- 1Department of Medical Biotechnology, University of Siena, Siena, Italy
- 2Department of Medical Sciences, Surgery and Neuroscience, University of Siena, Siena, Italy
- 3Center of Applied Biomedical Research (CRBA), S. Orsola-Malpighi Hospital, Bologna, Italy
- 4Department of Experimental, Diagnostic and Specialty Medicine, University of Bologna, Bologna, Italy
- 5Pathology Unit, Ospedale Civico di Carrara, Carrara, Italy
- 6Retired, Siena, Italy
Here we present the case of a patient affected by rectal squamous cell carcinoma in which we demonstrated the presence of Human Papillomavirus (HPV) by a variety of techniques. Collectively, the virus was detected not only in the tumor but also in some regional lymph nodes and in non-neoplastic mucosa of the upper tract of large bowel. By contrast, it was not identifiable in its common sites of entry, namely oral and ano-genital region. We also found HPV DNA in the plasma-derived exosome. Next, by in vitro studies, we confirmed the capability of HPV DNA-positive exosomes, isolated from the supernatant of a HPV DNA positive cell line (CaSki), to transfer its DNA to human colon cancer and normal cell lines. In the stroma nearby the tumor mass we were able to demonstrate the presence of virus DNA in the stromal compartment, supporting its potential to be transferred from epithelial cells to the stromal ones. Thus, this case report favors the notion that human papillomavirus DNA can be vehiculated by exosomes in the blood of neoplastic patients and that it can be transferred, at least in vitro, to normal and neoplastic cells. Furthermore, we showed the presence of viral DNA and RNA in pluripotent stem cells of non-tumor tissue, suggesting that after viral integration (as demonstrated by p16 and RNA in situ hybridization positivity), stem cells might have been activated into cancer stem cells inducing neoplastic transformation of normal tissue through the inactivation of p53, p21, and Rb. It is conceivable that the virus has elicited its oncogenic effect in this specific site and not elsewhere, despite its wide anatomical distribution in the patient, for a local condition of immune suppression, as demonstrated by the increase of T-regulatory (CD4/CD25/FOXP3 positive) and T-exhausted (CD8/PD-1positive) lymphocytes and the M2 polarization (high CD163/CD68 ratio) of macrophages in the neoplastic microenvironment. It is noteworthy that our findings depicted a static picture of a long-lasting dynamic process that might evolve in the development of tumors in other anatomical sites.
Introduction
Human papillomavirus (HPV) DNA has been detected in a variety of cancer, including colorectal cancer (CRC) (1–4). Through the integration of viral DNA into the human genome, expression of oncoproteins, and inactivation of tumor suppression genes, HPV damages cell proliferation in its site of infection, inducing oncogenesis (2). Recently, HPV DNA has been found as circulating DNA in the serum of patients with HPV-associated invasive carcinoma (5) and its presence has been considered as a useful biomarker for disease recurrence (6). Tumor-derived exosomes and extracellular vesicles are garnering increasing attention because of their ability to transfer bioactive molecules (mRNAs, microRNAs, DNA, and proteins) between neighboring cancerous or normal cells, and to contribute to human cancer progression. Moreover, exosomes and extracellular vesicles have been implicated in HPV transmission and carcinogenesis (7), and the presence of HPV DNA in the serum derived extracellular vesicles (EVs) of patients with breast diseases has been recently reported (8).
While there is a strong association between HPV and squamous cell carcinoma of some sites (e.g., genitals, anus, and head and neck region), the putative role of the virus in colorectal carcinogenesis still remains controversial (9). Detection of HPV in colonic tissue has led to a wide range of studies, analyzing the possibility of a casual or pathogenetic association between HPV and CRC. However, these studies applied different techniques for the detection of the virus, with discordant findings and inconsistencies in result reproducibility (10). In fact, it is very difficult that a causative role of HPV in a cancer can be explained only studying the molecular mechanisms. Since it is a very common virus, its presence can be occasional and the behave of the virus opportunistic. The proof of causation needs both studies on the molecular mechanisms and studies establishing that the probability a tumor occurs is higher when the HPV is present that when it is not, i.e., case control and cohort studies.
CRC is the third most common cause of cancer-related death in the world (11). Among its histotypes, pure squamous cell cancer (SCC) is very unusual, ranging from 0.1 to 0.25 per 1,000 CRC; its diagnosis is based on the restrictive criteria given by Williams et al. (12). Risk factors include proctitis, past history of radiotherapy to pelvic region, Schistosomiasis and Amoebiasis infection (13). The exact pathogenic mechanism remains speculative and several theories have been proposed (14, 15).
Here we present the case of a patient affected by rectal SCC in which we demonstrated HPV by immunohistochemistry, polymerase chain reaction (PCR), chromogenic in situ hybridization (CISH), and RNA in situ hybridization (ISH) for E6/E7 viral oncogenes mRNA in neoplastic and non-neoplastic tissues, including lymph nodes and sites far from the rectum. We also found HPV DNA in the plasma-derived from the patient, and by in vitro studies, we confirmed the capability of HPV DNA positive exosomes to transfer its DNA to recipient cells.
Background
Clinical Presentation
A 53 years-old caucasian man presented to our hospital complaining of sub-occlusive syndrome that lasted for 1 week. Family and medical history was unremarkable. Physical examination including digital rectal examination was negative. Colonoscopy showed a 5.0 × 4.5 × 4 cm lesion, 10 cm from the anal verge. The lesion was ulcerated and bleeding, it narrows the lumen and renders difficult to be overcome. Computed tomography (CT)-scan identified a heteroplastic and locally advanced lesion with enlarged lymph nodes (the greatest measuring 13 mm in maximum diameter) along the sigmoid chain. Neither pulmonary, hepatic, splenic localizations nor pleural or peritoneal effusions were identified. An anterior resection of the rectum and regional lymph nodes was performed without colostomy. Postoperatively, the patient underwent adjuvant radiotherapy of 45 Gy delivered to the pelvis in 25 fractions over 5 weeks. To date, after 60 months follow-up, the patient is alive and in good conditions, with no evidence of recurrence. Ethics approval for this study was obtained from the Institutional Review Board at the University of Siena (Italy) and written informed consent was obtained from the patient for the publication of this case report and any potentially-identifying information/images.
Materials and Methods
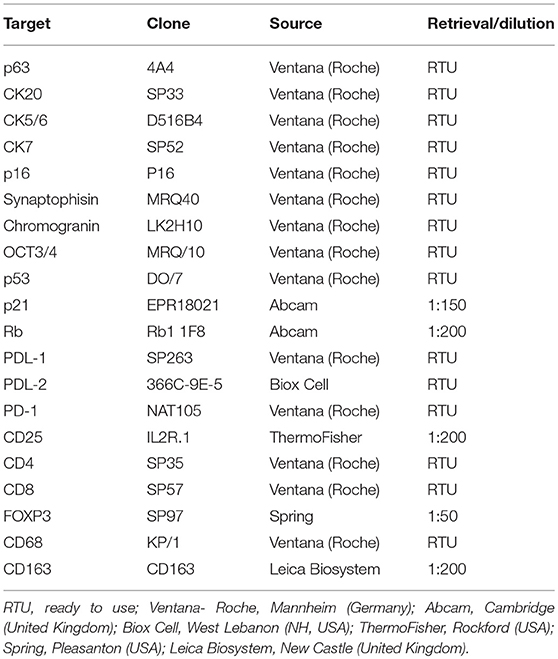
Tables 1–3 summarize the main techniques applied in the different samples.
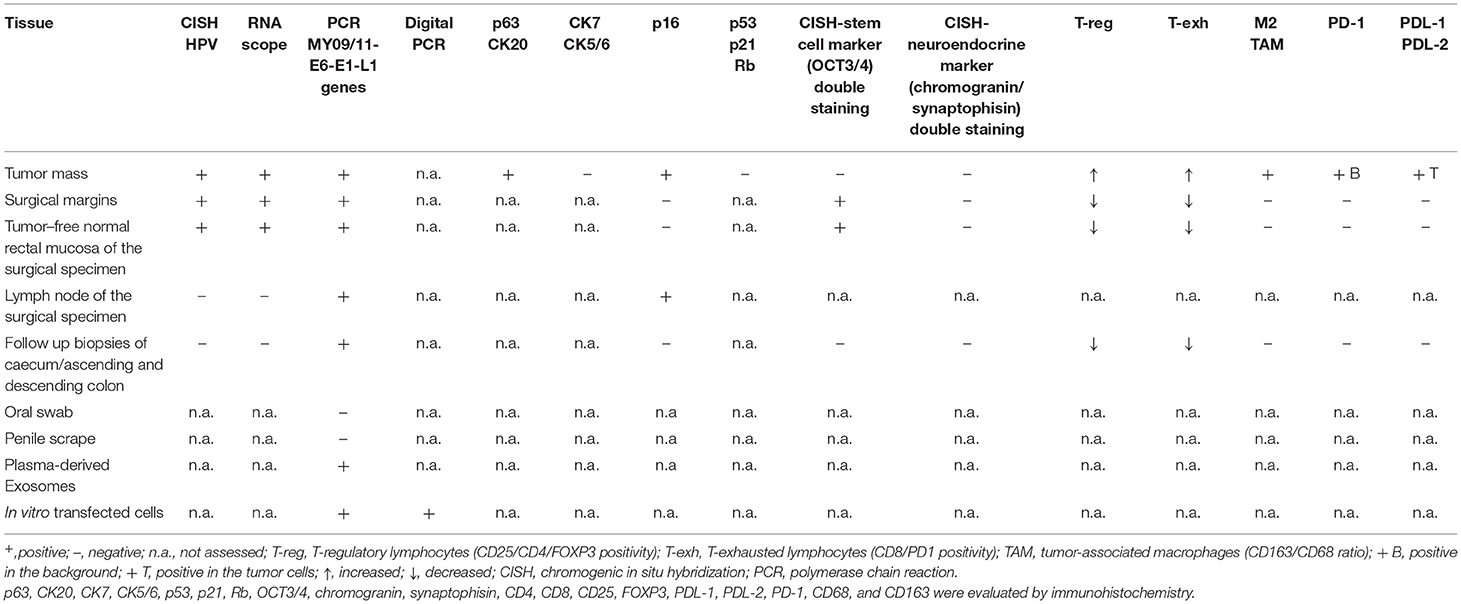
Table 1. Synoptical table of the methods applied in the different samples and the respective results obtained.
Results
Pathological Characterization
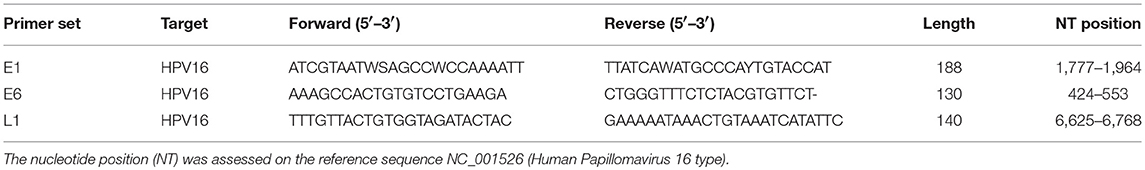
Grossly, an exophytic ulcerative mass with predominantly intraluminal growth and narrowing of the lumen was identified. The lesion measured 5.0 × 4.0 × 3.5 cm and extended throughout the muscular layer but without mesorectal involvement in the extraperitoneal tract of the specimen. On cut section, the mass had a relatively homogeneous appearance with focal areas of necrosis and hemorrhages. Microscopic examination demonstrated a moderately differentiated squamous cell carcinoma with basaloid features and koilocyte-like cells (Figure 1A, inset). Neither perineural nor lymphovascular invasion was present. Surgical margins as well as the regional lymph nodes examined showed no cancer infiltration. The final diagnosis according to Williams et al. criteria was G2 (12), pT3N0Mx, IIA (TNM 2017) primary squamous cell carcinoma of the rectum. By immunohistochemistry (IHC), the neoplastic cells were p63 and CK20 positive, and CK5/6 and CK7 negative, thus ruling out a possible rectal extension from an occult anal neoplasm.
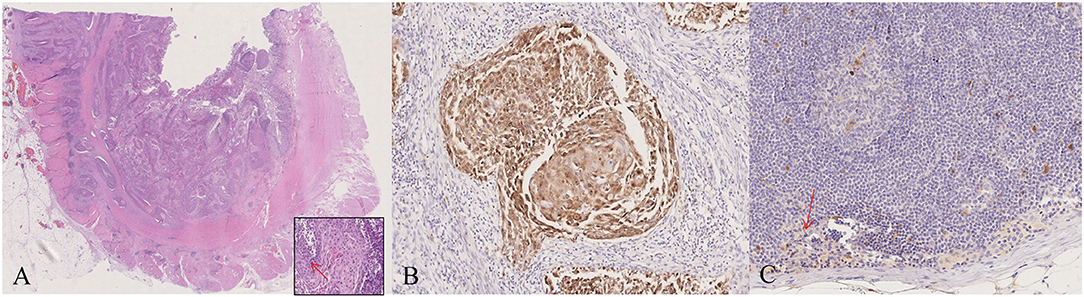
Figure 1. Pathological characterization. The morphological and immunohistochemical evaluation of the surgical specimen showed the presence of a squamous cell carcinoma with basaloid features and koilocyte-like cells (arrow) (A, inset), and p16 expression (B); the largest lymph node examined demonstrated p16 positivity in scattered large cells of the germinal center and the subcapsular sinus (arrow) (C). A, (A)-inset: haematoxylin and eosin (H&E); B,C: p16 staining. Original magnification (O.M.): A, 2.5x; (A)-inset, (B,C) 20x.
HPV Detection and Oncogenicity
The atypical localization of a SCC in the rectum and the detection of koilocyte-like differentiated cells within the tumor were indicators of the possible presence of HPV. Therefore, we searched the virus in the tumor mass, in its margins, in tumor-free normal rectal mucosa proximal to the tumor and in the lymph nodes by IHC for p16, PCR assays, CISH for HPV nucleic acids (ZytoFast PLUS CISH Implementation Kit HRP-DAB and ZytoFast HPV type 16/18 Probe, ZytoVision, Bio-Optica, Milan, Italy) and RNA ISH for E6/E7 mRNA transcripts (RNAscope®2.5 HD Assay- RED, probe HPV 16, Acdbio, Milan, Italy) (Table 1).
By IHC for p16, a useful surrogate biomarker of HPV integration and E7 over-expression (16), strong positivity was detected only in the neoplastic cells (Figure 1B) and in scattered large cells in the germinal center and in the subcapsular sinus of some lymph nodes (Figure 1C). The margins and tumor-free normal rectal mucosa did not show p16 expression.
PCR assays for HPV DNA detection were performed by MY09/11 (17) primer pool, able to amplify about forty mucosal HPV DNAs, then with different primer set, including E1, E6, and L1 primers (Table 2). HPV DNA was found in the tumor, surgical margins, tumor free normal rectal mucosa proximal to the neoplastic cells and in the largest dissected lymph node (Figure 2A, Table 1). Sequence analysis of PCR products sustained the specificity of the PCR results and identified HPV 16 genotype (Figure 2B). The presence of HPV DNA in the tumor, surgical margins and tumor free normal rectal mucosa proximal to the neoplastic cells was also confirmed by CISH (Figures 3A,B) and RNAscope assay (Figures 3C,D, D inset, Table 1). As far as CISH and RNA scope assays is concerned, intriguingly, we detected two different pattern of expression in tumor and cancer-free samples. In the neoplastic tissue we observed a “punctated” pattern with distinct multiple dot-like intranuclear signals by CISH (Figure 3A) and strong red dot-like signals by RNAscope (Figure 3C), which are typical of viral integration. Whereas, in the non-neoplastic tissue we detected a “diffuse” black pattern by CISH (Figure 3B) and only few weak red signals by RNAscope (Figure 3D, D inset), which are typical of episomal DNA (18, 19). Therefore, the virus was integrated only in neoplastic cells.
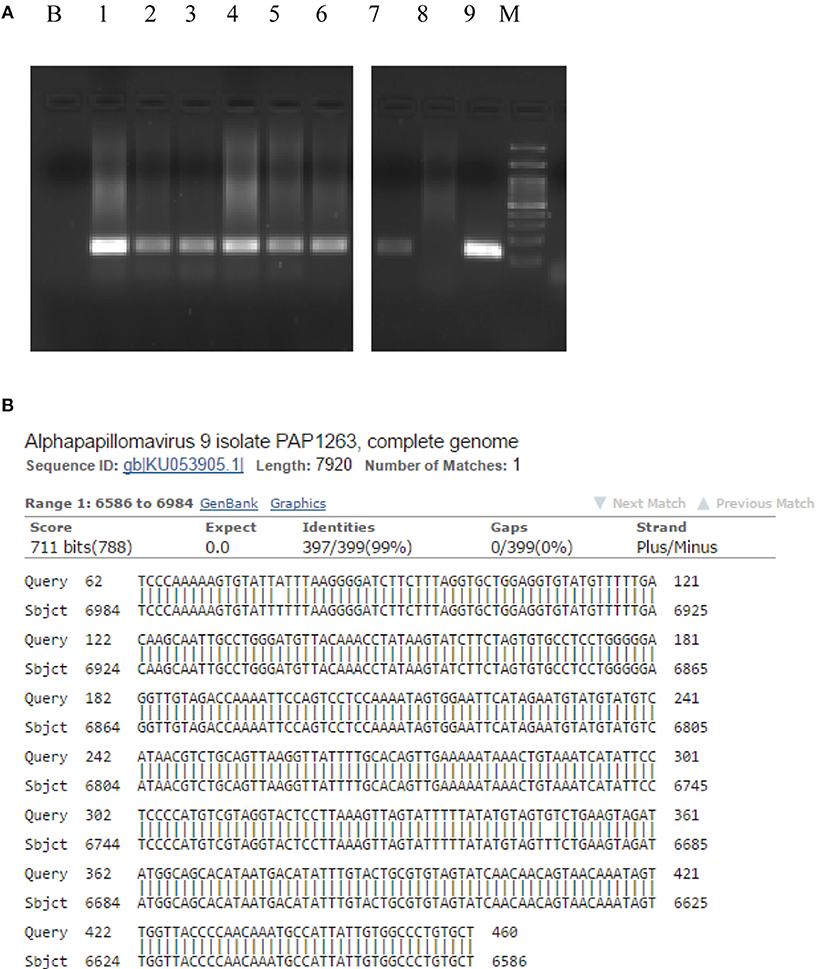
Figure 2. Human Papillomavirus polimerase chain reaction identification and typing. The presence of HPV 16 DNA was confirmed by HPV 16 genotype specific primer pair 5′- AAAGCCACTGTGTCCTGAAGA-3′ and 5′-CTGGGTTTCTCTACGTGTTCT-3′ able to amplify a 130 bps long fragment (424–553 nt, ref Seq Human Papillomavirus 16 type NC_001526). B, Blank, (1) Tumor mass, (2) Proximal margin, (3) Distal margin, (4) Lymph node, (5) Tumor-free mucosa of the surgical specimen, (6) Descending colon biopsies, (7) Caecum/ascending colon biopsies, (8) HPV DNA negative cervical cytological specimen, (9) HPV DNA positive cervical cytological specimen, M, Molecular weight marker (A). HPV 16 was present in the tumor mass as it is evident by the sequence alignment of the 460 bps L1 sequence obtained by MY11/09 PCR primers (B). HPV, Human Papillomavirus.
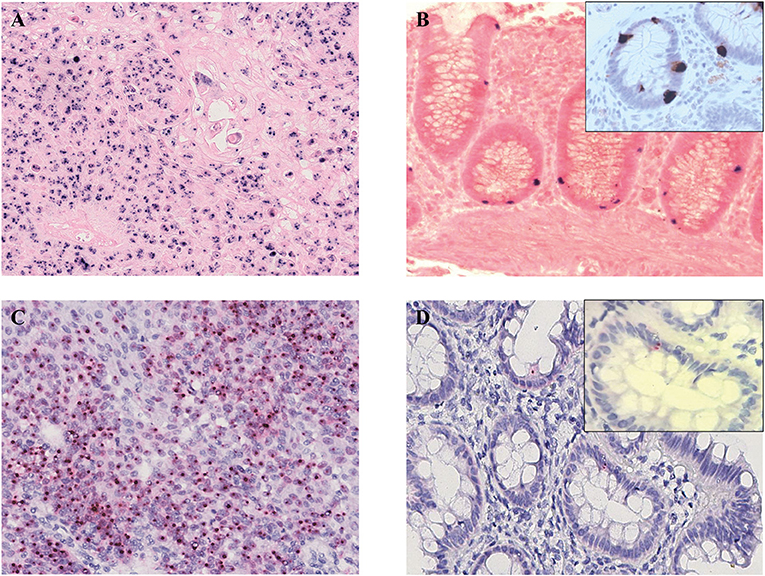
Figure 3. Human Papillomavirus detection and integration. In the neoplastic cells multiple black signals were shown by CISH with a “punctated” pattern characterized by multiple distinct dot-like intranuclear signals indicating viral integration (A); the normal mucosa of the resected specimen demonstrated scattered cells with HPV infection in a “diffuse” pattern with only few completely black stained nuclei corresponding to the episomal status of the virus (B). RNAscope assay detected E6 and E7 transcripts in the neoplastic (C) and normal mucosa cells of the surgical specimen (D, D inset) as multiple, strong red dot-like signals in the tumor and only few weak red signals in the cancer-free mucosa, corresponding the first pattern to viral integration and the second one to episomal infection. HPV-infected cells OCT3/4-positive (B inset). (A,B) CISH; (C,D) RNAscope; (A,C) original magnification (O.M.) 20x; (B,D) O.M. 40x; (B,D) inset, O.M. 63x. CISH, chromogenic in situ hybridization; HPV, Human Papillomavirus.
Interestingly, in the non-neoplastic tissue, the HPV16 positive signals by CISH and RNAscope were localized within the gland crypts (Figures 3B,D). To better characterize the nature of these cells (endocrine vs. stem-cell), double staining for HPV (by CISH) and chromogranin, synaptophyn, OCT3/4 (by IHC) was performed. The infected cells were OCT3/4-positive and chromogranin/synaptophyn-negative, thus presumably representing stem-cells (Figure 3B, B inset, Table 3).
The expression of tumor suppressor genes p53, p21, and Rb was absent in the tumor mass and in adjacent tissues, thus supporting the view that HPV was oncogenic in our case.
At the first follow-up, multiple biopsies of caecum/ascending, and descending colon, as well as oral swab and anal and uretral scrapes were collected and analyzed for HPV infection (Table 1). HPV was no detected in the oral and ano-genital regions; we demonstrated the presence of HPV DNA in all of the biopsies of right and left colon by PCR (Figure 2A), whereas CISH and RNAscope assays were negative, thus confirming that the virus was integrated only in the neoplastic cells.
HPV Circulation
We searched for presence of HPV DNA in the plasma-derived exosomes of the patient (Figure 4A). Exosomes were isolated from plasma specimens by CD9 immunobeads isolation kit (HansaBioMed Life Sciences Ltd. Cod. HBM-BOLC-CC/20-1) according to manufacturer's instruction. Prior to DNA extraction of the exosomes content, we performed a DNAseI digestion to remove contaminant DNA. We searched for HPV DNA by using PCR assay (MY09/11 and E6 primers) and we found the presence of HPV 16 DNA, as resulted by sequence alignment of the PCR product (Figure 4B). Thus, we tested the hypothesis that HPV DNA could be transferred to recipient cells by exposing cells to HPV DNA positive exosomes. HPV DNA positive exosomes were obtained from the supernatant of an HPV DNA positive cell line, the Caski cell line, which was established from a metastasis in the small bowel mesentery and contains HPV16 DNA integrated into the genome. We confirmed in vitro the capability of HPV DNA positive exosomes to transfer their content to HPV DNA negative cells, such as neoplastic and normal colon cell lines, HCT116 and NCM460, respectively, by digital PCR and conventional PCR (Figures 4C,D). The amplification reaction was performed by Digital PCR, with TaqMan assay (Vi03453396_s1, Invitrogen, Milan, Italy) for HPV 16 E1 gene amplification and conventional PCR with E6 primers (Table 1). Interestingly, by CISH we found the presence of HPV DNA in the stromal cells (fibroblasts and endothelial cells) nearby the neoplastic cells, suggesting an horizontal transfer of viral DNA from cancer cells (Figure 4E).
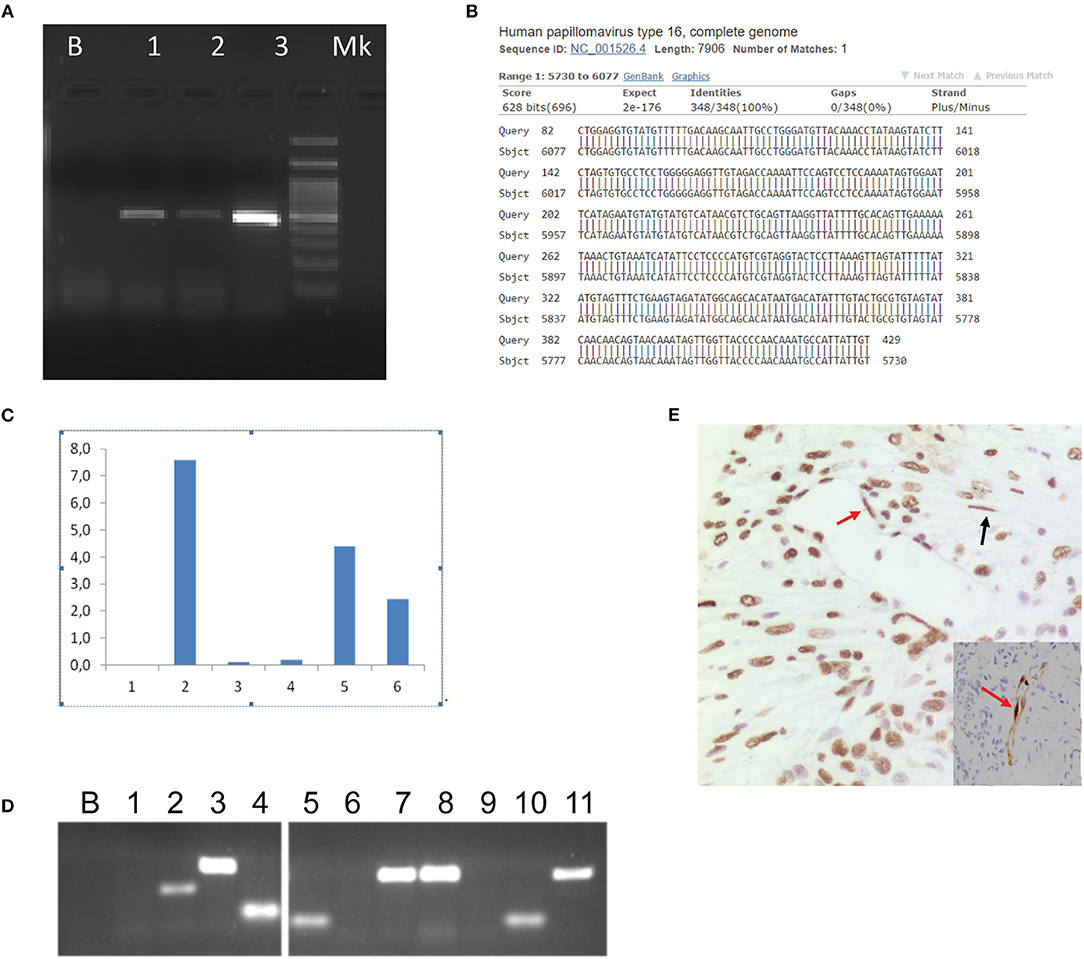
Figure 4. Human papillomavirus circulation. Electrophoresis showed the amplified HPV DNA obtained from plasma and Caski cells supernatant-derived exosomes. B, Blank; (1) Plasma-derived exosomes; (2) Caski cells; (3) Positive control (cervical HPV DNA positive cytological samples); M, Marker. The PCR assay was performed with MY11/09 primers (A). Nucleotide blast of HPV DNA amplified product obtained from plasma-derived exosomes by MY11/09 primers (B). HCT116 and NCM460 cell lines were exposed to CasKi supernatant derived exosomes and analyzed by Digital PCR (QuantStudio® 3D Digital PCR System, Life Technologies) to determine the capability of exosomes to transfer viral genetic material to recipient cells. Caski cell line was established from a metastasis in the small bowel mesentery and contains HPV16 DNA integrated into the genome. The reaction was performed using TaqMan Assay specific for HPV 16 E1 (Vi03453396_s1, Invitrogen, Milan, Italy). After 6 h of exposure the load of HPV DNA was greater than at 20 h in the normal human colon epithelial cell line (NCM460). In the human colon cancer cell line (HCT116) we report an HPV DNA burst at 6 h and a rapid decay, indeed it was absent at 20 h post exposure. (1) HCT116 at 3 h; (2) HCT116 at 6 h; (3) HCT116 at 20 h; (4) NCM460 at 3 h; (5) NCM460 at 6 h; (6) NCM4 60 at 20 h (C). The specimens illustrated in (C) were also amplified by conventional PCR with E6 HPV 16 specific primer pair showing concordant results with Digital PCR. B, Blank, (1) not exposed HCT116; (2) HCT116 at 3 h; (3) HCT116 at 6 h; (4) HCT116 at 20 h; (5) not exposed NCM460; (6) NCM460 at 3 h; (7) NCM460 at 6 h; (8) NCM460 at 20 h; (9) blank; (10) HPV DNA negative cervical specimen; (11) HPV DNA positive cervical specimen (D). The neoplastic and the neighbor cells demonstrated HPV DNA in the endothelial cells (red arrow) and in the fibroblasts (black arrow) by both CISH (brown chromogen) (E) and p16 IHC (E, inset). E, (E)-inset, original magnification 20x.
Microenvironment Characterization
More recently, local immune evasion has been involved in the development of gut cancer (20–22). Thus, we studied the neoplastic and non-neoplastic microenvironment of our patient by single and multiple IHC stainings. Interestingly, we demonstrated an increase of PDL-1 and PDL-2 expression in neoplastic cells coupled by PD-1 positivity of the reactive cells in the background (Figures 5A–C). This finding reflects a neoplastic environment with a reduced immune surveillance; in fact, the PD-1/PD-L1 molecular pathway can act to fine-tune the cellular fate of tumor-infiltrating T-cells. Interestingly, we detected an increase of T-regulatory cells (CD25/CD4/FOXP-3 positive) and a number of exhausted T-lymphocytes (CD8/PD-1 positive) in the neoplastic microenvironment when compared to non-neoplastic mucosa (Figures 5D,E). In addition, polarization of tumor-associated macrophages to an M2 phenotype was observed. In fact, the CD163/CD68 ratio was significantly higher in tumor than in non-neoplastic tissue (Figures 5F,G) (23) (Table 3).
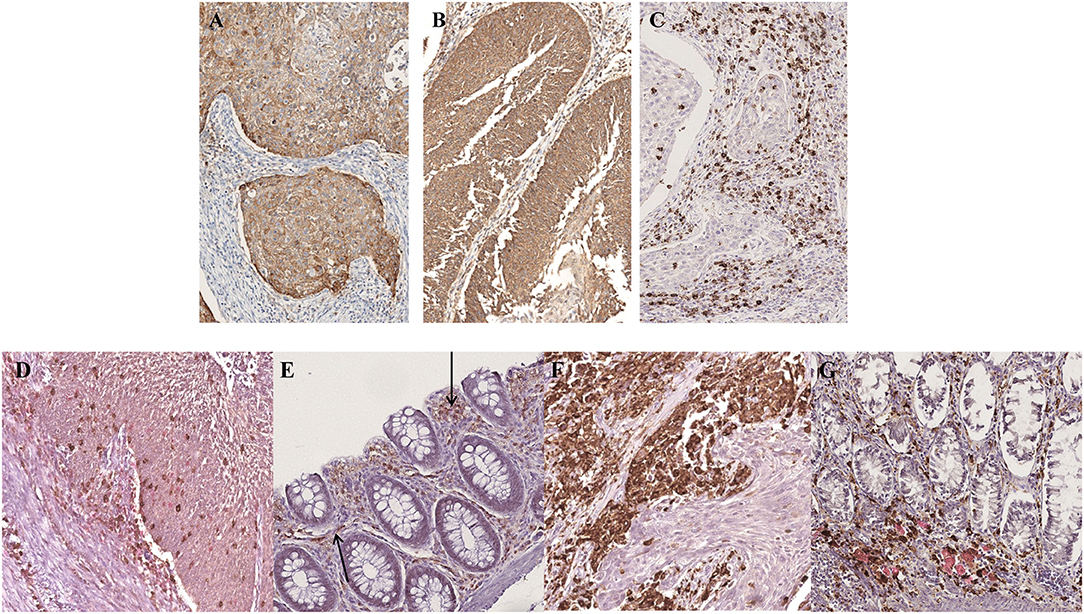
Figure 5. Microenvironment characterization. An increase of PDL-1 and PDL-2 expression in neoplastic cells was observed (A,B) whereas the reactive background showed a higher percentage of PD-1 positive elements (C). The tumor infiltrating lymphocytes were represented mainly by CD8/PD-1 positive T-cells (D) which were absent in normal mucosa (E). An increase of CD163/CD68-positive macrophages ratio was detected in the neoplastic component (F) as compared to the normal one (G). (A) PDL-1 staining; (B) PDL-2 staining; (C) PD-1 staining; (D,E) CD8/PD-1 double staining (CD8 brown, PD-1 red); (F,G) CD163/CD68 double staining (CD163 brown, CD68 red). (A–G), original magnification 20x.
Discussion
Previous studies on HPV in CRC are conflicting (24). While some of them report HPV DNA in 31 −53% of CRC, others identified no HPV DNA (25, 26). Moreover, some Authors recognized transcriptional activity of the HPV E6/E7 oncogenes critical to HPV's role in carcinogenesis, while others not (27–29). In our case study, HPV nucleic acids were detected in the neoplastic cells and in the normal crypts of the margins, non-neoplastic mucosa, random biopsies of the left and right colon as well as in some lymph nodes. It is known that inactivation of the E2 gene through genomic integration promotes the expression of the E6 and E7 oncoproteins, which induce a loss of cell-cycle control by antagonizing the function of p53 and Rb, respectively (30). The resulting degradation of p53 and Rb mediated by these oncoproteins facilitates viral DNA proliferation within the host and leads to neoplasia (31). Accordingly, in our case we detected viral integration by p16 IHC, CISH, and RNA ISH for E6/E7 mRNA only in neoplastic cells coupled with no expression of p53, p21, and Rb. This supports the view that HPV might be involved in tumorigenesis, rather than simply representing a fortuitous or chance passenger through tissues. Interestingly, we did not find the virus in its physiologic ports of entry (i.e., oral and ano-genital region). This, along with the wide anatomical distribution of HPV in our samples implies that the infection was not just the result of a retrograde viral transmission from the ano-genital area. However, we cannot exclude that a past productive infection could has been the primary source of the widespread infection in our patient.
Previous studies on cervical, oropharingeal, and breast diseases demonstrated the presence of circulating HPV DNA in the blood of affected patients (8, 32–35). Accordingly, we searched HPV DNA also in the blood of our patient. Intriguingly, it was present in the CD9-positive fraction of the plasma, namely the exosomes fraction. Then, we demonstrated by in vitro studies that HPV DNA positive exosomes are capable to transfer the viral nucleic acids to HPV DNA negative cells, such as normal and transformed colon cell lines. In vivo, we observed a horizontal transfer of HPV DNA by a cell to cell communication mechanism to stromal cells (endothelial cells and fibroblasts) as well as at distant sites (ascending/descending colon). It is reasonable that HPV penetrated in the host by one of the known site of entry. Following, the virus disappeared from the original site thanks to clearing mechanisms (that are highly active during the early phase of HPV infection) and it was no more detectable there (2). HPV entered the blood circulation via exosomes with shedding of nucleic acids in target tissues (7–16). It is conceivable that the virus has elicited its oncogenic effect (as demonstrated by the lack of p53, p21, and Rb expression by IHC) specifically in the middle rectum for a temporary condition of immune evasion (36) characterized by up-regulation of T-regulatory and T-exhausted lymphocytes and a polarization of tumor-associated macrophages with a switching from M1 to M2 (17–19, 37) as demonstrated by IHC. Moreover, we showed high expression of PDL-1 and PDL-2 by neoplastic cells and strong positivity of the reactive background to PD-1. It is also possible that the virus by itself induces an immunomodulation as previously demonstrated for other viruses (37, 38). Notably, we identified the reservoir of HPV in non-neoplastic epithelial cells within the crypts of colonic normal mucosa adjacent to the neoplastic mucosa and we demonstrated that these cells were stem-cells, which are known to be susceptible to transformation by HPV 16 (39, 40). It can be argued that following inflammatory response to a number of stimuli (also including dysbiosis) (41), non-cancer stem cells may be activated into cancer stem cells, sustaining a feed-forward circuit of self-renewal, proliferation, differentiation and neoplastic transformation in a condition of immune evasion, as previously demonstrated (40, 42–44). Due to the pluripotency of stem-cells, a squamous cell carcinoma may arise also in colorectal mucosa in the absence of any metaplastic changes, as in our case.
Concluding Remarks
Although important studies have been made for the understanding of HPV tumorigenicity in non-genital cancers, significant questions still remain. Our case-study seems to highlight the direct relationship of HPV with the pathogenesis of a squamous cell CRC; however, further studies including case control and cohort studies are necessary to evidence the causal link between HPV infection and colon cancer. The presence of HPV DNA positive plasma-derived exosomes in our patient shed important light on poorly understood mechanisms of HPV DNA horizontal transfer and on unconventional route of HPV spreading and carcinogenesis. It is noteworthy that HPV-induced cancerogenesis has a long-lasting history and our findings depicted only a static picture of a dynamic process for which we cannot exclude the development of cancers in other anatomic sites of the patient after viral spreading and DNA integration.
Author Contributions
MRA, MC, and SL conceived and developed the study. LM, SDC, AC, AG, and BJR performed experiments. MC, MRA, SL, and SDC analyzed data. RV, ALF, TC, and VN collected and provided patient samples. MC, SL, MRA, and PT wrote the paper. PT provided his experience in fruitful discussion. All the authors discussed the results and commented on the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Kurelac I, Salfi NC, Ceccarelli C, Alessandrini F, Cricca M, Caliceti U, et al. Human papillomavirus infection and pathogenic mitochondrial DNA mutation in bilateral multinodular oncocytic hyperplasia of the parotid. Pathology (2014) 46:250–3. doi: 10.1097/PAT.0000000000000079
2. Ambrosio MR, Onorati M, Rocca BJ, Santopietro R. Vulvar cancer and HPV infection: analysis of 22 cases. Pathologica (2008) 100:405–7.
3. Vidone M, Alessandrini F, Marucci G, Farnedi A, De Biase D, Ricceri F, et al. Evidence of association of human papillomavirus with prognosis worsening in glioblastoma multiforme. Neuro Oncol. (2014) 16:298–302. doi: 10.1093/neuonc/not140
4. Chen XZ, Waterboer T, Castro FA, Brenner H. Viral infections and colorectal cancer: a systematic review of epidemiological studies. Int J Cancer (2015) 137:12–24. doi: 10.1002/ijc.29180
5. Jeannot E, Becette V, Campitelli M, Calméjane MA, Lappartient E, Ruff E, et al. Circulating human papillomavirus DNA detected using droplet digital PCR in the serum of patients diagnosed with early stage human papillomavirus-associated invasive carcinoma. J Pathol Clin Res. (2016) 2:201–9. doi: 10.1002/cjp2.47
6. Dahlstrom KR, Li G, Hussey CS, Vo JT, Wei Q, Zhao C, et al. Circulating human papillomavirus DNA as a marker for disease extent and recurrence among patients with oropharyngeal cancer. Cancer (2015) 121:3455–64. doi: 10.1002/cncr.29538
7. Guenat D, Hermetet F, Prétet JL, Mougin C. Exosomes and other extracellular vesicles in HPV transmission and carcinogenesis. Viruses (2017) 9:E211. doi: 10.3390/v9080211
8. De Carolis S, Pellegrini A, Santini D, Ceccarelli C, De Leo A, Alessandrini F, et al. Liquid biopsy in the diagnosis of HPV DNA in breast lesions. Fut Microbiol. (2018) 13:187–94. doi: 10.2217/fmb-2017-0145
9. Zandberg DP, Bhargava R, Badin S, Cullen KJ. The role of human papillomavirus nongenital cancers. CA Cancer J Clin. (2013) 63:57–81. doi: 10.3322/caac.21167
10. Damin DC, Ziegelmann PK, Damin AP. Human papillomavirus infection and colorectal cancer risk: a meta-analysis. Colorectal Dis. (2012) 15:e420–8. doi: 10.1111/codi.12257
11. Kassir R, Baccot S, Bouarioua N, Petcu CA, Dubois J, Boueil-Bourlier A, et al. Squamous cell carcinoma of middle rectum: literature review. Int J Surg Case Rep. (2014) 5:86–90. doi: 10.1016/j.ijscr.2013.12.011
12. Williams GT, Blackshaw AJ, Morson BC. Squamous carcinoma of the colorectum and its genesis. J Pathol. (1979) 129:139–47. doi: 10.1002/path.1711290306
13. Ozuner G, Aytac E, Gorgun E, Bennett A. Colorectal squamous cell carcinoma: a rare tumor with poor prognosis. Int J Colorectal Dis. (2015) 30:127–30. doi: 10.1007/s00384-014-2058-9
14. Wang JF, Wang ZX, Xu XX, Wang C, Liu JZ. Primary rectal squamous cell carcinoma treated with surgery and radiotherapy. World J Gastroenterol. (2014) 20:4106–9. doi: 10.3748/wjg.v20.i14.4106
15. Guerra GR, Kong CH, Warrier SK, Lynch AC, Heriot AG, Ngan SY. Primary squamous cell carcinoma of the rectum: an update and implications for treatment. World J Gastrointest Surg. (2016) 8:252–65. doi: 10.4240/wjgs.v8.i3.252
16. Samana B, Lipsker D, Boehm N. p16 expression in relation to human papillomavirus in anogenital lesions. Hum Pathol. (2006) 37:513–9. doi: 10.1016/j.humpath.2006.01.001
17. Manos MM, Ting Y, Wright DK, Lewis AJ, Broker TR, Wolinsky SM. The use of polymerase chain reaction amplification for the detection of genital human papillomaviruses. Cancer Cells (1989) 7:209–14.
18. Zappacosta R, Colasante A, Viola P, D'Antuono T, Lattanzio G, Capanna S, et al. Chromogenic in situ hybridization and p16/Ki67 dual staining on formalin-fixed paraffin-embedded cervical specimens: correlation with HPV-DNA test, E6/E7 mRNA test, and potential clinical applications. Biomed Res Int. (2013) 2013:453606. doi: 10.1155/2013/453606
19. Evans MF, Peng Z, Clark KM, Adamson CS, Ma XJ, Wu X, et al. HPV E6/E7 RNA in situ hybridization signal patterns as biomarkers of three-tier cervical intraepithelial neoplasia grade. PLoS ONE (2014) 9:e91142. doi: 10.1371/journal.pone.0091142
20. Gopalakrishnan V, Helmink BA, Spencer CN, Reuben A, Wargo JA. The influence of the gut microbiome on cancer, immunity, and cancer immunotherapy. Cancer Cell (2018) 33:570–80. doi: 10.1016/j.ccell.2018.03.015
21. Zitvogel L, Galluzzi L, Viaud S, Vétizou M, Daillère R, Merad M, et al. Cancer and the gut microbiota: an unexpected link. Sci Transl Med. (2015) 7:271ps1. doi: 10.1126/scitranslmed.3010473
22. Schwabe RF, Jobin C. The microbiome and cancer. Nat Rev Cancer (2013) 13:800–12. doi: 10.1038/nrc3610
23. Weber M, Moebius P, Büttner-Herold M, Amann K, Preidl R, Neukam FW, et al. Macrophage polarisation changes within the time between diagnostic biopsy and tumour resection in oral squamous cell carcinomas—an immunohistochemical study. Br J Cancer (2015) 113:510–9. doi: 10.1038/bjc.2015.212
24. Audeau A, Han HW, Johnston MJ, Whitehead MW, Frizelle FA. Does human papilloma virus have a role in squamous cell carcinoma of the colon and upper rectum? Eur J Surg Oncol. (2002) 28:657–60. doi: 10.1053/ejso.2002.1304
25. Pelizzer T, Dias CP, Poeta J, Torriani T, Roncada C. Colorectal cancer prevalence linked to human papillomavirus: a systematic review with meta-analysis. Rev Bras Epidemiol. (2016) 19:791–802. doi: 10.1590/1980-5497201600040009
26. Lorenzon L, Mazzetta F, Pilozzi E, Uggeri G, Torrisi MR, Ferri M, et al. Human papillomavirus does not have a causal role in colorectal carcinogenesis. World J Gastroenterol. (2015) 21:342–50. doi: 10.3748/wjg.v21.i1.342
27. Bodaghi S, Yamanegi K, Xiao SY, Da Costa M, Palefsky JM, Zheng ZM. Colorectal papillomavirus infection in patients with colorectal cancer. Clin Cancer Res. (2005) 11:2862–7. doi: 10.1158/1078-0432.CCR-04-1680
28. Sotlar K, Köveker G, Aepinus C, Selinka HC, Kandolf R, Bültmann B. Human papillomavirus type 16-associated primary squamous cell carcinoma of the rectum. Gastroenterology (2001) 120:988–94.
29. Bernabe-Dones RD, Gonzalez-Pons M, Villar-Prados A, Lacourt-Ventura M, Rodríguez-Arroyo H, Fonseca-Williams S. High prevalence of human papillomavirus in colorectal cancer in hispanics: a case-control study. Gastroenterol Res Pract. (2016) 2016:7896716. doi: 10.1155/2016/7896716
30. Narisawa-Saito M, Kiyono T. Basic mechanisms of high-risk human papillomavirus-induced carcinogenesis: roles of E6 and E7 proteins. Cancer Sci. (2007) 98:1505–11. doi: 10.1111/j.1349-7006.2007.00546.x
31. Chen T, Huang CC, Yeh KT, Chang SH, Chang SW, Sung WW, et al. Human papilloma virus 16 E6 oncoprotein associated with p53 inactivation in colorectal cancer. World J Gastroenterol. (2012) 18:4051–8. doi: 10.3748/wjg.v18.i30.4051
32. Mazurek AM, Rutkowski T, Snietura M, Pigłowski W, Suwinski R, Składowski K. Detection of circulating HPV16 DNA as a biomarker in the blood of patients with human papillomavirus-positive oropharyngeal squamous cell carcinoma. Head Neck (2018). doi: 10.1002/hed.25368. [Epub ahead of print].
33. Jensen KK, Grønhøj C, Jensen DH, von Buchwald C. Circulating human papillomavirus DNA as a surveillance tool in head and neck squamous cell carcinoma: a systematic review and meta-analysis. Clin Otolaryngol. (2018) 43:1242–9. doi: 10.1111/coa.13136
34. Lee JY, Garcia-Murillas I, Cutts RJ, De Castro DG, Grove L, Hurley T, et al. Predicting response to radical (chemo)radiotherapy with circulating HPV DNA in locally advanced head and neck squamous carcinoma. Br J Cancer (2017) 117:876–83. doi: 10.1038/bjc.2017.258
35. Bodaghi S, Wood LW, Roby G, Ryder C, Steinberg SM, Zheng ZM. Could human papillomaviruses be spread through blood? J Clin Microbiol. (2005) 43:5428–34. doi: 10.1128/JCM.43.11.5428-5434.2005
36. Zitvogel L, Ayyoub M, Routy B, Kroemer G. Microbiome and anticancer immunosurveillance. Cell (2016) 165:276–87. doi: 10.1016/j.cell.2016.03.001
37. Garziera M, Toffoli G. Inhibition of host immune response in colorectal cancer: human leukocyte antigen-G and beyond. World J Gastroenterol. (2014) 20:3778–94. doi: 10.3748/wjg.v20.i14.3778
38. Morales-Sánchez A, Fuentes-Panana EM. The immunomodulatory capacity of an epstein-barr virus abortive lytic cycle: potential contribution to viral tumorigenesis. Cancers (2018) 10:98. doi: 10.3390/cancers10040098
39. Woappi Y, Hosseinipour M, Creek KE, Pirisi L. Stem cell properties of normal human keratinocytes determine transformation responses to human papillomavirus 16 DNA. J Virol. (2018) 92:e00331–18. doi: 10.1128/JVI.00331-18
40. Barker N, Van de Wetering M, Clevers H. The intestinal stem cell. Genes Dev. (2008) 22:1856–64. doi: 10.1101/gad.1674008
41. Wojciech K, Maria WC, Jan K, Wojciech W, Dorota K, Anna K, et al. Microbiota dysbiosis is associated with HPV-induced cervical carcinogenesis. Oncol Lett. (2018) 16:7035–47. doi: 10.3892/ol.2018.9509
42. Umar S. Intestinal stem cell. Curr Gastroenterol Rep. (2010) 12:340–8. doi: 10.1007/s11894-010-0130-3
43. Hou Q, Ye L, Huang L, Yu Q. The research progress on intestinal stem cells and its relationship with intestinal microbiota. Front Immunol. (2017) 8:599. doi: 10.3389/fimmu.2017.00599
Keywords: circulating HPV, immune evasion, exosomes, middle rectum, cancer
Citation: Ambrosio MR, Vernillo R, De Carolis S, Carducci A, Mundo L, Ginori A, Rocca BJ, Nardone V, Lucenti Fei A, Carfagno T, Lazzi S, Cricca M and Tosi P (2019) Putative Role of Circulating Human Papillomavirus DNA in the Development of Primary Squamous Cell Carcinoma of the Middle Rectum: A Case Report. Front. Oncol. 9:93. doi: 10.3389/fonc.2019.00093
Received: 19 November 2018; Accepted: 01 February 2019;
Published: 21 February 2019.
Edited by:
Konrad Steinestel, Bundeswehrkrankenhaus Ulm, GermanyReviewed by:
Guglielmina Nadia Ranzani, University of Pavia, ItalyPaolo Giorgi Rossi, Azienda Sanitaria Unità Locale di Reggio Emilia, Italy
Copyright © 2019 Ambrosio, Vernillo, De Carolis, Carducci, Mundo, Ginori, Rocca, Nardone, Lucenti Fei, Carfagno, Lazzi, Cricca and Tosi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stefano Lazzi, lazzi2@unisi.it
Monica Cricca, monica.cricca3@unibo.it
 Maria Raffaella Ambrosio
Maria Raffaella Ambrosio Remo Vernillo2
Remo Vernillo2 Sabrina De Carolis
Sabrina De Carolis Antonietta Carducci
Antonietta Carducci Lucia Mundo
Lucia Mundo Valerio Nardone
Valerio Nardone Stefano Lazzi
Stefano Lazzi Monica Cricca
Monica Cricca Piero Tosi
Piero Tosi