- 1Department of Science and Education, Bozhou Hospital of Anhui Medical University, Bozhou, China
- 2Department of Cardiovascular Medicine, Bozhou Hospital of Anhui Medical University, Bozhou, China
- 3Department of Pathology, Bozhou Hospital of Anhui Medical University, Bozhou, China
- 4Department of medicine, Anhui University of Science and Technology, Huainan, China
- 5Department of Otorhinolaryngology, Bozhou Hospital of Anhui Medical University, Bozhou, China
Objective: The present study was designed to investigate the role of the chemokine CXCL7 in angiogenesis and explore its prognostic value in colorectal cancer (CRC).
Methods: A total of 160 CRC patients who had undergone surgery were included in this study, and staged according to the guidelines of the AJCC, 7th Edition. Expression of CXCL7 and VEGF was detected by immunohistochemical (IHC) staining and divided into high and low expression subgroups. The correlation between CXCL7 and VEGF expression was evaluated by Spearman’s rank-correlation coefficient. Prognosis based on CXCL7 and VEGF was evaluated using the Cox proportional hazards regression model and a nomogram of 5-year overall survival (OS) time.
Results: CXCL7 was highly expressed in tumor tissues (65.63% vs 25.00% in paracancerous tissue, P < 0.001), as was VEGF. CXCL7 and VEGF expression correlated well with N and TNM stage cancers (all P < 0.001). Importantly, CXCL7 was positively correlated with VEGF expression in CRC tissues. CXCL7 was an independent predictor of poor OS of CRC patients (HR = 2.216, 95% CI: 1.069-4.593, P = 0.032), and co-expression of CXCL7 and VEGF of predicted poor OS of 56.96 months.
Conclusion: Expression of CXCL7 correlated with VEGF and was associated with poor clinical outcomes in CRC patients.
Introduction
Colorectal cancer (CRC) is one of the deadliest malignant tumors with over 1.8 million new cases worldwide each year, and contributes to about 10% of tumor-related deaths (1). In fact, 746,000 men and 614,000 women were diagnosed with CRC in developed countries, accounting for 55% of all cancer cases (2). Although the incidence of CRC has been stable and has actually declined in some developed countries owing to the improvements in lifestyle, environmental factors, medical and health conditions (3), new cases of CRC are expected to increase to 2.2 million and deaths to 1.1 million globally by 2030 (4). Therefore, it is vital to control the occurrence and development of CRC to better manage the substantial health burden. The incidence and mortality of CRC are increasing in China due to the aging population and advanced stages of the disease (5–7). Patients aged 75 years and over constitute a large proportion of new CRC cases (above 40%), and about 45% patients are in advanced stages when first diagnosed (8, 9). The 5-year survival rate is 92% in stage I CRC patients, but drops to 10% when patients are in advanced stage IV (10). Although progress in CRC diagnosis and treatment, including traditional surgical resection, radiotherapy, chemotherapy, and newly targeted immunotherapy, has been achieved, the long-term prognosis, especially in terms of 5-year survival rate, has not improved significantly in recent decades (11).
Angiogenesis is a physiological process whereby new blood vessels are generated from existing vessels, and is regulated by a variety of signaling pathways that dynamically balance pro- and anti-angiogenic responses under normal physiological conditions (12). However, angiogenesis can become abnormally active in response to injuries, the menstrual cycle, and some metabolic diseases (13). Many studies have shown that angiogenesis plays an important role in cancer by providing oxygen, nutrients and other factors in the tumor microenvironment to stimulate tumor growth and accelerate disease progression (14). Numerous factors are involved in angiogenesis, being roughly divided into two types: proangiogenic and antiangiogenic. Vascular endothelial growth factor (VEGF) and its corresponding receptors play an extremely important role in tumor angiogenesis. VEGF is a secreted glycoprotein dimer that promotes angiogenesis by binding to its receptors (15). VEGF exerts its biological functions by activating tyrosine protein kinase. Meanwhile, VEGF can increase capillary permeability, which allows fibrinogen and other proteins to diffuse into the extracellular matrix where they crosslink into a fibrous gel, thus effectively promoting formation of a capillary network (15, 16). VEGF is highly expressed in many tumors where it is the strongest driver of angiogenesis, thus contributing to tumor growth and metastasis (17, 18).
Chemokines are low-molecular-weight signaling proteins (8–12 kDa) that can regulate many biological processes, including cellular immune response, glucose metabolism and angiogenesis (19–22). Chemokines play important regulatory roles by binding to their specific receptors (23). Recently, numerous studies have shown that various chemokines play important roles in tumorigenesis, including regulation of proliferation, tumor metastasis, angiogenesis, among others (24–27). Chemokines also affect cancer diagnosis and treatment by interacting with tumor cells and the tumor immune environment (28, 29). CXCL7, also called neutrophil activating peptide 2, functions by binding to its receptors CXCR1 and CXCR2, and plays important roles in a variety of tumor processes (30–32).
Our previous study showed that CXCL7 is highly expressed in CRC with poor prognosis (30, 33). However, the role of CXCL7 in angiogenesis is unknown. In the current study we probed the function of CXCL7 in angiogenesis and evaluated its prognostic value by analyzing clinical data from a total of 160 CRC patients, including 2 in Stage I, 67 in Stage II, 69 in Stage III and 22 in Stage IV CRC. We assessed the correlation between CXCL7 and VEGF expression and systematically explored the value of CXCL7 for prognosis in CRC.
Materials and Methods
Patient Selection and Tissue Sample Collection
The subjects were enrolled according to the following criteria. (1) Patients were firstly diagnosed in Bozhou Hospital of Anhui Medical University from July 2013 to July 2018. (2) Patients whose condition met the criteria for surgical resection were enrolled in the study. (3) Preoperative clinical diagnosis was consistent with postoperative pathological diagnosis in indicating colorectal cancer. (4) Patients had not received radiotherapy and chemotherapy prior to surgery. (5) The patient’s clinical data was relatively complete. Other terms and selection criteria for healthy participants were described in our previous study (30, 33). These criteria were met by 200 patients. However, 40 people were not eligible during the follow-up. Therefore, 160 patients were included in this study finally (Supplementary Figure 1). Patient data included demographic characteristics and clinical pathology results. All patients were staged according to AJCC (American Joint Committee on Cancer) guidelines, 7th Edition (34). The study was approved by the Institutional Research Ethics Committee of our hospital, and 160 written informed consents were obtained. Tumor and adjacent non-tumor tissues were collected from all 160 patients, then fixed by formalin and embedded in paraffin.
Immunohistochemical Staining Assay
Serial sections of 4 μm thickness were cut from each of the 320 paraffin blocks. IHC staining was performed according to the manufacturer’s instructions using anti-CXCL7 mouse monoclonal antibody (1:200, Abcom Ltd., Cam-bridge, UK) and anti-VEGF rabbit monoclonal antibody (1:300, Abcom Ltd., Cam-bridge, UK). The IHC process made use of an automated immunostainer (Thermo Fisher Scientific, MA, USA). IHC staining was scored by two pathologists, and scores were only accepted when they were in agreement. Light microscopy images were obtained from each slice at 40× magnification. Overall IHC staining was scored as either 0 (none), 1 (weak), 2 (moderate), or 3 (strong). The percentage of positively-stained cells was recorded as either 0 (≤5%), 1(6%–25%), 2(26%–75%), or 3(>75%). The final score was 0–9, calculated as the product of the scores for overall IHC staining and percentage positive staining. The cutoff value for IHC staining was calculated using the receiver operating characteristic (ROC) curve and the Youden Index (sensitivity+specificity-1). The final score was taken to represent high expression when it was greater than the cutoff value, and low expression when less than or equal to the cutoff.
Methods of Postoperative Follow-Up and Collection of Related Information
Two doctors were responsible for follow-up and collection of patient information. Postoperative survival times of CRC patients were collected at 3 months and 1, 2, 3, 5, and 8 years after surgery; follow-up was halted if the patient died. Patient data was categorized according to (1) CXCL7 and VEGF staining in cancer and adjacent normal tissues, (2) age and gender, and (3) pathological parameters (30).
Statistical Analysis
The results of categorical variables were presented as frequencies (n) and percentages (%) in this study. The mean (M) and standard deviation (SD) were used to represent numerical variables. Expression of CXCL7 and VEGF were sequentially tested in different variables by Pearson’s chi-square test. Differences between CXCL7 and VEGF expression were analyzed by the Mann-Whitney U-test. Spearman’s rank-correlation test was used to evaluate the correlation between CXCL7 and VEGF expression. The 5-year overall survival (OS) time was calculated using Kaplan-Meier analysis, and graphs of survival rate are shown in Results. Cox proportional hazard regression models were used for analyzing risk factors used in prognoses for CRC patients. First, statistically significant indicators were selected by univariate analysis. Then, multivariate regression models were employed to seek out independent prognostic factors. R 4.0.0 software was used to draw a nomogram of 5-year OS. In addition, the concordance index (C-index), the area under the ROC curve (AUC), and the calibration curve were used to evaluate the predictive ability of the nomogram model. SPSS 22.0 software (IBM; Armonk, NY, USA) was used to analyze all data in this study. Statistical differences were significant for P value < 0.05.
Results
General Clinical Information of CRC Patients
One hundred and sixty patients who had been definitively diagnosed with CRC were recruited, including 73 women (45.63%, 73/160) and 87 men (54.37%, 87/160). The average age was 59.46 ± 9.13 years for women and 58.17 ± 11.24 years for men (Table 1). Patients were classified into two groups based on age: ≤ 60 (55.00%, 88/160) and > 60 (45.00%, 72/160). Other CRC patient information was shown in Table 1.
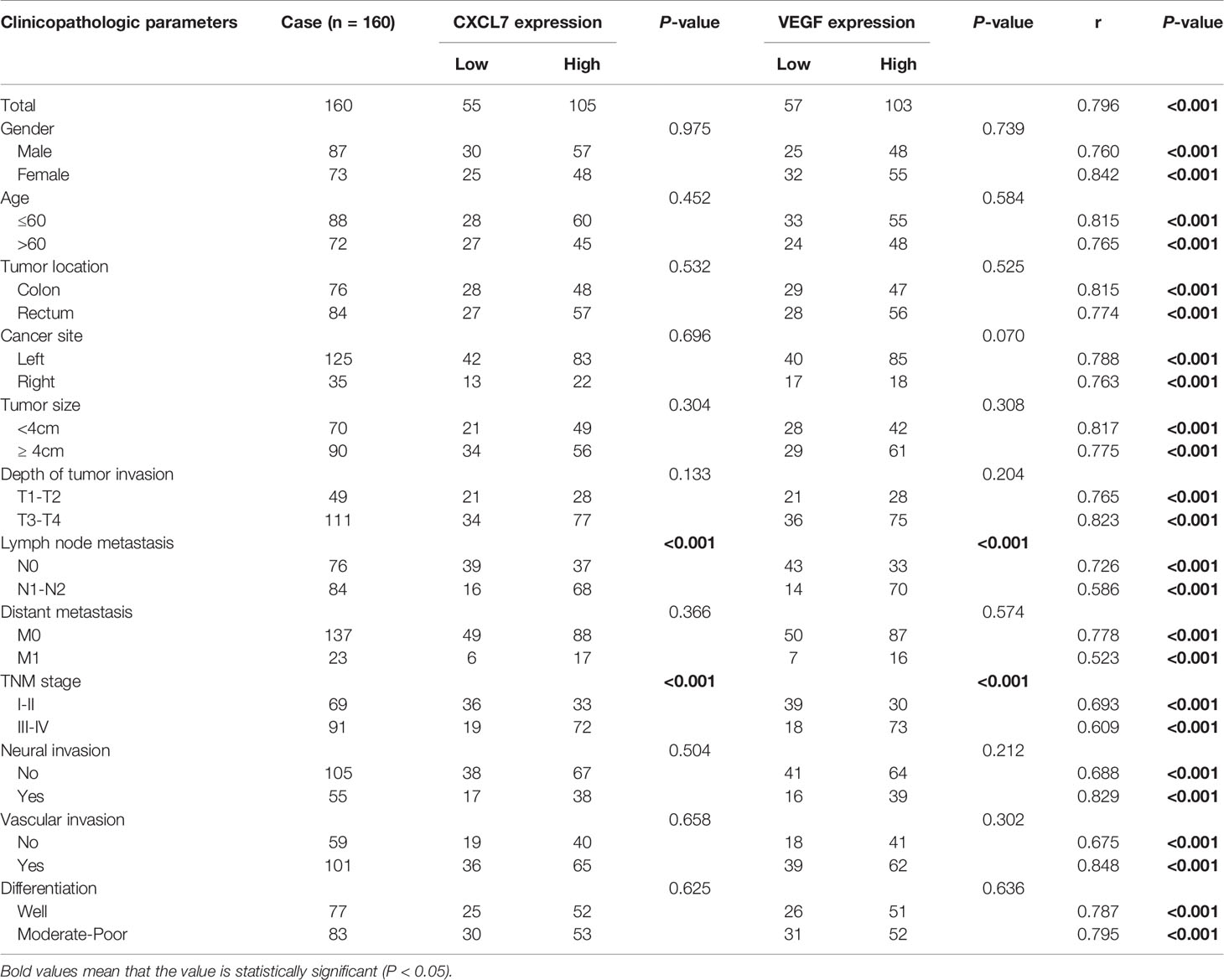
Table 1 Association of CXCL7 and VEGF with clinical pathological characteristics and the correlation between two markers in CRC patients.
Expression of CXCL7 and VEGF in CRC Tissues
IHC was used to monitor expression of CXCL7 and VEGF in CRC tumors and adjacent normal tissues. Based on the ROC curve, a score of 3.5 was selected as the cutoff value for CXCL7, and 2.8 for VEGF. Similar to our previous research, CXCL7 was highly expressed in tumor tissues (65.63%, 105/160) but not in paracancerous tissue (25.00%, 40/160, P < 0.001; Figures 1A, B). Positive staining was mainly concentrated in the cytoplasm and membranes of CRC cells (Figure 1A). Similarly, we found that VEGF was also highly expressed in CRC tissues (64.38%, 103/160 vs. 26.25%, 42/160 in normal tissues, Figures 1C, D). Number of ICH score was shown in Figure 1E.
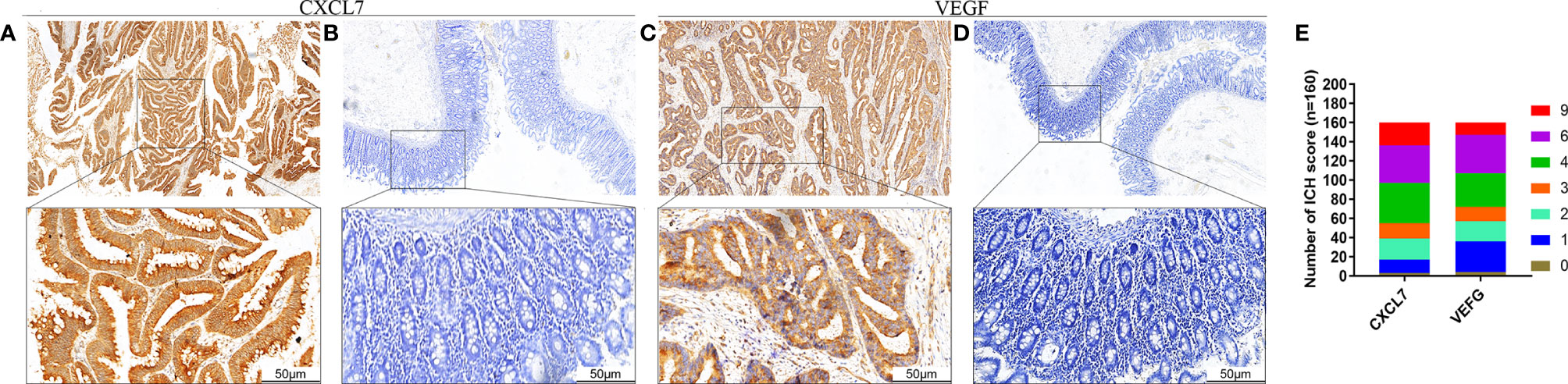
Figure 1 Expression of CXCL7 and VEGF in CRC patients. (A) Expression of CXCL7 in tumor tissues (magnification: 40× and 200×). (B) Expression of CXCL7 in normal tissues (40× and 200×). (C) Expression of VEGF in tumor tissues (40× and 200×). (D) Expression of VEGF in normal tissues (40× and 200×). (E) Patients were classified according to CXCL7 and VEGF IHC score from 0 to 9. Scale bar, 50 μm.
Associations Between CXCL7, VEGF and Clinicopathological Characteristics in CRC Patients
In order to probe the clinical significance of CXCL7 and VEGF in CRC, associations between these two markers and clinicopathological information were analyzed by the chi-square (χ2) test, and differences in expression were assessed by the Mann-Whitney U test. CXCL7 was correlated with N- and TNM-stage cancer (both P < 0.001; Figures 2A, B and Table 1), as was VEGF (both P < 0.001; Figures 2C, D and Table 1). However, there were no significant correlations between CXCL7 or VEGF and other clinicopathological characteristics (all P > 0.05; Table 1).
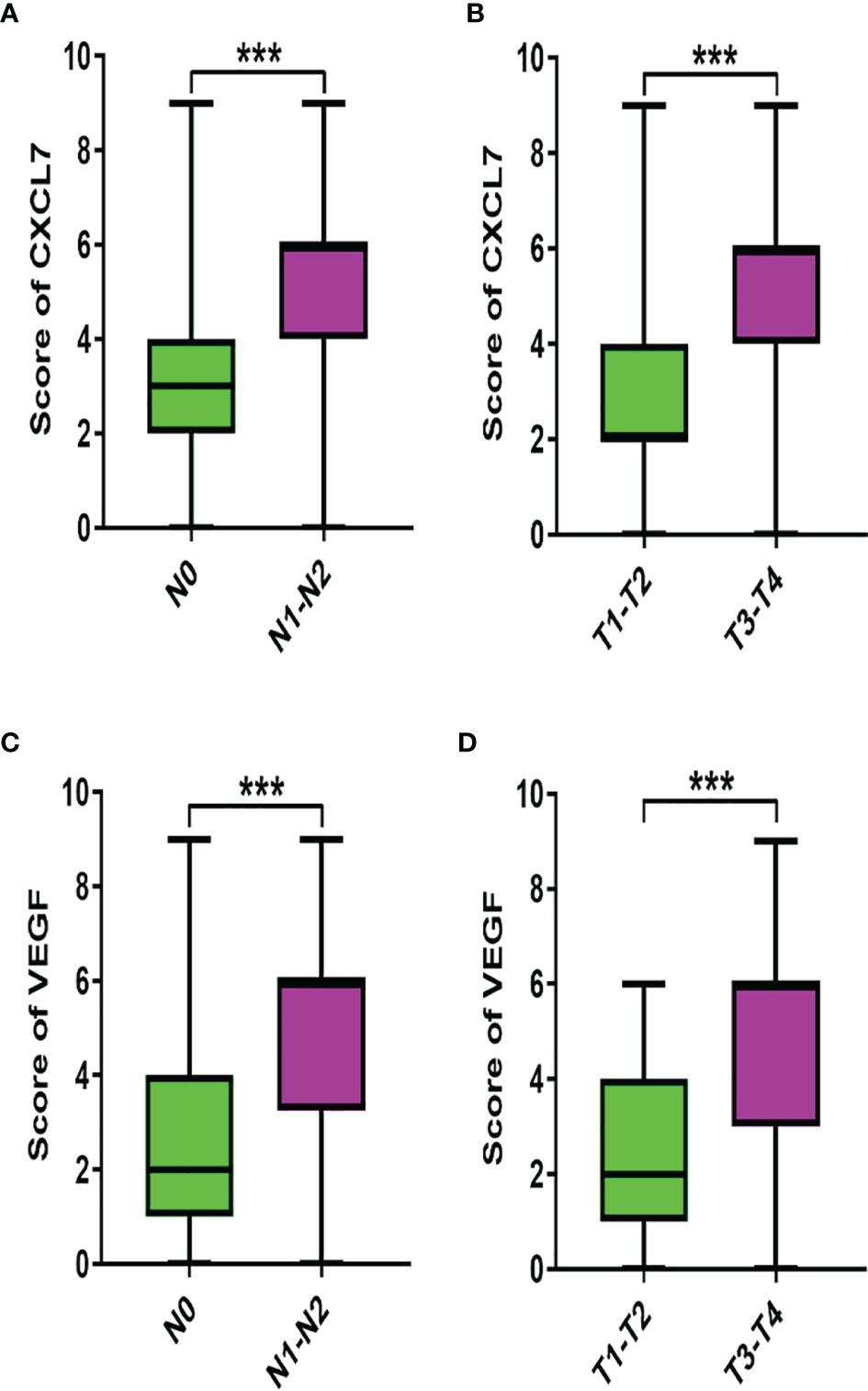
Figure 2 Associations between CXCL7 and VEGF and clinicopathological characteristics. (A) Expression of CXCL7 in different N-stage tumors. (B) Expression of CXCL7 in different TNM stages. (C) VEGF in N0 and N1-N2 stage tumors. (D) VEGF in I-II and III-IV stages. The Mann‐Whitney U-test was used for analysis. ***P < 0.001.
Clinical Correlation Between CXCL7 and VEGF in CRC Patients
To analyze whether expression of CXCL7 was related to the level of VEGF in CRC tissue, Spearman’s test was used to evaluate the correlation. Interestingly, there was a significant correlation between CXCL7 and VEGF in all CRC tissues (correlation coefficient: 0.796, P < 0.001, Figure 3A). We then explored whether there were correlations with other clinical features. Scatter plots were used to visualize results for the two markers. As shown in Figure 3, the correlation coefficients ranged from 0.523 to 0.842 (all P < 0.01), with the highest being for the female subgroup (r= 0.842) and the lowest for the M1 subgroup (r= 0.523, Figures 3A–Y and Table 1). These results illustrated a strong correlation between CXCL7 and VEGF in CRC tissues.
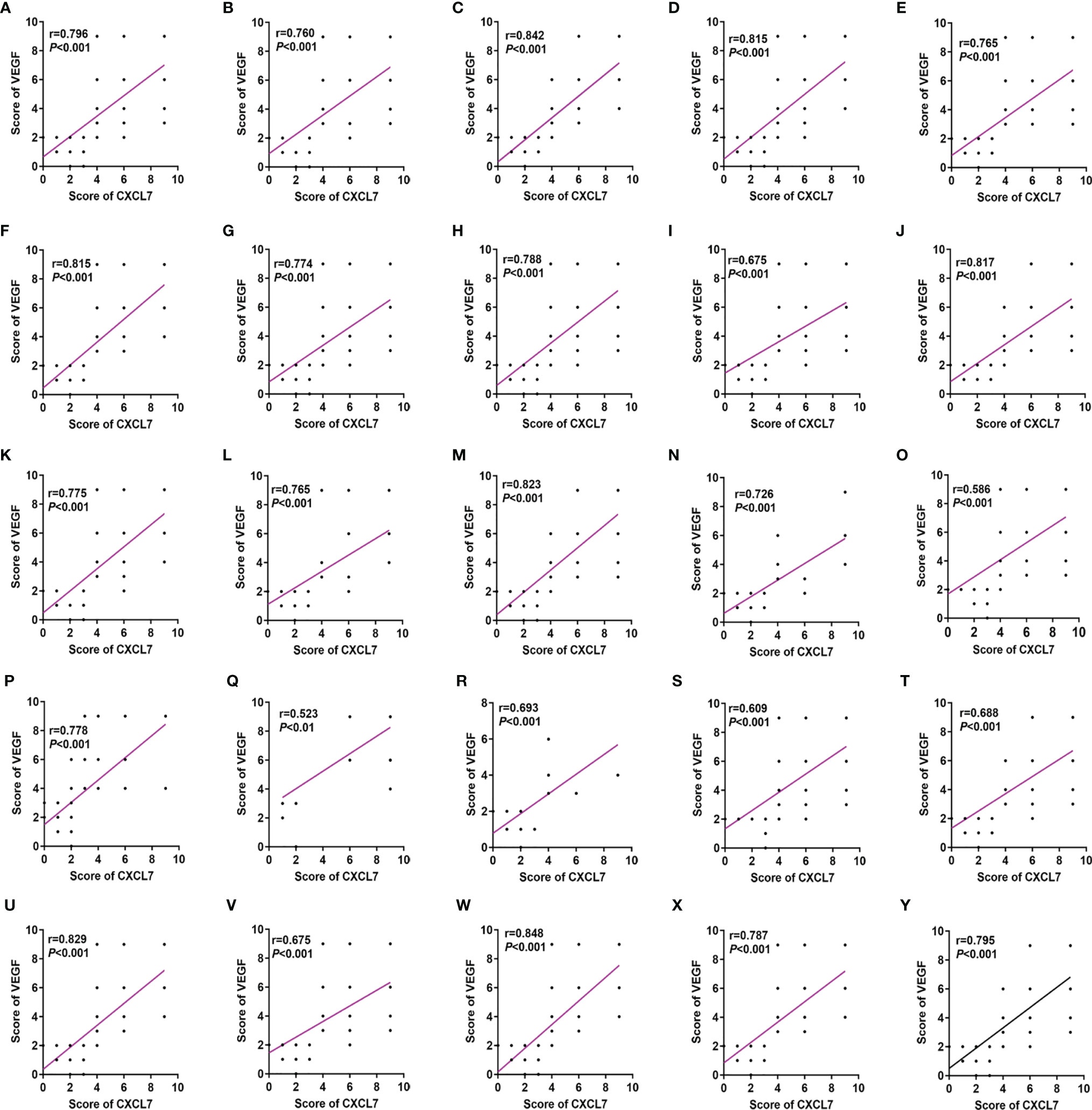
Figure 3 CXCL7 positively correlated with VEGF in CRC patients grouped according to various clinical features. (A) All CRC patients. (B) Male subgroup. (C) Female subgroup. (D) Age ≤ 60 years subgroup. (E) Age > 60 years subgroup. (F) Colon subgroup. (G) Rectum subgroup. (H) Left subgroup. (I) Right subgroup. (J) Tumor size <4 cm subgroup. (K) Tumor size ≥4 cm subgroup. (L) T1-T2 subgroup. (M) T3-T4 subgroup. (N) N0 subgroup. (O) N1-N2 subgroup. (P) M0 subgroup. (Q) M1 subgroup. (R) I-II subgroup. (S) III-IV subgroup. (T) Non-neural invasion subgroup. (U) Neural invasion subgroup. (V) Non-vascular invasion subgroup. (W) Vascular invasion subgroup. (X) Well differentiated subgroup. (Y) Moderately-poorly differentiated subgroup. The non-parametric Spearman’s test was used for these analyses.
High Expression of CXCL7 and VEGF Related to Poor Prognosis in CRC Patients
For the purpose of establishing the prognostic significance of CXCL7 and VEGF in CRC, the 160 patients were observed to have a median OS time of 67.00 (95% confidence interval [CI]: 61.37–72.63) months and a 5-year survival rate of 62.60% (Figure 4A). Interestingly, OS time was affected by extent of tumor invasion. There were significant differences in OS among the tumor stages: T (hazard ratio [HR]: 1.711; 95% CI: 1.048–2.793; P =0.032; Figure 4G), N (HR: 3.717; 95% CI: 2.160-6.397; P <0.001; Figure 4H), M (HR: 3.696; 95% CI: 1.991–6.862; P <0.001; Figure 4I), TNM (HR: 3.765; 95% CI: 1.828–7.756; P <0.001; Figure 4J), and level of CXCL7 (HR: 2.343; 95% CI: 1.431–3.837; P =0.001; Figure 4N) and VEGF (HR: 1.931; 95% CI: 1.189–3.136, P = 0.008; Figure 4O). Details are shown in Table 2. However, no significant differences were found among the other factors (Figures 4B–F, K–M and Table 2; all P >0.05). Multivariate analysis showed that high CXCL7 in tissues was independent of factors associated with poor OS of CRC patients (HR=2.363; 95% CI: 1.359–4.108; P = 0.002; Table 2). Patients with high levels of both CXCL7 and VEGF had poor outcomes (OS: 56.96 months vs 78.00 months in patients with low levels of each, HR: 2.410; 95% CI: 1.405-4.132; P = 0.001; Figure 4P).
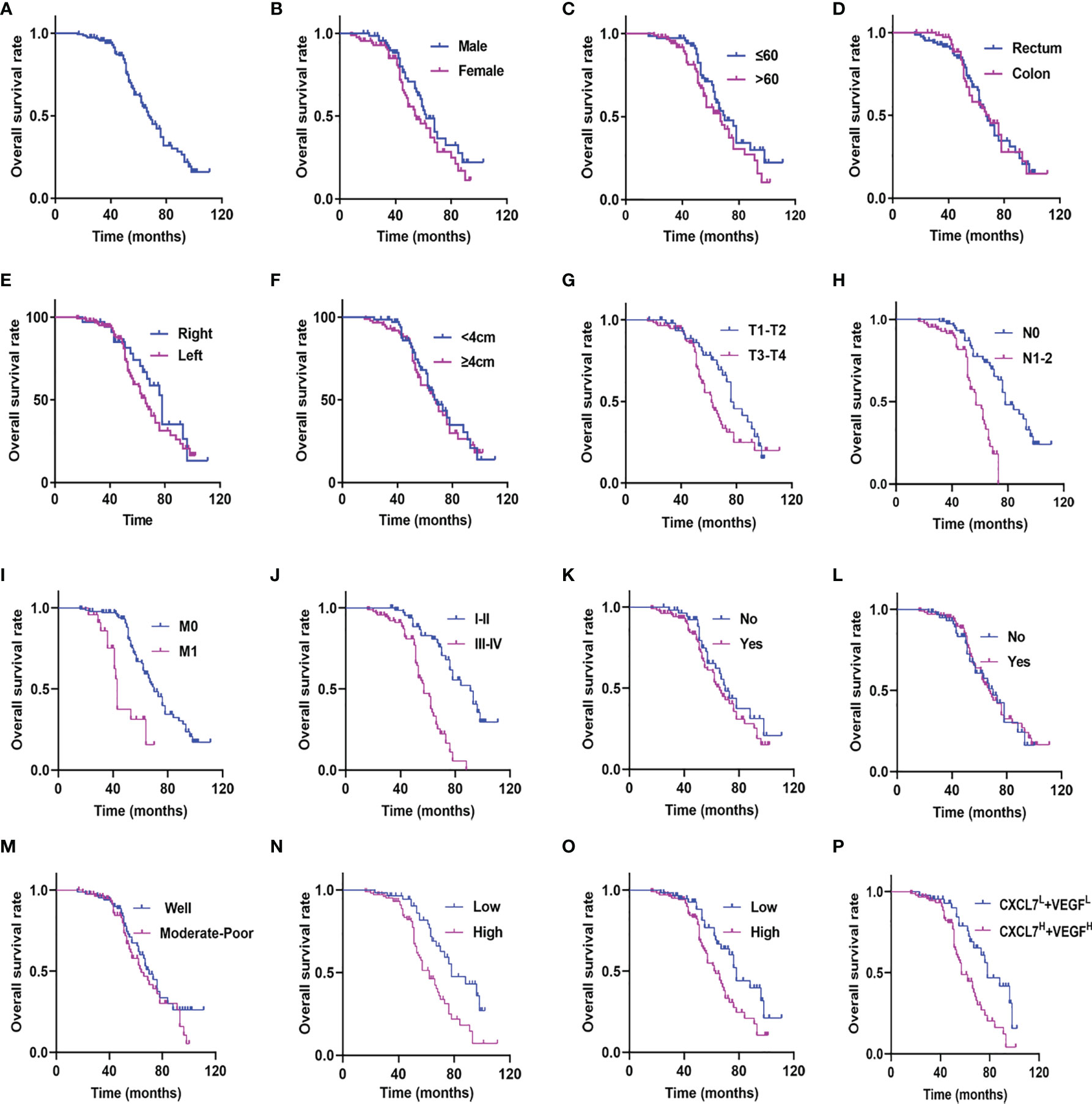
Figure 4 Kaplan-Meier curves for CRC patients stratified on the basis of CXCL7, VEGF and clinicopathological features. (A) OS in all 160 patients. (B) OS in male vs. female patients (P = 0.133). (C) OS in age ≤60 vs. age >60 patients (P = 0.117). (D) OS in colon vs. rectum patients (P = 0.899). (E) OS in left side vs. right side patients (P = 0.252). (F) OS in tumor size <4 cm vs. ≥4 cm patients (P = 0.740). (G) OS in T1-T2 vs. T3-T4 patients (P = 0.032). (H) OS in N0 vs. N1-N2 patients (P < 0.001). (I) OS in M0 vs. M1 patients (P < 0.001). (J) OS in I-II vs. III-IV patients (P < 0.001). (K) OS in non-neural invasion vs. neural invasion patients (P = 0.271). (L) OS in non-vascular invasion vs. vascular invasion patients (P = 0.859). (M) OS in well differentiated vs. moderately-poorly differentiated patients (P = 0.271). (N) OS in CXCL7 low expression (CXCL7L) vs. CXCL7 high expression (CXCL7H) patients (P = 0.001). (O) OS in VEGF low expression (VEGFL) vs. VEGF high expression (VEGFH) patients (P = 0.008). (P) OS in CXCL7H + VEGFH vs. CXCL7L +VEGFL patients (P = 0.001).
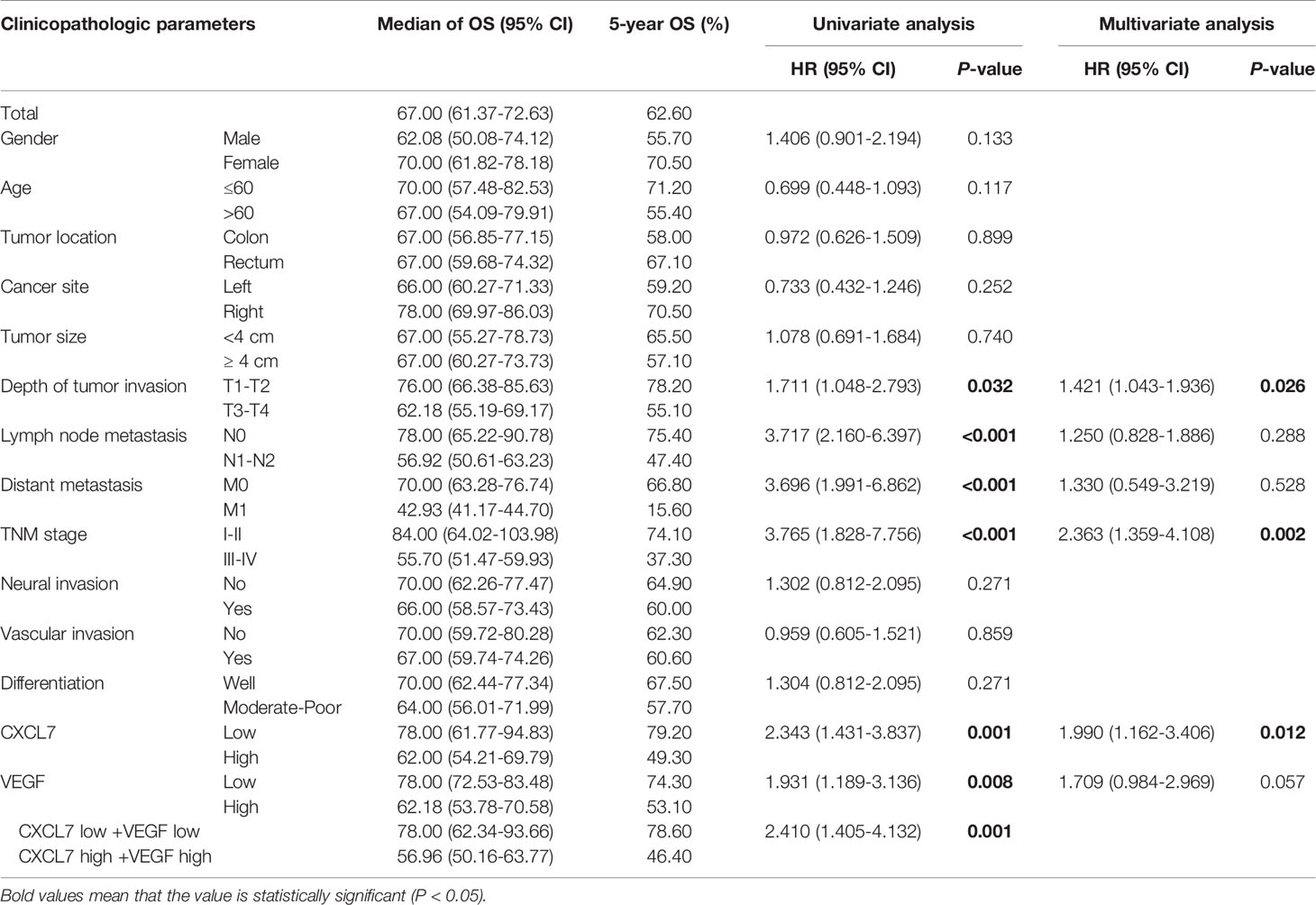
Table 2 Cox proportional hazard regression models for CXCL7, VEGF and clinical pathological characteristics.
A Prognostic Nomogram for Comprehensively Evaluating OS in CRC Patients
As nomograms are widely used in prognostic assessments, especially for cancer, we generated a nomogram using the R software package to analyze the value of CXCL7, VEGF and various pathological features in making a CRC prognosis (Figure 5A). First, a standard point-scale reference line was established on the top of the nomogram. Then, CXCL7, VEGF and related clinical and pathological information were listed in order. The total point score was then calculated for prediction of 5-year OS (only 5-year OS was evaluated in this study). From the nomogram, patients could be provided with a personalized evaluation for guiding clinical treatment following surgery. The length of each variable was associated with patient survival. TNM stage, neural invasion, CXCL7 expression and differentiation had the greatest impact on prognosis.
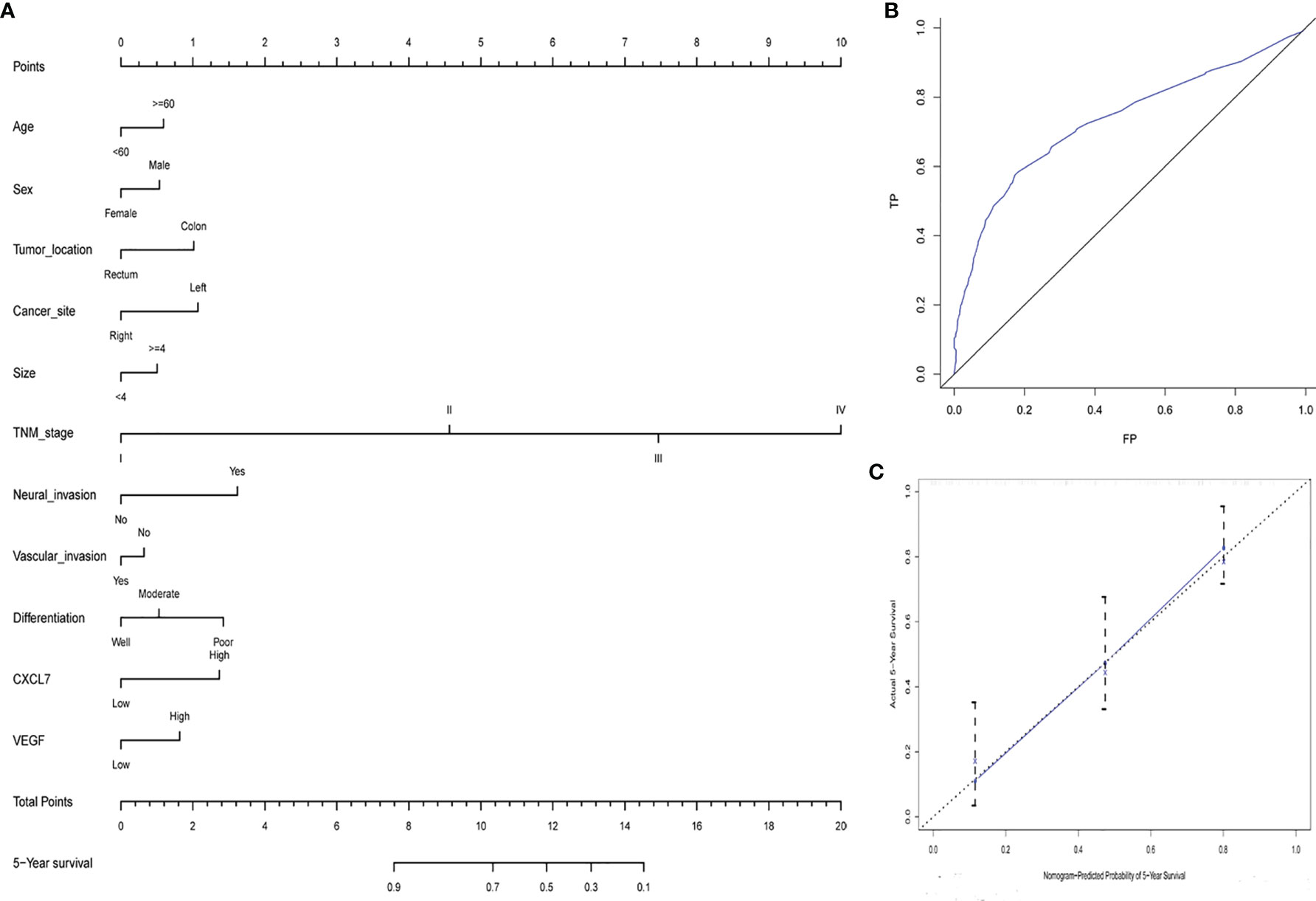
Figure 5 Nomogram of CRC patients’ 5-year survival time following surgery. (A) Nomogram for 5‐year OS on the basis of CXCL7 and VEGF expression and basic clinical data. (B) ROC curve for developing the nomogram. (C) Calibration curve of the nomogram.
The nomogram was also quantitatively assessed using the concordance index (C-index), area under the ROC curve (AUC), and calibration curve. The C-index was 0.747 (95% CI: 0.701–0.826). The 5‐year survival AUC was 0.734 (95% CI: 0.672–0.797; Figure 5B), and the calibration curve was shown in Figure 5C. Overall, the nomogram for 5-year OS could be used to make a reliable prognosis for CRC patients.
Discussion
CRC is a serious public health challenge associated with high mortality and morbidity worldwide, especially in developing countries such as China (35). Although numerous improvements related to diagnosis and treatment have been applied in clinical practice, the number of tumor-related deaths has continued to rise over the past few years (36). Surgery and postoperative radiotherapy and chemotherapy are standard treatments for CRC. Improvement of OS following surgery for CRC requires systematic evaluation and management (37). TNM stage has been used as a predictor of survival time in recent decades (38), although it is not always accurate. For this reason, recurrence and metastasis after treatment are usually included as risk factors for prognosis. Of course, a great many studies in the past few decades have identified novel prognostic biomarkers (39–41). Various studies have found that angiogenesis plays an important role in recurrence and metastasis (42, 43). Even though many proteins and signaling molecules have been associated with angiogenesis in CRC cells (44, 45), the connection between CXCL7 and angiogenesis has not previously been explored. In this study, we performed series of experiments to evaluate the association of CXCL7 with angiogenesis, and assess its value in prognosis of CRC patients.
CXCL7, a neutrophil-activating chemokine, is primarily derived from peripheral platelets (46). Traditionally, CXCL7 has been considered to be involved in regulating glycolysis, mitosis, and prostaglandin synthesis, among other processes (46, 47). Recently, several studies have reported that CXCL7 is associated with many types of tumors, and plays important roles in tumor proliferation and metastasis (48, 49). We used IHC to show that CXCL7 was significantly over-expressed in CRC tumor cells, correlated with N-stage and TNM-stage cancer, and associated with poor patient outcomes. CXCL7 was evaluated as a CRC biomarker in our previous study (30), and together with the present study has been shown be a potentially reliable marker for making prognoses in CRC patients.
Angiogenesis, an important physiological process, also plays a pivotal role in tumor proliferation, invasion and metastasis (12, 13). A variety of proteins are involved in regulation of angiogenesis, including VEGF and other cytokines and chemokines (13, 14). Here, VEGF was highly expressed in CRC tumors and correlated with poor prognosis. As the role of VEGF in angiogenesis is widely known, anti-VEGF treatment drugs such as bevacizumab and many traditional plant polysaccharides (50, 51) are commonly used in anti-cancer treatments.
Previously we have focused on CXCL7 in serum from CRC patients (30), and its potential application to prognosis of obstructive colorectal cancer (33); however, the relationship between CXCL7 and angiogenesis has not previously been evaluated. In recent years, the role of chemokines in regulating angiogenesis has been revealed in several studies (52, 53), including the ability of CCL19 to suppress angiogenesis by downregulating VEGF-A expression in CRC cells (53). So, numerous studies have provided us with data upon which to base an investigation of the role of CXCL7 in angiogenesis in CRC patients. We chose VEGF as a marker of angiogenesis and used IHC to evaluate its expression in CRC cells. Then, the relationship between CXCL7 and VEGF expression was analyzed, and we found that the two were positively correlated. Based on these results, we conclude that CXCL7 prominently correlates with VEGF and clinicopathological features in CRC patients. Furthermore, univariate analysis showed that high expression of CXCL7 with VEGF is a risk factor that can be considered in prognosis of CRC patients. However, VEGF was not an independent risk factor in CRC patients. The nomogram and its corresponding evaluation index also showed that CXCL7 was associated with outcome in CRC patients. Based on the above results, we suggest that CXCL7 may regulate expression of VEGF in CRC tissues, maybe for the reason that angiogenic functions can be induced by chemokine-regulated inflammatory stimuli (48, 54–56). Because the treatment methods are also very important for the patient’s prognosis, the related surgery, radiotherapy and chemotherapy methods will be taken into consideration for comprehensively exploring the factors which could affect patient survival time in future study. Furthermore, the relationship between CXCL7 and VEGF should be further studied in vivo and in vitro, including in CRC serum and cell lines.
In summary, this study analyzed the correlation between CXCL7 and VEGF, and illustrated that co-expression of the two markers leads to a poor prognosis in CRC patients. As chemokines have been suggested to be therapeutic targets in many studies (57, 58), CXCL7 may be a new target for regulating angiogenic signaling pathways, especially those controlling VEGF expression.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Author Contributions
LL, KJ, DPL, DXL, GD, ST, GW, and XL conceived the study. LL, DPL, and ST performed the experiments and were responsible for statistical analysis. LL, KJ, and DPL were in charge of writing review, revision and other related work in this study. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Bozhou science and technology major special projects (No. bzzd2020012), the Bozhou Key R&D projects (No.bzzc2021020) and the incubation project of Bozhou People’s Hospital (No.Byf202017).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2021.754221/full#supplementary-material
Supplementary Figure 1 | Flowchart for inclusion and exclusion of CRC patients.
Abbreviations
CRC, colorectal cancer; VEGF, vascular endothelial growth factor; IHC, immunohistochemical; TNM, tumor-node-metastasis; T, depth of tumor invasion; N, nodal involvement; M, distant metastasis; OS, overall survival time; C-index, concordance index; ROC, receiver operating characteristic; Mean (M) and standard deviation (SD); AUC, area under the ROC curve; HR, high risk factor.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin (2018) 68(6):394–424. doi: 10.3322/caac.21492
2. Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. Estimating the Global Cancer Incidence and Mortality in 2018: GLOBOCAN Sources and Methods. Int J Cancer (2019) 144(8):1941–53. doi: 10.1002/ijc.31937
3. Yang T, Li X, Montazeri Z, Little J, Farrington SM, Ioannidis JPA, et al. Gene-Environment Interactions and Colorectal Cancer Risk: An Umbrella Review of Systematic Reviews and Meta-Analyses of Observational Studies. Int J Cancer (2019) 145(9):2315–29. doi: 10.1002/ijc.32057
4. Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Patterns and Trends in Colorectal Cancer Incidence and Mortality. Gut (2017) 66(4):683–91. doi: 10.1136/gutjnl-2015-310912
5. Jacobs D, Zhu R, Luo J, Grisotti G, Heller DR, Kurbatov V, et al. Defining Early-Onset Colon and Rectal Cancer. Front Oncol (2018) 8:504. doi: 10.3389/fonc.2018.00504
6. Wan J, Yang J, Qiao CX, Sun X, Di A, Zhang L, et al. MicroRNA-362 Inhibits Cell Proliferation and Invasion by Directly Targeting SIX1 in Colorectal Cancer. Yonsei Med J (2019) 60(5):414–22. doi: 10.3349/ymj.2019.60.5.414
7. Chong RC, Ong MW, Tan KY. Managing Elderly With Colorectal Cancer. J Gastrointest Oncol (2019) 10(6):1266–73. doi: 10.21037/jgo.2019.09.04
8. Saleh R, Taha RZ, Toor SM, Sasidharan Nair V, Murshed K, Khawar M, et al. Expression of Immune Checkpoints and T Cell Exhaustion Markers in Early and Advanced Stages of Colorectal Cancer. Cancer Immunol Immunother (2020) 69(10):1989–99. doi: 10.1007/s00262-020-02593-w
9. Malvezzi M, Arfé A, Bertuccio P, Levi F, La Vecchia C, Negri E. European Cancer Mortality Predictions for the Year 2011. Ann Oncol (2011) 22(4):947–56. doi: 10.1093/annonc/mdq774
10. Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, et al. Colorectal Cancer Statistics, 2020. CA Cancer J Clin (2020) 70(3):145–64. doi: 10.3322/caac.21601
11. Dekker E, Rex DK. Advances in CRC Prevention: Screening and Surveillance. Gastroenterology (2018) 154(7):1970–84. doi: 10.1053/j.gastro.2018.01.069
12. De Heer EC, Jalving M, Harris AL. HIFs, Angiogenesis, and Metabolism: Elusive Enemies in Breast Cancer. J Clin Invest (2020) 130(10):5074–87. doi: 10.1172/JCI137552
13. Cao J, Liu X, Yang Y, Wei B, Li Q, Mao G, et al. Decylubiquinone Suppresses Breast Cancer Growth and Metastasis by Inhibiting Angiogenesis via the ROS/p53/ BAI1 Signaling Pathway. Angiogenesis (2020) 23(3):325–38. doi: 10.1007/s10456-020-09707-z
14. Bausch D, Fritz S, Bolm L, Wellner UF, Fernandez-Del-Castillo C, Warshaw AL, et al. Hedgehog Signaling Promotes Angiogenesis Directly and Indirectly in Pancreatic Cancer. Angiogenesis (2020) 23(3):479–92. doi: 10.1007/s10456-020-09725-x
15. Xie M, Yu T, Jing X, Ma L, Fan Y, Yang F, et al. Exosomal Circshkbp1 Promotes Gastric Cancer Progression via Regulating the miR-582-3p/HUR/VEGF Axis and Suppressing HSP90 Degradation. Mol Cancer (2020) 19(1):112. doi: 10.1186/s12943-020-01208-3
16. Braile M, Marcella S, Cristinziano L, Galdiero MR, Modestino L, Ferrara AL, et al. VEGF-A in Cardiomyocytes and Heart Diseases. Int J Mol Sci (2020) 21(15):5294. doi: 10.3390/ijms21155294
17. Hosaka K, Yang Y, Seki T, Du Q, Jing X, He X, et al. Therapeutic Paradigm of Dual Targeting VEGF and PDGF for Effectively Treating FGF-2 Off-Target Tumors. Nat Commun (2020) 11(1):3704. doi: 10.1038/s41467-020-17525-6
18. Eguchi R, Wakabayashi I. HDGF Enhances VEGF‐dependent Angiogenesis and FGF‐2 Is a VEGF‐independent Angiogenic Factor in Non‐Small Cell Lung Cancer. Oncol Rep (2020) 44(1):14–28. doi: 10.3892/or.2020.7580
19. Coperchini F, Chiovato L, Croce L, Magri F, Rotondi M. The Cytokine Storm in COVID-19: An Overview of the Involvement of the Chemokine/Chemokine-Receptor System. Cytokine Growth Factor Rev (2020) 53:25–32. doi: 10.1016/j.cytogfr.2020.05.003
20. Groblewska M, Litman-Zawadzka A, Mroczko B. The Role of Selected Chemokines and Their Receptors in the Development of Gliomas. Int J Mol Sci (2020) 21(10):3704. doi: 10.3390/ijms21103704
21. Morein D, Erlichman N, Ben-Baruch A. Beyond Cell Motility: The Expanding Roles of Chemokines and Their Receptors in Malignancy. Front Immunol (2020) 11:952. doi: 10.3389/fimmu.2020.00952
22. Wang L, Zhang S, Wang X. The Metabolic Mechanisms of Breast Cancer Metastasis. Front Oncol (2021) 10:602416. doi: 10.3389/fonc.2020.602416
23. Jin Y, Lin Q, Fei H, Xue L, Li L, Xi Q, et al. Bioinformatics Analysis of Potential Therapeutic Targets and Prognostic Biomarkers Amid CXC Chemokines in Ovarian Carcinoma Microenvironment. J Oncol (2021) 2021:8859554. doi: 10.1155/2021/8859554
24. Korbecki J, Grochans S, Gutowska I, Barczak K, Baranowska-Bosiacka I. CC Chemokines in a Tumor: A Review of Pro-Cancer and Anti-Cancer Properties of Receptors CCR5, CCR6, CCR7, CCR8, CCR9, and CCR10 Ligands. Int J Mol Sci (2020) 21(20):7619. doi: 10.3390/ijms21207619
25. Korbecki J, Kojder K, Simińska D, Bohatyrewicz R, Gutowska I, Chlubek D, et al. CC Chemokines in a Tumor: A Review of Pro-Cancer and Anti-Cancer Properties of the Ligands of Receptors CCR1, CCR2, CCR3, and CCR4. Int J Mol Sci (2020) 21(21):8412. doi: 10.3390/ijms21218412
26. Adekoya TO, Richardson RM. Cytokines and Chemokines as Mediators of Prostate Cancer Metastasis. Int J Mol Sci (2020) 21(12):4449. doi: 10.3390/ijms21124449
27. Liu H, Yang Z, Lu W, Chen Z, Chen L, Han S, et al. Chemokines and Chemokine Receptors: A New Strategy for Breast Cancer Therapy. Cancer Med (2020) 9(11):3786–99. doi: 10.1002/cam4.3014
28. Ferrari SM, Fallahi P, Elia G, Ragusa F, Ruffilli I, Paparo SR, et al. Thyroid Autoimmune Disorders and Cancer. Semin Cancer Biol (2020) 64:135–46. doi: 10.1016/j.semcancer.2019.05.019
29. Pawluczuk E, Łukaszewicz-Zając M, Mroczko B. The Role of Chemokines in the Development of Gastric Cancer -Diagnostic and Therapeutic Implications. Int J Mol Sci (2020) 21(22):8456. doi: 10.3390/ijms21228456
30. Li L, Zhang L, Tian Y, Zhang T, Duan G, Liu Y, et al. Serum Chemokine CXCL7 as a Diagnostic Biomarker for Colorectal Cancer. Front Oncol (2019) 9:921. doi: 10.3389/fonc.2019.00921
31. Finsterbusch M, Norman MU, Hall P, Kitching AR, Hickey MJ. Platelet Retention in Inflamed Glomeruli Occurs via Selective Prolongation of Interactions With Immune Cells. Kidney Int (2019) 95(2):363–74. doi: 10.1016/j.kint.2018.08.042
32. Cheng Y, Wang X, Wang B, Zhou H, Dang S, Shi Y, et al. Aging-Associated Oxidative Stress Inhibits Liver Progenitor Cell Activation in Mice. Aging (2017) 9(5):1359–74. doi: 10.18632/aging.101232
33. Li LH, Zhang LH, Zhang T, Qi XX, Cheng G, Xia LX. Serum Chemokine CXCL7 as a Potential Novel Biomarker for Obstructive Colorectal Cancer. Front Oncol (2021) 10:599363. doi: 10.3389/fonc.2020.599363
34. Meng ZW, Pan W, Hong HJ, Chen JZ, Chen YL. Modified Staging Classification for Intrahepatic Cholangiocarcinoma Based on the Sixth and Seventh Editions of the AJCC/UICC TNM Staging Systems. Med (Baltimore) (2017) 96(34):e7891. doi: 10.1097/MD.000000000000789
35. Abulimiti A, Zhang X, Shivappa N, Hébert JR, Fang YJ, Huang CY, et al. The Dietary Inflammatory Index Is Positively Associated With Colorectal Cancer Risk in a Chinese Case-Control Study. Nutrients (2020) 12(1):232. doi: 10.3390/nu12010232
36. Gu MJ, Huang QC, Bao CZ, Li YJ, Li XQ, Ye D, et al. Attributable Causes of Colorectal Cancer in China. BMC Cancer (2018) 18(1):38. doi: 10.1186/s12885-017-3968-z
37. Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2019 for the Treatment of Colorectal Cancer. Int J Clin Oncol (2020) 25(1):1–42. doi: 10.1007/s10147-019-01485-z
38. Lawler M, Alsina D, Adams RA, Anderson AS, Brown G, Fearnhead NS, et al. Critical Research Gaps and Recommendations to Inform Research Prioritisation for More Effective Prevention and Improved Outcomes in Colorectal Cancer. Gut (2018) 67(1):179–93. doi: 10.1136/gutjnl-2017-315333
39. Jung G, Hernández-Illán E, Moreira L, Balaguer F, Goel A. Epigenetics of Colorectal Cancer: Biomarker and Therapeutic Potential. Nat Rev Gastroenterol Hepatol (2020) 17(2):111–30. doi: 10.1038/s41575-019-0230-y
40. Sveen A, Kopetz S, Lothe RA. Biomarker-Guided Therapy for Colorectal Cancer: Strength in Complexity. Nat Rev Clin Oncol (2020) 17(1):11–32. doi: 10.1038/s41571-019-0241-1
41. Sawicki T, Ruszkowska M, Danielewicz A, Niedźwiedzka E, Arłukowicz T, Przybyłowicz KE. A Review of Colorectal Cancer in Terms of Epidemiology, Risk Factors, Development, Symptoms and Diagnosis. Cancers (2021) 13(9):2025. doi: 10.3390/cancers13092025
42. Long W, Wang M, Luo X, Huang G, Chen J. Murrangatin Suppresses Angiogenesis Induced by Tumor Cell-Derived Media and Inhibits AKT Activation in Zebrafish and Endothelial Cells. Drug Des Devel Ther (2018) 12:3107–15. doi: 10.2147/DDDT.S145956
43. Fahey E, Doyle SL. IL-1 Family Cytokine Regulation of Vascular Permeability and Angiogenesis. Front Immunol (2019) 10:1426. doi: 10.3389/fimmu.2019.01426
44. Zheng S, Han MY, Xiao ZX, Peng JP, Dong Q. Clinical Significance of Vascular Endothelial Growth Factor Expression and Neovascularization in Colorectal Carcinoma. World J Gastroenterol (2003) 9(6):1227–30. doi: 10.3748/wjg.v9.i6.1227
45. Yin C, Jiang C, Liao F, Rong Y, Cai X, Guo G, et al. Initial LDH Level can Predict the Survival Benefit From Bevacizumab in the First-Line Setting in Chinese Patients With Metastatic Colorectal Cancer. Onco Targets Ther (2014) 7:1415–22. doi: 10.2147/OTT.S64559
46. Brown AJ, Joseph PR, Sawant KV, Rajarathnam K. Chemokine CXCL7 Heterodimers: Structural Insights, CXCR2 Receptor Function, and Glycosaminoglycan Interactions. Int J Mol Sci (2017) 18(4):748. doi: 10.3390/ijms18040748
47. Brown AJ, Sepuru KM, Sawant KV, Rajarathnam K. Platelet-Derived Chemokine CXCL7 Dimer Preferentially Exists in the Glycosaminoglycan-Bound Form: Implications for Neutrophil-Platelet Crosstalk. Front Immunol (2017) 8:1248. doi: 10.3389/fimmu.2017.01248
48. Yu M, Berk R, Kosir MA. CXCL7-Mediated Stimulation of Lymphangiogenic Factors VEGF-C, VEGF-D in Human Breast Cancer Cells. J Oncol (2010) 2010:939407. doi: 10.1155/2010/939407
49. Chiang HC, Wang YS, Chou CH, Liao AT, Chu RM, Lin CS. Overexpression of Chemokine Ligand 7 Is Associated With the Progression of Canine Transmissible Venereal Tumor. BMC Vet Res (2012) 8:216. doi: 10.1186/1746-6148-8-216
50. Haunschild CE, Tewari KS. Bevacizumab Use in the Frontline, Maintenance and Recurrent Settings for Ovarian Cancer. Future Oncol (2020) 16(7):225–46. doi: 10.2217/fon-2019-0042
51. Gan QX, Wang J, Hu J, Lou GH, Xiong HJ, Peng CY, et al. Modulation of Apoptosis by Plant Polysaccharides for Exerting Anti-Cancer Effects: A Review. Front Pharmacol (2020) 11:792. doi: 10.3389/fphar.2020.00792
52. Reich N, Beyer C, Gelse K, Akhmetshina A, Dees C, Zwerina J, et al. Microparticles Stimulate Angiogenesis by Inducing ELR(+) CXC-Chemokines in Synovial Fibroblasts. J Cell Mol Med (2018) 15(4):756–62. doi: 10.1111/j.1582-4934.2010.01051.x
53. Xu Z, Zhu C, Chen C, Zong Y, Feng H, Liu D, et al. CCL19 Suppresses Angiogenesis Through Promoting miR-206 and Inhibiting Met/ERK/Elk-1/HIF-1α /VEGF-A Pathway in Colorectal Cancer. Cell Death Dis (2018) 9(10):974. doi: 10.1038/s41419-018-1010-2
54. Ghoncheh M, Pournamdar Z, Salehiniya H. Incidence and Mortality and Epidemiology of Breast Cancer in the World. Asian Pac J Cancer Prev (2016) 17(S3):43–6. doi: 10.7314/apjcp.2016.17.s3.43
55. Fülle L, Steiner N, Funke M, Gondorf F, Pfeiffer F, Siegl J, et al. RNA Aptamers Recognizing Murine CCL17 Inhibit T Cell Chemotaxis and Reduce Contact Hypersensitivity In Vivo. Mol Ther (2018) 26(1):95–104. doi: 10.1016/j.ymthe.2017.10.005
56. Groblewska M, Mroczko B. Pro- and Antiangiogenic Factors in Gliomas: Implications for Novel Therapeutic Possibilities. Int J Mol Sci (2021) 22(11):6126. doi: 10.3390/ijms22116126
57. Korbecki J, Kojder K, Barczak K, Simińska D, Gutowska I, Chlubek D, et al. Hypoxia Alters the Expression of CC Chemokines and CC Chemokine Receptors in a Tumor-A Literature Review. Int J Mol Sci (2020) 21(16):5647. doi: 10.3390/ijms21165647
Keywords: CXCL7, VEGF, angiogenesis, prognosis, colorectal cancer
Citation: Li L, Jiang K, Li D, Li D, Fan Z, Dai G, Tu S, Liu X and Wei G (2021) The Chemokine CXCL7 Is Related to Angiogenesis and Associated With Poor Prognosis in Colorectal Cancer Patients. Front. Oncol. 11:754221. doi: 10.3389/fonc.2021.754221
Received: 06 August 2021; Accepted: 13 September 2021;
Published: 08 October 2021.
Edited by:
Yuming Jiang, Stanford University, United StatesReviewed by:
Louise Catherine Connell, Cornell University, United StatesYuqian Feng, Zhejiang Chinese Medical University, China
Copyright © 2021 Li, Jiang, Li, Li, Fan, Dai, Tu, Liu and Wei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Longhai Li, cGVfbGlsb25naGFpQDEyNi5jb20=; Guangyou Wei, MTM1MTU2ODI2MjZAMTYzLmNvbQ==; Xiangyu Liu, NjMyNzgwMzI3QHFxLmNvbQ==
†These authors have contributed equally to this work
 Longhai Li
Longhai Li Kai Jiang2†
Kai Jiang2† Zitong Fan
Zitong Fan