
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol. , 22 September 2021
Sec. Gynecological Oncology
Volume 11 - 2021 | https://doi.org/10.3389/fonc.2021.724886
This article is part of the Research Topic Advances and Novel Technologies in Surgical Instruments for the Treatment of Cancer View all 19 articles
 Giacomo Corrado1*
Giacomo Corrado1* Enrico Vizza2
Enrico Vizza2 Anna Myriam Perrone3
Anna Myriam Perrone3 Liliana Mereu4
Liliana Mereu4 Vito Cela5
Vito Cela5 Francesco Legge6
Francesco Legge6 Georgios Hilaris7,8
Georgios Hilaris7,8 Tina Pasciuto9
Tina Pasciuto9 Marco D’Indinosante1
Marco D’Indinosante1 Eleonora La Fera1
Eleonora La Fera1 Camilla Certelli2
Camilla Certelli2 Valentina Bruno2
Valentina Bruno2 Stylianos Kogeorgos7
Stylianos Kogeorgos7 Francesco Fanfani9
Francesco Fanfani9 Pierandrea De Iaco3
Pierandrea De Iaco3 Giovanni Scambia1,10
Giovanni Scambia1,10 Valerio Gallotta1
Valerio Gallotta1Introduction: Elderly endometrial cancer (EEC) patients represent a challenging clinical situation because of the increasing number of clinical morbidities. In this setting of patients, minimally invasive surgery (MIS) has been shown to improve surgical and clinical outcomes. The aim of this study was to evaluate the peri-operative and oncological outcomes of EEC patients who had undergone laparoscopic (LS) or robotic surgery (RS).
Materials and Methods: This is a retrospective multi-institutional study in which endometrial cancer patients of 70 years or older who had undergone MIS for EC from April 2002 to October 2018 were considered. Owing to the non-randomized nature of the study design and the possible allocation biases arising from the retrospective comparison between LS and RS groups, we also performed a propensity score-matched analysis (PSMA).
Results: A total of 537 patients with EC were included in the study: 346 who underwent LS and 191 who underwent RS. No significant statistical differences were found between the two groups in terms of surgical and survival outcomes. 188 were analyzed after PSMA (94 patients in the LS group were matched with 94 patients in the RS group). The median estimated blood loss was higher in the LS group (p=0.001) and the median operative time was higher in the RS group (p=0.0003). No differences emerged between LS and RS in terms of disease free survival (DFS) (p=0.890) and overall survival (OS) (p=0.683).
Conclusions: Our study showed that when compared LS and RS, RS showed lower blood losses and higher operative times. However, none of the two approaches demonstrated to be superior in terms of survival outcomes. For this reason, each patient should be evaluated individually to determine the best surgical approach.
Endometrial cancer (EC) is the most common gynecological cancer in developed countries. A relevant percentage (15-25%) of women are older than 70 years at the diagnosis and the risk of EC increases according to the age (1, 2). Elderly patients present a higher rate of negative prognostic factors and the age itself represents a risk factor to consider in the choice of the adjuvant therapy (3). In fact, in this kind of patients more aggressive and advanced cancers are often diagnosed (4). The standard treatment is surgery in the majority of the cases. However, the main problem in the management of elderly patients is the comorbidities that increase the risk of surgical complications. For this reason, it is important on the one hand to obtain the best oncological outcome through radical surgery, and on the other hand, to reduce peri- and post-operative complications and to improve recovery times after surgery.
Several studies have investigated the feasibility of minimally invasive surgery (MIS) compared with laparotomic surgery and relevant advantages in terms of surgical outcomes have been demonstrated (5–10). However, studies in which different types of MIS in elderly patients are compared are missing.
In this study we evaluated the surgical and oncological outcomes of patients of 70 years or older who had undergone laparoscopic or robotic surgery for EC.
This is a retrospective multi-institutional study that involved patients from seven Institutes: Fondazione Policlinico Universitario A. Gemelli of Rome, Regina Elena National Cancer Institute of Rome, Santa Chiara Hospital of Trento, Azienda Ospedaliero-Universitaria di Bologna, University of Pisa, “Miulli hospital” of Acquaviva delle Fonti in Bari, Hygeia Hospital, Marousi, Athens Greece. Approval to conduct the study was obtained independently from an internal review board at each participating institution. Informed consent to laparoscopic or robotic surgery was obtained from all the patients in accordance with local and international legislation (Declaration of Helsinki) (11).
The data refer to a period from April 2002 to October 2018. All the EC patients of 70 years or older who had undergone MIS were considered. In the majority of the centers surgeons performed both laparoscopic and robotic surgery and the surgical approach was chosen according to clinical conditions or surgeons’ preference. The robotic platforms used were Da Vinci Si or Xi (Intuitive Surgical Sunnyvale, CA). The cut-off of 70 years was based on previous studies, in which the incidence of comorbidities relevant for surgery had been considered (5, 12). All the patients were evaluated before surgery by means of a medical history, physical examination, vaginal-pelvic examination, chest X-ray, ultrasound scans, pelvic magnetic resonance imaging (MRI) or computed tomography (CT) scans. The number of relevant comorbidities was collected for each patients. Because of the retrospective nature of the study, no comorbidity scoring systems were available. Details relative to the surgical procedure and lymph node assessment [i.e. systematic lymphadenectomy or lymph node sampling or sentinel lymph node technique (SLN)] were collected in both groups. Intra-operative and post-operative complications were defined according to Common Terminology Criteria for Adverse Events (CTCAE) version 5 (13).
Adjuvant therapy was tailored to the pathologic findings at the primary surgery after multidisciplinary tumor board (gynecologic oncology, pathology, radiation oncology, medical oncology) discussion. Treatment was based on the National Comprehensive Cancer Network (NCCN) guidelines (www.nccn.org > professionals > physician_gls) as well as ESGO, and ESTRO guidelines (14). Follow-up data were recorded through phone calls, if not available from medical records. Study data were stored using REDCap electronic data capture tools hosted at Fondazione Policlinico Universitario A. Gemellli, IRCCS (https://redcap-irccs.policlinicogemelli.it/) (15, 16).
Patient’s characteristics were described as absolute frequency and percentage for nominal variables and as median (min-max) and mean (standard deviation) for continuous variables. For the analysis, patients were divided into two groups according to the surgical procedure adopted. We distinguished women who underwent LPS (LPS group) and those who underwent RS (RS group). Moreover, in order to assess the impact of age on LPS and RS, patients were stratified according to four age classes: 70-74 years old, 75-79 years old, 80-85 years old, more than 85 years old. Comparisons between groups were made with Mann-Whitney test or Kruskal–Wallis test for continuous variables and χ2 or Fisher exact test for nominal variables, as appropriate. The normality of continuous variables was assessed with Shapiro–Francia test. In order to assess the rule of age, BMI, comorbidity, previous abdominal surgery, FIGO stage (17), histotype, grading, presence of metastasis, surgical approach (LPS vs RS), operative time (OT) and adjuvant therapy on surgical complications, univariable logistic regression analyses were run to identify possible factors significantly associated with intra-operative, early post-operative (≤30 days) and late post-operative (> 30 days) complications. The parameters were selected according to their clinical relevance and results were presented as Odds ratios (95% Confidence Intervals).
Owing to the non-randomized nature of the study design and the possible allocation biases arising from the retrospective comparison between LPS and RS groups, we also performed a propensity score-matched analysis (PSMA) (18). The PSMA was used to minimize potential selection bias and compare the treatment effects by taking into account all covariates that may influence the selection of the surgical approach (19, 20) namely laparoscopy or robotic surgery. Propensity score was developed through multivariable logistic regression model adjusting for: age, body mass index, comorbidity (present/absent), previous abdominal surgery, lymphadenectomy, histotype and FIGO stage. A 1:1 ‘‘nearest neighbor’’ match without replacement was applied (21) meaning that each patient treated by robotic surgery was matched with one patient treated by laparoscopy who had the closest estimated propensity score.
Survival analysis was performed both for the whole study and PSMA population in terms of DFS and OS. DFS was defined as the time elapsed from first diagnosis to recurrence or last follow-up while OS was defined as the time from first diagnosis to death or last follow-up. Median follow-up was calculated according to the inverted Kaplan-Meier technique (22) OS and DFS curves were estimated by Kaplan-Meier product limit method (23) and compared by log-rank test (24). For PSMA population, Cox proportional hazards models (25) were applied to evaluate the impact on DFS and OS of age, BMI, comorbidity, previous abdominal surgery, FIGO stage, histotype, grading, presence of metastasis, surgical approach (LPS vs RS) and adjuvant therapy. The parameters were selected according to their clinical relevance. All estimates were presented with two-sided 95% Confidence Intervals (CIs). All statistical calculations were performed using the STATA software version 13.0 (Stata Corp, College Station, TX). Two-sided tests were used and the significance level was set at p< 0.05. No imputation was carried out for missing data.
A total of 537 patients with EC were included in the study: 346 who underwent laparoscopic surgery (LS) and 191 who underwent robotic surgery (RS). Each center contributed with patients: Fondazione Policlinico Universitario A. Gemelli with 130 patients (54 LS and 76 RS), Regina Elena National Cancer Institute with 168 patients (143 LS and 25 RS), Santa Chiara Hospital with 75 patients (36 LS and 39 RS), Azienda Ospedaliero-Universitaria of Bologna with 83 patients (71 LS and 12 RS), University of Pisa with 18 patients (18 RS), “Miulli hospital” with 40 patients (24 LS and 16 RS), Hygeia Hospital with 23 patients (18 LS and 5 RS).
Clinical and pathological characteristics are shown in Table 1. The median age was 76 (range 70-94) and 75 (range 70-88) years, respectively, in the LS and the RS group. The distribution of patients according to age and BMI was not normally distributed and is shown, respectively, in Supplementary Figures S1 and S2. Analyses within both LS and RS groups didn’t show any significant statistical differences in terms of histology, grading, prior abdominal surgery and medical comorbidities. These results were also confirmed in a stratified analysis according to class age (Supplementary Table S1). The majority of the patients in both groups had FIGO stage I (81.5% and 82.2%, respectively, in the LS and the RS group). The 18% of the patients had a FIGO stage higher than II (Table 1).
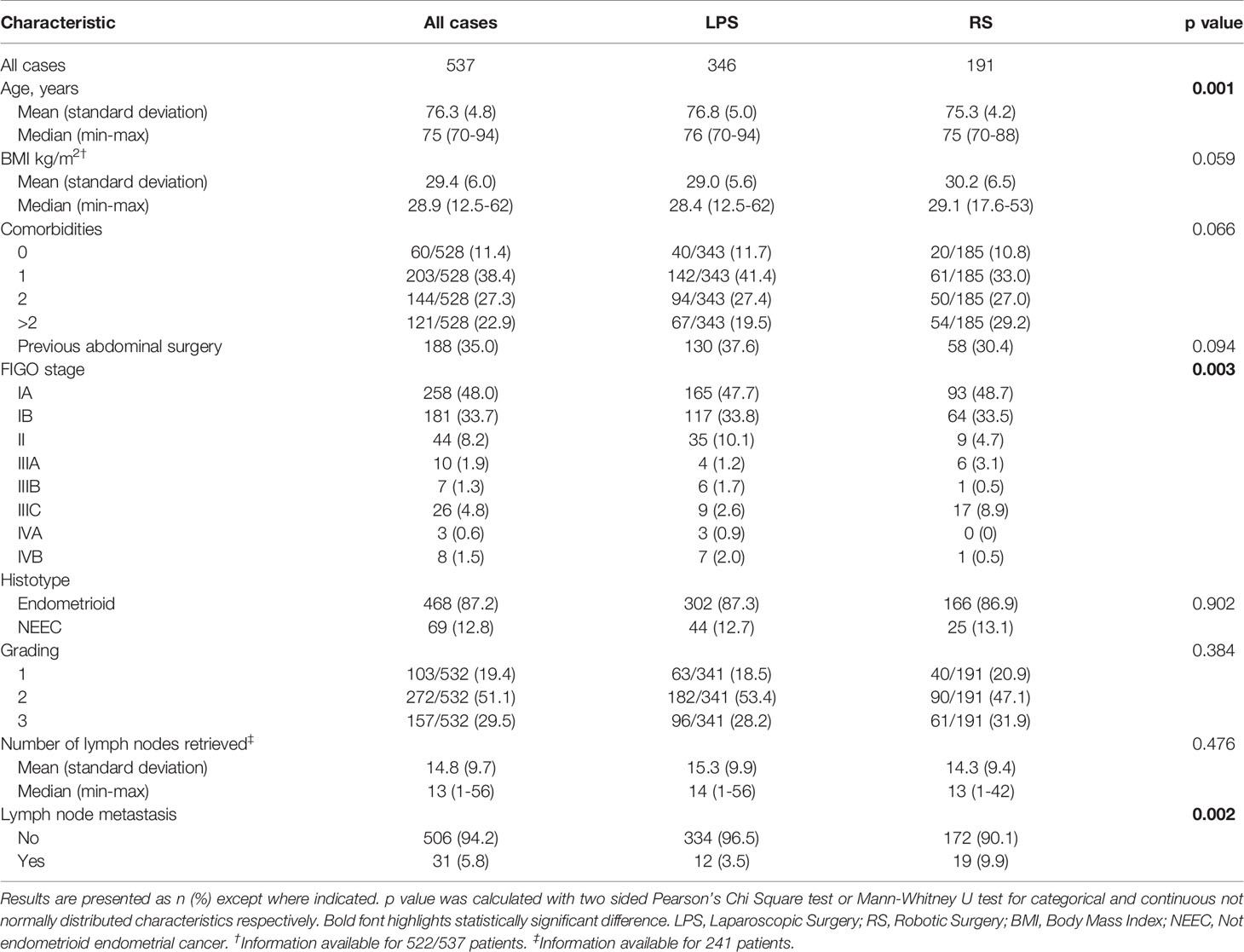
Table 1 Clinical and pathological characteristics of 537 patients with endometrial cancer according to the type of surgery.
Surgical, adjuvant and follow up characteristics are shown in Table 2. No significant statistical differences were found between the two groups in terms of type of surgery, intra-operative and post-operative complication and laparotomic conversion. In particular, the rate of intraoperative complications was 1.9%. Six intraoperative complications were documented in the LS group: 2 bowel injuries, 2 bladder injuries, 2 vaginal lacerations. Four intraoperative complications were documented in the RS group: 1 bladder injury, 1 iliac artery injury, 1 vaginal laceration, 1 bowel injury. All the intraoperative complications occurred in the two groups were classified as grade < 3 according the CTCAE. There were 4 grade 3 early postoperative complications: 1 bowel perforation in RS group and 1 bladder-vaginal fistula and 2 urinary site infections in LS group. Among late postoperative complications only 3 were classified as grade 3 according to the CTCAE: 2 laparocele or incisional hernia (1 in LS and 1 in RS group) and 1 bowel perforation in RS group. Furthermore, the total number of laparotomic conversions was 10: 5 in the LS group due to obesity reasons and an excessive visceral adipose tissue, 5 in the RS due to vessel lesion (2 cases), sigma infiltration (1case) and vessel involvement by the tumor (2 cases). One patient was converted from robotic to laparoscopic surgery to due obesity reasons. Lymphadenectomy was performed in 70.2% of RS compared to 38.9% of the LS (p<0.0001). Even if the number of the lymph nodes retrieved was the same in the two groups the rate of lymph nodes metastases was higher in the robotic group (p<0.002).
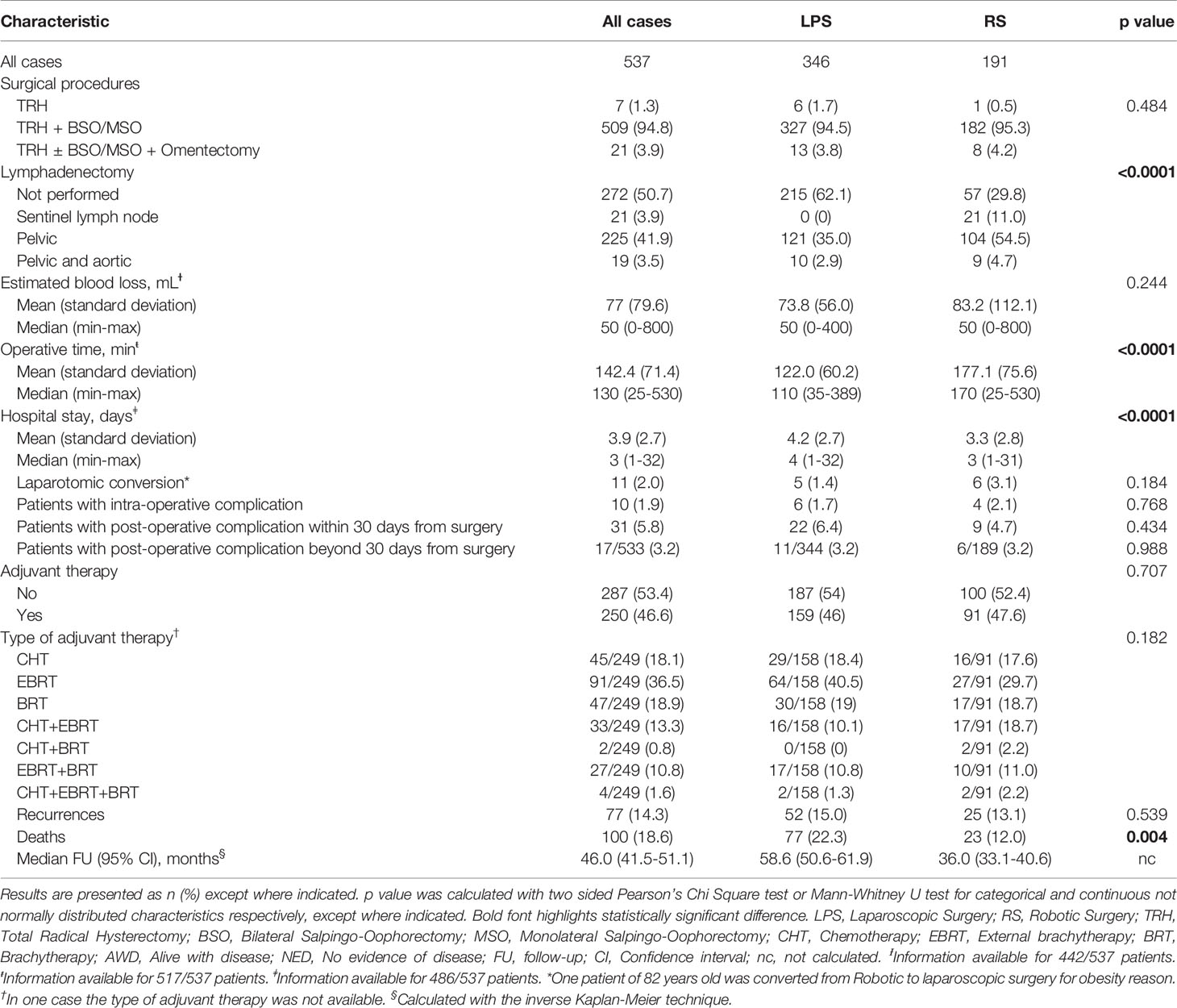
Table 2 Surgical, adjuvant and follow up characteristics of 537 patients with endometrial cancer according to the type of surgery.
The mean hospital stay was 4 days in LS group and 3 days in RS. This difference was statistically significant (p=0.0001). Days of hospitalization was statistically significant lower in robotic groups ranging from 75 to 85 years compared to laparoscopic groups (Supplementary Table S2). The absence of statistical significant differences between the two groups in terms of intra and post operative complications was also confirmed at univariable analysis (Supplementary Table S1).
Clinical and pathological characteristics according to the age class are shown in Supplementary Table S2. As regards the surgical outcomes, no differences emerged in terms of EBL, OT, laparotomic conversions and intra-operative and post-operative complications when the age increased, although the median OT was higher in the RS group of each age class (Supplementary Table S3).
One hundred eighty-eight were analyzed after PSMA (94 patients in the LS group were matched with 94 patients in the RS group). After matching, no differences emerged between the clinical and pathological characteristics of the two groups, (Table 3). Furthermore, there were no differences in terms of surgical procedures and adjuvant therapies (respectively, p=0.605 and p=0.461), as shown in Table 4. Although the median estimated blood loss (EBL) was higher in the LS group (p=0.001) and the median OT was higher in the RS group (p=0.0003), no differences were observed between the two groups in terms of intra-operative and post-operative complications rate (Table 4). Moreover, our results did not show differences in the laparotomic conversion rate (p=0.248).
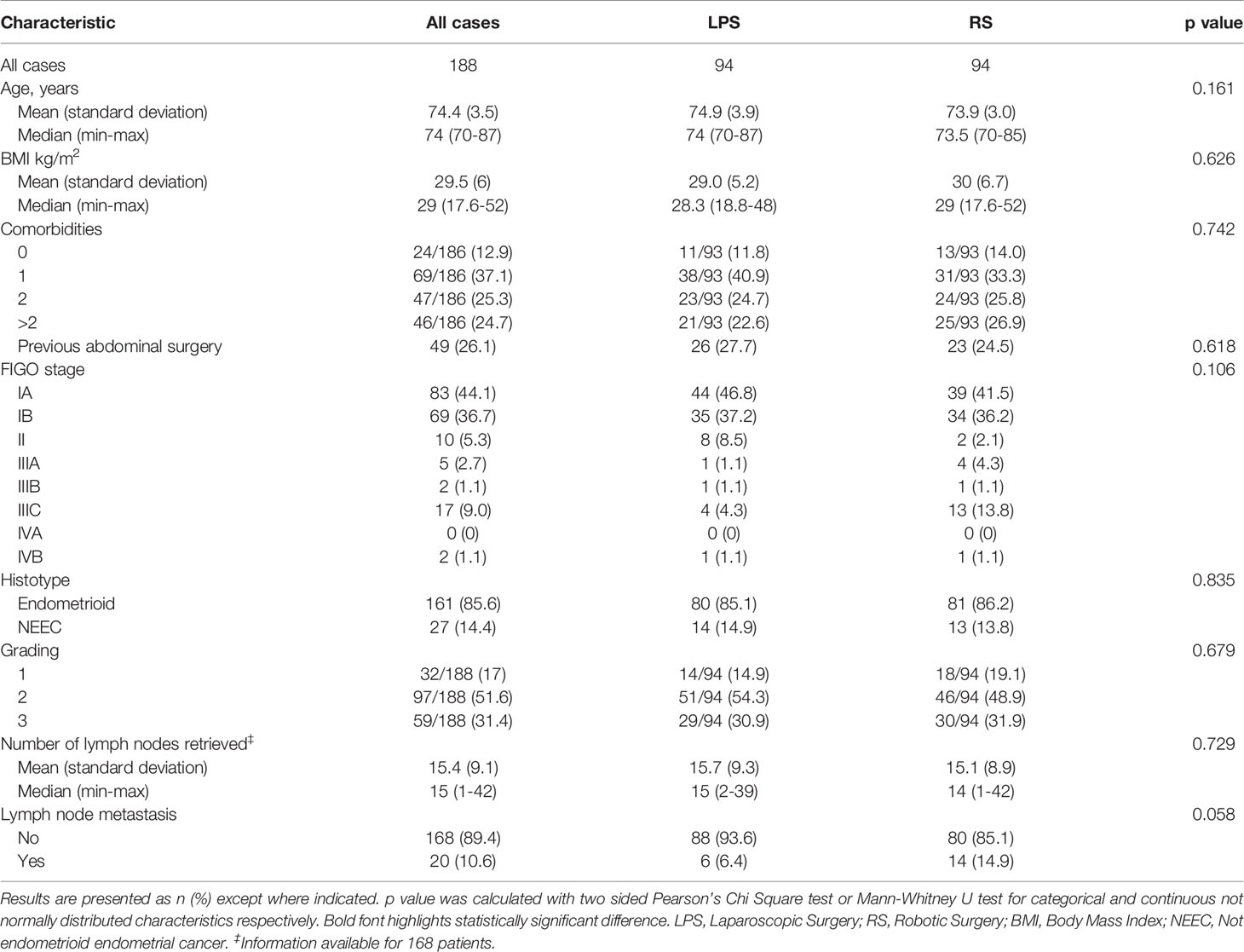
Table 3 Clinical and pathological characteristics of 188 matched patients with endometrial cancer according to the type of surgery.
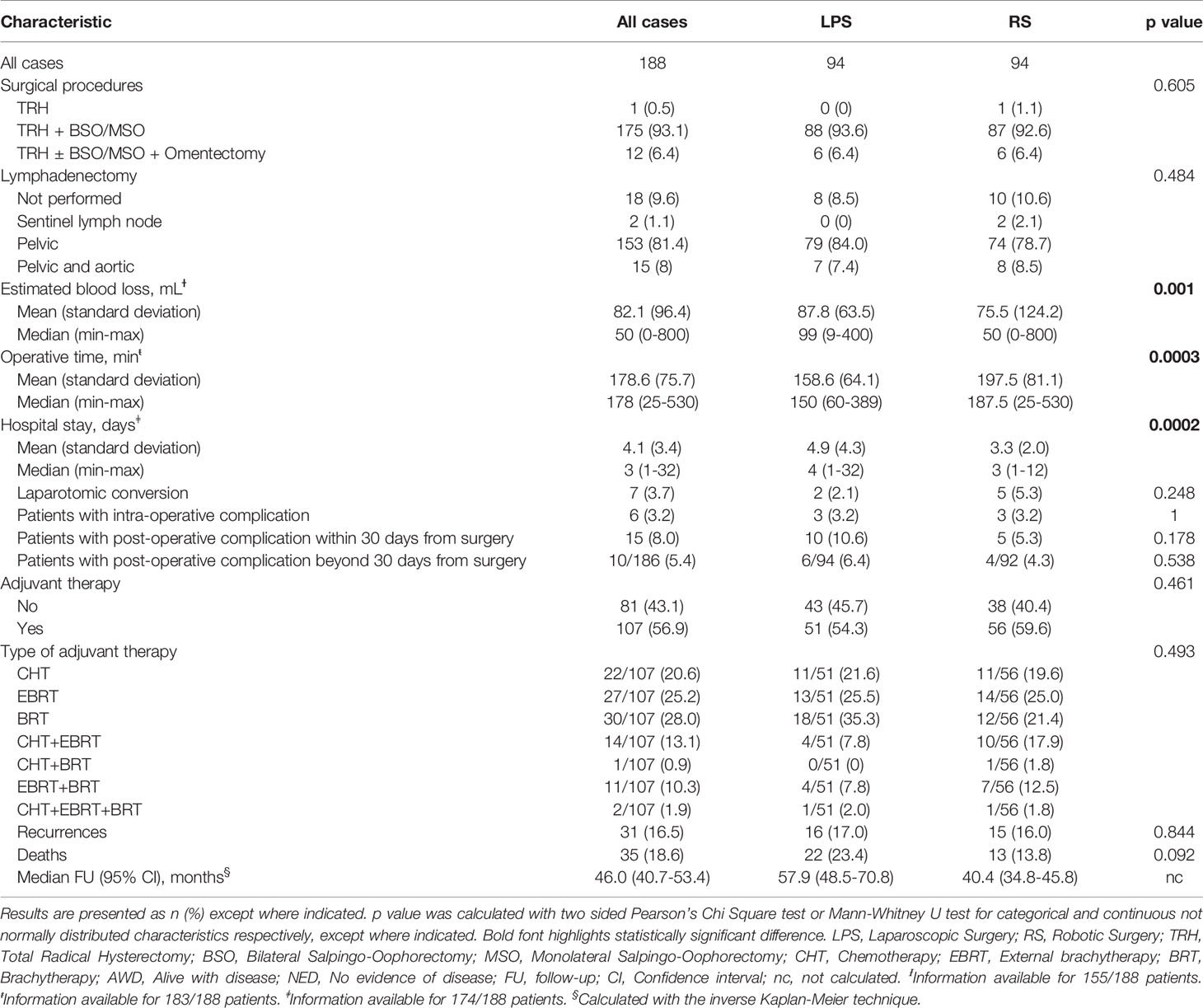
Table 4 Surgical, adjuvant and follow up characteristics of 188 matched patients with endometrial cancer according to the type of surgery.
No significant differences were found between the two groups regarding the rate of patients who underwent adjuvant therapy (p=0.707 and p=0.461 for the whole study and PSMA population respectively). Similarly, no significant differences were detected in terms of modality of adjuvant therapy (p=0.171 and p=0.493 for the whole study and PSMA population respectively). Median follow up was 46.0 months (95% CI: 41.5-51.1) and 46.0 months (95% CI: 40.7-53.4) for the whole study and PSMA population respectively. In this period, in the whole study population, we observed 77 recurrences: 15.0% and 13.1% had recurrence in LS and RS groups respectively (p=0.539); while in the PSMA population, we observed 31 recurrences: 17.0% and 16.6% had recurrence in LH and RH groups respectively (p=0.844) (Tables 2 and 4).
No differences emerged between LS and RS in terms of disease free survival (DFS) (p=0.614 and p=0.890 for the whole study and PSMA population respectively) and overall survival (OS) (p=0.171 and p=0.683 for the whole study and PSMA population respectively), as shown in Figure 1. At the univariable analysis, there were no differences in the DFS and the OS according to the age of the PSMA patients (Table 5). The only variables that affected survival were, respectively, the FIGO stage for DFS and the histotype for OS.
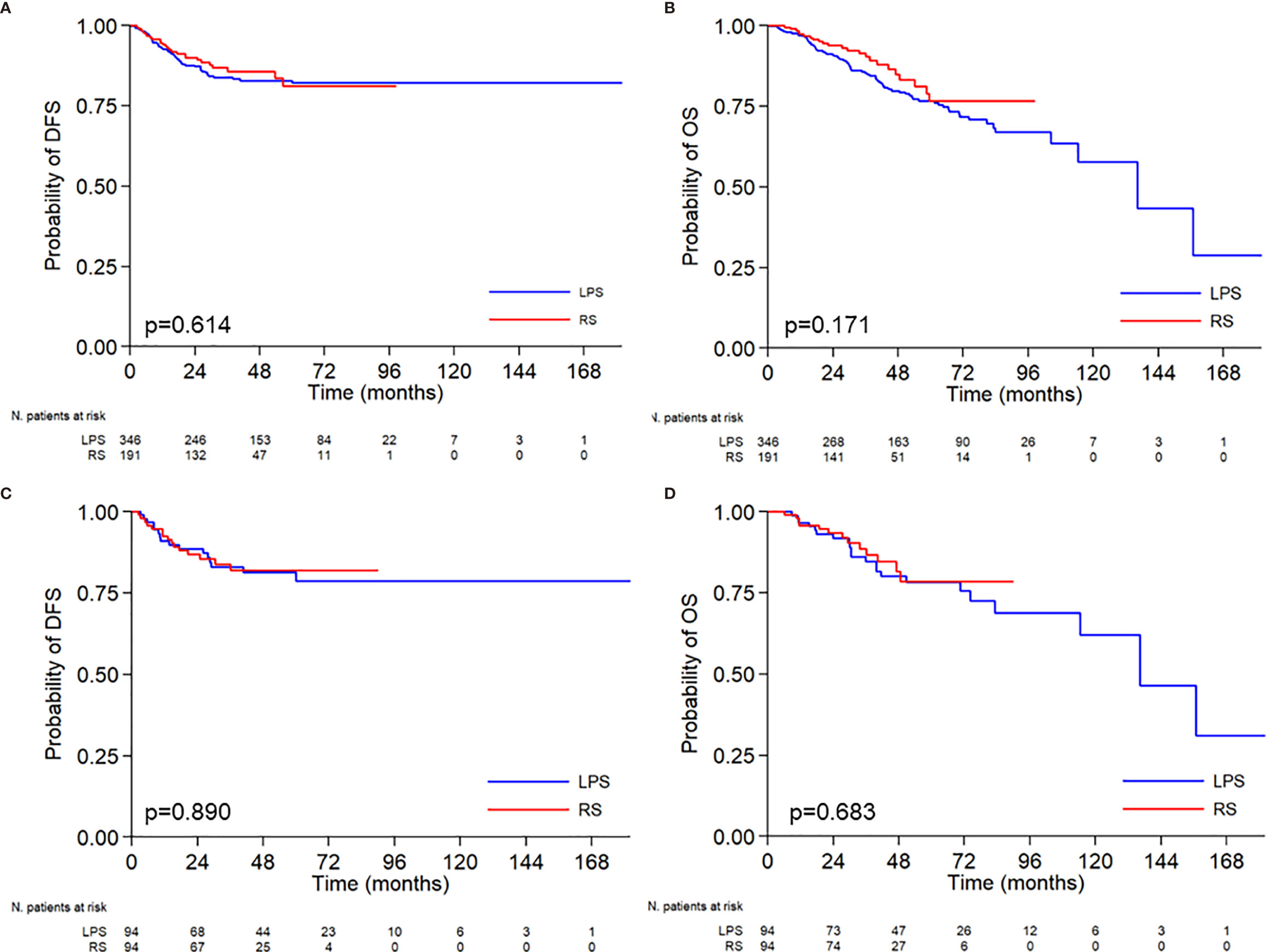
Figure 1 Kaplan-Meier curves relative to disease free survival-DFS (A–C), and overall survival-OS (B–D) according to the surgical approach. Median DFS: not reached vs not reached. Probability of DFS at 5 years 78.8% vs 81.9%. Median OS: 136.2 months vs not reached. Probability of OS at 5 years 78.2% vs 78.6%.
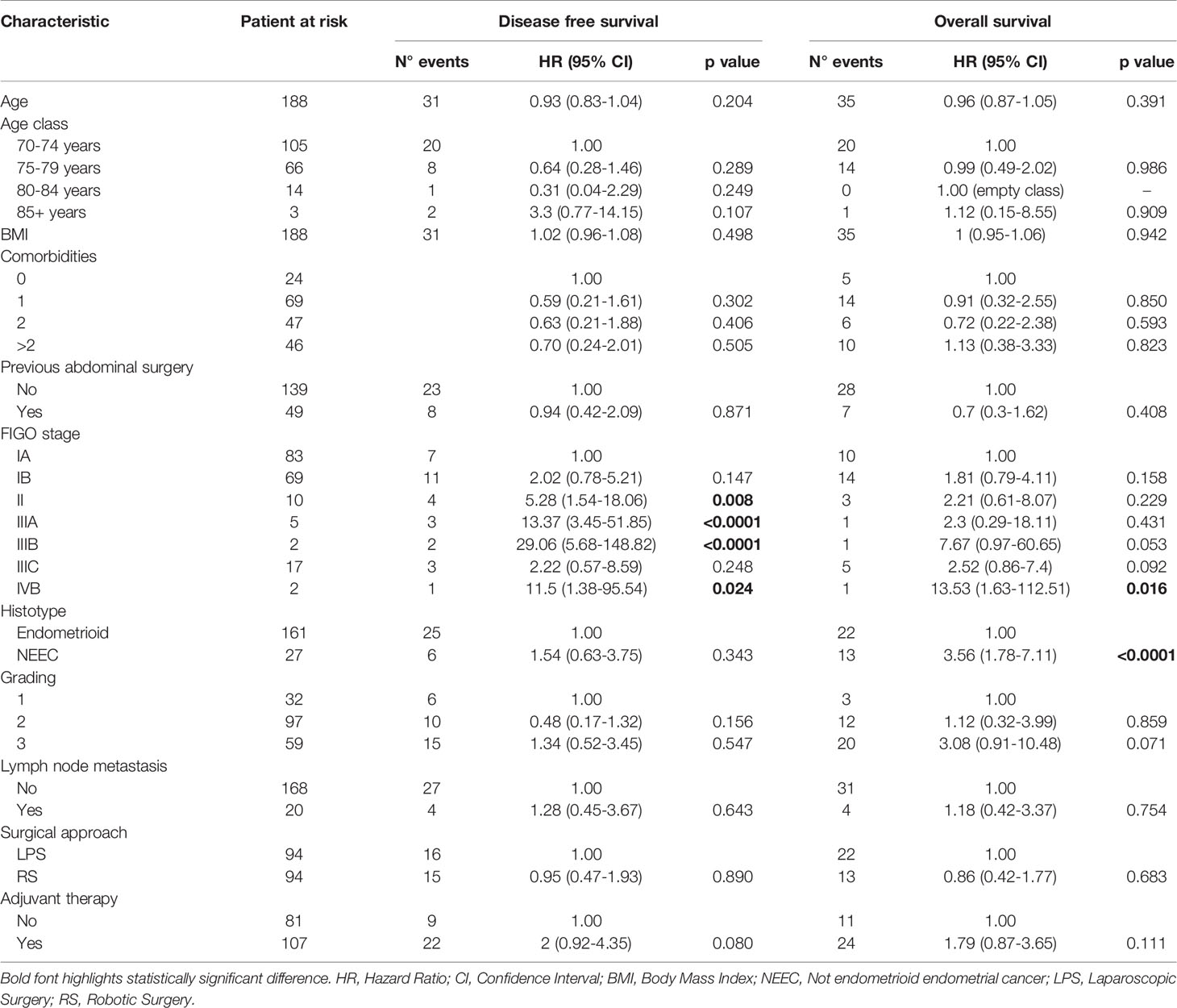
Table 5 Univariable analysis of clinical, pathological and treatment characteristics of 188 matched patients with endometrial cancer according to DFS and OS.
This study confirms the benefit of the MIS approach in elderly endometrial cancer patients (4–10). After 4 years of follow-up, the present data suggest that MIS in EEC patients is safe from an oncological standpoint in terms of comparable DFS and OS rates.
Based on our multicentric experience, we can assert that robotic and laparoscopic approach for elderly endometrial cancer patients can be well tolerated with no increase in complications. Although, the RS required longer operative time, on the other hand it showed advantages in terms of reduced blood loss and hospital stay compared to LS.
Overall, our data confirm the available lines of evidence supporting the safety of MIS. The incidence of overall post-operative complications in our cohort was 5.8%, a frequency in agreement with some previous results (4–10), without significant difference between the two groups, despite about 40% of obese patients in each group.
Since elderly patients usually present a higher comorbidity rate and a higher surgical risk, in recent years the efforts have focused on the choice of the best surgical approach for this kind of patients. The main issues related to MIS were anesthesiological: the maintenance of Trendelemburg position and the pneumoperitoneum increase abdominal pressure reducing cardiac output and respiratory movements (5, 6, 26). For this reason, the management of these patients require a close collaboration within a multidisciplinary team consisting of anesthesia, geriatric and gynecologic specialists in order to obtain a greater synergy for determining surgical indications and tailored approaches in these fragile patients (27, 28). However, the increasing expertise of the surgeons with lower operative times may reduce the relevance of these issues. Furthermore, MIS has shown good results in terms of lower complication rates and faster recovery times. Our series confirmed that MIS is associated with good post-operative results, with clinical benefits in terms of post-operative complications (29). When compared with laparotomic surgery in EC patients aged 70 years or older, RS showed a reduction of EBL, OT, complications and days of hospitalization (5, 9). Even when elderly and not elderly patients were compared, RS maintained its advantages (7) with no differences between robotic and laparotomic approaches in terms of survival (5). In the same way, LS showed better surgical outcomes when compared with a laparotomic approach. Laparotomy, in fact, was associated with a higher risk of thromboembolism, due to a longer recovery time, and higher surgical site infections rate (6). Furthermore, prolonged hospitalization times may delay the start of adjuvant therapies, compromising their efficacy. Although some recent studies compared the three different approaches (LS, RS and laparotomic surgery) according to the age of the patients, confirming an advantage of minimally invasive surgery (30, 31), studies in which the best minimally invasive approach was evaluated are missing. In our study we compared LS and RS in elderly patients (70 years and older) with EC and no differences emerged between the two surgical approaches in terms of complication rates, both intra-operative and post-operative. The LS group showed a higher median EBL, probably because of a better surgical field control with robotic arms, whereas the OT were longer in the RS group, due to docking times. In a recent study, de’ Angelis et al, who evaluated the LS and the RS in elderly patients with colorectal cancer, showed similar results with no differences in terms of surgical outcomes between the two approaches, except for a longer OT in the RS group (32). On the one hand, the increased OT in RS may be a disadvantage for elderly patients, since it may be related to a prolonged Trendelemburg position which is not reversible without the un-docking of the robot (5). On the other hand, in RS the insufflation system is different and the pressure of the pneumoperitoneum may be reduced, taking advantage from the lifting of the trocars and the abdomen during docking time.
Our results did not show a worsening of the surgical outcomes when the age increased, in agreement with Uccella et al. who demonstrated the maintenance of an advantage of LS compared with laparotomy even in patients aged 80 years or older (6) and Lowe et al. who showed a 96% successful robotic procedures in octogenarians and nonagenarians (33). Furthermore, although Walker et al. showed an increased conversion rate (from LS to Laparotomy) for each decade of age (34), our analysis did not reveal any differences in the conversion rate according to the age class. Another important aspect of surgery in elderly patients that emerged in some studies is the reduction of the lymphadenectomy rate (31), probably in order to reduce the invasiveness of the surgical procedure in this kind of patients. In our study, although the number of patients who underwent lymphadenectomy was lower when the age increased, the difference did not reach a statistical relevance. As regards survival outcomes, none of the two approaches demonstrated to be superior.
The major strengths of this study are represented by the number of patients included in the study, the PSMA and its specific focus on the role of MIS in EEC patients. Limitations include the retrospective nature of the study, which can result in underreporting adequate pre-operative frailty evaluation (28, 35) of the patients.
In conclusion, thanks to the successful cooperative efforts of multiple referral Gynecologic Oncology Units, we confirmed in a large series that MIS for EEC is feasible and safe, and provides survival outcomes comparable to those obtained with open surgical approach. In particular, when compared LS and RS, RS showed lower blood losses and higher operative times. However, none of the two approaches demonstrated to be superior in terms of survival outcomes.
Several efforts should be made and prospective collaborative study are needed to provide adequate preoperative work up and availability of a dedicated multidisciplinary approach, which plays a major role in the selection of patients for the optimal management strategy in elderly endometrial cancer patients.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Conceived and designed the study: GC and VG. Collected the data: AP, LM, VC, FL, GH, MD’I, EF, CC, and VB. Data analysis: TP. Manuscript writing: CC and GC. Manuscript revision: VG. Supervision and validation: PI, EV, FF, SK, and GS. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2021.724886/full#supplementary-material
Supplementary Figure 1 | Histograms of the distribution of the patients according to the age.
Supplementary Figure 2 | Histograms of the distribution of the patients according to body mass index (BMI).
1. Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2019. CA Cancer J Clin (2019) 69(1):7–34. doi: 10.3322/caac.21551
2. Bishop EA, Java JJ, Moore KN, Walker JL. Pathologic and Treatment Outcomes Among a Geriatric Population of Endometrial Cancer Patients: An NRG Oncology/ Gynecologic Oncology Group Ancillary Data Analysis of LAP2. Int J Gynecol Cancer (2017) 27(4):730–7. doi: 10.1097/IGC.0000000000000947
3. National Comprehensive Cancer Network guidelines. Available at: https://www.nccn.org/store/login/login.aspx?ReturnURL=https://www.nccn.org/professionals/physician_gls/pdf/uterine.pdf.
4. Koual M, Ngo C, Girault A, Lécuru F, Bats AS. Endometrial Cancer in the Elderly: Does Age Influence Surgical Treatments, Outcomes, and Prognosis? Menopause (2018) 25(9):968–76. doi: 10.1097/GME.0000000000001119
5. Lavoue V, Zeng X, Lau S, Press JZ, Abitbol J, Gotlieb R, et al. Impact of Robotics on the Outcome of Elderly Patients With Endometrial Cancer. Gynecol Oncol (2014) 133(3):556–62. doi: 10.1016/j.ygyno.2014.03.572
6. Uccella S, Bonzini M, Palomba S, Fanfani F, Malzoni M, Ceccaroni M, et al. Laparoscopic vs. Open Treatment of Endometrial Cancer in the Elderly and Very Elderly: An Age-Stratified Multicenter Study on 1606 Women. Gynecol Oncol (2016) 141(2):211–7. doi: 10.1016/j.ygyno.2016.02.029
7. Guy MS, Sheeder J, Behbakht K, Wright JD, Guntupalli SR. Comparative Outcomes in Older and Younger Women Undergoing Laparotomy or Robotic Surgical Staging for Endometrial Cancer. Am J Obstet Gynecol (2016) 214(3):350.e1–e10. doi: 10.1016/j.ajog.2015.09.085
8. Gallotta V, Conte C, D'Indinosante M, Federico A, Biscione A, Vizzielli G, et al. Robotic Surgery in Elderly and Very Elderly Gynecologic Cancer Patients. J Minim Invasive Gynecol (2018) 25(5):872–7. doi: 10.1016/j.jmig.2018.01.007
9. Lindfors A, Åkesson Å, Staf C, Sjöli P, Sundfeldt K, Dahm-Kähler P. Robotic vs Open Surgery for Endometrial Cancer in Elderly Patients: Surgical Outcome, Survival, and Cost Analysis. Int J Gynecol Cancer (2018) 28(4):692–6994. doi: 10.1097/IGC.0000000000001240
10. Perrone AM, Di Marcoberardino B, Rossi M, Pozzati F, Pellegrini A, Procaccini M, et al. Laparoscopic Versus Laparotomic Approach to Endometrial Cancer. Eur J Gynaecol Oncol (2012) 33(4):376–81.
11. World Medical Association Inc. Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects. J Indian Med Assoc (2009) 107:403–5.
12. Vaknin Z, Perri T, Lau S, Deland C, Drummond N, Rosberger Z, et al. Outcome and Quality of Life in a Prospective Cohort of the First 100 Robotic Surgeries for Endometrial Cancer, With Focus on Elderly Patients. Int J Gynecol Cancer (2010) 20(8):1367–73.
13. National Cancer Institute, National Institutes of Health, US Department of Health and Human Services. Common Terminology Criteria for Adverse Events (CTCAE). Version 5.0. Published November 27, 2017. Available at: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_8.5x11.pdf.
14. European Society of Gynaecological Oncology Guidelines. Available at: https://guidelines.esgo.org/uterine-cancer/guidelines/early-stage-algorithms/.
15. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap) – A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J BioMed Inform (2009) 42(2):377–81. doi: 10.1016/j.jbi.2008.08.010
16. Harris PA, Taylor R, Minor BL, Elliot V, Fernandez M, O'Neal L, et al. REDCap Consortium, The REDCap Consortium: Building an International Community of Software Partners. J BioMed Inform (2019). doi: 10.1016/j.jbi.2019.103208
17. Pecorelli S. Revised FIGO Staging for Carcinoma of the Vulva, Cervix, and Endometrium. Int J Gynaecol Obstet (2009) 105(2):103–4. doi: 10.1016/j.ijgo.2009.02.012
18. Stuart EA. Matching Methods for Causal Inference: A Review and a Look Forward. Stat Sci (2010) 25:1–21. doi: 10.1214/09-STS313
19. Heinze G, Juni P. An Overview of the Objectives of and the Approaches to Propensity Score Analyses. Eur Heart J (2011) 32:1704–8. doi: 10.1093/eurheartj/ehr031
20. Austin PC. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behav Res (2011) 46:399–424. doi: 10.1080/00273171.2011.568786
21. Austin PC. Balance Diagnostics for Comparing the Distribution of Baseline Covariates Between Treatment Groups in Propensity-Score Matched Samples. Stat Med (2009) 28:3083–107. doi: 10.1002/sim.3697
22. Schemper M, Smith TL. A Note on Quantifying Follow-Up in Studies of Failure Time. Control Clin Trials (1996) 17:343–6. doi: 10.1016/0197-2456(96)00075-X
23. Kaplan EL, Meier P. Nonparametric Estimation From Incomplete Observation. J Am Stat Assoc (1958) 53:457–81. doi: 10.1080/01621459.1958.10501452
24. Mantel N. Evaluation of Survival Data and Two New Rank Order Statistics Arising in its Consideration. Cancer Chem Rep (1966) 50:163–70.
25. Cox DR. Regression Models and Life Tables. J R Stat Soc B (1972) 34:187–220. doi: 10.1111/j.2517-6161.1972.tb00899.x
26. Grieco DL, Anzellotti GM, Russo A, Bongiovanni F, Costantini B, D'Indinosante M, et al. Airway Closure During Surgical Pneumoperitoneum in Obese Patients. Anesthesiology (2019) 131(1):58–73. doi: 10.1097/ALN.0000000000002662
27. Colloca G, Corsonello A, Marzetti E, Balducci L, Landi F, Extermann M, et al. Treating Cancer in Older and Oldest Old Patients. Curr Pharm Des (2015) 21(13):1699–705. doi: 10.2174/1381612821666150130122536
28. Aloisi A, Tseng J, Kuhn T, Feinberg J, Chi DS, Brown CL, Mueller JJ, et al. Robotic Surgery in the Frail Elderly: Analysis of Perioperative Outcomes. Ann Surg Oncol (2020) 27(10):3772–80. doi: 10.1245/s10434-020-08475-w
29. Madden N, Frey MK, Joo L, Lee J, Musselman K, CHern JY, et al. Safety of Robotic-Assisted Gynecologic Surgery and Early Hospital Discharge in Elderly Patients. Am J Obstet Gynecol (2019) 220(3):253.e1–7. doi: 10.1016/j.ajog.2018.12.014
30. Bishop EA, Java JJ, Moore KN, Spirtos NM, Pearl ML, Zivanovic O, et al. Surgical Outcomes Among Elderly Women With Endometrial Cancer Treated by Laparoscopic Hysterectomy: A NRG/Gynecologic Oncology Group Study. Am J Obstet Gynecol (2018) 218(1):109.e1–e11. doi: 10.1016/j.ajog.2017.09.026
31. Bourgin C, Lambaudie E, Houvenaeghel G, Foucher F, Leveque J, Lavoue V. Impact of Age on Surgical Staging and Approaches (Laparotomy, Laparoscopy and Robotic Surgery) in Endometrial Cancer Management. Eur J Surg Oncol (2017) 43:703e709. doi: 10.1016/j.ejso.2016.10.022
32. de'Angelis N, Abdalla S, Bianchi G, Memeo R, Charpy C, Petrucciani N, et al. Robotic Versus Laparoscopic Colorectal Cancer Surgery in Elderly Patients: A Propensity Score Match Analysis. J Laparoendosc Adv Surg Tech A (2018) 28(11):1334–45. doi: 10.1089/lap.2018.0115
33. Lowe MP, Kumar S, Johnson PR, Kamelle SA, Chamberlain DH, Tillmanns TD. Robotic Surgical Management of Endometrial Cancer in Octogenarians and Nonagenarians: Analysis of Perioperative Outcomes and Review of the Literature. J Robotic Surg (2010) 4:109–15. doi: 10.1007/s11701-010-0195-x
34. Walker JL, Piedmonte MR, Spirtos NM, Eisenkop SM, Schlaerth JB, Mannel RS, et al. Laparoscopy Compared With Laparotomy for Comprehensive Surgical Staging of Uterine Cancer: Gynecologic Oncology Group Study Lap2. J Clin Oncol (2009) 27:5331–6. doi: 10.1200/JCO.2009.22.3248
Keywords: endometrial cancer, elderly patients, laparoscopic surgery (LS), robotic surgery, minimally invasive surgery (MIS)
Citation: Corrado G, Vizza E, Perrone AM, Mereu L, Cela V, Legge F, Hilaris G, Pasciuto T, D’Indinosante M, La Fera E, Certelli C, Bruno V, Kogeorgos S, Fanfani F, De Iaco P, Scambia G and Gallotta V (2021) Comparison Between Laparoscopic and Robotic Surgery in Elderly Patients With Endometrial Cancer: A Retrospective Multicentric Study. Front. Oncol. 11:724886. doi: 10.3389/fonc.2021.724886
Received: 14 June 2021; Accepted: 06 September 2021;
Published: 22 September 2021.
Edited by:
Stefano Restaino, Ospedale Santa Maria della Misericordia di Udine, ItalyReviewed by:
Giuseppe Vizzielli, Azienda Sanitaria Universitaria Integrata di Udine, ItalyCopyright © 2021 Corrado, Vizza, Perrone, Mereu, Cela, Legge, Hilaris, Pasciuto, D’Indinosante, La Fera, Certelli, Bruno, Kogeorgos, Fanfani, De Iaco, Scambia and Gallotta. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Giacomo Corrado, Z2lhYy5jb3I3M0BnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.