Lampropoulou P, Melachrinou M, Labropoulou V, et al. The Incidence of Myelodysplastic Syndromes in Western Greece is Increasing. Ann Hematol (2013) 92:877–87. doi: 10.1007/s00277-013-1712-6
37. Niemeyer CM, Arico M, Basso G, Biondi A, Cantu Rajnoldi A, Creutzig U, et al. Chronic Myelomonocytic Leukemia in Childhood: A Retrospective Analysis of 110 Cases. European Working Group on Myelodysplastic Syndromes in Childhood (EWOG-MDS). Blood (1997) 89:3534–43. doi: 10.1182/blood.V89.10.3534
38. Passmore SJ, Chessells JM, Kempski H, Hann IM, Brownbill PA, Stiller CA. Paediatric Myelodysplastic Syndromes and Juvenile Myelomonocytic Leukaemia in the UK: A Population-Based Study of Incidence and Survival. Br J Haematol (2003) 121:758–67. doi: 10.1046/j.1365-2141.2003.04361.x
39. Broseus J, Florensa L, Zipperer E, Schnittger S, Malcovati L, Richebourg S, et al. Clinical Features and Course of Refractory Anemia With Ring Sideroblasts Associated With Marked Thrombocytosis. Haematologica (2012) 97:1036–41. doi: 10.3324/haematol.2011.053918
40. Broséus J, Alpermann T, Wulfert M, Florensa Brichs L, Jeromin S, Lippert E, et al. Age, JAK2(V617F) and SF3B1 Mutations are the Main Predicting Factors for Survival in Refractory Anaemia With Ring Sideroblasts and Marked Thrombocytosis. Leukemia (2013) 27:1826–31. doi: 10.1038/leu.2013.120
41. Atallah E, Nussenzveig R, Yin CC, Bueso-Ramos C, Tam C, Manshouri T, et al. Prognostic Interaction Between Thrombocytosis and JAK2 V617F Mutation in the WHO Subcategories of Myelodysplastic/Myeloproliferative Disease-Unclassifiable and Refractory Anemia With Ringed Sideroblasts and Marked Thrombocytosis. Leukemia (2008) 22:1295–8. doi: 10.1038/sj.leu.2405054
42. Wang SA, Hasserjian RP, Loew JM, Sechman EV, Jones D, Hao S, et al. Refractory Anemia With Ringed Sideroblasts Associated With Marked Thrombocytosis Harbors JAK2 Mutation and Shows Overlapping Myeloproliferative and Myelodysplastic Features. Leukemia (2006) 20:1641–4. doi: 10.1038/sj.leu.2404316
43. Wang SA, Hasserjian RP, Fox PS, Rogers HJ, Geyer JT, Chabot-Richards D. Atypical Chronic Myeloid Leukemia is Clinically Distinct From Unclassifiable Myelodysplastic/Myeloproliferative Neoplasms. Blood (2014) 123:2645–51. doi: 10.1182/blood-2014-02-553800
44. Breccia M, Biondo F, Latagliata R, Carmosino I, Mandelli F, Alimena G. Identification of Risk Factors in Atypical Chronic Myeloid Leukemia. Haematologica (2006) 91:1566–8. doi: 10.3324/%25x
45. Hernández JM, del Cañizo MC, Cuneo A, García JL, Gutiérrez NC, González M, et al. Clinical, Hematological and Cytogenetic Characteristics of Atypical Chronic Myeloid Leukemia. Ann Oncol (2000) 11:441–4. doi: 10.1023/a:1008393002748
46. Onida F, Ball G, Kantarjian HM, Smith TL, Glassman A, Albitar M, et al. Characteristics and Outcome of Patients With Philadelphia Chromosome Negative, Bcr/Abl Negative Chronic Myelogenous Leukemia. Cancer (2002) 95:1673–84. doi: 10.1002/cncr.10832
47. Kong JH, Nam H, Go TH, Hyun SY, Shim KY. Characteristics and Survival of Patients With Atypical Chronic Myeloid Leukemia. Blood Res (2019) 54:233–6. doi: 10.5045/br.2019.54.3.233
48. DiNardo CD, Daver N, Jain N, Pemmaraju N, Bueso-Ramos C, Yin CC, et al. Myelodysplastic/Myeloproliferative Neoplasms, Unclassifiable (MDS/MPN, U): Natural History and Clinical Outcome by Treatment Strategy. Leukemia (2014) 28:958–61. doi: 10.1038/leu.2014.8
49. Cannella L, Breccia M, Latagliata R, Frustaci A, Alimena G. Clinical and Prognostic Features of Patients With Myelodysplastic/Myeloproliferative Syndrome Categorized as Unclassified (MDS/MPD-U) by WHO Classification. Leuk Res (2008) 32:514–6. doi: 10.1016/j.leukres.2007.07.004
50. Orazi A, Germing U. The Myelodysplastic/Myeloproliferative Neoplasms: Myeloproliferative Diseases With Dysplastic Features. Leukemia (2008) 22:1308–19. doi: 10.1038/leu.2008.119
51. Clara JA, Sallman DA, Padron E. Clinical Management of Myelodysplastic Syndrome/Myeloproliferative Neoplasm Overlap Syndromes. Cancer Biol Med (2016) 13:360–72. doi: 10.20892/j.issn.2095-3941.2016.0043
52. Hall J, Foucar K. Diagnosing Myelodysplastic/Myeloproliferative Neoplasms: Laboratory Testing Strategies to Exclude Other Disorders. Int J Lab Hematol (2010) 32:559–71. doi: 10.1111/j.1751-553X.2010.01251.x
53. Cazzola M, Malcovati L, Invernizzi R. Myelodysplastic/Myeloproliferative Neoplasms. Hematol Am Soc Hematol Educ Program (2011) 2011:264–72. doi: 10.1182/asheducation-2011.1.264
54. Mughal TI, Cross NC, Padron E, Tiu RV, Savona M, Malcovati L, et al. An International Mds/Mpn Working Group’s Perspective and Recommendations on Molecular Pathogenesis, Diagnosis and Clinical Characterization of Myelodysplastic/Myeloproliferative Neoplasms. Haematologica (2015) 100:1117–30. doi: 10.3324/haematol.2014.114660
55. Germing U, Strupp C, Knipp S, Kuendgen A, Giagounidis A, Hildebrandt B, et al. Chronic Myelomonocytic Leukemia in the Light of the WHO Proposals. Haematologica (2007) 92:974–7. doi: 10.3324/haematol.11051
56. Niemeyer CM, Flotho C. Juvenile Myelomonocytic Leukemia: Who’s the Driver at the Wheel? Blood (2019) 133:1060–70. doi: 10.1182/blood-2018-11-844688
57. Xubo G, Xingguo L, Xianguo W, Rongzhen X, Xibin X, Lin W, et al. The Role of Peripheral Blood, Bone Marrow Aspirate and Especially Bone Marrow Trephine Biopsy in Distinguishing Atypical Chronic Myeloid Leukemia From Chronic Granulocytic Leukemia and Chronic Myelomonocytic Leukemia. Eur J Haematol (2009) 83:292–301. doi: 10.1111/j.1600-0609.2009.01283.x
58. Patnaik MM, Tefferi A. Chronic Myelomonocytic Leukemia: 2020 Update on Diagnosis, Risk Stratification and Management. Am J Hematol (2020) 95:97–115. doi: 10.1002/ajh.25684
59. Such E, Germing U, Malcovati L, Cervera J, Kuendgen A, Della Porta MG, et al. Development and Validation of a Prognostic Scoring System for Patients With Chronic Myelomonocytic Leukemia. Blood (2013) 121:3005–15. doi: 10.1182/blood-2012-08-452938
60. Patnaik MM, Padron E, LaBorde RR, Lasho TL, Finke CM, Hanson CA, et al. Mayo Prognostic Model for WHO-Defined Chronic Myelomonocytic Leukemia: ASXL1 and Spliceosome Component Mutations and Outcomes. Leukemia (2013) 27:1504–10. doi: 10.1038/leu.2013.88
61. Itzykson R, Kosmider O, Renneville A, Gelsi-Boyer V, Meggendorfer M, Morabito M, et al. Prognostic Score Including Gene Mutations in Chronic Myelomonocytic Leukemia. J Clin Oncol (2013) 31(19):2428–36. doi: 10.1200/JCO.2012.47.3314
62. Locatelli F, Nöllke P, Zecca M, Korthof E, Lanino E, Peters C, et al. Hematopoietic Stem Cell Transplantation (HSCT) in Children With Juvenile Myelomonocytic Leukemia (JMML): Results of the EWOG-MDS/EBMT Trial. Blood (2005) 105:410–9. doi: 10.1182/blood-2004-05-1944
63. Neukirchen J, Schoonen WM, Strupp C, Gattermann N, Aul C, Haas R, et al. Incidence and Prevalence of Myelodysplastic Syndromes: Data From the Dusseldorf MDS-Registry. Leuk Res (2011) 35:1591–6. doi: 10.1016/j.leukres.2011.06.001
64. Ma X, Does M, Raza A, Mayne ST. Myelodysplastic Syndromes: Incidence and Survival in the United States. Cancer (2007) 109:1536–42. doi: 10.1002/cncr.22570
65. Maynadié M, Verret C, Moskovtchenko P, Mugneret F, Petrella T, Caillot D, et al. Epidemiological Characteristics of Myelodysplastic Syndrome in a Well-Defined French Population. Br J Cancer (1996) 74:288–90. doi: 10.1038/bjc.1996.354
66. Merlevede J, Droin N, Qin T, Meldi K, Yoshida K, Morabito M, et al. Mutation Allele Burden Remains Unchanged in Chronic Myelomonocytic Leukaemia Responding to Hypomethylating Agents. Nat Commun (2016) 7:10767. doi: 10.1038/ncomms10767
67. Barrington-Trimis JL, Cockburn M, Metayer C, Gauderman WJ, Wiemels J, McKean-Cowdin R. Trends in Childhood Leukemia Incidence Over Two Decades From 1992 to 2013. Int J Cancer (2017) 140:1000–8. doi: 10.1002/ijc.30487
68. Xavier AC, Kutny M, Costa LJ. Incidence and Outcomes of Paediatric Myelodysplastic Syndrome in the United States. Br J Haematol (2018) 180:898–901. doi: 10.1111/bjh.14460
69. Gattermann N, Billiet J, Kronenwett R, Zipperer E, Germing U, Nollet F, et al. High Frequency of the JAK2 V617F Mutation in Patients With Thrombocytosis (Platelet Count>600x109/L) and Ringed Sideroblasts More Than 15% Considered as MDS/MPD, Unclassifiable. Blood (2007) 109:1334–5. doi: 10.1182/blood-2006-05-022491
71. Vardiman JW, Harris NL, Brunning RD. The World Health Organization (WHO) Classification of the Myeloid Neoplasms. Blood (2002) 100:2292–302. doi: 10.1182/blood-2002-04-1199
72. Hehlmann R, Hochhaus A, Baccarani M. European Leukemianet. Chronic Myeloid Leukaemia. Lancet (2007) 370:342–50. doi: 10.1016/S0140-6736(07)61165-9
73. Rohrbacher M, Hasford J. Epidemiology of Chronic Myeloid Leukaemia (CML). Best Pract Res Clin Haematol (2009) 22:295–302. doi: 10.1016/j.beha.2009.07.007
74. Petrova-Drus K, Chiu A, Margolskee E, Barouk-Fox S, Geyer J, Dogan A, et al. Bone Marrow Fibrosis in Chronic Myelomonocytic Leukemia is Associated With Increased Megakaryopoiesis, Splenomegaly and With a Shorter Median Time to Disease Progression. Oncotarget (2017) 8:103274–82. doi: 10.18632/oncotarget.21870
75. Gur HD, Loghavi S, Garcia-Manero G, Routbort M, Kanagal-Shamanna R, Quesada A, et al. Chronic Myelomonocytic Leukemia With Fibrosis is a Distinct Disease Subset With Myeloproliferative Features and Frequent JAK2 P.V617F Mutations. Am J Surg Pathol (2018) 42:799–806. doi: 10.1097/PAS.0000000000001058
76. Khan M, Muzzafar T, Kantarjian H, Badar I, Short N, Wang X, et al. Association of Bone Marrow Fibrosis With Inferior Survival Outcomes in Chronic Myelomonocytic Leukemia. Ann Hematol (2018) 97:1183–91. doi: 10.1007/s00277-018-3289-6
77. Vitte F, Fabiani B, Bénet C, Dalac S, Balme B, Delattre C, et al. Specific Skin Lesions in Chronic Myelomonocytic Leukemia: A Spectrum of Myelomonocytic and Dendritic Cell Proliferations: A Study of 42 Cases. Am J Surg Pathol (2012) 36:1302–16. doi: 10.1097/PAS.0b013e31825dd4de
78. Lucas N, Duchmann M, Rameau P, Noël F, Michea P, Saada V, et al. Biology and Prognostic Impact of Clonal Plasmacytoid Dendritic Cells in Chronic Myelomonocytic Leukemia. Leukemia (2019) 33:2466–80. doi: 10.1038/s41375-019-0447-3
79. Lebecque B, Vial JP, Pigneux A, Lechevalier N. Chronic Myelomonocytic Leukaemia Followed by Blastic Plasmacytoid Dendritic Cell Neoplasm. Br J Haematol (2019) 185:398. doi: 10.1111/bjh.15794
80. Zahid MF, Barraco D, Lasho TL, Finke C, Ketterling RP, Gangat N, et al. Spectrum of Autoimmune Diseases and Systemic Inflammatory Syndromes in Patients With Chronic Myelomonocytic Leukemia. Leuk Lymphoma (2017) 58:1488–93. doi: 10.1080/10428194.2016.1243681
81. Peker D, Padron E, Bennett JM, Zhang X, Horna P, Epling-Burnette PK, et al. A Close Association of Autoimmune-Mediated Processes and Autoimmune Disorders With Chronic Myelomonocytic Leukemia: Observation From a Single Institution. L.Acta Haematol (2015) 133:249–56. doi: 10.1159/000365877
82. Elbæk MV, Sørensen AL, Hasselbalch HC. Chronic Inflammation and Autoimmunity as Risk Factors for the Development of Chronic Myelomonocytic Leukemia? Leuk Lymphoma (2016) 57:1793–9. doi: 10.3109/10428194.2016.1143938
83. Elbæk MV, Sørensen AL, Hasselbalch HC. Cardiovascular Disease in Chronic Myelomonocytic Leukemia: Do Monocytosis and Chronic Inflammation Predispose to Accelerated Atherosclerosis? Ann Hematol (2019) 98:101–9. doi: 10.1007/s00277-018-3489-0
84. Palomo L, Meggendorfer M, Hutter S, Twardziok S, Ademà V, Fuhrmann I, et al. Molecular Landscape and Clonal Architecture of Adult Myelodysplastic/Myeloproliferative Neoplasms. Blood (2020) 136:1851–62. doi: 10.1182/blood.2019004229
85. Patnaik MM, Vallapureddy R, Yalniz FF, Hanson CA, Ketterling RP, Lasho TL, et al. Therapy Related-Chronic Myelomonocytic Leukemia (CMML): Molecular, Cytogenetic, and Clinical Distinctions From De Novo CMML. Am J Hematol (2018) 93:65–73. doi: 10.1002/ajh.24939
86. Schuler E, Frank F, Hildebrandt B, Betz B, Strupp C, Rudelius M, et al. Myelodysplastic Syndromes Without Peripheral Monocytosis But With Evidence of Marrow Monocytosis Share Clinical and Molecular Characteristics With CMML. Leuk Res (2018) 65:1–4. doi: 10.1016/j.leukres.2017.12.002
87. Valent P. Oligo-Monocytic CMML and Other Pre-CMML States: Clinical Impact, Prognostication and Management. Best Pract Res Clin Haematol (2020) 33:101137. doi: 10.1016/j.beha.2019.101137
88. Heibl S, Gisslinger B, Jäger E, Barna A, Gurbisz M, Stegemann M, et al. Clinical, Hematologic, Biologic and Molecular Characteristics of Patients With Myeloproliferative Neoplasms and a Chronic Myelomonocytic Leukemia-Like Phenotype. Cancers (Basel) (2020) 12:1891. doi: 10.3390/cancers12071891
89. Brizard A, Huret JL, Lamotte F, Guilhot F, Benz-Lemoine E, Giraud C, et al. Three Cases of Myelodysplastic-Myeloproliferative Disorder With Abnormal Chromatin Clumping in Granulocytes. Br J Haematol (1989) 72:294–5. doi: 10.1111/j.1365-2141.1989.tb07703.x
90. Felman P, Bryon PA, Gentilhomme O, Ffrench M, Charrin C, Espinouse D, et al. The Syndrome of Abnormal Chromatin Clumping in Leucocytes: A Myelodysplastic Disorder With Proliferative Features? Br J Haematol (1988) 70:49–54. doi: 10.1111/j.1365-2141.1988.tb02433.x
91. Gustke SS, Becker GA, Garancis JC, Geimer NF, Pisciotta AV. Chromatin Clumping in Mature Leukocytes: A Hitherto Unrecognized Abnormality. Abnormal Chromatin Clumping in Leucocytes: A Clue to a New Subtype of Myelodysplastic Syndrome. Blood (1970) 35:637–58. doi: 10.1182/blood.V35.5.637.637
92. Jaén A, Irriguible D, Milla F, Vallespi T, Torrabadella M, Abella E, et al. Abnormal Chromatin Clumping in Leucocytes: a Clue to a New Subtype of Myelodysplastic Syndrome. Eur J Haematol (1990) 45:209–14. doi: 10.1111/j.1600-0609.1990.tb00459.x
93. Germing U, Kündgen A, Gattermann N. Risk Assessment in Chronic Myelomonocytic Leukemia (CMML). Leuk Lymphoma (2004) 45(7):1311–8. doi: 10.1080/1042819042000207271
94. Schuler E, Schroeder M, Neukirchen J, Strupp C, Xicoy B, Kündgen A, et al. Refined Medullary Blast and White Blood Cell Count Based Classification of Chronic Myelomonocytic Leukemias. Leuk Res (2014) 38:1413–9. doi: 10.1016/j.leukres.2014.09.003
95. Meggendorfer M, Roller A, Haferlach T, Eder C, Dicker F, Grossmann V, et al. SRSF2 Mutations in 275 Cases With Chronic Myelomonocytic Leukemia (CMML). Blood (2012) 120:3080–8. doi: 10.1182/blood-2012-01-404863
96. Hasle H, Aricò M, Basso G, Biondi A, Cantù Rajnoldi A, Creutzig U, et al. Myelodysplastic Syndrome, Juvenile Myelomonocytic Leukemia, and Acute Myeloid Leukemia Associated With Complete or Partial Monosomy 7. European Working Group on MDS in Childhood (EWOG-MDS). Leukemia (1999) 13:376–85. doi: 10.1038/sj.leu.2401342
97. Piazza R, Valletta S, Winkelmann N, Redaelli S, Spinelli R, Pirola A, et al. Recurrent SETBP1 Mutations in Atypical Chronic Myeloid Leukemia. Nat Genet (2013) 45:18–24. doi: 10.1038/ng.2495
Keywords: MDS/MPN, overlap syndromes, CMML, MDS/MPN-RS-T, aCML, JMML, MDS/MPN-U, epidemiology
Citation: Kuendgen A, Kasprzak A and Germing U (2021) Hybrid or Mixed Myelodysplastic/Myeloproliferative Disorders – Epidemiological Features and Overview. Front. Oncol. 11:778741. doi: 10.3389/fonc.2021.778741
Received: 17 September 2021; Accepted: 25 October 2021;
Published: 16 November 2021.
Edited by:
Cyrus Khandanpour, University Hospital Münster, GermanyReviewed by:
Rosa Ayala, Research Institute Hospital 12 de Octubre, SpainRoberto Latagliata, Unitelma Sapienza University, Italy
Copyright © 2021 Kuendgen, Kasprzak and Germing. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrea Kuendgen, a3VlbmRnZW5AbWVkLnVuaS1kdWVzc2VsZG9yZi5kZQ==
 Andrea Kuendgen
Andrea Kuendgen Annika Kasprzak
Annika Kasprzak Ulrich Germing
Ulrich Germing