- 1Department of Gastric Surgery, Fujian Medical University Union Hospital, Fuzhou, China
- 2Department of General Surgery, Fujian Medical University Union Hospital, Fuzhou, China
- 3Key Laboratory of Ministry of Education of Gastrointestinal Cancer, Fujian Medical University, Fuzhou, China
- 4Fujian Key Laboratory of Tumor Microbiology, Fujian Medical University, Fuzhou, China
- 5Section of Hepatobiliary and Pancreatic Surgery, Division of Subspecialty General Surgery, Department of Surgery, Mayo Clinic, Rochester, MN, United States
Objective: To validate the prognostic value of tumor regression grading (TRG) and to explore the associated factors of TRG for advanced gastric cancer (AGC) with neoadjuvant chemotherapy (NACT) plus surgery.
Methods: Two hundred forty-nine AGC patients treated with NACT followed by gastrectomy at the Mayo Clinic, USA and the Fujian Medical University Union Hospital, China between January 2000 and December 2016 were enrolled in this study. Cox regression was used to identify covariates associated with overall survival (OS) and recurrence-free survival (RFS). Logistic regression was used to reveal factors predicting tumor regression grading.
Results: For patients with TRG 0-1, the 3- and 5-year OS rates were 85.2% and 74.5%, respectively, when compared to 56.1% and 44.1% in patients with TRG 2 and 28.2% and 23.0% in patients with TRG 3, respectively (p<0.001). TRGs were independent risk factors for OS. Similar findings were observed in RFS. Multivariable analysis revealed that an oxaliplatin-based regimen (p=0.017) was an independent predictor of TRG. The oxaliplatin-based regimen was superior to the nonoxaliplatin-based regimen for OS (38.4 months vs 19.5 months, respectively; p=0.01). Subgroup analyses by histological subtype indicated that the oxaliplatin-based regimen improved the OS in nonsignet ring cell carcinoma compared to the nonoxaliplatin-based regimen (53.7 months vs 19.5 months, respectively; p=0.011). However, similar findings were not observed in RFS.
Conclusion: TRG was an independent factor of AGC treated with neoadjuvant chemotherapy plus surgery. Oxaliplatin-based neoadjuvant chemotherapy regimens improve tumor response and may have an overall survival benefit for patients with nonsignet ring cell carcinoma.
Introduction
Gastric cancer is a leading cause of cancer-related mortality worldwide, with approximately 951,600 new cases diagnosed and 723,100 patients who succumb to the disease annually (1). The use of neoadjuvant chemotherapy in the treatment of patients with localized advanced gastric cancer has become more prevalent over the past ten years. Several advantages have been associated with this approach, including downgrading of the tumor, increasing the likelihood of achieving an R0 resection, and eradicating micrometastasis to reduce recurrence (2, 3). Neoadjuvant chemotherapy followed by gastrectomy could provide significant overall survival (OS) benefits over surgery alone (4).
Tumor regression grade (TRG) is a descriptive measurement defined as a histological response to neoadjuvant therapy and has shown prognostic value for digestive system tumors (5, 6). In 2003, TRG was first used by Becker et al. to evaluate the histological response in gastric cancer (7). TRG has been reported to be a predictor of survival in patients with gastric cancer in several studies (8, 9). A good tumor response rate significantly improved the OS and recurrence-free survival (RFS) (10). However, the factors associated with a better tumor response rate and an optimal neoadjuvant chemotherapy regimen that improved survival are uncertain.
Therefore, we investigated the role of TRG in neoadjuvant chemotherapy for gastric cancer and analyzed the factors affecting TRG to reveal the potential survival benefits of neoadjuvant chemotherapy for patients.
Methods
Patient Selection
Patients diagnosed with advanced clinical stage gastric cancer (more than clinical T2 category or clinical stage N1) were enrolled in this study. The exclusion criteria were as follows: multiple primary gastric cancer tumors, gastric cancer combined with other malignancies, history of radiotherapy or radiochemotherapy, types I and II esophagogastric junction tumors, and patients without tumor resection. Ultimately, a total of 249 patients were analyzed. Of these patients, 131 patients were submitted from the Fujian Medical University Union Hospital, and 118 patients were from the Mayo Clinic. Tumor staging was evaluated by the eighth edition of the Union for International Cancer Control (UICC) TNM classification system (11). Because the survival of patients with ypT0 and ypT1 was similar, we merged the patients with ypT0 into the ypT1 group.
Variable and Definition
The RFS was calculated from surgery to the first event (i.e., local recurrence, distant recurrence, or death from any cause). The OS was calculated from when the disease was diagnosed to death or the final follow-up date in December 2017. According to the Japanese gastric cancer treatment guidelines (12), we divided the extent of lymph node dissection into D1 or D2. Similarly, we divided the resection margins into R0, R1 or R2. The score of tumor response regression was defined according to the recommendations of the College of American Pathologists as follows: 0=No viable cancer cells (complete response); 1=Minimal residual cancer with single cells or small groups of cancer cells (near complete response); 2=Residual cancer with evident tumor regression, which is more than single cells or small groups of cancer cells (partial response); and 3=Extensive residual cancer with no evident tumor regression (poor or no response) (13). The results were reviewed by two independent pathologists who were blinded to the clinical data. If the results of the same sample were discordant, then the pathologists would discuss to reach a final score.
Treatment
Final decision to administer neoadjuvant chemotherapy, dose and cycles were made after careful discussion between the clinician and the patients. An oxaliplatin-based regimen was defined as a neoadjuvant chemotherapy regimen containing oxaliplatin. An epirubicin-based regimen was defined as a neoadjuvant chemotherapy regimen containing epirubicin. A total of 58 patients received the regimen containing both oxaliplatin and epirubicin. The median number of cycles of neoadjuvant chemotherapy was 3 (range 1-12).
Adjuvant chemotherapy: According to the patient’s wishes and their physical condition, fluoride-based adjuvant chemotherapy was recommended for most patients with pathological stage II and III disease in our center, as previously described. For patients who did not show histologic tumor regression before surgery, the adjuvant regimen was given different from the neoadjuvant regimen.
Surgery
In general, resection of the gastric tumor with D2 lymphadenectomy was performed within 4 weeks after the last day of chemotherapy.
Follow-up
Follow-up visits for both cohorts generally consist of clinic visits every 3 months for the first 2 years and every 6 months for years 3 to 5. Most routine patient follow-up appointments include a physical examination, laboratory tests, chest radiography, abdominal ultrasonography or CT, and an annual or biannual endoscopic examination for patients with a remnant stomach (14, 15).
Statistical Analysis
Statistical analysis was performed using SPSS 20.0 software (SPSS, Chicago, IL). Intergroup comparisons for discrete variables were analyzed with the chi-squared test or Fisher’s exact test. The Kaplan–Meier method was used to calculate OS and RFS. A log-rank test was used to compare survival curves. The reverse Kaplan–Meier method was used to calculate the median follow-up time. A Cox regression model was used to calculate hazard ratios of ACT treatment. Ordinal regression was performed for relationships of covariates with TRG. Two-sided p-values < 0.05 were considered statistically significant.
Results
Patient Demographics and Neoadjuvant Treatment
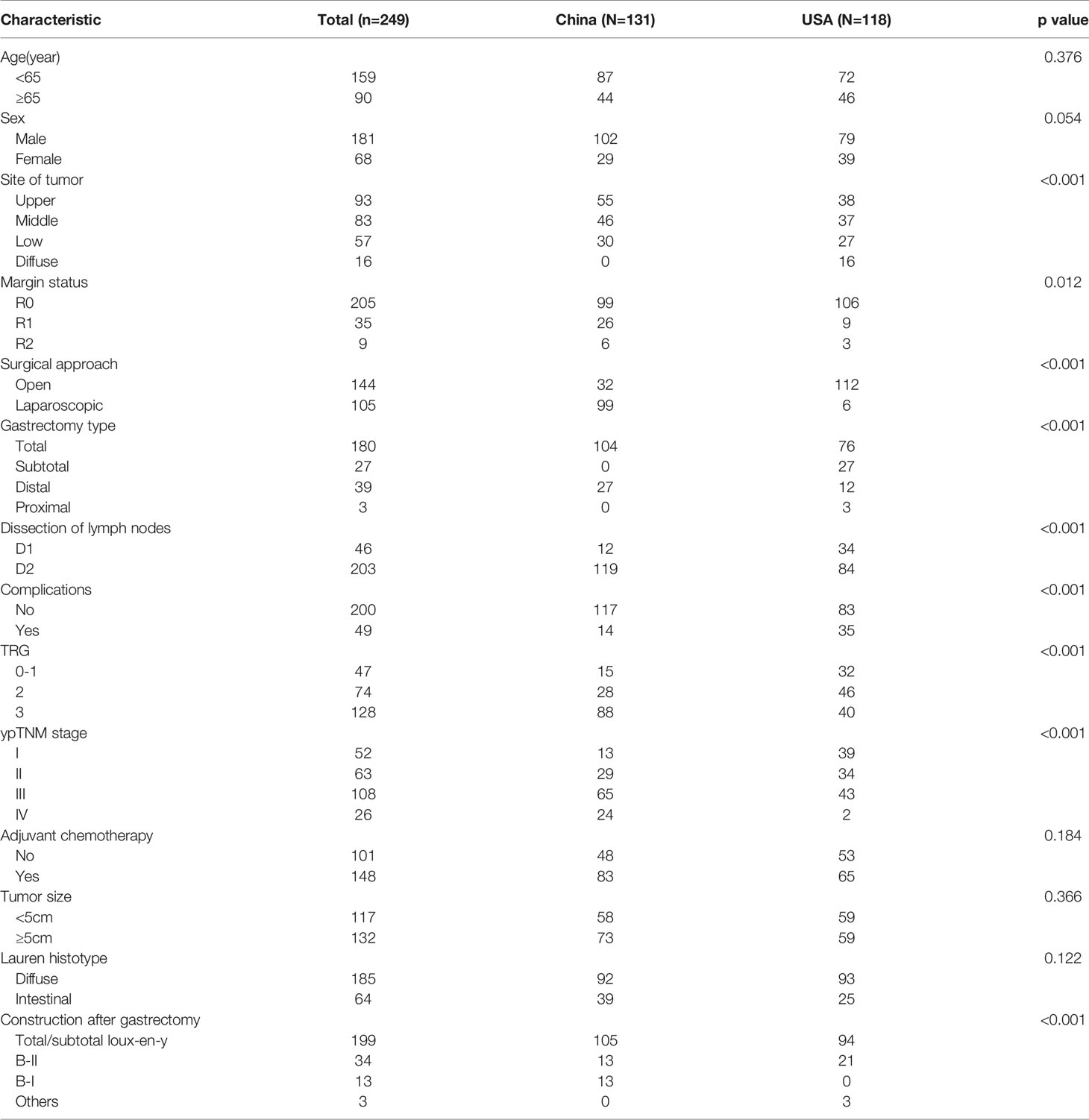
The baseline characteristics of 249 patients are listed in Table 1. One hundred seventy-two (69%) patients were administered the oxaliplatin-based regimen, and 77 (31%) patients were administered the nonoxaliplatin-based regimen. The median number of cycles of neoadjuvant chemotherapy was 3 (range 1-12). Concerning histopathologic response evaluation, the TRG results for patients treated with neoadjuvant chemotherapy were as follows: TRG 0 (n = 12, 4.8%); TRG 1 (n = 35, 14.1%); TRG 2 (n = 74, 29.7%); and TRG 3 (n = 128, 51.4%). Because the survival of patients with TRG 0 and TRG 1 was similar, the cohort was divided into three groups: TRG 0 or TRG 1 (TRG 0-1), TRG 2, and TRG 3 (Table 1). The patient demographics among different TRG groups are listed in Supplementary Table 1.
Impact of TRG on Survival
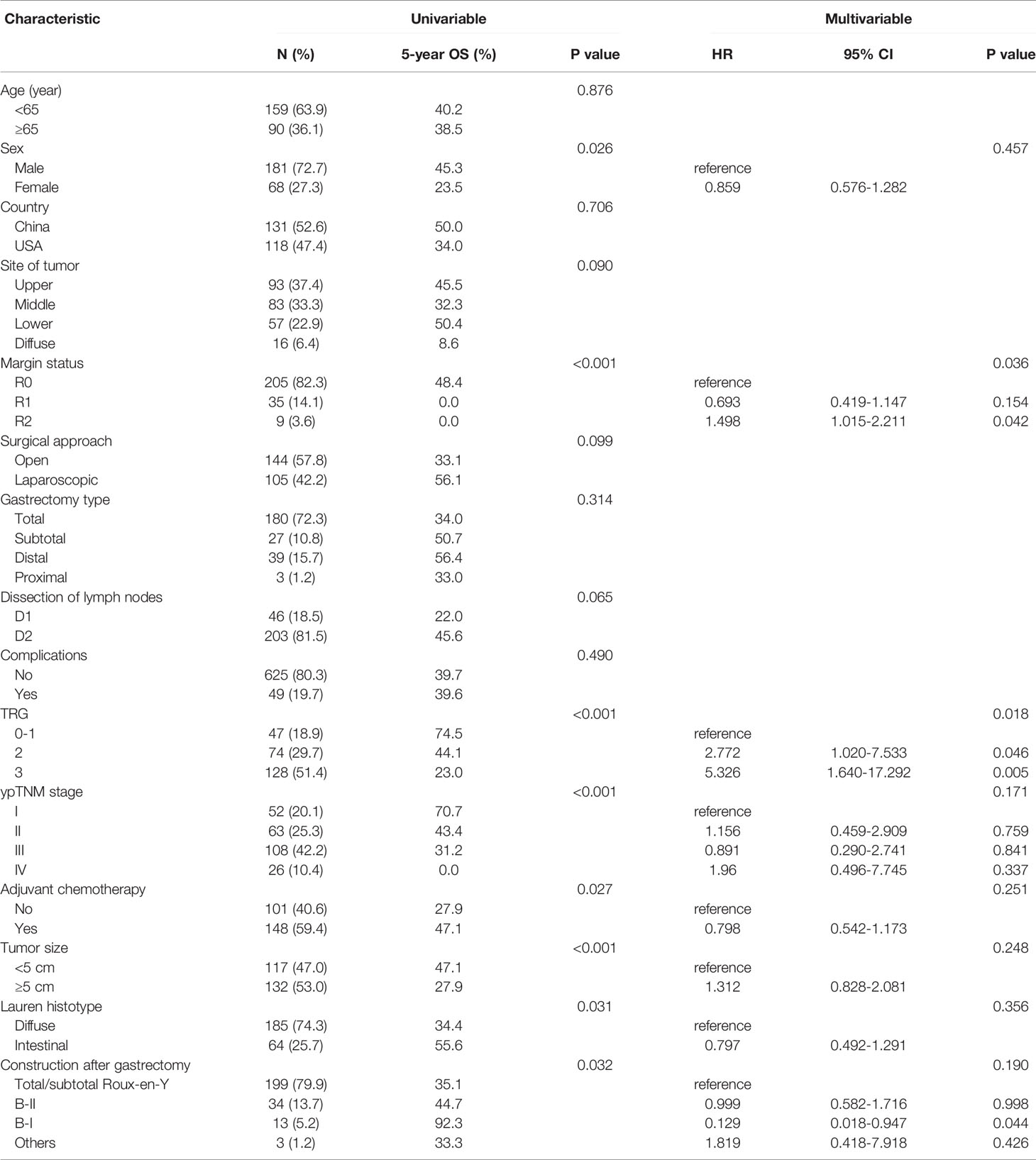
After a median follow-up of 38.8 (95% CI: 34.1–43.6) months, the overall survival rates at 3 and 5 years were 48.1% and 39.5%, respectively, in the total cohort. For patients with TRG 0-1, the 3- and 5-year survival rates were 85.2% and 74.5%, respectively, when compared to 56.1% and 44.1% with TRG 2, and 28.2% and 23.0% with TRG 3, respectively (p<0.001) (Figure 1A). Univariable Cox analyses revealed sex (p=0.026), margin status (p<0.001), TRG (p=0.001), ypTNM stage (p<0.001), adjuvant chemotherapy (p=0.001), tumor size (p=0.001), Lauren histotype (p=0.031), and construction after gastrectomy (p=0.032) as significant risk factors for overall survival. Multivariable Cox analyses revealed that only margin status (p=0.001) and TRG (p=0.001) were independent risk factors for overall survival (Table 2). Overall survival curves adjusted by multivariate models was shown in Figure S1A.
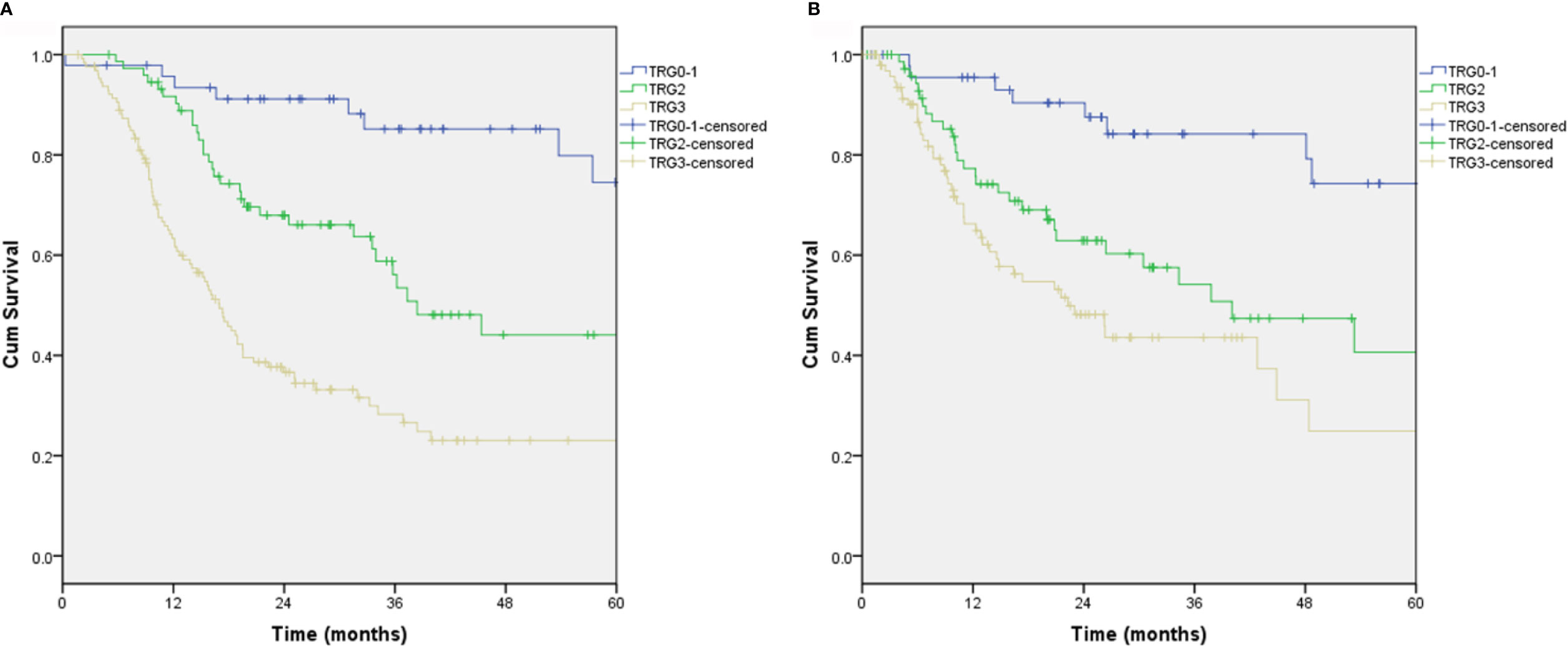
Figure 1 Overall survival and recurrence-free survival from TRG scores. (A) Overall survival, P<0.001; (B) Recurrence-free survival, P<0.001.
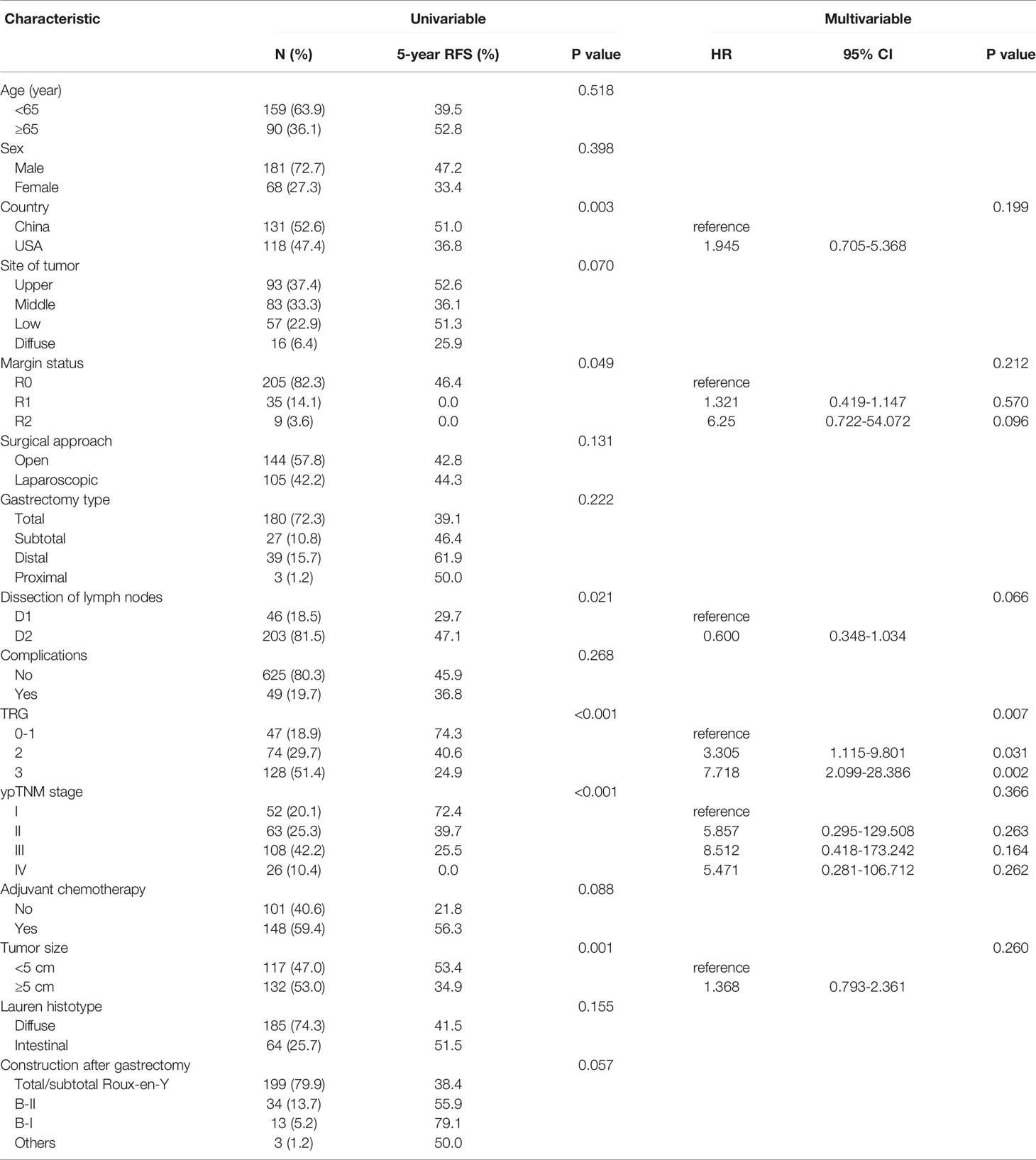
The recurrence-free survival rates at 3 and 5 years were 56.7% and 44.3%, respectively. For patients with TRG 0-1, the 3- and 5-year recurrence-free survival rates were 84.2% and 74.3%, respectively, when compared to 54.2% and 40.6% with TRG 2 and 43.6% and 24.9% with TRG 3, respectively (p<0.001) (Figure 1B). Univariable Cox analyses revealed country (p=0.026), margin status (p=0.049), dissection of lymph nodes (p=0.021), TRG (p<0.001), ypTNM stage (p<0.001), and tumor size (p=0.001) as significant risk factors for recurrence-free survival. Multivariable Cox analyses revealed that only TRG (p=0.007) was an independent risk factor for recurrence-free survival (Table 3). Recurrence-free survival curves adjusted by multivariate models was shown in Figure S1B.
The analyses of disease-free survival and distant-metastasis-free survival yielded the similar findings. (Figures S2A, B)
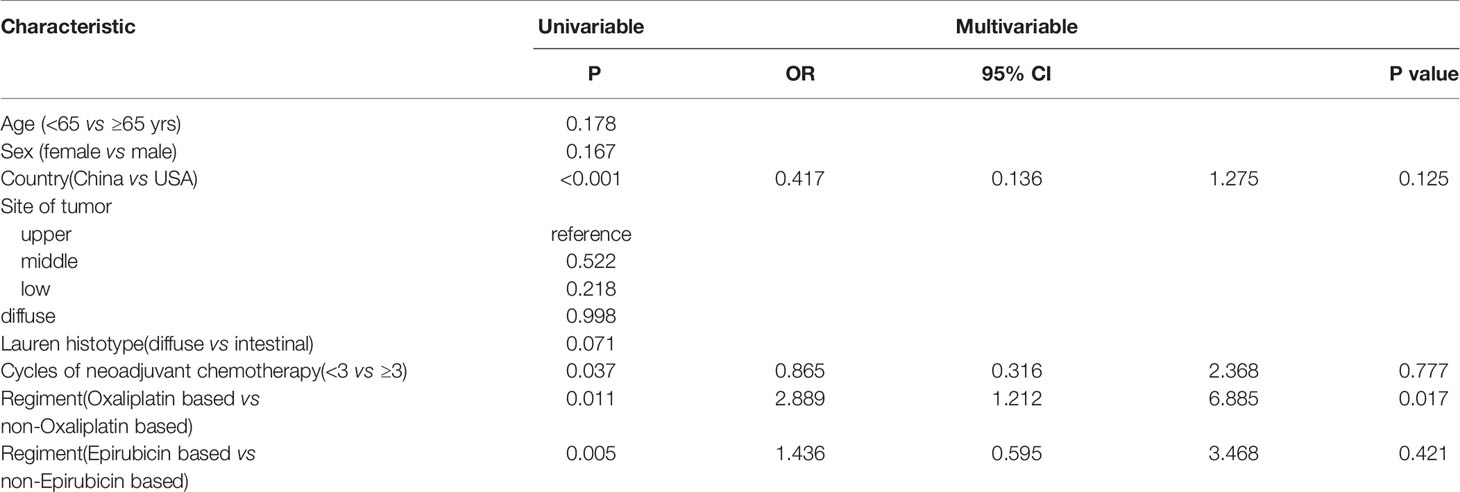
Factors Predicting Pathologic Response
Univariable Cox analyses revealed that country (p<0.001), cycles of neoadjuvant chemotherapy (p=0.037), regimen (oxaliplatin-based vs nonoxaliplatin based) (p=0.011), and regimen (epirubicin-based vs nonepirubicin-based) (p=0.005) were associated with TRG. Multivariable analysis revealed that only oxaliplatin-based regimen (p=0.017) was the strongest predictor of TRG (Table 4).
Effects of Oxaliplatin-Based Regimen on Overall Survival and Recurrence-Free Survival
Kaplan-Meier survival estimates comparing adjuvant oxaliplatin-based regimens with nonoxaliplatin-based regimens are illustrated in Figure 2. The median OS of patients receiving the oxaliplatin-based regimen was significantly better than those receiving the nonoxaliplatin-based regimen (38.4 vs 19.5 months, respectively; p=0.01) (Figure 2A). There was a trend toward improving recurrence-free survival in patients receiving the oxaliplatin-based regimen; however, this trend did not reach statistical significance (48.4 vs 23 months, respectively; p=0.178) (Figure 2B).
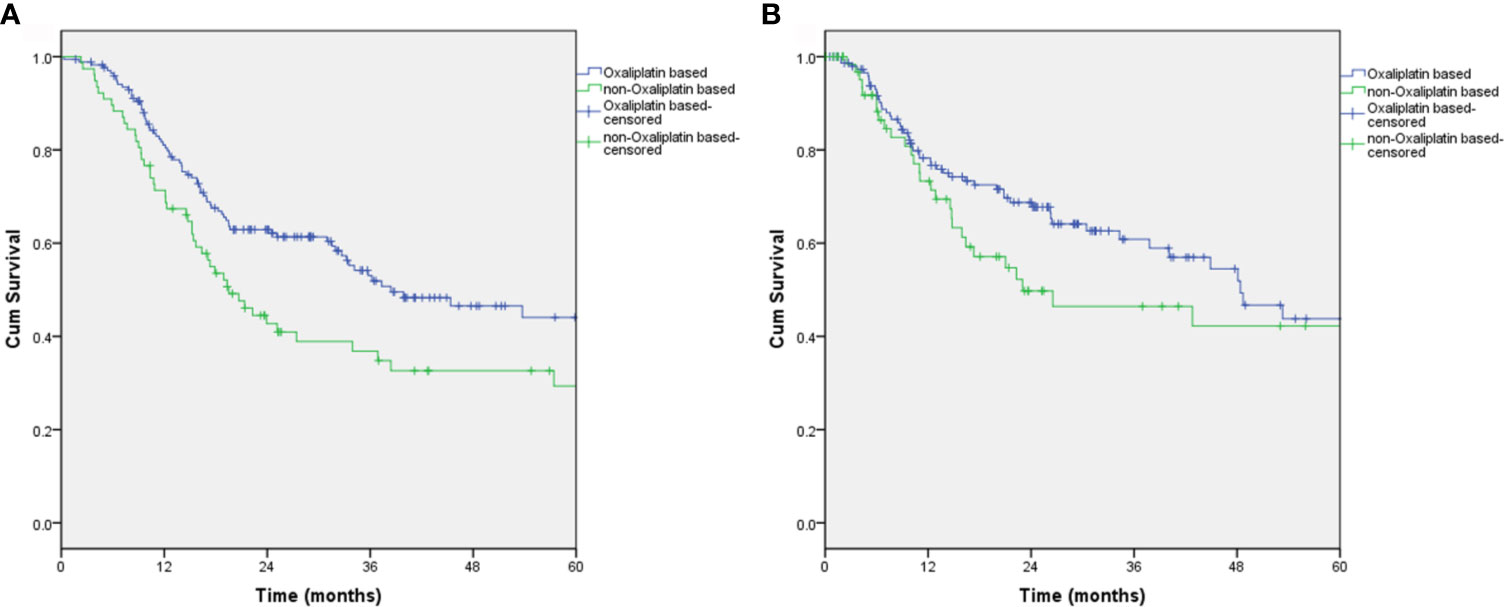
Figure 2 Overall survival and recurrence-free survival of patients who received the oxaliplatin-based regimen. (A) Overall survival, P=0.01; (B) Recurrence-free survival, P=0.178.
Subgroup Analyses by Histology All Subtype
Among the 65 signet-ring cell carcinoma (SRCC) patients, 51 (78.5%) had received the oxaliplatin-based regimen, and 14 (21.5%) had not. When comparing with and without oxaliplatin-based SRCC patient groups, the median OS rates were 31.5 months versus 18.9 months (p=0.272), and the median RFS was 21.5 months versus 17.3 months (p=0.371), respectively. Among the 184 non-SRCC patients, 121 (65.8%) had received an oxaliplatin-based regimen, and 63 (34.2%) had not. When comparing with and without oxaliplatin-based non-SRCC patient groups, the median OS rates were 53.7 months versus 19.5 months, respectively (p=0.011) (Figure 3A). There was a significant improvement in the overall survival in patients who received-oxaliplatin-based regimens. The oxaliplatin-based regimen for patients with neoadjuvant chemotherapy showed a trend toward improving recurrence-free survival (Figure 3B); however, this result did not reach statistical significance when compared to the nonoxaliplatin-based regimen (53.3 versus 42.8 months, p=0.14, respectively).
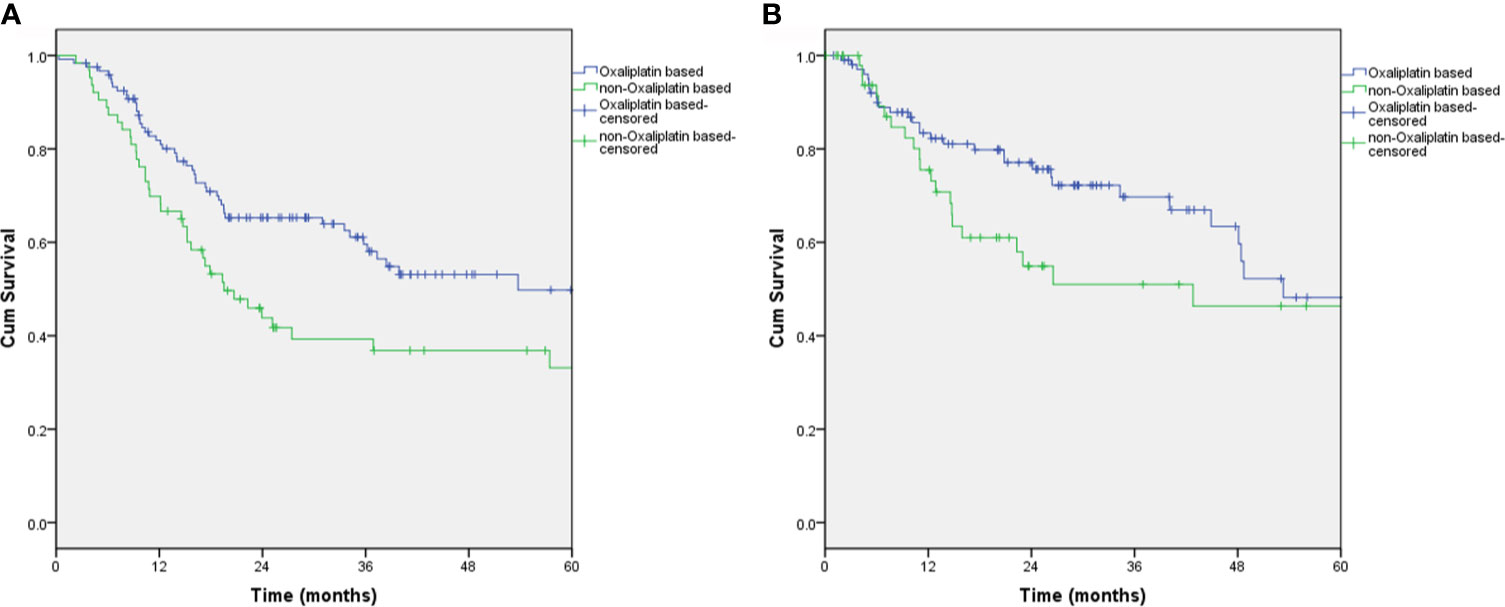
Figure 3 Overall survival and recurrence-free survival of non-SRCC patients who received the oxaliplatin-based regimen. (A) Overall survival, P=0.011; (B) Recurrence-free survival, P=0.14.
Discussion
The present study has demonstrated that the results of the histological-based evaluation were a good prognostic predictor for advanced gastric cancer patients receiving neoadjuvant chemotherapy. In addition, the factors predicting the histological tumor regression grading were explored.
Recently, a study suggested that TRG 1a/b is associated with improved survival (median OS>69.8 vs 22.8 months), but this association was not statistically significant, and a multivariate analysis was unable to confirm the predictive value of TRG. However, it should be noted that only 58 patients with neoadjuvant chemotherapy were included in this study (16). In contrast, Becker K et al. reported that TRG was an independent prognostic factor in the analysis of 480 patients with locally advanced gastric cancer treated with neoadjuvant chemotherapy followed by radical gastrectomy (17). In addition, a meta-analysis of 17 published studies also confirmed that major pathologic response is associated with a significant improvement in OS compared to no response or minor pathologic changes after neoadjuvant therapy in gastro-esophageal cancers (18). These findings were strongly supported by the results of the present study, in which multivariate survival analysis demonstrated that TRG was an independent prognostic factor for predicting worse OS.
A poorer prognosis of patients with SRCC compared to patients with non-SRCC has been identified in many reports. A French study revealed that perioperative chemotherapy provides no survival benefit in patients with gastric SRCC (19). To investigate the benefit of the oxaliplatin-based regimen, we stratified the analyzed differences in the survival rates between the SRCC and non-SRCC patient groups. Our data reveal that the oxaliplatin-based regimen failed to improve OS and RFS in patients with SRCC, indicating that the oxaliplatin-based regimen may not be the optimal choice of neoadjuvant chemotherapy for these patients.
There were several limitations in the present study. First, selected bias was inevitable in this retrospective study. Second, due to the diversity of chemotherapy regimens used in the two investigated countries and the data limited, we were unable to obtain a specific regimen (including dose and cycles) that was effective for a particular histopathological type. Despite these limitations, the present study was the first international study to explore the factors affecting TRG and to reveal that oxaliplatin-based neoadjuvant chemotherapy has potential benefits for OS in patients with nonsignet ring cell carcinoma.
In conclusion, our results suggested that TRG was an independent factor of gastric cancer treated with neoadjuvant chemotherapy plus surgery. Oxaliplatin-based neoadjuvant chemotherapy regimens improve tumor response and may benefit the OS of patients with nonsignet ring cell carcinoma.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by The Institutional Review Board of Fujian Medical University Union Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
J-WX, JL, B-bX, MT, and C-MH conceived the study, analyzed the data, and drafted the manuscript. C-HZ helped critically revise the manuscript for important intellectual content. PL, J-BW, J-XL, Q-YC, L-LC, ML, R-HT, Z-NH, and J-LL helped collect data and design the study. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the Joint Funds for the innovation of science and Technology, Fujian province (2017Y9011, 2017Y9004, 2018Y9041); the second batch of special support funds for Fujian Province innovation and entrepreneurship talents (2016B013); Construction Project of Fujian Province Minimally Invasive Medical Center (No. [2017]171); Natural Science Foundation of Fujian Province (2019J01155); Fujian provincial science and technology innovation joint fund project plan (2018Y9005); Fujian provincial health technology project (2019-ZQN-37).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2021.587856/full#supplementary-material
Supplementary Figure 1 | Survival curves adjusted by multivariate models from TRG scores. (A) Overall survival, P<0.001; (B) Recurrence-free survival, P<0.001.
Supplementary Figure 2 | Disease-free survival and distant-metastasis-free survival from TRG scores. (A) Disease-free survival, P<0.001; (B) Distant-metastasis-free survival, P<0.001.
References
1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global Cancer Statistics, 2012. Ca- Cancer J Clin (2015) 65(2):87–108. doi: 10.3322/caac.21262
2. Schuhmacher C, Gretschel S, Lordick F, Reichardt P, Hohenberger W, Eisenberger CF, et al. Neoadjuvant Chemotherapy Compared With Surgery Alone for Locally Advanced Cancer of the Stomach and Cardia: European Organisation for Research and Treatment of Cancer Randomized Trial 40954. J Clin Oncol (2010) 28(35):5210–8. doi: 10.1200/JCO.2009.26.6114
3. Wang X, Zhao L, Liu H, Zhong D, Liu W, Shan G, et al. A Phase II Study of a Modified FOLFOX6 Regimen as Neoadjuvant Chemotherapy for Locally Advanced Gastric Cancer. Br J Cancer (2016) 114(12):1326–33. doi: 10.1038/bjc.2016.126
4. Ychou M, Boige V, Pignon JP, Conroy T, Bouche O, Lebreton G, et al. Perioperative Chemotherapy Compared With Surgery Alone for Resectable Gastroesophageal Adenocarcinoma: An FNCLCC and FFCD Multicenter Phase III Trial. J Clin Oncol (2011) 29(13):1715–21. doi: 10.1200/JCO.2010.33.0597
5. He J, Blair AB, Groot VP, Javed AA, Burkhart RA, Gemenetzis G, et al. Is a Pathological Complete Response Following Neoadjuvant Chemoradiation Associated With Prolonged Survival in Patients With Pancreatic Cancer? Ann Surg (2018) 268(1):1–8. doi: 10.1097/SLA.0000000000002672
6. Karagkounis G, Thai L, Mace AG, Wiland H, Pai RK, Steele SR, et al. Prognostic Implications of Pathological Response to Neoadjuvant Chemoradiation in Pathologic Stage III Rectal Cancer. Ann Surg (2019) 269(6):1117–23. doi: 10.1097/SLA.0000000000002719
7. Becker K, Mueller JD, Schulmacher C, Ott K, Fink U, Busch R, et al. Histomorphology and Grading of Regression in Gastric Carcinoma Treated With Neoadjuvant Chemotherapy. Cancer (2003) 98(7):1521–30. doi: 10.1002/cncr.11660
8. Martin-Romano P, Sola JJ, Diaz-Gonzalez JA, Chopitea A, Iragorri Y, Martinez-Regueira F, et al. Role of Histological Regression Grade After Two Neoadjuvant Approaches With or Without Radiotherapy in Locally Advanced Gastric Cancer. Br J Cancer (2016) 115(6):655–63. doi: 10.1038/bjc.2016.252
9. Lowy AM, Mansfield PF, Leach SD, Pazdur R, Dumas P, Ajani JA. Response to Neoadjuvant Chemotherapy Best Predicts Survival After Curative Resection of Gastric Cancer. Ann Surg (1999) 229(3):303–8. doi: 10.1097/00000658-199903000-00001
10. Smyth EC, Fassan M, Cunningham D, Allum WH, Okines AF, Lampis A, et al. Effect of Pathologic Tumor Response and Nodal Status on Survival in the Medical Research Council Adjuvant Gastric Infusional Chemotherapy Trial. J Clin Oncol (2016) 34(23):2721–7. doi: 10.1200/JCO.2015.65.7692
11. Sano T, Coit DG, Kim HH, Roviello F, Kassab P, Wittekind C, et al. Proposal of a New Stage Grouping of Gastric Cancer for TNM Classification: International Gastric Cancer Association Staging Project. Gastric Cancer (2017) 20(2):217–25. doi: 10.1007/s10120-016-0601-9
12. Japanese Gastric Cancer A. Japanese Gastric Cancer Treatment Guidelines 2014 (Ver. 4). Gastric Cancer (2017) 20(1):1–19. doi: 10.1007/s10120-016-0622-4
13. Ryan R, Gibbons D, Hyland JM, Treanor D, White A, Mulcahy HE, et al. Pathological Response Following Long-Course Neoadjuvant Chemoradiotherapy for Locally Advanced Rectal Cancer. Histopathology (2005) 47(2):141–6. doi: 10.1111/j.1365-2559.2005.02176.x
14. Lu J, Xu BB, Zheng CH, Li P, Xie JW, Wang JB, et al. Development and External Validation of a Nomogram to Predict Recurrence-Free Survival After R0 Resection for Stage II/III Gastric Cancer: An International Multicenter Study. Front Oncol (2020) 10:574611. doi: 10.3389/fonc.2020.574611
15. Xu BB, Lu J, Zheng ZF, Huang CM, Zheng CH, Xie JW, et al. Comparison of Short-Term and Long-Term Efficacy of Laparoscopic and Open Gastrectomy in High-Risk Patients With Gastric Cancer: A Propensity Score-Matching Analysis. Surg Endosc (2019) 33(1):58–70. doi: 10.1007/s00464-018-6268-z
16. Blackham AU, Greenleaf E, Yamamoto M, Hollenbeak C, Gusani N, Coppola D, et al. Tumor Regression Grade in Gastric Cancer: Predictors and Impact on Outcome. J Surg Oncol (2016) 114(4):434–9. doi: 10.1002/jso.24307
17. Becker K, Langer R, Reim D, Novotny A, Meyer zum Buschenfelde C, Engel J, et al. Significance of Histopathological Tumor Regression After Neoadjuvant Chemotherapy in Gastric Adenocarcinomas: A Summary of 480 Cases. Ann Surg (2011) 253(5):934–9. doi: 10.1097/SLA.0b013e318216f449
18. Tomasello G, Petrelli F, Ghidini M, Pezzica E, Passalacqua R, Steccanella F, et al. Tumor Regression Grade and Survival After Neoadjuvant Treatment in Gastro-Esophageal Cancer: A Meta-Analysis of 17 Published Studies. Eur J Surg Oncol (2017) 43(9):1607–16. doi: 10.1016/j.ejso.2017.03.001
19. Messager M, Lefevre JH, Pichot-Delahaye V, Souadka A, Piessen G, Mariette C, et al. The Impact of Perioperative Chemotherapy on Survival in Patients With Gastric Signet Ring Cell Adenocarcinoma: A Multicenter Comparative Study. Ann Surg (2011) 254(5):684–93; discussion 693. doi: 10.1097/SLA.0b013e3182352647
Keywords: gastric cancer, neoadjuvant chemotherapy, tumor regression grading, signet-ring cell carcinoma (SRCC), recurrence-free survival (RFS) rate and overall survival (OS)
Citation: Xie J-W, Lu J, Xu B-b, Zheng C-H, Li P, Wang J-B, Lin J-X, Chen Q-Y, Cao L-L, Lin M, Tu R-H, Huang Z-N, Lin J-L, Truty MJ and Huang C-M (2021) Prognostic Value of Tumor Regression Grading in Patients Treated With Neoadjuvant Chemotherapy Plus Surgery for Gastric Cancer. Front. Oncol. 11:587856. doi: 10.3389/fonc.2021.587856
Received: 27 July 2020; Accepted: 29 June 2021;
Published: 26 July 2021.
Edited by:
Alberto Biondi, Catholic University of the Sacred Heart, ItalyReviewed by:
Kimberly Washington, Texas Christian University, United StatesHui Chang, Sun Yat-sen University Cancer Center (SYSUCC), China
Copyright © 2021 Xie, Lu, Xu, Zheng, Li, Wang, Lin, Chen, Cao, Lin, Tu, Huang, Lin, Truty and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mark J. Truty, dHJ1dHkubWFya0BtYXlvLmVkdQ==; Chang-Ming Huang, aGNtbHIyMDAyQDE2My5jb20=
 Jian-Wei Xie
Jian-Wei Xie Jun Lu
Jun Lu Bin-bin Xu
Bin-bin Xu Chao-Hui Zheng
Chao-Hui Zheng Ping Li
Ping Li Jia-Bin Wang1,2,3,4
Jia-Bin Wang1,2,3,4 Qi-Yue Chen
Qi-Yue Chen Ju-Li Lin
Ju-Li Lin Mark J. Truty
Mark J. Truty Chang-Ming Huang
Chang-Ming Huang