
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol. , 13 April 2021
Sec. Surgical Oncology
Volume 11 - 2021 | https://doi.org/10.3389/fonc.2021.629582
This article is part of the Research Topic State-Of-The-Art Fluorescence Image-Guided Surgery: Current and Future Developments View all 7 articles
Background and Purpose: Pelvic tumor involving Type I + IV resections are technically challenging, along with various reconstructions methods presenting unsatisfactory outcomes and high complication rates. Since predominating studies preferred adopting pedicle screw-rod system (PRSS) to address this issue, we designed a novel three-dimensional-printed, multimodality imaging (3DMMI) based endoprosthesis with patient-specific instrument (PSI) assistance to facilitate the surgical reconstruction of pelvic tumor involving Enneking Type I + IV resection. We aimed to investigate the clinical effectiveness of this novel endoprosthesis and compare it with PRSS in Type I + IV reconstruction.
Methods: We retrospective studied 28 patients for a median follow-up of 47 months (range, 10 to 128 months) in this study with either 3D-printed endoprosthesis reconstruction (n = 10) or PRSS reconstruction (n = 18) between January 2000 and December 2017. Preoperative 3DMMI technique was used for tumor evaluation, PSI design, virtual surgery, and endoprosthesis fabrication. Clinical, oncological outcomes, functional assessments, and complications were analyzed between the two groups.
Results: Minor surgical trauma with mean operative duration of 251 ± 52.16 minutes (p = 0.034) and median intraoperative hemorrhage of 2000ml (range, 1600, 4000ml) (p = 0.032) was observed in endoprosthesis group. Wide margins were achieved in 9 patients of the endoprosthesis group compared with 10 in the PRSS group (p = 0.09). The 1993 version of the Musculoskeletal Tumor Society score (MSTS-93) was 23.9 ± 3.76 in endoprosthesis group, which was higher than PRSS group (p = 0.012). No statistical significance was found in relapse between two groups (p = 0.36). Complications were observed in two patients in endoprosthesis group compared with 12 patients in PRSS group (p = 0.046).
Conclusion: The novel design of this 3D-printed endoprosthesis, together with 3DMMI and PSI assisted, is technically accessible with favorable clinical outcomes compared with PRSS. Further study is essential to identify its long-term outcomes.
Pelvic bone tumors invading sacroiliac joint are rare, and its reconstruction after wide resection still remains one of the most technically challenging procedures (1, 2). In contrast to the anatomical characteristics of extremities, pelvic tumors with occult symptoms are frequently not diagnosed until considerable tumor size (3, 4). Wide oncological resection combined with adjuvant therapies has shown its therapeutic advantage over hindquarter amputation in terms of expected survival, local tumor control, and quality of life (5, 6). With the advancements of multi-modality fusion imaging, adjuvant therapies, and three-dimensional printing technologies, various researchers have illustrated limb preservations are feasible for selected cases (1, 2, 4, 7–9). The main concern in reconstruction is to re-establish the continuity of the pelvic girdle and prevent the subsequent collapses or rotations of residual ilium under weight-bearing conditions and retain favorable limb functions in the long term. Though various surgical reconstructions after wide resection have been proposed, complications such as infection, implant loosening, breakage, and limb length discrepancy after limb-salvage procedures, staying at a high level, cannot be ignored (7, 10–12).
Some studies have adopted 3D-printed endoprosthesis, on the strength of a single or two image modalities, to accommodate the unique defect in the reconstruction of pelvis defect after wide resection (13, 14).However, solitary modality of image has its limitations in revealing complex structures because different modality images exhibit distinctive advantages and disadvantages for revealing different anatomical structures with various purposes (15). Surgeons rely on comprehensive analysis and clinical experience to integrate different and complex imaging information to form a stereoscopic image, which is subjective among individuals and may contribute to inaccurate resection and reconstruction. 3D-multimodality image (3DMMI) has fully exploited the strengths of different imaging technologies by integrating different modality images to a single visualized 3D model with both comprehensive informativeness and precision, which has been first applied in complex neurosurgery and has yielded satisfactory outcomes but less reported in orthopedics field (16–18). Since the application of 3DMMI in the pelvic girdle reconstruction, especially in type I+IV reconstruction, are rare. Studies either focus on PRSS reconstruction (1, 4) or 3D-printed endoprosthesis reconstruction for periacetabular region invading sacroiliac joint with a single modality of the image used (8, 10, 19). The purpose of this retrospective study was to present our experience that adopting the 3DMMI technique in reconstruction of type I+IV resection and describe the clinical outcomes, as well as complications compared with PRSS reconstruction.
This is a retrospective case-control study of patients who had undergone iliosacral resection (Enneking Type I + IV) with reconstruction in our institution between January 2000 and December 2017. Data on demographics, tumor evaluations, operative duration, intraoperative hemorrhage, functional and oncological outcomes, as well as postoperative complications were collected (Table 1). The inclusion criteria for eligible participants were summarized as follows: (1) bone neoplasms classified as Enneking Type I + IV; (2) discontinuity of posterior pelvic ring after surgical resection; (3) anticipated surgical margin with a width of 20 mm for malignancies and 10mm for benign tumors as preoperatively evaluated; and (4) without major neurovascular structures involved. Exclusion criteria: patients underwent previous surgery at other institutions, recurrent tumor, pelvic neoplasms classified as any other Enneking Type, as well as hematologic malignancies were excluded from the study. To minimize surgical technique heterogeneity, all the surgeries were performed by two senior surgeons (Dr. Hong Duan and Dr. Chongqi Tu) from a single subdivision in orthopedic department
A total of 28 patients matching the study criteria were identified, of whom 18 patients received pedicle rod-screw system reconstruction (PRSS) and 10 patients were reconstructed with a novel 3D-printed endoprosthesis. There were six males and 4 females who underwent endoprosthesis reconstruction with a mean age of 32.7 years (range, 19 to 45 years). In the PRSS group, there were nine males and 9 females with a mean age of 39 years (range, 19 to 64 years). All patients diagnosed with osteosarcoma were administrated a two cycle neo-adjuvant chemotherapy (doxorubicin and cisplatin) before surgery, and another two-cycle protocol (vincristine, doxorubicin, ifosfamide, and etoposide) were applied in two patients with Ewing sarcoma. Three patients diagnosed with metastatic tumor received corresponding chemotherapy at the oncology department in our institution. Preoperative radiotherapy was not a routine procedure in our department and was only applied in patients with inadequate margin and recurrences after operation.
In this study, a complete preoperative radiological examination was administrated for a detailed evaluation of the involvements and implementation of 3DMMI. Preoperative radiography assessments including a chest computed tomography (CT) and total-skeleton technetium-99 bone scanning were performed to confirm the distal metastasis sites of bone. X-ray was performed to evaluate the general condition of the bone and define whether a bone deformity exists. Contrast-enhanced CT (SOMATOM Emotion CT scanner) and magnetic resonance imaging (MRI) (Siemens Trio Tim 3.0T MRI scanner) of the pelvis were administrated to assess the extent of involvements in bony structures and soft tissue (Figures 1A–C). Vascular involvements were evaluated by computed tomography angiography (CTA), while neural involvements were evaluated by magnetic resonance water imaging (MRWI). MRI images were mapped to CT images through affine and diffeomorphic registration algorithm, which were all implemented in open-source software named Advanced Normalization Tools (ANTS). Bony structures and nerves were segmented from CT and MRI respectively using a level-set based segmentation algorithm implemented in open-source software ITK-SNAP (20). Quality assurance and manual correction were performed after automatic segmentation (accuracy of registration >95%, maximum segmentation error <2 mm compared with the raw DICOM data). The 3DMMI of tumor model based on 3DMMI technique was then accomplished (Figures 1D, E) and then exported to stereolithographic (STL) format and opened in a workstation running Reverse Engineering (RE) software Creo Parametric 2.0 (Parametric Technology Co., USA) to identify the characteristics for the resection margin and cut plane. In this study, the minimum tumor-free margin of 20 mm in bone were regarded as sufficient as indicated by a series of studies reporting the satisfactory tumor-free margin ranging from 5 to 15 mm and 20 mm for chondrosarcoma (21–23) and osteosarcoma with sensitive response to neoadjuvant chemotherapy (24). The cut plane was then designed with a minimum 20-mm margin to the tumor with comprehensive consideration of surgical approach, tumor-free requirement, avoidance of neurovascular injury and viscera organs, feasibility to the installation of the patient-specific instrument (PSI). Virtual PSI was added to the 3DMMI model once the cut plane was defined (Figures 2A, B).
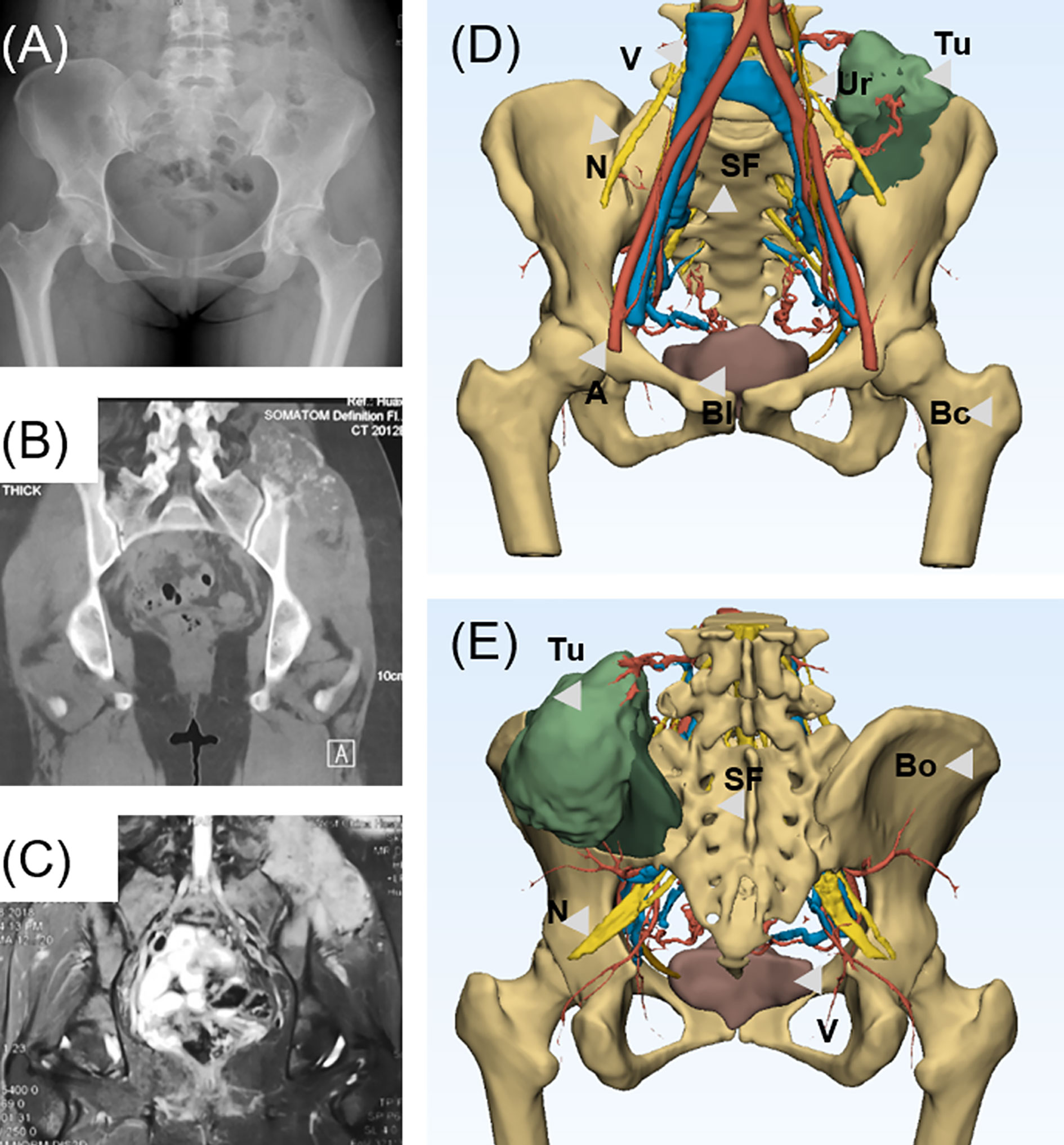
Figure 1 (A) Preoperative X-ray shows the bone destruction invading the left ilium and sacroiliac region. (B) Computed tomography shows the chondrogenic bone destruction in left sacroiliac region with soft tissue mass. (C) Magnetic resonance imaging shows an extensive soft tissue involvement invading sacroiliac region. (D) Anterior view of 3D-multimodality image of tumor model of various structures presented. (E) Posterior view of 3D-multimodality image of tumor model. 3DMMi, 3D-multimodality image; A, artery; Bl, bladder; Bo, bone; Bc, bone cortex; Ki, kidney; N, nerve; SF, sacral foramina; Tu, tumor; Ur, ureter; V, vein.
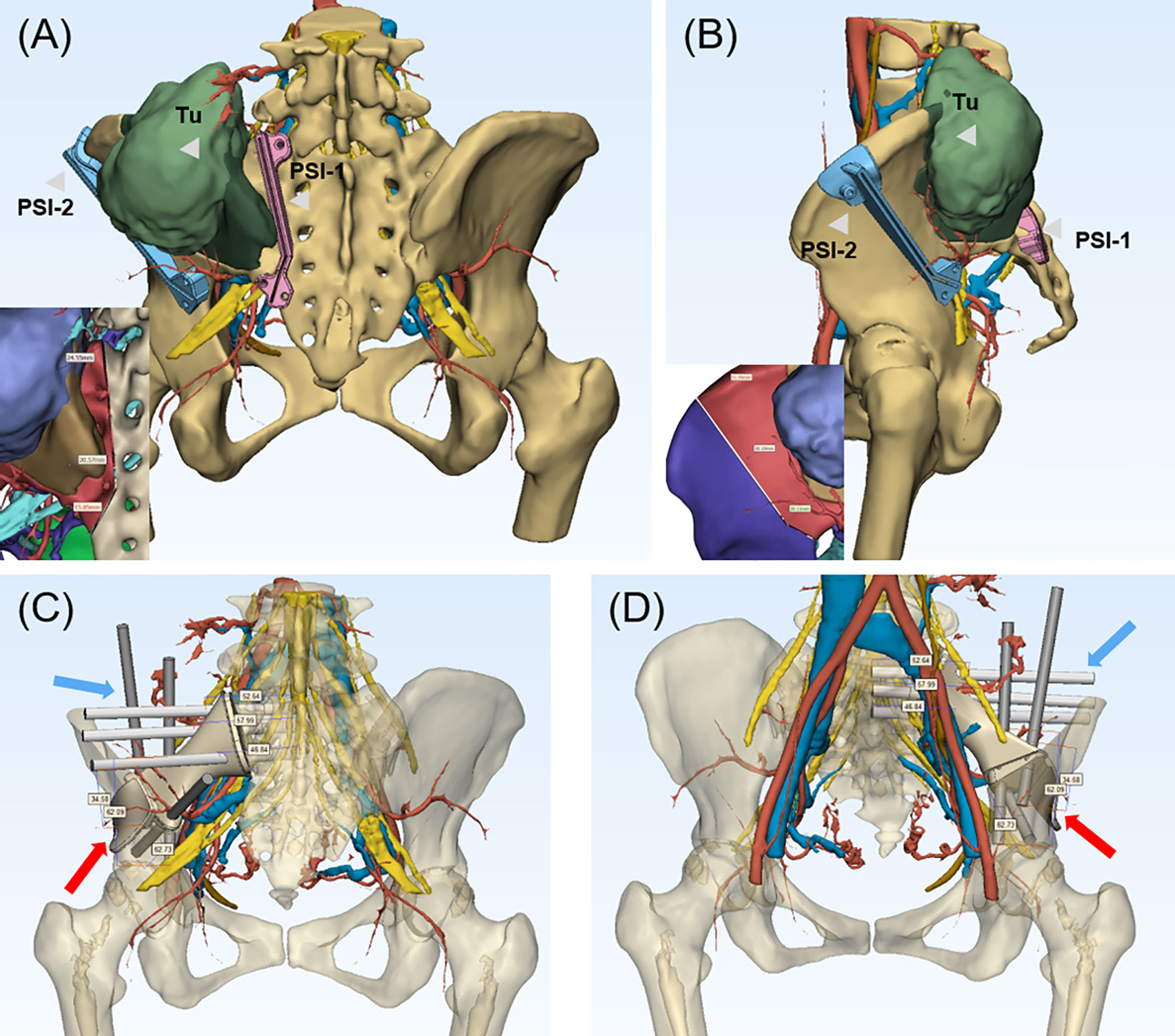
Figure 2 (A, B) 3D-multimodality image of tumor model with PSI and surgical margin designed. The PSI-1 was placed on the sacral ala adjacent to sacral foramina and PSI-2 was placed on ilium with a adequate margin designed. The neurovascular structure were clearly shown to avoid intraoperative damage. In the left bottom, the purple region represented tumor, and the brown region represented the tumor edema with details of neurovascular structures, which guaranteed the accuracy of the resection. (A) (Posterior view), (B) (Lateral view). (C, D) The endoprosthesis and screw fixation design with the length of screws shown on the 3DMMI of the patient after tumor resection. The screws in the sacral side was expected to reach the middle line of sacrum and the residual ilium was crossed fixed with the screws of the ilium side. The blue arrow indicated the screws and the red arrow indicated the endoprosthesis. PSI, patient-specific instrument; Tu, tumor.
The endoprosthesis design was then designed to match the bony defect after resection, with several screw channels on the sacral lateral and iliac lateral. The length of cancellous bone screws was required to reach or exceed the cancellous bone screw for enhanced stabilization in implant-sacrum conjunction (Figures 2C, D). On the iliac side, conjunction was achieved through a T-shaped design with crossed screw fixation. Polyaxial screw was designed for extra stabilization and intraoperative adjustments in case of unexpected failure during the surgery. Furthermore, the polyaxial screw can be either fixed to the sacroiliac joint or designed to be a PRSS connecting vertebra and ilium. Finally, a rudimentary endoprosthesis (ChunLi Co, Beijing, China) was manufactured after streamlined modification for virtual operation on the printed tumor model (Figures 3A, B).
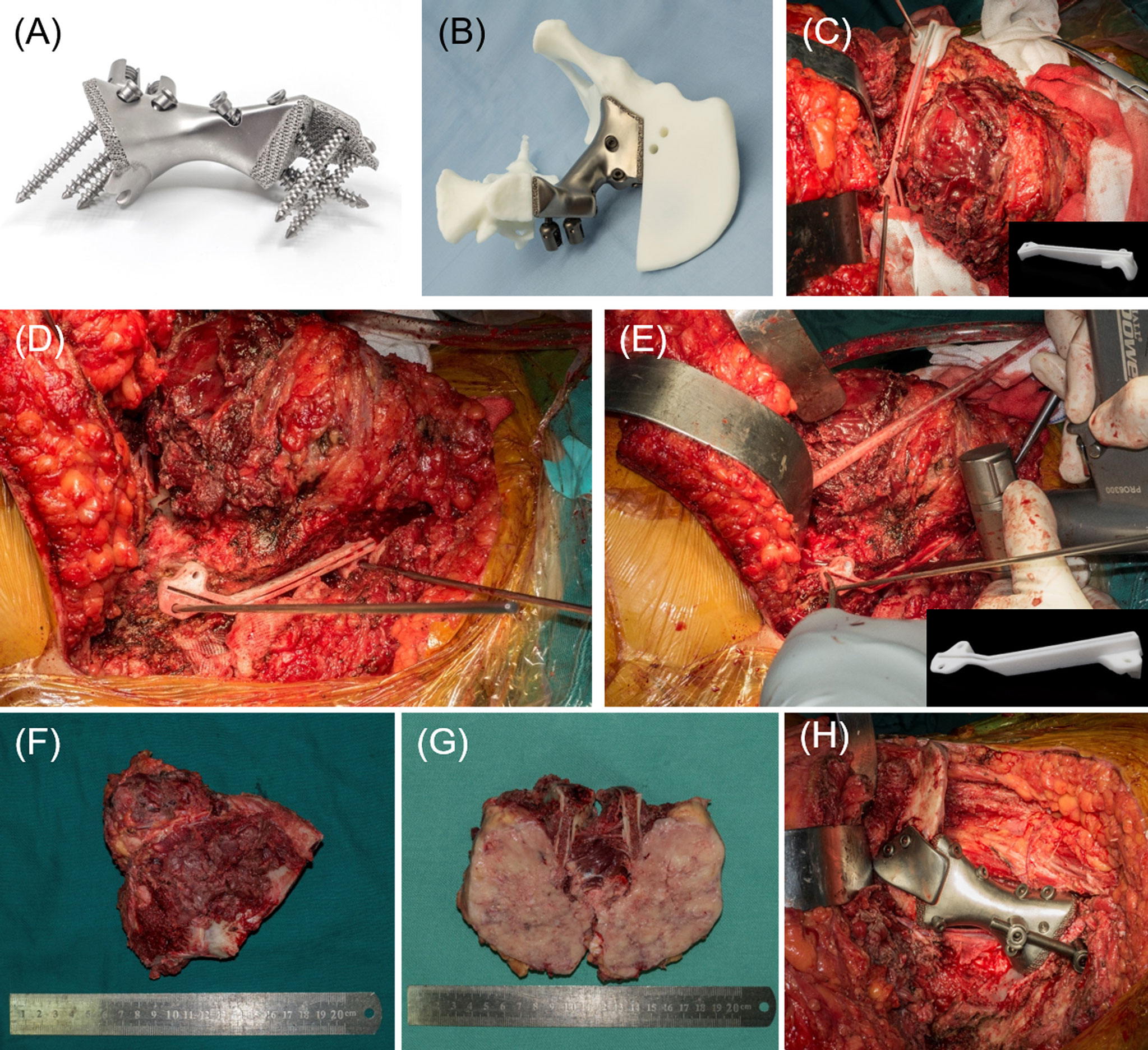
Figure 3 (A) The 3D-printed endoprosthesis with screws fixed on. Extra pedicle screw design was added in case of unsatisfactory implantation of the endoprosthesis. The contact interface of endoprosthesis-iliosacral region was modified as porous hydroxyapatite design to facilitate bone ingrowth and osseointegration. (B) The virtual surgery on printed model with 3D-printed endoprosthesis implantation. (C) The resection of the ilium side and tumor exposure with complete capsule. The PSI was fixed on the ilium with Kirschner wire. (D) The resection of the sacrum side. (E) The resection was done in a straightforward manner with swing saw through the groove designed in the PSI. (F) The resected tumor. (G) Section view of the resected tumor. (H) The endoprosthesis has been implanted precisely.
The patients were placed in a lateral position on the contralateral side for patients who underwent endoprosthesis reconstruction. A posterior iliac incision extended with a posterior longitudinal midline approach was applied as previously reported in similar resections (25, 26). On the endopelvic side, abdominal muscles were detached from the iliac crest for exposure and protection of the external iliac vessels, femoral vessels, and nerves. On exoplevic side, gluteus muscles were detached from their origins to form a myocutaneous flap with superior gluteal neurovascular structures preserved. Subsequently, the dissection was performed on the endopelvic side down to the anterior cortex of the sacrum and identify the L4/L5 roots. Then, expose on the exopelvic side of ilium to the posterior aspect of sacrum. The exposure should be complete on previously located sites of PSI for the feasibility of PSI fixation and subsequent osteotomies. The PSIs were fixed with several 2-mm Kirschner wires (Figures 3C–E) and the osteotomies were performed in a straightforward manner using a swing saw on the sites of the ilium and sacral wing. If osteotomy was required to the sacral midline, osteotome would be applied on the anterior aspect. The tumor (Figures 3F, G) could be removed after dissection of sacrotuberous and sacrospinal ligaments. Since the endoprosthesis was a unique match to the defect, the reconstruction process, which has been described in the prosthesis design section, was carried on feasibly as preoperatively designed (Figures 3H, 4A, B).
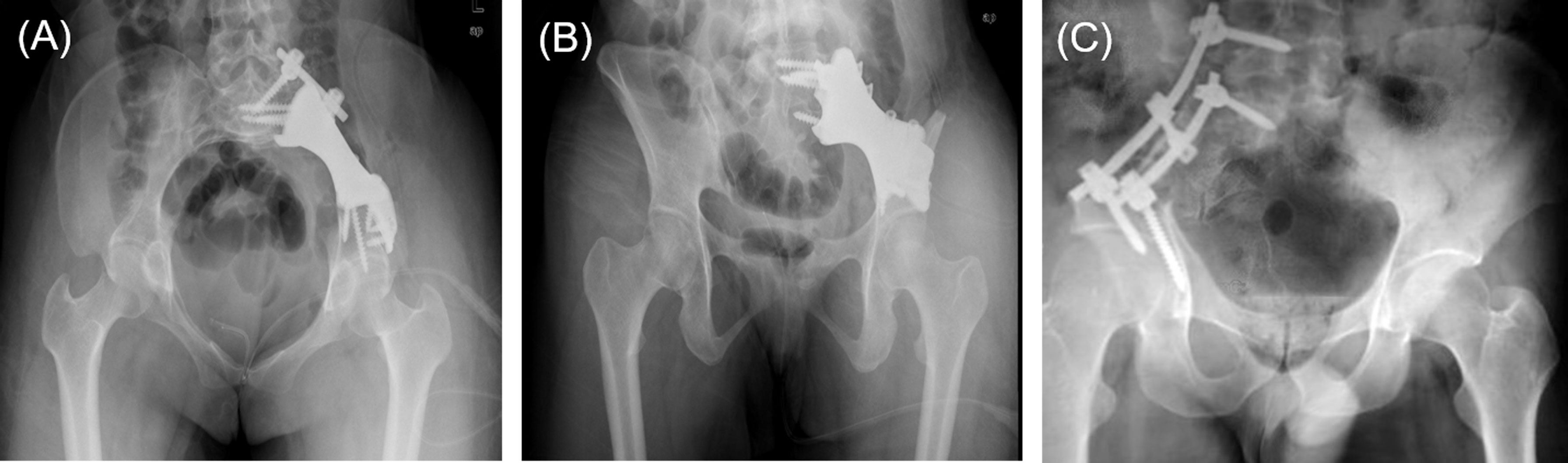
Figure 4 (A, B) Anteroposterior view of postoperative plain film of the patient underwent 3D-printed endoprosthesis. (C) An example of patient received pedicle screw-rod fixation.
The reconstruction method in PRSS (Medtronic, Inc., USA) group was performed in the same surgical approach. Two pedicle screws were implanted in the lateral side of L5 vertebral bodies and sacrum while another two screws were placed in the supraacetabular regions. Two titanium rods were used to connect the screws (Figure 4C). Technological process of how 3DMMI, PSI and endoprosthesis were implemented in this study has been presented in Video S1.
Customized lumbar pelvic hip braces were placed on all patients after surgery with the affected leg in a rotary neutral, 15° - 25°abduction, and 15°hip-flexion position. Three patients in the PRSS group presented with hemodynamic instability were admitted to the surgical intensive care unit (SICU) in our institution. The remaining patients were encouraged to early rehabilitation on the first day after surgery. Quadriceps isometric exercise and ankle flexion-extension exercises were executed during the first three days. Later on, active hip flexion not exceed 90° was executed to patents with a walking aid in the following two weeks. Partial weight-bearing was administrated since the third week and was gradually increased until normal weight-bearing status. The patients in the PRSS group started active hip flexion after 4 weeks and partial weight-bearing at 6 weeks timepoint. The adjuvant chemotherapy regimen was administrated in all patients with osteosarcoma and Ewing sarcoma. The follow-up regimen including physical examination and radiological tests were conducted monthly for the first three months and every 3 months thereafter in the first two years. After that, the follow-up was performed every 6 months. The function was evaluated by the Musculoskeletal Tumor Society (MSTS-93) score[13].
Continuous data with normal distribution were expressed as the mean ± standard deviation and data with non-normal distribution were expressed as median and range. Student’s t-test was used for continuous data with normal distribution, otherwise, Mann–Whitney U test was used. Overall survival (OS) was defined as death due to any cause. Disease-free survival (DFS) was defined as the time to relapse or death from any cause. Implant survival was defined as implant complication whether required revision or not. The OS, DFS and implant survival was analyzed with the Kaplan-Meier method. The log-rank test was used to compare the overall survival difference between the two groups. A p-value <0.05 was considered to indicate a statistically significant difference. Statistical analysis was performed with STATA 14.0 (StataCorp LLC., Texas, USA).
According to the Enneking and Dunham system (27), all patients were operated on a Type I/IV resection. Primary tumor origins and stage based on the Enneking staging system (28) were osteosarcomas in 12 patients (42.9%) with IIB, chondrosarcomas in 8 (25.8%) with IIB, Ewing sarcomas in 2 (7.1%) with IIB, giant cell tumor in 2 (7.1%) (malignant in one with IIB and benign in one with stage 3), and aneurysmal bone cyst in 1 (3.5%) with stage 3. Three patients diagnosed with metastatic cancers, which consist of pulmonary origin and renal cancer, were classified as stage III. The baseline data regarding age, gender, and adjuvant therapy in two groups showing no statistical significance. (p= 0.20, p=0.71 and p=0.68, respectively) (Table 2). The median follow-up in this study was 47 months (range, 10 to 128 months) for all patients and 28.5 months for the 3D-printed endoprosthesis group (range, 10 to 48 months) and 52 months for the PRSS group (range, 10 to 128 months). No patient lost follow-up by the time when data collected, or until the death of the patient. Adequate margins (wide margin) were biopsy-confirmed and were achieved in 9 (90.0%) patients in the endoprosthesis group and 10 patients (55.56%) in the PRSS group, which presented no statistical significance (p=0.09). We didn’t find significance regarding local recurrence rates between the endoprosthesis group (1/10, 10%) and PRSS group (6/18, 33.3%) (p=0.36). The cumulative OS was 96.4% (95% confidence interval, 77.2% to 99.5%), and 79.3% (95% confidence interval, 56.9% to 90.0%), 45.3% (95% confidence interval, 17.0% to 70.1%) at 1 year, 3 years, and 5 years, respectively for all patients. The DFS was 85.7% (95% confidence interval, 66.3% to 94.4%), and 69.5% (95% confidence interval, 47.9% to 83.6%), 43.3% (95% confidence interval, 18.7% to 66.0%) at 1 year, 3 years, and 5 years, respectively for all patients. Log-rank test for equality of overall survivor functions and disease-free survival showing no statistical significance (Figures 5A, B) (p = 0.68, p = 0.94, respectively).
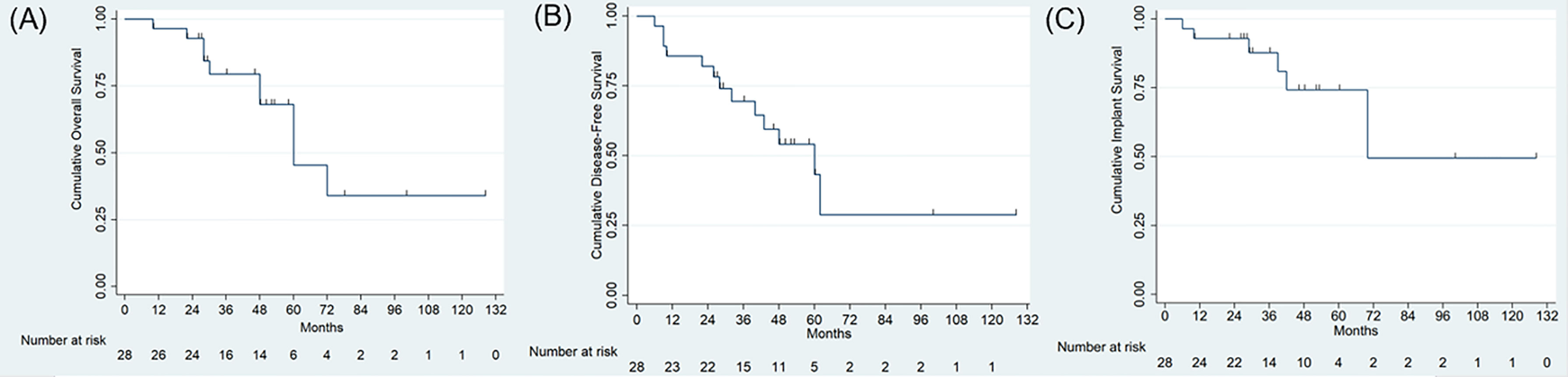
Figure 5 (A, B) Survival analysis using Kaplan-Meier curve showing the cumulative overall survival (A), and disease-free survival (B) and implant survival (C) for all patients.
We observed less intraoperative surgical trauma in patients who underwent 3D-printed endoprosthesis reconstruction evaluated by blood loss and operative time in this study. The median intraoperative hemorrhage was 3000 ml (range, 1600, 7700ml) in PRSS group, which was higher than 2000ml (range, 1600, 4000ml) in endoprosthesis group with statistical significance (p=0.032). The mean operation duration showing a statistically higher time cost of 307.78 ± 70.0 (range, 170, 430) minutes in PRSS reconstruction procedure compared with 251 ± 52.16 minutes (150, 350) in endoprosthesis group (p = 0.034).
The mean postoperative MSTS-93 score (%) at the last follow-up was 23.9 ± 3.76 (79.6%, range, 50% to 93.3%) in endoprosthesis group, compared with 19.83 ± 3.82 (66.1%, range, 33.3% to 86.7%) in PRSS group (p=0.012). Limb discrepancy was identified in four patients received endoprosthesis reconstruction and 12 in the PRSS group, which showed a significant difference of limb-length discrepancy between the endoprosthesis group (median=1.5 cm, range, 1 to 2 cm) and PRSS group (median=2.5 cm, range, 1 to 4 cm) (p=0.03). Seven of 18 patients in the PRSS group had more than 2 cm of discrepancy, while no patient with more than 2cm of discrepancy was observed in endoprosthesis group. The patient in 3DMMI group, with mildly abnormal gait, could walk and squat in a full range of motion freely without mobility assistive devices at the final follow-up (Videos S2) and (S3).
We observed 22 complications in 14 patients (50%), which presented as 20 complications in 12 patients in PRSS group compared with 2 patients in endoprosthesis group (p=0.046) (Tables 1 and 2). Wound-related problem (10/28, 35.7%) was the most frequent complication in this study. We treated these patients with dressing change, bacterial culture, and silver ion dressing (Atrauman Ag, Paul Hartmann Ag, German) and found no subsequent infection. One patient with pulmonary embolism was treated with anticoagulation therapy. Deep infection was found in 5 patients and was treated by debridement, intravenous antibiotics, and dressing change. The cumulative implant survival for PRSS group was 88.9% (95% confidence interval, 62.4% to 97.1%), and 82.1% (95% confidence interval, 53.7% to 93.9%), 67.1% (95% confidence interval, 37.5% to 85.1%) at 1 year, 3 years, and 5 years, respectively. Since no components related loosening, breakage, or implant-related revision was found in endoprosthesis group, we could not perform a log-rank test for comparison. The overall implant survival was shown in Figure 5C. Two patients (#14 and #27) with infection underwent curettage of the bony lesion in the debridement and were found subsequent implant-related complications, namely screw loosening and breakage. They presented chronic pain and walked with crutches and were treated with NSAIDs, and were closely followed without further surgical intervene. Another two patients (#2 and #8) were found screw breakages at the 24-month and 40-month follow-up. One (#2) of them was diagnosed with pulmonary metastasis with poor condition and refused further treatment. Another patient had screw breakage at residual ilium site with bursitis and received revision. Malposition of loosening rods occurred in Case 9 and Case 16 with restriction of activity and pain. They were all young patients and received revision surgery for functional demands.
Limb-sparing surgical procedure is much more challenging and demanding in the pelvis as compared with hindquarter amputation but has been proved to be associated with comparable life expectancies, relapse-free survival, and improved QOL (quality-of-life) (1, 7, 25). Due to the complex three-dimensional structures of the pelvis, especially when iliosacral regions involved, tumors are frequently related to the invasion of pelvic viscera and neurovascular structures and tend to develop into considerable sizes before confirmed, which render Type I + IV resection more difficult to achieve (1, 4, 7, 26). When the supra-acetabular region and the partial sacrum are resected, the discontinuity of the posterior pelvic girdle contributed to considerable limb shortening and decreased lumbopelvic stability if without reconstruction (19, 25). Nevertheless, few studies have presented reasonable outcomes in selected participants with no reconstruction (11, 12, 29). Currently, rare studies have unequivocally provided preferable functional outcomes with the known reconstruction methods (1, 7, 10, 25). The major concern is that practicable reconstructive modalities have not been proved to remain preferable functional outcomes and are related to various complications regarding mechanical failures and deep infections (7, 25, 30). To address the current issues, we adopted 3DMMI techniques with Patient-Specific Instruments (PSI) and customized 3D printed endoprosthesis, which allows surgeons to precisely resect the involved pelvis, restore integrity between the sacrum and the ilium and retain the acceptable functional outcomes.
Since the massive musculoskeletal resections are frequently mandatory for iliosacral tumors, it is still under debate whether the unstable pelvic girdle defects should be reconstructed (11, 12, 29). Beadel et al. (12) reported a retrospective case-control study with 16 patients who underwent Type I + IV resections involved, of which 12 patients received no reconstruction. In their study, shorter operative duration, minor hemorrhage, and fewer complications were observed in patients without reconstruction with functional evaluation showing no statistical difference in the two groups. In their updated retrospective observational study (29), 32 patients who underwent Type I or Type I/IV resections without reconstruction were enrolled with a mean MSTS-93 score of 67.3% and a 3% local recurrence rate. However, the complications were observed in 17 patients with 40.6% (13 of 32 patients) wound-related complications. They have achieved favorable oncological outcomes with adequate margins, which may indicate that more structures must be removed as they stated ‘aggressive resections’. If excessive resection without reconstruction, especially in the sacrum, the insufficient vascularized tissues with a large residual cavity may contribute to the infection (7). The main concept they prefer no reconstruction is that iliosacral defect induces the medialization of the hip joint center, accompanied with decreased body-weight moment exerting on a shorter abductor lever arm, which leads to an improved single-leg gait (12, 29). Nevertheless, the limb function is at the cost of the loss of lumbopelvic stability and integrity of pelvic ring. Besides, several studies have reported that sacroiliac arthrodesis contributes to progressive scoliosis and flail hips with considerable limb shortening (5, 7, 31). Wang et al. (32) reported a contrasting view that the functional outcomes of 12 patients with autograft and plate or pedicle screw fixation were superior to 12 cases without reconstruction, and the minor limb-length discrepancy was also defined in the reconstruction group. In the current study, we found no patient with more than 2cm limb discrepancy in endoprosthesis group, which leads us to believe that the lumbopelvic stability and pelvic girdle integrity should be restored with comparable results after Type I/IV resection.
The precision of resection with safe margins has a substantial impact on the oncological outcomes with regard to local relapse and patient survival. Peripheral regions of tumor are abundant with blood supply, which means resection process with positive margin is associated with a higher amount of hemorrhage and longer intraoperative duration. The results in our study have shown a minor surgical trauma in the prosthesis group with mean blood loss of 2270 ml (1600, 4000 ml) and mean operation time of 251 minutes (range, 150 to 350 minutes) which was comparable to the results of other studies ranging from 3153 to 5600ml and 256 minutes to 5.27 hours in similar resections regardless whether reconstruction performed or not (10–12, 26, 32, 33). Adequate surgical margins are particularly difficult to achieve when the sacroiliac joint is invaded (34) because substantial tumor size is frequently combined with extracompartmental feature, and occasionally responsible for distant tumor thrombi in the Baston plexus (31). Thus, 3D-printed endoprosthesis, characterized with individual design to fit the defects and improved accuracy of resection, is gaining growing popularities for precise resection purposes. However, most published literature presented their application of 3D-printed endoprosthesis based on one or two modalities of radiography with extremely limited structures merged into a 3D model (8, 13, 19, 35). Besides, the lack of PSI may lead to higher demands of surgical skills because inaccuracy resection wound make this technically difficult procedure even harder to perform (19). In this study, the cost for 3DMMI design was ¥3,000 to ¥5,000 and for PSI manufacture and 3D-printed endoprosthesis was ¥800 and ¥50,000, respectively, which is cost efficient when compared with the cost ranging from ¥50,000 to ¥60,000 in PRSS.
Although endoprosthesis group showed better outcomes than PRSS group regarding margin status, local relapse, we did not find a statistical difference between the two groups. The current study presenting an overall recurrence rate of 10% in the 3DMMI group with a wide margin rate of 90% is superior in resection of similar studies (Table 3). The reasons may be as follows. First, multiple modalities (CT, CTA, MRI, and MRWI) can be utilized and more details of the tumor can be presented, resulting in improved preoperative imaging assessments for the following resection and reconstruction. Unlike the most frequently used 3D printed endoprosthesis, designed and manufactured on the basis of a single modality of image mainly depends on bony structure (three-dimensional CT scan of the pelvis, design in Mimics), our 3DMMI technique implementing the algorithm in symmetric diffeomorphic and growcut manner, regionalization-adaptive registration, nD morphological contour interpolation, and Gaussian smoothing (18). Second, the application of PSI based on 3DMMI was precisely designed to be fixed in the tumor-free anatomic regions guarantees the reliability of the margin and accuracy. Due to the irregular shape of the pelvis and heterogeneity of the individuals, each PSI was unique and customized, which can only be fixed on the previously designated site. Third, the resection process was done in a straight-forward manner with time saved. PSI was firmly fixed on with K-wires and was designed with a groove. Osteotomy can easily be performed using a swing saw through the groove, which can prevent insufficient or excessive resection. Fourth, the preoperative virtual operation was performed, on the 3D-printed pelvis model with a customized endoprosthesis. Thus, we can test modify the design and operation plan to minimize the possible error and risk before surgery.
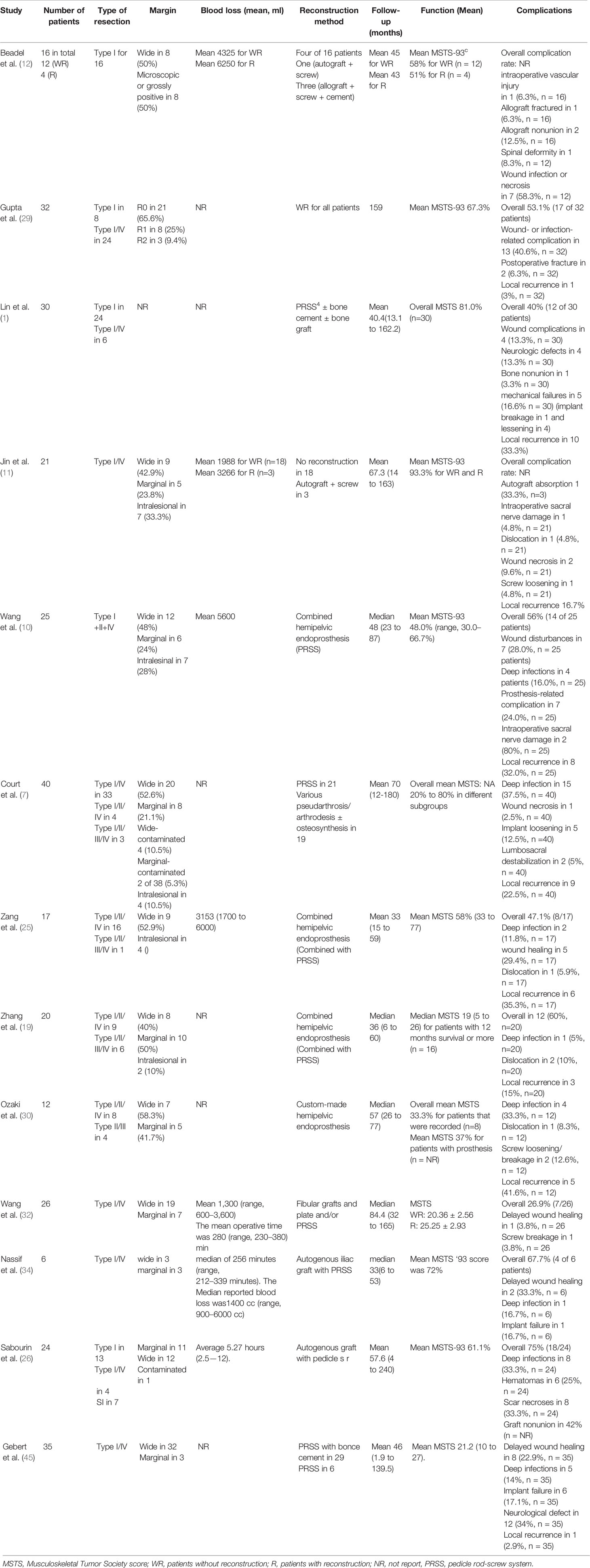
Table 3 A review of previous studies on sacroiliac resection and reconstruction, the margin, blood loss, proportion of patients with complications, and functional outcomes.
Among the existing reconstruction methods, we prefer to adopt endoprosthesis reconstruction of pelvic girdle for its mechanical superiority of transferring weight-bearing force from the lumbar spine to hip and limb via sacroiliac joint. In this study, the conjunction between the prosthesis and residual sacrum was enhanced by enlarged implant-sacrum contact surface and more screw fixation compared with similar studies (8, 19, 25). The contact of implant-sacrum was anatomic match with three screws perpendicularly fixed and one extra rod-screw fixation perpendicular to sacroiliac joint, while the interface of implant-ilium was strengthened by an ‘L’ shaped design with crossed screws fixed. The polyaxial screw design can be either directly fixed or adjusted for a rod-screw fixation purpose. The advantage of this design lies in transferring the shear stress to compression stress in the stress conduction (35). Pedicle screw and rod systems were favored predominantly in many studies. In this type of reconstruction, stress mainly concentrated on both ends of the connecting rods in the supraacetabular region, and on the pedicle bodies of L4/L5 or residual sacrum, which is vulnerable to torsional force (36, 37). Hence, some studies recommended a compound rod and screw system with bone grafts for improved lumbopelvic stability (1, 19, 32, 37). However, problems remain for bone healing, graft fracture, and infections (1, 7, 26, 32). Allografts have been widely recognized with high infection risks (1, 30), whereas autografts are limited by donor site morbidities and extra operations (1, 33). Despite the superiorities of autograft, Sabourin et al. reported poor functional outcomes and a graft nonunion rate of 42% using polyaxial screws and titanium rods in 24 patients who underwent autogenous graft with pedicle screw-rod system fixation (26).
Endoprosthesis reconstructions presented various functional performance according to types of resection and reconstruction, which include allograft/prosthesis composite (38), modular hemipelvic endoprosthesis (39, 40), modular saddle prosthesis (41), and custom-made hemipelvic endoprosthesis (19, 25, 42) (Table 3). Combined pedicle-hemipelvic endoprosthesis, the most frequently applied method in treating pelvis tumors invading sacroiliac joint, of which the mean MSTS score ranging from 48% to 63% (8, 10, 19, 25). These prostheses were pedicle-hemipelvic design with connecting rods fixed on the acetabular components and L4/L5 vertebra (8, 10, 25). The similar problems confronting the connecting rods with peak prosthetic stress at the conjunction regions (10, 37), as Wang et al. highlighted in their continuous studies (8, 10). Zhang et al. reported high complications concerning pedicle screw-rod failures, and prosthetic dislocation in their previous study (25) and improve the prosthesis design with enhanced stabilization by extra fixation to the residual sacrum (19). These pedicle-hemipelvic prostheses emphasized the fixation should be embedded in bone cement, thus enhanced stabilization can be retained. However, bone cement is well compression-resistant but vulnerable to torsion, as proved by the high failure rates of screw-rod with bone cement enhancement (19). Since studies specifically focused on this anatomic region are rare, it is difficult to make between-approach comparisons with other endoprosthesis. However, our endoprosthesis showing a mean MSTS-93 score of 23.9 (79.7%) was favorable in the Type I + IV resections. Apart from the mechanical limitations of stress concentration of connecting rods and screws, the sacroiliac joint is characterized with physiological micromotion and hip movements induce rotation in the supraacetabular region (43). This type of enhancements may yield initial stability rather than long-term benefits. Our implant failure of 33.3% in PRSS group may also support the above statements. The fixation of rod-screw on L5 or L4/5 may be another potential risk for decreased implant stability. Lin et al. conducted a study with various types of pedicle rod-screw fixations and found that extrapelvic fixation in L4/5 was less stable than intrapelvic fixation in residual sacrum (1). The study recommends intrapelvic fixation if possible, because micromotions between intervertebral discs may contribute to increased stress level (8) and further fatigue broken or loosening of implant (1).
Other complications that are mainly focused on wound-related disturbances and deep infections were the most frequent complications in this study, as widely recognized (7, 25, 29, 35). We found two delayed unions (20%) and no deep infection in the endoprosthesis group, compared with 44.4% and 27.8% in PRSS group. Apart from inherent potential risks that sacrum adjacent to rectum, presacral venous hemorrhage, and undermined tissue regeneration caused by neoadjuvant therapy, the prolonged operative duration, increased blood loss and insufficient soft tissue coverage may also contribute to the infection and wound union (9, 44). Minor surgical trauma is difficult to achieve by conventional freehand surgical techniques that reported deep infection rate ranging from 11.8% to 37.5% (7, 10, 25, 26, 33, 34, 45). However, we minimized the chances of infection in a few aspects. On the one hand, the size and shape of endoprosthesis volume are not necessary to be the same as the bone defect. Decreased volume design of endoprosthesis that maintain the biomechanics contributes to better soft-tissue coverage. On the other hand, PSI based on 3DMMI allows the surgeon to perform planned resections, which diminish unnecessary surgical manipulations (9, 14, 46). Hence, we think patients may benefit from a well-designed implant with 3DMMI-based preoperative evaluation, which yields decreased infection in this study.
Though we presented encouraging clinical outcomes in patients with endoprosthesis reconstruction in Type I/IV resections, this study had a few limitations. First, the present study was retrospective in nature and was limited by its small sample enrolled. However, studies focused on Type I/IV resection are few (4) and mainly included Type I resection without a control group. Hence, the clinical outcomes may be comparable and able to justify the application of the novel prosthesis design. Second, the follow-up was not long enough to detect major complications, especially implant-related complications in the endoprosthesis group. Since the contact surface of endoprosthesis was highly porous surface design mimicking bone trabecula structure, we think a mean follow-up of 30.1 months (endoprosthesis group) in a group with a limited lifespan may be sufficient to report its early implant function, as the similar design has proved its long-term stability (19, 44). Third, tumor heterogeneity exists in this study. Despite we included benign tumors, the main purpose of this study was to evaluate the performance of resection and reconstruction adopting this novel design with 3DMMI and PSI. And the baseline data were comparable between groups. To date, this may be the first study reporting specific Type I/IV resections reconstructed with 3D-printed endoprosthesis assisted by 3DMMI and PSI.
In conclusion, the novel design of this 3D-printed endoprosthesis, together with 3DMMI and PSI assisted, are technically accessible with relatively minor trauma and better implant stability in facilitating Type I/IV resections compared with PRSS. It must be noted that long-term follow-up is essential to validate its capacity.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Medical Ethics Committee of West China Hospital, Sichuan University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Study Design: HD. Data Collection: ZY and WZ. Methodology: ZY, XF, and CT. Written Work: ZY and WZ. Review and Revision: HD and WZ. Visualization: HD and WZ. Resource: HD and CT. Project Administration: HD and CT. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2021.629582/full#supplementary-material
Supplementary Video S1 | The video shows the flow in the current study including how three-dimensional multimodality imaging (3DMMI) works and the implantation of 3D-printed endoprosthesis.
Supplementary Videos S2 and S3 | The patient, with mildly abnormal gait, could walk and squat in a full range of motion freely without mobility assistive devices at the final follow-up.
1. Lin P, Shao Y, Lu H, Zhang Z, Lin H, Wang S, et al. Pelvic reconstruction with different rod-screw systems following Enneking type I/I + IV resection: a clinical study. Oncotarget (2017) 8:38978–89. doi: 10.18632/oncotarget.17164
2. Wei R, Guo W, Yang R, Tang X, Yang Y, Ji T, et al. Reconstruction of the pelvic ring after total en bloc sacrectomy using a 3D-printed sacral endoprosthesis with re-establishment of spinopelvic stability. Bone Joint J (2019) 101:9. doi: 10.1302/0301-620X.101B7.BJJ-2018-1010.R2
3. Li D, Guo W, Tang X, Yang R, Tang S, Qu H, et al. Preservation of the contralateral sacral nerves during hemisacrectomy for sacral malignancies. Eur Spine J (2014) 23:1933–9. doi: 10.1007/s00586-013-3136-3
4. Xu M, Zheng K, Zhao J, Bai W, Yu X. En Bloc Resection and Pelvic Ring Reconstruction for Primary Malignant Bone Tumors Involving Sacroiliac Joint. Orthop Surg (2019) 11:1120–6. doi: 10.1111/os.12563
5. Kollender Y, Shabat S, Bickels J, Flusser G, Isakov J, Neuman Y, et al. Internal hemipelvectomy for bone sarcomas in children and young adults: surgical considerations. Eur J Surg Oncol (2000) 26:398–404. doi: 10.1053/ejso.1999.0906
6. Sucato DJ, Rougraff B, Mcgrath BE, Sizinski J, Mindell ER. Ewing’s sarcoma of the pelvis. Long-term survival and functional outcome. Clin Orthop Relat Res (2000) 373:193–201. doi: 10.1097/00003086-200004000-00023
7. Court C, Bosca L, Cesne AL, Nordin JY, Missenard G. Surgical Excision of Bone Sarcomas Involving the Sacroiliac Joint. Clin Orthop Relat Res (2006) 451:189–94. doi: 10.1097/01.blo.0000229279.58947.91
8. Wang B, Sun P, Xie X, Wu W, Tu J, Ouyang J, et al. A novel combined hemipelvic endoprosthesis for peri-acetabular tumours involving sacroiliac joint: a finite element study. Int Orthop (SICOT) (2015) 39:2253–9. doi: 10.1007/s00264-015-2891-7
9. Cartiaux O, Paul L, Francq BG, Banse X, Docquier P-L. Improved Accuracy with 3D Planning and Patient-Specific Instruments During Simulated Pelvic Bone Tumor Surgery. Ann BioMed Eng (2014) 42:205–13. doi: 10.1007/s10439-013-0890-7
10. Wang B, Zou C, Hu X, Tu J, Yao H, Yin J, et al. Reconstruction with a novel combined hemipelvic endoprosthesis after resection of periacetabular tumors involving the sacroiliac joint: a report of 25 consecutive cases. BMC Cancer (2019) 19:861. doi: 10.1186/s12885-019-6049-7
11. Jin T, Liu W, Xu H, Li Y, Hao L, Niu X. How does iliosacral bone tumor resection without reconstruction affect the ipsilateral hip joint? BMC Musculoskelet Disord (2018) 19:102. doi: 10.1186/s12891-018-2023-9
12. Beadel GP, McLaughlin CE, Aljassir F, Turcotte RE, Isler MH, Ferguson P, et al. Iliosacral Resection for Primary Bone Tumors: Is Pelvic Reconstruction Necessary? Clin Orthop Relat Res (2005) NA:22–9. doi: 10.1097/01.blo.0000180046.97466.bc
13. Ji T, Yang Y, Tang X, Liang H, Yan T, Yang R, et al. 3D-Printed Modular Hemipelvic Endoprosthetic Reconstruction Following Periacetabular Tumor Resection: Early Results of 80 Consecutive Cases. J Bone Joint Surg (2020) 1530–41. doi: 10.2106/JBJS.19.01437
14. Jentzsch T, Vlachopoulos L, Fürnstahl P, Müller DA, Fuchs B. Tumor resection at the pelvis using three-dimensional planning and patient-specific instruments: a case series. World J Surg Onc (2016) 14:249. doi: 10.1186/s12957-016-1006-2
15. Nomikos GC, Murphey MD, Kransdorf MJ, Bancroft LW, Peterson JJ. Primary bone tumors of the lower extremities. Radiol Clin North Am (2002) 40:971–90. doi: 10.1016/s0033-8389(02)00038-6
16. Murphy MA, O’Brien TJ, Morris K, Cook MJ. Multimodality image-guided surgery for the treatment of medically refractory epilepsy. J Neurosurg (2004) 100:452–62. doi: 10.3171/jns.2004.100.3.0452
17. Nowell M, Rodionov R, Zombori G, Sparks R, Winston G, Kinghorn J, et al. Utility of 3D multimodality imaging in the implantation of intracranial electrodes in epilepsy. Epilepsia (2015) 56:403–13. doi: 10.1111/epi.12924
18. Cao X, Yang J, Gao Y, Wang Q, Shen D. Region-adaptive Deformable Registration of CT/MRI Pelvic Images via Learning-based Image Synthesis. IEEE Trans Image Process (2018) 3500–12. doi: 10.1109/TIP.2018.2820424
19. Zhang Y, Tang X, Ji T, Yan T, Yang R, Yang Y, et al. Is a Modular Pedicle-hemipelvic Endoprosthesis Durable at Short Term in Patients Undergoing Enneking Type I + II Tumor Resections With or Without Sacroiliac Involvement? Clin Orthop Relat Res (2018) 476:1751–61. doi: 10.1007/s11999.0000000000000121
20. Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC, et al. User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage (2006) 31:1116–28. doi: 10.1016/j.neuroimage.2006.01.015
21. Wong KC, Kumta SM, Geel NV, Demol J. One-step reconstruction with a 3D-printed, biomechanically evaluated custom implant after complex pelvic tumor resection. Comput Aided Surg (2015) 20:14–23. doi: 10.3109/10929088.2015.1076039
22. Nandra R, Matharu G, Stevenson J, Parry M, Grimer R, Jeys L. Long-term outcomes after an initial experience of computer-navigated resection of primary pelvic and sacral bone tumours: soft-tissue margins must be adequate to reduce local recurrences. Bone Joint J (2019) 101-B:484–90. doi: 10.1302/0301-620X.101B4.BJJ-2018-0981.R1
23. Zhang Y, Guo W, Tang X, Yang R, Ji T, Yang Y, et al. En bloc resection of pelvic sarcomas with sacral invasion: a classification of surgical approaches and outcomes. Bone Joint J (2018) 100-B:798–805. doi: 10.1302/0301-620X.100B6.BJJ-2017-1212.R1
24. Kawaguchi N, Ahmed AR, Matsumoto S, Manabe J, Matsushita Y. The concept of curative margin in surgery for bone and soft tissue sarcoma. Clin Orthop Relat Res (2004) 419:165–72. doi: 10.1097/00003086-200402000-00027
25. Zang J, Guo W, Yang Y, Xie L. Reconstruction of the hemipelvis with a modular prosthesis after resection of a primary malignant peri-acetabular tumour involving the sacroiliac joint. Bone Joint J (2014) 96-B:399–405. doi: 10.1302/0301-620X.96B3.32387
26. Sabourin M, Biau D, Babinet A, Dumaine V, Tomeno B, Anract P. Surgical management of pelvic primary bone tumors involving the sacroiliac joint. Orthop Traumatol: Surg Res (2009) 95:284–92. doi: 10.1016/j.otsr.2009.04.008
27. Enneking WF, Dunham WK. Resection and reconstruction for primary neoplasms involving the innominate bone. J Bone Joint Surg Am (1978) 60:731–46. doi: 10.2106/00004623-197860060-00002
28. Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res (1980) 153:106–20. doi: 10.1097/00003086-198011000-00013
29. Gupta S, Griffin AM, Gundle K, Kafchinski L, Zarnett O, Ferguson PC, et al. Long-term outcome of iliosacral resection without reconstruction for primary bone tumours. Bone Joint J (2020) 102-B:779–87. doi: 10.1302/0301-620X.102B6.BJJ-2020-0004
30. Ozaki T, Hoffmann C, Hillmann A, Gosheger G, Lindner N, Winkelmann W. Implantation of Hemipelvic Prosthesis After Resection of Sarcoma. Clin Orthop Relat Res (2002) 396:197–205. doi: 10.1097/00003086-200203000-00030
31. Wirbel RJ, Schulte M, Mutschler WE. Surgical treatment of pelvic sarcomas: oncologic and functional outcome. Clin Orthop Relat Res (2001) 390:190–205. doi: 10.1097/00003086-200109000-00022
32. Wang J, Tang Q, Xie X, Yin J, Zhao Z, Li Z, et al. Iliosacral Resections of Pelvic Malignant Tumors and Reconstruction with Nonvascular Bilateral Fibular Autografts. Ann Surg Oncol (2012) 19:4043–51. doi: 10.1245/s10434-012-2339-x
33. Nassif NA, Buchowski JM, Osterman K, McDonald DJ. Surgical Technique: Iliosacral Reconstruction With Minimal Spinal Instrumentation. Clin Orthop Relat Res (2013) 471:947–55. doi: 10.1007/s11999-012-2643-6
34. Ozaki T, Flege S, Kevric M, Lindner N, Maas R, Delling G, et al. Osteosarcoma of the pelvis: experience of the Cooperative Osteosarcoma Study Group. J Clin Oncol (2003) 21:334–41. doi: 10.1200/JCO.2003.01.142
35. Dai K-R, Yan M-N, Zhu Z-A, Sun Y-H. Computer-Aided Custom-Made Hemipelvic Prosthesis Used in Extensive Pelvic Lesions. J Arthroplasty (2007) 22:981–6. doi: 10.1016/j.arth.2007.05.002
36. Jia Y, Cheng L, Yu G, Du C, Yang Z, Yu Y, et al. A finite element analysis of the pelvic reconstruction using fibular transplantation fixed with four different rod-screw systems after type I resection. Chin Med J (Engl) (2008) 121:321–6. doi: 10.1097/00029330-200802020-00008
37. Wu T, Ren X, Cui Y, Cheng X, Peng S, Hou Z, et al. Biomechanical study of three kinds of internal fixation for the treatment of sacroiliac joint disruption using biomechanical test and finite element analysis. J Orthop Surg Res (2018) 13:152. doi: 10.1186/s13018-018-0858-2
38. Schwameis E, Dominkus M, Krepler P, Dorotka R, Lang S, Windhager R, et al. Reconstruction of the pelvis after tumor resection in children and adolescents. Clin Orthop Relat Res (2002) 402:220–35. doi: 10.1097/00003086-200209000-00022
39. Tang X, Guo W, Ji T. Reconstruction with modular hemipelvic prosthesis for the resection of solitary periacetabular metastasis. Arch Orthop Trauma Surg (2011) 131:1609–15. doi: 10.1007/s00402-011-1359-5
40. Zhou Y, Duan H, Liu Y, Min L, Kong Q, Tu C. Outcome after pelvic sarcoma resection and reconstruction with a modular hemipelvic prostheses. Int Orthop (SICOT) (2011) 35:1839–46. doi: 10.1007/s00264-011-1222-x
41. Aljassir F, Beadel GP, Turcotte RE, Griffin AM, Bell RS, Wunder JS, et al. Outcome after pelvic sarcoma resection reconstructed with saddle prosthesis. Clin Orthop Relat Res (2005) 438:36–41. doi: 10.1097/00003086-200509000-00009
42. Barrientos-Ruiz I, Ortiz-Cruz EJ, Peleteiro-Pensado M. Reconstruction After Hemipelvectomy With the Ice-Cream Cone Prosthesis: What Are the Short-term Clinical Results? Clin Orthop Relat Res (2017) 475:735–41. doi: 10.1007/s11999-016-4747-x
43. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3512279/ (Accessed September 2, 2020).
44. Wang J, Min L, Lu M, Zhang Y, Wang Y, Luo Y, et al. What are the Complications of Three-dimensionally Printed, Custom-made, Integrative Hemipelvic Endoprostheses in Patients with Primary Malignancies Involving the Acetabulum, and What is the Function of These Patients? Clin Orthop Relat Res (2020) 478:2487–501. doi: 10.1097/CORR.0000000000001297
45. Gebert C, Wessling M, Gosheger G, Aach M, Streitbürger A, Henrichs MP, et al. Pelvic reconstruction with compound osteosynthesis following hemipelvectomy: A clinical study. Bone Joint J (2013) 95-B:1410–6. doi: 10.1302/0301-620X.95B10.31123
Keywords: Sacroiliac joint, pelvic tumor, hemipelvic reconstruction, pedicle screw-rod system, 3D-printed endoprosthesis
Citation: Yu Z, Zhang W, Fang X, Tu C and Duan H (2021) Pelvic Reconstruction With a Novel Three-Dimensional-Printed, Multimodality Imaging Based Endoprosthesis Following Enneking Type I + IV Resection. Front. Oncol. 11:629582. doi: 10.3389/fonc.2021.629582
Received: 15 November 2020; Accepted: 18 March 2021;
Published: 13 April 2021.
Edited by:
Tomoharu Sugie, Kansai Medical University Hospital, JapanReviewed by:
Stefano Restaino, Ospedale Santa Maria della Misericordia di Udine, ItalyCopyright © 2021 Yu, Zhang, Fang, Tu and Duan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hong Duan, ZHVhbmhvbmcxOTcwQDEyNi5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.