
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Oncol., 12 July 2021
Sec. Cancer Immunity and Immunotherapy
Volume 11 - 2021 | https://doi.org/10.3389/fonc.2021.667650
 Yuan Tian1,2†
Yuan Tian1,2† Ran Li3†
Ran Li3† Yan Liu4†
Yan Liu4† Meng Li5
Meng Li5 Yuxiao Song6
Yuxiao Song6 Yan Zheng7,8
Yan Zheng7,8 Aiqin Gao1
Aiqin Gao1 Qing Wen9
Qing Wen9 Guohai Su10*
Guohai Su10* Yuping Sun1,11*
Yuping Sun1,11*Background: Thyroid dysfunction is common for cancer patients receiving PD-1/PD-L1 inhibitor therapies. To clarify the incidence risk of thyroid dysfunction would be important for guiding anti-PD-1 and anti-PD-L1 immunotherapy. Therefore, the updated meta-analysis was conducted to evaluate the incidence risk of thyroid dysfunction caused by PD-1/PD-L1 inhibitors.
Methods: PD-1/PD-L1 inhibitor related clinical trials were collected by a systematic search of the PubMed. Some relevant studies were identified by a manual search. The incidence risk of all grades and grades 3-5 was analyzed and evaluated by random effect model. The Newcastle Ottawa Scale was used for the quality assessment of all clinical trials.
Results: Forty-three clinical trials were collected. Compared with chemotherapy, the risk of hypothyroidism of all grades was significantly higher (OR=7.15, 95%CI:[4.85, 10.55], I2 = 40%, Z=9.91(P <0.00001)) in PD-1/PD-L1 group. Similar results could also be noted, when the control group was placebo or CTLA-4. When PD-1/PD-L1 was combined with other treatments for cancer patients, the risk of hypothyroidism of all grades was also significantly increased. Similar to the analysis results of hypothyroidism, PD-1/PD-L1 inhibitors played the same role in increasing the risk of hyperthyroidism and thyroiditis. Few significant analysis results was noted, when the risk of thyroid dysfunction of grades 3-5 was assessed.
Conclusion: Whether used alone or in combination with other anti-tumor drugs, PD-1/PD-L1 inhibitors increased the risk of thyroid dysfunction, especially for hypothyroidism. Furthermore, PD-1/PD-L1 was better than chemotherapy and CTLA-4 in increasing the risk of thyroid dysfunction.
Programmed cell death protein 1 (PD-1) and its ligand (PD-L1) inhibitors, developed to overcome the immune escape mechanisms of cancer progression and manipulate the immune system to recognize and attack cancer cells, have been widely used for cancers (1). While achieving satisfactory clinical anti-tumor treatment effects, more and more drug-induced toxic and side effects have also been reported, and more and more attention has been drawn from clinicians (1–3). Treatment guidelines for PD-1/PD-L1 related side effects have been made and used to guide clinical works (2).
Thyroid dysfunction was one of the common toxic side effects of PD-1/PD-L1 inhibitors and had been reported in plenty of clinical trials (4–50). Moreover, It was reported that the incidence of PD-1/PD-L1 induced thyroid dysfunction was related to the clinical response and the prognosis of patients (51, 52). Therefore, clarifying the incidence risk of PD-1/PD-L1 related thyroid dysfunction would be of great significance for guiding clinical immunotherapy and judging the prognosis (51, 52). Although thyroid dysfunction might appear in different forms (53), hyperthyroidism, hypothyroidism, and thyroiditis were still the most common manifestations (1), which were also reported most frequently in clinical trials (4–50). Due to more and more clinical trials investigating the clinical efficacy and safety of PD-1/PD-L1 in cancer patients have been finished in recent two years (4–23), we conducted this updated meta-analysis to reassess the incidence risk of PD-1/PD-L1 induced hyperthyroidism, hypothyroidism, and thyroiditis.
The process of the meta-analysis was put into practice followed the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) (54).
Clinical trials, involving PD-1 or PD-L1 inhibitors, were identified by the PubMed search. Hematological malignancies were excluded first. Phase III clinical trials for all kinds of cancer patients would be taken as the priority. Clinical trials, reported with partial results or belonging to other phases, would be arranged in an alternative location. For all clinical trials included in the study, the control group was necessary, but there was no specific requirement for the treatment regimen of them. The results of the enrolled clinical trial must be reported in English.
Just as proposed by the PRISMA, keywords (neoplasm, cancer, precancer, malignant, premalignant, tumor, PD-1, PD-L1, and clinical trial) for search were set according to the PICOS (participants, interventions, comparisons, outcomes, and study design) guidelines (54). The range of published time was set between Nov 23, 2010 and Nov 23, 2020. Four members of us were appointed for eligibility assessment and data extraction. In the case of duplicated reports of the same clinical trial, only one of them was used for the final analysis, and others would be included in the systematic review. The corresponding authors (Yuping Sun and Guohai Su) had the right to deal with all results and disagreements.
Assessment for publication bias and risk of bias of individual trials were finished by Funnel plots, Egger’s test, Harbord’s test, and the Newcastle-Ottawa scale (NOS) (54–59). Risk of bias summary, including selection bias, performance bias, detection bias, attrition bias, reporting bias and other bias, would be checked and shown in a single figure. A P-value of <0.05 was used as the cut-off value for statistical significance.
Baseline characteristics of all enrolled clinical trials, including duplicating reported ones, would be collected and summarized in a table. Grading of thyroid dysfunction, including hyperthyroidism, hypothyroidism, and thyroiditis, ranging from 1 (mild symptoms that do not interfere with activities of daily living) to 5 (fatal thyroid toxicities), was collected and gathered in excel tables. Dichotomous data would be given a priority, and other types of data would be collected first and then converted into dichotomous data.
Heterogeneity of all the data, identified by Cochrane’s Q statistic test, was assessed by the DerSimonian-Laird method and quantified by I2 values (54, 59). Three different grades, including low, moderate, and high, were divided according to I2 values ( < 25%, 25-50%, and > 50%). All the process of analyses was finished by the software Review Manager 5.3. The random effect model (RE) was used to deal with all the data to calculate odds ratio (OR) and their corresponding 95% confidence interval (CI) (60). The fixed effects (FE) model was only used for calculation of the funnel plots. All reported P values are 2-sided, and P<0.05 was taken to indicate statistically significance. Subgroup and stratification analyses would be performed according to tumor types, treatment regimens, and PD-1/PD-L1 inhibitors.
The PRISMA flow diagram was shown in (Figure 1), while the bias assessment summary of all enrolled clinical trials were provided in (Supplementary Figure 1). A total of 589 published studies was found by PubMed search, while 37 studies were gotten from the former published meta-analysis (61–63). After eligibility assessment, 5 articles were only used for the systematic review (13, 20–23), while 42 articles were used for the final comprehensive analysis (4–12, 14–19, 24–50). The clinical trial ‘CheckMate 067’ (NCT01844505) was reported 4 times (47–50), while the clinical trial ‘PACIFIC’ (NCT02125461) was reported 2 times (45, 46).
Forty-three clinical trials, including 1 phase I (20), 1 phase I/II (40), 3 phase II (6, 9, 41), 1 phase II/III (39), and 37 phase III (4, 5, 7, 8, 10–12, 14–19, 21–38, 42–50), were collected and listed in (Table 1). Among all of them, 25 clinical trials (involving 28 articles) was found to be PD-1 related (4, 6, 7, 11, 12, 15, 16, 23, 25, 27–29, 32, 34–44, 47–50), while 18 clinical trials (involving 19 articles) was reported to be PD-L1 related (5, 8–13, 16, 17, 20–22, 24, 26, 30, 31, 33, 45, 46). PD-1 or PD-L1 inhibitors were prescribed as the first line treatment regimen in 22 clinical trials (7, 8, 10–12, 14, 16, 18, 20–23, 27, 29, 33, 36, 37, 41, 47–50), and previous therapy was found in the other 21 clinical trials (4–6, 9, 13, 15, 17, 19, 24–26, 28, 34, 35, 38–40, 42–46). In all the clinical trials included in the study, 8 tumor types are mainly involved, of which lung cancer accounts for the largest proportion (Table 1) (12–14, 16, 17, 24, 26, 27, 29, 30, 32, 33, 37, 39, 40, 42, 44–46).
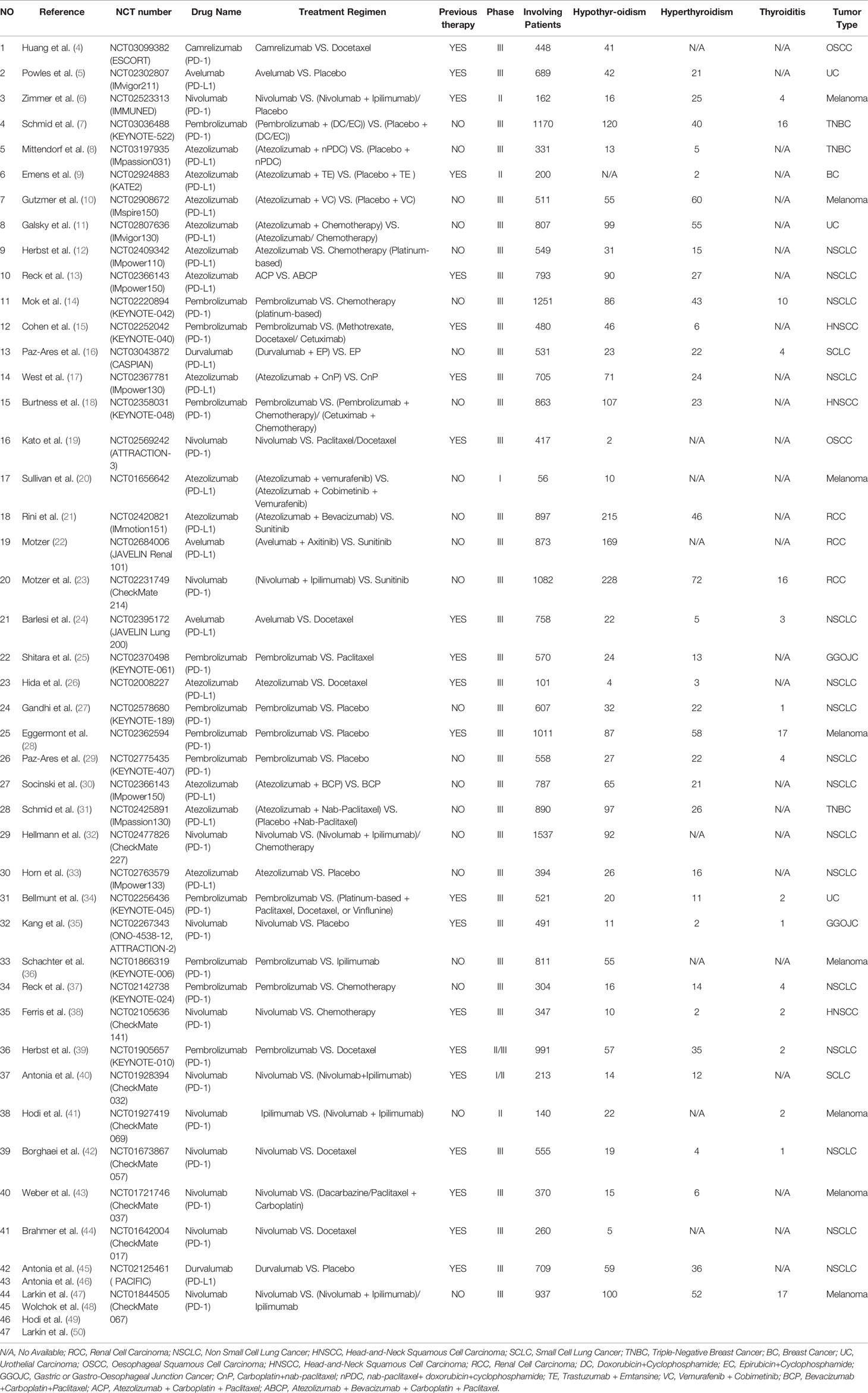
Table 1 Baseline characteristics of all enrolled clinical trials (N = 47 articles of 43 clinical trials).
Bias assessment summary was provided in (Supplementary Figure 1). High attrition bias was only found in 1 articles (Supplementary Figure 1) (47), while unclear risk was identified in 21 articles (4, 8, 9, 13, 18–22, 25, 26, 30, 32, 36, 40, 41, 43–47). Publication bias assessment was displayed in the form of funnel plots, which were provided in the supplement (Supplementary Figures 2–6).
Hypothyroidism was identified in 42 clinical trials (4–8, 10–50), 36 of which were used for the final meta-analysis (4–8, 10–12, 14–19, 24–50). For high attrition bias, one reported results of CheckMate 067 was excluded (Table 1) (47).
Compared with chemotherapy (PD-1/PD-L1 VS. Chemotherapy), the risk of hypothyroidism of all grades was significantly higher (OR=7.15, 95%CI:[4.85, 10.55], I2 = 40%, Z=9.91(P <0.00001); Figure 2A) (4, 11, 12, 14, 15, 18, 19, 24–26, 32, 34, 37–39, 42–44). Subgroup analysis suggested that PD-1 appeared to be associated with a higher incidence risk of hypothyroidism (OR=8.34, 95%CI:[5.24, 13.28], I2 = 37%, Z=8.94(P <0.00001); Supplementary Figure 7) (4, 14, 15, 18, 19, 25, 32, 34, 37–39, 42–44). Further stratification of subgroup analysis suggested that this risk trend was especially obvious in NSCLC subgroup (PD-1 VS. Docetaxel), when the control group was Docetaxel (OR=25.35, 95%CI:[7.95, 80.78], I2 = 0%, Z=5.47(P <0.00001)) (Chi2 = 20.89, df=8(P=0.007), I2 = 61.67%; Figure 2A) (39, 42, 44). Through subgroup analysis, moderate heterogeneity (I2 = 40%, Figure 2A) was considered to be mainly caused by one of NSCLC subgroups (PD-L1 VS. Docetaxel) (I2 = 67%, Figure 2A) (24, 26). No obvious publication bias was found in the funnel plot (Supplementary Figure 2A). No significant results was noted (OR=3.18, 95%CI:[0.64, 15.77], I2 = 0%, Z=1.41(P =0.16); Figure 3A), when the risk of hypothyroidism of grades 3-5 was assessed (14, 15, 24, 32). The corresponding funnel plot was shown in the supplement (Supplementary Figure 3A) (14, 15, 24, 32).
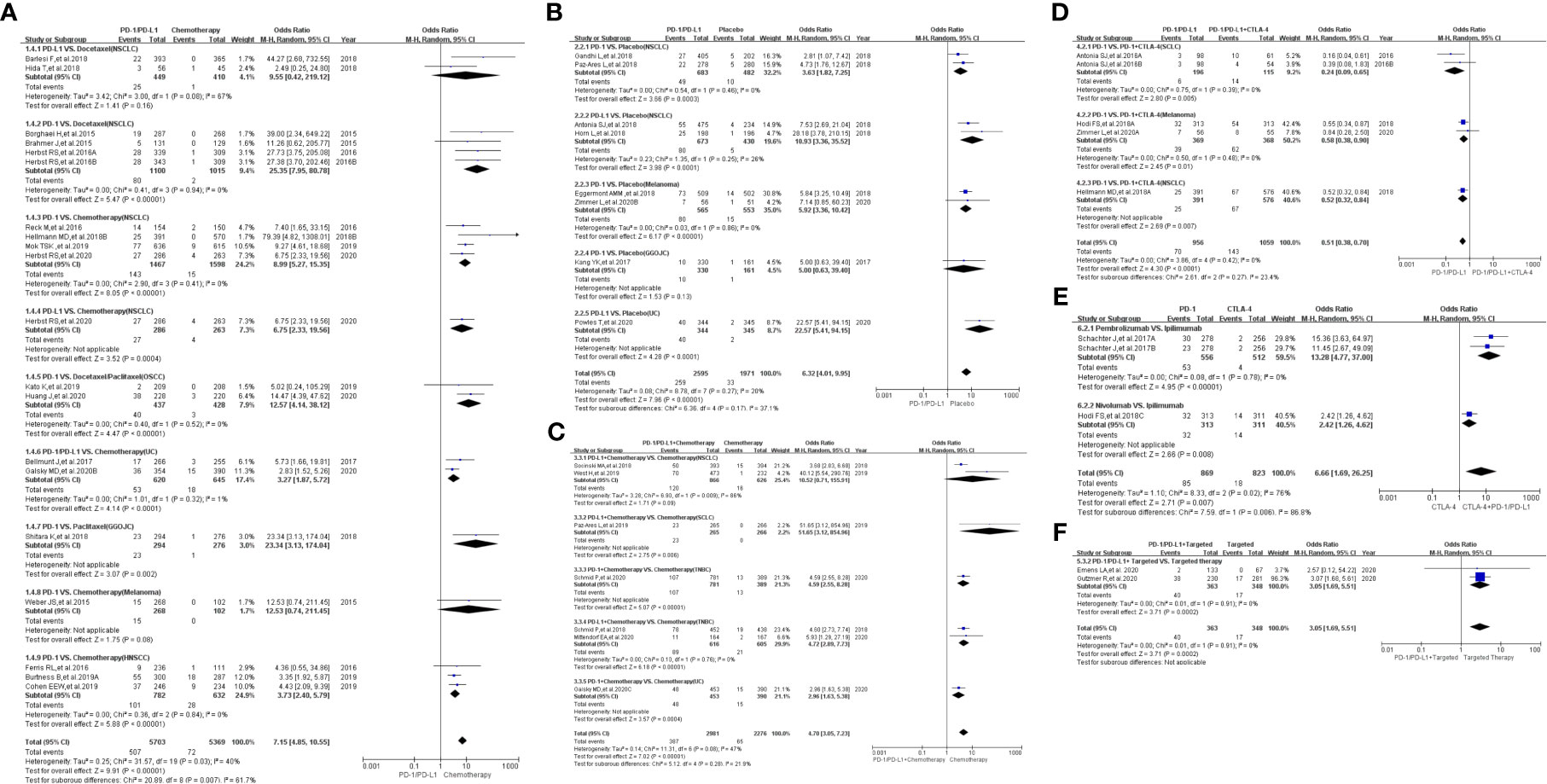
Figure 2 Forest plots of the risk of all-grade hypothyroidism. (A) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1, chemotherapy drugs and tumor types in both groups. (B) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Placebo): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (C) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1+Chemotherapy VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (D) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. PD-1/PD-L1+CTLA-4): subgroup analysis was conducted based on tumor types in the control group. (E) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1 VS. CTLA-4): subgroup analysis was conducted based on the PD-1 group. (F) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1+Targeted VS. Targeted).
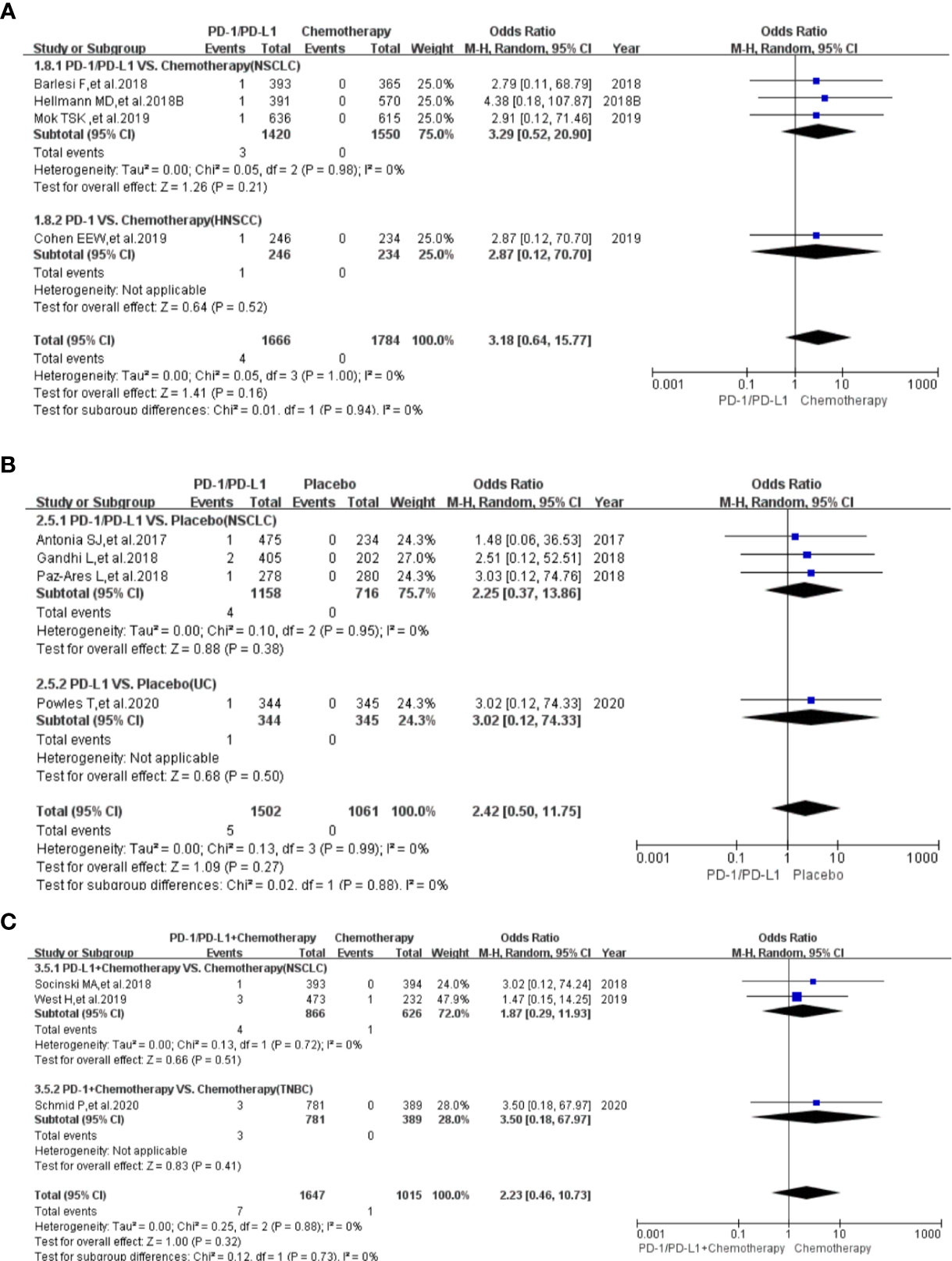
Figure 3 Forest plots of the risk of hypothyroidism for grades 3-5. (A) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (B) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Placebo): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (C) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1+Chemotherapy VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups.
Compared with placebo (PD-1/PD-L1 VS. Placebo), the risk of hypothyroidism of all grades was significantly higher (OR=6.32, 95%CI:[4.01, 9.95], I2 = 20%, Z=7.96(P <0.00001); Figure 2B) (5, 6, 27–29, 33, 35, 46). Through subgroup analysis, low heterogeneity (I2 = 20%, Figure 2B) was considered to be mainly caused by one of NSCLC subgroups (PD-L1 VS. Chemotherapy) (I2 = 26%, Figure 2B) (33, 46). No obvious publication bias was found in the corresponding funnel plot (Supplementary Figure 2B). No significant results was noted (OR=2.42, 95%CI:[0.50, 11.75], I2 = 0%, Z=1.09(P =0.27); Figure 3B), when the risk of hypothyroidism of grades 3-5 was calculated (5, 27, 29, 45). The corresponding funnel plot was shown in the supplement (Supplementary Figure 3B) (5, 27, 29, 45).
When PD-1/PD-L1 combined with chemotherapy was compared with chemotherapy (PD-1/PD-L1+Chemotherapy VS. Chemotherapy), the risk of hypothyroidism of all grades was found to be significantly higher (OR=4.70, 95%CI:[3.05, 7.23], I2 = 47%, Z=7.02(P <0.00001); Figure 2C) in the PD-1/PD-L1 group (7, 8, 11, 16, 17, 30, 31). Through subgroup analysis, moderate heterogeneity (I2 = 47%, Figure 2C) was considered to be mainly caused by the NSCLC subgroup (I2 = 86%, Figure 2C) (17, 30). No obvious publication bias was found in the funnel plot (Supplementary Figure 2C).
No significant results was noted (OR=2.23, 95%CI:[0.46, 10.73], I2 = 0%, Z=1.00(P =0.32); Figure 3C), when the risk of hypothyroidism of grades 3-5 was assessed (7, 17, 30). The corresponding funnel plot was shown in the supplement (Supplementary Figure 3C) (7, 17, 30).
When PD-1/PD-L1 combined with CTLA-4 was compared with PD-1/PD-L1 (PD-1/PD-L1 VS. PD-1/PD-L1+CTLA-4), the risk of hypothyroidism of all grades was found to be significantly lower (OR=0.51, 95%CI:[0.38, 0.70], I2 = 0%, Z=4.30(P <0.00001); Figure 2D) in the PD-1/PD-L1 group (6, 32, 40, 49). No heterogeneity (I2 = 0%) was found. No obvious publication bias was found in the funnel plot (Supplementary Figure 2D). There were too few data to calculate the risk of hypothyroidism of grades 3-5 (49).
Compared with CTLA-4 (PD-1 VS. CTLA-4), the risk of hypothyroidism of all grades was found to be significantly higher (OR=6.66, 95%CI:[1.69, 26.25], I2 = 76%, Z=2.71(P =0.007); Figure 2E) in the PD-1 group (36, 49). Through subgroup analysis, high heterogeneity (I2 = 76%, Figure 2E) might be related to the Nivolumab subgroup (Figure 2E) (49). The corresponding funnel plot was shown in the supplement (Supplementary Figure 3E). No data of hypothyroidism of grades 3-5 was found.
When PD-1/PD-L1 combined with targeted therapy was compared with PD-1/PD-L1 (PD-1/PD-L1+Targeted VS. Targeted), the risk of hypothyroidism of all grades was found to be significantly increased (OR=3.05, 95%CI:[1.69, 5.51], I2 = 0%, Z=3.71(P =0.0002); Figure 2F) (9, 10). No heterogeneity (I2 = 0%) was found. No obvious publication bias was found in the funnel plot (Supplementary Figure 2F). No data of hypothyroidism of grades 3-5 was found.
Hyperthyroidism was identified in 36 clinical trials (5–18, 21, 23–31, 33–35, 37–40, 42, 43, 45–50), 31 of which were used for the final meta-analysis (5–12, 14–18, 24–31, 33–35, 37–40, 42, 43, 45–50).
Compared with chemotherapy (PD-1/PD-L1 VS. Chemotherapy), the risk of hyperthyroidism of all grades was significantly higher (OR=4.79, 95%CI:[3.22, 7.13], I2 = 0%, Z=7.73(P <0.00001); Figure 4A) in PD-1/PD-L1 group (11, 12, 14, 15, 18, 24–26, 34, 37–39, 42, 43). Subgroup analysis suggested that PD-1 appeared to be associated with a higher incidence risk of hyperthyroidism (OR=5.59, 95%CI:[3.46, 9.04], I2 = 0%, Z=7.03(P <0.00001); Supplementary Figure 8) (14, 15, 18, 25, 34, 37–39, 42, 43). However, no statistical significant difference was found between PD-1 and PD-L1 subgroup (P =0.26, Supplementary Figure 8). No heterogeneity (I2 = 0%) was found (Figure 4A). No obvious publication bias was found in the corresponding funnel plot (Supplementary Figure 4A). No significant results was noted (OR=2.83, 95%CI:[0.45, 18.00], I2 = 0%, Z=1.10(P =0.27); Figure 5A), when the risk of hyperthyroidism of grades 3-5 was assessed (14, 18, 39). The corresponding funnel plot was shown in the supplement (Supplementary Figure 5A) (14, 18, 39).
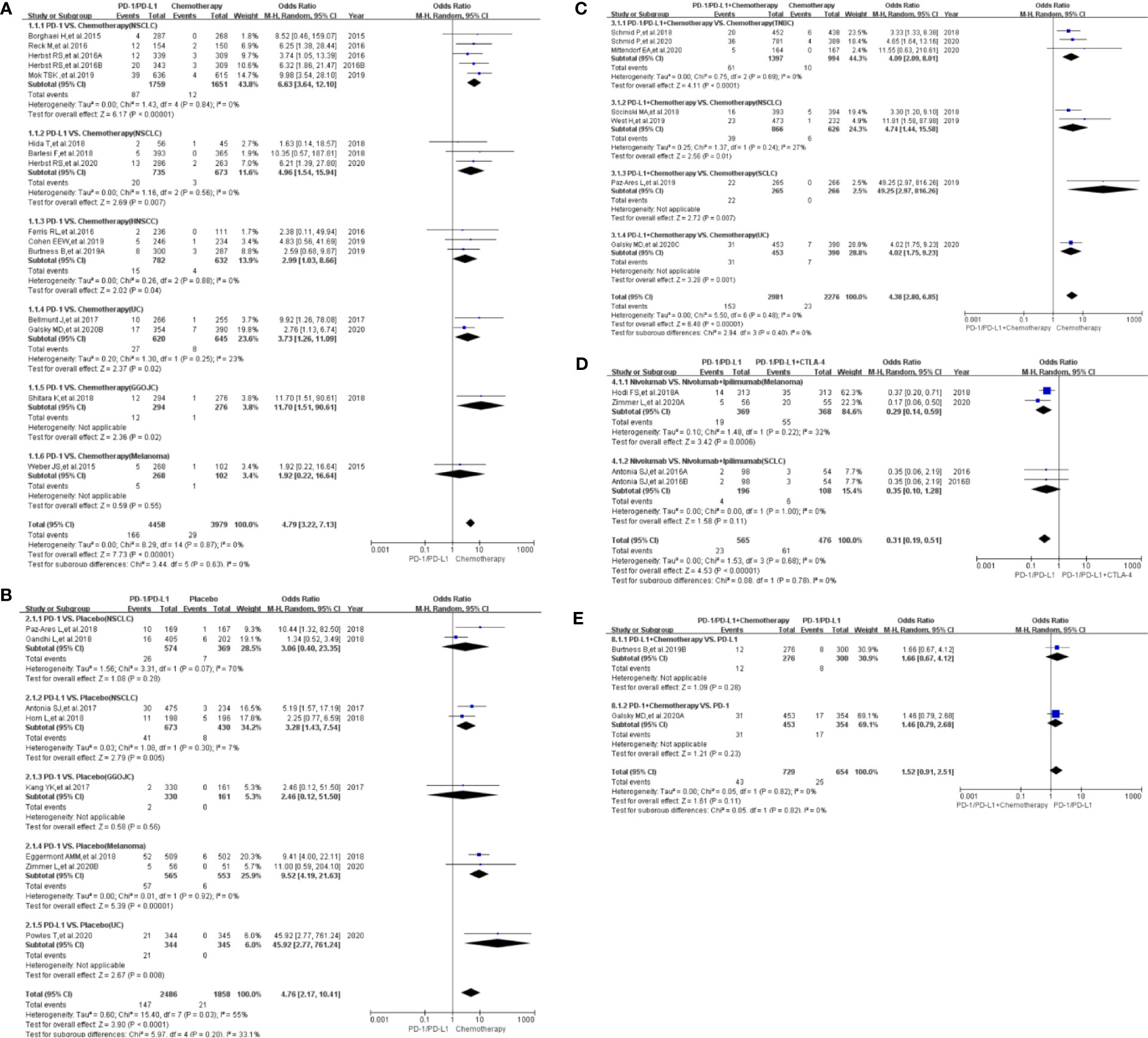
Figure 4 Forest plots of the risk of all-grade hyperthyroidism. (A) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (B) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Placebo): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (C) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1+Chemotherapy VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (D) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. PD-1/PD-L1+CTLA-4): subgroup analysis was conducted based on tumor types in the control group. (E) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1+chemotherapy VS. PD-1/PD-L1): subgroup analysis was conducted based on PD-1/PD-L1 in both groups.
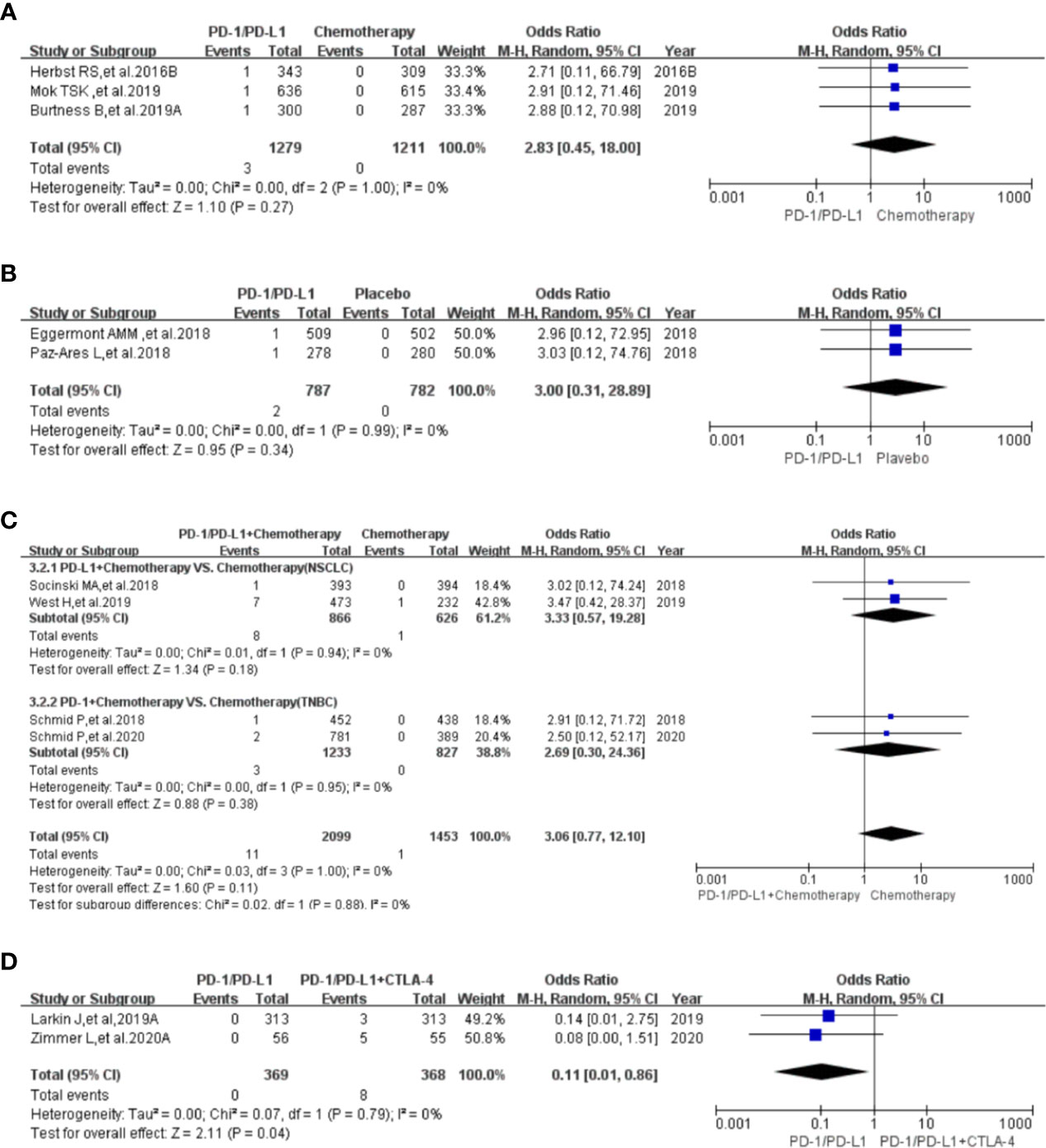
Figure 5 Forest plots of the risk of hyperthyroidism for grades 3-5. (A) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Chemotherapy). (B) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Placebo). (C) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1+Chemotherapy VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (D) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. PD-1/PD-L1+CTLA-4).
Compared with placebo (PD-1/PD-L1 VS. Placebo), the risk of hyperthyroidism of all grades was significantly higher (OR=4.76, 95%CI:[2.17, 10.41], I2 = 55%, Z=3.90(P <0.0001); Figure 4B) (5, 6, 27–29, 33, 35, 45). Through subgroup analysis, high heterogeneity (I2 = 55%) was considered to be mainly caused by PD-1 related NSCLC subgroup (I2 = 70%, Figure 4B) (27, 29). No obvious publication bias was found in the corresponding funnel plot (Supplementary Figure 4B). No significant results was noted (OR=3.00, 95%CI:[0.31, 28.89], I2 = 0%, Z=0.95 (P =0.34); Figure 5B), when the risk of hyperthyroidism of grades 3-5 was calculated (28, 29). The corresponding funnel plot was shown in the supplement (Supplementary Figure 5B) (28, 29).
When PD-1/PD-L1 combined with chemotherapy was compared with chemotherapy (PD-1/PD-L1+Chemotherapy VS. Chemotherapy), the risk of hyperthyroidism of all grades was found to be significantly higher (OR=4.38, 95%CI:[2.80, 6.85], I2 = 0%, Z=6.48(P <0.00001); Figure 4C) in the PD-1/PD-L1 related group (7, 8, 11, 16, 17, 30, 31). No heterogeneity (I2 = 0%) was found (Figure 4C). No obvious publication bias was found in the corresponding funnel plot (Supplementary Figure 4C). No significant results was noted (OR=3.06, 95%CI:[0.77, 12.10], I2 = 0%, Z=1.60(P =0.11); Figure 5C), when the risk of hyperthyroidism of grades 3-5 was assessed (7, 17, 30, 31). The corresponding funnel plot was shown in the supplement (Supplementary Figure 5C) (7, 17, 30, 31).
When PD-1/PD-L1 combined with CTLA-4 was compared with PD-1/PD-L1 (PD-1/PD-L1 VS. PD-1/PD-L1+CTLA-4), the risk of hyperthyroidism of all grades was found to be significantly lower (OR=0.31, 95%CI:[0.19, 0.51], I2 = 0%, Z=4.53 (P <0.00001); Figure 4D) in the PD-1/PD-L1 mono-therapy group (6, 40, 49). No heterogeneity (I2 = 0%) was found. No obvious publication bias was found in the funnel plot (Supplementary Figure 5D). Similar risk trend could also be seen, when the risk of hyperthyroidism of grades 3-5 was assessed (OR=0.11, 95%CI:[0.01, 0.86], I2 = 0%, Z=2.11(P =0.04); Figure 5D) (6, 50). The corresponding funnel plot was shown in the supplement (Supplementary Figure 5D) (6, 50).
When PD-1/PD-L1 combined with chemotherapy was compared with PD-1/PD-L1 (PD-1/PD-L1+Chemotherapy VS. PD-1/PD-L1), no statistical analysis results of hyperthyroidism of all grades was found (OR=1.52, 95%CI:[0.91, 2.51], I2 = 0%, Z=1.61(P =0.011); Figure 4E) (11, 18). No heterogeneity (I2 = 0%) was found. No obvious publication bias was found in the funnel plot (Supplementary Figure 4E). There were too few data to calculate the risk of hyperthyroidism of grades 3-5 (18).
Thyroiditis was reported in 17 clinical trials (6, 7, 14, 16, 23, 24, 27–29, 34, 35, 37–39, 41, 42, 47–50), 16 of which were used for the final meta-analysis (6, 7, 14, 16, 24, 27–29, 34, 35, 37–39, 41, 42, 47–50).
Compared with chemotherapy (PD-1/PD-L1 VS. Chemotherapy), the risk of thyroiditis of all grades was significantly higher (OR=5.88, 95%CI:[1.89, 18.30], I2 = 0%, Z=3.06(P =0.002); Figure 6A) in PD-1/PD-L1 group (14, 24, 34, 37–39, 42). Subgroup analysis suggested that PD-1 appeared to be associated with a higher incidence risk of thyroiditis in NSCLC subgroup (OR=7.47, 95%CI:[1.67, 33.37], I2 = 0%, Z=2.63(P =0.008); Figure 6A) (14, 37, 39, 42). However, no statistical significant difference was found indifferent subgroups (P =0.93, Figure 6A). No heterogeneity (I2 = 0%) was found (Figure 6A). No obvious publication bias was found in the corresponding funnel plot (Supplementary Figure 6A). No data of thyroiditis of grades 3-5 was found.
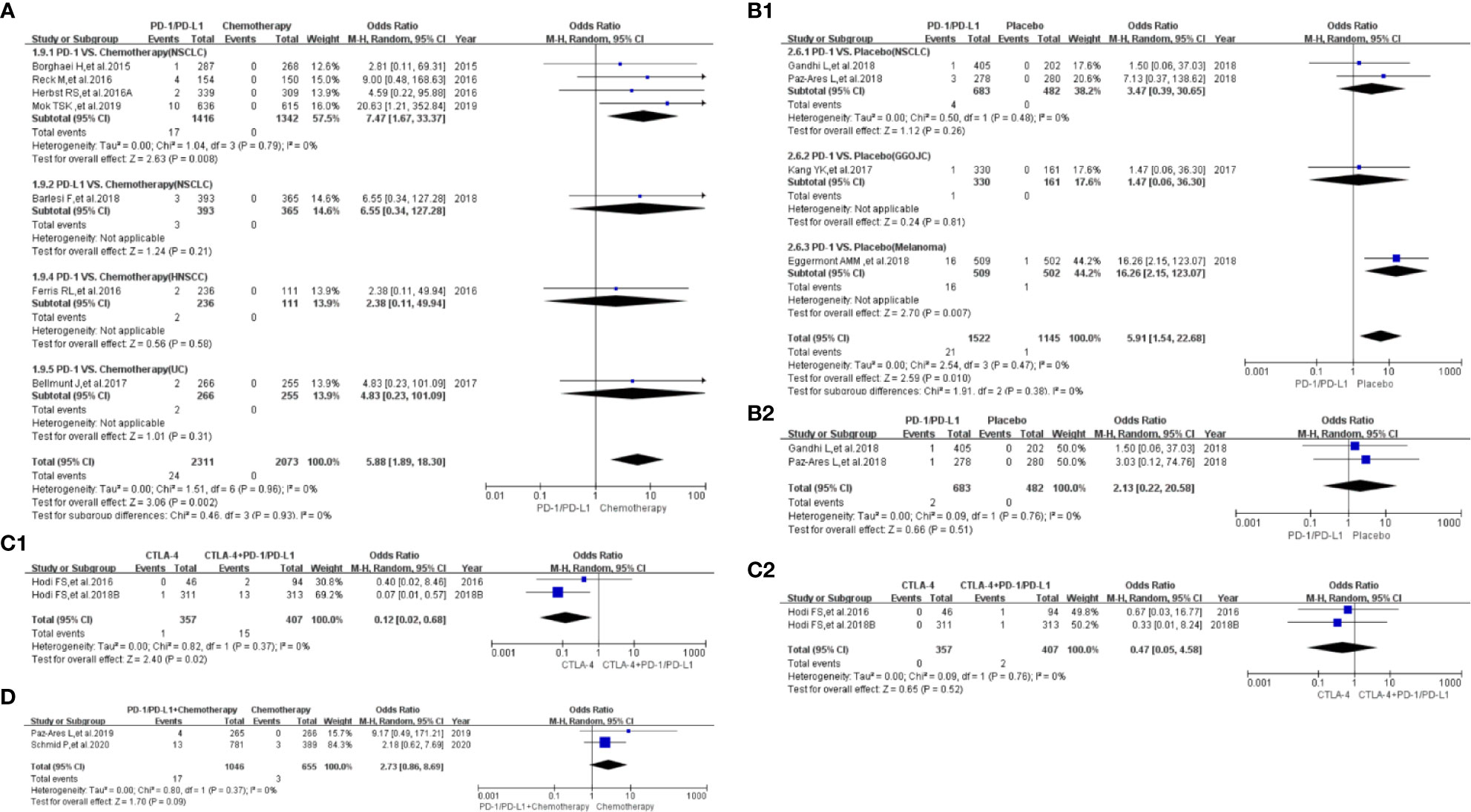
Figure 6 Forest plots of the risk of thyroiditis. (A) The risk of all-grade thyroiditis calculated by the random effect (RE) model (PD-1/PD-L1 VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (B1) The risk of all-grade thyroiditis calculated by the random effect (RE) model (PD-1/PD-L1 VS. Placebo): subgroup analysis was conducted based on tumor types in the control group. (B2) The risk of thyroiditis for grade 3-5 calculated by the random effect (RE) model (PD-1/PD-L1 VS. Placebo). (C1) The risk of all-grade thyroiditis calculated by the random effect (RE) model (CTLA-4 VS. PD-1/PD-L1+CTLA-4): subgroup analysis was conducted based on tumor types in the control group. (C2) The risk of thyroiditis for grades 3-5 calculated by the random effect (RE) model (CTLA-4 VS. PD-1/PD-L1+CTLA-4). (D) The risk of all-grade thyroiditis calculated by the random effect (RE) model (PD-1/PD-L1+Chemotherapy VS. Chemotherapy).
Compared with placebo (PD-1/PD-L1 VS. Placebo), the risk of thyroiditis of all grades was significantly higher (OR=5.91, 95%CI:[1.54, 22.68], I2 = 0%, Z=2.59(P =0.010); Figure 6B1) (27–29, 35). No heterogeneity (I2 = 0%) was found. No obvious publication bias was found in the funnel plot (Supplementary Figure 6B1). No statistical significant analysis results was found, when the risk of thyroiditis of grades 3-5 was checked (OR=2.13, 95%CI:[0.22, 20.58], I2 = 0%, Z=0.66(P =0.051); Figure 6B2) (27, 29). The corresponding funnel plot was shown in the supplement (Supplementary Figure 6B2) (27, 29).
When PD-1/PD-L1 combined with CTLA-4 was compared with CTLA-4 (CTLA-4 VS. PD-1/PD-L1+CTLA-4), the risk of thyroiditis of all grades was found to be significantly lower (OR=0.12, 95%CI:[0.02, 0.68], I2 = 0%, Z=2.40(P =0.02); Figure 6C1) in CTLA-4 group (41, 49). No heterogeneity (I2 = 0%) was found. No obvious publication bias was found in the funnel plot (Supplementary Figure 6C1). Similar risk trend could also be found, when the risk of thyroiditis of grades 3-5 was evaluated (OR=0.47, 95%CI:[0.05, 4.58], I2 = 0%, Z=0.65(P =0.52); Figure 6C2) (41, 49). Np heterogeneity (I2 = 0%, Figure 6C2) was found. The corresponding funnel plot was shown in the supplement (Supplementary Figure 6C2) (41, 49).
When PD-1/PD-L1 combined with chemotherapy was compared with chemotherapy (PD-1/PD-L1+Chemotherapy VS. Chemotherapy), no statistical analysis results of thyroiditis of all grades was found (OR=2.73, 95%CI:[0.86, 8.69], I2 = 0%, Z=1.70(P =0.09); Figure 6D) (7, 16). No heterogeneity (I2 = 0%) was found. No obvious publication bias was found in the funnel plot (Supplementary Figure 6D). No data of thyroiditis of grades 3-5 was found.
Programmed cell death protein 1 (PD-1) and its ligand (PD-L1) inhibitors were developed to overcome the immune escape mechanisms of cancer progression and manipulate the immune system to recognize and attack cancer cells (1). A large number of PD-1/PD-L1 related immune-related toxicities, including thyroid dysfunction, had been reported (1, 4–50), which might be related to this immune regulation mechanism. Clinical manifestations of thyroid dysfunction ranged from life threatening to no signs or symptoms (64–66). Therefore, systematic assessment of the risk of thyroid dysfunction had an important guiding significance for clinical work (1).
Consistent with previous reports (1), hypothyroidism was much more common with PD-1/PD-L1 inhibitors than others (Table 1) (4–50). Through comprehensive analysis, we found that the risk of hypothyroidism of all grades in the PD-1/PD-L1 mono-therapy group was significantly higher compared to the chemotherapy arm (Figure 2A) (4, 11, 12, 14, 15, 18, 19, 24–26, 32, 34, 37–39, 42–44). Similar results could also be noted, when the control group was placebo or CTLA-4 (Figures 2B, E) (5, 6, 27–29, 33, 35, 36, 46, 49). When PD-1/PD-L1 was combined with other treatments for cancer patients, the risk of hypothyroidism of all grades was also significantly increased (Figures 2C, D, F) (6–11, 16, 17, 30–32, 40, 49). Subgroup analysis suggested that PD-1 appeared to be associated with a higher incidence risk of hypothyroidism compared to PD-L1 (Supplementary Figure 7) (4, 14, 15, 18, 19, 25, 32, 34, 37–39, 42–44). But this difference between PD-1 and PD-L1 subgroup was not statistical significant (Supplementary Figure 7) (4, 14, 15, 18, 19, 25, 32, 34, 37–39, 42–44). Due to the lack of clinical trials on PD-1 and PD-L1 head-to-head comparisons, we could not clarify the difference in the risk of hypothyroidism between the two. For the existence of heterogeneity (Figures 2A–C, E), we conducted a sufficient stratified subgroup analysis and inferred the source of the heterogeneity. Furthermore, no obvious publication bias was found among all the enrolled clinical trials (Supplementary Figure 2). Therefore, the conclusion that PD-1/PD-L1 increased the risk of hypothyroidism of all grades was considered to be much more reliable. No significant results was noted, when the risk of hypothyroidism of grades 3-5 was calculated (Figure 3 and Supplementary Figure 3).
Drug-induced thyroid dysfunction is one of the common causes of hyperthyroidism (67). Whether PD-1/PD-L1 inhibitors were used alone or in combination with other drugs, it indicated that PD-1/PD-L1 inhibitors increased the risk of hyperthyroidism of all grades (Figures 4A–D). When PD-1/PD-L1 combined with chemotherapy was compared with PD-1/PD-L1, no statistical analysis results of hyperthyroidism of all grades was found (Figure 4E) (11, 18). Through the above analysis, we clarified the role of PD-1/PD-L1 inhibitors in increasing the risk of hyperthyroidism of all grades (Figure 4 and Supplementary Figure 4) (5–12, 14–18, 24–31, 33–35, 37–40, 42, 43, 45–50). Through subgroup analysis, high heterogeneity (I2 = 55%) was considered to be mainly caused by PD-1 related NSCLC subgroup (I2 = 70%, Figure 4B) (27, 29). No obvious publication bias was found among all the enrolled clinical trials (Supplementary Figure 4). Though similar incidence trend could also be seen in the assessment of hypothyroidism of grades 3-5 (Figure 5), statistical significant result was only found in (Figure 5D). Since only two clinical trials were included (Figure 5D), the analysis results need to be further verified.
In the clinical trials included in the study, the incidence rate of thyroiditis was lower than those of hyperthyroidism and hypothyroidism (Table 1). Similar to the previous analysis results, PD-1/PD-L1 inhibitors played the same role in increasing the risk of thyroiditis (Figure 6). No obvious heterogeneity and publication bias was found among all enrolled clinical trials (Figure 6 and Supplementary Figure 6) (6, 7, 14, 16, 24, 27–29, 34, 35, 37–39, 41, 42, 47–50).
Thyroid dysfunction had also been reported in other 5 PD-1/PD-L1 investigated clinical trials (13, 20–23). For the heterogeneity among these 5 clinical trials, it was impossible for us to conduct a meta-analysis. However, we found that sunitinib might play a similar role to PD-1/PD-L1 on increasing the risk of thyroid dysfunction (21–23).
By reviewing and analyzing PD-1/PD-L1 related literature (4–50), we found that PD-1/PD-L1 increased the risk of thyroid dysfunction. It reminds us that we need to monitor and evaluate the thyroid function status in time for patients receiving PD-1/PD-L1 treatment to prevent the occurrence of adverse events (1–3, 64–67).
Strengths: This meta-analysis was conducted according to the PRISMA guidelines. The literature searching process was put into practice in accordance with the PICOS principle. The quality of all enrolled clinical trials was high. Stratification and subgroup analyses were conducted as much as possible. Therefore, the conclusion was much more reliable.
Limitations: First, some clinical trials related to PD-1/PD-L1 inhibitors cannot be included for meta-analysis due to obvious heterogeneity. Second, the low number of studies that reported the data of thyroid dysfunction made it difficult to get a definite conclusion.
Whether used alone or in combination with other anti-tumor drugs, PD-1/PD-L1 inhibitors increased the risk of thyroid dysfunction, especially for hypothyroidism. Furthermore, PD-1/PD-L1 was better than chemotherapy and CTLA-4 in increasing the risk of thyroid dysfunction.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
The corresponding authors (YPS and GS) had the right to deal with all the data and were responsible for the decision to submit this manuscript for publication. YT, RL, YL, ML, YXS, YZ, AG and QW had the full data of the manuscript. YT, RL, YL, ML, and YXS were responsible for checking and evaluating the quality of the data and enrolled studies. YT was appointed for writing the draft of this manuscript. All authors contributed to the article and approved the submitted version.
This study was funded by the Academic Promotion Program of Shandong First Medical University (2019QL025; YPS), Natural Science Foundation of Shandong Province (ZR2019MH042; YPS), Jinan Science and Technology Program (201805064; YPS), the National Science and Technology Major Project of the Ministry of Science and Technology of China (2020ZX09201025; GS), Postdoctoral Innovation Project of Jinan (YT), the National Natural Science Foundation of China (No. 81170087; GS), the Provincial Natural Science Foundation of Shandong (ZR2018MH003; GS), the Clinical Medical Science and Technology Innovation Program of Jinan (201805004; GS).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2021.667650/full#supplementary-material
Supplementary Figure 1 | A summary table of review authors’ judgements for each risk of bias item for each study.
Supplementary Figure 2 | Funnel plots of the risk of all-grade hypothyroidism. (A) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1, chemotherapy drugs and tumor types in both groups. (B) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Placebo): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (C) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1+Chemotherapy VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (D) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. PD-1/PD-L1+CTLA-4): subgroup analysis was conducted based on tumor types in the control group. (E) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1 VS. CTLA-4): subgroup analysis was conducted based on the PD-1 group. (F) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1+Targeted VS. Targeted).
Supplementary Figure 3 | Funnel plots of the risk of hypothyroidism for grades 3-5. (A) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (B) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Placebo): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (C) The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1+Chemotherapy VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups.
Supplementary Figure 4 | Funnel plots of the risk of all-grade hyperthyroidism. (A) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (B) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Placebo): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (C) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1+Chemotherapy VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (D) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. PD-1/PD-L1+CTLA-4): subgroup analysis was conducted based on tumor types in the control group. (E) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1+chemotherapy VS. PD-1/PD-L1): subgroup analysis was conducted based on PD-1/PD-L1 in both groups.
Supplementary Figure 5 | Funnel plots of the risk of hyperthyroidism for grades 3-5. (A) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Chemotherapy). (B) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Placebo). (C) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1+Chemotherapy VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (D) The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. PD-1/PD-L1+CTLA-4).
Supplementary Figure 6 | Funnel plots of the risk of thyroiditis. (A) The risk of all-grade thyroiditis calculated by the random effect (RE) model (PD-1/PD-L1 VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 and tumor types in both groups. (B1) The risk of all-grade thyroiditis calculated by the random effect (RE) model (PD-1/PD-L1 VS. Placebo): subgroup analysis was conducted based on tumor types in the control group. (B2) The risk of thyroiditis for grade 3-5 calculated by the random effect (RE) model (PD-1/PD-L1 VS. Placebo). (C1) The risk of all-grade thyroiditis calculated by the random effect (RE) model (CTLA-4 VS. PD-1/PD-L1+CTLA-4): subgroup analysis was conducted based on tumor types in the control group. (C2) The risk of thyroiditis for grades 3-5 calculated by the random effect (RE) model (CTLA-4 VS. PD-1/PD-L1+CTLA-4). (D) The risk of all-grade thyroiditis calculated by the random effect (RE) model (PD-1/PD-L1+Chemotherapy VS. Chemotherapy).
Supplementary Figure 7 | Forest plots of the risk of all-grade hypothyroidism. The risk of hypothyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 in both groups.
Supplementary Figure 8 | Forest plots of the risk of all-grade hyperthyroidism. The risk of hyperthyroidism calculated by the random effect (RE) model (PD-1/PD-L1 VS. Chemotherapy): subgroup analysis was conducted based on PD-1/PD-L1 in both groups.
PD-1, Programmed Cell Death-1; PD-L1, Programmed Cell Death Ligand 1; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; PICOS, Participants, Interventions, Comparisons, Outcomes, and Study design; N/A, No Available; HR, Hazard Ratios; OR, Odds Ratio; CI, Confidence Interval; RE, Random Effect; NSCLC, Non-Small Cell Lung Cancer; SCLC, Small Cell Lung Cancer; OSCC, Oesophageal Squamous Cell Carcinoma; HNSCC, Head and Neck Squamous Cell Carcinoma; UC, Urothelial Cancer; BC, Breast Cancer; RCC, Renal Cell Carcinoma; NOS, Newcastle-Ottawa scale; TNBC, Triple-Negative Breast Cancer; GGOJC, Gastric or Gastro-Oesophageal Junction Cancer.
1. Kennedy LB, Salama AKS. A Review of Cancer Immunotherapy Toxicity. CA Cancer J Clin (2020) 70(2):86–104. doi: 10.3322/caac.21596
2. Thompson JA. New NCCN Guidelines: Recognition and Management of Immunotherapy-Related Toxicity. J Natl Compr Canc Netw (2018) 16(suppl 5):594–6. doi: 10.6004/jnccn.2018.0047
3. Postow MA, Sidlow R, Hellmann MD. Immune-Related Adverse Events Associated With Immune Checkpoint Blockade. N Engl J Med (2018) 378:158–68. doi: 10.1056/NEJMra1703481
4. Huang J, Xu J, Chen Y, Zhuang W, Zhang Y, Chen Z, et al. Camrelizumab Versus Investigator’s Choice of Chemotherapy as Second-Line Therapy for Advanced or Metastatic Oesophageal Squamous Cell Carcinoma (ESCORT): A Multicentre, Randomised, Open-Label, Phase 3 Study [Published Online Ahead of Print, 2020 May 13]. Lancet Oncol (2020), S1470–2045(20)30110-8.
5. Powles T, Park SH, Voog E, Caserta C, Valderrama BP, Gurney H, et al. Avelumab Maintenance Therapy for Advanced or Metastatic Urothelial Carcinoma. N Engl J Med (2020) 383(13):1218–30. doi: 10.1056/NEJMoa2002788
6. Zimmer L, Livingstone E, Hassel JC, Fluck M, Eigentler T, Loquai C, et al. Adjuvant Nivolumab Plus Ipilimumab or Nivolumab Monotherapy Versus Placebo in Patients With Resected Stage IV Melanoma With No Evidence of Disease (IMMUNED): A Randomised, Double-Blind, Placebo-Controlled, Phase 2 Trial. Lancet (2020) 395(10236):1558–68. doi: 10.1016/S0140-6736(20)30417-7
7. Schmid P, Cortes J, Pusztai L, McArthur H, Kümmel S, Bergh J, et al. KEYNOTE-522 Investigators. Pembrolizumab for Early Triple-Negative Breast Cancer. N Engl J Med (2020) 382(9):810–21. doi: 10.1056/NEJMoa1910549
8. Mittendorf EA, Zhang H, Barrios CH, Saji S, Jung KH, Hegg R, et al. Neoadjuvant Atezolizumab in Combination With Sequential Nab-Paclitaxel and Anthracycline-Based Chemotherapy Versus Placebo and Chemotherapy in Patients With Early-Stage Triple-Negative Breast Cancer (IMpassion031): A Randomised, Double-Blind, Phase 3 Trial. Lancet (2020) 396(10257):1090–100. doi: 10.1016/S0140-6736(20)31953-X
9. Emens LA, Esteva FJ, Beresford M, Saura C, De Laurentiis M, Kim SB, et al. Trastuzumab Emtansine Plus Atezolizumab Versus Trastuzumab Emtansine Plus Placebo in Previously Treated, HER2-Positive Advanced Breast Cancer (KATE2): A Phase 2, Multicentre, Randomised, Double-Blind Trial. Lancet Oncol (2020) 21(10):1283–95. doi: 10.1016/S1470-2045(20)30465-4
10. Gutzmer R, Stroyakovskiy D, Gogas H, Robert C, Lewis K, Protsenko S, et al. Atezolizumab, Vemurafenib, and Cobimetinib as First-Line Treatment for Unresectable Advanced BRAFV600 Mutation-Positive Melanoma (IMspire150): Primary Analysis of the Randomised, Double-Blind, Placebo-Controlled, Phase 3 Trial. Lancet (2020) 395(10240):1835–44. doi: 10.1016/S0140-6736(20)30934-X
11. Galsky MD, Arija JÁA, Bamias A, Davis ID, De Santis M, Kikuchi E, et al. Atezolizumab With or Without Chemotherapy in Metastatic Urothelial Cancer (IMvigor130): A Multicentre, Randomised, Placebo-Controlled Phase 3 Trial. Lancet (2020) 395(10236):1547–57. doi: 10.1016/S0140-6736(20)30230-0
12. Herbst RS, Giaccone G, de Marinis F, Reinmuth N, Vergnenegre A, Barrios CH, et al. Atezolizumab for First-Line Treatment of PD-L1-Selected Patients With NSCLC. N Engl J Med (2020) 383(14):1328–39. doi: 10.1056/NEJMoa1917346
13. Reck M, Wehler T, Orlandi F, Nogami N, Barone C, Moro-Sibilot D, et al. Safety and Patient-Reported Outcomes of Atezolizumab Plus Chemotherapy With or Without Bevacizumab Versus Bevacizumab Plus Chemotherapy in Non-Small-Cell Lung Cancer. J Clin Oncol (2020) 38(22):2530–42. doi: 10.1200/JCO.19.03158
14. Mok TSK, Wu YL, Kudaba I, Kowalski DM, Cho BC, Turna HZ, et al. Pembrolizumab Versus Chemotherapy for Previously Untreated, PD-L1-Expressing, Locally Advanced or Metastatic Non-Small-Cell Lung Cancer (KEYNOTE-042): A Randomised, Open-Label, Controlled, Phase 3 Trial. Lancet (2019) 393(10183):1819–30. doi: 10.1016/S0140-6736(18)32409-7
15. Cohen EEW, Soulières D, Le Tourneau C, Dinis J, Licitra L, Ahn MJ, et al. Pembrolizumab Versus Methotrexate, Docetaxel, or Cetuximab for Recurrent or Metastatic Head-and-Neck Squamous Cell Carcinoma (KEYNOTE-040): A Randomised, Open-Label, Phase 3 Study [Published Correction Appears in Lancet. 2019 Jan 12;393(10167):132]. Lancet (2019) 393(10167):156–67.
16. Paz-Ares L, Dvorkin M, Chen Y, Reinmuth N, Hotta K, Trukhin D, et al. Durvalumab Plus Platinum-Etoposide Versus Platinum-Etoposide in First-Line Treatment of Extensive-Stage Small-Cell Lung Cancer (CASPIAN): A Randomised, Controlled, Open-Label, Phase 3 Trial. Lancet (2019) 394(10212):1929–39. doi: 10.1016/S0140-6736(19)32222-6
17. West H, McCleod M, Hussein M, Morabito A, Rittmeyer A, Conter HJ, et al. Atezolizumab in Combination With Carboplatin Plus Nab-Paclitaxel Chemotherapy Compared With Chemotherapy Alone as First-Line Treatment for Metastatic Non-Squamous Non-Small-Cell Lung Cancer (IMpower130): A Multicentre, Randomised, Open-Label, Phase 3 Trial. Lancet Oncol (2019) 20(7):924–37. doi: 10.1016/S1470-2045(19)30167-6
18. Burtness B, Harrington KJ, Greil R, Soulières D, Tahara M, de Castro G Jr, et al. Pembrolizumab Alone or With Chemotherapy Versus Cetuximab With Chemotherapy for Recurrent or Metastatic Squamous Cell Carcinoma of the Head and Neck (KEYNOTE-048): A Randomised, Open-Label, Phase 3 Study. Lancet (2019) 394(10212):1915–28. doi: 10.1016/S0140-6736(19)32591-7
19. Kato K, Cho BC, Takahashi M, Okada M, Lin CY, Chin K, et al. Nivolumab Versus Chemotherapy in Patients With Advanced Oesophageal Squamous Cell Carcinoma Refractory or Intolerant to Previous Chemotherapy (ATTRACTION-3): A Multicentre, Randomised, Open-Label, Phase 3 Trial. Lancet Oncol (2019) 20(11):1506–17. doi: 10.1016/S1470-2045(19)30626-6
20. Sullivan RJ, Hamid O, Gonzalez R, Infante JR, Patel MR, Hodi FS, et al. Atezolizumab Plus Cobimetinib and Vemurafenib in BRAF-Mutated Melanoma Patients. Nat Med (2019) 25(6):929–35. doi: 10.1038/s41591-019-0474-7
21. Rini BI, Powles T, Atkins MB, Escudier B, McDermott DF, Suarez C, et al. Atezolizumab Plus Bevacizumab Versus Sunitinib in Patients With Previously Untreated Metastatic Renal Cell Carcinoma (IMmotion151): A Multicentre, Open-Label, Phase 3, Randomised Controlled Trial. Lancet (2019) 393(10189):2404–15. doi: 10.1016/S0140-6736(19)30723-8
22. Motzer RJ, Penkov K, Haanen J, Rini B, Albiges L, Campbell MT, et al. Avelumab Plus Axitinib Versus Sunitinib for Advanced Renal-Cell Carcinoma. N Engl J Med (2019) 380(12):1103–15. doi: 10.1056/NEJMoa1816047
23. Motzer RJ, Rini BI, McDermott DF, Arén Frontera O, Hammers HJ, Carducci MA, et al. Nivolumab Plus Ipilimumab Versus Sunitinib in First-Line Treatment for Advanced Renal Cell Carcinoma: Extended Follow-Up of Efficacy and Safety Results From a Randomised, Controlled, Phase 3 Trial. Lancet Oncol (2019) 20(10):1370–85. doi: 10.1016/S1470-2045(19)30413-9
24. Barlesi F, Vansteenkiste J, Spigel D, Ishii H, Garassino M, de Marinis F, et al. Avelumab Versus Docetaxel in Patients With Platinum-Treated Advanced Non-Small-Cell Lung Cancer (JAVELIN Lung 200): An Open-Label, Randomised, Phase 3 Study. Lancet Oncol (2018) 19(11):1468–79. doi: 10.1016/S1470-2045(18)30673-9
25. Shitara K, Özgüroğlu M, Bang YJ, Di Bartolomeo M, Mandalà M, Ryu MH, et al. Pembrolizumab Versus Paclitaxel for Previously Treated, Advanced Gastric or Gastro-Oesophageal Junction Cancer (KEYNOTE-061): A Randomised, Open-Label, Controlled, Phase 3 Trial. Lancet (2018) 392(10142):123–33. doi: 10.1093/annonc/mdy208.004
26. Hida T, Kaji R, Satouchi M, Ikeda N, Horiike A, Nokihara H, et al. Atezolizumab in Japanese Patients With Previously Treated Advanced Non-Small-Cell Lung Cancer: A Subgroup Analysis of the Phase 3 OAK Study. Clin Lung Cancer (2018) 19(4):e405–15. doi: 10.1016/j.cllc.2018.01.004
27. Gandhi L, Rodríguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F, et al. Pembrolizumab Plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. N Engl J Med (2018) 378(22):2078–92. doi: 10.1056/NEJMoa1801005
28. Eggermont AMM, Blank CU, Mandala M, Long GV, Atkinson V, Dalle S, et al. Adjuvant Pembrolizumab Versus Placebo in Resected Stage III Melanoma. N Engl J Med (2018) 378(19):1789–801. doi: 10.1056/NEJMoa1802357
29. Paz-Ares L, Luft A, Vicente D, Tafreshi A, Gümüş M, Mazières J, et al. Pembrolizumab Plus Chemotherapy for Squamous Non-Small-Cell Lung Cancer. N Engl J Med (2018) 379(21):2040–51. doi: 10.1056/NEJMoa1810865
30. Socinski MA, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N, et al. Atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. N Engl J Med (2018) 378(24):2288–301. doi: 10.1056/NEJMoa1716948
31. Schmid P, Adams S, Rugo HS, Schneeweiss A, Barrios CH, Iwata H, et al. Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. N Engl J Med (2018) 379(22):2108–21. doi: 10.1056/NEJMoa1809615
32. Hellmann MD, Ciuleanu TE, Pluzanski A, Lee JS, Otterson GA, Audigier-Valette C, et al. Nivolumab Plus Ipilimumab in Lung Cancer With a High Tumor Mutational Burden. N Engl J Med (2018) 378(22):2093–104. doi: 10.1056/NEJMoa1801946
33. Horn L, Mansfield AS, Szczęsna A, Havel L, Krzakowski M, Hochmair MJ, et al. First-Line Atezolizumab Plus Chemotherapy in Extensive-Stage Small-Cell Lung Cancer. N Engl J Med (2018) 379(23):2220–9. doi: 10.1056/NEJMoa1809064
34. Bellmunt J, de Wit R, Vaughn DJ, Fradet Y, Lee JL, Fong L, et al. KEYNOTE-045 Investigators.Pembrolizumab as Second-Line Therapy for Advanced Urothelial Carcinoma. N Engl J Med (2017) 376(11):1015–26. doi: 10.1056/NEJMoa1613683
35. Kang YK, Boku N, Satoh T, Ryu MH, Chao Y, Kato K, et al. Nivolumab in Patients With Advanced Gastric or Gastro-Oesophageal Junction Cancer Refractory to, or Intolerant of, at Least Two Previous Chemotherapy Regimens (ONO-4538-12, ATTRACTION-2): A Randomised, Double-Blind, Placebo-Controlled, Phase 3 Trial. Lancet (2017) 390(10111):2461–71. doi: 10.1016/S0140-6736(17)31827-5
36. Schachter J, Ribas A, Long GV, Arance A, Grob JJ, Mortier L, et al. Pembrolizumab Versus Ipilimumab for Advanced Melanoma: Final Overall Survival Results of a Multicentre, Randomised, Open-Label Phase 3 Study (KEYNOTE-006). Lancet (2017) 390(10105):1853–62. doi: 10.1016/S0140-6736(17)31601-X
37. Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, et al. Pembrolizumab Versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med (2016) 375(19):1823–33. doi: 10.1056/NEJMoa1606774
38. Ferris RL, Blumenschein G Jr, Fayette J, Guigay J, Colevas AD, Licitra L, et al. Nivolumab for Recurrent Squamous-Cell Carcinoma of the Head and Neck. N Engl J Med (2016) 375(19):1856–67. doi: 10.1056/NEJMoa1602252
39. Herbst RS, Baas P, Kim DW, Felip E, Pérez-Gracia JL, Han JY, et al. Pembrolizumab Versus Docetaxel for Previously Treated, PD-L1-Positive, Advanced Non-Small-Cell Lung Cancer (KEYNOTE-010): A Randomised Controlled Trial. Lancet (2016) 387(10027):1540–50. doi: 10.1016/S0140-6736(15)01281-7
40. Antonia SJ, López-Martin JA, Bendell J, Ott PA, Taylor M, Eder JP, et al. Nivolumab Alone and Nivolumab Plus Ipilimumab in Recurrent Small-Cell Lung Cancer (CheckMate 032): A Multicentre, Open-Label, Phase 1/2 Trial. Lancet Oncol (2016) 17(7):883–95. doi: 10.1016/S1470-2045(16)30098-5
41. Hodi FS, Chesney J, Pavlick AC, Robert C, Grossmann KF, McDermott DF, et al. Combined Nivolumab and Ipilimumab Versus Ipilimumab Alone in Patients With Advanced Melanoma: 2-Year Overall Survival Outcomes in a Multicentre, Randomised, Controlled, Phase 2 Trial. Lancet Oncol (2016) 17(11):1558–68. doi: 10.1016/S1470-2045(16)30366-7
42. Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, et al. Nivolumab Versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med (2015) 373(17):1627–39. doi: 10.1056/NEJMoa1507643
43. Weber JS, D’Angelo SP, Minor D, Hodi FS, Gutzmer R, Neyns B, et al. Nivolumab Versus Chemotherapy in Patients With Advanced Melanoma Who Progressed After Anti-CTLA-4 Treatment (CheckMate 037): A Randomised, Controlled, Open-Label, Phase 3 Trial. Lancet Oncol (2015) 16(4):375–84. doi: 10.1016/S1470-2045(15)70076-8
44. Brahmer J, Reckamp KL, Baas P, Crinò L, Eberhardt WE, Poddubskaya E, et al. Nivolumab Versus Docetaxel in Advanced Squamous-Cell Non-Small-Cell Lung Cancer. N Engl J Med (2015) 373(2):123–35. doi: 10.1056/NEJMoa1504627
45. Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, et al. Durvalumab After Chemoradiotherapy in Stage III Non-Small-Cell Lung Cancer. N Engl J Med (2017) 377(20):1919–29.
46. Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, et al. Overall Survival With Durvalumab After Chemoradiotherapy in Stage III NSCLC. N Engl J Med (2018) 379(24):2342–50. doi: 10.1056/NEJMoa1809697
47. Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Cowey CL, Lao CD, et al. Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. N Engl J Med (2015) 373(1):23–34. doi: 10.1056/NEJMoa1504030
48. Wolchok JD, Chiarion-Sileni V, Gonzalez R, Rutkowski P, Grob JJ, Cowey CL, et al. Overall Survival With Combined Nivolumab and Ipilimumab in Advanced Melanoma. N Engl J Med (2017) 377(14):1345–56. doi: 10.1056/NEJMoa1709684
49. Hodi FS, Chiarion-Sileni V, Gonzalez R, Grob JJ, Rutkowski P, Cowey CL, et al. Nivolumab Plus Ipilimumab or Nivolumab Alone Versus Ipilimumab Alone in Advanced Melanoma (CheckMate 067): 4-Year Outcomes of a Multicentre, Randomised, Phase 3 Trial. Lancet Oncol (2018) 19(11):1480–92. doi: 10.1016/S1470-2045(18)30700-9
50. Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Rutkowski P, Lao CD, et al. Five-Year Survival With Combined Nivolumab and Ipilimumab in Advanced Melanoma. N Engl J Med (2019) 381(16):1535–46. doi: 10.1056/NEJMoa1910836
51. von Itzstein MS, Lu R, Ali S, Xie D, Cai J, Xie Y, et al. Thyroid Dysfunction and Immune Checkpoint Inhibitor Outcomes. J Clin Oncol (2020) 38(15). doi: 10.1200/jco.2020.38.15_suppl.e15103
52. Kim HI, Kim M, Lee SH, Park SY, Kim YN, Kim H, et al. Development of Thyroid Dysfunction Is Associated With Clinical Response to PD-1 Blockade Treatment in Patients With Advanced Non-Small Cell Lung Cancer. Oncoimmunology (2017) 7(1):e1375642. doi: 10.1080/2162402X.2017.1375642
53. Jiang Y, Yang L, Han Y, Zhang Y, Kong F-M. Patterns of Thyroid Dysfunctions During Treatment With Immune Checkpoint Inhibitors (ICI) in 59 Solid Cancer Patients. J Clin Oncol (2020) 38(15). doi: 10.1200/jco.2020.38.15_suppl.e18567
54. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann Intern Med (2009) 151:264–69. W64. doi: 10.7326/0003-4819-151-4-200908180-00135
55. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ (2011) 343:d5928. doi: 10.1136/bmj.d5928
56. Begg CB, Mazumdar M. Operating Characteristics of a Rank Correlation Test for Publication Bias. Biometrics (1994) 50(4):1088–101. doi: 10.2307/2533446
57. Egger M, Davey Smith G, Schneider M, Minder C. Bias in Meta-Analysis Detected by a Simple, Graphical Test. BMJ (1997) 315(7109):629–34. doi: 10.1136/bmj.315.7109.629
58. Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for Assessing the Quality If Nonrandomized Studies in Meta-Analyses (2009). Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (Accessed July 6, 2012).
59. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring Inconsistency in Meta-Analyses. BMJ (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
60. DerSimonian R, Laird N. Meta-Analysis in Clinical Trials. Control Clin Trials (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
61. Liu H, Xu D, Wang W, Sun F, Zhang S, Yang X, et al. Systematic Assessment of Risk of Fever in Solid Tumor Patients Treated With PD-1/PD-L1 Inhibitors: A Systematic Review and Meta-Analysis. Front Oncol (2020) 10:570080. doi: 10.3389/fonc.2020.570080
62. Tian Y, Zhang Z, Yang X, Li D, Zhang L, Li Z, et al. The Risk Ratio of Immune-Related Colitis, Hepatitis, and Pancreatitis in Patients With Solid Tumors Caused by PD-1/PD-L1 Inhibitors: A Systematic Review and Meta-Analysis. Front Oncol (2020) 10:261. doi: 10.3389/fonc.2020.00261
63. Si Z, Zhang S, Yang X, Ding N, Xiang M, Zhu Q, et al. The Association Between the Incidence Risk of Peripheral Neuropathy and PD-1/PD-L1 Inhibitors in the Treatment for Solid Tumor Patients: A Systematic Review and Meta-Analysis. Front Oncol (2019) 9:866. doi: 10.3389/fonc.2019.00866
64. Chaker L, Bianco AC, Jonklaas J, Peeters RP. Hypothyroidism. Lancet (2017) 390(10101):1550–62. doi: 10.1016/S0140-6736(17)30703-1
65. McDermott MT. Hyperthyroidism. Ann Intern Med (2020) 172(7):ITC49–64. doi: 10.7326/AITC202004070
66. Hamburger JI. The Various Presentations of Thyroiditis. Diagn Considerations Ann Intern Med (1986) 104(2):219–24. doi: 10.7326/0003-4819-104-2-219
Keywords: thyroid dysfunction, PD-1/PD-L1 inhibitors, cancer, meta-analysis, risk
Citation: Tian Y, Li R, Liu Y, Li M, Song Y, Zheng Y, Gao A, Wen Q, Su G and Sun Y (2021) The Risk of Immune-Related Thyroid Dysfunction Induced by PD-1/PD-L1 Inhibitors in Cancer Patients: An Updated Systematic Review and Meta-Analysis. Front. Oncol. 11:667650. doi: 10.3389/fonc.2021.667650
Received: 14 February 2021; Accepted: 25 June 2021;
Published: 12 July 2021.
Edited by:
Rodabe N Amaria, University of Texas MD Anderson Cancer Center, United StatesReviewed by:
Anne Jarry, Institut National de la Santé et de la Recherche Médicale (INSERM), FranceCopyright © 2021 Tian, Li, Liu, Li, Song, Zheng, Gao, Wen, Su and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guohai Su, Z3VvaGFpc3UwNTMxQDEyNi5jb20=; Yuping Sun, MTMzNzA1ODIxODFAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.